Abstract
Objective
Clinical research has faced new challenges during the COVID-19 pandemic, leading to excessive operational demands affecting all stakeholders. We evaluated the impact of COVID-19 on clinical research strategies and compared different adaptations by regulatory bodies and academic research institutions in a global context, exploring what can be learned for possible future pandemics.
Methods
We conducted a cross-sectional online survey and identified and assessed different COVID-19-specific adaptation strategies used by academic research institutions and regulatory bodies.
Results
All 19 participating academic research institutions developed and followed similar strategies, including preventive measures, manpower recruitment, and prioritisation of COVID-19 projects. In contrast, measures for centralised management or coordination of COVID-19 projects, project preselection, and funding were handled differently amongst institutions. Regulatory bodies responded similarly to the pandemic by implementing fast-track authorisation procedures for COVID-19 projects and developing guidance documents. Quality and consistency of the information and advice provided was rated differently amongst institutions.
Conclusion
Both academic research institutions and regulatory bodies worldwide were able to cope with challenges during the COVID-19 pandemic by developing similar strategies. We identified some unique approaches to ensure fast and efficient responses to a pandemic. Ethical concerns should be addressed in any new decision-making process.
Keywords: COVID-19, pandemic, clinical trial unit, academic research institution, clinical research, research ethics, regulatory authorities, trial management, central trial coordination, rapid review
Introduction
Pandemics or infectious disease outbreaks, such as the COVID-19 public health crisis, require fast and efficient adaption and response to save as many lives as possible. Consequently, it is essential to conduct coordinated clinical research into therapeutics, vaccines, diagnostics, protective equipment, and disease characteristics during a pandemic. This leads to excessive operational demands for all stakeholders in clinical research. In the COVID-19 pandemic, academic research institutions have had to adapt to conducting and supporting a large number of COVID-19 studies, and regulatory bodies (i.e., regulatory authorities, research ethics committees, and governmental health departments) have also had to adapt so as to rapidly review related research projects. At the same time, the health of research staff and study participants involved in non-COVID-19 clinical research projects has had to be protected. For this reason, many countries and jurisdictions decided to impose partial or full lockdowns at different points during the COVID-19 pandemic, including travel restrictions. Owing to all of these factors, it has become necessary for established operating models and procedures among various stakeholders to be adapted and remodelled in a timely manner.
The Ebola outbreak in 2014 revealed important ethical issues, including performing clinical research in the middle of an infectious disease outbreak, allocating scarce resources, and restricting freedom of movement. To address these issues, the World Health Organization (WHO) developed the “Guidance for Managing Ethical Issues in Infectious Disease Outbreaks.” The guidance underlines the moral commitment to promote and conduct scientific research on short notice. 1 In 2020, there were 9873 registrations of COVID-19-related clinical studies in the WHO International Clinical Trials Registry Platform (with search settings restricted to COVID-19 and date of registration in 2020). 2 The WHO itself is supporting and facilitating collaboration and accelerated efforts in research by conducting large global platform trials, such as the Solidarity Therapeutics Trial. 3
In the COVID-19 pandemic, constraints of time and personnel resources together with prioritisation of COVID-19 studies has challenged many ethical principles in the conduct of medical research involving human subjects, as addressed in the Declaration of Helsinki.4–7 Moreover, the prioritisation of COVID-19 projects has severely impaired the conduct of non-COVID-19 clinical research and may therefore negatively affect future treatment options in standard health care.8–11 Consequently, the European Union and countries like Switzerland and Turkey have released guidelines for managing ongoing research studies.12–14 However, national and international coordination is still lacking.
In this article, we summarise, compare, and evaluate different adaptations made by academic research institutions and regulatory bodies in a global context and explore what can be learned in preparation for possible future pandemics.
Methods
Study design
We designed a cross-sectional survey-based study, which was administered within the International Clinical Trial Center Network (ICN) and associated institutions. The reporting of this study conforms to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines. 15
This study did not use any personal data from survey respondents. The study does not fall within the scope of the Swiss Human Research Act and hence did not require ethics approval or informed consent.
