Abstract
Context
A relationship between obesity and poor oral health has been reported.
Objective
To investigate the association between overweight/obesity and oral health in Mexican children and adolescents.
Data Sources
A literature search was conducted of 13 databases and 1 search engine for articles published from 1995 onward.
Data Analysis
A total of 18 publications were included. Evidence was inconclusive and varied according to sociodemographic factors or outcome measuring tools. The Decayed, Missing, and Filled Teeth and Filled Teeth Surfaces indices and the decayed extracted filled teeth index outcomes were included in a random effects model meta-analysis. Pooled estimates showed no statistically significant oral health differences (measured via the decayed extracted filled teeth or the Decayed, Missing, and Filled Teeth Surfaces indexes) among body mass index (BMI) categories. However, pooled estimates of 6 studies showed that children with higher BMI had worse oral health in permanent teeth (measured via the Decayed Missing Filled Teeth Index) than children with lower BMI (overall mean difference, –0.42; 95%CI, –0.74, –0.11).
Conclusion
Whether there is an association between poor oral health and high BMI is inconclusive; however, both co-exist among Mexican children. Therefore, health promotion and prevention efforts should address common risk factors and broader risk social determinants shared between noncommunicable diseases.
Keywords: adolescents, caries, children, obesity, oral health, Mexico
BACKGROUND
Oral health is an integral component of overall health and well-being, enabling vital daily functions.1,2 Dental caries (also known as tooth decay) is among the most prevalent oral chronic diseases affecting children and adolescents worldwide.3–6 Dental caries negatively affects children’s quality of life7 because of discomfort, pain, infection, or altered sleeping habits.1 Dental caries also might alter children’s normal growth and development and may increase the risk of hospitalization.5 It has been suggested that oral health outcomes might vary according to income, ethnicity, or other sociodemographic factors.6 Dental caries continues to be a public health problem, even with technological advancements and a better understanding of the carious process.1,8
Several studies have examined the relationship between overweight or obesity with children’s oral health, especially dental caries. Obesity and dental caries are 2 conditions that share several predisposing factors, such as unhealthy lifestyles, a diet high in sugar, sociodemographic characteristics, and other environmental factors.5–9 One of the most frequently studied factors is diet, mainly high consumption of sugar. Consuming high amounts of sugar might lead to both high body mass index (BMI) and a high prevalence of caries.3–8 Consequently, many researchers have hypothesized that excess weight might be linked with children’s dental caries. However, recent evidence suggests that any association between obesity and dental caries might vary according to different factors, including the country of the studied cohort’. The finding has been reported of significantly more caries among children with overweight or obesity (in both primary and permanent teeth) in high-income countries, but not those in low- and middle-income countries.9
Several individual studies and systematic reviews have recently evaluated the association between overweight or obesity and oral health outcomes (eg, caries).5,8–10 However, the results and methodologies are mixed and provided uncertain and inconclusive evidence. Furthermore, most of the published systematic reviews include only English-language publications, excluding valuable evidence from non–English-speaking or low- and middle-income countries, such as Mexico.
To our knowledge, no systematic review have been conducted on oral health, dental caries, and obesity in Mexican children and adolescents. Mexico is an upper-middle–income Latin -American country experiencing a double burden of malnutrition (ie, the coexistence of overweight and obesity alongside stunning and wasting) in the past few decades.11 The “Childhood and Adolescent Obesity in Mexico: Evidence, Challenges, and Opportunities” (COMO) project intends to synthesize and use data to comprehend the extent, nature, effects, and costs of childhood and adolescent obesity in Mexico.12 The aim for this systematic review, which is part of the COMO project, is to evaluate the association of oral health outcomes (eg, oral health indexes, caries, dental plaque, gingivitis) with overweight or obesity in Mexican children and adolescents.
METHODS
This project’s systematic review has been registered in the International Prospective Register of Systematic Reviews13 (PROSPERO registration no. CRD42019154132). It has been reported according to Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) guidelines.14 The research question and inclusion and exclusion criteria were established following the Population, Exposure, Comparison, Outcomes, Study Design (PECOS) framework. (Table 1)
Table 1.
PECOS criteria for inclusion of studies
| Population | Children and adolescents from zero to 18 years old from any ethnicity or sex living in Mexico |
|---|---|
| Exposure | Overweight or obesity measured via BMI and categorized with national or international references |
| Comparator | Studies that compared the prevalence of oral health outcomes across BMI categories |
| Outcomes | Oral health outcomes measured with indexes such as Decayed, Missing, and Filled Teeth; Decayed, Missing, and Filled (permanent) Teeth Surfaces; Decayed, Extracted, and Filled (primary) Teeth; International Caries Detection and Assessment System |
| Study design | Observational studies |
Abbreviations: BMI, body mass index; PECOS, population, exposure, comparison, outcomes, study design.
The databases searched included MEDLINE, EMBASE, the Cochrane Library, Global Health Library, LILACS, CINAHL, CAB abstracts, ERIC, PsycINFO, ScienceDirect, Scopus, AGRICOLA, and SciELO Citation Index. Also, we searched for relevant material in the search engine Google Scholar. When possible, searches were also done in Spanish to capture relevant references. A sensitive search was developed to include index terms, free-text words, abbreviations, and synonyms to combine the key concepts for this review. Terms such as “overweight,” “obesity,” “body mass index,” “bodyweight,” “child,” “adolescent,” “dental caries,” and “oral health” were included in the strategy with different term variations or synonyms and Boolean connectors to capture relevant publications. Full reports or conference abstracts were included if these met the inclusion criteria. Reference lists of included papers also were scrutinized for additional publications, and experts in the field were contacted for additional relevant reports. Original searches were conducted in January 2020 and updated in January 2021.
Selection criteria
As noted, the eligibility criteria were based on the PECOS framework (Table 1). The criteria are detailed by category in the following paragraphs.
Population
Studies that included children and adolescents from zero to 18 years old (mean reported age at the start of the study) from any ethnicity or sex living in Mexico were considered. Mexican children living in a different country were excluded from this review to better conceptualize the obesity problem within the country’s sociodemographic characteristics and avoid confounding information inherent to migration phenomena. Likewise, studies that analyzed children’s severe conditions (eg, HIV, cancer, fibrosis, Down syndrome) or pregnant adolescents were excluded.
