Abstract
Objectives
This systematic review assessed the influence of the COVID‐19 pandemic and associated restrictions on body image, disordered eating (DE), and eating disorder outcomes.
Methods
After registration on PROSPERO, a search was conducted for papers published between December 1, 2019 and August 1, 2021, using the databases PsycINFO, PsycARTICLES, CINAHL Plus, AMED, MEDLINE, ERIC, EMBASE, Wiley, and ProQuest (dissertations and theses).
Results
Data from 75 qualitative, quantitative, and mixed‐methods studies were synthesized using a convergent integrated approach and presented narratively within four themes: (1) disruptions due to the COVID‐19 pandemic; (2) variability in the improvement or exacerbation of symptoms; (3) factors associated with body image and DE outcomes; (4) unique challenges for marginalized and underrepresented groups. Disruptions due to the pandemic included social and functional restrictions. Although most studies reported a worsening of concerns, some participants also reported symptom improvement or no change as a result of the pandemic. Factors associated with worse outcomes included psychological, individual, social, and eating disorder‐related variables. Individuals identifying as LGBTQ+ reported unique concerns during COVID‐19.
Discussion
There is large variability in individuals' responses to COVID‐19 and limited research exploring the effect of the pandemic on body image, DE, and eating disorder outcomes using longitudinal and experimental study designs. In addition, further research is required to investigate the effect of the COVID‐19 pandemic on body image and eating concerns among minoritized, racialized, underrepresented, or otherwise marginalized participants. Based on the findings of this review, we make recommendations for individuals, researchers, clinicians, and public health messaging.
Public Significance
This review of 75 studies highlights the widespread negative impacts that the COVID‐19 pandemic and associated restrictions have had on body image and disordered eating outcomes. It also identifies considerable variations in both the improvement and exacerbation of said outcomes that individuals, researchers, clinicians, and other public health professionals should be mindful of if we are to ensure that vulnerable people get the tailored support they require.
Keywords: body image, coronavirus, COVID‐19, disordered eating, eating and feeding disorders, health inequality, isolation, lockdown, narrative synthesis, pandemic
Abstract
Objetivos
Esta revisión sistemática evaluó la influencia de la pandemia de COVID‐19 y las restricciones asociadas en los resultados en imagen corporal, la alimentación disfuncional y los trastornos alimentarios.
Método
Después del registro en PROSPERO, se realizó una búsqueda de artículos publicados entre el 1 de diciembre de 2019 y el 1 de agosto de 2021, utilizando las bases de datos PsycINFO, PsycARTICLES, CINAHL Plus, AMED, MEDLINE, ERIC, EMBASE, Wiley y ProQuest (disertaciones y tesis).
Resultados
Los datos de 75 estudios cualitativos, cuantitativos y de métodos mixtos se sintetizaron utilizando un enfoque integrado convergente y se presentaron narrativamente dentro de cuatro temas: (1) interrupciones debidas a la pandemia de COVID‐19; (2) variabilidad en la mejoría o exacerbación de los síntomas; (3) factores asociados con resultados de la imagen corporal y alimentarios disfuncional; (4) desafíos únicos para los grupos marginados y subrepresentados. Las interrupciones debidas a la pandemia incluyeron restricciones sociales y funcionales. Aunque la mayoría de los estudios informaron un empeoramiento de las preocupaciones, algunos participantes también informaron una mejoría de los síntomas o ningún cambio como resultado de la pandemia. Los factores asociados con peores resultados incluyeron variables psicológicas, individuales, sociales y relacionadas con el trastorno alimentario. Las personas que se identificaron como LGBTQ + informaron preocupaciones únicas durante COVID‐19.
Discusión
Existe una gran variabilidad en las respuestas de los individuos a COVID‐19 y una investigación limitada que explora el efecto de la pandemia en los resultados de la imagen corporal, la alimentación disfuncional y los trastornos de la conducta alimentaria utilizando diseños de estudios longitudinales y experimentales. Además, se requiere más investigación para investigar el efecto de la pandemia de COVID‐19 en la imagen corporal y las preocupaciones alimentarias entre los participantes minoritarios, racializados, subrepresentados o marginados. Basados en los hallazgos de esta revisión, se hacen recomendaciones para individuos, investigadores, médicos y mensajes de salud pública.
1. INTRODUCTION
The novel coronavirus disease (COVID‐19) is an infectious respiratory illness that has claimed millions of lives globally (World Health Organization, 2021) and has had significant psychological ramifications. Individuals with disordered eating (DE) and eating disorders (EDs) may be particularly vulnerable due to the impact of distancing measures on social support and access to mental health services (Christensen, Hagan, et al., 2021; Touyz et al., 2020), as well as their problematic relationships with food in a time of food insecurity (Islam et al., 2021). Emerging evidence suggests that public health messaging associated with COVID‐19 and increased reliance on videoconferencing technologies have had a negative impact on body image (BI; Pearl & Schulte, 2021; Pikoos et al., 2021), which is closely associated with DE and ED symptoms (Smolak & Levine, 2015). A systematic investigation is therefore warranted to explore the ways in which the ongoing pandemic might impact BI, DE, and ED outcomes.
1.1. Lockdown and social distancing measures
Previous reviews have documented the negative impact of social restrictions (e.g., “lockdowns” and related physical distancing measures) associated with the COVID‐19 pandemic on psychological well‐being (Brooks et al., 2020; Rajkumar, 2020; Schneider et al., 2021). Early commentary has indicated that social restrictions may be particularly challenging for individuals living with, and vulnerable to, EDs due to changes in daily routine and increased psychological distress (Rodgers et al., 2020). Furthermore, there have been notable disruptions to treatment and access to professional support (Weissman et al., 2020), though some studies have highlighted a potential benefit of increased online service provision for those not already connected with care (Simpson et al., 2021). In addition, studies have found that changes to meal patterns, food planning and buying, and physical activity have negatively impacted cognitions and behaviors across the spectrum of ED diagnoses (Hansen & Menkes, 2021; Hayes & Smith, 2021). Individuals with higher levels of psychological distress related to COVID‐19 restrictions are more likely to report increased BI concerns and DE (Flaudias et al., 2020; Swami, Horne, et al., 2021), as well as worsened ED symptomatology (Baenas et al., 2020; Chan & Chiu, 2021). This may be exacerbated by increased social media use due to limits on in‐person interactions (Pikoos et al., 2021) and increased exposure to content related to eating and appearance (Holland & Tiggemann, 2016).
1.2. Harmful messaging around quarantine weight gain
Research has also highlighted harmful messaging around weight gain during the COVID‐19 pandemic. Terms such as “covibesity” (Khan & Smith, 2020), “COVID‐15” (Pearl, 2020), and “Quarantine‐15” (Pearl & Schulte, 2021) are considered new risk factors for ED cognitions and behaviors, as well as increased BI concerns. Although considerable research has been conducted on the prevalence of weight gain during COVID‐19, less research has considered the exposure effects associated with this messaging (Pearl & Schulte, 2021). Previous literature shows a negative impact of weight stigmatizing public health messages on multiple physical and mental health outcomes, including reduced physical activity, increased binge eating, greater psychological distress, and an increase in body dissatisfaction (Bristow et al., 2020; Emmer et al., 2020; Mensinger et al., 2021). As such, media coverage of COVID‐19 related to weight gain is likely to exacerbate weight stigma and psychological distress in individuals with EDs, as well as DE behaviors and BI concerns in the general population (Lessard & Puhl, 2021).
1.3. Food insecurity and food shortages
Food insecurity (i.e., concern about, or actual changes in, food availability) has been associated with binge eating and binge eating disorder (BED), bulimia nervosa (BN), as well as general ED pathology and symptomatology (Becker et al., 2017; Hazzard et al., 2020; Lydecker & Grilo, 2019; Rasmusson et al., 2019; Zickgraf et al., 2022). Food insecurity may be exacerbated during COVID‐19 due to increased financial stress and economic limitations, as well as the “panic buying” behaviors and shortage of staple foods that characterized the initial phases of the pandemic (Khosravi, 2020; Weissman et al., 2020). These effects may be further strengthened by the pervasive media coverage about threats of food shortages (Rasmusson et al., 2019). Early research has shown increased food insecurity across multiple countries as a result of the pandemic (Mishra & Rampal, 2020; Niles et al., 2020; Zidouemba et al., 2020), but fewer studies have explored the influence of food insecurity on eating outcomes (Christensen, Forbush, et al., 2021; Coulthard et al., 2021).
1.4. Eating and BI concerns in marginalized groups
To date, most BI and ED research has been conducted with predominantly White, cisgender, and heterosexual participants, with the vast majority of studies taking place in Western, educated, industrialized, rich, and democratic (WEIRD) countries (Mikhail & Klump, 2021). ED research is often conducted with female samples, thus underrepresenting men and nonbinary or genderqueer participants (Burke et al., 2020). This is despite evidence showing that participants who identify as Black, Indigenous, or other People of Color (BIPOC) and participants from non‐WEIRD countries experience equivalent, if not higher, rates of EDs (Acle et al., 2021; Alfalahi et al., 2021). In addition, recent studies have found higher prevalence of BI and DE concerns in lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ+) participants (Nowaskie et al., 2021). Such effects are compounded among individuals who experience multiple intersecting inequalities (e.g., Black, LGBTQ+ women; Crenshaw, 2017), and are thus likely to show the highest prevalence of BI concerns and DE (Beccia et al., 2021). A recent review on the impact of inequality factors on mental health outcomes during COVID‐19 found that certain individual characteristics, such as female gender, existing psychological health conditions, and being subjected to stigma because of one's identity as a member of an ethnic or sexual minority group predicted worse mental health outcomes (Gibson et al., 2021). However, to date, no reviews have looked specifically at BI and eating outcomes during COVID‐19 among marginalized and underrepresented populations.
1.5. The current review
The current mixed‐studies systematic review aimed to assess the influence of COVID‐19 on BI, DE behaviors, and ED outcomes. Several reviews have investigated the effect of COVID‐19 on EDs (Miniati et al., 2021; Monteleone, Cascino, Barone, et al., 2021; Sideli et al., 2021), reporting worsening of symptoms, increased levels of anxiety, and difficulties in treatment compliance during lockdown. However, little is still known about the adverse effects of the pandemic on ED outcomes and no systematic review has hitherto considered the influence of COVID‐19 on BI and DE behaviors in the general population. Furthermore, no previous reviews have adopted a mixed‐studies approach to assess the influence of COVID‐19 on BI and eating concerns. Mixed‐studies reviews maximize the findings of traditional systematic reviews (i.e., reviews summarizing qualitative or quantitative studies), and thus the ability of those findings to inform policy and practice (Harden, 2010; Stern et al., 2020). As such, the current mixed‐studies review will provide a more comprehensive depiction of the influence of COVID‐19 on BI and eating outcomes, and enhance the utility and impact of findings (Harden & Thomas, 2010; Noyes et al., 2019).
Specifically, we aimed to: (1) identify studies that assess the influence of the COVID‐19 pandemic and related variables (e.g., experience of quarantine, social distancing measures, “stay at home” orders, lockdown) on BI, DE, and EDs; (2) evaluate the influence of the COVID‐19 pandemic on ED‐specific and general psychopathology in individuals with EDs; (3) explore possible differences in the experiences of, and responses to, the pandemic among participants from marginalized and underrepresented populations; and (4) provide evidence‐based recommendations for individuals, researchers, clinicians, and public health messaging.
2. METHODS
This review was conducted in collaboration with researchers who have lived experience of EDs (J.S., G.P., and N.C.), clinical experience in nutrition and EDs (A.T. and E.M.), and research expertise in health psychology (B.G. and M.F.), BI (J.S., G.P., A.T., N.C., and E.M.), EDs (J.S., G.P., N.C., D.T., and E.M.), public health (B.G. and M.F.), and conducting systematic reviews (J.S., B.G., D.T., E.M., and M.F.). The review follows the updated Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement (PRISMA; Page et al., 2021) and was preregistered on PROSPERO (ref no. CRD42021247921) prior to commencement (May 10, 2021).
2.1. Data sources and search strategy
Searches were conducted for papers published between December 1, 2019 and August 1, 2021, using the databases PsycINFO, PsycARTICLES, CINAHL Plus, AMED, MEDLINE, ERIC (all accessed via EBSCO), EMBASE, Wiley, and ProQuest (dissertations and theses). We did not limit searches by language or country of publication. Boolean combinations of the following search terms and their abbreviations were used: anorexia; appearance anxiety; appearance comparison; appearance concern; atypical anorexia; atypical bulimia; atypical eating disorder; binge; binge eating; body anxiety; body checking; body dissatisfaction; body dysmorphia; body dysmorphic disorder; body image; body image concern; bulimia; compulsive exercise; dietary restriction; disordered eating; eating disorder; eating pathology; eating disorders not otherwise specified; excessive exercise; feeding disorder; food intake disorder; food restriction; laxative; obsessive exercise; orthorexia; other specified feeding and eating disorders; over exercising; pica; purging; restrictive diet; rumination disorder; shape concern; vomit; weight concern; coronavirus; COVID; COVID‐19; lockdown; pandemic; quarantine; SARS‐CoV‐2; social distancing. The full search strategy can be found on the project's Open Science Framework page (https://osf.io/pz48w/).
Reference sections of the included articles were scanned to identify additional studies that met inclusion criteria. We also searched for “gray literature” and unpublished studies uploaded to PsyArXiv or registered on ClinicalTrials.gov, as well as conference abstracts (Appearance Matters 9 Online Conference, July 13–15, 2021; International Conference on Eating Disorders, June 10–12, 2021) to ensure we captured all relevant research, given the timeliness of COVID‐19. In addition, Emeritus Professor Michael Levine forwarded our request for published and unpublished research to the Levine Prevention/Sociocultural Factors TinyLetter email group, consisting of approximately 1060 researchers across 49 countries who are actively involved in BI and ED research.
2.2. Study eligibility criteria
We included papers that examined the influence of the COVID‐19 pandemic or variables directly related to the pandemic (e.g., experience of quarantine, social distancing measures, “stay at home” orders, lockdown, COVID‐19‐related anxiety or stress) on BI, DE, and ED outcomes. BI outcomes included, for example, experiences of weight stigma, appearance concerns, and body anxiety. DE and ED outcomes included onset of, exacerbation of, or change in specific symptoms (e.g., binge eating, purging, compulsive exercise, food restriction), mental health and well‐being in individuals with diagnosed or undiagnosed EDs (e.g., anxiety, stress, depression, psychological distress, negative affect), and treatment outcomes (e.g., adherence to treatment, treatment efficacy). This was a mixed‐studies review; as such, we included controlled trials, cohort studies, cross‐sectional studies, case reports, and qualitative studies that examined the influence of the COVID‐19 pandemic on target outcomes. We excluded: (1) review papers, commentaries, opinion pieces, and editorials; (2) studies that did not assess the direct relationship between the COVID‐19 pandemic and target outcomes (e.g., studies that were conducted during the pandemic, but did not examine the influence of COVID‐19 or related predictors on target outcomes, or studies that did not compare current levels of BI concerns or ED symptoms with prepandemic levels); and (3) studies related to eating habits, dieting, or exercise unrelated to BI or ED symptomatology (e.g., adherence to a Mediterranean diet, changes in physical activity in the general population).
2.3. Study selection
Two authors (J.S. and G.P.) screened titles and abstracts of retrieved papers against the inclusion and exclusion criteria outlined above. Duplicates and irrelevant papers were removed. J.S. and A.T., and G.P. and B.G. independently screened 50% of the full texts that were identified as potentially eligible. The authors held regular meetings to discuss uncertainties and clarify eligibility criteria. Any discrepancies in selecting the final papers for inclusion were resolved through discussion and consultation with the full review team.
2.4. Data extraction
Data extraction was completed by four researchers who cross‐checked each other's data extraction (J.S., A.T., G.P., and B.G.). In line with Harden (2010), we used two separate protocols for quantitative and qualitative data. Data extracted for quantitative and qualitative studies are presented in Tables 1 and 2, respectively. For studies that described statistically significant outcomes, a p < .05 was considered significant.
TABLE 1.