Survey conception
To identify and assess adaptations among different academic research institutions (clinical trial units, CTUs) and regulatory bodies for procedures specific to COVID-19, we designed a standardised questionnaire. Key topics were identified through informal discussions with representatives of different CTUs around the world. These inputs, as well as results from a literature search, were incorporated into the survey. For each question, participants could elaborate on their responses in a free-text section. To ensure consistency and comprehensibility, the questionnaire was divided into five subcategories: 1) general information, 2) local COVID-19 situation, 3) institutional organisation and situation, 4) approaches for review and approval procedures of COVID-19 projects, and 5) what can be learned in preparation for possible future pandemics.
The survey was refined and finalised after review and input from the ICN COVID-19 working group. The final version (File 1) consisted of 40 questions and was transferred to the SurveyMonkey platform, 16 which allowed us to compose questions on a modular basis.
Survey population and procedure
The survey population comprised members of the ICN and ICN-associated academic research institutions. Several survey respondents became part of the present author group, which was established after the analysis of survey results to ensure correct interpretation of results.
On 19 August 2020, invitation emails containing a short instruction and the SurveyMonkey web link were sent to the survey population seeking feedback on institutional or regulatory adaptations to COVID-19 in the respective countries/jurisdictions or regions. The survey was open for 1 month and was closed on 16 September 2020. Reminders were sent on 2 September and 9 September 2020.
Data management and analysis
Quantitative analysis was performed using standard descriptive methods in Microsoft Excel (Microsoft Corporation, Redmond, Washington, USA). Information entered in free-text or comment fields was reviewed and manually tabulated. Missing data were handled using pairwise deletion.
Results
Population overview
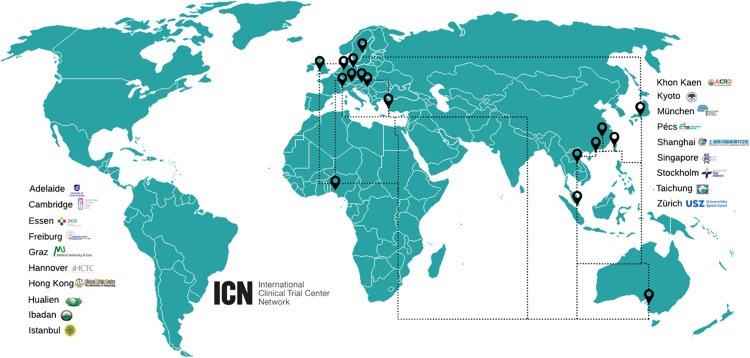
We received 19 responses from among 22 survey invitations (86.4% response rate), which included representatives of institutions in 14 different countries/jurisdictions of Asia, Europe, Africa, and Australia (Figure 1). Whenever possible, surveys were completed and verified by more than one representative of the respective institution to guarantee appropriateness and consistency. Respondents were from an array of specialties and subspecialties, including quality management, project coordination, monitoring, education and training, medical professionals, and institutional management. The completion rate of the survey was 95%.
Figure 1.
World map including all survey respondents.
Institutional organisation and situation during the COVID-19 pandemic
Research institutions responded to challenges arising from COVID-19 pandemic by adapting on different levels. This included the organisation of staff, institutional adaptations of operational modes or functions, and the management and coordination of clinical research projects (Table 1).
Table 1.
Adaptations at different levels implemented by research institutions in response to COVID-19.
| Level | Item |
|---|---|
| Staff |
|
| Institution |
|
| Management of clinical trials |
|
On an institutional organisation level, all respondents reported taking similar approaches to adapt to the COVID-19 pandemic situation, with 95% introducing full-time or part-time home office work for their employees. However, only half of research institutions had already implemented well-functioning remote systems. Further established measures included shift work, redeployment of staff, hygiene and preventive measures (i.e., hand disinfection, face masks, temperature checks, physical distancing, and restriction of business trips), fast and productive communication lines (e.g., targeted meetings, instant conference calls, virtual meetings), as well as internal training and knowledge transfer.
During the pandemic, half of all respondents experienced a full (4/19) or partial (6/19) restructuring of their functions, particularly regarding staff allocation to dedicated COVID-19 wards, intensive care units, and clinical study sites. Most research institutions also introduced visitor restrictions, workplace disinfection protocols, and regular internal updates on COVID-19 cases.