Exposure
Included studies had to report baseline participants’ BMI. The assessment of childhood and adolescent overweight and obesity differs worldwide and relies intensely on the reference data, making BMI comparisons challenging.5,9,15 For this reason, articles that used references of calculated BMI (ie, weight [in kilograms]/height [in meters] squared) and categorized with national or international references (eg, World Health Organization [WHO], International Obesity Task Force, Centers for Disease Control and Prevention) were considered.
Outcomes
Studies testing the association between overweight and/or obesity with oral health were included. Oral health indexes such as Decayed, Missing, and Filled (permanent) Teeth (DMFT); Decayed, Missing, and Filled (permanent) Teeth Surfaces (DMFS); decayed, extracted, and filled primary teeth (deft); and International Caries Detection and Assessment System were included. Also, any other reported oral health outcome (eg, dental plaque index, gingival state) was considered.
Study design
Human observational studies were considered in this review.
Since the early 1990s, there is evidence of a continued increase in the prevalence of childhood and adolescent obesity in Mexico.11 To focus on contemporary epidemiological and environmental circumstances of childhood and adolescent obesity in Mexico, evidence published from 1995 onward was included in this review. Relevant studies included English, Spanish, or Portuguese publications to capture reports from the most widespread languages spoken in the Americas.
Data selection and extraction
Titles, abstracts, and relevant full texts were screened by 2 reviewers (L.L.-C., M.G.-B.) and all were checked by a third reviewer (M.A.-M). In addition, 2 reviewers (M.A.-M., N.L.G.-F.) extracted data from relevant studies independently. In case of any disagreement, a third author was contacted (Y.Y.G.-G.).
A data extraction form was structured following the PECOS framework. Relevant data from the included studies included population characteristics (ie, target population, mean and range of age, sex distribution, other socioeconomic or demographic characteristics); study design; references linked to the study; setting characteristics (eg, city, Mexican state, recruitment location); exposure (ie, BMI and any other anthropometric or adiposity measurement considered), BMI categorization (ie, number of children who were underweight, of normal weight, overweight, or obese), and references used to categorize BMI (eg, WHO, International Obesity Task Force, Centers for Disease Control and Prevention); outcomes: oral health evaluated through commonly used indexes (eg, DMFT, DMFS, deft, International Caries Detection and Assessment System), or any other oral health outcomes (eg, dental plaque, gingival state). It was also recorded if outcomes were measured in primary, permanent, or both types of teeth.
Data synthesis
As reported in previous reviews,9 BMI classification in children and adolescents may vary according to included participants’ age or the references used to categorize BMI. The 4 BMI classifications used across child- and adolescent-targeted studies include “underweight,” “normal weight,” “at risk of overweight,” and “overweight.” In contrast, some others categorized BMI as “underweight,” “normal weight,” “overweight,” and “obese.” For the synthesis purposes, the categories “at risk of overweight” and “overweight” were unified in this review. The categories “overweight” and “obesity” refer to children and adolescents in the 2 highest BMI categories, respectively, regardless of the anthropometric reference used in the studies. The data obtained from the included studies were synthesized narratively, and key characteristics were tabulated. In addition, textual descriptions of studies and reported statistical analysis were recorded and tabulated. Reported outcomes presented per tool or index used are reported narratively in the Results section.
Statistical analysis
Studies that reported oral health using the DMFT, DMFS, and deft indexes were included in a random-effects meta-analysis. The analysis did not combine indexes (ie, DMFT, DMFS, and deft), because the numbers of teeth and surfaces with dental caries reveal a different severity of dental caries, which have been reported as not suitable for direct combination.9
The included studies reported oral health data using several BMI categories: overweight, obesity, underweight, and normal weight. As a primary analysis, higher BMI categories (overweight and obesity) were pooled and compared with data on lower BMIs (underweight or normal weight). Also, as secondary analysis, meta-analyses of specific BMI categories were conducted, and results are provided in Appendix S1 in the Supporting Information online. The weighted mean difference was used to compare oral health indexes’ continuous variables among BMI categories. All results were reported with 95%CIs. Considering that all the included papers were observational studies, we used the DerSimonian and Laird method to construct a random-effects model.16. Whenever possible, sensitivity analyses were performed to exclude studies considered having a “low” quality to test the impact of study quality on the heterogeneity and effect size. The analysis was performed with R statistical software using the library metafor. The main results are presented in forest plots.
Risk of bias and quality assessment
The JBI (formerly, Joanna Briggs Institute) critical appraisal tool for cross-sectional studies17 was used to assess the quality of the included studies. This tool assesses the methodological quality of observational studies and determines the extent to which a study has addressed the possibility of bias.17 The tool evaluates 8 critical items: explicit inclusion and exclusion criteria; details about study participants and the setting; method of measurement of exposure; standard criteria used for measurement of the condition; identification of confounding factors; strategies to deal with confounding factors; outcome measurement validity and reliability; and appropriate statistical analysis. Articles were not included or excluded on the basis of their quality. However, the appreciation of the quality was used to categorize the papers: high quality for those papers that reported sufficient detail for the critical items; unclear quality was assigned for those papers with ≥ 1 “unclear” appreciation in the items; And low quality for those papers that did not report or consider ≥ 1 items of the tool. Two reviewers (M.A.-M., N.L.G.-F.) performed this evaluation independently. If there was any disagreement, a third reviewer was consulted (Y.Y.G.-G.) to reach an agreement.
