Abstract
Background:
Anaemia is a common sequela of advanced disease and is associated with significant symptom burden. No specific guidance exists for the investigation and management of anaemia in palliative care patients.
Aim:
We aim to offer a pragmatic overview of the approaches to investigate and manage anaemia in advanced disease, based on guidelines and evidence in disease specific patient groups, including cancer, heart failure and chronic kidney disease.
Design:
Scoping review methodology was used to determine the strength of evidence supporting the investigation and management of anaemia in patients with advanced disease.
Data sources:
A search for guidelines was performed in 2020. National or international guidelines were examined if they described the investigation or management of anaemia in adult patients with health conditions seen by palliative care services written within the last 5 years in the English language. Searches of MEDLINE, the Cochrane library and WHO guidance were made in 2019 to identify key publications that provided additional primary data.
Results:
Evidence supports patient-centred investigation of anaemia, results of which should guide targeted intervention. Blanket use of blood transfusion should be avoided, with evidence supporting a more restrictive approach to transfusion. Routine use of oral iron and erythropoetin stimulating agents (ESAs) are not recommended. Insufficient evidence exists to determine the effectiveness of IV iron in this patient group.
Conclusion:
We advocate early consideration and investigation of anaemia, guided by symptom burden and patient preferences. Correction of reversible causes should be the mainstay of treatment, with a restrictive approach to blood transfusion. Research is required to evaluate the efficacy of IV iron in these patients.
Keywords: Anaemia, palliative care, guideline, iron, blood transfusion
What is already known about this topic
The majority of palliative patients are anaemic, with a variety of underlying causes.
No guideline exists for the overarching investigation and management of anaemia in palliative care patients, although certain disease states have their own tailored guidelines.
Differences in the approach to investigation and management is common in practice.
What this paper adds
We make recommendations for practice which include investigating the cause of anaemia, consideration of targeted treatments, discussion of risks and benefits of treatments with patients and reducing blood loss.
Implications for practice, theory or policy
Anaemia should not be considered a diagnosis in itself, and should be acknowledged, investigated and management tailored in patients with advanced disease.
The blanket use of red blood cell transfusion should be avoided, with evidence supporting a more restrictive approach to transfusion.
Oral iron and ESAs should not be routinely used in practice.
Further research is required to determine the efficacy of intravenous iron in palliative care patients.
Introduction
Anaemia is a common sequela of advanced disease and can cause symptoms including fatigue and breathlessness.
A study of palliative care patients found that 77% of men and 68.2% of women were anaemic. 1 In terms of severity and cause of anaemia a cohort of 1797 patients with advanced cancer referred to palliative care services showed 38% had moderate to severe anaemia (defined as haemoglobin between 80 and 110 g/dL and below 80 g/dL, respectively). Functional iron deficiency, a component of anaemia of chronic disease was present in 39%–43% of all patients. 2 Anaemia is also common in non-malignant disease. Prevalence in chronic obstructive pulmonary disease can be as high as 33%, with anaemia of chronic disease likely the most common cause.3,4
Despite its prevalence in palliative care patients, no specific guidelines for the management of anaemia in this patient group exist. Some treatments for anaemia, such as red cell transfusion, carry their own risks,5–7 particularly in frail patients with advanced disease. A UK audit of red cell transfusions in hospices found that haematinics (serum B12, folate and iron levels) were not checked in 70% of anaemic patients, highlighting a lack of investigation in this setting. 8 Furthermore, treatments such as B12, folate and iron were rarely used. 8 Although evidence in a specific palliative cohort is lacking, the management of anaemia in actively treated oncology patients demonstrated improvements in symptoms and improved quality of life. 1
Detailed guidance for the management of anaemia exists for several disease specific patient groups, which overlap with palliative care. We aim to offer palliative care professionals practical guidance on the management of anaemia in advanced disease, based on guidelines and evidence in disease specific patient groups, such as cancer, heart failure and chronic kidney disease.
Methods
A scoping methodology was employed for this practice review. Scoping reviews can report on the types of evidence that address and inform practice in the field and the way the research has been conducted. 9 As it had already been established that there no specific guidelines for palliative care the authors agreed by consensus a list of conditions which would include patients under the care of palliative care services. This included:
Cancer
Chronic kidney disease (CKD)
Heart failure
Guidelines were identified by searching databases and grey literature (Table 1). We included guidelines written within the last 5 years in the English language (Table 2). WHO guidance, the trial registry and Cochrane database were searched using the term ‘anaemia’ (May 2019). An additional search of MEDLINE was made for further key publications that provided additional primary data to add to the evidence base for the interventions considered (search date: 31 May 2019 – see Appendix 1 for search strategy). Studies relating to patients with cancer who were receiving chemotherapy were excluded.
Table 1.
Medline search for guidelines 20/1/21.
| Practice Guideline/ or guideline.mp. or Guideline/ or Guideline Adherence/ | 119,230 |
| limit 1 to yr=“2016” | 6893 |
| anaemia | 51,187 |
| AND | 13 |
Table 2.
Guidelines examined: Shading indicated whether the intervention is included.
| Investigate cause of anaemia | Reduce blood loss inc Tranexamic acid | Target Hb | Education | B12 | Folate | Oral iron | IV iron | Blood transfusion | ESA’s | |
|---|---|---|---|---|---|---|---|---|---|---|
| ESMO Management of anaemia and iron deficiency in patients with cancer: ESMO clinical practice guidelines 7 |
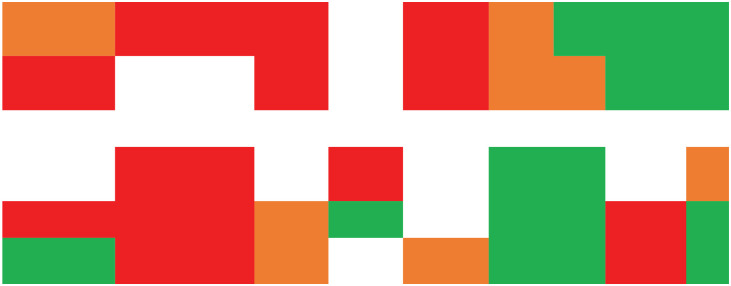
|
|||||||||
| Management of cancer-associated anaemia with erythropoiesis-stimulating agents: ASCO/ASH clinical practice guideline update 10 | ||||||||||
| NICE NG 106 chronic heart failure in adults: Diagnosis and management 11 | ||||||||||
| Diagnosis and management of iron deficiency in CKD: A summary of the NICE guideline recommendations and their rationale12,13 | ||||||||||
| Chronic kidney disease: Managing anaemia; NICE guideline 14 | ||||||||||
| Clinical practice guideline – anaemia of chronic kidney disease – The Renal Association 15 | ||||||||||
Key:  –
not discussed/mentioned.