Characteristics of quantitative studies
| Author(s) (year) | Country | Participants | Methods | Key findings | Study quality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N (% female) a | Age M (SD) | Race and ethnicity | Sexual orientation | Socioeconomic status | Diagnosis | Design | Measures | ||||
| Akgül et al. (2021) | Turkey | 38 (95%) | 15.1 (1.6) | Not reported | Not reported | Not reported | AN‐R n = 26; AN‐BP n = 5; AAN n = 3; BN n = 3; OSFED n = 1 | Cross‐sectional | ED examination; depression; anxiety; obsessive–compulsive symptoms | 42% reported improved ED symptomatology, 37% reported no change, 21% reported worse ED symptomatology from pre‐ to during lockdown; 24% reported that lockdown affected access to ED‐related healthcare; depression score had the highest predictive value for ED behavior (r 2 = .537) | 3 |
| Baceviciene and Jankauskiene (2021) | Lithuania | 230 (79%) | 23.9 (5.4) | Not reported | Not reported | Not reported | n/a | Longitudinal | Attitudes toward appearance; BI; ED examination; self‐esteem | No change in DE or self‐esteem from pre‐ to during lockdown; body appearance evaluation (women only), media pressures (women only), and internalization of thin/low body fat appearance standards (men: d = 1.46; women: d = 1.18) increased from pre‐ to during lockdown | 3 |
| Baenas et al. (2020) | Spain | 74 (96%) | 32.1 (12.8) | Not reported | Not reported | Not reported | AN n = 19; BN n = 12; BED n = 10; OSFED n = 33 | Cross‐sectional | ED inventory; food addiction; symptom checklist; temperament and character; telephone survey | 26% reported worsened symptoms during confinement (highest in AN and OSFED), 74% reported improvements or no change; patients with worsened symptoms reported lower self‐directedness (d = 0.51) and higher prevalence of future concerns (d = 0.51), nonadaptive reactions (d = 0.79), symptoms of anxiety (d = 0.89) and depression (d = 0.96), adverse situations (d = 0.62), and familiar conflict (d = 0.68) | 2 |
| Bellapigna et al. (2021) | United States | 239 (gender: 79% women; 1.3% nonbinary/nonconforming) | 24.7 (11.1) | 6.7% Black/African American; 10% Hispanic; 5.9% Asian; 67.8% White; 9.2% multiracial/biracial; 0.4% “other” | Not reported | Education: 25.6% high school degree or equivalent; 46.2% some college; 10.1% 2‐year degree; 11.8% bachelor's degree; 3.4% master's degree; 2.1% doctorate; 2.8% other | 6.3% diagnosed with ED | Cross‐sectional | Need for structure; loneliness; social networking; body appreciation; eating attitudes; social phobia; patient health | 64% reported more disturbances in BI during COVID; loneliness (β = −.138), negative BI (β = .253), and social media exposure (β = −.161) predicted DE; loneliness (β = −.485), negative BI (β = .123), and social media exposure (β = −.154) predicted depressive symptoms | 3 |
| Branley‐Bell and Talbot (2020) b | United Kingdom | 129 (94%) | 29.3 (9.0) | Not reported | Not reported | Not reported | 62% current ED/relapse; in recovery 6.2% <3 m, 6.2% 3–12 m, 25.6% >12 m | Cross‐sectional | Mental well‐being; perceived stress; social support; sense of control; rumination | 87% reported worsened symptoms as a result of COVID, 30% reported symptoms were much worse, 2% reported slight improvement, 9% reported no change; changes in living situation, social isolation, usual support network(s), physical activity, and time spent online impacted ED symptoms | 3 |
| Branley‐Bell and Talbot (2021) b | United Kingdom | 58 (98%) | 30.9 (11.1) | Not reported | Not reported | Not reported | 63.8% current ED/relapse; 36.2% in recovery; AN n = 28; BN n = 7; OSFED n = 3; BED n = 2; symptoms of multiple EDs n = 12; undisclosed ED n = 7 | Longitudinal | Mental well‐being; perceived stress; social support; sense of control; rumination | 15.5% reported relapsing, 19% reported recovering, and 65.5% reported no change in ED status from during to postlockdown; higher perceived control associated with recovery | 2 |
| Breiner et al. (2021) | United States | 159 (91%) | 27.6 (11.7) | 90.6% White; 5% Hispanic/Latino; 6.3% Asian; 0.6% American Indian or Alaska Native; 0.6% Native Hawaiian or Pacific Islander; 1.3% Native American | 74.8% heterosexual; 2.5% homosexual; 14.5% bisexual | Education: 5% high school graduate; 8.8% less than 2 years of college; 0.6% technical or vocational program; 6.9% associate degree; 62.3% college graduate; 14.5% master's degree; 1.9% doctorate | AN n = 22; BN n = 8; BED n = 4; “other” n = 3 | Cross‐sectional (retrospective) | ED examination; exercise behaviors; exercise motives; ED diagnosis | No significant changes in exercise or eating pathology from pre‐ to during COVID; eating pathology increased in participants with a prior ED diagnosis (d = 0.26), but decreased in participants without a prior ED diagnosis (d = −0.14); there were decreases in episodes of eating more than usual (d = −0.23) and loss of control over eating (d = −0.23), but no changes in objective binge eating (d = −0.04), self‐induced vomiting (d = −0.05), or laxative use (d = −0.14); participants reported increased endorsement of pressure to get in shape from pre‐ to during the pandemic | 3 |
| Buckley et al. (2021) b | Multiple | 204 (86%) | 27.0 (8.1) | Not reported | Not reported | Not reported | 10.7% current ED; 32.8% previous diagnosis (AN n = 29; BN n = 11; ON n = 9; BED n = 7; “other” n = 11) | Cross‐sectional | Eating attitudes; BI and food relationship | 34.8% reported worse BI, 50.5% reported no change, and 14.6% reported better BI from pre‐ to during COVID; 32.8% reported worse relationship with food, 53.0% reported no change, and 14.1% reported better relationship with food from pre‐ to during COVID | 3 |
| Castellini et al. (2020) | Italy | Patients/healthy controls: 74/97 (sex assigned at birth: 100/100% female) | Patients/healthy controls: 31.7/30.5 (12.8/10.9) | 100% White | Not reported | Not reported | AN n = 37; BN n = 37 | Longitudinal | Brief symptom inventory; ED examination; psychological distress | Patients reported increased compensatory exercise during lockdown (AN: d = 0.32; BN: d = 0.30); patients with BN/previously remitted patients reported increased binge eating after lockdown (d = 0.32); household arguments (d = 0.62) and fear for safety of loved ones (d = 0.67) predicted increased symptoms; patients with BN reported more severe COVID‐related posttraumatic symptoms than patients with AN and healthy controls, predicted by childhood trauma (β = .34) and insecure attachment (β = .57) | 1 |
| Cecchetto et al. (2021) | Italy | 365 (73%) | 35.1 (13.6) | Not reported | Not reported | Not reported | n/a | Cross‐sectional | Binge eating screener; alexithymia; anxiety; eating behaviors; patient health; perceived stress | Binge eating and emotional eating decreased from during to postlockdown; emotional eating was predicted by higher depression, anxiety, lower quality of personal relationships, and lower quality of life; increase in binge eating was predicted by higher stress | 2 |
| Chan and Chiu (2021) | Hong Kong | 316 (71%) | 25.1 (5.0) | Not reported | Not reported | 88.3% university educated | n/a | Cross‐sectional | ED screening; patient health; anxiety; psychological well‐being; eating behaviors and emotions | Among individuals with elevated depression, those who attributed depression to COVID reported higher levels of symptoms; no effect on anxiety | 3 |
| Christensen, Forbush, et al. (2021) | United States | 579 (gender identity: 76% women; 2% “other”) | 21.8 (5.3) | 9% Hispanic; 91% non‐Hispanic; 84.1% White; 3.5% Black/African American; 1% American Indian/Alaskan Native; 5.5% Asian/Pacific Islander; 5.2% multiracial; 0.7% not disclosed | Not reported | Years of posthigh school: 20.3% <1 year; 18.7% 1 year; 19.4% 2 years; 22.0% 3 years; 9.9% 4 years; 2.4% 5 years; 5.0% 6+ years 5%; 2.3% continuing education; food insecurity: 52.8% none; 6.6% household food insecurity; 40.6% individual food insecurity | AN n = 4; BN n = 75; BED n = 14; OSFED n = 135; no ED diagnosis n = 344 | Cross‐sectional | Clinical impairment; ED diagnosis; food insecurity | Students with food insecurity showed higher prevalence of ED diagnoses and reported greater frequency of objective binge eating, compensatory fasting, and ED‐related impairment compared with individuals without food insecurity; there were no differences in food insecurity before or during the beginning of the COVID pandemic; participants who identified as Black were significantly more likely to report individual food insecurity relative to other racialized groups | 2 |
| Conceição et al. (2021) | Portugal | COVID/non‐COVID group: 35/66 (94/83%) | COVID/non‐COVID group: 50.8/50.1 (12.4/10.7) | Not reported | Not reported | Education (COVID/non‐COVID group): ≤6 years (42.9/31.8%; 9–12 years (34.3/48.5%); college degree (22.9/19.7%); professional status: student (2.9/1.5%); employed (62.9/57.6%); unemployed (11.4/25.8%); retired: (22.9/15.2%) | n/a | Cohort | ED examination; repetitive eating; depression, anxiety, stress; impulsivity | Participants assessed post‐COVID showed a greater increase in weight concern scores (ƞ 2 p = 0.094) and repetitive eating (ƞ 2 p = 0.076) compared with participants assessed pre‐COVID; no difference between groups in shape concern, food concerns, or restraint eating | 1 |
| Coulthard et al. (2021) | United Kingdom | 620 (88%) | 39.9 (14.0) | 88% White‐British/European; 6% Asian/British Asian; 1% Black/Black British; 4% “other”; 1% not disclosed | Not reported | Occupation: 39% professional; 21% intermediate; 15% manual; 25% not working; food insecurity: 65% none; 29% mild; 6% moderate/severe | n/a | Cross‐sectional | Food consumption; ED symptoms; coping strategies; anxiety; food insecurity | Emotional eating decreased from pre‐ to during lockdown; women and those isolating at home were more likely to report higher emotional eating during lockdown; there was no differences in eating behavior based on occupation or ethnicity; higher emotional eating during lockdown associated with higher BMI, higher prelockdown emotional eating, and maladaptive coping strategies | 2 |
| Czepczor‐Bernat et al. (2021) | Poland | 671 (100%) | 32.5 (11.4) | 98.8% White; 0.3% mixed race; 0.9% “other” | 91.3% heterosexual; 1.6% lesbian; 4.9% bisexual; 0.7% pansexual/queer; 0.9% asexual; 0.6% “other” | Education: cluster 1 32% secondary/technical school; cluster 2 32% secondary/technical school; cluster 3 37% master's degree; cluster 4 45% master's degree | n/a | Cross‐sectional | COVID‐related stress; COVID‐related anxiety; ED inventory; BI | Higher levels of ED symptoms and negative BI were observed in women with excess body weight, high anxiety, and stress related to COVID as compared with women with a healthy body weight and with low levels of anxiety and stress | 3 |
| Félix et al. (2021) | Portugal | 24 (100%) | 50.9 (12.8) | Not reported | Not reported | Education: 29.2% elementary school; 25.0% middle school; 12.5% high school; 33.3% college degree; employment: 66.7% employed; 8.3% unemployed; 25.0% retired | n/a | Cross‐sectional | Depression, anxiety, stress; impulsivity; DERS; ED examination; loss of control over eating; repetitive eating; ED symptoms; impact on emotions, eating, and weight; COVID impact | Living with fewer people, higher difficulties in dealing with emotionally activating situations, and higher fear of gaining weight during lockdown associated with greater fear of gaining weight, greater fear of losing control over eating, and greater DE psychopathology | 2 |
| Fernández‐Aranda, Munguía, et al. (2020) | Spain | 121 (86%) | 33.7 (15.8) | Not reported | Not reported | Not reported | AN n = 55; BN n = 18; OSFED n = 14 | Cross‐sectional | COVID isolation eating scale | Patients with AN reported a positive response to treatment during confinement; no significant changes found in patients with BN; patients with OSFED reported an increase in eating symptomatology and psychopathology; patients with AN reported greatest dissatisfaction and accommodation difficulty with remote therapy | 3 |
| Fernández‐Aranda, Casas, et al. (2020) Study 1 | Spain | 32 (91%) | 29.2 (range 16–49 years) | Not reported | Not reported | Not reported | AN n = 13; BN n = 10; BED n = 4; OSFED n = 5 | Cross‐sectional | Telephone survey | Most patients presented worries about increased uncertainties, such as the risk of COVID infection of themselves or their loved ones, the negative impact on their work, and their treatment; 38% reported impairments in ED symptomatology; 56% reported additional anxiety symptoms | 3 |
| Flaudias et al. (2020) | France | 5738 (75%) | 21.2 (4.5) | Not reported | Not reported | University students, 48.8% with scholarship | 38.3% at risk for ED symptoms | Cross‐sectional | Anxiety and depression; perceived stress; ED inventory; ED screening; ideal body stereotypes | Greater likelihood of binge eating (BE) and dietary restriction (DR) over past week and/or future intentions to binge eat (FBE) and restrict (FDR) associated with lockdown‐related stress (all odds ratios [OR]; BE = 1.12; DR = 1.17; FBE = 1.33; FDR = 1.12), exposure to COVID‐related media (BE = 1.02; DR = 1.05; FBE = 1.20; FDR = 1), female gender (BE = 1.40; DR = 1.79; FBE = 1.09; FDR = 1.48), greater levels of anxiety (BE = 1.09; DR = 1.11; FBE = 0.95; FDR = 1.04) and depression (BE = 1.14; DR = 0.94; FBE = 1.40; FDR = .95), low impulse regulation (BE = 1.10; DR = 1.04; FBE = 1.23; FDR = 1.12), higher BMI (BE = 1.26; DR = 1.07; FBE = 1.19; FDR = 1.04), body dissatisfaction (BE = 1.08; DR = 1.80; FBE = 0.84; FDR = 2.05), and concurrent probable ED (BE = 2.82; DR = 2.65; FBE = 2.11; FDR = 2.58) | 3 |
| Giel et al. (2021) | Germany | 42 (81%) | 45.5 (12.6) | Not reported | Not reported | Not reported | BED n = 17 | Longitudinal | ED examination; perceived stress; binge eating frequency; depression; emotion regulation; coherence | Binge eating frequency (χ 2 = 15.22), general ED pathology (χ 2 = 35.52), and depressive symptoms (χ 2 = 5.41) increased from pre‐ to post‐COVID; individuals scoring high on reappraisal and sense of coherence scored lower on general ED pathology | 3 |
| Graell et al. (2020) | Spain | Day hospital/outpatient clinic: 27/338 (93/87%) | Day hospital/outpatient clinic: 13.2/14.7 (3.0/2.3) | Not reported | Not reported | Not reported | ARFID n = 48; AN n = 255; BN n = 26; OSFED n = 37 | Cross‐sectional (retrospective) | Outpatient and face‐to‐face consultations | 42% reported reactivation of ED symptoms following COVID confinement (>adolescents); 68% of patients and their families reported onset of confinement and 41% reported social isolation from peers as influencing factors for admission | 2 |
| Gullo and Walker (2021) | United States | 143 (gender: 53% ciswomen; 1% transmen; 0% transwomen; 1% nonbinary) | 77% 18–44 years | 79.7% White: 9.8% Black: 4.2% Asian; 3.5% Latinx: 1.4% mixed; 0.7% Native American; 0.7% “other” | Not reported | Household annual income (USD): 2.8% <15,000; 9.1% 15,000–29,999; 11.9% 30,000–49,999; 23.8% 50,000–75,999; 16.8% 75,000–99,999; 17.5% 100,000–150,000; 14.0% >150,000; 4.2% prefer not to answer | n/a | Cross‐sectional (retrospective) | Depression, anxiety, stress; BI; binge eating; body satisfaction | Time spent videoconferencing increased from pre‐ to post‐COVID; appearance dissatisfaction increased (β = .75), but appearance orientation decreased (β = .75) following lockdown; no change in binge eating from pre‐ to postlockdown; videoconferencing time did not predict BI or binge eating postlockdown | 3 |
| Haddad et al. (2020) | Lebanon | 407 (51%) | 30.6 (10.1) | Not reported | Not reported | Education: 90.9% university level; 9.1% secondary school or lower | n/a | Cross‐sectional | Boredom; ED examination; quarantine/ confinement stressors; fear of COVID; anxiety; physical activity | Dietary restraint (DR), eating concerns (EC), shape concerns (SC) and weight concerns (WC) were associated with female gender (all β; EC = 0.52; SC = 0.19; WC = 0.20), higher anxiety (EC = 0.04; SC = 0.23; WC = 0.19), sense of insecurity (EC = 0.41), greater fear of COVID (DR = 0.02; SC = 0.20; WC = 0.12), higher BMI (DR = 0.05; EC = 0.06; SC = 0.39; WC = 0.41), physical activity (DR = 1.04; EC = 0.43; SC = 0.15; WC = 0.19), and a higher number of adults living together in quarantine/confinement (SC = 0.10; WC = 0.15) | 2 |
| Haddad et al. (2021) | Lebanon | 407 (51%) | 30.6 (10.1) | Not reported | Not reported | Household monthly income (USD): 31.0% no income; 20.4% <1000; 29.1% 1000–2000; 19.3% >2000 | n/a | Cross‐sectional | Boredom; ED examination; quarantine/ confinement stressors; fear of COVID; anxiety; physical activity; perceived weight change | Longer confinement duration (OR = 1.07), higher anxiety (OR = 1.05), and higher eating concerns (OR = 1.81) associated with higher weight change perception; greater fear of COVID (OR = 0.96) and higher self‐reported weight change (OR = 0.47) associated with lower weight change perception | 2 |
| Jordan et al. (2021) | United States | 140 (89%) | 39.8 (6.9) | 88.4% White | Not reported | 82.2% middle to upper‐middle class | n/a | Cross‐sectional | Perceived stress; concern about weight gain; ED examination; emotional eating |
Disordered eating associated with concern about weight gain before (β=.18) and during (β=.32) COVID; stress and concern about weight gain during COVID predicted variance in eating pathology among caregivers (r 2 = 0.48). |
2 |
| Keel et al. (2020) | United States | 90 (88%) | 19.5 (1.3) | 22% Latinx; 78% White; 12% Black/African American; 4% Asian; 1% American; Indian/Alaskan Native; 3% “other” | 89% heterosexual | Not reported | n/a | Longitudinal | Weight perception; physical activity; eating; concerns about weight and shape; body, eating, exercise comparisons; ED diagnosis; screen time | Participants reported increased body weight (d = 0.23), eating (d = 0.54), screen time (d = 1.08), and concerns about weight/shape (d = 0.93) and eating (d = 0.79), and decreased physical activity (d = −0.63) from pre‐ to post‐COVID; no change in weight or BMI, but participants reported shifts in body weight perception from pre‐ to post‐COVID | 3 |