Management and coordination of COVID-19 clinical studies were handled in different manners amongst institutions. COVID-19 projects were generally prioritised by most research institutions (94%). In comparison, many non-COVID-19 projects were put on hold (90%) depending on the risk–benefit ratio of individual studies (e.g., medical importance, vulnerability of research population, and study status). Nevertheless, structured (pre)selection systems for COVID-19 projects were implemented by only 4 of 19 survey respondents. In these respective research institutions, COVID-19 studies were evaluated by newly established institutional COVID-19 decision boards, which either prioritised or rejected the submitted projects. In the context of prioritising COVID-19 projects, the workload for non-COVID-19 projects decreased (42.1%) or remained consistent (42.1%). Only 15% of respondents experienced an increased workload for non-COVID-19 projects. Altogether, 58% of respondents reported that they experienced a higher overall workload during the pandemic, particularly clinical research specialists (e.g., CTU staff, study nurses, and investigators), physicians, and nurses. The increased demand for support in ethics/regulatory submissions, study conduct, regulatory questions, and grant applications led to an elevated workload for CTUs and academic research institutions. Most respondents (93.3%) reported that they experienced a much faster set-up of clinical studies during the pandemic compared with normal conditions. This was mainly achieved via dynamic staff allocation, extended working hours, efficient communication, centralised coordination, fast protocol development, and regulatory and institutional fast-track authorisation processes.
Most COVID-19 projects conducted or supported by academic research institutions were interventional clinical trials, followed by observational studies, registries, and biobanks. The most in-demand CTU supports in the context of COVID-19 studies involved essential tasks during the stages of study preparation (i.e., submissions, timelines, prioritisation, and medical writing) and study conduct (i.e., informed consent, sample handling, safety monitoring and reporting, registries, and further use of data and samples).
Financing of COVID-19 projects was reported to be handled differently, depending on the country/jurisdiction, region, and institution. Funding and grants from research institutions, governments, foundations, commercial/private organisations, and universities, as well as collaborations with industry, were mentioned as the main financial resources.
Approaches to approval procedures for COVID-19 projects
Apart from academic research institutions adapting to the pandemic situation, regulatory bodies also implemented measures to face the challenges arising from COVID-19 (Table 2). Most respondents stated that COVID-19 studies were organised in a centralised manner (14/19), either on a national (3/14) or institutional (5/14) level, or both (6/14). Fast-track authorisation procedures for COVID-19 studies were implemented in all countries/jurisdictions and regions.
Table 2.
Adaptations implemented by regulatory bodies in response to COVID-19.
| Items |
|---|
|
Regulatory guidance for clinical studies during the COVID-19 pandemic was reported to be available for academic research institutions and CTUs (14/17) in most countries. Guidance documents included instructions concerning monitoring, approval processes, management of Good Clinical Practice issues, amendments, and project selection. These were provided by ethics committees and regulatory authorities at continent (e.g., Europe) or national levels, governmental health departments, and industry. Nevertheless, some respondents mentioned that guidance documents were developed quickly but did not cover all issues arising from the COVID-19 situation. Therefore, additional communication with regulatory bodies was necessary in some cases, which was reported to be uncomplicated by most respondents (11/17). Among the total, 79% of research institutions were able to directly contact regulatory bodies to discuss topics in the context of COVID-19 research and rated the information received from and interactions with the regulatory systems (e.g., ethics committees and governmental authorities) as mostly satisfactory (average rating of 7.8 with a range 1–10).
Discussion
On the basis of responses to our survey, we identified some unique approaches and best practices to ensure rapid and efficient responses to a pandemic situation, which we discuss below (Table 3).
Table 3.
