Abstract
Purpose
This study presents our initial experience with endoscopic combined intrarenal surgery (ECIRS) for large renal stones and compares the results of a propensity score-matched cohort of patients undergoing shock-wave lithotripsy (SWL).
Materials and Methods
A total of 100 adults underwent ECIRS for renal stones between August 2017 and January 2019. For comparison, 2172 patients who underwent a first session of SWL between January 2005 and May 2018 were included in the SWL cohort. Propensity score matching was performed using maximal stone length (MSL), mean stone density (MSD), and stone heterogeneity index (SHI) scores. Stone-free rate (SFR) and success rate were compared between ECIRS and SWL.
Results
In the ECIRS group, the mean MSL, mean MSD, and mean SHI were 28.7±15.2 mm, 1013.9±360.0 Hounsfield units (HU), 209.4±104.0 HU, respectively. The SFR was 70%, and the success rate was 82.0% in this group. Although the ECIRS group had larger, harder, and more homogeneous stones than the SWL group, ECIRS showed a higher SFR and success rate than SWL. After propensity-score matching, SFR and success rate remained higher with ECIRS than with SWL (both, p<0.001). In multivariate logistic regression, smaller stone size [odds ratio (OR): 0.947, 95% confidence interval (CI): 0.913–0.979, p=0.002] and lower Seoul National University Renal Stone Complexity score (OR: 0.759, 95% CI: 0.610–0.935, p=0.011) were independent predictors of successful ECIRS.
Conclusion
ECIRS showed a higher SFR and success rate than SWL for large renal stones. Smaller stone size and lower complexity of stones were associated with a higher likelihood of successful ECIRS.
Keywords: Kidney, nephrolithiasis, lithotripsy, urinary calculi
INTRODUCTION
Improvements in renal access, optics, radiology, and lithotripsy have all contributed to the development of modern percutaneous nephrolithotomy (PCNL).1 In 1976, Fernström and Johannsson2 reported the first use of a novel technique for extracting renal stones using radiation-controlled percutaneous nephrostomy. Since then, PCNL has become widely used, and various methods of patient positioning have been suggested. In 1987, Valdivia Uría, et al.3 described the first supine PCNL, and in 1992, Ibarluzea, et al.4,5 reported the first use of a modified supine position [the Galdakao-modified supine Valdivia (GMSV) position] for PCNL. The Ibarluzea group was the first to perform simultaneous transurethral and percutaneous approaches in the GMSV position.
Endoscopic combined intrarenal surgery (ECIRS), which combines PCNL with retrograde ureteroscopy, was first described by Scoffone, et al.6 in 2008. A distinct advantage of ECIRS is its ability to produce higher stone-free rates (SFRs) than PCNL monotherapy.7,8 Thus, ECIRS has received much attention as a novel method of successfully treating complex renal stones.9 Recently, mini-ECIRS was introduced, using mini-PCNL for safer and more efficient ECIRS.10 The advent of digital flexible ureteroscopy has also contributed to the development of ECIRS.11 The aim of this study was to share our experience in maximizing the effectiveness of ECIRS for large renal stones in real-world practice. We also used propensity-score matching to investigate whether ECIRS produced better outcomes than shock-wave lithotripsy (SWL).
MATERIALS AND METHODS
ECIRS patient population and technique
We retrospectively created a database of patients who underwent ECIRS at Severance Hospital, Seoul, Korea. This database included the first 100 consecutive adults who underwent ECIRS between August 2017 and January 2019.