–
not discussed/mentioned.  – minimal
discussion.
– minimal
discussion.  – some discussion.
– some discussion.
 –
detailed discussion.
–
detailed discussion.
In addition, evidence for specific treatments used to treat anaemia in palliative care has been included. Red cell transfusions have been researched in palliative care patients, but evidence is more limited for other treatments in this cohort.
Methods were compliant with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist. We determined the strength of evidence for commonly recommended treatments and strategies. Each treatment was then allocated to a practice recommendation category of ‘Do’, ‘Do not’ or ‘Don’t know’ based on the direction and strength of the supporting evidence (Table 3). A ‘strong’ recommendation was made if a large and consistent body of evidence existed, such as a systematic review. Comparatively, solid empiric evidence from one or more papers or a guideline advocacy justified a ‘moderate’ recommendation, with a ‘tentative’ recommendation made if limited empiric evidence existed. Please see Table 4 for summary of recommendations.
Table 3.
How categories of recommendation were decided.
| Do | Published evidence for effectiveness in managing anaemia in palliative care patients OR Clear favourable benefit to risk ratio |
| Do not | Evidence that the approach is not effective in palliative care patients with anaemia OR Lack of high-quality evidence to support its use AND Unfavourable benefit to risk balance |
| Don’t know | Limited evidence for effectiveness of treating anaemia in palliative care |
| Strength of recommendations | |
| Strong | A large and consistent body of evidence, such as a systematic review |
| Moderate | Solid empiric evidence from one or more papers OR recommended in guideline |
| Tentative | Limited empiric evidence |
Table 4.
Summary of recommendations.
| Strength of recommendation | |
|---|---|
| Do | |
| Investigate cause of anaemia | Moderate |
| Consider targeted treatments based on results e.g correct haematinics | Strong |
| Discuss the risks and benefits of treatments to allow an informed decision to be made with the patient | Moderate |
| Reduce blood loss where possible | Tentative |
| Do not | |
| Consider red blood cell transfusion unless haemoglobin is below 70 g/dL (or 80 g/dL in presence of acute coronary syndrome) | Strong |
| Transfuse more than one unit of blood without reassessing | Strong |
| Routinely use ESAs | Strong |
| Routinely use oral iron | Moderate |
| Don’t know | |
| The effectiveness of IV iron in this patient group | |
Results
Do
Investigate the cause of anaemia (moderate)
Anaemia is the end point in a process, not a diagnosis. The majority of patients referred to palliative care services are elderly. 2 In the general elderly population anaemia is caused by nutritional deficiencies, chronic inflammation/CKD, or other causes in approximately one third each. 13 It is important to establish the cause of a patient’s anaemia in order to consider appropriate treatments. Renal guidance outlines baseline blood parameters to check.13–15 Equally, NICE recommends a haemoglobin threshold and symptoms that warrant investigation, as well as the acknowledgement of excluding blood loss. 14 Oncology guidelines advocate investigating for cause of anaemia. 10
Consider targeted treatments based on results for example, correct haematinics (strong)
This is a heterogeneous group of patients but who are likely to share some commonalities, such as an underlying inflammatory process. Review of haematinics and iron studies should form part of the assessment and a targeted treatment plan instigated. While the ESMO guidance states B12 and folate deficiencies are rare causes of anaemia in cancer patients, an audit of blood transfusion practice in UK hospices (96% cancer diagnosis) found that of the patients who had a B12 level checked, 12% may have benefitted from B12 injections, of the patients who had a folate level checked, 41% may have benefitted from folic acid. 8 NICE guidance recommends and outlines the management of folate and B12 deficiency 16 ; longitudinal studies support the effectiveness of replacement. 17 This recommendation is made based on the evidence and favourable risk benefit ratio.
Reduce bleeding where possible (tentative)
While not all the guidance we reviewed specifically discusses reducing blood loss it is part of a logical approach that this should be done. This would include investigating any ongoing bleeding, consider endoscopic cautery and reducing the amount of blood taken during blood sample investigations. Oncology guidelines discuss patient blood management, includes minimising blood loss and bleeding. 18 A review of a patient’s medications to consider stopping any that could exacerbate bleeding, such as NSAIDs, 10 and potentially a trial of tranexamic acid can be considered.
Discuss the risks and benefits of treatments to allow an informed decision to be made with the patient (strong)
Palliative care advocates a holistic, person centred approach. 19 This is only possible through involvement of a patient (or their family) with decisions. Education is included in NICE guidance in CKD 14 including practical information about how anaemia of CKD is managed and knowledge about symptoms, and causes of anaemia. The guidelines specifically discuss education around adaptation to chronic disease, including managing patient expectations. An audit of blood transfusion practice in UK hospices found that only 18% of patients had lasting benefit from a blood transfusion, 8 information that should be discussed with patients when taking informed consent.