RESULTS
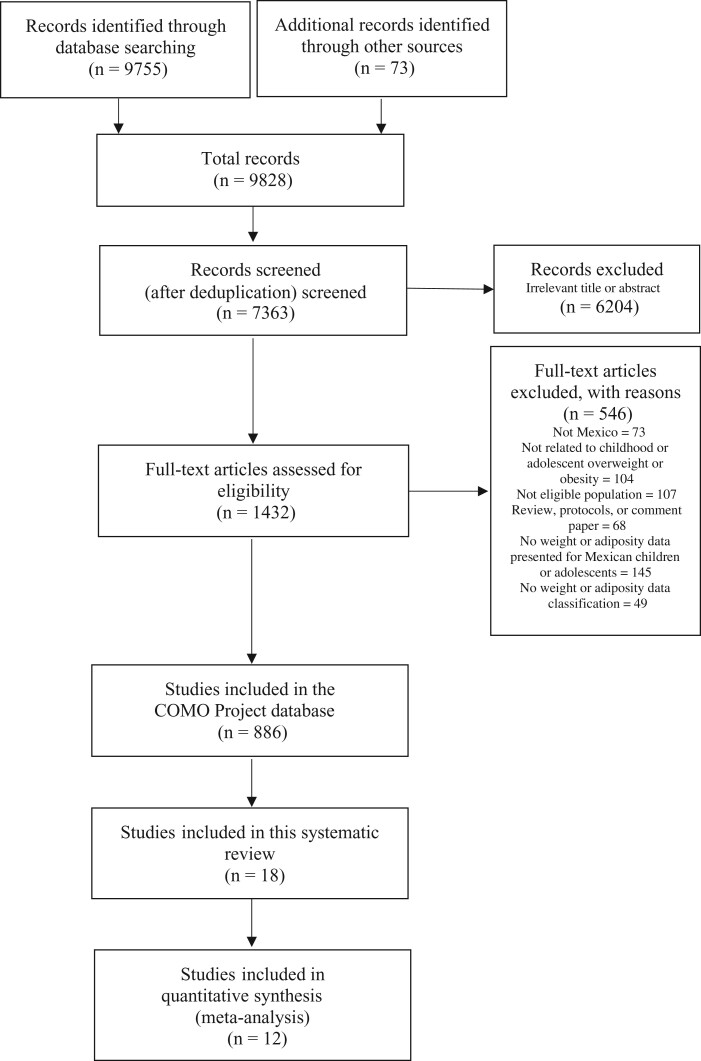
After searching the literature databases, 7363 references were identified, of which 1432 were retrieved for full-text review. Overall, 886 references were identified by reporting obesity-related data from Mexican children and are included in the COMO database (Figure 1). Of these, 18 publications met the eligibility criteria and were included in this review.18–35 The overall characteristics of included studies are presented in Table 2.18–35 All the included studies had a cross-sectional design, except 1,30 which had a longitudinal design. Studies were conducted in 8 of the 32 states in Mexico (Figure 2).
Figure 1.
PRISMA flowchart of the Childhood and Adolescent Obesity in Mexico (COMO): Evidence, Challenges, and Opportunities project.
Table 2.
General characteristics of included studies
| Reference | Setting in Mexico | Population | Outcome measurements | Reported outcome |
|---|---|---|---|---|
| Adriano-Anaya et al 201418; cross-sectional |
|
|
|
|
| Aguilera-Galaviz et al 201919; cross-sectional |
|
|
|
|
| Ashi et al 201920; cross-sectional |
|
|
|
|
| Caudillo-Joya et al 201421; cross-sectional |
|
|
|
|
| De la Cruz Cardoso et al 201522; cross-sectional |
|
|
|
|
| Garcia-Perez et al 202023; cross-sectional |
|
|
|
|
| Irigoyen-Camacho et al 201324; cross-sectional |
|
|
|
|
| Juarez-Lopez et al 201025; cross-sectional |
|
|
|
|
| Lara-Capi et al 201826; cross-sectional |
|
|
|
|
| Loyola-Rodriguez et al 201127; cross-sectional |
|
|
|
|
| Patiño-Marín et al 201828; cross-sectional |
|
|
|
|
| Ramirez-De los Santos et al 202029; cross-sectional |
|
|
|
|
| Sanchez-Perez et al 201030; longitudinal |
|
|
|
|
| Serrano-Piña et al 202031; cross-sectional |
|
|
|
|
| Silva-Flores et al 201332; cross-sectional |
|
|
|
|
| Vazquez-Nava 2010 et al33; cross-sectional |
|
|
|
|
| Zelocuatecatl-Aguilar et al 200534; cross-sectional |
|
|
|
|
| Zúñiga-Manríquez et al 201335; cross-sectional |
|
|
|
The deft Index and SCI values did not differ according to nutritional status (P > 0.05). The caries experience between girls and boys was similar (P > 0.05), as were the different levels of nutrition between girls and boys. |
Abbreviations: BMI, body mass index; CDC, Centers for Disease Control and Prevention; CPI, Community Periodontal Index; deft, decayed, extracted, and filled teeth; DMF, Decayed, Missing, and Filled; DMFS, Decayed, Missing, and Filled Surfaces; DMFT, Decayed, Missing, and Filled Teeth; ICDAS, International Caries Detection and Assessment System; IOTF, International Obesity Task Force; LOA, loss of periodontal attachment; NR, not reported; OHI-S, Simplified Oral Hygiene Index; OB, prevalence of obesity; OR, odds ratio; OW, prevalence of overweight; SCI, Significant Caries Index; SD, Dtandard Deviation, TNI, Treatment Needs Index; WHO, World Health Organization. It was unclear from the text if Adriano-Anaya et al 2014 and Caudillo-Joya et al 2014 were part of the same study, hence these were presented separately.
BMI percentiles classification: < 10th, underweight; < 10th–85th, normal weight; ≥ 85th, overweight; ≥ 95th, obesity; ≥ 97th, severe obesity.
Thinness: < −2 SD; overweight: > +1 SD; obesity: > +2 SD.
Figure 2.
Map of the Mexican 8 states from which evidence was reported.
Most of the studies recruited participants in schools, but 322,27,29 recruited participants in clinics. The study samples varied from 4022 to 6230 participants.21 The age range of included participants was 2.535 to 15 years.24 All the studies included both girls and boys and targeted a general population (including, but not limited to, children with overweight and obesity), except for 122 study that included only children with obesity. Overweight or obesity prevalence varied across studies from 19% to 66% of the included participants. (Table 2)
Various tools were used to measure oral health of participants, and some used >1 tool. The DMFT Index was used in 10 of the 18 studies18,19,21–23,25,27,31,32,34; 6 used deft28,30–33,35; 4 used the DMFS Index20,22,25,30; 4 used the Simplified Oral Hygiene Index19,23,28,34; 2 used the International Caries Detection and Assessment System20,29; 2 used the Significant Caries Index18,21; 2 used the Community Periodontal Index19,24; 2 used the O’Leary’s dental plaque index25,31; 1 used the Treatment Needs Index18; 1 estimated the loss of periodontal attachment24; and 2 evaluated the gingival state28,32 (Table 2).