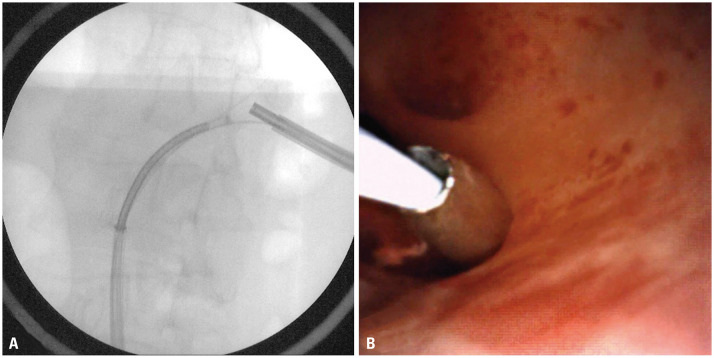
An interventional radiologist or urologic surgeon (JYL) performed calyceal puncture using fluoroscopic or ultrasonic guidance before surgery or during the same session as ECIRS. ECIRS was performed with the patient receiving general anesthesia and placed in the GMSV position. In this position, the patient was placed in a slightly lateral position, with a 1-L bag of normal saline inserted under the ipsilateral flank. Therefore, the ipsilateral flank was elevated approximately 20 degrees, and the posterior calyx was located more laterally.12 A retrograde 11/13-Fr ureteral access sheath was inserted over an Amplatz Super Stiff guidewire (Boston Scientific, Marlborough, MA, USA). After visualizing and confirming the entry point in the collecting system with the flexible ureteroscope, the tract was safely punctured with a Chiba needle under ultrasound guidance and/or dilated using an 18-Fr balloon dilator (Ultraxx Nephrostomy Balloon Catheter; Cook Medical, Bloomington, IN, USA), a 15/16-Fr single-step dilator (MIP-M, Karl Storz Endoskope, Tuttlingen, Germany), or a 24-Fr or 30-Fr balloon dilator (NephroMax; Boston Scientific). Either a 24-Fr nephroscope (Richard Wolf, Knittlingen, Germany) or a 12-Fr mini-nephroscope (Karl Storz Endoskope and Richard Wolf) was used (Fig. 1).
Fig. 1. Percutaneous track formation. (A) The nephroscope and flexible ureterorenoscope were inserted in close proximity so they could visualize each other. (B) Under flexible ureteroscopic visualization, a one-step dilator was inserted into the intrarenal space.
SWL cohort and technique
We retrospectively created a database of 2172 patients who underwent their first session of SWL at our institute from January 2005 to May 2018. Ultimately, 439 patients with renal stones were eligible for the propensity-score matching analysis.
SWL was performed using electroconductive and electromagnetic generative lithotripters (EDAP Sonolith Praktis, Technomed, Lyon, France; Dornier Compact Delta II crushers, Dornier Medtech, Wesling, Germany), with fluoroscopic visualization. The number of shock waves per SWL session varied from 2500 to 4000, which were administered at a rate of 60–90 shock waves per minute. If the stone was difficult to identify during SWL, the session was terminated prematurely. Launch intensity was established such that the peak focal pressure was in the range of 16–55 MPa, as determined by the patients’ reported pain levels during SWL.
Baseline patient and stone characteristics
The following data were collected for inclusion in the databases: patient characteristics (including demographics), detailed history of urolithiasis (including time of pain onset), and stone characteristics [maximal stone length (MSL), stone heterogeneity index (SHI), skin-to-stone distance (SSD), and mean stone density (MSD)]. The stone characteristics were obtained from three-dimensional measurements of non-contrast computed tomography (NCCT) images, using the GE Centricity System (GE Healthcare Bio-Sciences Corp., Piscataway, NJ, USA). MSD was measured using bone windows of enlarged axial NCCT images of stones at their maximum diameter: the elliptical area of interest incorporated the maximum cross-sectional area of the stone, not including the adjacent soft tissue.13 SHI was the standard deviation of Hounsfield units (HU) for the same region.14 Stone complexity was described by calculating Seoul National University Renal Stone Complexity (S-ReSC) and modified S-ReSC scores.15,16
Treatment outcomes were recorded, including complication rates and post-treatment complications (hemoglobin change, creatinine change, estimated glomerular filtration rate change). Successful treatment was defined as no residual stone (stone-free) or a clinically insignificant, asymptomatic residual fragment with a maximum diameter of 3 mm at 3 months after treatment (measured by plain X-ray),17 as well as the lack of need for additional treatment during 3 months of follow-up.
Statistical analyses
Data are expressed as means±standard deviations, except where otherwise indicated. After analyzing the entire cohort, propensity score-matched analysis was performed to further characterize patients with renal stones. Each ECIRS patient was matched 1:1 with the closest SWL patient. Propensity scores were calculated using logistic regression with multivariate analysis based on MSL, MSD, and SHI with binomial methods. This propensity score-matching improved matching according to stone characteristics, thus providing better comparison groups.18 With propensity scores, the conditional distribution of preprocessing characteristics was the same between the two groups.19
Patient baseline characteristics were compared using Student’s or Welch’s two-sample t-test for continuous variables and the Pearson chi-square test with Yates’ continuity correction for categorical variables. We performed univariate and multivariate logistic regression analyses using the binomial method to identify factors significantly associated with successful treatment.
