Key Points
Question
Is the clinical decision for an elective birth at 39 weeks’ gestation associated with adverse childhood developmental outcomes, compared with expectant management?
Findings
In this cohort study of 88 165 births, elective birth at 39 weeks’ gestation, compared with expectant management, was not associated with developmental vulnerability. Additionally, for elective births at 39 weeks’ gestation, induction of labor had a comparable risk of childhood developmental vulnerability as planned cesarean delivery.
Meaning
Elective birth at 39 weeks’ gestation when compared with expectant management was not associated with adverse childhood developmental outcomes.
This cohort study examines the association of elective birth at 39 weeks’ gestation, compared with expectant management, with the risk of adverse childhood developmental outcomes.
Abstract
Importance
Elective births at 39 weeks’ gestation are increasing. While this option may improve maternal and perinatal outcomes compared with expectant management, longer-term childhood developmental outcomes are uncertain.
Objective
To investigate the association between elective birth at 39 weeks’ gestation and the risk of childhood developmental vulnerability.
Design, Setting, and Participants
For this cohort study, 2 causal inference analyses were conducted using Australian statewide, population-based data. Perinatal data from births between January 1, 2005, and December 31, 2013, were linked to childhood developmental outcomes at age 4 to 6 years (assessed using multiple imputation via inverse probability-weighted regression adjustment). Data analyses were conducted between September 7 and November 9, 2021.
Exposures
Two exposure groups were considered: (1) elective birth between 39 weeks and 0 days’ and 39 weeks and 6 days’ gestation vs expectant management and (2) birth via induction of labor vs planned cesarean delivery among those born electively at 39 weeks’ gestation.
Main Outcomes and Measures
Childhood developmental vulnerability at school entry, defined as scoring below the 10th percentile in at least 2 of 5 developmental domains (physical health and well-being, social competence, emotional maturity, school-based language and cognitive skills, and communication skills and general knowledge).
Results
Of 176 236 births with linked outcome data, 88 165 met the inclusion criteria. Among these, 15 927 (18.1%) were elective births at 39 weeks’ gestation (induction of labor or planned cesarean delivery), and 72 238 (81.9%) were expectantly managed with subsequent birth between 40 and 43 weeks’ gestation. Compared with expectant management, elective birth at 39 weeks’ gestation was not associated with an altered risk of childhood global developmental vulnerability (adjusted relative risk [aRR], 1.03; 95% CI, 0.96-1.12) or with developmental vulnerability in any of the individual domains. In an analysis restricted to elective births at 39 weeks’ gestation, induction of labor (n = 7928) compared with planned cesarean delivery (n = 7999) was not associated with childhood developmental vulnerability (aRR, 0.96; 95% CI, 0.82-1.12) or with vulnerability in any individual domains.
Conclusions and Relevance
In this cohort study, elective birth at 39 weeks’ gestation was not associated with childhood developmental vulnerability. For those born electively at 39 weeks’ gestation, birth after induction of labor or by elective cesarean delivery had similar developmental outcomes.
Introduction
The ARRIVE trial (A Randomized Trial of Induction Versus Expectant Management), published in 2018,1 provided reassurance about the safety of elective induction of labor at 39 weeks’ gestation and changed clinical practice. This randomized trial of 6106 participants showed that compared with expectant management, electively inducing labor at 39 weeks’ gestation significantly reduces the risk of cesarean delivery and may reduce serious perinatal complications.1 Meta-analyses of large observational studies have concluded that elective induction at 39 weeks’ gestation is associated with marked reductions in the risk of major perinatal adverse events, including stillbirth.2 The apparent fetal and maternal benefits of elective induction of labor have prompted a shift in contemporary practice and led to a revised position statement from the American College of Obstetricians and Gynecologists stating that it is “reasonable to offer elective induction of labor at 39 weeks’ gestation to women considered low-risk.”3
Although there is now evidence of improved short-term maternal and perinatal outcomes following elective birth at 39 weeks’ gestation compared with expectant management,1,2,4 concerns linger about whether this intervention could result in adverse developmental outcomes for the children. A large retrospective cohort study from Scotland demonstrated a step-wise decrease in the probability of special education needs with advancing gestation, a trend that extended into postterm gestations.5 Recent cohort studies have concluded that those born electively at 39 or 40 weeks’ gestation had similar year 3 school performance outcomes compared with those born following expectant management (from Australia, where 1353 were induced at 39 weeks’ gestation6; and Rhode Island, where 455 were induced at 39 or 40 weeks’ gestation7). To our knowledge, no large cohort studies have examined the impact of inducing birth at 39 weeks’ gestation on global childhood developmental outcomes beyond educational performance, such as social competency, emotional maturity, and communication skills. Such data are urgently required given a likely swing toward elective induction of labor across the globe.8,9,10
Addressing the issue of childhood developmental outcomes by performing randomized trials is a challenge, because very large numbers and many years of follow-up are needed to ensure adequate power. Instead, we analyzed statewide linked data using a causal inference framework that allowed us to establish study conditions similar to a target trial and examine the association of elective birth at 39 weeks’ gestation with childhood development vulnerability at school entry. This analytical approach uses principles from the potential outcomes approach to causal inference to (1) identify a research question that reflects a specific clinical decision point (intervention) that could be examined in an randomized clinical trial, (2) identify the outcome of interest, (3) determine a statistical method that can estimate the average treatment outcome using available data from the population of interest, and (4) spell out steps 1 through 3 in an a priori statistical analysis protocol.11
We performed 2 such causal inference analyses. The first compared elective birth at 39 weeks’ gestation (induction of labor and planned cesarean delivery) with expectant management. The second compared outcomes following the 2 options for elective birth at 39 weeks’ gestation: an induction of labor vs a planned elective cesarean delivery. Secondary analyses examined the risk of developmental vulnerability by mode of birth following induction of labor at 39 weeks’ gestation only.