Do Not
Consider red blood cell transfusion unless haemoglobin is below 70 g/dL (or 80 g/dL in presence of acute coronary syndrome) (strong)
Red blood cell transfusions are commonly used in palliative care to treat anaemia or its symptoms, despite little evidence of benefit to patients and risk of harms. A systematic review of 13 studies of blood transfusion in palliative care found that any symptom benefit is short lived. 20 Equally, a Cochrane review of 12 observational studies found limited benefits, and that approximately one-third of patients died within 2 weeks of transfusion. 21 Nice published red blood cell transfusion guidelines for adults and recommends the use of a restrictive approach: transfusing one unit when haemoglobin falls below 70 g/L to a target concentration of 70–90 g/L. 22 The trigger threshold is raised to 80 g/L in those who are actively bleeding, have acute coronary syndrome or chronic anaemia (as the reason for their transfusion). Recent guidance from the American Association of Blood Banks (AABBs) 23 also recommends a restrictive threshold but concluded that there is insufficient evidence in some patient groups to guide trigger thresholds. The European Society for Medical Oncology (ESMO) 18 advocates a threshold of 70–80 g/L and recommends that transfusions are only used in anaemic patients with severe symptoms in need of rapid haemoglobin improvement. A review found that restrictive transfusion strategies reduced the risk of receiving a blood transfusion by 43% with no impact on clinical outcomes, 30-day mortality or adverse events. Importantly, the authors felt that there were insufficient data to draw firm conclusions about the safety of transfusion policies in certain subgroups including acute coronary syndrome, bone marrow failure and blood cancers. 24
Transfuse more than one unit of blood without reassessing (strong)
A national audit of blood transfusion practice in UK hospices 8 found that 84% of patients were given more than one unit of blood. Transfusion-associated circulatory overload (TACO) is cardiogenic pulmonary oedema caused by the infusion of blood products, with a mortality of 6%–10%. 25 TACO is more common with rapid or large volume infusions. Patients treated in hospices commonly have risk factors for TACO which include hypo-albuminaemia, low body weight, being physiologically compromised by cardiac, respiratory or renal insufficiency, as well as older age.5–7 TACO is likely underdiagnosed; one study across 157 UK hospitals showed that 4.3% of inpatients aged over 60 years developed increasing respiratory distress after transfusion. 26 Despite this, only one-third of patients diagnosed with TACO were reported to the SHOT Haemovigilance Group. 26 Patients should receive a weight-related transfusion, which may be less than one unit if the patient weighs less than 70 kg.
Routinely use Erythropoetin Stimulating Agents (ESAs) (strong)
ESAs are used in chemotherapy induced anaemia. The palliative population is likely to have a different cause of their anaemia. With the exception of selected patients with myelodysplastic syndromes, ESAs should not be offered to most patients with non- chemotherapy associated anaemia. 18
In those with heart failure ESAs successfully correct haemoglobin levels, but without significant improvement in clinical outcome. ESAs increase rates of thromboembolic events and ischemic stroke, therefore their use for anaemia in heart failure is not recommended. In those with chronic kidney disease there may be specific situations in which ESA’s may be indicated. 27 For example, NICE recommend ESAs with concurrent iron supplementation. 14
Routinely use oral iron (moderate)
Oral iron is poorly tolerated and is not well absorbed when systemic inflammatory processes are present (indicated by raised C-reactive protein (CRP) marker). These processes raise serum hepcidin and inhibit gastrointestinal iron uptake. In many advanced diseases, raised CRP is a common finding and would make oral iron supplementation ineffective. In a study of palliative care patients CRP was raised in 84% of participants in which it was recorded, highlighting the prevalence of inflammation in this population. 2
A RCT comparing oral iron with placebo in heart failure noted increased iron stores but no significant effect on exercise capacity. 28 A significant relationship between higher baseline hepcidin levels and lack of iron repletion was noted, supporting the view that oral iron is unlikely to be helpful in those with active inflammation.
Due to the effects of inflammation on oral iron absorption, the difference between absolute and functional iron deficiency should be considered. In absolute iron deficiency, total body iron stores are reduced, therefore demand cannot be met. Comparatively, in functional iron deficiency, body iron stores are adequate but alterations in iron homeostasis limit the supply of iron for erythropoiesis. This is most frequently observed in chronic inflammatory states and/or infection, from which pro-inflammatory cytokines, especially interleukin-6 and tumour necrosis factor, induce hepcidin production, a peptide produced by the liver. Hepcidin inhibits intestinal iron absorption and limits the recycling of iron from red blood cell by degrading the macrophage transmembrane protein ferroportin. The processes underlying functional iron deficiency are considered a component of the pathophysiology of the anaemia of chronic disease. The distinction between absolute, functional or a mixed deficiency is challenging, considering a history of inflammation and chronic disease alongside appropriate laboratory investigation. 29 Although not in a palliative population, a trial of oral iron replacement in management of sole absolute iron deficiency has shown benefit and is advocated in guidelines. 29 Translation to a palliative population remains unevidenced but, considering the prevalence of inflammation, the routine use of oral iron should be avoided. 2 A more detailed discussion about functional iron deficiency or the anaemia of chronic disease is not possible in this review.
Don’t know
The effectiveness of IV iron in this patient group
Trials of IV iron in palliative care patient groups are rare. Studies in heart failure indicate that IV iron may be effective in improving symptoms (functional class, exercise capacity and QOL) but further trials are needed. Oncology guidelines 18 advocate treatment of absolute iron deficiency with IV iron, as well as those with functional iron deficiency being considered for ESA treatment. Advantages include a reduction in the number of red blood cell transfusions required and an improved response to ESAs. However, the long-term safety in oncology has not yet been fully established.
Recent British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults 29 advocate the consideration of IV iron when oral iron is contraindicated, ineffective or not tolerated. Therefore, there may be scope for the wider use of IV iron in patients with either absolute or functional iron deficiency, in whom inflammation would render oral administration ineffective or following a failed or poorly tolerated trial of oral iron in absolute iron deficiency. IV iron is significantly more expensive than oral iron and more invasive to administer, factors which need to be taken into account. Considering its complex pathophysiology, research is required to define the role, if any, of IV iron replacement in many patient groups with functional iron deficiency.
Management of anaemia in patients with myelodysplastic syndrome (MDS) receiving palliative care
Only a minority of patients with MDS can be treated with curative intent (i.e. allogenic haematopoietic cell transplantation). Therefore, a combined approach that includes both disease-modifying agents and palliative care is needed early in the course of illness. The supportive management of anaemia in MDS may include ESAs and occasionally granulocyte colony stimulating factor (G-CSF), but this is often limited to MDS patient with lower risk factors. Even in this subgroup only the minority patients (approximately 1/3) show improvement in erythropoiesis, and with no overall survival benefit. 30 RBC transfusions are generally reserved for patients with symptomatic anaemia with a haemoglobin of <80–100 g/L (8–10 g/dL). 18
Limitations
Limitations include the method of using a scoping review technique which is not as rigorous as a systematic review. Therefore there may be additional guidelines or studies not included.