Statistical analyses were performed using R software (version 4.1.1, R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org) and its MatchIt package for propensity score matching.
Ethics statement
The protocol for this study was reviewed and approved by the Institutional Review Board of our medical institute (Approval No. 4-2021-0941). The review board deemed the study exempt from the requirement for written informed consent from the participants because the design was retrospective and all patient data were anonymized prior to analysis.
RESULTS
Baseline characteristics and procedure success rates
Of the 100 ECIRS patients, 64 were male and 36 were female. The mean age was 56.8±14.5 years. The treated stones were on the right in 39 patients and on the left in 61 patients. Eight patients underwent ipsilateral ureteroscopic surgery. In 14 patients, contralateral retrograde intrarenal surgery (RIRS) was performed simultaneously with ECIRS. Multiple stones were present in 75 patients. The mean MSL was 28.7±15.2 mm, mean MSD was 1013.9±360.0 HU, and mean SHI was 209.4±104.0 HU. The SFR was 70%, and the success rate was 82.0% in the ECIRS group.
Of the 439 patients in the SWL group, 263 were male and 176 were female. The mean age was 52.3±14.4 years. The mean MSL was 12.7±10.5 mm, mean MSD was 815.6±338.9 HU, and mean SHI was 244.9±109.4 HU. The mean SSD was 76.88±20.47 mm. The SFR was 52.8%, and the success rate was 67.7% in the SWL group.
Comparison of total ECIRS and SWL cohorts
Table 1 compares the ECIRS and SWL groups when considering all patients, before propensity-score matching. Age (p=0.006), MSL (p<0.001), MSD (p<0.001), and SHI (p<0.003) differed significantly between the groups. Stones were larger, harder, and more homogeneous in the ECIRS group than in the SWL group. SFR and success rates were higher in the ECIRS group than in the SWL group (p=0.003 and 0.007, respectively).
Table 1. Baseline Characteristics and Treatment Outcomes of SWL vs. ECIRS.
| Characteristics | SWL group (n=439) | ECIRS group (n=100) | p value | |
|---|---|---|---|---|
| Age (yr) | 52.3±14.4 | 56.8±14.5 | 0.006 | |
| Sex | 0.521 | |||
| Female | 176 (40.1) | 36 (36.0) | ||
| Male | 263 (59.9) | 64 (64.0) | ||
| MSL (mm) | 12.7±10.5 | 28.7±15.2 | <0.001 | |
| MSD (HU) | 815.6±338.9 | 1013.9±360.0 | <0.001 | |
| SHI (HU) | 244.9±109.4 | 209.4±104.0 | 0.003 | |
| SFR | 232 (52.8) | 70 (70.0) | 0.003 | |
| Success rate | 297 (67.7) | 82 (82.0) | 0.007 | |
| Multiple stones | - | 75 (75) | ||
| Operating room time (min) | - | 82.23±35.68 | ||
| LOS (day) | - | 2 (1–3) | ||
| Hemoglobin change | - | -1.21±1.17 | ||
| Creatinine change | - | 0.058±0.30 | ||
| eGFR change | - | -1.19±18.15 | ||
SWL, shock-wave lithotripsy; ECIRS, endoscopic combined intrarenal surgery; MSL, maximal stone length; MSD, mean stone density; HU, Hounsfield units; SHI, stone heterogeneity index; SFR, stone-free rate; LOS, length of stay; eGFR, estimated glomerular filtration rate.
Data are presented as means±standard deviations, numbers (percentage), or medians (interquartile range).
Comparison of propensity score-matched ECIRS and SWL cohorts
After propensity score matching, there were 70 patients in each group. There were no significant differences in age (p=0.170), sex (p>0.999), MSL (p=0.331), MSD (p=0.229), or SHI (p=0.376) between the propensity score-matched groups. There were also no significant differences in S-ReSC and modified S-ReSC scores between the groups (p=0.354; p=0.330). SFR and success rates remained significantly higher with ECIRS than with SWL after propensity-score matching (p<0.001 for both comparisons) (Table 2).