Recommendations on how to ensure and expedite high-quality clinical research in pandemic situations.
| Clinical trial units/researchinstitutions | Protection of staff and study volunteers by implementing preventive measures (i.e., hygiene measures, remote working, and restriction of visitors). |
| Preselection of studies by establishing regional or institutional scientific review boards that allow for centralised and non-competitive study coordination to ensure high-quality research. | |
| Flexible redeployment and adequate training of staff to expedite efficient and high-quality set-up of COVID-19-related studies while sustaining important non-COVID-19 studies. | |
| Development of strategies that are not disadvantageous to non-COVID-19 research areas. A thorough risk–benefit assessment is recommended in all cases. | |
| Regulatory bodies | Implementation of fast-track authorisation procedures for COVID-19 research while maintaining an adequate balance between the speed and quality of project assessment. |
| Development of nationally, regionally, and/or internationally standardised guidelines to avoid inconsistency and confusion among research institutions and other stakeholders in clinical research. |
Newly adapted institutional approaches may raise ethical concerns
Academic research institutions were shown to react quickly to new circumstances in the COVID-19 pandemic so as to cope with the rapid upsurge in demand. These institutions developed and followed similar strategies, which now must be evaluated to prepare for possible future pandemics as well as to improve standard processes after a return to normalcy. Reorganisation of CTUs provides new possibilities but may also lead to problems owing to premature decisions and increased workload.
Staff organisation
Remote working, hygiene and preventive measures, as well as allocation of staff to COVID-19-specific tasks were implemented by nearly all research institutions in this study. It must be taken into account that staff redeployment in particular may lead to quality impairment owing to insufficient training, lack of practical experience, extra workload, and time pressure. Therefore, as a preventive tool, it is crucial to ensure adequate training and knowledge transfer for redeployed personnel.
To fulfil governmental requirements and restrictions in future pandemics, academic research institutions would undoubtedly benefit from well-functioning remote systems, pandemic plans and guidelines, and a matrix organisation of staff comprising staff allocation, training, and communication.
Prioritisation of COVID-19 clinical research projects
All participating research institutions prioritised COVID-19 projects over non-COVID-19 projects, many of which were put on hold depending on their risk–benefit ratio. This approach was considered beneficial with regard to workload. However, the reduction or pausing of non-COVID-19 research was not only related to regulatory guidelines or decisions by CTUs but also to logistical consequences of the pandemic, such as limited participant recruitment owing to lockdowns or patient reticence, and reduced resources with respect to staff because of sick leave. Furthermore, high numbers of hospitalisations in countries worldwide made the search for medical treatments and vaccines an urgent matter to prevent the collapse of health care systems; this explains the enormous shift in resources to COVID-19 research. Hence, the reduction of non-COVID-19 research cannot be considered a violation of ethical principles per se, but this may nevertheless raise ethical concerns. Discontinuation or pausing of non-COVID-19 projects may not only result in limited disease treatments owing to the fact that physicians cannot provide psychosocial support in consultations because of time constraints, and interrupted surveillance of medical conditions and treatments, this also may cause financial issues owing to reduced funding, suspension of collaborations, or the need to sustain the workforce and resources for research projects. 17 Non-COVID-19 studies are also disadvantaged in terms of the enhanced participant recruitment for COVID-19 studies.11,18 Non-COVID-19 studies and non-COVID-19 diseases have therefore been indirectly judged as less important.
The urgency of combating COVID-19 is undeniable. However, without clinical studies, there can be no progress in developing treatments for other widespread and life-threatening diseases like cancer, malaria, and HIV. Therefore, COVID-19 can be considered a new source of human suffering but one that should not take the place of other diseases in terms of prioritisation.8–10 The main goal of clinical research should be the maximisation of public health benefits. 17 However, it is difficult to establish a general definition regarding which groups comprise the relevant “public” and what should be considered a “benefit”. 19 Furthermore, an oversupply of research opportunities may negatively affect study participants in terms of overload and pressure.
In the future, it is advisable to formulate strategies that are not disadvantageous to research in some areas. A thorough risk–benefit assessment should be carried out for every non-COVID-19 study, focusing not only on the risks of potential COVID-19 infection but also on the risks of not having access to non-COVID-19 interventional clinical trials, as well as other negative effects such as socioeconomic factors.