Conclusion
Anaemia is common in those with advanced disease and a large proportion of this may be due to functional iron deficiency. We recommend early consideration and investigation of anaemia, guided by symptom burden and patient preferences. Correction of reversible causes should be the mainstay of treatment, with a restrictive approach to red blood cell transfusion considered only in circumstances supported by international guidelines. Routine use of oral iron and ESAs are not recommended. Research is required to evaluate the efficacy of IV iron in palliative care patients.
Appendix 1
Medline Search strategy
“Hospice and Palliative Care Nursing”/ [Section 1 – Population: lines 1-13]
Palliative Care/
Terminal Care/
Hospice Care/
Hospices/
*Neoplasms/
(hospice* or palliat* or terminal* or endstage or end-stage).ti,kf.
((end adj3 life) or ((care or treatment* or therap*) adj3 dying)).tw,kf.
((advanced or late* or last or end or final) adj3 (stage* or phase*)).ti.
((hospice* or palliat* or terminal* or endstage or end-stage or EOL) adj3 (care or medicine or treatment* or intent* or patient* or cancer*)).ab,kf.
((advanced or metastatic or late* stage* or final stage* or terminal*) adj2 (cancer* or malignan* or disease* or illness*)).tw,kf.
(palliative therap* or cancer palliation).tw,kf.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
Anemia/ or Anemia, Hypochromic/ or Anemia, Iron-deficiency/ [Section 2 – Population: lines 14-16]
(anemi* or anaemi* or ferrop?eni* or siderop?eni* or ((iron or folate) adj2 (status or deficien* or count* or level* or insufficien* or deplet* or test*)) or low h?emoglobin or low blood count* or low red cell count* or low red blood cell count* or low iron or low serum ferritin or low ferritin or low serum iron or low transferrin saturation or low h?ematocrit).tw,kf.
14 or 15
13 and 16
Iron Compounds/ [Section 3 – Interventions: lines 18-55]
exp Ferric Compounds/
exp Ferrous Compounds/
exp Iron/
Iron, Dietary/
(alvofer or colliron or faremio or ferion or feriv or fermed or ferri saccharate or ferric hydroxide sucrose or ferric oxide saccharate or ferric oxide,saccharated or ferric saccharate or ferrinemia or ferrisaccharate or ferrivenin or ferrologic or ferrous saccharate or ferrovin or fesin or hemafer s or hemafer-s or idafer or (iron adj2 hydroxide sucrose complex) or iron saccharate or iron sucrose or ironcrose or iviron or nefro-fer or nefrofer or neo ferrum or nephroferol or proferrin or referen or reoxyl or saccharate ferric or saccharate iron or saccharated ferric oxide or saccharated iron oxide or sucro fer or sucrofer or sucroven or veniron or venofer or venotrix).tw,kf.
(anaemex or cosmofer or dexferrum or dexiron or dextrafer or dextran fe or dextran ferrous or dextran iron or driken or fenate or fer dextran or ferric dextran or ferridex or tranferrisat or ferrodex or ferrodextran or ferrous dextran or ferrum lek or fervetag or hibiron or imferdex or imferon or impheron or imposil or infed or infufer or iron dextran complex or ironate or monofar or proferdex or uniferon or uniferon or uniferron).tw,kf.
(ferlecit or ferlixit or ferric gluconate or ferrigluconate or ferrlecit or gluconate ferric sodium or (iron adj2 gluconate) or sodium ferrigluconate or intravenous iron sucrose or iron sucrose injection* or venofer).tw,kf.
(diafer or ferric derisomaltose or iron isomaltoside or monofer or monafer or monoferro or monover or ferumoxytol or feraheme or rienso).tw,kf.
(IV iron or “I.V. iron” or iron therapy or ((intravenous* or inject* or infus* or parenteral) adj3 iron)).tw,kf.
(iron or ferritin or ferrous).ti.
(iron adj3 (rich or enrich* or food* or diet* or absorp* or store* or storing or status or deficien* or deplet* or oral* or supplement* or salt* or complex or inject* or infusion* or intravenous* or replace* or product* or tablet* or pill* or capsule* or sulphate or sulfate or therap*)).ab,kf.
(ferrous adj (sulfate or sulphate or fumarate or fumerate)).ab.
(Albafort* or Fchem-Sol* or Fe-Max or Femiron or CapletFeostat* or Feosol or Fer Iron or Fer-Gen-Sol or Fer-in-Sol or Ferate or TRFer* or Feratab or FeroSul or Fergon* or Ferra or TDFerretts* or Ferro-Sequels* or Ferro-Time* or Ferrospace* or Fumasorb* or Hemocyte or Ironmar* or Mol-Iron* or Nephro-Fer* or FernNephro* or Siderol* or IronTandem* or Yiero-Gota* or Yieronia* or (Ferra adj2 Caps) or Ferro-Bob or Slow Fe or Slow Release Iron or Infed* or Dexferrum* or Ferrlecit* or Venofer*).tw,kf.