Table 2. Baseline Characteristics and Treatment Outcomes of SWL vs. ECIRS Groups after Propensity Score Matching.
| Characteristics | SWL group (n=70) | ECIRS group (n=70) | p value | |
|---|---|---|---|---|
| Age (yr) | 53.6±14.6 | 56.9±13.5 | 0.170 | |
| Sex | >0.999 | |||
| Female | 27 (38.6) | 26 (37.1) | ||
| Male | 43 (61.4) | 44 (62.9) | ||
| MSL (mm) | 21.4±13.2 | 23.7±13.9 | 0.331 | |
| MSD (HU) | 1082.6±488.9 | 995.5±352 | 0.229 | |
| SHI (HU) | 202.3±91.1 | 217.2±107.5 | 0.376 | |
| SFR | 20 (28.6) | 50 (71.4) | <0.001 | |
| Success rate | 29 (41.4) | 61 (87.1) | <0.001 | |
| S-ReSC score | 4.73±11.62 | 3.41±20.5 | 0.354 | |
| Modified S-ReSC score | 6.54±11.61 | 5.14±2.78 | 0.330 | |
| Multiple stones | - | 47 (67.1) | ||
| Operating room time (min) | - | 73.14±28.23 | ||
| LOS (day) | - | 2 (1.25–2) | ||
| Hemoglobin change | - | -1.05±1.26 | ||
| Creatinine change | - | 0.07±0.35 | ||
| eGFR change | - | -3.83±12.30 | ||
SWL, shock-wave lithotripsy; ECIRS, endoscopic combined intrarenal surgery; MSL, maximal stone length; MSD, mean stone density; HU, Hounsfield units; SHI, stone heterogeneity index; SFR, stone-free rate; S-ReSC, Seoul National University Renal Stone Complexity; LOS, length of stay; eGFR, estimated glomerular filtration rate.
Data are presented as means±standard deviations, numbers (percentage), or medians (interquartile range).
Predictive factors of successful ECIRS
Univariate and multivariate analyses with logistic regression models were conducted to identify predictors of successful ECIRS. Multivariate analysis showed that smaller stone size [odds ratio (OR): 0.947, 95% confidence interval (CI): 0.913–0.979, p=0.002] and lower S-ReSC score (OR: 0.759, 95% CI: 0.610–0.935, p=0.011) were independent predictors of successful ECIRS (Table 3).
Table 3. Logistic Regression Analyses of Factors Associated with Successful ECIRS.
| Variables | Odds ratio | 95% CI | p value | |
|---|---|---|---|---|
| Univariate analysis | ||||
| Age | 1.039 | 1.003–1.079 | 0.039 | |
| BMI | 1.047 | 0.901–1.227 | 1.079 | |
| MSL | 0.943 | 0.909–0.975 | <0.001 | |
| MSD | 0.999 | 0.998–1.001 | 0.297 | |
| SHI | 0.997 | 0.992–1.002 | 0.311 | |
| S-ReSC score | 0.747 | 0.602–0.914 | 0.005 | |
| Multiplicity | 0.321 | 0.048–1.249 | 0.150 | |
| Multivariate analysis with age and MSL | ||||
| Age | 1.031 | 0.994–1.073 | 0.108 | |
| MSL | 0.947 | 0.913–0.979 | 0.002 | |
| Multivariate analysis with age and S-ReSC score | ||||
| Age | 1.032 | 0.996–1.073 | 0.087 | |
| S-ReSC score | 0.759 | 0.610–0.935 | 0.011 | |
ECIRS, endoscopic combined intrarenal surgery; CI, confidence interval; BMI, body mass index; MSL, maximal stone length; MSD, mean stone density; SHI, stone heterogeneity index; S-ReSC, Seoul National University Renal Stone Complexity.
DISCUSSION
ECIRS further enhances the advantages of PCNL and RIRS and allows the disadvantages of these procedures to be counterbalanced by the other procedure. Thus, ECIRS can be employed to effectively treat large renal stones through a synergistic approach combining RIRS and PCNL.20 Several studies have shown that ECIRS is an effective treatment for large renal stones. Wen, et al.21 compared ECIRS with mini-PCNL in the prone position for patients with partial staghorn calculi. They found a significantly higher SFR with ECIRS (87.88% vs. 58.82%, p=0.007) and no statistical difference in complications. Recently, Zhao, et al.22 also reported a higher SFR with ECIRS than with mini-PCNL (88.06% vs. 66.67%, p=0.003), as well as a lower (although not statistically significant) complication rate with ECIRS (7.5% vs. 16.0%, p=0.12).