Overall, results were poorly reported and varied according to the tool used to measure oral health and how the tool was used. For instance, the DMTF Index was the most used tool to measure oral health among the included studies. However, some studies presented just the summary data for DMFT. In contrast, others reported individual index components (ie, number of decayed or missing teeth because of caries or filled teeth) or in a dichotomized form.
Reported results are presented by age group in Table 3.18–35 Overall, the results are inconclusive within and across different age groups. Some studies found no association between BMI and oral health indexes or prevalence of caries.20,25,26,29,35 Some study findings suggested a significant relationship between poorer oral health and overweight or obesity.18,21,27,33 Others reported worst oral health among underweight or normal-weight children.19,23,30–32,34 However, some results varied with other variables considered in the analysis, such as the setting (ie, rural or urban),18,26 socioeconomic status,30 or the sex25 of included participants, and the tool used to measure outcomes.21 Also, 1 study reported that oral health was worst among those adolescents with obesity and insulin resistance27 (Table 3).
Table 3.
Oral Health outcomes per age group
| Age group, y | Reported outcomes |
|---|---|
| ≤526,29,34,37 |
|
| 6–1219,22–24,30–33 |
|
| 13–180,21,25,28,35,38 |
|
Abbreviations: BMI, body mass index; CPI, Community Periodontal Index; OHI-S, Simplified Oral Hygiene Index; OR, odds ratio; SES, socioeconomic status.
For children younger than 5 years, 2 studies reported that visible plaque and higher BMI categories were associated.25,28 However, for children 6–12 years old, no statistical relationship between this dental plaque and BMI was reported in 1 study.31 According to another study, adolescents (aged 13–18 years) who had overweight or obesity were more likely to have bleeding on probing (odds ratio [OR], 1.57; P < 0.01) and periodontal pockets (OR, 1.78; P < 0.01) than those with normal weight. The odds were higher for those with obesity only (OR, 7.07; P < 0.01) and (OR, 5.56; P < 0.01).24
Only 3 studies23,26,33 considered other habits or lifestyles factors to analyze BMI and its relationship with oral health outcomes. The authors of these 3 studies concurred that sugar consumption, bottle feeding, and tooth-brushing frequency were strongly associated with caries (P < 0.05).
Quality of the included studies
Overall, 10 of the 18 included studies were of high quality,23–30,33,34 4 were of unclear quality,18,21,31,32 and another 4 were of low quality.19,20,22,35 The population inclusion and exclusion criteria were not reported clearly in 2 studies.18,21 All the studies measured oral health outcomes validly and reliably. All but 232,35 recorded weight and nutritional status validly and reliably. In 4 studies,19,20,22,35 confounding factors were not identified or the authors did not state their strategies to deal with confounding factors. In almost all the studies, statistical analysis was appropriate (Table 4).18–35
Table 4.
Overall quality appraisal of included studies
| Reference | Clearly defined inclusion criteria | Study participants and setting described in detail | Exposure measured in a valid and reliable way | Objective standard measurements of the condition | Confounding factors identified | Strategies to deal with confounding factors stated | Outcomes measured in a valid and reliable way | Appropriate statistical analysis used | Overall quality appraisal |
|---|---|---|---|---|---|---|---|---|---|
| Adriano-Anaya et al 201418 | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Unclear |
| Aguilera-Galaviz et al 201919 | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ? | Low |
| Ashi et al 201920 | ✓ | × | ✓ | ✓ | × | × | ✓ | ✓ | Low |
| Caudillo-Joya et al 201421 | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Unclear |
| De la Cruz Cardoso et al 201522 | ✓ | ? | ✓ | ? | × | × | ✓ | ? | Low |
| Garcia-Perez et al 202023 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Irigoyen-Camacho et al 201324 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Juarez-Lopez et al 201025 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Lara-Capi et al 201826 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Loyola-Rodriguez et al 201127 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Patiño-Marín et al 201828 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Ramirez-De los Santos et al 202029 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Sanchez-Perez et al 201030 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Serrano-Piña et al 202031 | ✓ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | Unclear |
| Silva-Flores et al 201332 | ✓ | ✓ | ? | ? | ✓ | ✓ | ✓ | ✓ | Unclear |
| Vázquez-Nava et al 201033 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Zelocuatecatl-Aguilar et al 200534 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | High |
| Zúñiga-Manríquez et al 201335 | ✓ | ✓ | ? | ✓ | × | ? | ✓ | ✓ | Low |
Symbols: ✓, yes; ×, no;?, unclear.
Meta-analyses
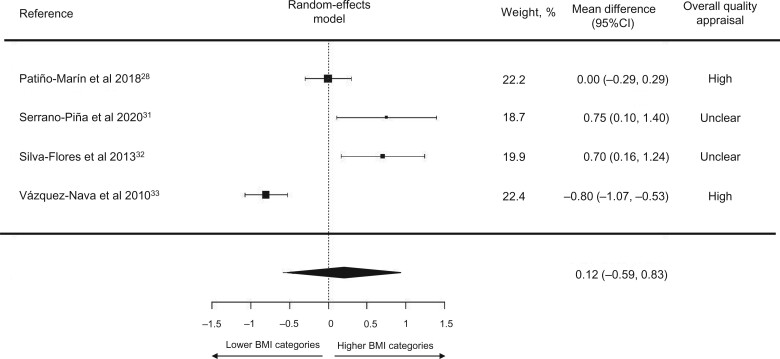
BMI and oral health (using deft Index in primary teeth).
Among the 18 included studies, 528,31–33,35 studies that assessed oral health with the deft index for primary teeth provided sufficient data to be included in the analysis. Overall, no significant differences in the mean deft index were found among children with lower or higher BMIs (overall mean difference [MD], 0.13; 95%CI, –0.49, 0.75). Sensitivity analyses were performed with the only low-quality study removed,35 and the result remained insignificant (overall MD, −0.12; 95%CI, –0.59, 0.83) (Figure 329,32–34).
Figure 3.
Decayed extracted filled teeth index in primary teeth (deft) difference between children with lower or higher BMIs (lower BMI categories, n = 1904; higher BMI categories, n = 1516; I2 = 92.37%). BMI, body mass index.
BMI and oral health (using the DMFS Index in permanent teeth).