Advantage of scientific review boards and central coordination
Reduced study set-up time was experienced by most respondents, which may have a negative impact on data quality and study participant safety because the quality of study planning, set-up, and conduct are likely to be adversely affected by competition and time pressure. However, the Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial showed that quality and speed of a study set-up can go hand in hand. The RECOVERY project was initiated in March 2020 in the United Kingdom (UK), aiming to identify treatments that may be beneficial for people hospitalised with suspected or confirmed COVID-19 infection. The first patient was enrolled just 2 days after the protocol was approved and 9 days after the protocol was finalised. The first 1000 patients were enrolled in only 16 days, peaking with enrolment of 500 patients per day. The first positive result (regarding the benefit of dexamethasone treatment) was reported only 3 months after study initiation. As of 2 March, 2022, RECOVERY was extended to 194 active sites in six countries, over 47,000 patients were enrolled, 16 treatments were included, and nine conclusions reached. The fast set-up and high enrolment number were owing to the priority status given to RECOVERY by the National Institute for Health Research in the UK.20–22
Importantly, the present urgent situation should not be used to promote unnecessary research or as an excuse for lowering scientific standards. Important information is needed to advance individual and public health during a pandemic as well as under normal conditions. The implementation of scientific review boards (institutional or national) can facilitate the selection of relevant research questions by surveying the landscape of ongoing studies. Established mechanisms for “priority review” and personnel allocation will be valuable for supporting the selection, planning, set-up, and conduct of high-quality projects.
A framework for institutional, national, or regional scientific review boards should be established to review, organise, and prioritise COVID-19 studies. This will avoid the conduct of non-essential or low-quality research and sustain important non-COVID-19 research. Furthermore, centralised and non-competitive coordination of COVID-19 projects would prevent project duplication and ensure a fair distribution of resources. Despite the considerable pressure concerning fast, valuable, and significant study outcomes, study participant safety and data quality should always be given top priority.
Internationally standardised guidelines to support fast-track approval of COVID-19 projects
All participating academic research organisations reported that their regulatory bodies provided fast-track authorisation procedures for COVID-19 projects. For example, COVID-19 studies in Switzerland were approved within 1 week, on average, instead of 24 days. 13 Ethical issues concerning time sensitivity, study quality, and participant safety in a rapid review were addressed during the Ebola outbreak in 2014 as well as within the current context of the COVID-19 pandemic.5,23–25
In addition to the rapid evaluation of COVID-19-related studies by regulatory authorities, a recently published study by Jung et al. remarked on the accelerated publication process and lower quality of COVID-19 clinical research in comparison with historical non-COVID-19 clinical research. 26 As observed with the proposed use of hydroxychloroquine as a COVID-19 treatment early during the pandemic, limited data and lower-quality clinical studies can cause scepticism regarding the scientific findings of COVID-19 clinical trials.27–29 Therefore, an adequate balance between the speed and quality of project assessment is crucial.5,23,30 To support this concept, the WHO has developed a guideline for research ethics committees conducting rapid reviews of research during a public health emergency. 31 However, it must be considered that ethics committees, independent review boards, and other regulatory bodies do not bear sole responsibility. Other stakeholders like sponsors, researchers, funders, regulatory bodies, research institutions, and the affected communities are also responsible for upholding the ethical principles in human research. 23
The availability and quality of guidance documents and support received by regulatory authorities in the countries/jurisdictions were mixed in our study. To prepare for possible future pandemics, it is advisable to develop nationally, regionally, and/or internationally standardised guidelines to avoid inconsistency and confusion among research institutions and other stakeholders in clinical research.