| H. Kim, Rackoff, et al. (2021) | United States | Pre‐/during COVID: 3643/4970 (sex assigned at birth: 73/70% female; 0.05/0.02% intersex; gender identity: 70/68% women; 4/2% trans, nonconforming, or self‐identify) | Not reported | Pre‐/during COVID: 12/10% Hispanic; 88/90% non‐Hispanic; 72/75% White; 9/6% Black/African American; 10/14% Asian; 0.7/0.5% American Indian or Alaskan Native; 0.4/0.2% Native Hawaiian or Pacific Islander; 8/5% multiracial | Pre‐/during COVID: 71/81% heterosexual; 29/19% lesbian, gay, bisexual, queer, questioning, or self‐identify | Not reported | Pre‐/during COVID: AN n = 64/88; BN/BED n = 320/643 | Longitudinal | Anxiety; posttraumatic stress; patient health; presence of EDs; insomnia; alcohol use | Depression (χ 2 = 21.67), alcohol use disorder (χ 2 = 67.26), BN/BED (χ 2 = 20.83), and comorbidity (χ 2 = 6.83) were greater during than before COVID; posttraumatic stress disorder was lower during than pre‐COVID (χ 2 = 5.46); no differences in anxiety, insomnia, AN, or suicidality between pre‐ and during COVID; no effect of gender, ethnicity/racialized group, or sexuality on EDs | 2 |
| S. Kim, Wang, et al. (2021) | United States | 7317 (59%) | 50.6 (16.1) | 64.7% non‐Hispanic White; 7.9% non‐Hispanic Black; 16.8% Hispanic; 5.1% non‐Hispanic Asian; 0.9% Native American; 4.5% “other”; 0.2% not disclosed | Not reported | Education: 5.4% <high school; 16.7% high school or less; 22.8% some college; 14.3% associate degree; 24.3% bachelor's degree; 16.5% advanced college degree | Diagnosed ED n = 157; unsure about ED status n = 122 | Longitudinal | Patient health; perceived stress; loneliness | Individuals with EDs/unsure EDs reported higher levels of psychological distress (all B; EDs = 2.18; unsure EDs = 2.01), stress (EDs = 1.17; unsure EDs = 2.08), and loneliness (unsure EDs = 0.90) compared to those without EDs; those unsure about their EDs reported initial decreases in stress and loneliness, but started increasing again since institution of virus containment procedures; levels of loneliness among those with EDs increased initially then began to decrease; individuals with EDs showed steady decreases in stress; identifying as Black, older age, and higher education associated with lower psychological distress (Black = −0.59; age = −0.03; education = −0.03), stress (age = −0.04; education = −0.13), and loneliness (Black = −0.10; age = −0.01); female gender and identifying as Asian associated with higher psychological distress (female = 0.61; Asian = 0.29), stress (female = 0.56; Asian = 1.07), and loneliness (female = 0.14) | 1 |
| Koenig et al. (2021) | Germany | Pre/postlockdown: 324/324 (69/69%) | 14.9 (1.9) | Not reported | Not reported | Family affluence (pre‐/postlockdown): low (1.9/1.9%); medium (24.4/ 21.6%); high (73.9/76.5%) | n/a | Longitudinal | Strengths and difficulties; patient health; weight concerns; ED examination; quality of life; suicidality | No differences between pre‐ and postlockdown samples in emotional and behavioral problems, depression, thoughts of suicide/suicide attempts, ED symptoms, or quality of life | 1 |
| Larkin (2021) | United States | 290 (not reported) | Range 18–25 years | 0.3% American Indian/Alaskan Native; 2.8% Asian; 10.3% Black/African American; 14.5% Hispanic/Latino; 1.7% biracial/multiracial; 80.7% White | Not reported | Not reported | n/a | Cross‐sectional (retrospective) | Physical activity, social media use; subjective well‐being; BI | 32.7% increase in negative BI perceptions from pre‐ to post‐COVID | 3 |
| Leenaerts et al. (2021) | Belgium | 15 (100%) | Median (IQR) = 23 years (21.5–25.5) | 87% European; 13% Asian | Not reported | Not reported | BN | Longitudinal | Affect; location; social context; binge eating frequency | Patients reported higher negative affect (β = .15), lower positive affect (β = −.10), and changes in surroundings and social context (at home: β = 3.19; with housemates: β = 3.91; with friends: β = −2.45; with family: β = .99; with partner: β = −2.39) from pre‐ to postlockdown; changes of negative affect associated with binge eating frequency during lockdown (β = .61) | 2 |
| Lessard and Puhl (2021) | United States | 452 (gender identity: 55% women; 2% transgender; 1% “other”; sex assigned at birth: not reported) | 14.9 (2.1) | 69.9% White; 8.2% Black/African American; 8.0% Latinx; 6.6% multiethnic; 5.5% Asian/Pacific Islander; 1.8% “other” | Not reported | 72% had a parent with a college degree or higher | n/a | Cross‐sectional | Body dissatisfaction; exposure to weight stigma on social media; experienced weight stigma | 53% reported increased exposure to weight stigmatizing social media content; 41% reported increased body dissatisfaction from pre‐ to post‐COVID (>girls; higher weight), 49% reported no change, 10% reported a decrease | 3 |
| Lin et al. (2021) | United States | Not reported | Range 8–26 years | Not reported | Not reported | Not reported | Patients with any ED diagnosis | Longitudinal | COVID‐related trends in ED care‐seeking | Inpatient admissions, hospital bed‐days, outpatient inquiries increased over time post‐COVID compared to stable volume pre‐COVID; outpatient assessments decreased initially following COVID‐related limitations, then rebounded | 2 |
| Machado et al. (2020) | Portugal | 43 (95%) | 27.6 (8.5) | Not reported | Not reported | Not reported | AN n = 20; BN n = 14; BED n = 2; OSFED n = 7 | Longitudinal | ED examination; clinical impairment; impulsivity; difficulties in emotion regulation; COVID impact | Of 26 patients in treatment 31% remained unchanged, 27% deteriorated, and 42% improved; of 17 participants not in treatment 53% remained unchanged, 18% deteriorated, and 29% improved from during to postlockdown; higher impact correlated with ED symptoms, impulsivity (r = .380), psychopathology (r = .451), emotion regulation difficulties (r = .393) and clinical impairment (r = .569) | 3 |
|
Martínez‐de‐Quel et al. (2021) |
Spain | 161 (37%) | 35.0 (11.2) | Not reported | Not reported | Not reported | n/a | Longitudinal | Eating attitudes | No change in ED risk from before to during COVID lockdown | 2 |
| Meda et al. (2021) | Italy | 358 (80%) | 21.3 (2.1) | Not reported | Not reported | Not reported | Not reported | Longitudinal | ED inventory; eating habits; obsessive–compulsive symptoms; anxiety; depression | Only students with ED history reported an increase in ED symptomatology from pre‐ to postlockdown (β = .1). | 3 |
| Monteleone, Cascino, Marciello, et al. (2021) | Italy | 312 (gender identity: 96% women; 0.3% nonbinary) | AN: 26.9 (10.3); other EDs: 32.3 (13.5) | Not reported | Not reported | Employment (AN/other EDs): paid job (26/39%); student (56/49%) | AN n = 179; BN n = 63; BED n = 48; OSFED n = 22 | Cross‐sectional (retrospective) | Factors related to COVID concerns; illness duration; treatment‐related variables; ED psychopathology | General (GP) and specific psychopathology (SP) worsened from pre‐ to postlockdown; perceived low quality of therapeutic relationships (GP: β = −.16; SP: β = −.22), fear of contagion and increased isolation (GP: β = .22; SP: β = .22), reduced satisfaction with relationships (SP: β = .24), and reduced social support (GP: β = .23) associated with worsened psychopathology; no effect of intimate relationships, illness duration, diagnosis, economic change, or type of treatment | 2 |
| Monteleone, Marciello, et al. (2021) | Italy | 312 (gender identity: 96% women; 0.3% nonbinary) | 29.2 (12.1) | Not reported | Not reported | Not reported | AN n = 179; BN n = 63; BED n = 48; OSFED n = 22 | Cross‐sectional (retrospective) | Anxiety; posttraumatic stress; obsessive–compulsive symptoms; patient health; ED inventory | General and specific psychopathology worsened from pre‐ to postlockdown; symptoms persisted postlockdown, apart from suicide ideation; individuals with AN reported higher anxiety, obsessive–compulsive symptoms, suicide ideation, and physical activity levels, and lower binge eating; no effect of age or illness duration | 2 |
| Nisticò et al. (2021) | Italy | 40 (95%) | 30.9 (14.2) | 100% White | Not reported | Not reported | AN n = 15; BN n = 11; BED n = 14 | Longitudinal | ED examination; depression, anxiety, stress; psychological distress | Posttraumatic stress (IES‐R total score: η 2 p = 0.145) and ED symptoms (η 2 p = 0.142–0.249) improved from during to postlockdown; no change in stress, anxiety, or depression | 2 |
| Pfund et al. (2020) | United States | 438 (gender identity: 100% women; 434 ciswomen and 4 transwomen) | 31.3 (12.7) | 11% African American/Black; 22% Asian/Asian American; 52% European American/White; 10% Latinx American/Hispanic; 2% Middle Eastern, and 3% “other”/not disclosed | Not reported | Not reported | n/a | Cross‐sectional | Body surveillance; appearance comparison; body satisfaction | Time video chatting increased from pre‐ to post‐COVID (d = 0.53). Time video chatting not associated with appearance satisfaction; self‐objectification moderated relationship between time video chatting and appearance satisfaction (B = −.04 for face satisfaction and B = −.02 for body satisfaction); participants who spent more time engaged with their families over video chatting services reported greater face (r = .21) and body (r = .17) satisfaction | 2 |
| Phelan et al. (2021) | Ireland | 1031 (sex assigned at birth: 100% female) | 36.7 (6.6) | 97% White; 2% Asian; 0.3% Black; 0.5% “other” | Not reported | Not reported | n/a | Cross‐sectional | Mental health symptoms, diet, exercise | Participants reported an increase in binge eating from pre‐ to during COVID | 3 |
| Philippe et al. (2021) | France | 498 (52%) | 7.3 (2.3) | Not reported | Not reported | Not reported | n/a | Cross‐sectional (retrospective) | Eating difficulties; eating behavior; parental feeding practices | Parents reported an increase in their child's emotional overeating, food responsiveness, food enjoyment, and appetite, but no change in their child's pickiness from pre‐ to during lockdown; boredom predicted increased food responsiveness (β = .14), emotional overeating (β = .20), and snack frequency between meals (β = .28) | 2 |
| Phillipou et al. (2020) | Australia | 5469 (96% women; 3% preferred to self‐describe) | 30.5 (8.2) | Not reported | Not reported | Not reported | AN n = 88; BN n = 23; BED n = 6; OSFED n = 4; UFED n = 68; recovering/in recovery n = 10 | Cross‐sectional | Depression, anxiety, stress; ED examination | Participants with ED history reported increased restricting (64.5%), binge eating (35.5%), purging (18.9%), and exercise behaviors (47.3%); participants without ED history reported both increased restricting (27.6%) and binge eating behaviors (34.6%), but decreased exercise (43.4%) from pre‐ to during COVID | 3 |
| Pikoos et al. (2020) | Australia | 216 (gender: 88% women; 0.01% “other”) | 32.5 (11.8) | Not reported | Not reported | Not reported | n/a | Cross‐sectional | Dysmorphic concern; depression, anxiety, stress; appearance‐focused behaviors | Appearance‐focused behaviors decreased in participants with low dysmorphic concerns, but not in participants with high dysmorphic concerns from pre‐ to during COVID; living alone, younger age, higher dysmorphic concern, and greater distress over beauty service closure predicted appearance‐focused behaviors | 2 |
| Puhl et al. (2020) | United States | 584 (gender identity: 64% women; 1% “other”) | 24.6 (2.0) | 30.2% White; 16.8% African American/ Black; 17.1% Hispanic; 24.3% Asian American; 11.6% “other” | Not reported | 31.5% lower class; 20.0% lower middle class; 17.4% middle class; 19.4% upper middle class; 11.7% upper class (assumed self‐report) | n/a | Longitudinal | Psychological distress; eating behaviors; binge eating; physical activity; weight stigma | Pre‐COVID experiences of weight stigma predicted higher levels of depressive symptoms (β = .15), stress (β = .15), eating as a coping strategy (β = .16), and an increased likelihood of binge eating during COVID (OR = 2.88), but were unrelated to physical activity; no effect of gender | 2 |
| Ramalho et al. (2021) | Portugal | 254 (83%) | 35.8 (11.8) | Not reported | Not reported | Education: 13.0% high school; 27.2% bachelor's degree; 59.8% master's degree/doctorate | n/a | Cross‐sectional | DE behaviors; COVID impact; depression, anxiety, stress; ED symptoms | Psychosocial impact of COVID predicted DE behaviors mediated through psychological distress (>women; younger age) (β = .10); psychosocial impact of COVID associated with emotional eating (r = .23) and uncontrolled eating (r = .18) | 2 |
| Richardson et al. (2020) b | Canada | 439 (gender: 80% women; 2% transgender; 11% did not disclose) | Not reported | Not reported | Not reported | Not reported | AN n = 83; BN n = 44; ARFID n = 4; BED n = 66; OSFED n = 9; undisclosed/ undiagnosed n = 233 | Cross‐sectional (retrospective) | Telephone survey | Service utilization, ED symptoms, anxiety, and depression increased from pre‐ to during COVID among patients with EDs | 3 |
| Robertson et al. (2021) | United Kingdom | 264 (78%) | Range 18–79 years | 92% White | Not reported | Not reported | 13.8% current or past ED diagnosis | Cross‐sectional | Perceived change in eating, exercise, and BI; patient health | 53% reported more difficulty regulating eating; 60% reported more preoccupation with food/eating; 50% reported exercising more; 68% reported thinking more about exercise; 49% reported more appearance concerns from pre‐ to during lockdown (>women; participants with past/current ED); psychological distress was correlated with finding it more difficult to control/regulate one's eating (rs = .36), being more preoccupied with food/eating (rs = .29), thinking more about exercise (rs = .17), and being more concerned about one's appearance (rs = .41) | 3 |
| Scharmer et al. (2020) | United States | 295 (65%) | 19.7 (2.0) | 48% White; 21% African American; 11% Asian; 14% Hispanic/Latino; 1% Native American; 1% Native Hawaiian/Pacific Islander; 3% “other” | Not reported | Not reported | n/a | Cross‐sectional | ED examination; compulsive exercise; anxiety; fear of illness and virus evaluation; intolerance of uncertainty; physical activity | COVID anxiety and intolerance of uncertainty was associated with ED pathology, but not compulsive exercise; trait and COVID intolerance of uncertainty moderated associations between COVID anxiety and compulsive exercise and ED pathology; COVID anxiety was more strongly related to compulsive exercise and ED pathology for individuals with lower intolerance of uncertainty | 3 |
| Schlegl, Maier, et al. (2020) | Germany | 159 (100%) | 22.4 (8.7) | Not reported | Not reported | Not reported | AN | Cross‐sectional (retrospective) | Psychological consequences of COVID | >70% reported that eating, shape and weight concerns, drive for physical activity, loneliness, sadness, and inner restlessness increased from pre‐ to during COVID and access to in person care decreased; participants reported daily routines, day planning, and enjoyable activities as the most helpful coping strategies; reduction in overall ED symptoms/taking on responsibility to recover, reduction in specific ED symptoms, more flexibility regarding meals and foods, wake‐up call/will to live, trying out therapy content, and accepting uncertainty in life were reported as positive impacts of COVID | 3 |
| Schlegl, Meule, et al. (2020) | Germany | 55 (100%) | 24.4 (6.4) | Not reported | Not reported | Not reported | BN | Cross‐sectional (retrospective) | Psychological consequences of COVID | 49% reported deterioration of ED symptomatology and 62% reported reduced quality of life; frequency of binge eating increased in 47% of patients, self‐induced vomiting in 36%, laxative use in 9%, and diuretic abuse in 7%; face‐to‐face psychotherapy decreased by 56%, videoconferencing therapy was used by 22% of patients; enjoyable activities, virtual contact with friends, and mild physical activity rated as most helpful coping strategies | 3 |
| Serin and Koç (2020) | Turkey | 1064 (59%) | Not reported | Not reported | Not reported | Not reported | n/a | Cross‐sectional | Eating behaviors; depression | External eating, but not emotional or restrictive eating, higher in participants who reported self‐isolating, compared to those who did not (>women) | 2 |
| Spettigue et al. (2021) | Canada | 48 (gender: 83% ciswomen; 2% transwomen; 4% transmen) | 14.6 (1.8) | Not reported | Not reported | Not reported | AN‐R n = 24; AN‐BP n = 7; ARFID n = 7; AAN n = 6; BN n = 1; UFED n = 3 | Cohort | ED examination; eating attitudes; clinical impairment | 40% cited pandemic as trigger for ED; inpatient admissions, emergency room consultation requests, and outpatient referrals deemed “urgent” were higher during COVID compared to pre‐COVID; compared to 2019 ED patients, ED patients in 2020 reported worse clinical impairment from ED symptoms (d = 0.44) and higher levels of eating restraint (d = 0.63) | 2 |
| Stoddard (2021) b | United States | 69 (gender identity: 96% women; 4% nonbinary) | 96% 18–34 years | 91% White; 7% Black; 3% Asian; 6% Latina; 3% “other” | Not reported | Not reported | Previous/current: 83/71% BI disturbance; 84/51% DE habits; 72/13% ED | Cross‐sectional | ED/BI status/concern level; impact of COVID; experiences of ED/BI; coping mechanisms | 84% reported concern about how their weight/bodies might be affected by COVID; 59% reported that their BI/ED worsened from pre‐ to post‐COVID; 78% reported that their relationships with their bodies have changed (70% negative, 26% positive, 4% neutral) | 2 |