Among the 18 included studies, only 220,25 studies that assessed oral health with the DMFS Index provided relevant data to the analysis. One20 was considered to have a low quality, and the other25 was of high quality. When pooling the means and SD estimates for the DMFS Index, no significant differences were found among children with lower BMIs vs children with higher BMIs (overall MD, 0.21; 95%CI, −0.20, 0.62).
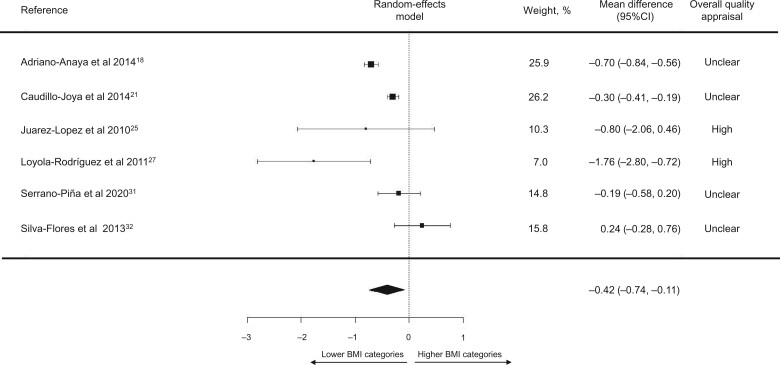
BMI and oral health (using the DMFT Index in permanent teeth).
Among the 18 included studies, 718,19,21,25,27,31,32 assessed oral health with the DMFT Index in permanent teeth and provided relevant data to the analysis. When pooling the means and SD estimates for the DMFT Index, no significant differences were found among children with different BMIs (overall MD, −0.28; 95%CI, −0.63, 0.07). However, when conducting the sensitivity analyses by removing the low-quality study,19 there were statistically significant lower DMFT Index values among children with lower BMIs than among children with higher BMI (overall MD, −0.42; 95%CI, −0.74, −0.11) (Figure 4).18,21,25,27,31,32 Nevertheless, the underweight group had significantly lower DMFT Index values than did other BMI groups (Appendix S1 in the Supporting Information online).
Figure 4.
Decayed Missing Filled Teeth Index in permanent teeth (DMFT) difference between children with lower or higher BMIs (lower BMI categories, n = 6999; higher BMI categories, n = 4986; I2 = 85.92%). BMI, body mass index.
DISCUSSION
For this systematic review, we aimed to investigate oral health outcomes in overweight or obesity in Mexican children and adolescents. Overall, the evidence was inconclusive and varied depending on the study’s methods, appraised quality, the population included, sociodemographic factors considered, tools used to measure outcomes, and how such tools were used. According to pooled estimates, no differences in oral health (measured with the deft or DMTS indexes) were found between children with lower or higher BMIs. However, the pooled estimates of 6 of the 18 studies of high or unclear quality showed that children with higher BMIs (overweight or obesity) have worse oral health (measured with the DMTF Index) than children with lower BMIs (normal weight or underweight).
Some of the results of this review are in line with those presented in a recent meta-analysis by Chen et al.9 For instance, no significant differences were found among BMI categories and oral health outcomes in primary teeth (deft Index). Nevertheless, for permanent teeth (DMFT Index), childhood overweight and obesity were related to poorer oral health and caries. However, Chen et al9 suggested that this association was only found in high-income countries and did not include Mexican population data.
Some have suggested that nutrients such as vitamin A, vitamin D, calcium, or phosphate play crucial roles in teeth morphology, chemical composition, and eruption patterns.37–40 Reduced consumption of these nutrients may affect the susceptibility of teeth to dental caries.41 Although some micronutrient deficiencies might be produced, in part, by behaviors (eg, decreased outdoor activities because of social distress, which results in vitamin D deficiency), diet plays a crucial role in vitamin and mineral deficiencies. It is estimated that vitamin D deficiency affects 26% of preschoolers and approximately 37% of school-age children in Mexico.42 Some suggest vitamin D intake is low among Mexican children, and this vitamin deficiency is also associated with overweight in school-age children.42 Moreover, as shown in Figure 2, evidence for these observations comes from different areas of Mexico. The definition and composition of the diet consumed in Mexico can vary according to the geographical region.43 Most of the country consumes maize and cereals as a base, but consumption of fish, vegetables, and fruits depends on the area.43
Some speculative biological and biomolecular causal pathways between BMI and oral health have been defined.44 Some biomolecular theories suggest that because of the infection caused by dental caries, chronic inflammation can be present, affecting not only oral health but also could be linked to other health issues such as anemia, which could affect weight-related outcomes.44 Physiological theories include a compromised ability to bite or chew foods in the presence of worst oral health or caries, which could lead to an altered BMI, because teeth with more severe lesions may have a higher impact while chewing and could affect the nutritional intake of some children.44 Likewise, eating difficulties are more commonly reported in children with dental caries.45,46
The relation of body composition and oral health outcomes among children and adolescent is complex and multifactorial. Such a relationship may be bidirectional, because both might be perceived as exposure or outcome. It has been described that although overweight and obesity shared some causal factors with poor oral health outcomes (eg, high-sugar diets), there seem to be more factors influencing this association. Other studies have suggested that genetic or biological factors,47 sedentary behaviors,48 socioeconomic status,49,50 lower parental education levels,47 and food insecurity51 might determine the development of both conditions (ie, obesity and poor oral health) in children.
Some methodological issues have also been highlighted when studying the relationship between obesity and oral health in children. For instance, age and sex might influence the results.47,52,53 Because caries indexes represent a cumulative disease status, older groups may demonstrate a greater disease experience. This might be influenced by the differences in diet among age groups, the prevalence of dental caries over time, and the exfoliation of primary teeth.54 The evidence in Mexico was inconclusive within and across different age groups (ie, ≤5 years, 6–12 years, and 13–18 years).
Some of the included studies reported relevant data from subanalyses. For instance, 1 study25 found no association between BMI and the prevalence of caries. However, when analyzing per sex, girls had a higher risk of caries than did boys. Two other studies,18,26 suggested that residence area (urban or rural) was associated with caries severity. In 1 study,30 children with fewer economic resources had the worst oral health indexes. One reported the worst oral health outcomes in those adolescents with obesity and insulin resistance.27 Likewise, only 323,26,33 of the 18 studies considered other lifestyles behaviors in the analysis. The authors of the 3 studies agree that caries prevalence was strongly associated with dietary (high-sugar consumption and bottle feeding) and hygiene (tooth brushing) factors. However, few included studies clarified if they adjusted their analysis to relevant confounders or considered other lifestyles in the analysis.