Methods
Study Population, Exposures, and Outcomes
This population-based cohort study linked perinatal data of births in Victoria, Australia, from January 1, 2005, to December 31, 2013, with developmental outcomes collected in 2012, 2015, and 2018 from the triennial Australian Early Development Census (AEDC). Perinatal data were obtained from a centralized state collection registry, the Victorian Perinatal Data Collection Unit. Two primary exposure groups were examined.
The first group (cohort A) included elective births at 39 weeks and 0 days’ gestation that were either induced labors (resulting in any mode of birth) or planned cesarean delivery, which were compared with expectant management (any onset of labor or mode of birth that occurred between 40 weeks and 0 days’ and 43 weeks and 6 days’ gestation). Elective births included all indications (maternal request or maternal or neonatal indication). This cohort was used to investigate the question of whether AEDC-defined developmental vulnerability in the first year of school differs for children born electively at 39 weeks’ gestation compared with those born beyond 39 weeks’ gestation. It was not possible to establish exposure before the 39th week.
The second group (cohort B) examined the mode of elective birth and compared induction of labor between 39 weeks and 0 days’ and 39 weeks and 6 days’ gestation with planned cesarean delivery also in the same gestational period. Cohort B was used to investigate the question of whether AEDC-defined developmental vulnerability differed for children born at 39 weeks’ gestation following an induction of labor compared with elective cesarean delivery birth. Both exposure groups were identifiable from the data.
For both cohorts, the estimand under investigation was the difference in the mean of AEDC-defined childhood developmental vulnerability at school had all pregnancies received the intervention and the corresponding mean had none of the pregnancies received the alternative (ie, control or comparator intervention).
We studied singleton births and excluded infants born with congenital anomalies, those with missing data for labor onset, mode of birth or gestational age at birth, and implausible birth weights. Because the purpose of our study was to examine long-term outcomes of elective birth at 39 weeks’ gestation, we excluded those born between 39 weeks and 0 days’ and 39 weeks and 6 days’ gestation after spontaneous or augmented labor. In addition, those diagnosed with placenta previa, placental abruption, and vaginal breech birth were excluded, as they could not have been feasibly randomized to expectant management or induction of labor. An a priori statistical analysis plan (eAppendix in the Supplement) was used to determine eligibility for inclusion in the study, which allowed for a casual inference framework.
The AEDC assesses children in their first year of school (ages 4-6 years). Five individual developmental domains are assessed: physical health and well-being, social competence, emotional maturity, language and cognitive skills (school-based), and communication skills and general knowledge. The primary outcome of our study was developmental vulnerability, defined dichotomously by the AEDC as a child scoring in the lowest decile in 2 or more domains in the AEDC assessment.12 We examined the 5 domains individually (risk of scoring in the lowest decile) as secondary outcomes. Age variability at school entry is routinely adjusted for by the AEDC.
Perinatal maternal data were linked to AEDC childhood data by a third-party governmental agency, the Centre for Victorian Data Linkage. This study was approved by the Mercy Health Human Research Ethics Committee. Given the retrospective and deidentified nature of this study, the requirement for individual participant consent was waived. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Covariates
An a priori statistical analysis plan was agreed upon by all contributing authors (eAppendix in the Supplement). This plan included a direct acyclic graph for both primary analyses, outlining known and potential confounders, effect modifiers, and covariates on the causal pathway of interest. This informed our causal approach to statistical modeling with covariates included in analysis models chosen to block backdoor pathways accounting for potential collider nodes. For the first analysis (cohort A), these covariates were parity, perinatal complications, assisted conception (such as in vitro fertilization), maternal level of education, socioeconomic position (Socio-Economic Index For Areas [SEIFA]), infant birth weight and sex, child’s age at AEDC testing, year of testing, and an interaction term between maternal age and mode of birth. For the second analysis (cohort B), these covariates were maternal body mass index, maternal age, assisted conception, parity, perinatal complications, socioeconomic position (SEIFA), infant birth weight and sex, child’s age at AEDC testing, and year of testing.
Where feasible, data were retained in their original format: continuous, binary, or categorical. Gestational age at birth was based on early pregnancy ultrasound; where ultrasound was not available, menstrual cycle dates were used. Gestation was assessed as completed week from 39 to 43 weeks. Onset of labor was defined as spontaneous, augmented, or induced, and mode of birth as unassisted vaginal birth, assisted vaginal birth (forceps or ventouse), planned cesarean delivery, or emergency cesarean delivery. Information on maternal age at delivery, height, weight, parity, use of assisted reproduction, and perinatal complications (via International Statistical Classification of Diseases and Related Health Problems, Tenth Revision diagnostic codes) were obtained from the Victorian Perinatal Data Collection Unit. Perinatal complications were categorized according to similar pathological processes and included hypertensive disorders, diabetes, suspected small for gestational age, suspected fetal macrosomia, antepartum hemorrhage, premature rupture of membranes, and group b streptococcus colonization. Body mass index, recorded at the obstetric booking visit (first antenatal consultation), was calculated as weight in kilograms divided by height in meters squared. Parental level of education and language background other than English status were based on data obtained from the AEDC, and SEIFA was based on residential postcode at school entry. Children were identified as Aboriginal or Torres Strait Islander if this information had ever been declared on birth or school data. Year of AEDC testing was included to account for variations in outcome data between testing years.