In this study, we analyzed the initial 100 cases of ECIRS at our institute and compared the efficacy of ECIRS to that of SWL for large renal stones. Before propensity score matching, ECIRS was associated with a significantly higher SFR (70.0% vs. 52.8%, p=0.003) and success rate (82.0% vs. 67.7%, p=0.007), although stones in the ECIRS group had a higher MSL and MSD. After propensity score matching, ECIRS remained associated with a significantly higher SFR (71.4% vs. 28.6%, p<0.001) and one-session success rate (87.1% vs. 41.4%, p<0.001).
Large stones located in minor and major renal calyces require a variety of treatment approaches. After removing large stones through a percutaneous approach, removing small stones in other calyces creates additional percutaneous tracts, which can increase the risk of bleeding. In particular, when removing stones located in the mid-pole, an excessive angle for approaching these stones via lower or upper pole tracts increases the risk of perioperative bleeding. Thus, a flexible ureteroscope can be used to remove stones in other calyces far from the target calyx. This is one of most important advantages of ECIRS, contributing to its increased SFRs and decreased complication rates. Furthermore, when a ureter is completely obstructed by an impacted stone, a retrograde approach can be difficult because of severe kinking of the ureter. In this situation, the impacted stone can be more easily removed via a percutaneous approach.
We performed ECIRS in the GMSV position, which has the advantage of reducing the risk of prone-related anesthetic complications.23 Another advantage of this position is that it can enhance passive removal of stones by the washout mechanism.9 Renal puncture with retrograde flexible ureterorenoscopy can increase safety and effectiveness. The main disadvantages of ECIRS are increased costs and the need for more space because a second surgeon and additional equipment are required.9,24 The Urological Association of Asia guidelines note the following indications for ECIRS: renal stone >2 cm in diameter, with or without a large lower pole burden; renal stone with concomitant ureter stone; and renal stone >1 cm in diameter, with anatomic abnormalities (e.g., diverticular stones in horseshoe kidneys).25
Although the SWL group had a very low one-session success rate in the present study, SWL is generally accompanied by less frequent and less severe complications, compared to endoscopic treatment.26,27 Thus, SWL remains an important treatment option, despite the development of endourologic techniques. The European Association of Urology guidelines state that for large (>2 cm) renal stones, RIRS or SWL can be performed when PCNL is not an option, although they may require additional treatment sessions. SWL can be also performed for lower pole stones 1–2 cm in diameter if there are no unfavorable factors for SWL, such as a steep infundibular-pelvic angle, long calyx, long SSD, narrow infundibulum, or shock wave-resistant stones (calcium oxalate monohydrate, brushite, or cystine stones).24
SWL is the most common stone treatment in South Korea. Since the topic of this study was also our first 100 cases experience with ECIRS, it would be most appropriate to compare with SWL. With 200 cases or 300 cases, we think that the number of cases will be sufficient to compare ECIRS with PCNL or compare miniature and conventional procedures. For a fair comparison, we performed propensity-score matching to identify stones that are closest to 2 cm. After propensity-score matching, the mean MSL was 21.4±13.2 cm in the SWL group and 23.7±13.9 cm in the ECIRS group (p=0.331).
This study had some limitations. First, it was retrospective, and the sample size was relatively small. Second, we did not compare complications of ECIRS and SWL. The reason is that we could not identify the complications of SWL in our institute database. Third, we did not categorize the location of renal stones that impact SFR, although we evaluated S-ReSC and modified S-ReSC scores. However, the S-ReSC scoring system predicts the SFR after PCNL. S-ReSC scores denote the distributional complexity of renal stones by counting the number of sites (renal pelvis; superior and inferior major calyces; and the anterior and posterior minor calyces of the superior, middle, and inferior calyces).15 Also, the modified S-ReSC scoring system predicts the SFR after RIRS. The modified S-ReSC score was assigned according to the number of sites involved in the renal pelvis (#1); superior and inferior major calyceal groups (#2–3); and anterior and posterior minor calyceal groups of the superior (#4–5); middle (#6–7); and inferior calyx (#8–9). One point was given for each location, and then if a stone was involved in the inferior sites (#3, #8–9), one further point per site was added to the original score.16 To the best of our knowledge, however, this is the first study to directly compare the effectiveness of ECIRS and SWL. Prospective randomized trials with larger sample sizes are required to confirm the effectiveness and safety of ECIRS.
In conclusion, ECIRS was significantly more effective than SWL for large renal stones, producing a higher SFR and success rate. Smaller stone size and lower complexity of stones were associated with a higher likelihood of successful ECIRS.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Joo Yong Lee.