Furthermore, different obesity diagnosis standards were used among included studies, with some not reporting the standards used to classify participants’ BMI. Some studies reported using international references (eg, WHO or International Obesity Taskforce), whereas others used references relevant to Latin America or the Mexican region. Although some studies used similar references, the cutoffs differed among some studies, as shown in Table 2. This is a major limitation, considering that the BMI classification and diagnosis of overweight or obesity could differ among references and alter the correlation with dental health. A systematic review and meta-analysis by Hayden et al55 showed a significant association between obesity and dental caries when the BMI for age and sex percentile (using Centers for Disease Control and Prevention standards) were reported and no significant associations when z-scores (WHO standards) were reported. Nevertheless, in the analysis, those children and adolescents in the 2 highest BMI categories were considered, regardless of the anthropometric reference, similar to previous meta-analyses.9
Some other limitations of the present review include heterogeneity among included observational studies. For instance, a variety of tools were used to measure oral health (eg, deft, DMTS, DMTF indices), sample sizes (range, 40–6230 participants), and the quality appraisal across studies (only 55.5% were high quality). In addition, studies reported different age groups, data were presented for both girls and boys (only 1 study provided data per sex), and obesity was diagnosed with a mix of national and international BMI classification references, as we discussed previously. Consequently, insufficient studies were available to conduct a subgroup analysis. Also, the retrieved evidence was from 8 of 32 states in Mexico, so the results did not present a nationwide picture. This is relevant, considering that some lifestyles (eg, diet) might vary depending on the geographic region and setting (urban vs rural).
This work’s strengths include an exhaustive search for evidence across 13 databases and 1 search engine performed in 2 languages, which helped us capture relevant publications. As part of the COMO project, an extensive search for gray literature was conducted, but no relevant information about oral health among Mexican children was identified.12 This is important because recent meta-analyses and reviews have not considered data from Mexican children or adolescents.5,8,9,56
Mexico had led the implementation of different nationwide strategies to tackle obesity among the general population, which might also affect oral health outcomes. For instance, Mexico recently introduced a 1 peso/L excise tax on sugar-sweetened beverages.57,58 More recently, implementing a front-of-pack labelling system has been achieved.59 Still, effective and targeted efforts to identify vulnerable populations are needed in Mexico. In addition, different organizations, including WHO and the British Society of Paediatric Dentistry, are calling for more coordinated efforts to tackle both oral health issues (eg, caries) and obesity.60,61 Although whether an association exists between BMI and oral health among Mexican children and adolescents remains inconclusive, health professionals involved in young people’s care should consider individual, family, and environmental factors that might affect dental health and unfavorable BMI, because these are likely to have shared trails, such as diets with a high sugar content. More evidence is available on interventions to prevent62 or treat63 obesity among Mexican children and adolescents. However, understanding how development, dental caries, and nutritional status are linked could inform broader risk factor–based preventive strategies. Doing so could facilitate collaborative and multidisciplinary approaches among public health, nutrition, clinic, and dental specialists involved in children’s and adolescents’ care.
CONCLUSION
Although whether there is an association between oral health and high BMI in Mexican children and adolescents remains inconclusive, both conditions (ie, poor oral health and high BMI) coexist in this population. Therefore, health promotion and prevention efforts should address common risk factors and social determinants of broader risk shared with a number of other noncommunicable diseases.
Supplementary Material
Acknowledgments
We thank Dr Beatriz Goulao and Dr David Cooper, who kindly revised our analyses.
Contributor Information
Magaly Aceves-Martins, The Rowett Institute of Nutrition and Health, University of Aberdeen, Foresterhill, Aberdeen, UK.
Naara L Godina-Flores, Nutrition Department, School of Medicine and Health Sciences, Tecnológico de Monterrey, Col. Ejidos de Huipulco, Tlalpan, Mexico City, Mexico.
Yareni Yunuen Gutierrez-Gómez, Nutrition Department, School of Medicine and Health Sciences, Tecnológico de Monterrey, Col. Ejidos de Huipulco, Tlalpan, Mexico City, Mexico.
Derek Richards, School of Dentistry, University of Dundee, Park Place, Dundee, UK.
Lizet López-Cruz, Universidad Europea del Atlantico, Parque Científico y Tecnologico de Cantabria, Santander, Cantabria, Spain.
Marcela García-Botello, Universidad de Monterrey, Nuevo León, Mexico.
Carlos Francisco Moreno-García, School of Computing, Robert Gordon University, Garthdee House, Aberdeen, Scotland, UK.
Supporting Information
The following Supporting Information is available through the online version of this article at the publisher’s website.
Appendix S1 Meta-analyses of specific body mass index (BMI) categories
Figure S1 DMFT between obesity and normal weight
Figure S2 DMFT between obesity and overweight
Figure S3 DMFT between obesity and underweight
Figure S4 DMFT between overweight and obesity and underweight
Figure S5 DMFT between overweight and obesity and normal weight
Author contributions
M.A.-M. and C.F.M.-G. conceptualized and led the COMO project. All authors contributed significantly to the data collection, interpretation, and analysis; participated in the critical writing and revision of the article; and read and approved the versions submitted to the journal.
Funding
No funding was received to do this work. M.A.-M. is currently funded by the Scottish Government’s Rural and Environment Science and Analytical Services Division.
Declaration of interest
MA-M, NLGF, DR, LL-C, MG-B, CFMG have no conflict of interest to declare. Y.Y.G.-G. received funding from Bonafont to present data at a congress in 2016 and funding from Abbott to write 2 book chapters in 2020. The other authors have nothing to declare.