A look at the United States
The literature shows that COVID-19 disrupted all aspects of clinical care in the United States (US), including clinical trials. Research organisations and regulatory bodies provided guidance documents and developed new policies to address safety and scientific challenges with respect to conducting clinical trials in a pandemic environment. The U.S. Food and Drug Administration (FDA) and regulatory agencies released guidance for industry, investigators, and institutional review boards, including recommendations on risk assessment for all research projects, establishment or revision of policies and procedures, risk-based pausing of enrolment, remote/virtual study visits, delay of visits and extension of trial/visit windows, and remote monitoring. 32
Furthermore, the National Institutes of Health advised investigators to discuss with their institutional review boards and institutions the establishment of potential measures to protect participants and research staff. In our study, responses from academic research institutions varied from mandatory suspension of research projects involving human participants (except when this increased the risk to participants) to relying on principal investigator discretion. 33 Furthermore, ethics committees experienced a very high workload as researchers submitted requests to modify their clinical trial plans in ways that would minimise participant visits to the clinic and research facilities. 33
A notable measure was the announcement by the US National Cancer Institute allowing investigators to remotely assess the health of trial participants. Audits of clinical trial procedures and inspections were also conducted remotely rather than by visiting clinics to assess standards.34,35
As another example in the US, the Mayo Clinic took the COVID-19 pandemic as a unique opportunity to activate and mobilise a new approach to aligning and accelerating research activities across the Mayo Clinic enterprise. A COVID-19 Research Task Force led by medical, scientific, and administrative leaders was implemented to develop processes for study selection, real-time eligibility assessment of hospitalised patients, alignment of trials with sites in terms of drug availability and patient need, mobilisation of operational teams, and creation of bidirectional communication channels. By doing so, the COVID-19 Research Task Force has enabled scientific, patient care, and administrative thought leaders to accelerate and align research focused on the unmet needs of COVID-19 patients. 36
It is important to note that there is room for improvement in regulatory coordination and standardisation of pandemic and non-COVID-19 research in the US. To illustrate this fact, there have been an excessive number of trials authorised with essentially the same research objectives. For example, there have been at least 18 clinical research projects investigating hydroxychloroquine in the US alone, involving more than 75,000 patients. 9
Study limitations
We have invested considerable effort to involve different stakeholders, representative CTUs, and academic research institutions from all over the world in the present work. We consider the 19 respondents from 14 countries/jurisdictions and the completion rate of approximately 95% to be satisfactory because we could not cover all regions globally. However, our study findings may not be generalisable to those regions that were not included in the survey. This limitation particularly applies to North and South America, which are underrepresented in our results. For this reason, we included the section “A look at the United States,” to provide information from the US literature.
Only representatives of ICN members, which are all academic governmental institutions, participated in the survey. Future studies should examine whether private research institutions and research institutions outside the ICN developed different strategies during the COVID-19 pandemic.
Additionally, some authors of this paper were also survey respondents. This may have introduced bias to some extent. However, we see this as an important advantage for correct interpretation, discussion, and confirmation of the survey results as well as for capturing more detailed insights and information. Furthermore, the author group was established after analysis of the survey results to avoid any influence on the results.
Conclusion
Both academic research institutions and regulatory bodies were able to cope with the challenging situation brought about by the COVID-19 pandemic. Our study showed that institutions worldwide developed and followed similar strategies, with a few exceptions. We suggest that this underlines a convergent understanding among clinical research stakeholders of problem-oriented approaches in a pandemic situation. We identified some unique approaches and best practices to ensure fast and efficient responses in a pandemic. Our findings highlight the importance of well-functioning research infrastructure to promote and maintain high-quality, valuable, and efficient clinical research. An adequate balance among speed, quality, and risk is crucial, and the importance of non-COVID-19 research should not be ignored. The safety and well-being of study participants, whether in COVID-19-related or non-COVID-19 research, must always be the first priority.
In preparation for the future, regular exchange of knowledge and experiences among countries/jurisdictions and research institutions will help to further improve their respective strategies. We are confident that our study findings will contribute to the understanding of how to improve, ensure, and expedite high-quality clinical research in pandemic situations while maintaining the safety of study participants.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605221093179 for How COVID-19 changed clinical research strategies: a global survey by Annina Bauer, Anja Eskat, Atara Ntekim, Creany Wong, Deborah Eberle, Elham Hedayati, Fabian Tay, Henry Yau, Louise Stockley, María de Medina Redondo, Selçuk Şen, Silvia Egert-Schwender, Yağız Üresin and Regina Grossmann in Journal of International Medical Research
Acknowledgements
The authors thank the ICN for encouraging and supporting this project. In particular, the authors gratefully acknowledge the efforts of our survey respondents who took their valuable time to participate in this work.
Footnotes
Declaration of competing interests: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The ICN has no financial interest in this work.
Additional information: ICN Network
The ICN is an international network of academic clinical trial centres built on the core values of Global, Excellence, Harmonization, and Impacts. The mission of the ICN is to enhance the global availability of high-quality clinical research centres and study sites by promoting and supporting the top-level services and proven capabilities of the ICN and its members. Through close and coordinated contact amongst its members, the ICN is able to connect teams and relevant stakeholders in clinical research. The top priority is to enable advanced study centres to join forces and young study centres to build up their clinical research infrastructure and expertise.