(ferric carboxymaltose or Ferinject or Injectafer or Iroprem or ferlecit or ferlixit or ferric gluconate or ferrigluconate or ferrlecit or gluconate ferric sodium or (iron adj2 gluconate) or iron isomaltoside or iron sucrose or sodium ferrigluconate or diafer or ferric derisomaltose or venofer or monofer or monafer or monoferro or monover or ferumoxytol or feraheme or rienso or “IV iron” or “I.V. iron”).tw,kf.
or/18-32
exp Vitamin B 12/
(cobalamin* or cyanocobalamin or eritron or vitamin b 12 or vitamin b12 or schilling test* or cobamide* or deoxyadenosinecobalamin* or vitamin b 12 coenzyme* or vitamin b12 coenzyme* or hydroxo-cobalamin* or hydroxocobalamin* or hydroxycobalamin* or cyanocobalamin* or 12 oral or acravit b12 or almeret or anacobin or anacobine or antipernicin or antipernicine or apavit b12 or aquocobinamide cyanide or arcored or b docin or b12 or b12 delagrange or b12 flavin or b12 galto or b12 horfervit or b12 mille or b12 monovit or b12 pierrel or b12 siegfried or b12 vicotrat or b12 vitamin or b12 weber or bagovit b12 or bedoc or bedoce or bedodec or bedodeka or bedoxyl or bedoz or bedozane or bedumil or behepan or behepane or beniform or benol or bentavit b12 or berubi or berubigen or berubigene or berubin or berubine or betalily 12 or betalin 12 or betaline 12 or betamine b12 or beterapion 12 or betolvex or bevatine or bevatine 12 or bevidoral or bevidox or bevitex or bex or bexii or bexitab or bimil or biocres or biopar or bitevan or bivetan or byladoce or cabadon m or calomist or catavin or catavine or clarentin 12 or clarentine 12 or cn cobalamin or cn cobalamine or cobadoce forte or cobal-1000 or cobalamide or cobalin or cobaline or coballamine or cobalmed or cobaltron or cobaltrone or cobamin or cobamin ophth soln or cobamine or cobastab or cobavite or cobeminum or cobione or cobolin-m or cobrumin or cobrumine or cohemin or cohemine or “compensal 25,000” or covit or creliverol-12 or cresiro or cresirol or crodabion b12 or crystal b-12 or crystamin or crystamine or crystimin 1000 or crystwel or cyanacobalamin or cyanaton or cyanatone or cyancobalamin or “cyano 5,6 dimethylbenzimidazolylcobamide” or cyano cobalamin or cyano cobalamine or cyanobalamin or cyanocobal or cyanocobalamine or cyanocobalomin or cycobemin or cycobemine or cycobeminet or cycolamin or cycolamine or cycoplex or cyomin or cyredin or cytacone or cytagon or cytamen or cytamene or cytaton or cytatone or cytobex or cytobion or cytobione or davitamon b12 or depo-cobolin or dicibin or dicopac or distivit or dobetin or dobetine or doce oral or docecrisina or docemine or doceoral or docibin or docibine or docigram or docivit or dodecabee or dodecavite or dodevitina or dodex or douzoral b12 or dozefull or ducobee or ducobee depot or dumovit b12 or duodebex or duodecibin or duodecibine or embiol or emobione or endoglobin or erftamin 12 or erftamine 12 or eritrone or eritrosir or eritrovit b12 or eruhaemon or erycytol or erythrotin or erythrotine or examen or examene or extrinsic factor or fermin or fresmin or godabione b12 or griseovit or grisevit or grisovit or hematolamin or hemo b doze or hemoergene or hemomin or hemomine or hemosalus b12 or hepagon or hepagone or hepavis or hepavit or hepcovite or heptenyl 12 or hypovitaminosis b12 or ido b12 or intrinase or intrindon or intrinolone or kaybovite or la-12 or lactobacillus lactis dorner factor or lagavit b12 or lifaton b12 or livonal schering or lld factor or macrabin or mavena B12 or megabione or megalovel or mepharnbin or mepharubine or milbedoce or millevit or nascobal or nascobal intranasal gel or navagron or navagrone or neurobaltina or neurobaltine or neuroforte-r or norivite-12 or normocytin or osfavit b12 or palvite or parentosol b12 or pernaevit or pernical or pernicipur or pernipuvon or pernoral or pharmatovit b12 or pinkamin or pinkamine or plecyamin or plecyamine or poyamin or poyamine or rametine or rectocenga or recytomin or recytomine or redamin or redamine or redisol or regividerm or reticulogen or reticulogene or rhodacryst or robelvit or rojamin or rotamin or rotamine or rubavit or rubentin or rubentine or rubesol or rubion or rubione or rubivitan or rubivite or rubramin or rubramin pc or rubranova or rubrine or rubripca or rubrocitol or rubrovit or rubyvan or rubyvit or ruvite or “s.p. cycolamin” or “s.p. cycolamine” or sytobex or transcyanocobalamin or twel be or twelbe or tweltone or twelve oral or twelveoral or ucemine b12 or vi-twel or vibalt or vibecon or vibecone or vibicon or vibicone or vibisone or vicapan n or viemin 12 or virubra or “vita no. 12” or vitabee 12 or vitadom or vitamin b 12 or vitamin b-12 or vitamin B12 or vitamin b12 r or vitamina b12-ecar or vitapur b 12 or vitarubin).tw.
34 or 35
exp Folic Acid/
(folate therap* or folic acid or vitamin B9 or vitamin M or acfol or acide folique ccd or acido folico or apo-folic or filicine or folacin or folart or folate or folate acid or folate sodium or foldine or foliamin or folic acid dha or folicet or folicid or folina or folinsyre or folitab or folium acid or folivit or folsan or folverlan or folvite or gravi-fol or ingafol or lactobacillus casei factor or lafol or lexpec or megafol or mission prenatal or neocepri or nsc 3073 or pteroyglutamic acid tablets or pteroyl glutamate or pteroyl l glutamic acid or pteroyl monoglutamate or pteroylglutamate or pteroylglutamic acid or pteroylmonoglutamate or pteroylmonoglutamic acid or rubiefol or sodium folate or vifolin or vitamin bc or methyltetrahydrofolic acid or tetrahydropteroylglutamic acid or methyltetrahydrofolate or methyltetrahydropteroyl glutamate).tw,kf.