| Swami, Horne, et al. (2021) | United Kingdom | 506 (gender identity: 44% women) | 34.3 (11.4) | 88.5% White | 89.1% heterosexual | Education: 10.9% high school; 27.9% advanced qualification; 38.3% undergraduate degree; 19.0% postgraduate degree; 3.9% other | n/a | Cross‐sectional | Perceived stress; ED inventory; body attitude; COVID‐related stress and anxiety | In women, COVID‐related anxiety associated with body dissatisfaction and COVID‐related anxiety and stress was associated with drive for thinness; in men, COVID‐related anxiety was associated with low body fat dissatisfaction and COVID‐related anxiety and stress was associated with muscularity dissatisfaction | 2 |
| Swami, Todd, et al. (2021) | United Kingdom | 600 (gender identity: 49% women) | 34.6 (12.3) | 85% White; 9% Asian; 2% Black; 4% mixed race; 0.3% “other” | 87% heterosexual; 3% gay/lesbian; 8% bisexual; 2% identified with another orientation | Not reported | n/a | Cross‐sectional | BI disturbance; COVID‐related stress; self‐compassion | COVID‐related stress associated with greater BI disturbance, mediated by lower self‐compassion; self‐compassion did not moderate effects of stress on BI disturbance | 2 |
| Tabler et al. (2021) b | United States | 411 (74% women; 5% transgender, genderqueer, or nonbinary) | 28.5 (11.4) | 86% White; 14% Latinx | 71% heterosexual; 29% lesbian, gay, bisexual, or queer | 44% working class; 44% middle class; 12% upper middle class (self‐report) | n/a | Cross‐sectional | ED examination; pandemic‐related stress | Pandemic‐related stress associated with ED symptoms and perceived weight gain (>LGBTQ+ individuals) | 2 |
| Taquet et al. (2021) | United States | 5,186,451 (55%) | 15.4 (9.0) | Not reported | Not reported | Not reported | Patients with any ED diagnosis | Cross‐sectional (retrospective) | Incidence of ED diagnosis | Diagnostic incidence of EDs 15.3% higher in 2020 compared with previous 3 years; increase occurred solely in women, and primarily related to teenagers and AN; higher proportion of patients with EDs in 2020 had suicidal ideation or attempted suicide | 1 |
| Termorshuizen et al. (2020) | United States; Netherlands | United States/Netherland: 511/510 (gender identity: 95/98% women; 2/0.6% nonbinary/genderfluid/“other”) | United States: 30.6 (9.4); Netherlands: 90% 16–39 years | Not reported | Not reported | Not reported | AN n = 665; BN n = 295; BED n = 216; AAN n = 203; OSFED n = 192; purging disorder n = 47; ARFID n = 36; night‐eating syndrome n = 25 | Cross‐sectional | Impact of COVID on EDs, general physical and mental well‐being, and ED treatment | Participants with AN reported increased restriction and fears about being able to find foods consistent with meal plan from pre‐ to during COVID; participants with BN and BED reported increases in binge eating and urges to binge; participants reported positive effects of COVID including greater connection with family, more time for self‐care, and motivation to recover | 2 |
| Trott et al. (2021) | United Kingdom | 319 (84%) | 36.7 (11.8) | Not reported | Not reported | Not reported | n/a | Longitudinal | Body dysmorphic symptoms; eating attitudes; exercise addiction | ED symptomatology and exercise increased while exercise addiction decreased from pre to postlockdown; no changes in body dysmorphic symptoms from pre‐ to postlockdown | 2 |
| Vall‐Roqué et al. (2021) | Spain | 2601 (gender: 100% women) | 24.1 (5.0) | Not reported | Not reported | Not reported | n/a | Cross‐sectional (retrospective) | ED inventory; social network sites use; self‐esteem | Social media network site use increased from pre‐ to during lockdown and was associated with lower self‐esteem (g = 0.15 for 14–24 year olds), higher body dissatisfaction (g = −0.14 for 14–24 year olds), and higher drive for thinness (g = −0.18 for 14–24 year olds, g = −0.22 for 25–35 year olds) (>younger age) | 2 |
| Vitagliano et al. (2021) | United States | 89 (sex assigned at birth: 89% female) | 18.9 (2.9) | 78% White, non‐Hispanic; 8% Asian; 7% Multiracial; 4% Hispanic; 1% Black; 2% “other” | Not reported | Not reported | 84% restrictive ED diagnosis; 16% other ED diagnosis | Cross‐sectional | ED related concerns and motivation to recover; triggering environment; ED diagnosis | 63% reported concern for worsening of their ED due to a “triggering environment”; 74% reported an increase in ED thoughts, 77% reported anxiety, 73% reported depression, and 80% reported isolation they perceived to be related to COVID; 29% reported decrease in motivation to recover they perceived to be related to COVID; participants who reported concern for worsening of their ED due to a triggering environment expressed decreased motivation to recover (OR = 18.1) and increased ED thoughts (OR = 23.8) compared to those who did not report concern for worsening of their ED due to a triggering environment | 3 |
| Vuillier et al. (2021) b | United Kingdom | 207 (63%) | 30.0 (9.7) | 93.7% White British/Irish/Scottish/European; 5.3% Asian; 0.5% Black; 0.5% Arab | Not reported | Not reported | AN n = 91; BN n = 46; BED n = 44; OSFED n = 26 | Cross‐sectional | Depression, anxiety, stress; ED examination | 83.1% reported worsening of ED symptomatology, 7.7% reported no change, 6.8% reported improvements in ED symptomatology; changes did not differ based on diagnosis; changes to routine and physical activity and emotion difficulties were most important factors in predicting change in ED symptoms | 3 |
| White III (2021) | United States | 311 (70%) | Not reported | 33.1% African American; 55.3% White; 11.6% “other” | Not reported | Not reported | n/a | Cross‐sectional (retrospective) | Physical activity; self‐esteem; BI | Self‐esteem and BI worsened from pre‐ to during COVID | 3 |
| Zhou and Wade (2021) | Australia | 100 (100%) | 19.9 (2.0) | 88% White; 6% Asian; 6% “other” | Not reported | Not reported | n/a | Cohort (part of randomized controlled trial) | ED examination; BI acceptance; self‐compassion | Weight concerns (d = 0.46), DE (fasting, binge eating, vomiting, and driven exercise; d = 0.55), and negative affect (d = 0.40) increased from pre‐ to during COVID, all associated with moderate effect sizes | 2 |
Note: Study quality was assessed using the EPHPP guidelines as follows: 1 = “strong,” 2 = “moderate,” 3 = “weak.” Effect size interpretation: Cohen's d/Hedge's g: 0.2 = small, 0.5 = medium, 0.8 = large; η 2/η 2 p: 0.01 = small, 0.06 = medium, 0.14 = large; r 2: 0.01 = small, 0.09 = medium, 0.25 = large; odds ratio (OR): 1.68 = small, 3.47 = medium, 6.71 = large c ; Pearson's r: 0.1 = small, 0.3 = medium, 0.5 = large.
Abbreviations: AN, anorexia nervosa; AAN, atypical anorexia; AN‐BP, binging/purging anorexia subtype; AN‐R, restrictive anorexia subtype; ARFID, avoidant restrictive food intake disorder; BED, binge eating disorder; BI, body image; BN, bulimia nervosa; DE, disordered eating; ED, eating disorder; OSFED, other specified feeding or eating disorder; UFED, unspecified feeding or eating disorder.
The majority of included studies did not specify whether they assessed sex assigned at birth, gender, or gender identity; where this information is available, sex assigned at birth, gender, and gender identity are reported separately.
Signifies a multimethods paper. Information detailed here concerns the quantitative methods, analysis, and findings. See Table 2 for the qualitative characteristics of this study.
Chen, H., Cohen, P., & Chen, S. (2010). How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics—Simulation and Computation, 39(4), 860–864.
TABLE 2.
Characteristics of qualitative studies
| Author(s) (year) | Country | Participants | Methodology | Key findings | Study quality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N (% female) a | Age M (SD) | Race and ethnicity | Sexual orientation | Socioeconomic status | Diagnosis | Data collection methods | Data analysis | ||||
| Branley‐Bell and Talbot (2020) b | United Kingdom | 129 (94%) | 29.3 (89.0) | Not reported | Not reported | Not reported | 62% current ED/relapse; in recovery 6.2% <3 m, 6.2% 3–12 m, 25.6% >12 m | Online survey | Thematic analysis | Themes generated: (1) disruption to living situation; (2) increased social isolation and reduced access to usual support networks; (3) changes to physical activity rates; (4) reduced access to healthcare services; (5) disruption to routine and perceived control; (6) increased exposure to triggering messages; (7) changes to the individual's relationship with food; (8) positive outcomes | 6.5 |
| Branley‐Bell and Talbot (2021) b | United Kingdom | 58 (98%) | 30.9 (11.1) | Not reported | Not reported | Not reported | 63.8% current ED/relapse; 36.2% in recovery; AN n = 28; BN n = 7; OSFED n = 3; BED n = 2; symptoms of multiple EDs n = 12; undisclosed ED n = 7 | Online survey | Thematic analysis | Themes generated: (1) ED behaviors as an ‘auxiliary control mechanism’; (2) loss of auxiliary control after lockdown | 6.5 |
| Brown et al. (2021) | United Kingdom | 10 (90% women; 10% nonbinary) | 29.5 (5.0) | 100% White | Not reported | Not reported | OSFED n = 2; AN n = 6; BED n = 1; “other” n = 1 | Semi‐structured interviews | Thematic analysis | Themes generated: (1) social restrictions; (2) functional restrictions; and (3) restrictions in access to mental health services | 10 |
| Buckley et al. (2021) b | Multiple | 204 (86%) | 27.0 (8.1) | Not reported | Not reported | Not reported | 10.7% current ED diagnosis; 32.8% previous ED diagnosis (AN n = 29; BN n = 11; ON n = 9; BED n = 7; “other” n = 11) | Online survey | Content analysis | Content analysis highlighted worsened BI, worsened relationship with food, and additional COVID challenges; DE occurred predominantly in the form of binge eating, body preoccupation, fear of body composition changes, and inhibitory food control | 7.5 |
| Clark Bryan et al. (2020) | United Kingdom | 21 (86%) | 25.5 (5.6) | Not reported | Not reported | Not reported | AN | Semi‐structured interviews | Thematic analysis | Themes generated: (1) reduced access to ED services; (2) disruption to routine and activities in the community; (3) heightened psychological distress and ED symptoms; and (4) increased attempts at self‐management in recovery | 6 |
| Fernández‐Aranda, Casas, et al. (2020) Study 2 | Spain | 8 (not reported) | Not reported | Not reported | Not reported | Not reported | AN | Text‐based focus group | Thematic analysis | Themes generated: (1) connecting in isolation; (2) helping others versus helping oneself; (3) challenges of reduced professional support; (4) balancing the needs of the individual within the family | 3 |
| Frayn et al. (2021) | United States | 11 (64% women; 9% transmen) | 42.8 (14.2) | 81.8% White; 18.2% Black | Not reported | Household annual income (USD): 9.1% 0–10,000; 9.1% 25,001–30,000; 9.1% 30,001–35,000; 9.1% 45,001–50,000; 9.1% 70,001–75,000; 45.5% 100,000+ | BED n = 7; BN n = 2; OSFED n = 2 | Semi‐structured interviews | Thematic analysis | Themes generated: (1) variability in improvement or exacerbation of symptoms due to COVID; (2) changes in the physical environment were associated with symptom improvement; (3) social implications of COVID associated with both symptom improvement and deterioration; (4) greater overall stress/anxiety levels led to more binge episodes | 7.5 |
| Hunter and Gibson et al. (2021) | United States; Greece; United Kingdom | 12 (92%) | 31.8 (not reported) | Not reported | Not reported | Not reported | AN n = 10; AN and BN n = 1; BN n = 1 | Semi‐structured interviews | Thematic analysis | Themes generated: (1) loss of control; (2) support during confinement; (3) time of reflection on recovery | 8 |
| McCombie et al. (2020) | United Kingdom | 32 (94%) | 35.2 (10.3) | 100% White | Not reported | Not reported | AN n = 23; BN n = 3; BED n = 1; “other” n = 5 | Online survey | Thematic analysis | Themes generated: (1) mechanisms contributing to ED exacerbation; (2) positive aspects of lockdown | 7.5 |
| Nutley et al. (2021) | Multiple | 305 social media posts | Not reported | Not reported | Not reported | Not reported | Not reported | Subreddit posts (r/EatingDisorders, r/AnorexiaNervosa, r/BingeEatingDisorder | Thematic analysis | Themes generated: (1) change in ED symptoms; (2) change in exercise routine; (3) impact of quarantine on daily life; (4) emotional well‐being; (5) help‐seeking behavior; (6) associated risks and health outcomes | 7.5 |
| Quathamer and Joy (2021) | Canada | Survey: 70 (gender: 45% women; 22% agendered, nonbinary, genderfluid, or gender vague; 9% transgender); interview: 8 (gender: 50% ciswomen; 12.5% transwomen; 25% nonbinary) | Not reported | Survey: 81% White; 9% Indigenous; 6% Latinx; 3% Asian; 1% Middle Eastern; interview: 87.5% White; 12.5% South Asian | Survey: 27% gay; 23% bisexual; 17% lesbian; 12% queer; 6% pansexual; 3% 2‐spirit; 3% demisexual; 1% nonfixed; 1% questioning; interview: 12.5% gay; 25% lesbian; 25% bisexual; 12.5% queer; 12.5% asexual; 12.5% nonspecified | Not reported | n/a | Online survey and semi‐structured interviews | Foucauldian discourse analysis | Discursive considerations generated: (1) time for reflection; (2) time away from social surveillance; (3) time to work on oneself; and (4) time to (dis)connect; woven through these considerations were social discourses of hetero‐cis‐normativity, healthism, and resistance | 10 |
| Richardson et al. (2020) b | Canada | 56 chat transcripts | Not reported | Not reported | Not reported | Not reported | Not reported | Textual analysis of chat transcripts | Thematic analysis | Themes generated: (1) lack of access to treatment; (2) worsening of symptoms; (3) feeling out of control; (4) need for support | 8 |
| Simone et al. (2021) | United States | 510 (not reported) | 24.7 (2.0) | 29.6% White; 23.9% Asian; 16.5% Latino/Hispanic; 18.2% African American/Black; 11.8% mixed/“other” | Not reported | 32.7% low; 20.7% low‐middle; 17.0% middle; 18.5% upper‐middle; 11.2% high (parental socioeconomic status primarily based on baseline educational attainment) | n/a | Online survey | Thematic analysis | Themes generated: (1) mindless eating and snacking; (2) increased food consumption; (3) generalized decrease in appetite or dietary intake; (4) eating to cope; (5) pandemic‐related reductions in dietary intake; (6) re‐emergence or marked increase in ED symptoms | 8 |
| Stoddard (2021) b | United States | 17 (gender identity: 100% women) | Not reported | Not reported | Not reported | Not reported | Not reported | Semi‐structured interviews and autoethnography | Content analysis | Themes generated: (1) influencing factors for BI disturbance/EDs during COVID (stress and distress; social isolation; time; activity level changes; media; control; external situations; other mental health issues; weight change); (2) coping mechanisms; (3) hopes and fears | 9.5 |
| Tabler et al. (2021) b | United States | 43 (63% ciswomen; 2% transwomen; 7% nonbinary; 5% queer) | 27.7 (9.2) | 79% White; 7% biracial/multiracial; 12% Latinx/Hispanic; 2% Asian American | 19% lesbian; 16% gay; 35% bisexual; 7% queer; 12% pansexual; 5% asexual; 7% expansive sexuality/unlabeled | 44% working class; 44% middle class; 12% upper middle class (self‐report) | n/a | Semi‐structured interviews | Thematic analysis | Themes generated: (1) physical activity constraints; (2) eating patterns; (3) weight concerns | 7 |
| Vuillier et al. (2021) b | United Kingdom | 207 (63%) | 30.0 (9.7) | 93.7% White British/Irish/Scottish/European; 5.3% Asian; 0.5% Black; 0.5% Arab | Not reported | Not reported | AN n = 91; BN n = 46; BED n = 44; OSFED n = 26 | Online survey | Thematic Analysis | Themes generated regarding impact of COVID: (1) difficult emotions; (2) changes to routine; (3) confinement; (4) unhelpful social messages—making a transformation; (5) emotional support from others; (6) emotion coping skills; (7) accessibility—barriers and facilitators; (8) loss of support | 7 |
| Zeiler et al. (2021) | Austria | 13 (100%) | 15.9 (1.4) | Not reported | Not reported | Not reported | AN‐R n = 9; AN‐BP n = 4 | Semi‐structured interviews | Thematic analysis | Themes generated: (1) restrictions of personal freedom; (2) interruption of treatment routine; (3) changes in psychopathology; (4) opportunities of COVID period | 7.5 |
Note: Study quality was assessed using an adapted version of the critical appraisal skills program (CASP) tool (Long et al., 2020).
Abbreviations: AAN, atypical anorexia; AN, anorexia nervosa; AN‐BP, binging/purging anorexia subtype; AN‐R, restrictive anorexia subtype; ARFID, avoidant restrictive food intake disorder; BED, binge eating disorder; BI, body image; BN, bulimia nervosa; DE, disordered eating; ED, eating disorder; OSFED, other specified feeding or eating disorder; UFED, unspecified feeding or eating disorder.
The majority of included studies did not specify whether they assessed sex assigned at birth, gender, or gender identity; where this information is available, sex assigned at birth, gender, and gender identity are reported separately.
Signifies a multimethods paper. Information detailed here concerns the qualitative methods, analysis, and findings. See Table 1 for the quantitative characteristics of this study.
2.5. Synthesis of results
Due to the inclusion of mixed‐methods studies and the heterogeneity of existing evidence, we adopted a narrative synthesis approach informed by the guidance by Popay et al. (2006): (1) developing a theory; (2) developing a preliminary synthesis; (3) exploring relationships in the data; and (4) assessing robustness of the synthesis.
2.5.1. Stage 1: Development of theory
This stage was performed early on in the review process and helped shape the review aims. Through an initial review of the literature and discussion among the research team, we identified several possible mechanisms whereby the COVID‐19 pandemic and related factors may influence BI, DE, and EDs, such as psychological distress due to the ongoing pandemic, disruption of access to support and treatment, food shortage and insecurity, and increased loneliness and social isolation. Key findings from the literature review are outlined in the introduction section of this manuscript. This process also highlighted a lack of studies focusing on individuals from marginalized and underrepresented populations, which we included as a key aim of our review.