Statistical Analysis
Statistical analyses were conducted from September 7 to November 9, 2021. We analyzed the primary outcomes as follows. First, the distribution of outcome and covariates by exposure status was described with raw data presented as number (%) or mean (SD), and the proportion of missing data was documented for each outcome and covariate. Next, multiple imputation of missing data under a fully conditional specification using a predictive mean model for continuous and unordered categorical covariates and a logistic model for binary covariates was performed. The imputation model included outcome, exposure, all covariates used in the analysis model, and auxiliary variables with standard errors calculated to account for maternal clustering. Imputation diagnostics included graphical assessment of convergence and comparison of distributional shape between both imputed (complete) and observed (nonimputed) covariates. The number of imputed data sets was set to 20.
For each of the imputed data sets, the probability of exposure and associated inverse probability weight were estimated using a logistic regression model conditional on all analysis model covariates listed above and estimated using robust standard errors. Inverse probability weight adjustment for covariate imbalance was assessed as adequate if the standardized mean difference between exposure groups across all covariates was less than 0.1. Observations were then trimmed at the highest minimum and lowest maximum probability of exposure; if substantial numbers of observations were trimmed or inverse probability weighting was large, then alternate forms of weighting (stabilized and overlap) were considered. Using the same logistic model, a new probability of exposure and inverse probability weight was estimated for each trimmed imputed data set. Finally, the average treatment outcome, relative difference, and relative risk were estimated using a doubly robust regression-adjusted model of outcome, exposure and covariates, weighted by the revised inverse probability weights. A pooled estimate of potential outcome means, risk difference, and relative risk with associated 95% CIs adjusted for imputation was derived using Rubin’s rule. This process was automated using Stata’s mi estimate command. This process was repeated for the primary outcome (developmental vulnerability) and the secondary outcomes (individual domains) for both exposure cohorts.
Maternal clustering was accounted for using robust standard errors in all imputation, probability of exposure, and analysis models. Results of regression adjustment using imputed data were compared with complete case results (eTable 1 in the Supplement) and alternative analysis models (eTable 2 in the Supplement).
Secondary analyses were performed using unadjusted and adjusted regression models across imputed data sets. These analyses examined the risk of developmental vulnerability by mode of birth (instrumental vaginal birth vs spontaneous vaginal birth and emergency cesarean delivery vs spontaneous vaginal birth) following induction of labor at 39 weeks’ only. Statistical analysis was conducted using Stata software, version 17 (StataCorp LLC).13
Results
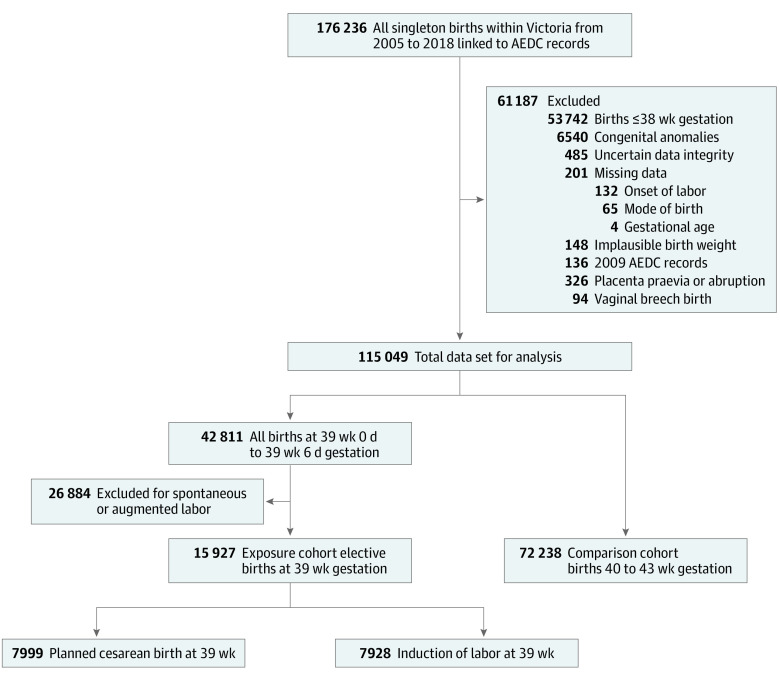
Of the 176 236 singleton infants born in Victoria, Australia, with outcome data, 88 165 met the inclusion criteria (Figure). In our first analysis (cohort A), we compared childhood developmental outcomes among 15 927 infants (18.1% of included births) who were born electively between 39 weeks and 0 days’ and 39 weeks and 6 days’ gestation and 72 238 infants (81.9% of included births) from pregnancies expectantly managed beyond 39 weeks’ gestation and subsequently born between 40 weeks and 0 days’ and 43 weeks and 6 days’ gestation. In our second analysis (cohort B), restricted to elective births at 39 weeks’ gestation, we compared childhood developmental outcomes among 7928 infants born after an induction of labor and 7999 born by planned cesarean delivery. Baseline clinical information for both cohorts is shown in Table 1 and is missing for 0.1% to 42.0% of the study population. Data on AEDC outcomes were missing for 5.3% of the linked study population. Missing covariate and outcome data were imputed and included in analyses.
Figure. Study Flow Diagram.