(methyltetrahydropteroylglutamate or methyltetrahydropteroylglutamic acid or bay 86 7660 or bay 86-7660 or bay86 7660 or bay86-7660 or bodyfolin or calcium levomefolate or levomefolate calcium or levomefolic acid or metafolin or methyltetrahydrofolate or methyltetrahydrofolic acid or methyl tetrahydrofolate or methyltetrahydrofolate or n 5 methyltetrahydrofolic acid or methyltetrahydrofolic acid or methyltetrahydrofolate or methyltetrahydrofolic acid or nutrifolin or folicobalamine or rubrafolin or delphicol or dihydrofolic acid or dihydrofolate or dihydropteroylglutamic acid or beyaz or drospirenone plus ethinyl estradiol plus levomefolate calcium or drospirenone plus ethinyl estradiol plus mefolate calcium or drospirenone plus ethinylestradiol plus levomefolate calcium or drospirenone plus mefolate calcium plus ethinyl estradiol or drospirenone plus mefolate calcium plus ethinylestradiol or ethinyl estradiol plus drospirenone plus mefolate calcium or ethinyl estradiol plus mefolate calcium plus drospirenone or ethinylestradiol plus drospirenone plus mefolate calcium or ethinylestradiol plus mefolate calcium plus drospirenone or mefolate calcium plus drospirenone plus ethinyl estradiol or mefolate calcium plus drospirenone plus ethinylestradiol or mefolate calcium plus ethinyl estradiol plus drospirenone or mefolate calcium plus ethinylestradiol plus drospirenone or safyral or nicomide or folinate calcium).tw,kf.
(formyltetrahydrofolate calcium or antrex or asovorin or calcium folinate or calcium leucovorin or calciumfolinat-ebewe or citrec or citrovorum factor or citrovorum factor rescue or folina 15 or folinoxan or isovorin or kw 2264 or kw2264 or lederfolin or lederfoline or lederle leucovorin or ledervorin or ledervorin calcium or leucocalcin or leucovorin calcium or leucovorin factor or leucovorina calcica or leucovorine abic or litacor or lovorin or medsavorin or nsc 3590 or nsc3590 or nyrin or oncofolic or refolinon or rescufolin or rescuvolin or rontafur or tecnovorin or tonofolin or uzel or wellcovorin or folinic acid or tetrahydrofolic acid or formyltetrahydrofolate or formyltetrahydrofolic acid or formyltetrahydropteroylglutamic acid or folinic acid or formyltetrahydrofolate or formyltetrahydrofolates or formyltetrahydropteroylglutamic acid or lencovorin or leucovorin or leukovoran or leukovorin or n formyltetrahydrofolic acid or tetrahydropteroylglutamic acid or n5 formyl tetrahydrofolic acid or n5 formyltetrahydrofolate or formyltetrahydrofolic acid or levoleucovorin or calcium levofolinate or calcium levoleucovorin or cl 307782 or cl307782 or elvorine or fusilev or levofolinate or levofolinate calcium or levoleucovorin calcium or methylenetetrahydrofolic acid or tetrahydropteroylglutamic acid or methylenetetrahydrofolate or methylenetetrahydrofolic acid).tw,kf.
(methylenetetrahydropteroylglutamic acid or methylenepteroylglutamic acid or anx 510 or anx510 or folitixorin or methylene tetrahydrofolate or methylenetetrahydrofolate or pteroptin or folate oligoglutamate or folate polyglutamate or folatic acid polyglutamate or folylpolyglutamate or benzoyl glutamic acid polyglutamate or polyglutamic folate or polyglutamic folic acid or polyglutamyl folate or pteroylglutamic acid polyglutamate or pteroylpoly* or pteroylpolyglutamate or pteroylpolyglutamic acid or pteroylpolyglutamic acids or pteroylpolyglutamylglutamic acid or tetrahydrofolic acid or tetrahydrofolic acid or tetrahydrofolate or tetrahydropteroyl glutamate or tetrahydropteroylglutamate or tetrahydropteroylglutamic acid or tetrahydrofolic acid derivative or tetrahydrofolate*).tw,kf.
37 or 38 or 39 or 40 or 41
exp Erythropoietin/ or exp Hematinics/tu
(erythropoietin or erythropoetin or erythropoiesis stimulating agent* or erythropoietic or erythroid maturation agent* or luspatercept or ESA administration or ESA therap* or ESA treatment*).tw,kf.
(abseamed or aranesp or aranest or “bi 71.052” or “bi71.052” or binocrit or biopoin or biosynthetic erythropoietin or darbepoetin or darbepoetin alfa or darbepoetin alpha or darbepoietin or darbepoietin alfa or darbepoietin alpha or darbopoetin or darbopoetin alfa or darbopoetin alpha or darbopoietin or darbopoietin alfa or darbopoietin alpha or dynepo or epoade or epoch or epoconn or epoetin or epoetin alfa or epoetin alfa hexal or epoetin beta or epoetin delta or epoetin epsilon or epoetin gamma or epoetin kappa or epoetin omega or epoetin theta or epoetin zeta or epogen* or epogin or epoietin or epoietin alfa or epoietin alpha or epoietin beta or epoietin delta or epoietin epsilon or epoietin gamma or epoietin kappa or epoietin omega or epoietin theta or epoietin zeta or epokine or epomax or eporatio or epostim or epoxitin or eprex or erantin or erypo or erythropoetin or espo or exprex or globuren or heberitro or hemapo or hematopoietin or hemopoietin or hemax or recombinant erythropoietin or “hx 575” or hx575 or “krn 321” or “krn 5702” or krn321 or krn5702 or marogen or neorecormon or NESP or nespo or novel erythropoiesis stimulating protein or procrit or erythropoietin alfa or erythropoietin alpha or recombinant human erythropoietin or recormon or recormone or retacrit or silapo or “snb 5001” or snb5001 or “tyb 5220” or tyb5220 or pegerythropoietin or “bcd 131” or bcd131 or peg darbepoetin or pegdarbepoetin beta or pegylated darbepoetin or pegylated darbepoetin beta or pegylated erythropoietin or rhuepo or “R huepo” or “rhu epo” or rEpo or rhepo).tw,kf.
(epo or cera).tw.