ORCID iD: Annina Bauer https://orcid.org/0000-0002-5379-7418
References
- 1.World Health Organization. Guidance for managing ethical issues in infectious disease [Internet]. 2016. [cited 2021 Aug 16]. Available from: https://apps.who.int/iris/bitstream/handle/10665/250580/9789241549837-eng.pdf?sequence=1&isAllowed=y
- 2.World Health Organization. International Clinical Trials Registry Platform (ICTRP) [Internet]. [cited 2021. Sep 6]. Available from: https://www.who.int/clinical-trials-registry-platform
- 3.WHO–Solidarity [Internet]. WHO COVID-19 Solidarity Therapeutics Trial. 2022. [cited 2022 Feb 28]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments
- 4.Meagher KM, Cummins NW, Bharucha AE, et al. COVID-19 Ethics and Research. Mayo Clin Proc 2020; 95: 1119–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bahans C, Leymarie S, Malauzat D, et al. Ethical considerations of the dynamics of clinical trials in an epidemic context: Studies on COVID-19. Ethics Med Public Health 2021; 16: 100621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kramer JB, Brown DE, Kopar PK. Ethics in the Time of Coronavirus: Recommendations in the COVID-19 Pandemic. J Am Coll Surg 2020; 230: 1114–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The World Medical Association (WMA). World Medical Association Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects [Internet]. 2013. [cited 2021 Aug 13]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ [DOI] [PubMed]
- 8.Lalova T, Negrouk A, Deleersnijder A, et al. Conducting Non-COVID-19 Clinical Trials during the Pandemic: Can Today’s Learning Impact Framework Efficiency? Eur J Health Law 2020; 27: 425–450. [DOI] [PubMed] [Google Scholar]
- 9.London AJ, Kimmelman J. Against pandemic research exceptionalism. Science 2020; 368: 476–477. [DOI] [PubMed] [Google Scholar]
- 10.Yanow SK, Good MF. Nonessential Research in the New Normal: The Impact of COVID-19. Am J Trop Med Hyg 2020; 102: 1164–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelinas L, Lynch HF, Bierer BE, et al. When clinical trials compete: prioritising study recruitment. J Med Ethics 2017; 43: 803–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.European Medicines Agency, and Clinical Practice Inspectors WG, Clinical Trials Facilitation and Coordination Group, Clinical Trials Expert Group, European Commission. Guidance on the management of clinical trials during the COVID-19 (coronavirus) pandemic, V4 [Internet]. 2021. [cited 2021 Aug 13]. Available from: https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-10/guidanceclinicaltrials_covid19_en.pdf
- 13.Swissmedic, swissethics. Joint Guidance of Swissmedic and swissethics on the management of clinical trials with medicinal drug products in Switzerland during the COVID-19 pandemic; Version 2.4 [Internet]. 2020 [cited 2021. Sep 23]. Available from: https://swissethics.ch/covid-19/guidance-docs
- 14.Turkish Medicine and Medical Device Agency. COVID-19 Pandemisi Nedeniyle Klinik Araştırmalarda Alınacak Tedbirler. V2.0 [Internet]. 2020. [cited 2021 Sep 23]. Available from: https://titck.gov.tr/storage/Archive/2020/announcement/COVID19KATedbirlerv2.0_ed21cd3b-4e35-4ff1-a109-f74540a2683b.pdf
- 15.O’Brien BC, Harris IB, Beckman TJ, et al. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Acad Med 2014; 89: 1245–1251. [DOI] [PubMed] [Google Scholar]
- 16.SurveyMonkey. Free online survey software and questionnaire tool [Internet]. SurveyMonkey. [cited 2021. Sep 6]. Available from: https://www.surveymonkey.com/welcome/sem/
- 17.Emanuel EJ, Wendler D, Grady C. What Makes Clinical Research Ethical? JAMA 2000; 283: 2701–2711. [DOI] [PubMed] [Google Scholar]
- 18.Wieten S, Burgart A, Cho M. Resource Allocation in COVID-19 Research: Which Trials? Which Patients? Am J Bioeth 2020; 20: 86–88. [DOI] [PubMed] [Google Scholar]