Table 1. Maternal Demographic and Perinatal Characteristics Among the 2 Primary Comparison Cohortsa.
| Characteristics | No. (%) | |||
|---|---|---|---|---|
| Cohort A: elective birth at 39 wk gestation vs expectant management (n = 88 165) | Cohort B: induction of labor at 39 wk gestation vs planned cesarean delivery at 39 wk gestation (n = 15 927) | |||
| Expectant management (n = 72 238) | Elective birth (n = 15 927) | Planned cesarean (n = 7999) | Induced labor (n = 7928) | |
| Maternal age at birth, y | ||||
| Mean (SD) | 30.7 (5.4) | 32.3 (5.4) | 33.1 (4.9) | 31.5 (5.4) |
| ≥35 | 15 911 (22.0) | 5017 (31.5) | 2911 (36.3) | 2111 (26.6) |
| Missing | 0 | 0 | 0 | 0 |
| BMI, median (IQR) | 24.7 (22.0-28.6) | 25.6 (22.5-30.5) | 25.9 (22.7-30.8) | 25.3 (22.3-30.1) |
| Missing | 30 348 (42.0) | 6362 (17.3) | 3139 (39.2) | 3114 (39.3) |
| Parity | ||||
| Nulliparous | 36 490 (50.5) | 5479 (34.4) | 1566 (19.7) | 3913 (49.4) |
| Multiparous | 35 748 (49.5) | 10 448 (65.6) | 6433 (80.3) | 4015 (50.6) |
| Missing | 0 | 0 | 0 | 0 |
| Parental marital status | ||||
| Married or de facto | 62 592 (86.7) | 14 357 (90.1) | 7313 (91.4) | 7044 (88.9) |
| Single | 9132 (12.6) | 1474 (9.3) | 638 (8.0) | 836 (10.5) |
| Divorced or separated | 514 (0.7) | 96 (0.6) | 48 (0.6) | 48 (0.6) |
| Missing | 0 | 0 | 0 | 0 |
| Socioeconomic status (SEIFA category)b | ||||
| 1 | 11 616 (16.1) | 2250 (14.1) | 1056 (13.2) | 1194 (15.1) |
| 2 | 13 060 (18.1) | 2647 (16.7) | 1301 (16.3) | 1346 (17.0) |
| 3 | 16 052 (22.2) | 3581 (22.5) | 1843 (23.0) | 1738 (21.9) |
| 4 | 17 005 (23.5) | 3825 (24.0) | 1900 (23.8) | 1925 (24.3) |
| 5 | 14 426 (20.0) | 3607 (22.6) | 1890 (23.6) | 1717 (21.7) |
| Missing | 79 (0.1) | 17 (0.1) | 9 (0.1) | 8 (0.1) |
| Maternal education | ||||
| University | 18 164 (25.1) | 4334 (27.2) | 2210 (27.6) | 2124 (26.8) |
| Diploma or TAFE | 18 158 (25.1) | 4149 (26.1) | 2053 (25.7) | 2096 (26.4) |
| High school | 6112 (8.5) | 1414 (8.9) | 749 (9.4) | 665 (8.4) |
| <12 y | 2826 (3.9) | 592 (3.7) | 301 (3.8) | 291 (3.7) |
| Missing | 26 978 (37.4) | 5438 (34.1) | 2686 (33.6) | 2752 (34.7) |
| Second parent level of education | ||||
| University | 13 977 (19.3) | 3384 (21.3) | 1680 (21.0) | 1704 (21.5) |
| Diploma or TAFE | 18 647 (25.8) | 4315 (27.1) | 2226 (27.8) | 2089 (26.4) |
| High school | 5292 (7.3) | 1264 (7.9) | 683 (8.5) | 581 (7.3) |
| <12 y | 3074 (4.3) | 638 (4.0) | 301 (3.8) | 337 (4.3) |
| Missing | 31 248 (43.3) | 6326 (39.7) | 3109 (38.9) | 3217 (40.6) |
| Assisted reproduction | ||||
| Yes | 1269 (1.8) | 452 (2.8) | 214 (2.7) | 238 (3.0) |
| Missing | 25 439 (35.2) | 5054 (31.7) | 2533 (31.7) | 2521 (31.8) |
| Perinatal complications (ICD-10 codes) | ||||
| Hypertensive disorders (all) | 858 (1.2) | 568 (3.6) | 142 (1.8) | 416 (5.3) |
| Diabetes (all) | 1123 (1.6) | 913 (5.7) | 289 (3.6) | 624 (7.8) |
| Suspected small for gestational age (antenatal) | 706 (1.0) | 446 (2.8) | 39 (0.5) | 405 (5.1) |
| Fetal macrosomia | 357 (0.5) | 374 (2.4) | 1 (0.01) | 372 (4.7) |
| Antepartum hemorrhage (excluding known previa or abruption) | 1004 (1.4) | 301 (1.9) | 101 (1.3) | 200 (2.5) |
| Premature rupture of membranes or positive for group B streptococcus | 199 (0.3) | 112 (0.7) | 8 (0.1) | 104 (1.3) |
| None recorded | 67 991 (94.1) | 13 213 (83.2) | 7427 (92.9) | 5795 (73.1) |
| Infant sex, female | 36 192 (50.1) | 7945 (49.9) | 4045 (50.6) | 3937 (49.7) |
| Aboriginal or Torres Strait Islander | 1529 (2.1) | 289 (1.8) | 136 (1.7) | 153 (1.9) |
| Missing | 0 | 0 | 0 | 0 |
| Language background other than English | 12 579 (17.4) | 2724 (17.1) | 1331 (16.6) | 1393 (17.6) |
| Missing | 0 | 0 | 0 | 0 |
| Gestational age, completed wk | ||||
| 39 | NA | 15 927 (100.0) | 7999 (100) | 7928 (100) |
| 40 | 45 085 (62.4) | NA | NA | NA |
| 41 | 25 154 (34.8) | NA | NA | NA |
| 42 | 1939 (2.7) | NA | NA | NA |
| 43 | 60 (0.1) | NA | NA | NA |
| Missing | 0 | NA | NA | NA |
| Birth weight, mean (SD), g | 3638 (442) | 3475 (447) | 3514 (437) | 3436 (453) |
| Missing | 0 | 0 | 0 | 0 |
| Mode of birth | ||||
| Unassisted vaginal birth | 44 566 (61.7) | 4964 (31.2) | NA | 4964 (62.6) |
| Forceps birth | 5677 (7.8) | 653 (4.1) | NA | 653 (8.2) |
| Vacuum birth | 7348 (10.2) | 866 (5.4) | NA | 866 (10.9) |
| Unplanned cesarean delivery | 12 073 (16.7) | 1445 (9.1) | NA | 1445 (18.3) |
| Planned cesarean delivery | 2574 (3.6) | 7999 (50.2) | 7999 | 0 |
| Missing | 0 | 0 | 0 | NA |
| AEDC year of testing | ||||
| 2012 | 24 729 (34.2) | 4882 (30.6) | 2443 (30.5) | 2439 (30.8) |
| 2015 | 23 531 (32.6) | 5042 (31.7) | 2520 (31.5) | 2522 (31.8) |
| 2018 | 24 978 (33.2) | 6003 (37.7) | 3036 (38.0) | 2967 (37.4) |
| Missing | 0 | 0 | 0 | 0 |
| Location of school | ||||
| Major cities | 52 030 (72.0) | 11 865 (74.5) | 5950 (74.4) | 5915 (74.6) |
| Inner regional | 16 255 (22.5) | 3253 (20.4) | 1652 (20.7) | 1601 (20.2) |
| Outer regional | 3746 (5.2) | 773 (4.9) | 381 (4.8) | 392 (4.9) |
| Remote | 207 (0.3) | 36 (0.2) | 16 (0.2) | 20 (0.3) |
| Missing | 0 | 0 | 0 | 0 |
Abbreviations: AEDC, Australian Early Development Census; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; NA, not applicable; SEIFA, Socio-Economic Index For Areas; TAFE, technical and further education.