43 or 44 or 45 or 46
Tranexamic Acid/
(tranexamic or cyclohexanecarboxylic acid* or amcha or trans-4-aminomethyl-cyclohexanecarboxylic acid* or t-amcha or amca or “kabi 2161” or “kabi 2161r” or amchafibrin or amstat or anvitoff or anexan or cyklokapron or cyclo-F or aminomethylcyclohexanecarbonic acid or aminomethylcyclo-hexanecarboxylic acid or AMCHA or amchafibrin or amikapron or aminomethyl cyclo-hexane carboxylic acid or aminomethyl cyclohexanecarboxylic acid or aminomethylcyclohexane carbonic acid or aminomethylcyclohexane carboxylic acid or aminomethylcyclo-hexanecarbonic acid or aminomethylcyclo-hexanecarboxylic acid or aminomethylcyclohexanocarboxylic acid or aminomethylcyclohexanoic acid or caprilon or cl?65336 or cl65336 or cyclocapron or cyclokapron or cyklocapron or cyklokapron or espercil or exacyl or frenolyse or fibrinon or hemostan or hexacapron or hexakapron or kalnex or kapron or lysteda or micranex or nicolda or rikaparin or ronex or spotof or theranex or tracid or tramic or tranex or tranexam or tranexanic or tranexic or tranhexamic or trans achma or transamin or transcam or transexamic or traxamic or trenaxin or TXA or ugurol or xp12b).tw,kf.
(Agretax or Bio-Stat or Capiloc or Capitrax or Clip Inj or Clot-XL or Clotawin-T or Coastat or Cuti or Cymin or Dubatran or Espercil or Examic or Existat or Extam or Fibran or Gynae-Pil or Hemstate or Kapron or Menogia or Monitex or Nestran or Nexamic or Nexi-500 or Nexmeff or Nicolda or Nixa-500 or Pause or Rheonex or Sylstep TX or Synostat or T-nex or T Stat or T Stat or Tanmic or Temsyl-T or Texakind or Texanis or Texapar or Texid or Thams or Tonopan or Traklot or Tramic or Tramix or Tranarest or Trance Inj or Tranecid or Tranee or Tranemic or Tranex or Tranexa or Tranfib or Tranlok or Transtat or Transys or Transcam or Tranxi or Trapic or Traxage or Traxamic or Traxyl or Trenaxa or Trexamic or Trim Inj or Tx-1000 or Tx 500 or Wistran or X-Tran or Xamic).tw,kf.
48 or 49 or 50
Ethamsylate/
(aglumin or altodor or cyclonamine or dicinone or dicynene or dicynone or etamsylate or ethamsylate or “hemo 141” or “141 md” or 141md or “compound 263 e” or “compound 263e” or diphenolsulfonic acid or diethylamine or “e 263” or e141 or e263 or “md 141” or md141 or “om dicinoma”).tw,kf.
52 or 53
33 or 36 or 42 or 47 or 51 or 54
17 and 55
exp Controlled Clinical Trial/ [Section 4 – Study Filters: lines 57-109]
CONTROLLED CLINICAL TRIAL.pt.
(randomi* or trial*).tw,kf.
(placebo* or randomly or groups).ab.
CLINICAL TRIALS AS TOPIC.sh.
or/57-61
exp COHORT STUDIES/
EPIDEMIOLOGIC STUDIES/
exp CASE CONTROL STUDIES/
(cohort* or controlled trial* or controlled stud* or comparative trial* or comparative stud* or comparison group* or comparator group* or control group*).tw,kf.
(case control* or case series or cohort*).tw,kf.
((follow up or observational) adj (study or studies)).tw,kf.
(longitudinal* or retrospective* or prospective* or cross sectional*).mp.
CONTROLLED BEFORE-AFTER STUDIES/
OBSERVATIONAL STUDY/
HISTORICALLY CONTROLLED STUDY/
INTERRUPTED TIME SERIES ANALYSIS/
(nonrandom* or non random*).tw,kf.
((before adj15 (after or during)) or “before-after” or time series or time point* or repeated measur*).tw,kf.
(pre-post or pre-test* or pretest* or posttest* or post-test* or (pre adj5 post)).tw,kf.
or/63-76
Meta-Analysis/
(meta analy* or metaanaly*).ab.
or/78-79
(studies or trials).ab.
80 and 81
Systematic Review.pt.
Network Meta-Analysis/
(meta analy* or metaanaly*).ti.
((systematic* adj2 (review* or overview*)) or network meta-analys*).tw,kf.
(evidence synthes* or cochrane or medline or pubmed or embase or cinahl or cinhal or lilacs or “web of science” or science citation index or search terms or literature search or published articles or search strateg* or reference list* or bibliograph* or handsearch* or hand search* or manual* search*).ab.
(additional adj (papers or articles or sources)).ab.
((electronic or online) adj (sources or resources or databases)).ab.
(relevant adj (journals or articles)).ab.
“REVIEW LITERATURE AS TOPIC”/
“Systematic Reviews as Topic”/
META-ANALYSIS AS TOPIC/
or/82-93
Review.pt.
exp CLINICAL TRIALS AS TOPIC/
selection criteria.ab. or critical appraisal.ti.
(data adj (extraction or analys*)).ab.
RANDOMIZED CONTROLLED TRIALS/
OBSERVATIONAL STUDY/
((cohort* or observational or retrospective*) adj1 (trial* or stud*)).tw,kf.
or/96-101
95 and 102
94 or 103
(Comment or Editorial).pt.
exp animals/ not humans/
105 or 106
104 not 107
62 or 77 or 108
56 and 109
limit 110 to yr=“2000 -Current”
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Karen Neoh  https://orcid.org/0000-0003-1563-2070
https://orcid.org/0000-0003-1563-2070
Andrew Page  https://orcid.org/0000-0002-4587-134X
https://orcid.org/0000-0002-4587-134X
Nicolas Chin-Yee  https://orcid.org/0000-0003-0855-7324
https://orcid.org/0000-0003-0855-7324
Michael I Bennett  https://orcid.org/0000-0002-8369-8349
https://orcid.org/0000-0002-8369-8349
References
- 1. Dunn A, Carter J, Carter H. Anemia at the end of life: prevalence, significance, and causes in patients receiving palliative care. J Pain Symptom Manag 2003; 26(6): 1132–1139. [DOI] [PubMed] [Google Scholar]
- 2. Neoh K, Stanworth S, Pasricha SR, et al. Neoh estimating prevalence of functional iron deficiency anaemia in advanced cancer. Support Care Cancer 2016; 25(4): 1209–1214. [DOI] [PubMed] [Google Scholar]
- 3. Sarkar M, Rajta PN, Khatana J. Anemia in Chronic obstructive pulmonary disease: prevalence, pathogenesis, and potential impact. Lung India 2015; 32(2): 142–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McMahon TJ, Prybylowski AC. Anemia in the patient with chronic lung disease. In: Provenzano R, Lerma E, Szczech L. (eds) Management of anemia. New York, NY: Springer, 2018, pp.143–155. [Google Scholar]
- 5. Roubinian NH, Hendrickson JE, Triulzi DJ, et al.; NHLBI Recipient Epidemiology and Donor Evaluation Study-III (REDS-III). Incidence and clinical characteristics of transfusion-associated circulatory overload using an active surveillance algorithm. Vox Sang 2017; 112(1): 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bolton-Maggs PHB. (Ed) Poles D, et al. on behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2015 annual SHOT report, https://www.shotuk.org/wp-content/uploads/myimages/SHOT-2015-Annual-Report-Web-Edition-Final-bookmarked-1.pdf (2016, accessed 5 January 2018).