References
- 1. Peres MA, Macpherson LM, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249–260. [DOI] [PubMed] [Google Scholar]
- 2. Kassebaum NJ, Bernabé E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94:650–658. [DOI] [PubMed] [Google Scholar]
- 3. Bernabe E, Marcenes W, Hernandez CR, et al. ; GBD 2017 Oral Disorders Collaborators. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99:362–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kassebaum NJ, Smith AG, Bernabé E, et al. ; GBD 2015 Oral Health Collaborators. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 2017;96:380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Manohar N, Hayen A, Fahey P, et al. Obesity and dental caries in early childhood: a systematic review and meta‐analyses. Obes Rev. 2020;21:E12960. [DOI] [PubMed] [Google Scholar]
- 6. Manton DJ. Child dental caries–a global problem of inequality. EClinicalMedicine. 2018;1:3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abanto J, Carvalho TS, Mendes FM, et al. Impact of oral diseases and disorders on oral health‐related quality of life of preschool children. Community Dent Oral Epidemiol. 2011;39:105–114. [DOI] [PubMed] [Google Scholar]
- 8. Shivakumar S, Srivastava A, Shivakumar GC. Body mass index and dental caries: a systematic review. Int J Clin Pediatr Dent. 2018;11:228–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen D, Zhi Q, Zhou Y, et al. Association between dental caries and BMI in children: a systematic review and meta-analysis. Caries Res. 2018;52:230–245. [DOI] [PubMed] [Google Scholar]
- 10. Carson SJ, Abuhaloob L, Richards D, et al. The relationship between childhood body weight and dental caries experience: an umbrella systematic review protocol. Syst Rev. 2017;6:216– 215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aceves-Martins M, Llauradó E, Tarro L, et al. Obesity-promoting factors in Mexican children and adolescents: challenges and opportunities. Glob Health Action. 2016;9:29625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aceves-Martins M. The “Childhood and adolescent Obesity in MexicO: evidence, challenges and opportunities” (COMO) project perspectives. 2021. Available at: https://www.comoprojectmx.com. Accessed 15 February 2021
- 13.International prospective register of systematic reviews (PROSPERO). 2020. Available at: https://www.crd.york.ac.uk/prospero. Accessed 15 February 2021
- 14. Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. [DOI] [PubMed] [Google Scholar]
- 15. Flegal KM, Ogden CL. Childhood obesity: are we all speaking the same language? Adv Nutr. 2011;2:159S–166S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Metelli S, Chaimani A. Challenges in meta-analyses with observational studies. Evid Based Ment Health. 2020;23:83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moola S, Munn Z, Tufanaru C, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. Adelaide, South Australia, Australia: JBI; 2020. Available at: https://synthesismanual.jbi.global.com Accessed 02 February 2021.
- 18. Adriano Anaya MD, Caudillo Joya T, Juárez López ML, et al. Obesidad y caries dental problemas de salud publica en una población escolar. Int J Odontostomat. 2014;8:475–480. [Google Scholar]
- 19. Aguilera-Galaviz LA, Hernández-Vázquez B, Frausto-Esparza S, et al. Nutritional and oral health conditions in high school students. Odovtos Int J Dent Sci. 2019;21:83–93. [Google Scholar]
- 20. Ashi H, Campus G, Klingberg G, et al. Childhood obesity in relation to sweet taste perception and dental caries–a cross-sectional multicenter study. Food Nutr Res. 2019;63:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Caudillo JT, del P, Adriano-Anaya M, Caudillo-Adriano PA. Asociación de la caries dental y el índice de masa corporal en una población escolar de la Ciudad de México. Rev Invest Clin. 2014;66:512–519. [PubMed] [Google Scholar]
- 22. De la Cruz Cardoso D, Rodríguez Carrillo A, Muñoz Cervantes P, et al. Experiencia de caries en niños de 6 a 12 años de edad con obesidad exógena del Hospital General de México. Revista ADM. 2015;72: 184–188. [Google Scholar]
- 23. Garcia-Pérez A, Ortega CB, Pineda ÁG, et al. An inverse relationship between obesity and dental caries in Mexican schoolchildren: a cross-sectional study. Public Health. 2020;180:163–167. [DOI] [PubMed] [Google Scholar]
- 24. Irigoyen-Camacho ME, Sanchez-Perez L, Molina-Frechero N, et al. The relationship between body mass index and body fat percentage and periodontal status in Mexican adolescents. Acta Odontol Scand. 2014;72:48–57. [DOI] [PubMed] [Google Scholar]
- 25. Juárez-López ML, Villa-Ramos A. Prevalencia de caries en preescolares con sobrepeso y obesidad. Rev Invest Clín. 2010;62:115–120. [PubMed] [Google Scholar]
- 26. Lara-Capi C, Cagetti MG, Cocco F, et al. Effect of body weight and behavioural factors on caries severity in Mexican rural and urban adolescents. Int Dent J. 2018;68:190–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Loyola-Rodriguez JP, Villa-Chavez C, Patiño-Marin N, et al. Association between caries, obesity and insulin resistance in Mexican adolescents. J Clin Pediatr Dent. 2011;36:49–54. [DOI] [PubMed] [Google Scholar]
- 28. Patiño‐Marín N, Zavala‐Alonso NV, Martínez‐Castañón GA, et al. Association between dental hygiene, gingivitis and overweight or the risk of overweight in primary teeth of 4‐and 5‐year‐old preschoolers in México. Int J Dent Hyg. 2018;16:411–418. [DOI] [PubMed] [Google Scholar]
- 29. Ramírez-De los Santos S, López-Pulido EI, del Carmen Medrano-González I, et al. Alteration of cytokines in saliva of children with caries and obesity. Odontology. 2021;109:11–17. [DOI] [PubMed] [Google Scholar]
- 30. Sánchez-Pérez L, Irigoyen M, Zepeda M. Dental caries, tooth eruption timing and obesity: a longitudinal study in a group of Mexican schoolchildren. Acta Odontol Scand. 2010;68:57–64. [DOI] [PubMed] [Google Scholar]
- 31. Serrano Piña R, Aguilar Ayala FJ, Scougall Vilchis RJ, et al. Prevalence of obesity in elementary school children and its association with dental caries. Oral Health Prev Dent. 2020;18:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Silva-Flores XD, Benavides RC, Barrera JC, et al. Prevalencia de caries, gingivitis y maloclusiones en escolares de Ciudad Victoria, Tamaulipas y su relación con el estado nutricional. Rev Odontol Mexicana. 2013;17:221–227. [Google Scholar]