Cohort A included planned births at 39 weeks’ gestation (induction of labor or elective, planned cesarean delivery) vs expectant management after 39 weeks’ gestation. Cohort B included intervention of induction of labor (vs planned cesarean delivery) among the 39-week cohort only. Data on AEDC outcomes were missing for 5.3% of the study population. Missing covariate and outcome data were imputed and included in analyses.
1 Indicates most relatively disadvantaged.
Primary Analyses
Elective birth at 39 weeks’ gestation, compared with expectant management (any onset of labor and mode of birth from 40 to 43 weeks’ gestation; cohort A), had no causal effect on the risk of developmental vulnerability at school entry, with an adjusted relative risk (aRR) of 1.03 (95% CI, 0.96-1.12) after adjusting via inverse probability weighted in a regression model (Table 2). The unadjusted results were similar, with an unadjusted relative risk of 1.03 (95% CI, 0.95-1.13) and percentage risk difference of 0.28 (95% CI, –0.42 to 0.99) (Table 2). Investigating secondary outcomes, we did not identify a difference between elective birth at 39 weeks’ gestation and expectant management in the risk of vulnerability for any of the 5 individual developmental domains (Table 2).
Table 2. Elective Birth at 39 Weeks’ Gestation vs Expectant Management and the Risk of Developmental Vulnerability Using Imputed Data.
| Inverse probability weighted regression adjustmenta | Unadjusted risk estimates | ||||
|---|---|---|---|---|---|
| Relative risk (95% CI) | Percentage risk difference (95% CI) | Relative risk (95% CI) | Percentage risk difference (95% CI) | ||
| Primary outcome | |||||
| Developmental vulnerability in 2 or more domains | 1.03 (0.96 to 1.12) | 0.28 (−0.38 to 0.94) | 1.03 (0.95 to 1.13) | 0.28 (−0.42 to 0.99) | |
| Secondary outcomes | |||||
| Physical health and well-being | 0.94 (0.86 to 1.02) | −0.46 (−1.08 to 0.16) | 0.94 (0.86 to 1.03) | −0.43 (−1.1 to 0.24) | |
| Social competence | 1.04 (0.96 to 1.13) | 0.32 (−0.31 to 0.94) | 1.04 (0.95 to 1.14) | 0.32 (−0.36 to 0.99) | |
| Emotional maturity | 1.03 (0.94 to 1.12) | 0.20 (−0.44 to 0.84) | 1.03 (0.94 to 1.12) | 0.18 (−0.50 to 0.86) | |
| Language and cognitive skills (school-based) | 1.02 (0.92 to 1.13) | 0.08 (−0.46 to 0.63) | 1.03 (0.92 to 1.15) | 0.15 (−0.44 to 0.73) | |
| Communication skills and general knowledge | 1.04 (0.94 to 1.14) | 0.22 (−0.33 to 0.77) | 1.04 (0.94 to 1.16) | 0.24 (−0.35 to 0.84) | |
Adjusted analyses were pooled from inverse probability weighted regression–adjusted modeling for each imputed data set. Parity, perinatal complications, assisted conception (in vitro fertilization), maternal level of education, socioeconomic position, infant birth weight and sex, child’s age at Australian Early Development Census testing, year of testing, and an interaction term between maternal age and mode of birth were included as covariates.
Next, we examined the risk of developmental vulnerability among those born electively at 39 weeks’ and compared children born via induction of labor (any mode of birth) with those born via planned cesarean delivery (cohort B). Induction of labor at 39 weeks’ gestation, compared with planned cesarean delivery at 39 weeks’ gestation, was not associated with the risk of developmental vulnerability at school entry (aRR, 0.96; 95% CI, 0.82 to 1.12; aRD, –0.34; 95% CI, –1.71 to 1.03) (Table 3). Investigating our secondary outcomes, we did not identify differences in the risk of developmental vulnerability in any of the 5 individual developmental domains between those born via induction of labor vs planned cesarean delivery (Table 3).