2.5.2. Stage 2: Development of the preliminary synthesis
The second stage involved organizing and describing the included papers to explore patterns across studies. We followed Stern et al.'s (2020) guidance on conducting mixed‐studies systematic reviews, as outlined in the Joanna Briggs Institute (JBI) manual for evidence synthesis. Accordingly, we conducted the current review using the convergent integrated approach (Hong et al., 2017), whereby findings from the qualitative, quantitative, and mixed‐methods studies were integrated in the narrative synthesis. Quantitative data were transformed (or qualitized) into “textual descriptions” and presented in conjunction with qualitative data. This approach is recommended over its counterpart where qualitative data are assigned numerical values (quantitized), as codifying quantitative data is less error‐prone than attributing numerical values to qualitative data. One of the distinguishing features of mixed‐studies systematic reviews is the inclusion of primary mixed‐methods studies, from which data are extracted so they can be classified as quantitative or qualitative (Stern et al., 2020). Therefore, quantitative data from mixed‐methods studies were also transformed and synthesized with quantitative data from quantitative studies and nontransformed qualitative data from qualitative and mixed‐methods studies. Due to the variability in the emerging literature and the need to comprehensively capture all relevant findings, the themes and resulting narrative synthesis were based on a comprehensive examination of all included papers, regardless of study quality.
2.5.3. Stage 3: Exploring the relationships within and between studies
In this stage, four main themes (and two subthemes) were generated from the integrated qualitative and transformed quantitative data to answer the key research aims. The themes were generated using deductive, or theory‐driven approaches (i.e., considering data relevant to answering the review questions) and inductive, or data‐driven approaches (i.e., being open to the data that are present across studies and unexpected findings; Clarke & Braun, 2014). All themes were informed by both qualitative and quantitative research. For clarity, a selection of references is provided in the narrative synthesis; please see Tables 1 and 2 for a detailed breakdown of study findings and associated citations. Illustrative quotes for each theme are presented in Table 3.
TABLE 3.
Participant quotes
| Theme | Quote | Author | |
|---|---|---|---|
| 1. Disruptions due to COVID‐19 | “Feeling frustrated because I've been learning how to control the bulimic symptoms and normally able to manage them. Yet the change in routine (or lack of) and general stress/anxiety is unsettling it and I noticed my thoughts and behaviors changing” (participant details not provided) | Branley‐Bell and Talbot (2020) | |
| “Without structure and focus (and meaning) of uni [university] and friends and having a life that feels worth living, now it's just old habits and misery” (participant details not provided) | McCombie et al. (2020) | ||
| “My routine has gotten lost, which tampers with my sleep, which in turn tampers with my ability to follow my meal plan” (30, female participant, anorexia nervosa) | Hunter and Gibson (2021) | ||
| “For me, it was like, I go to my therapist, I leave my problems there, I go home. […] Now, many things take place in my room, and I have all these problems, these conversations right on the spot. This felt strange for me at the beginning” (participant details not provided) |
Zeiler et al. (2021) |
||
| 2. Variability in the improvement or exacerbation of symptoms | 2.1 Negative outcomes of the COVID‐19 pandemic | “I have been in recovery from AN [anorexia nervosa] and BN [bulimia nervosa] for about 2 years now, and ever since this whole isolation thing started, my symptoms have come back, and worsened almost immediately” (participant details not provided) | Richardson et al. (2020) |
| “The pandemic has increased my self‐harm, as I've felt so restricted by the government in terms of what I can do to deal with my feelings (i.e., initially – only exercise once a day, not able to exercise with anyone else). Using healthy means to deal with difficult feelings (i.e., go for a walk, meet a friend for coffee) have been more limited and so it is really easy to go back to unhelpful ways of coping such as self‐harm” (female participant, anorexia nervosa) | Vuillier et al. (2021) | ||
| “My ED feels more valuable to me than ever. It is the only constant in what feels like a completely upside down and scary world, it is my only locus of control” (participant details not provided) | Branley‐Bell and Talbot (2021) | ||
| “With the recent quarantine, I am unable to work out the same… just running and doing as much as I can. I've found my body changing in ways I am very uncomfortable with. I'm waking up daily weighing myself, logging my food, and checking my Fitbit constantly. I recently started staring in the mirror more and despising the person who looks back” (participant details not provided) | Nutley et al. (2021) | ||
| “Times when I would normally kind of be doing something potentially social or something like that over the weekend… Obviously with more free time, I might have gone back to see my parents–that […] feeling, of like, existential loneliness felt incredibly desperate and really quite painful. But it was… It came in bursts to begin with, and I think as lockdown has gone on, it's that feeling of real painful loneliness” (25, female participant, White, anorexia nervosa) | Brown et al. (2021) | ||
| “Everything is dramatically worse because of being home all the time. I have constant access to all of my food and my scale and everything to evaluate where I'm at and to facilitate eating” (participant details not provided) | Frayn et al. (2021) | ||
| “I definitely walk past the mirror more often and do some body checking” (participant details not provided) | McCombie et al. (2020) | ||
| “In the initial stages of the pandemic it seemed pointless to try to manage my ED [eating disorder]. The stress and anxiety regarding the future meant that I did not see the point in investing energy in my own physical or mental health” (female participant, binge eating disorder) | Vuillier et al. (2021) | ||
| “It's sort of paradoxical because on one hand, I was really anxious realizing it was going to stall my progress but then on the other, I was really anxious that it would stall my disordered behaviors, so it's been quite complex” (27, female participant, anorexia nervosa) | Hunter and Gibson (2021) | ||
| “COVID‐19 has affected my general mental health quite a lot through isolation and anxiety. I think this is having as much of an effect on my fitness and relationship with my body as anything else” (participant details not provided) | Buckley et al. (2021) | ||
| 2.2 Positive outcomes of the COVID‐19 pandemic | “Binging […] and purging has reduced. I was doing this five times a day. Now people are home with me my binge purge has reduced to every other day” (participant details not provided) | Branley‐Bell and Talbot (2020) | |
| “Your immune system is really weakened because of an ED [eating disorder] and for me, I do not want that anymore so I'm feeling really motivated to kind of improve my physical health as much as possible” (participant details not provided) | Clark Bryan et al. (2020) | ||
| “But I very quickly was able to turn it around and make it an opportunity for healing and like, I've dedicated so much time to eating disorder recovery during quarantine that I felt like that's what it was for. […] And so, I literally like am living in this renaissance of intuitive eating and of like, anti‐diet‐culture activism, because I found so much space for it during quarantine” (female participant) | Stoddard et al. (2021) | ||
| “Having the space to do that [reflect on recovery] is really good but I definitely did think that I was further along in my recovery than I am, but I guess that is a good thing because it means yeah I guess it is a good thing because it means I am aware of it as well which is helpful” (29, female participant, anorexia nervosa) | Hunter and Gibson (2021) | ||
| 3. Factors associated with body image and disordered eating outcomes | “I'm furloughed so have had the mental space to acknowledge that I do actually have a problem. I have started recognizing my own ED [eating disorder] thought patterns and behaviors and am working on challenging them” (participant details not provided) | McCombie et al. (2020) | |
| “My symptoms have probably gotten better because I am home and cannot go anywhere. Before my binge episodes were on the road and I was by myself. The fact that I am physically constrained and do not have access to what I had before helps. I do not go out much, not by myself. I am with my kids and family, so I do not have privacy and am very conscious of that” (participant details not provided) | Frayn et al. (2021) | ||
| “I am also a lot more honest with my family and friends about the struggles I face so I have constant support from them when I need it” (female participant, anorexia nervosa) | Vuillier et al. (2021) | ||
| “[Messages were] about not ‘letting oneself go’ or how terrible it would be to gain weight in quarantine, or how people were supposed to work hard to somehow come out of this ‘better than ever’, and boy, did the ED [eating disorder] voice in me love that” (White, bisexual, genderfluid participant) | Quathamer and Joy (2021) | ||
| “COVID‐19 has brought back many of the habits I had when I was struggling with my ED [eating disorder]. The spread of the jokes about the ‘corona 15′ were what sparked a lot of the unhealthy habits resurfacing” (22, female participant, White) | Simone et al. (2021) | ||
| “My mom had always joked about my body/weight (since I used to be overweight, she would joke about me not being able to fit through my door). She does not mean any harm, but I get really devastated when she mentioned that I've gained weight during quarantine. I started to restrict even more” (participant details not provided) | Nutley et al. (2021) | ||
| “I'm trapped at home with people who do not know I have anorexia. I am hiding and lying constantly” (participant details not provided) | Branley‐Bell and Talbot (2020) | ||
| It has meant that I have no one around to keep an eye on me so I can binge when I want to and then make myself sick to make myself feel better and I do not have to explain it to anyone because there is no one there to hear me” (male participant, bulimia nervosa) | Vuillier et al. (2021) | ||
| “It's a very secretive disorder and if I'm face to face with someone [for treatment] I cannot lie, I cannot hide the fact that I've lost weight or hide the fact that I'm drained energy‐wise, whereas on the phone I can cover up” (29, female participant, anorexia nervosa) | Hunter and Gibson (2021) | ||
| 4. Unique challenges for marginalized and underrepresented groups | “I was always concerned about how I look externally but ever since the pandemic the focus has been so much more because the way I justify it is I have more time to work on my body” (South Asian, gay, cisgender man) | Quathamer and Joy (2021) | |
| “I found myself snacking more than usual. Some days I would overeat, other days I would barely eat anything. The major concern has always been my weight. So that's something I'm looking forward to, like getting back on track with the whole, exercising, and trying not to snack as much as before” (Latina, pansexual, cisgender woman) | Tabler et al. (2021) | ||
| “I relished the opportunity to be comfortable at home so much and to not have to feel like I was presenting my body and gender in a socially acceptable way. I loved eating things that gave me pleasure without fear of outside judgment and connecting with my body through exercise in a slow and easy way” (White, bisexual, genderfluid participant) | Quathamer and Joy (2021) | ||
| “The pandemic made me stay with my unaccepting parents who do not respect my identity and limited my presentation to ways that made me feel very dysphoric and negative about my body” (White, lesbian, transgender woman) | Quathamer and Joy (2021) | ||
2.5.4. Stage 4: Evaluating the robustness of the synthesis
In the final stage, the methodological quality of the included studies and of the review process was examined to assess the strength of the evidence presented within the review. We provide considerations and implications of the review's findings in the discussion section of this manuscript.
2.6. Quality assessment
Due to the novelty of COVID‐19 and the need to gain a comprehensive understanding of its impact on BI and DE, no studies were excluded as a result of the quality assessments. Rather, quality scores of the included studies are provided in Tables 1 and 2 and considered in the results and discussion sections of this manuscript.
2.6.1. Quantitative studies
Quality of quantitative studies was assessed using the Quality Assessment Tool for Quantitative Studies, developed by the Effective Public Health Practice Project (EPHPP; Thomas et al., 2004). The EPHPP provides an overall methodological quality rating of “strong” (no weak component ratings), “moderate” (one weak component rating), or “weak” (two or more weak component ratings). The ratings are based on the following components: selection bias, study design, confounders, blinding, data collection method, and withdrawals and dropouts. The EPHPP is suitable for evaluating the methodological quality of various study designs (Jackson & Waters, 2005). In addition, the EPHPP has excellent interrater reliability for overall scores when compared to the Cochrane Collaboration Risk of Bias Tool (Armijo‐Olivo et al., 2012) and established construct and content validity (Jackson & Waters, 2005). Two authors (B.G. and D.T.) independently assessed all studies. Cohen's kappa (Cohen, 1960) was calculated to determine interrater reliability, showing good agreement (92%) between total scores (κ = 0.866, p < .001). Discrepancies were resolved by a third author (J.S.), who rated all papers in line with either BG or DT, and the majority score was assigned.
2.6.2. Qualitative studies
Quality of qualitative studies was assessed using a modified version of the 10‐item Critical Appraisal Skills Program (CASP) qualitative checklist, as detailed by Long et al. (2020). The CASP checklist is the most commonly used checklist‐based tool for quality appraisal in health‐related qualitative evidence syntheses, and is endorsed by the Cochrane Qualitative and Implementation Methods Group (Long et al., 2020). Each of the 10 items focus on a different methodological aspect of a qualitative study. To improve the tool's sensitivity to theoretical validity, the following question was added by Long et al. (2020): “Are the study's theoretical underpinnings (e.g., ontological and epistemological assumptions; guiding theoretical framework(s)) clear, consistent and conceptually coherent?” The CASP checklist questions were scored independently as “yes” (1), “no” (0), “somewhat” (0.5), or “cannot tell” (0) by two authors (N.C. and G.P.), and assigned a total score (out of 10). Cohen's κ was calculated to determine interrater reliability, showing moderate agreement (76%) between total scores (κ = 0.712, p < .001). Four studies with differences of one point were independently scored by a third author (A.T.), who rated all in line with either GP or NC, and the majority score was assigned.
3. RESULTS
3.1. Paper selection
As of August 1, 2021, the search protocol yielded 3230 papers (see Figure 1). After removing duplicates (n = 93) and incomplete or nonrelevant records (n = 192), 2945 papers were screened based on title and abstract. Of these, 2790 were excluded and 155 were sought for retrieval, of which one report could not be retrieved. In total, 154 articles were assessed for eligibility. Thirteen papers were excluded because they did not describe an empirical study, 31 studies were excluded because they did not assess target outcomes, and 36 studies were excluded because they did not assess the influence of COVID‐19 on target outcomes.
FIGURE 1.
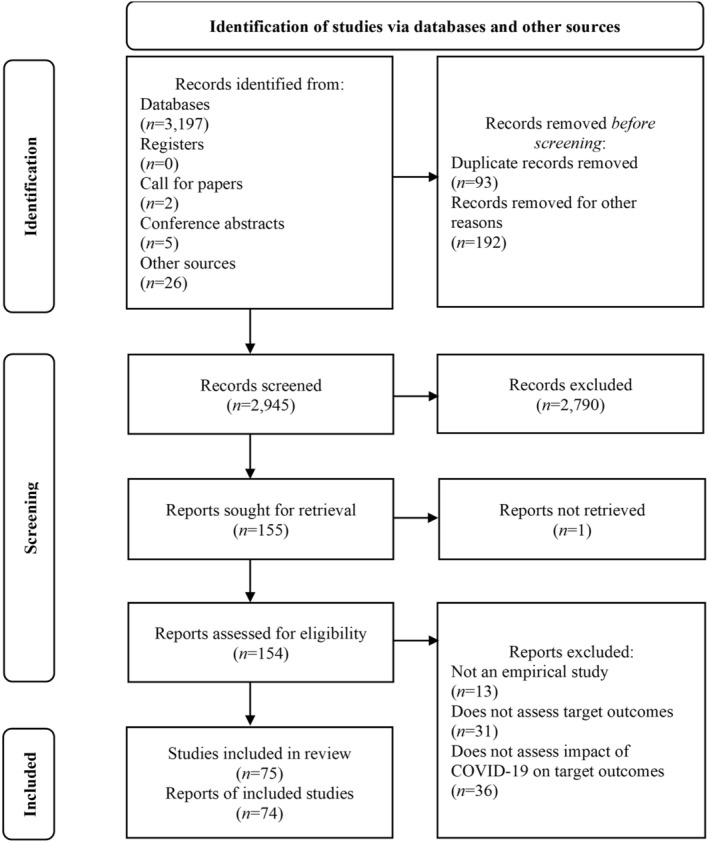
PRISMA flowchart of study selection
3.2. Study characteristics
A final sample of 74 reports, describing 75 studies (quantitative n = 58, mixed‐methods n = 7, qualitative n = 10), was included in this review. Characteristics of quantitative studies (including quantitative data from mixed‐methods studies) are described in Table 1 and characteristics of qualitative studies (including qualitative data from mixed‐methods studies) are described in Table 2. Of the 65 studies that reported quantitative findings, 46 were cross‐sectional (of which 13 were retrospective), 16 were longitudinal, and 3 were cohort studies. Of the 17 studies that reported qualitative findings, six used online surveys for data collection, six used semi‐structured interviews, one used focus groups, one used a combination of semi‐structured interviews and autoethnography, one used a combination of online surveys and semi‐structured interviews, one used textual analysis of chat transcripts, and one analyzed individual posts from the social media platform Reddit. The majority of qualitative studies analyzed the data using thematic analysis (n = 14), two used content analysis, and one used Foucauldian discourse analysis. The studies were conducted in more than 20 countries, predominantly in Europe and North America, including the United States (n = 23), the United Kingdom (n = 12), Spain (n = 7), Italy (n = 6); Germany (n = 4), Portugal (n = 4), Australia (n = 3), Canada (n = 3), France (n = 2), Lebanon (n = 2), Turkey (n = 2), Austria (n = 1), Belgium (n = 1), Greece (n = 1), Hong Kong (n = 1), Ireland (n = 1), Lithuania (n = 1), Netherlands (n = 1), Poland (n = 1), and multiple countries (n = 2). Participants were mostly adults, with nine studies being conducted with children and/or adolescents.
3.3. Study quality
Of the studies evaluated using the EPHPP, 28 were rated as “weak,” 32 were rated as “moderate,” and 5 were rated as “strong.” Most studies lacked quality in study design (e.g., bias due to allocation process) and selection bias (e.g., how representative the sample is of the target population). Of the studies assessed using the CASP, 1 was rated as “weak,” 10 were rated as “moderate,” and 6 were rated as “strong.” Most studies lacked information regarding theoretical underpinnings, including ontological and epistemological approaches, as well as sufficient consideration of the researcher–participant relationship and ethical issues.
3.4. Theme 1: Disruptions due to the COVID‐19 pandemic
Participants with BI and eating concerns reported both social and functional restrictions resulting from the COVID‐19 pandemic. Social restrictions included social isolation and confinement (e.g., Brown et al., 2021), increased responsibility for self and others (e.g., Brown et al., 2021), and loss of, or reduced access to, usual support networks (e.g., Vuillier et al., 2021). Functional restrictions included a lack of routine and structure or disruption to previous living routine (e.g., Clark Bryan et al., 2020; McCombie et al., 2020), changes or constraints to physical activity or exercise routine (e.g., Branley‐Bell & Talbot, 2020), and restrictions to personal freedom (e.g., Zeiler et al., 2021). Alongside restrictions to social support, individuals with EDs specifically reported that the COVID‐19 pandemic had caused reduced access or interruption to professional support and treatment, including ED services, general healthcare, and mental health services (e.g., Fernández‐Aranda, Casas, et al., 2020; Fernández‐Aranda, Munguía, et al., 2020). Moreover, some participants with EDs increased their reliance on family and friends in response to a lack of access to professional support and perceived risks of replacement telehealth approaches (e.g., Hunter & Gibson, 2021).