- 7. Tinegate H, Birchall J, Gray A, et al. Guideline on the investigation and management of acute transfusion reactions prepared by the BCSH Blood Transfusion Task Force. Br J Haematol 2012; 159(2): 143–153. [DOI] [PubMed] [Google Scholar]
- 8. Neoh K, Gray R, Grant-Casey J, et al. National comparative audit of red blood cell transfusion practice in hospices: recommendations for palliative care practice. Palliat Med 2019; 33(1): 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018; 18(1): 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bohlius J, Bohlke K, Castelli R, et al. Management of cancer-associated anemia with erythropoiesis-stimulating agents: ASCO/ASH clinical practice guideline update. Blood Adv 2019; 3(8): 1197–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. NICE. Chronic heart failure in adults: diagnosis and management. NICE guideline [NG106], www.nice.org.uk/guidance/ng106 (2018, accessed 13 July 2020). [PubMed]
- 12. Anand IS, Gupta P. Anemia and iron deficiency in heart failure: current concepts and emerging therapies. Circulation 2018; 138(1): 80–98. [DOI] [PubMed] [Google Scholar]
- 13. Ratcliffe LE, Thomas W, Glen J, et al. Diagnosis and management of iron deficiency in CKD: a summary of the NICE guideline recommendations and their rationale. Am J Kidney Dis 2016; 67(4): 548–558. [DOI] [PubMed] [Google Scholar]
- 14. NICE. Chronic kidney disease: managing anaemia. NICE guideline [NG8], www.nice.org.uk/guidance/ng8 (2015, accessed 13 July 2020).
- 15. Mikhail A, Brown C, Williams JA, et al. Renal association clinical practice guideline on Anaemia of Chronic Kidney Disease. BMC Nephrol 2017; 18(1): 345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. NICE Clinical Knowledge Summaries. Anaemia – B12 and folate deficiency, cks.nice.org.uk/topics/anaemia-b12-folate-deficiency/ (2020). Anaemia - B12 and folate deficiency | Health topics A to Z | CKS | NICE (accessed 1 July 2021). [Google Scholar]
- 17. Laird EJ, O’Halloran AM, Carey D, et al. Voluntary fortification is ineffective to maintain the vitamin B12 and folate status of older Irish adults: evidence from the Irish Longitudinal Study on Ageing (TILDA). Br J Nutr 2018; 120(1): 111–120. [DOI] [PubMed] [Google Scholar]
- 18. Aapro M, Beguin Y, Bokemeyer C, et al. Management of anaemia and iron deficiency in patients with cancer: ESMO Clinical Practice Guidelines. Ann Oncol 2018; 29(Suppl. 4): iv96– iv110. [DOI] [PubMed] [Google Scholar]
- 19. National Partnership for Palliative and End of Life Care. Ambitions for palliative and end of life care: a national framework for local action: 2015–2020, http://endoflifecareambitions.org.uk/ (2015, accessed 1 July 2021).
- 20. Chin-Yee N, Taylor J, Rourke K, et al. Red blood cell transfusion in adult palliative care: a systematic review. Transfusion 2018; 58(1): 233–241. [DOI] [PubMed] [Google Scholar]
- 21. Preston NJ, Hurlow A, Brine J, et al. Blood transfusions for anaemia in patients with advanced cancer. Cochrane Database Syst Rev 2012; 2012(2): CD009007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. NICE. Blood transfusion. NICE guideline [NG24], 18 November 2015. Overview | Blood transfusion | Guidance | NICE (accessed 13 July 2020) [Google Scholar]
- 23. Carson JL, Guyatt G, Heddle NM, et al. CLinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. .JAMA 2016; 316(19): 2025–2035. [DOI] [PubMed] [Google Scholar]
- 24. Carson JL, Stanworth SJ, Roubinian N, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 2016; 10(10): CD002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Popovsky MA. Breathlessness and blood: a combustible combination. Vox Sang 2002; 83(Suppl. 1): 147–150. [DOI] [PubMed] [Google Scholar]
- 26. Morton S, Grant-Casey J, Bolton-Maggs P, et al. Skating on thin ice: national audit of TACO demonstrates poor recognition of risk factors. Blood 2017; 130: 2406. [Google Scholar]
- 27. Chow KM, Szeto CC, Choy ASM, et al. Effect of erythropoiesis-stimulating agent therapy in patients receiving palliative care of chronic kidney disease. Am J Hosp Palliat Care 2019; 36(8): 718–721. [DOI] [PubMed] [Google Scholar]
- 28. Lewis GD, Malhotra R, Hernandez AF, et al. Effect of oral iron repletion on exercise capacity in patients with heart failure with reduced ejection fraction and iron deficiency: the IRONOUT HF randomized clinical trial. JAMA 2017; 317(19): 1958–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Snook J, Bhala N, Beales ILP, et al. British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults. Gut 2021; 70: 2030–2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Messa E, Gioia D, Masiera E, et al. Effects of erythropoiesis-stimulating agents on overall survival of International Prognostic Scoring System Low/Intermediate-1 risk, transfusion-independent myelodysplastic syndrome patients: a cohort study. Haematologica 2019; 104(1): e4–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]