- Data curation: Young Joon Moon, Ali Abdullah Alqahtani, and Mohammed Ali Alkhureeb.
- Formal analysis: Hae Do Jung and Ahmad J. Almujalhem.
- Investigation: Hae Do Jung and Ahmad J. Almujalhem.
- Methodology: Hae Do Jung and Joo Yong Lee.
- Project administration: Joo Yong Lee.
- Resources: Joo Yong Lee.
- Software: Hae Do Jung and Young Joon Moon.
- Supervision: Joo Yong Lee.
- Validation: Joo Yong Lee.
- Visualization: Young Joon Moon, Ali Abdullah Alqahtani, and Mohammed Ali Alkhureeb.
- Writing—original draft: Hae Do Jung and Joo Yong Lee.
- Writing—review & editing: Joo Yong Lee.
- Approval of final manuscript: all authors.
References
- 1.Patel SR, Nakada SY. The modern history and evolution of percutaneous nephrolithotomy. J Endourol. 2015;29:153–157. doi: 10.1089/end.2014.0287. [DOI] [PubMed] [Google Scholar]
- 2.Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976;10:257–259. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 3.Valdivia Uría JG, Lachares Santamaría E, Villarroya Rodríguez S, Taberner Llop J, Abril Baquero G, Aranda Lassa JM. [Percutaneous nephrolithectomy: simplified technic (preliminary report)] Arch Esp Urol. 1987;40:177–180. [PubMed] [Google Scholar]
- 4.Ibarluzea G, Scoffone CM, Cracco CM, Poggio M, Porpiglia F, Terrone C, et al. Supine Valdivia and modified lithotomy position for simultaneous anterograde and retrograde endourological access. BJU Int. 2007;100:233–236. doi: 10.1111/j.1464-410X.2007.06960.x. [DOI] [PubMed] [Google Scholar]
- 5.Ibarluzea JG, Gamarra MG, Leibar A, Pereira JG. In: Supine percutaneous nephrolithotomy and ECIRS. Scoffone C, Hoznek A, Cracco C, editors. Paris: Springer; 2014. The evolution from prone to supine PNL and from supine PNL to ECIRS: the basque history of endourology; pp. 15–23. [Google Scholar]
- 6.Scoffone CM, Cracco CM, Cossu M, Grande S, Poggio M, Scarpa RM. Endoscopic combined intrarenal surgery in Galdakao-modified supine Valdivia position: a new standard for percutaneous nephrolithotomy? Eur Urol. 2008;54:1393–1403. doi: 10.1016/j.eururo.2008.07.073. [DOI] [PubMed] [Google Scholar]
- 7.Hamamoto S, Yasui T, Okada A, Taguchi K, Kawai N, Ando R, et al. Endoscopic combined intrarenal surgery for large calculi: simultaneous use of flexible ureteroscopy and mini-percutaneous nephrolithotomy overcomes the disadvantageous of percutaneous nephrolithotomy monotherapy. J Endourol. 2014;28:28–33. doi: 10.1089/end.2013.0361. [DOI] [PubMed] [Google Scholar]
- 8.Ping H, Zhang JH, Wang MS, Xing NZ. Endoscopic combined intrarenal surgery for the treatment of postpercutaneous nephrolithotomy residual stones. Chin Med J (Engl) 2016;129:2885–2887. doi: 10.4103/0366-6999.194659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung HD, Kim JC, Ahn HK, Kwon JH, Han K, Han WK, et al. Real-time simultaneous endoscopic combined intrarenal surgery with intermediate-supine position: washout mechanism and transport technique. Investig Clin Urol. 2018;59:348–354. doi: 10.4111/icu.2018.59.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwon O, Park J, Cho MC, Son H, Jeong H, Cho SY. Feasibility of single-session endoscopic combined intrarenal surgery for ipsilateral large renal stones and retrograde intrarenal surgery for contralateral renal stones: initial experience. Int J Urol. 2017;24:377–382. doi: 10.1111/iju.13313. [DOI] [PubMed] [Google Scholar]