3.5. Theme 2: Variability in the improvement or exacerbation of symptoms
Findings were mixed regarding the impact of COVID‐19 on BI, DE behaviors, and EDs. Studies reported inconsistent rates of symptom deterioration and improvement during COVID‐19. For example, studies found that between 33% and 70% of participants reported worse BI during COVID‐19, 10%–26% reported improved BI, and 4%–51% reported no change in BI as a result of the pandemic. In terms of EDs, 16%–87% of participants reported worsened ED symptoms or reactivation of ED symptoms during COVID‐19, 2%–51% reported improved ED symptoms, and 8%–66% reported no change in ED symptoms as compared to prepandemic levels. In addition, there was great variation in which symptoms were most affected by the COVID‐19 pandemic, with some studies showing no differences in target outcomes from pre‐ to postlockdown (e.g., Koenig et al., 2021; Martínez‐de‐Quel et al., 2021). As such, two subthemes were generated: (1) negative outcomes of the COVID‐19 pandemic and (2) positive outcomes of the COVID‐19 pandemic. Of note, multiple participants reported experiencing both positive and negative outcomes simultaneously; however, for simplicity, negative and positive outcomes are presented separately.
3.5.1. Negative outcomes of the COVID‐19 pandemic
Overall, most studies reported some negative outcomes of the COVID‐19 pandemic for individuals living with EDs and the general population. Multiple studies reported deterioration in participants' BI outcomes, such as body esteem, body dissatisfaction, weight and shape concerns, and drive for thinness (e.g., Conceição et al., 2021; Keel et al., 2020; Larkin, 2021; Nutley et al., 2021; White, 2021), as well as DE behaviors, such as dietary restriction, emotional eating, binging and purging, and compulsive exercise (e.g., Giel et al., 2021; Phelan et al., 2021; Philippe et al., 2021; Zhou & Wade, 2021). Moreover, studies showed a higher prevalence of EDs during the pandemic compared to previous years (e.g., Lin et al., 2021; Spettigue et al., 2021; Taquet et al., 2021). Patients with EDs reported reduced psychological well‐being (e.g., H. Kim, Rackoff, et al., 2021; Leenaerts et al., 2021); feeling out of control (e.g., Branley‐Bell & Talbot, 2021; Richardson et al., 2020); increased suicide ideation, suicidal thoughts, and self‐harm (e.g., Monteleone et al., 2021); higher levels of loneliness (e.g., S. Kim, Wang, et al., 2021; Schlegl, Maier, et al., 2020); increased posttraumatic stress (e.g., Nisticò et al., 2021); and changes in ED‐specific and general psychopathology (e.g., Castellini et al., 2020; Simone et al., 2021; Trott et al., 2021; Vitagliano et al., 2021).
3.5.2. Positive outcomes of the COVID‐19 pandemic
Positive outcomes of the pandemic relating to BI, DE, and ED experiences included making time for self‐care (e.g., McCombie et al., 2020; Termorshuizen et al., 2020); having space away from in‐person appearance comparisons and reduced weight monitoring (e.g., Graell et al., 2020; Quathamer & Joy, 2021); and connecting virtually with friends, family, and the community (e.g., Termorshuizen et al., 2020; Zeiler et al., 2021). Patients with EDs specifically reported a reduction in ED symptomatology (e.g., Schlegl, Maier, et al., 2020); increased attempts at self‐management in recovery (e.g., Schlegl, Maier, et al., 2020); greater motivation to recover (e.g., Clark Bryan et al., 2020; Termorshuizen et al., 2020); and more time for reflection on recovery (e.g., Hunter & Gibson, 2021).
3.6. Theme 3: Factors associated with BI and DE outcomes
As described above, social implications of the COVID‐19 pandemic and changes in participants' physical environment were associated with both symptom deterioration and improvement. As such, several associated factors were identified to explain these discrepancies. Factors that were associated with worse BI and eating outcomes during the pandemic included psychological, individual, social, and ED‐related characteristics. Psychological variables associated with worse outcomes included higher levels of worry, rumination, loneliness, anxiety, depression, stress, psychological distress, and fear of COVID‐19 (e.g., Akgül et al., 2021; Chan & Chiu, 2021; Frayn et al., 2021; Swami, Horne, et al., 2021); comorbidity of mental health concerns and childhood trauma (e.g., Castellini et al., 2020; Chan & Chiu, 2021); insecure attachment, lower self‐directedness, and poor coping strategies (e.g., Baenas et al., 2020; Haddad et al., 2020); poor emotion regulation (e.g., Félix et al., 2021; Flaudias et al., 2020; Machado et al., 2020); higher levels of uncertainty intolerance (e.g., Scharmer et al., 2020); and greater food insecurity (e.g., Christensen, Forbush, et al., 2021).
Individual variables associated with worse outcomes included identifying as a woman (e.g., Baceviciene & Jankauskiene, 2021; Buckley et al., 2021; Serin & Koç, 2020); increased time spent online or on social media (e.g., Bellapigna et al., 2021; Vall‐Roqué et al., 2021); identifying as an ethnic minority participant (e.g., Christensen, Forbush, et al., 2021; S. Kim, Wang, et al., 2021); pre‐COVID‐19 experiences of weight stigma (e.g., Puhl et al., 2020); and higher body mass index or body weight, or reporting changes in weight during COVID‐19 (e.g., Lessard & Puhl, 2021; Stoddard, 2021). Findings were inconclusive regarding the effect of age, with some studies showing younger age to be a risk factor and older age to be a protective factor (e.g., Pikoos et al., 2020; Ramalho et al., 2021), one study showing that adolescents reported higher reactivation of ED symptoms than children (Graell et al., 2020), and one study showing no influence of age on target outcomes (Monteleone, Marciello, et al., 2021). Contrary to expectations, increased videoconferencing as a result of confinement did not predict BI or binge eating postlockdown (Gullo & Walker, 2021; Pfund et al., 2020).
Social variables associated with worse outcomes included household arguments or family conflicts (e.g., Baenas et al., 2020; Castellini et al., 2020); change in living situation and access to usual support networks (e.g., Branley‐Bell & Talbot, 2020; Monteleone, Cascino, Marciello, et al., 2021); fear for the safety of loved ones (e.g., Castellini et al., 2020); longer social isolation and confinement (e.g., Coulthard et al., 2021; Haddad et al., 2021); perceived low quality of personal and therapeutic relationships (e.g., Cecchetto et al., 2021; Monteleone, Cascino, Marciello, et al., 2021); and exposure to COVID‐19‐related media and triggering messages regarding quarantine weight gain and exercise (e.g., Nutley et al., 2021; Vuillier et al., 2021). Evidence was mixed regarding participants' living situation, with some studies showing that living alone or living with fewer people was associated with less favorable outcomes (Félix et al., 2021; Pikoos et al., 2020), and other studies showing the detrimental effects of living with a higher number of adults in confinement (Haddad et al., 2020; Zeiler et al., 2021).
Finally, ED‐related variables associated with worse outcomes included a prior or current ED diagnosis (e.g., Breiner et al., 2021; Meda et al., 2021; Phillipou et al., 2020; Robertson et al., 2021) and higher levels of BI and/or eating concerns at baseline (e.g., Jordan et al., 2021; Pfund et al., 2020). Results were inconclusive regarding ED subtype. Two studies found that patients with anorexia nervosa (AN; Baenas et al., 2020; Monteleone, Marciello, et al., 2021) and other specified feeding or eating disorders (OSFED; Baenas et al., 2020) were more likely to report symptom deterioration and worse mental health outcomes during confinement. In addition, patients with AN reported the greatest dissatisfaction and accommodation difficulty with remote therapy (Fernández‐Aranda, Munguía, et al., 2020). However, another study found that patients with BN reported more severe COVID‐19‐related posttraumatic symptomatology than patients with AN and healthy controls (Castellini et al., 2020). Similarly, patients with AN reported a positive response to treatment during confinement, while no changes were found in patients with BN, and patients with OSFED reported an increase in eating symptomatology and psychopathology (Fernández‐Aranda, Munguía, et al., 2020). In terms of prevalence, one study found that increased diagnostic incidence of EDs in 2020 was primarily related to AN (Taquet et al., 2021), while another study showed increased prevalence of BN and BED during the pandemic, with no differences found in prevalence of AN from pre‐ to during COVID‐19 (H. Kim, Rackoff, et al., 2021). However, it should be noted that Taquet et al.'s study included health records of more than 5 million people to compare ED incidence risk in 2020 with previous years, while H. Kim, Rackoff, et al. (2021) longitudinally examined change in frequencies of psychological health conditions in a sample of 4970 participants from pre‐ to during COVID‐19, making comparison between studies difficult. Finally, several studies showed no effect of ED diagnosis on target outcomes (e.g., Monteleone, Cascino, Marciello, et al., 2021; Vuillier et al., 2021).
Multiple factors were also identified that were associated with more positive and less negative BI and eating outcomes during the pandemic, including personal characteristics, such as adaptive coping mechanisms (e.g., Baenas et al., 2020), self‐compassion (e.g., Swami, Todd, et al., 2021), emotion regulation (e.g., reappraisal; Giel et al., 2021), sense of coherence (e.g., Giel et al., 2021), and higher perceived control (e.g., Branley‐Bell & Talbot, 2020); social characteristics, such as emotional and social support from others (e.g., Tabler et al., 2021), virtual social contact with friends and family (e.g., Schlegl, Meule, et al., 2020), and more time spent with family and improved family relationships (e.g., Vuillier et al., 2021); and individual behaviors, such as mild physical activity (e.g., Schlegl, Meule, et al., 2020), taking part in enjoyable activities (e.g., Schlegl, Maier, et al., 2020; Schlegl, Meule, et al., 2020), maintaining daily routines (e.g., Schlegl, Maier, et al., 2020), and day planning (e.g., Schlegl, Maier, et al., 2020).
Notably, findings were inconsistent regarding the influence of physical activity on BI and eating outcomes. Some studies have suggested that change in an individuals' physical activity routine as a result of restrictions may be associated with worse outcomes, regardless of their current level of physical activity. For example, Martínez‐de‐Quel et al. (2021) found that the lockdown period due to COVID‐19 negatively influenced physical activity levels, sleep quality, and well‐being in participants who had a physically active lifestyle before the COVID‐19 pandemic, but not in participants who were classed as physically inactive prepandemic. However, they did not assess the relationship between changes in physical activity levels and ED risk. Two studies found that change in physical activity was associated with worsened ED symptoms (Branley‐Bell & Talbot, 2020; Vuillier et al., 2021). Specifically, for some people, reduced physical activity as a result of restrictions was associated with increased ED cognitions or compensatory disordered behaviors (e.g., food restriction), while others engaged in more excessive exercise at home to cope with the loss of their usual physical activity routine. Indeed, several studies found that physical activity was positively associated with adverse outcomes in participants with EDs and in the general population, such as dietary restraint, eating concerns, shape and weight concerns, and eating symptomatology (Haddad et al., 2020; Monteleone, Marciello, et al., 2021).
3.7. Theme 4: Unique challenges for marginalized and underrepresented groups
In line with the aim to highlight the impact of the COVID‐19 pandemic on BI and DE outcomes in marginalized and underrepresented populations, the final theme relates to findings from studies that have included such participant samples. Specifically, we considered the influences of sexuality, gender identity, belonging to a racialized group, and ethnicity. As the majority of studies were conducted in Europe or North America, we were not able to explore differences in the effect of COVID‐19 on target outcomes in countries that are typically less represented in psychological research (i.e., non‐WEIRD countries).
Among studies that reported race or ethnicity data (n = 32; 43%), a majority of participants were White, with few studies comparing outcomes between participants who identified with different ethnicities or racialized groups. S. Kim, Wang, et al. (2021) found that identifying as Black was associated with lower psychological distress, stress, and loneliness, while identifying as Asian was associated with higher psychological distress, stress, and loneliness in participants with confirmed or suspected EDs. Moreover, Christensen, Forbush, et al. (2021) found that participants who identified as Black were significantly more likely to report individual food insecurity relative to other racialized groups, but found no differences in food insecurity from before to during the beginning of the COVID‐19 pandemic. Overall, participants who identified as BIPOC reported similar BI and eating concerns as outlined in previous themes.
Only nine studies (12%) reported participants' sexual orientation and 19 studies (25%) included participants with nonbinary or transgender identities. Of note, the majority of the included studies did not specify whether they assessed sex assigned at birth, gender, or gender identity, and many used “sex” and “gender” interchangeably. In addition, most studies included predominantly cisgender and heterosexual participants, apart from Quathamer and Joy (2021), who specifically explored the impact of the COVID‐19 pandemic on BI among LGBTQ+ individuals in Canada, and Tabler et al. (2021), who investigated the impact of COVID‐19 on self‐reported ED symptoms and perceived weight gain among LGBTQ+ adults in the United States. None of the studies included in this review directly investigated the unique experiences of BI, DE, or EDs during COVID‐19 among individuals who identified as nonbinary or transgender. Of the 19 studies that reported the inclusion of nonbinary and transgender participants, only four studies conducted analyses based on gender, of which two excluded these participants due to small group size (<6%), instead focusing on differences in target outcomes within the male–female gender binary. In addition, one study grouped all participants who identified as LGBTQ+ in their analyses. Indeed, even in studies that specifically targeted LGBTQ+ samples (Quathamer & Joy, 2021; Tabler et al., 2021), the majority of participants identified as cisgender. As such, findings across all participants who identified as LGBTQ+ are presented together in this review, while we acknowledge the possible differences in experiences across various identities.
Overall, findings indicate that pandemic‐related stress was associated with ED symptoms and perceived weight gain, and this association was stronger in women and individuals who identified as LGBTQ+ compared to cisgender and heterosexual men (Tabler et al., 2021). Although findings regarding the impact of the COVID‐19 pandemic on BI and eating outcomes generally mirrored those discussed above, individuals who identified as LGBTQ+ discussed challenges of COVID‐19 through a lens of gender identity and sexuality. For example, some participants reported unique challenges directly related to restrictions imposed as a result of the COVID‐19 pandemic, such as being confined with family members who were not aware of, or did not approve of, their gender identity or sexuality (Quathamer & Joy, 2021). In addition, participants reported gender dysphoria‐related body issues due to the fear of gaining weight during quarantine (Quathamer & Joy, 2021). On the other hand, several participants reported that the restrictions associated with the pandemic gave them a break from the pressure to present their body and gender in a socially acceptable way (Quathamer & Joy, 2021). Some participants further reported that the removal of distractions and a break from engaging with a heteronormative society allowed them to be present more fully in their body and explore their gender identity in greater depth (Quathamer & Joy, 2021). Of note, several studies reported no effect of gender (e.g., H. Kim, Rackoff, et al., 2021; Puhl et al., 2020), ethnicity/racialized group belonging (e.g., Coulthard et al., 2021; Czepczor‐Bernat et al., 2021; H. Kim, Rackoff, et al., 2021), or sexual orientation (e.g., Czepczor‐Bernat et al., 2021; H. Kim, Rackoff, et al., 2021) on BI or eating outcomes during COVID‐19.
4. DISCUSSION
The current review is the first to investigate the influence of the COVID‐19 pandemic and related restrictions on BI, DE behaviors, and ED outcomes. The findings of this review complement and extend findings from previous reviews conducted on the impact of COVID‐19 on EDs (Miniati et al., 2021; Monteleone, Cascino, Barone, et al., 2021; Sideli et al., 2021). First, previous reviews evaluate earlier research on COVID‐19 (spanning the time period from January 2020 to January 2021). Our review extends this time period until August 2021, which includes the easing of restrictions in many countries. Second, previous reviews have included between 21 and 26 papers, most of which were quantitative, and have predominantly focused on ED outcomes. We include 75 studies (including 16 longitudinal studies and 17 studies that report qualitative findings) and adopt a mixed‐studies approach to explore both quantitative and qualitative outcomes. Moreover, the current review contributes novel findings on the impact of COVID‐19 on BI and DE behaviors in the general population. As such, we also extend existing recommendations beyond clinical practice and treatment (see Table 4). Four themes were generated across qualitative, quantitative, and mixed‐methods studies, including: (1) disruptions due to the COVID‐19 pandemic; (2) variability in the improvement or exacerbation of symptoms; (3) factors associated with BI and DE outcomes; and (4) unique challenges for marginalized and underrepresented groups.
TABLE 4.
Recommendations for individuals, researchers, clinicians, and public health messaging
| Important findings | Recommendations for individuals | Recommendations for researchers | Recommendations for clinicians | Recommendations for public health messaging |
|---|---|---|---|---|
Weight stigma/stigmatizing messaging:
|
|
|
|
|
Disruptions/changes to treatment:
|
|
|
|
|
| Lack of access to personal/professional support: |
|
|
|
|
Physical activity/daily routines:
|
|
|
|
|
Impact on marginalized groups:
|
|
|
|
4.1. The influence of COVID‐19 on BI and DE outcomes
Overall, qualitative and quantitative data complemented each other and showed a negative influence of the COVID‐19 pandemic on BI and DE. Specifically, with respect to BI, studies showed increased shape and weight concerns (Schlegl, Maier, et al., 2020), drive for thinness/muscularity (Swami, Horne, et al., 2021), body and appearance dissatisfaction (Vall‐Roqué et al., 2021), and decreased self‐esteem (White, 2021). Worsened DE behaviors included binge eating (Zhou & Wade, 2021), dietary restriction (Termorshuizen et al., 2020), and compulsive exercise (Scharmer et al., 2020). Furthermore, specific and general symptomatology as well as mental health outcomes worsened in individuals living with EDs, including increases in stress (Fernández‐Aranda, Casas, et al., 2020), anxiety (Richardson et al., 2020), and depression (H. Kim, Rackoff, et al., 2021). The majority of participants also reported perceived disruptions of the pandemic to their daily routine (Nutley et al., 2021), social support networks (Vuillier et al., 2021), and access to treatment and professional support (Hunter & Gibson, 2021).