Table 3. Induction of Labor at 39 Weeks’ Gestation vs Planned Cesarean Delivery at 39 Weeks’ Gestation and the Risk of Developmental Vulnerability Using Imputed Data.
| Inverse probability weighted regression adjustmenta | Unadjusted risk estimates | |||
|---|---|---|---|---|
| Relative risk (95% CI) | Percentage risk difference (95% CI) | Relative risk (95% CI) | Percentage risk difference (95% CI) | |
| Primary outcome | ||||
| Developmental vulnerability in 2 or more domains | 0.96 (0.82 to 1.12) | −0.35 (−1.71 to 1.03) | 1.07 (0.96 to 1.19) | 0.58 (−0.32 to 1.48) |
| Secondary outcomes | ||||
| Physical health and well-being | 1.05 (0.90 to 1.18) | 0.22 (−0.77 to 1.21) | 1.09 (0.97 to 1.22) | 0.61 (−0.23 to 1.45) |
| Social competence | 0.96 (0.81 to 1.06) | −0.59 (−1.76 to 0.58) | 1.05 (0.94 to 1.18) | 0.38 (−0.47 to 1.24) |
| Emotional maturity | 1.03 (0.92 to 1.19) | 0.32 (−0.71 to 1.35) | 1.16 (1.03 to 1.31) | 1.05 (0.21 to 1.89) |
| Language and cognitive skills (school-based) | 1.03 (0.88 to 1.15) | 0.04 (−0.82 to 0.90) | 1.11 (0.97 to 1.27) | 0.56 (−0.14 to 1.26) |
| Communication skills and general knowledge | 0.89 (0.79 to 1.02) | −0.65 (−1.56 to 0.25) | 1.01 (0.89 to 1.15) | 0.08 (−0.69 to 0.84) |
Adjusted analyses were pooled from inverse probability weighted regression–adjusted modeling for each imputed data set. Maternal body mass index, maternal age, assisted conception (in vitro fertilization), parity, perinatal complications, socioeconomic position, infant birth weight and sex, child’s age at Australian Early Development Census testing, and year of testing were included as covariates.
Unadjusted and adjusted results were similar when complete case data (excluding missing data; n = 52 637 in cohort A and n = 9178 in cohort B) were analyzed for both exposure cohorts (eTable 1 in the Supplement), using alternative modeling (eTable 2 in the Supplement) and when performing sensitivity analyses in which missing outcome data were considered cases of developmental vulnerability.
Secondary Analyses
Developmental Vulnerability by Mode of Birth Following Induction of Labor at 39 Weeks’ Gestation
Next, restricting our cohort to children born via induction of labor at 39 weeks’ gestation only, we investigated whether varying modes of birth were associated with developmental vulnerability (with unassisted vaginal birth designated as the reference group and compared with either assisted vaginal births or birth by emergency cesarean delivery). In unadjusted analysis, assisted vaginal birth when compared with unassisted vaginal birth was associated with a reduced risk of developmental vulnerability (aRR, 0.80; 95% CI, 0.65-0.99). However, after adjusting, there was little evidence against the null hypothesis of no association with assistance in vaginal birth (aRR, 0.84; 95% CI, 0.60-1.18). The risk of developmental vulnerability was similar between those born via emergency cesarean and unassisted vaginal birth in both unadjusted and unadjusted analyses (aRR, 1.08; 95% CI, 0.70-1.65). Similarly, while there were some differences in unadjusted analyses across the 5 individual developmental domains, there were no differences in any of the adjusted analyses (Table 4). Results were similar when using complete case data (missing data excluded) (eTable 3 in the Supplement).
Table 4. Secondary Analysis of Developmental Vulnerability by Mode of Birth.
| Multivariate regression adjusted (noncausal)a | Unadjusted risk estimates | |||
|---|---|---|---|---|
| Relative risk (95% CI) | Percentage risk difference (95% CI) | Relative risk (95% CI) | Percentage risk difference (95% CI) | |
| Developmental vulnerability in 2 or more domains | ||||
| Unassisted vaginal birth (n = 4964) | 1 [Reference] | 0 [Reference] | 1 [Reference] | 0 [Reference] |
| Instrumental vaginal birth (n = 1519) | 0.84 (0.60 to 1.18) | −0.39 (−2.50 to 1.72) | 0.80 (0.65 to 0.99) | −1.77 (−3.34 to −0.20) |
| Unplanned cesarean delivery (n = 1445) | 1.08 (0.70 to 1.65) | 1.24 (−2.21 to 4.70) | 1.05 (0.87 to 1.27) | 0.45 (−1.31 to 2.20) |
| Vulnerability in physical health and well-being domain | ||||
| Instrumental vaginal birth | 0.75 (0.53 to 1.05) | −1.52 (−3.43 to 0.39) | 0.70 (0.55 to 0.88) | −2.53 (−4.02 to −1.03) |
| Unplanned cesarean delivery | 0.74 (0.46 to 1.21) | −1.67 (−4.81 to 1.47) | 0.83 (0.67 to 1.03) | −1.44 (−3.02 to 0.14) |
| Vulnerability in social competence domain | ||||
| Instrumental vaginal birth | 0.77 (0.53 to 1.11) | −1.15 (−3.02 to 0.73) | 0.87 (0.70 to 1.08) | −1.03 (−2.56 to 0.50) |
| Unplanned cesarean delivery | 0.75 (0.45 to 1.25) | −1.99 (−4.75 to 0.78) | 1.04 (0.85 to 1.29) | 0.34 (−1.36 to 2.03) |
| Vulnerability in emotional maturity domain | ||||
| Instrumental vaginal birth | 0.94 (0.68 to 1.30) | 0.02 (−1.98 to 2.01) | 0.93 (0.75 to 1.16) | −0.51 (−2.02 to 1.00) |
| Unplanned cesarean delivery | 1.15 (0.75 to 1.75) | 1.40 (−1.91 to 4.70) | 1.20 (0.98 to 1.47) | 1.48 (−0.21 to 3.17) |
| Vulnerability in language and cognitive skills domain (school-based) | ||||
| Instrumental vaginal birth | 0.79 (0.47 to 1.32) | 0.05 (−1.66 to 1.77) | 0.65 (0.49 to 0.86) | −2.13 (−3.35 to −0.91) |
| Unplanned cesarean delivery | 1.05 (0.63 to 1.75) | 1.06 (−1.78 to 3.90) | 0.81 (0.62 to 1.06) | −1.13 (−2.50 to 0.24) |
| Vulnerability in communication skills and general knowledge domain | ||||
| Instrumental vaginal birth | 1.01 (0.70 to 1.45) | 0.03 (−1.74 to 1.80) | 0.74 (0.57 to 0.97) | −1.57 (−2.85 to −0.29) |
| Unplanned cesarean delivery | 1.41 (0.87 to 2.27) | 1.86 (−1.19 to 4.90) | 1.04 (0.83 to 1.32) | 0.26 (−1.22 to 1.75) |
Adjusted analyses were retrieved using a multivariate Gaussian regression model across imputed data sets, with maternal body mass index, maternal age, assisted conception (in vitro fertilization), parity, perinatal complications, socioeconomic position, infant birth weight and sex, child’s age at Australian Early Development Census testing, and year of testing included as covariates.