- 19.Giubilini A, Savulescu J, Wilkinson D. Queue questions: Ethics of COVID‐19 vaccine prioritization. Bioethics 2021; 35: 348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nuffield Department of Population Health, Health OP. RECOVERY [Internet]. RECOVERY–Randomised Evaluation of COVID-19 Therapy. 2022. [cited 2022 Mar 2]. Available from: https://www.recoverytrial.net
- 21.Clinicaltrials.gov [Internet]. RECOVERY. [cited 2022. Mar 2]. Available from: https://clinicaltrials.gov/ct2/show/NCT04381936
- 22.Goossens H, Derde L, Horby P, et al. The European clinical research response to optimise treatment of patients with COVID-19: lessons learned, future perspective, and recommendations. Lancet Infect Dis 2021; S1473–30992100705–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reyes M. Research in the Time of COVID-19: Challenges of Research Ethics Committees. JAFES 2020; 35: 29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunt M, Tansey CM, Anderson J, et al. The Challenge of Timely, Responsive and Rigorous Ethics Review of Disaster Research: Views of Research Ethics Committee Members. Zhou X, editor. PLoS ONE 2016; 11: e0157142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schopper D, Ravinetto R, Schwartz L, et al. Research Ethics Governance in Times of Ebola. Public Health Ethics 2017; 10: 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jung RG, Di Santo P, Clifford C, et al. Methodological quality of COVID-19 clinical research. Nat Commun 2021; 12: 943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magagnoli J, Narendran S, Pereira F, et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. Med 2020; 1: 114–127. 10.1016/j.medj.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glasziou PP, Sanders S, Hoffmann T. Waste in Covid-19 research–A deluge of poor quality research is sabotaging an effective evidence based response. BMJ 2020; 369: m1847. [DOI] [PubMed] [Google Scholar]
- 29.Vinetz JM. Lack of efficacy of hydroxychloroquine in Covid-19. BMJ 2020; 369: m2018. [DOI] [PubMed] [Google Scholar]
- 30.Swissmedic. Guidance document. Authorisation procedures for Covid-19 medicinal products during a pandemic [Internet]. 2021. [cited 2021 Aug 12]. Available from: https://www.swissmedic.ch/swissmedic/en/home/news/coronavirus-covid-19/zl_am_praevention_covid19_erkrankung.html
- 31.World Health Organization. Guidance for research ethics committees for rapid review of research during public health emergencies [Internet]. 2020. [cited 2021 Aug 12]. Available from: https://www.who.int/publications/i/item/9789240006218
- 32.US Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 pandemic: guidance for industry, investigators, and institutional review boards [Internet]. 2020. [cited 2022 Mar 2]. Available from: https://www.fda.gov/media/136238/download
- 33.McDermott MM, Newman AB. Preserving Clinical Trial Integrity During the Coronavirus Pandemic. JAMA 2020; 323: 2135–2136. [DOI] [PubMed] [Google Scholar]
- 34.Ledford H. Coronavirus shuts down trials of drugs for multiple other diseases. Nature 2020; 580: 15–16. [DOI] [PubMed] [Google Scholar]
- 35.Waterhouse DM, Harvey RD, Hurley P, et al. Early Impact of COVID-19 on the Conduct of Oncology Clinical Trials and Long-Term Opportunities for Transformation: Findings From an American Society of Clinical Oncology Survey. JCO Oncol Pract 2020; 16: 417–421. [DOI] [PubMed] [Google Scholar]
- 36.Burger CD, Mikhail AE, Orenstein R, et al. Research Response to SARS-CoV-2/COVID-19. Mayo Clin Proc 2020; 95: S52–S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605221093179 for How COVID-19 changed clinical research strategies: a global survey by Annina Bauer, Anja Eskat, Atara Ntekim, Creany Wong, Deborah Eberle, Elham Hedayati, Fabian Tay, Henry Yau, Louise Stockley, María de Medina Redondo, Selçuk Şen, Silvia Egert-Schwender, Yağız Üresin and Regina Grossmann in Journal of International Medical Research