Conversely, many studies also reported positive outcomes of the COVID‐19 pandemic, including reduction in ED symptomatology, more time to reflect on recovery and engage in self‐care, greater motivation to recover, and more time to connect with family in person or online (e.g., McCombie et al., 2020; Schlegl, Maier, et al., 2020; Termorshuizen et al., 2020; Zeiler et al., 2021). From the, albeit limited, studies that reported socioeconomic status, the current data likely reflects participants with higher social privilege. Therefore, we speculate that, across studies, participants may have incurred fewer financial pressures, which afforded greater access to leisure time and facilities during quarantine, compared with the general population. As such, this may have facilitated engagement with self‐care, recovery strategies, and social support as discussed in the qualitative literature, thus contributing to the reduced ED symptomatology reported across several studies. Based on the findings of this review, Table 4 outlines multiple recommendations for individuals, researchers, clinicians, and public health messaging.
Collectively, the included studies identified several factors that may contribute to an individual's risk and/or protection from adverse outcomes during the pandemic. The most commonly reported factors associated with worse outcomes during the pandemic included psychological distress, comorbidity, poor coping and emotion regulation strategies, female gender, increased time spent online, longer periods of social isolation and confinement, and higher levels of BI and eating concerns at baseline (e.g., Baenas et al., 2020; Castellini et al., 2020; Coulthard et al., 2021; Haddad et al., 2020). Notably, body mass index was also reported as a correlate of adverse BI and DE/ED outcomes; however, this is likely due to the effect of societal stigma (i.e., through weight‐centric healthcare and public health messaging) and internalized weight stigma (Lessard & Puhl, 2021; Pearl & Schulte, 2021). Unsurprisingly, the most commonly reported factors associated with better outcomes were contradictory of the abovementioned factors, and included adaptive coping mechanisms and emotion regulation strategies, social support, taking part in enjoyable activities, and maintaining daily routines (e.g., Baenas et al., 2020; Branley‐Bell & Talbot, 2020; Giel et al., 2021; Schlegl, Maier, et al., 2020; Schlegl, Meule, et al., 2020).
Findings were inconsistent regarding the role of ED subtype as a risk factor for more adverse outcomes. There are several possible explanations for this. First, study findings are likely to be influenced by the type of measures used and which symptoms the measures target. In the current review, there was high variability in measures used to assess BI and eating outcomes, making comparison across studies challenging. Second, multiple studies clustered different EDs when comparing the impact of COVID‐19 on target outcomes. For example, combining participants with various EDs and comparing them to a healthy control group or comparing participants with AN to a combined participant group with BN, BED, and other EDs. Finally, it should be noted that most studies relied on self‐reporting of ED diagnosis or self‐report questionnaires of ED symptoms. Limited empirical evidence currently exists from treatment centers and clinical trials that include objective assessment of ED diagnosis and symptomatology.
4.2. The influence of COVID‐19 on marginalized and underrepresented populations
Very few studies have hitherto explored the influence of the COVID‐19 pandemic on participants from historically marginalized or underrepresented groups. A majority of investigations were conducted in WEIRD countries (i.e., Europe or North America), and few included participants' ethnicity or racialized group belonging, nor their sexual orientation. There was also limited consideration of how intersectionality of multiple marginalized identities may have influenced adverse mental health outcomes during the COVID‐19 pandemic. Of studies that provided information about participants' ethnicity or racialized group belonging, sexual orientation, and/or socioeconomic status, the majority of participants were White, cisgender, heterosexual, highly educated, and of a higher socioeconomic status.
There is some evidence showing that participants who identify as LGBTQ+ and/or BIPOC are more at risk of reporting adverse mental health, BI, and eating outcomes during COVID‐19 (Christensen, Forbush, et al., 2021; S. Kim, Wang, et al., 2021; Quathamer & Joy, 2021; Tabler et al., 2021). Contrary to expectations, several studies reported no effect of gender (e.g., H. Kim, Rackoff, et al., 2021; Puhl et al., 2020), ethnicity/racialized group belonging (e.g., Coulthard et al., 2021; Czepczor‐Bernat et al., 2021; H. Kim, Rackoff, et al., 2021), or sexuality (e.g., Czepczor‐Bernat et al., 2021; H. Kim, Rackoff, et al., 2021) on BI or DE. However, such studies included predominantly White, female, and heterosexual participants, which could have obscured unique effects. Future research should explicitly take into account participants' experiences of discrimination and racism as a possible mechanism of effects.
In addition, when conducting comparisons across participants, some studies combined multiple sexualities (e.g., heterosexual compared to lesbian, bisexual, queer, questioning, or other sexualities) and ethnicities (e.g., Hispanic compared to non‐Hispanic); thus, ignoring important differences between specific participant subgroups. In fact, in the majority of studies, gender, sexual orientation, and ethnicity were not reported, or were assessed as dichotomous variables (e.g., male, female; heterosexual, nonheterosexual; White, non‐White). Finally, in longitudinal studies, the proportion of LGBTQ+ and/or BIPOC participants tended to decrease over time, indicating higher attrition rates for these populations. Future studies should therefore consider employing novel strategies to ensure equitable recruitment and analysis of participant subgroups, while considering intersecting identities and the impact of experiencing multiple inequalities on mental health outcomes during COVID‐19 (Gibson et al., 2021). Furthermore, clinicians, researchers, and other practitioners should be aware of their own implicit and explicit biases, and consider how inequalities might affect their patients and/or participants with regards to symptomatology, treatment/research experiences, and outcomes (Crisp, 2021).
4.3. Strengths and limitations
Strengths of this review include the preregistration of the protocol with PROSPERO, the rigorous dual screening process for inclusion and quality assessment, and the use of validated and rigorous tools (EPHPP and CASP) specifically targeted for evaluation of quantitative and qualitative studies. The inclusion of qualitative, quantitative, and mixed‐methods studies allowed for a more comprehensive and global understanding of the impact of COVID‐19 on target outcomes, not limited to quantifiable measures. Finally, the insights generated from this review led to a practical recommendation guide for individuals living and/or working with EDs and those responsible for public health messaging (see Table 4).
The findings of the present review should also be considered in light of some limitations. Overall, given the range of divergent findings of studies, it is at present challenging to understand and synthesize these studies in more depth. Although presenting multiple advantages above traditional systematic reviews, mixed‐studies reviews may compound the methodological challenges of selecting, appraising, and synthesizing quantitative and qualitative research with the added difficulty of integrating the data in a meaningful way. Although we followed predetermined inclusion and exclusion criteria and multiple authors were engaged in the study selection and data extraction processes, we did not assess interrater reliability. As such, a limitation is that the accuracy of the study selection and data extraction procedures in the current review were not evaluated. Furthermore, no consensus currently exists regarding at which point and in which manner quantitative and qualitative components should be integrated, although existing guidelines were used to minimize this limitation. In addition, mixed‐studies reviews present theoretical and methodological challenges of bringing together differently structured studies, addressing different, yet related, questions, and studies conducted within different paradigms (Grant & Booth, 2009). For the current review, we adopted the convergent integrated approach (Hong et al., 2017) to ensure that the data from qualitative and quantitative studies were combined and evaluated using an established methodology to increase the richness and robustness of the synthesis (Grant & Booth, 2009; Stern et al., 2020).
5. CONCLUSION
The findings of this review show both negative and positive influences of the COVID‐19 pandemic and related restrictions on individuals' BI, DE outcomes, ED symptomatology, and overall mental health and well‐being. There is currently high variability in study designs, measures used, and findings across different studies and participant samples, precluding firm conclusions regarding the impact of COVID‐19 on target outcomes, particularly in the long term. However, the combined findings of this review highlight multiple important considerations for future research, including the need to identify risk and protective factors to enhance BI and eating outcomes, as well as overall mental health during the ongoing pandemic and beyond.
AUTHOR CONTRIBUTIONS
Jekaterina Schneider: Conceptualization; formal analysis; investigation; methodology; project administration; writing – original draft; writing – review and editing. Georgina Pegram: Formal analysis; methodology; writing – original draft; writing – review and editing. Benjamin Gibson: Formal analysis; methodology; writing – review and editing. Deborah Talamonti: Conceptualization; formal analysis; methodology; writing – review and editing. Aline Tinoco: Formal analysis; writing – review and editing. Nadia Craddock: Formal analysis; methodology; writing – review and editing. Emily Louise Matheson: Methodology; writing – review and editing. Mark Forshaw: Project administration; supervision; writing – review and editing.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
The authors want to thank Emeritus Professor Michael Levine for his support in identifying relevant studies and for the work he does within eating disorder communities, and Professor Sarah Grogan for her insightful comments on the manuscript.
Schneider, J. , Pegram, G. , Gibson, B. , Talamonti, D. , Tinoco, A. , Craddock, N. , Matheson, E. , & Forshaw, M. (2022). A mixed‐studies systematic review of the experiences of body image, disordered eating, and eating disorders during the COVID‐19 pandemic. International Journal of Eating Disorders, 1–42. 10.1002/eat.23706
Action Editor: Kelly L. Klump
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
*Indicates references included in systematic review.
- Acle, A. , Cook, B. J. , Siegfried, N. , & Beasley, T. (2021). Cultural considerations in the treatment of eating disorders among racial/ethnic minorities: A systematic review. Journal of Cross‐Cultural Psychology, 52(5), 468–488. 10.1177/00220221211017664 [DOI] [Google Scholar]
- * Akgül, S. , Akdemir, D. , Nalbant, K. , Derman, O. , Alan, B. E. , Tüzün, Z. , & Kanbur, N. (2021). The effects of the COVID‐19 lockdown on adolescents with an eating disorder and identifying factors predicting disordered eating behaviour. Early Intervention in Psychiatry. 10.1111/eip.13193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfalahi, M. , Mahadevan, S. , Balushi, R. A. , Chan, M. F. , Saadon, M. A. , Al‐Adawi, S. , & Qoronfleh, M. W. (2021). Prevalence of eating disorders and disordered eating in Western Asia: A systematic review and meta‐analysis. Eating Disorders. 10.1080/10640266.2021.1969495 [DOI] [PubMed] [Google Scholar]
- Armijo‐Olivo, S. , Stiles, C. R. , Hagen, N. A. , Biondo, P. D. , & Cummings, G. G. (2012). Assessment of study quality for systematic reviews: A comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: Methodological research. Journal of Evaluation in Clinical Practice, 18(1), 12–18. 10.1111/j.1365-2753.2010.01516.x [DOI] [PubMed] [Google Scholar]
- * Baceviciene, M. , & Jankauskiene, R. (2021). Changes in sociocultural attitudes towards appearance, body image, eating attitudes and behaviours, physical activity, and quality of life in students before and during COVID‐19 lockdown. Appetite, 166, 105452. 10.1016/j.appet.2021.105452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Baenas, I. , Caravaca‐Sanz, E. , Granero, R. , Sánchez, I. , Riesco, N. , Testa, G. , Vintró‐Alcaraz, C. , Treasure, J. , Jiménez‐Murcia, S. , & Fernández‐Aranda, F. (2020). COVID‐19 and eating disorders during confinement: Analysis of factors associated with resilience and aggravation of symptoms. European Eating Disorders Review, 28(6), 855–863. 10.1002/erv.2771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beccia, A. L. , Baek, J. , Austin, S. B. , Jesdale, W. M. , & Lapane, K. L. (2021). Eating‐related pathology at the intersection of gender, gender expression, sexual orientation, and weight status: An intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) of the growing up today study cohorts. Social Science & Medicine, 281, 114092. 10.1016/j.socscimed.2021.114092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker, C. B. , Middlemass, K. , Taylor, B. , Johnson, C. , & Gomez, F. (2017). Food insecurity and eating disorder pathology. International Journal of Eating Disorders, 50(9), 1031–1040. 10.1002/eat.22735 [DOI] [PubMed] [Google Scholar]
- * Bellapigna, C. R. , Kalibatseva, Z. , Martino, S. , & Yang, K. (2021). Need for structure, loneliness, social media use, and body image as predictors of mental health symptoms in the context of COVID‐19. Stockton University.
- * Branley‐Bell, D. , & Talbot, C. V. (2020). Exploring the impact of the COVID‐19 pandemic and UK lockdown on individuals with experience of eating disorders. Journal of Eating Disorders, 8, 44. 10.1186/s40337-020-00319-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Branley‐Bell, D. , & Talbot, C. V. (2021). “It is the only constant in what feels like a completely upside down and scary world”: Living with an eating disorder during COVID‐19 and the importance of perceived control for recovery and relapse. Appetite, 167, 105596. 10.31234/osf.io/tqfsz [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Breiner, C. E. , Miller, M. L. , & Hormes, J. M. (2021). Changes in eating and exercise behaviors during the COVID‐19 pandemic in a community sample: A retrospective report. Eating Behaviors, 42, 101539. 10.1016/j.eatbeh.2021.101539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bristow, C. , Meurer, C. , Simmonds, J. , & Snell, T. (2020). Anti‐obesity public health messages and risk factors for disordered eating: A systematic review. Health Promotion International, 35(6), 1551–1569. 10.1093/heapro/daaa018 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Brown, S. , Opitz, M.‐C. , Peebles, A. I. , Sharpe, H. , Duffy, F. , & Newman, E. (2021). A qualitative exploration of the impact of COVID‐19 on individuals with eating disorders in the UK. Appetite, 156, 104977. 10.1016/j.appet.2020.104977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Buckley, G. L. , Hall, L. E. , Lassemillante, A.‐C. M. , & Belski, R. (2021). Disordered eating & body image of current and former athletes in a pandemic; a convergent mixed methods study‐what can we learn from COVID‐19 to support athletes through transitions? Journal of Eating Disorders, 9(1), 73. 10.1186/s40337-021-00427-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke, N. L. , Schaefer, L. M. , Hazzard, V. M. , & Rodgers, R. F. (2020). Where identities converge: The importance of intersectionality in eating disorders research. International Journal of Eating Disorders, 53(10), 1605–1609. 10.1002/eat.23371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Castellini, G. , Cassioli, E. , Rossi, E. , Innocenti, M. , Gironi, V. , Sanfilippo, G. , Felciai, F. , Monteleone, A. M. , & Ricca, V. (2020). The impact of COVID‐19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. International Journal of Eating Disorders, 53(11), 1855–1862. 10.1002/eat.23368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Cecchetto, C. , Aiello, M. , Gentili, C. , Ionta, S. , & Osimo, S. A. (2021). Increased emotional eating during COVID‐19 associated with lockdown, psychological and social distress. Appetite, 160, 105122. 10.1016/j.appet.2021.105122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Chan, C. Y. , & Chiu, C. Y. (2021). Disordered eating behaviors and psychological health during the COVID‐19 pandemic. Psychology, Health & Medicine, 27, 249–256. 10.1080/13548506.2021.1883687 [DOI] [PubMed] [Google Scholar]
- * Christensen, K. A. , Forbush, K. T. , Richson, B. N. , Thomeczek, M. L. , Perko, V. L. , Bjorlie, K. , Christian, K. , Ayres, J. , Wildes, J. E. , & Mildrum Chana, S. (2021). Food insecurity associated with elevated eating disorder symptoms, impairment, and eating disorder diagnoses in an American University student sample before and during the beginning of the COVID‐19 pandemic. International Journal of Eating Disorders, 54(7), 1213–1223. 10.1002/eat.23517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen, K. A. , Hagan, K. E. , & Forbush, K. T. (2021). Clinical science can address rising eating disorder psychopathology during the Covid‐19 pandemic: Comment on Gruber et al., 2020. PsyArXiv. 10.31234/osf.io/592za [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Clark Bryan, D. , Macdonald, P. , Ambwani, S. , Cardi, V. , Rowlands, K. , Willmott, D. , & Treasure, J. (2020). Exploring the ways in which COVID‐19 and lockdown has affected the lives of adult patients with anorexia nervosa and their carers. European Eating Disorders Review, 28(6), 826–835. 10.1002/erv.2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, V. , & Braun, V. (2014). Thematic analysis. In Teo T. (Ed.), Encyclopedia of critical psychology (pp. 1947–1952). Springer. 10.1007/978-1-4614-5583-7_311 [DOI] [Google Scholar]
- Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46. 10.1177/001316446002000104 [DOI] [Google Scholar]