Discussion
In this cohort study, we examined the association of elective birth at 39 weeks’ gestation with developmental vulnerability at school entry. Children born electively at 39 weeks’ had the same risk of developmental vulnerability at age 4 to 6 years compared with those whose birth was expectantly managed beyond this gestation. Furthermore, for those electively birthed at 39 weeks’ gestation, there was no difference in developmental vulnerability after an induction of labor vs a planned cesarean delivery.
In further analyses confined to those born at 39 weeks’ gestation, developmental vulnerability did not vary according to mode of birth. Together, our findings provide evidence that the decision for an elective birth at 39 weeks’ gestation does not adversely impact childhood developmental outcomes at age 4 to 6 years. This outcome is particularly reassuring given the possibility that some elective births at 39 weeks’ gestation would have been undertaken for unmeasured indicators of perinatal risk (eg, decreased fetal movements). If these pregnancies were disproportionately affected by placental insufficiency, medically indicated birth at 39 weeks’ gestation may have been associated with increased developmental vulnerability, yet no such association was seen.
Elective birth at 39 weeks’ gestation is becoming increasingly common.8,9,10 Although the short-term perinatal outcomes have been described,2,14 there are little data on the longer-term impact of these interventions on global childhood developmental outcomes. In the present study, we have, to our knowledge, assessed for the first time the associated between elective birth at 39 weeks’ gestation and developmental vulnerability. We have also compared the 2 modes of elective birth (induction of labor and planned cesarean delivery). We used data from triennial assessments conducted by teachers across the state, providing a holistic measure of childhood development at school entry beyond just educational performance. Importantly, a child’s developmental performance at school entry has been shown to have a strong and persistent association with primary school performance.12 Furthermore, developmental vulnerability identified through the AEDC is associated with poor numeracy and literacy skills in school grades 3,15 5, and 7.12,16
Although the ARRIVE trial provided robust evidence of the safety of induction of labor at 39 weeks’ gestation vs expectant management for perinatal outcomes,1 there have been no randomized clinical trials assessing longer-term childhood outcomes. Previous cohort studies have investigated gestational age at birth and childhood outcomes. It is well established that preterm birth is associated with an increased risk of poor childhood outcomes,17,18,19 but outcomes for those who deliver at term and postterm gestations have not been well studied. Late-term birth has been associated with improved cognitive20 but poorer physical21 outcomes. Studies of mode of birth have been inconclusive. Children born via planned cesarean delivery have been reported to be at increased risk of early childhood delay when compared with “normal births.”22 Other studies have reported no difference in third-grade outcomes between children born via planned cesarean delivery and those born via unassisted vaginal birth.23 We note that none of these prior studies have focused on clinical decision-making around elective birth at 39 weeks’ gestation and the mode of elective birth at this gestation.
Limitations
This study has some limitations. Because this was a population-based cohort study, there were inherent baseline differences between exposure groups and missing data. To overcome this limitation, an a priori statistical analysis plan based on a causal inference framework11 was used. This approach used an inverse probability weighted regression adjusted model as an attempt to mimic the randomization of a controlled trial. The success of this model is demonstrated by achieving adequate covariate balance and sufficient overlap between exposure groups after inverse probability weighting. However, it is possible that unmeasured confounding or model misspecification could have led to bias in estimating the average treatment outcomes. To overcome the potential biases of missing data, we performed multiple imputation for covariates included in our model and compared results using complete case and imputed data.
Conclusions
In this statewide, population-based cohort study, elective birth at 39 weeks’ gestation was not associated with an altered risk of developmental vulnerability at school entry. These findings offer reassurance about the long-term impact of elective birth at 39 weeks’ gestation and provide information that may assist in shared decision-making with patients when planning birth.