- 11.Jeong JY, Kim JC, Kang DH, Lee JY. Digital videoscopic retrograde intrarenal surgeries for renal stones: time-to-maximal stone length ratio analysis. Yonsei Med J. 2018;59:303–309. doi: 10.3349/ymj.2018.59.2.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung DY, Lee JY, Kim KH, Choi JH, Cho KS. Feasibility and efficacy of intermediate-supine percutaneous nephrolithotomy: initial experience. Chonnam Med J. 2014;50:52–57. doi: 10.4068/cmj.2014.50.2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung DY, Cho KS, Lee DH, Han JH, Kang DH, Jung HD, et al. Impact of colic pain as a significant factor for predicting the stone free rate of one-session shock wave lithotripsy for treating ureter stones: a Bayesian logistic regression model analysis. PLoS One. 2015;10:e0123800. doi: 10.1371/journal.pone.0123800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee JY, Kim JH, Kang DH, Chung DY, Lee DH, Jung HD, et al. Stone heterogeneity index as the standard deviation of Hounsfield units: a novel predictor for shock-wave lithotripsy outcomes in ureter calculi. Sci Rep. 2016;6:23988. doi: 10.1038/srep23988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeong CW, Jung JW, Cha WH, Lee BK, Lee S, Jeong SJ, et al. Seoul National University Renal Stone Complexity Score for predicting stone-free rate after percutaneous nephrolithotomy. PLoS One. 2013;8:e65888. doi: 10.1371/journal.pone.0065888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jung JW, Lee BK, Park YH, Lee S, Jeong SJ, Lee SE, et al. Modified Seoul National University renal stone complexity score for retrograde intrarenal surgery. Urolithiasis. 2014;42:335–340. doi: 10.1007/s00240-014-0650-7. [DOI] [PubMed] [Google Scholar]
- 17.Seitz C, Tanovic E, Kikic Z, Memarsadeghi M, Fajkovic H. Rapid extracorporeal shock wave lithotripsy for proximal ureteral calculi in colic versus noncolic patients. Eur Urol. 2007;52:1223–1227. doi: 10.1016/j.eururo.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27:2037–2049. doi: 10.1002/sim.3150. [DOI] [PubMed] [Google Scholar]
- 19.Rubin DB, Thomas N. Matching using estimated propensity scores: relating theory to practice. Biometrics. 1996;52:249–264. [PubMed] [Google Scholar]
- 20.Cracco CM, Scoffone CM. ECIRS (Endoscopic Combined Intrarenal Surgery) in the Galdakao-modified supine Valdivia position: a new life for percutaneous surgery? World J Urol. 2011;29:821–827. doi: 10.1007/s00345-011-0790-0. [DOI] [PubMed] [Google Scholar]
- 21.Wen J, Xu G, Du C, Wang B. Minimally invasive percutaneous nephrolithotomy versus endoscopic combined intrarenal surgery with flexible ureteroscope for partial staghorn calculi: a randomised controlled trial. Int J Surg. 2016;28:22–27. doi: 10.1016/j.ijsu.2016.02.056. [DOI] [PubMed] [Google Scholar]
- 22.Zhao F, Li J, Tang L, Li C. A comparative study of endoscopic combined intrarenal surgery (ECIRS) in the galdakao-modified supine valdivia (GMSV) position and minimally invasive percutaneous nephrolithotomy for complex nephrolithiasis: a retrospective single-center study. Urolithiasis. 2021;49:161–166. doi: 10.1007/s00240-020-01207-5. [DOI] [PubMed] [Google Scholar]
- 23.Scoffone CM, Cracco CM. Invited review: the tale of ECIRS (Endoscopic Combined IntraRenal Surgery) in the Galdakao-modified supine Valdivia position. Urolithiasis. 2018;46:115–123. doi: 10.1007/s00240-017-1015-9. [DOI] [PubMed] [Google Scholar]
- 24.Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 25.Taguchi K, Cho SY, Ng AC, Usawachintachit M, Tan YK, Deng YL, et al. The Urological Association of Asia clinical guideline for urinary stone disease. Int J Urol. 2019;26:688–709. doi: 10.1111/iju.13957. [DOI] [PubMed] [Google Scholar]
- 26.Yang SY, Jung HD, Kwon SH, Lee EK, Lee JY, Lee SH. Does early retrograde intrarenal surgery improve the cost-effectiveness of renal stone management? Yonsei Med J. 2020;61:515–523. doi: 10.3349/ymj.2020.61.6.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang KD, Lee JY, Park SY, Kang DH, Lee HH, Cho KS. Impact of pretreatment hydronephrosis on the success rate of shock wave lithotripsy in patients with ureteral stone. Yonsei Med J. 2017;58:1000–1005. doi: 10.3349/ymj.2017.58.5.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]