- 33. Vázquez-Nava F, Vázquez-Rodríguez EM, Saldívar-González AH, et al. Association between obesity and dental caries in a group of preschool children in Mexico. J Public Health Dent. 2010;70:124–30. [DOI] [PubMed] [Google Scholar]
- 34. Zelocuatecatl-Aguilar AZ, Maldonado MO, de la Fuente Hernández J. Asociación entre el índice de masa corporal y las condiciones bucales en escolares. Rev Odonto=Mexicana. 2005;9:185–190. [Google Scholar]
- 35. Zúñiga-Manríquez AG, Medina-Solís CE, Lara-Carrillo E, et al. Experiencia, prevalencia y severidad de caries dental asociada con el estado nutricional en infantes Mexicanos de 17 a 47 meses de edad. Rev Invest Clin. 2013;65:228–236. [PubMed] [Google Scholar]
- 36. Kuczmarski RJ. 2000 CDC Growth Charts for the United States: methods and Development. Hyattsville, MD: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2002. [PubMed] [Google Scholar]
- 37. Botelho J, Machado V, Proença L, et al. Vitamin D deficiency and oral health: a comprehensive review. Nutrients. 2020;12:1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bafti LS, Hashemipour MA, Poureslami H, et al. Relationship between body mass index and tooth decay in a population of 3–6-year-old children in Iran. Int J Dent. 2015;2015:126530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Chauhan A, Nagarajappa S, Dasar PL, et al. Association of body mass index with dental caries among malnourished tribal children of Indore division. Clujul Med. 2016;89:542–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Panwar NK, Mohan M, Arora R, et al. Study on relationship between the nutritional status and dental caries in 8-12 year old children of Udaipur City, India. Kathmandu Univ Med J (KUMJ). 2014;12:26–31. [DOI] [PubMed] [Google Scholar]
- 41. Seminario AL, Velan E. Vitamin D and dental caries in primary dentition. J Dent Child (Chic). 2016;83:114–119. [PubMed] [Google Scholar]
- 42. Flores A, Flores M, Macias N, et al. Vitamin D deficiency is common and is associated with overweight in Mexican children aged 1–11 years. Public Health Nutr. 2017;20:1807–1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Valerino-Perea S, Lara-Castor L, Armstrong ME, et al. Definition of the traditional Mexican diet and its role in health: a systematic review. Nutrients. 2019;11:2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Silva MJ, Kilpatrick NM, Craig JM, et al. A twin study of body mass index and dental caries in childhood. Sci Rep. 2020;10:568– 567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Alsumait A, ElSalhy M, Raine K, et al. Impact of dental health on children’s oral health-related quality of life: a cross-sectional study. Health Qual Life Outcomes. 2015;13:98–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gilchrist F, Marshman Z, Deery C, et al. The impact of dental caries on children and young people: what they have to say? Int J Paediatr Dent. 2015;25:327–338. [DOI] [PubMed] [Google Scholar]
- 47. Alshihri AA, Rogers HJ, Alqahtani MA, Aldossary MS. Association between dental caries and obesity in children and young people: a narrative review. Int J Dent. 2019;2019:9105759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. El Qomsan MA, Alasqah MN, Alqahtani FA, et al. Intricate evaluation of association between dental caries and obesity among the children in Al-Kharj City (Saudi Arabia). J Contemp Dent Pract. 2017;18:29–33. [DOI] [PubMed] [Google Scholar]
- 49. Marshall TA, Eichenberger‐Gilmore JM, Broffitt BA, et al. Dental caries and childhood obesity: roles of diet and socioeconomic status. Commun Dent Oral Epidemiol. 2007;35:449–458. [DOI] [PubMed] [Google Scholar]
- 50. Baker SR, Foster Page L, Thomson WM, et al. Structural determinants and children’s oral health: a cross-national study. J Dent Res. 2018;97:1129–1136. [DOI] [PubMed] [Google Scholar]
- 51. Hill B. Evaluating the association between food insecurity and dental caries in US children 1‐19 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013‐2014. J Public Health Dent. 2020;80:14–17. [DOI] [PubMed] [Google Scholar]
- 52. Mathus‐Vliegen EM, Nikkel D, Brand HS. Oral aspects of obesity. Int Dent J. 2007;57:249–256. [DOI] [PubMed] [Google Scholar]
- 53. Hooley M, , SkouterisH, , Boganin C, et al.. Body mass index and dental caries in children and adolescents: a systematic review of literature published 2004 to 2011. Syst Rev. 2012;1:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Liang JJ, Zhang ZQ, Chen YJ, et al. Dental caries is negatively correlated with body mass index among 7-9 years old children in Guangzhou, China. BMC Public Health. 2016;16:638– 637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hayden C, Bowler JO, Chambers S, et al. Obesity and dental caries in children: a systematic review and meta‐analysis. Community Dent Oral Epidemiol. 2013;41:289–308. [DOI] [PubMed] [Google Scholar]
- 56. Angelopoulou MV, Beinlich M, Crain A. Early childhood caries and weight status: a systematic review and meta-analysis. Pediatr Dent. 2019;41:261–272. [PubMed] [Google Scholar]
- 57. Mostert CM. Sugar-sweetened beverage tax in Mexico. Health Aff (Millwood). 2017;36:1144. [DOI] [PubMed] [Google Scholar]
- 58. Colchero MA, Rivera-Dommarco J, Popkin BM, et al. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Aff (Millwood). 2017;36:564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kaufer-Horwitz M, Tolentino-Mayo L, Jáuregui A, et al. [A front-of-pack labelling system for food and beverages for Mexico: a strategy of healthy decision-making]. Salud Publica Mex. 2018;60:479–486. [DOI] [PubMed] [Google Scholar]
- 60.British Society of Paediatric Dentistry. Dental caries and obesity must be tackled together. Br Dent J. 2020;229:768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Delli Bovi AP, Di Michele L, Laino G, et al. Obesity and obesity related diseases, sugar consumption and bad oral health: a fatal epidemic mixtures: the pediatric and odontologist point of view. Transl Med UniSa. 2017;16:11–16. [PMC free article] [PubMed] [Google Scholar]
- 62. Aceves-Martins M, , López-CruzL, , García-Botello M, et al.. Interventions to Prevent Obesity in Mexican Children and Adolescents: Systematic Review. Prev Sci. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Aceves-Martins M, López-Cruz L, García-Botello M, et al. Interventions to treat obesity in Mexican children and adolescents: systematic review and meta-analysis. Nutrition Rev. 2022;80:544–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.