eAppendix. A priori statistical analysis plan
eTable 1. Primary analyses using complete (nonmissing) case data
eTable 2. Primary analyses using alternative modelling techniques
eTable 3. Secondary analysis of mode of birth at 39 weeks’ gestation and developmental vulnerability using complete case (nonmissing) data
References
- 1.Grobman WA, Rice MM, Reddy UM, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network . Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379(6):513-523. doi: 10.1056/NEJMoa1800566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grobman WA, Caughey AB. Elective induction of labor at 39 weeks compared with expectant management: a meta-analysis of cohort studies. Am J Obstet Gynecol. 2019;221(4):304-310. doi: 10.1016/j.ajog.2019.02.046 [DOI] [PubMed] [Google Scholar]
- 3.Clinical Guidance for Integration of the Findings of the ARRIVE Trial: labor induction versus expectant management in low-risk nulliparous women. Accessed April 5, 2022. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2018/08/clinical-guidance-for-integration-of-the-findings-of-the-arrive-trial
- 4.Middleton P, Shepherd E, Crowther CA. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2018;5(5):CD004945. doi: 10.1002/14651858.CD004945.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacKay DF, Smith GC, Dobbie R, Pell JP. Gestational age at delivery and special educational need: retrospective cohort study of 407,503 schoolchildren. PLoS Med. 2010;7(6):e1000289. doi: 10.1371/journal.pmed.1000289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yisma E, Mol BW, Lynch JW, Mittinty MN, Smithers LG. Elective labor induction vs expectant management of pregnant women at term and children’s educational outcomes at 8 years of age. Ultrasound Obstet Gynecol. 2021;58(1):99-104. doi: 10.1002/uog.23141 [DOI] [PubMed] [Google Scholar]
- 7.Werner EF, Schlichting LE, Grobman WA, Viner-Brown S, Clark M, Vivier PM. Association of term labor induction vs expectant management with child academic outcomes. JAMA Netw Open. 2020;3(4):e202503-e202503. doi: 10.1001/jamanetworkopen.2020.2503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patterson JA, Roberts CL, Ford JB, Morris JM. Trends and outcomes of induction of labour among nullipara at term. Aust N Z J Obstet Gynaecol. 2011;51(6):510-517. doi: 10.1111/j.1479-828X.2011.01339.x [DOI] [PubMed] [Google Scholar]
- 9.Laughon SK, Zhang J, Grewal J, Sundaram R, Beaver J, Reddy UM. Induction of labor in a contemporary obstetric cohort. Am J Obstet Gynecol. 2012;206(6):486.e1-486.e9. doi: 10.1016/j.ajog.2012.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekéus C, Lindgren H. Induced labor in Sweden, 1999-2012: a population-based cohort study. Birth. 2016;43(2):125-133. doi: 10.1111/birt.12220 [DOI] [PubMed] [Google Scholar]
- 11.Hernán MA. Methods of public health research—strengthening causal inference from observational data. N Engl J Med. 2021;385(15):1345-1348. doi: 10.1056/NEJMp2113319 [DOI] [PubMed] [Google Scholar]
- 12.Brinkman S, Zubrick S, Silburn S. Predictive validity of a school readiness assessment on later cognitive and behavioral outcomes. Accessed October 22, 2021. https://www.aedc.gov.au/resources/detail/the-predictive-validity-of-the-aedc-predicting-later-cognitive-and-behavioural-outcomes
- 13.Stata Statistical Software . Release 17 [computer program]. College Station, TX: StataCorp LLC; 2021.
- 14.Gülmezoglu AM, Crowther CA, Middleton P, Heatley E. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2012;6(6):CD004945. doi: 10.1002/14651858.CD004945.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Connor M, Chong S, Quach J, Goldfeld S. Learning outcomes of children with teacher-identified emerging health and developmental needs. Child Care Health Dev. 2020;46(2):223-231. doi: 10.1111/cch.12737 [DOI] [PubMed] [Google Scholar]
- 16.Brinkman S, Gregory T, Harris J, Hart B, Blackmore S, Janus M. Associations between the early development instrument at age 5, and reading and numeracy skills at ages 8, 10 and 12: a prospective linked data study. Child Indic Res. 2013;6(4):695-708. doi: 10.1007/s12187-013-9189-3 [DOI] [Google Scholar]
- 17.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288(6):728-737. doi: 10.1001/jama.288.6.728 [DOI] [PubMed] [Google Scholar]
- 18.Dhamrait GK, Christian H, O’Donnell M, Pereira G. Gestational age and child development at school entry. Sci Rep. 2021;11(1):14522. doi: 10.1038/s41598-021-93701-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allotey J, Zamora J, Cheong-See F, et al. Cognitive, motor, behavioural and academic performances of children born preterm: a meta-analysis and systematic review involving 64 061 children. BJOG. 2018;125(1):16-25. doi: 10.1111/1471-0528.14832 [DOI] [PubMed] [Google Scholar]
- 20.Chan E, Leong P, Malouf R, Quigley MA. Long-term cognitive and school outcomes of late-preterm and early-term births: a systematic review. Child Care Health Dev. 2016;42(3):297-312. doi: 10.1111/cch.12320 [DOI] [PubMed] [Google Scholar]
- 21.Figlio DN, Guryan J, Karbownik K, Roth J. Long-term cognitive and health outcomes of school-aged children who were born late-term vs full-term. JAMA Pediatr. 2016;170(8):758-764. doi: 10.1001/jamapediatrics.2016.0238 [DOI] [PubMed] [Google Scholar]
- 22.Hanrahan M, McCarthy FP, O’Keeffe GW, Khashan AS. The association between caesarean section and cognitive ability in childhood. Soc Psychiatry Psychiatr Epidemiol. 2020;55(9):1231-1240. doi: 10.1007/s00127-019-01798-4 [DOI] [PubMed] [Google Scholar]
- 23.Ayala NK, Schlichting LE, Kole MB, et al. Operative vaginal delivery and third grade educational outcomes. Am J Obstet Gynecol MFM. 2020;2(4):100221. doi: 10.1016/j.ajogmf.2020.100221 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. A priori statistical analysis plan
eTable 1. Primary analyses using complete (nonmissing) case data
eTable 2. Primary analyses using alternative modelling techniques
eTable 3. Secondary analysis of mode of birth at 39 weeks’ gestation and developmental vulnerability using complete case (nonmissing) data