- * Conceição, E. , de Lourdes, M. , Ramalho, S. , Félix, S. , Pinto‐Bastos, A. , & Vaz, A. R. (2021). Eating behaviors and weight outcomes in bariatric surgery patients amidst COVID‐19. Surgery for Obesity and Related Diseases, 17(6), 1165–1174. 10.1016/j.soard.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Coulthard, H. , Sharps, M. , Cunliffe, L. , & van den Tol, A. (2021). Eating in the lockdown during the Covid 19 pandemic; self‐reported changes in eating behaviour, and associations with BMI, eating style, coping and health anxiety. Appetite, 161, 105082. 10.1016/j.appet.2020.105082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw, K. W. (2017). On intersectionality: Essential writings. The New Press. [Google Scholar]
- Crisp, C. (2021). Beyond tolerance: An examination of LGBTQ+ cultural competence in eating disorder treatment centers. Pepperdine University. [Google Scholar]
- * Czepczor‐Bernat, K. , Swami, V. , Modrzejewska, A. , & Modrzejewska, J. (2021). COVID‐19‐related stress and anxiety, body mass index, eating disorder symptomatology, and body image in women from Poland: A cluster analysis approach. Nutrients, 13(4), 1384. 10.3390/nu13041384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmer, C. , Bosnjak, M. , & Mata, J. (2020). The association between weight stigma and mental health: A meta‐analysis. Obesity Reviews, 21(1), e12935. 10.1111/obr.12935 [DOI] [PubMed] [Google Scholar]
- * Félix, S. , de Lourdes, M. , Ribeiro, I. , Cunha, B. , Ramalho, S. , Vaz, A. R. , Machado, P. P. , & Conceição, E. (2021). A preliminary study on the psychosocial impact of COVID‐19 lockdown in post‐bariatric surgery women: The importance of eating behavior, health care access, and social support. Current Psychology, 40, 6275–6281. 10.1007/s12144-021-01529-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Fernández‐Aranda, F. , Casas, M. , Claes, L. , Bryan, D. C. , Favaro, A. , Granero, R. , Gudiol, C. , Jiménez‐Murcia, S. , Karwautz, A. , & Le Grange, D. (2020). COVID‐19 and implications for eating disorders. European Eating Disorders Review, 28(3), 239–245. 10.1002/erv.2738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Fernández‐Aranda, F. , Munguía, L. , Mestre‐Bach, G. , Steward, T. , Etxandi, M. , Baenas, I. , Granero, R. , Sánchez, I. , Ortega, E. , & Andreu, A. (2020). COVID isolation eating scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. European Eating Disorders Review, 28(6), 871–883. 10.1002/erv.2784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Flaudias, V. , Iceta, S. , Zerhouni, O. , Rodgers, R. F. , Billieux, J. , Llorca, P.‐M. , Boudesseul, J. , De Chazeron, I. , Romo, L. , & Maurage, P. (2020). COVID‐19 pandemic lockdown and problematic eating behaviors in a student population. Journal of Behavioral Addictions, 9(3), 826–835. 10.1556/2006.2020.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Frayn, M. , Fojtu, C. , & Juarascio, A. (2021). COVID‐19 and binge eating: Patient perceptions of eating disorder symptoms, tele‐therapy, and treatment implications. Current Psychology, 40, 6249–6258. 10.1007/s12144-021-01494-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson, B. , Schneider, J. , Talamonti, D. , & Forshaw, M. (2021). The impact of inequality on mental health outcomes during the COVID‐19 pandemic: A systematic review. Canadian Psychology/Psychologie Canadienne, 62(1), 101–126. 10.1037/cap0000272 [DOI] [Google Scholar]
- * Giel, K. E. , Schurr, M. , Zipfel, S. , Junne, F. , & Schag, K. (2021). Eating behaviour and symptom trajectories in patients with a history of binge eating disorder during COVID‐19 pandemic. European Eating Disorders Review, 29(4), 657–662. 10.1002/erv.2837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Graell, M. , Morón‐Nozaleda, M. G. , Camarneiro, R. , Villaseñor, Á. , Yáñez, S. , Muñoz, R. , Martínez‐Núñez, B. , Miguélez‐Fernández, C. , Muñoz, M. , & Faya, M. (2020). Children and adolescents with eating disorders during COVID‐19 confinement: Difficulties and future challenges. European Eating Disorders Review, 28(6), 864–870. 10.1002/erv.2763 [DOI] [PubMed] [Google Scholar]
- Grant, M. J. , & Booth, A. (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26(2), 91–108. 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- * Gullo, N. , & Walker, D. C. (2021). Increased videoconferencing after COVID‐19 stay‐at‐home orders increased depression and anxiety but did not impact appearance satisfaction or binge eating. Computers in Human Behavior Reports, 3, 100080. 10.1016/j.chbr.2021.100080 [DOI] [Google Scholar]
- * Haddad, C. , Zakhour, M. , Haddad, R. , Al Hachach, M. , Sacre, H. , & Salameh, P. (2020). Association between eating behavior and quarantine/confinement stressors during the coronavirus disease 2019 outbreak. Journal of Eating Disorders, 8(1), 40. 10.1186/s40337-020-00317-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Haddad, C. , Zakhour, M. , Siddik, G. , Haddad, R. , Sacre, H. , & Salameh, P. (2021). COVID‐19 outbreak: Does confinement have any impact on weight change perception? Nutrition Clinique et Métabolisme, 35(2), 137–143. 10.1016/j.nupar.2021.02.003 [DOI] [Google Scholar]
- Hansen, S. J. , & Menkes, D. B. (2021). What is driving the pandemic related surge in disordered eating? BMJ, 374, n2175. 10.1136/bmj.n2175 [DOI] [PubMed] [Google Scholar]
- Harden, A. (2010). Mixed‐methods systematic reviews: Integrating quantitative and qualitative findings. Focus, 25, 1–8. [Google Scholar]
- Harden, A. , & Thomas, J. (2010). Mixed methods and systematic reviews: Examples and emerging issues. In Tashakkori A. & Teddlie C. (Eds.), SAGE handbook of mixed methods in social & behavioral research (2nd ed., pp. 749–774). SAGE. [Google Scholar]
- Hayes, S. , & Smith, E. (2021). Eating disorders during a coronavirus pandemic. In Moustafa A. A. (Ed.), Mental health effects of COVID‐19 (pp. 159–170). Academic Press. [Google Scholar]
- Hazzard, V. M. , Loth, K. A. , Hooper, L. , & Becker, C. B. (2020). Food insecurity and eating disorders: A review of emerging evidence. Current Psychiatry Reports, 22(12), 74. 10.1007/s11920-020-01200-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland, G. , & Tiggemann, M. (2016). A systematic review of the impact of the use of social networking sites on body image and disordered eating outcomes. Body Image, 17, 100–110. 10.1016/j.bodyim.2016.02.008 [DOI] [PubMed] [Google Scholar]
- Hong, Q. N. , Pluye, P. , Bujold, M. , & Wassef, M. (2017). Convergent and sequential synthesis designs: Implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Systematic Reviews, 6, 61. 10.1186/s13643-017-0454-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Hunter, R. , & Gibson, C. (2021). Narratives from within ‘lockdown’: A qualitative exploration of the impact of COVID‐19 confinement on individuals with anorexia nervosa. Appetite, 166, 105451. 10.1016/j.appet.2021.105451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam, T. , Pitafi, A. H. , Arya, V. , Wang, Y. , Akhtar, N. , Mubarik, S. , & Xiaobei, L. (2021). Panic buying in the COVID‐19 pandemic: A multi‐country examination. Journal of Retailing and Consumer Services, 59, 102357. 10.1016/j.jretconser.2020.102357 [DOI] [Google Scholar]
- Jackson, N. , & Waters, E. (2005). Criteria for the systematic review of health promotion and public health interventions. Health Promotion International, 20(4), 367–374. 10.1093/heapro/dai022 [DOI] [PubMed] [Google Scholar]
- * Jordan, A. K. , Barnhart, W. R. , Studer‐Perez, E. I. , Kalantzis, M. A. , Hamilton, L. , & Musher‐Eizenman, D. R. (2021). ‘Quarantine 15’: Pre‐registered findings on stress and concern about weight gain before/during COVID‐19 in relation to caregivers' eating pathology. Appetite, 166, 105580. 10.1016/j.appet.2021.105580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Keel, P. K. , Gomez, M. M. , Harris, L. , Kennedy, G. A. , Ribeiro, J. , & Joiner, T. E. (2020). Gaining “The Quarantine 15:” Perceived versus observed weight changes in college students in the wake of COVID‐19. International Journal of Eating Disorders, 53(11), 1801–1808. 10.1002/eat.23375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, M. A. , & Smith, J. E. M. (2020). “Covibesity,” a new pandemic. Obesity Medicine, 19, 100282. 10.1016/j.obmed.2020.100282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khosravi, M. (2020). The challenges ahead for patients with feeding and eating disorders during the COVID‐19 pandemic. Journal of Eating Disorders, 8(1), 43. 10.1186/s40337-020-00322-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Kim, H. , Rackoff, G. N. , Fitzsimmons‐Craft, E. E. , Shin, K. E. , Zainal, N. H. , Schwob, J. T. , Eisenberg, D. , Wilfley, D. E. , Taylor, C. B. , & Newman, M. G. (2021). College mental health before and during the COVID‐19 pandemic: Results from a nationwide survey. Cognitive Therapy and Research, 46, 1–10. 10.1007/s10608-021-10241-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Kim, S. , Wang, W.‐L. , & Mason, T. (2021). Eating disorders and trajectory of mental health across the COVID‐19 pandemic: Results from the understanding America study. Journal of Affective Disorders Reports, 5, 100187. 10.1016/j.jadr.2021.100187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Koenig, J. , Kohls, E. , Moessner, M. , Lustig, S. , Bauer, S. , Becker, K. , Thomasius, R. , Eschenbeck, H. , Diestelkamp, S. , & Gillé, V. (2021). The impact of COVID‐19 related lockdown measures on self‐reported psychopathology and health‐related quality of life in German adolescents. European Child & Adolescent Psychiatry. 10.1007/s00787-021-01843-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Larkin, R. (2021). Impact of COVID‐19 on physical activity and health influences among college students. University of Mississippi. https://egrove.olemiss.edu/hon_thesis/1771
- * Leenaerts, N. , Vaessen, T. , Ceccarini, J. , & Vrieze, E. (2021). How COVID‐19 lockdown measures could impact patients with bulimia nervosa: Exploratory results from an ongoing experience sampling method study. Eating Behaviors, 41, 101505. 10.1016/j.eatbeh.2021.101505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Lessard, L. M. , & Puhl, R. M. (2021). Adolescents' exposure to and experiences of weight stigma during the COVID‐19 pandemic. Journal of Pediatric Psychology, 46(8), 950–959. 10.1093/jpepsy/jsab071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Lin, J. A. , Hartman‐Munick, S. M. , Kells, M. R. , Milliren, C. E. , Slater, W. A. , Woods, E. R. , Forman, S. F. , & Richmond, T. K. (2021). The impact of the COVID‐19 pandemic on the number of adolescents/young adults seeking eating disorder‐related care. Journal of Adolescent Health, 69(4), 660–663. 10.1016/j.jadohealth.2021.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long, H. A. , French, D. P. , & Brooks, J. M. (2020). Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Research Methods in Medicine & Health Sciences, 1(1), 31–42. 10.1177/2632084320947559 [DOI] [Google Scholar]
- Lydecker, J. A. , & Grilo, C. M. (2019). Food insecurity and bulimia nervosa in the United States. International Journal of Eating Disorders, 52(6), 735–739. 10.1002/eat.23074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Machado, P. P. , Pinto‐Bastos, A. , Ramos, R. , Rodrigues, T. F. , Louro, E. , Gonçalves, S. , Brandão, I. , & Vaz, A. (2020). Impact of COVID‐19 lockdown measures on a cohort of eating disorders patients. Journal of Eating Disorders, 8(1), 57–64. 10.1186/s40337-020-00340-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Martínez‐de‐Quel, Ó. , Suárez‐Iglesias, D. , López‐Flores, M. , & Pérez, C. A. (2021). Physical activity, dietary habits and sleep quality before and during COVID‐19 lockdown: A longitudinal study. Appetite, 158, 105019. 10.1016/j.appet.2020.105019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * McCombie, C. , Austin, A. , Dalton, B. , Lawrence, V. , & Schmidt, U. (2020). “Now it's just old habits and misery”–understanding the impact of the Covid‐19 pandemic on people with current or life‐time eating disorders: A qualitative study. Frontiers in Psychiatry, 11, 1140. 10.3389/fpsyt.2020.589225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Meda, N. , Pardini, S. , Slongo, I. , Bodini, L. , Zordan, M. A. , Rigobello, P. , Visioli, F. , & Novara, C. (2021). Students' mental health problems before, during, and after COVID‐19 lockdown in Italy. Journal of Psychiatric Research, 134, 69–77. 10.1016/j.jpsychires.2020.12.045 [DOI] [PubMed] [Google Scholar]
- Mensinger, J. L. , Cox, S. A. , & Henretty, J. R. (2021). Treatment outcomes and trajectories of change in patients attributing their eating disorder onset to anti‐obesity messaging. Psychosomatic Medicine, 83(7), 777–786. 10.1097/PSY.0000000000000962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikhail, M. E. , & Klump, K. L. (2021). A virtual issue highlighting eating disorders in people of black/African and indigenous heritage. International Journal of Eating Disorders, 54(3), 459–467. 10.1002/eat.23402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miniati, M. , Marzetti, F. , Palagini, L. , Marazziti, D. , Orrù, G. , Conversano, C. , & Gemignani, A. (2021). Eating disorders spectrum during the COVID pandemic: A systematic review. Frontiers in Psychology, 12, 663376. 10.3389/fpsyg.2021.663376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra, K. , & Rampal, J. (2020). The COVID‐19 pandemic and food insecurity: A viewpoint on India. World Development, 135, 105068. 10.1016/j.worlddev.2020.105068 [DOI] [Google Scholar]
- Monteleone, A. M. , Cascino, G. , Barone, E. , Carfagno, M. , & Monteleone, P. (2021). COVID‐19 pandemic and eating disorders: What can we learn about psychopathology and treatment? A systematic review. Current Psychiatry Reports, 23(12), 83. 10.1007/s11920-021-01294-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Monteleone, A. M. , Cascino, G. , Marciello, F. , Abbate‐Daga, G. , Baiano, M. , Balestrieri, M. , Barone, E. , Bertelli, S. , Carpiniello, B. , & Castellini, G. (2021). Risk and resilience factors for specific and general psychopathology worsening in people with eating disorders during COVID‐19 pandemic: A retrospective Italian multicentre study. Eating and Weight Disorders‐Studies on Anorexia, Bulimia and Obesity, 26, 2443–2452. 10.1007/s40519-020-01097-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Monteleone, A. M. , Marciello, F. , Cascino, G. , Abbate‐Daga, G. , Anselmetti, S. , Baiano, M. , Balestrieri, M. , Barone, E. , Bertelli, S. , & Carpiniello, B. (2021). The impact of COVID‐19 lockdown and of the following “re‐opening” period on specific and general psychopathology in people with eating disorders: The emergent role of internalizing symptoms. Journal of Affective Disorders, 285, 77–83. 10.1016/j.jad.2021.02.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles, M. T. , Bertmann, F. , Belarmino, E. H. , Wentworth, T. , Biehl, E. , & Neff, R. (2020). The early food insecurity impacts of COVID‐19. Nutrients, 12(7), 2096. 10.3390/nu12072096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Nisticò, V. , Bertelli, S. , Tedesco, R. , Anselmetti, S. , Priori, A. , Gambini, O. , & Demartini, B. (2021). The psychological impact of COVID‐19‐related lockdown measures among a sample of Italian patients with eating disorders: A preliminary longitudinal study. Eating and Weight Disorders, 26, 2771–2777. 10.1007/s40519-021-01137-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowaskie, D. Z. , Filipowicz, A. T. , Choi, Y. , & Fogel, J. M. (2021). Eating disorder symptomatology in transgender patients: Differences across gender identity and gender affirmation. International Journal of Eating Disorders, 54(8), 1493–1499. 10.1002/eat.23539 [DOI] [PubMed] [Google Scholar]
- Noyes, J. , Booth, A. , Moore, G. , Flemming, K. , Tunçalp, Ö. , & Shakibazadeh, E. (2019). Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: Clarifying the purposes, designs and outlining some methods. BMJ Global Health, 4(Suppl 1), e000893. 10.1136/bmjgh-2018-000893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Nutley, S. K. , Falise, A. M. , Henderson, R. , Apostolou, V. , Mathews, C. A. , & Striley, C. W. (2021). Impact of the COVID‐19 pandemic on disordered eating behavior: Qualitative analysis of social media posts. JMIR Mental Health, 8(1), e26011. 10.2196/26011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , & Brennan, S. E. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl, R. L. (2020). Weight stigma and the “Quarantine‐15”. Obesity, 28(7), 1180–1181. 10.1002/oby.22850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl, R. L. , & Schulte, E. M. (2021). Weight bias during the COVID‐19 pandemic. Current Obesity Reports, 10, 181–190. 10.1007/s13679-021-00432-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Pfund, G. N. , Hill, P. L. , & Harriger, J. (2020). Video chatting and appearance satisfaction during COVID‐19: Appearance comparisons and self‐objectification as moderators. International Journal of Eating Disorders, 53(12), 2038–2043. 10.1002/eat.23393 [DOI] [PubMed] [Google Scholar]
- * Phelan, N. , Behan, L. A. , & Owens, L. (2021). The impact of the COVID‐19 pandemic on women's reproductive health. Frontiers in Endocrinology, 12, 642755. 10.3389/fendo.2021.642755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Philippe, K. , Chabanet, C. , Issanchou, S. , & Monnery‐Patris, S. (2021). Child eating behaviors, parental feeding practices and food shopping motivations during the COVID‐19 lockdown in France: (how) did they change? Appetite, 161, 105132. 10.1016/j.appet.2021.105132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Phillipou, A. , Meyer, D. , Neill, E. , Tan, E. J. , Toh, W. L. , Van Rheenen, T. E. , & Rossell, S. L. (2020). Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders, 53(7), 1158–1165. 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Pikoos, T. D. , Buzwell, S. , Sharp, G. , & Rossell, S. L. (2020). The COVID‐19 pandemic: Psychological and behavioral responses to the shutdown of the beauty industry. International Journal of Eating Disorders, 53(12), 1993–2002. 10.1002/eat.23385 [DOI] [PubMed] [Google Scholar]
- Pikoos, T. D. , Buzwell, S. , Sharp, G. , & Rossell, S. L. (2021). The zoom effect: Exploring the impact of video calling on appearance dissatisfaction and interest in aesthetic treatment during the COVID‐19 pandemic. Aesthetic Surgery Journal, 41, NP2066–NP2075. 10.1093/asj/sjab257 [DOI] [PubMed] [Google Scholar]
- Popay, J. , Roberts, H. , Sowden, A. , Petticrew, M. , Arai, L. , Rodgers, M. , Britten, N. , Roen, K. , & Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods Programme. Version 1. 10.13140/2.1.1018.4643 [DOI]
- * Puhl, R. M. , Lessard, L. M. , Larson, N. , Eisenberg, M. E. , & Neumark‐Stzainer, D. (2020). Weight stigma as a predictor of distress and maladaptive eating behaviors during COVID‐19: Longitudinal findings from the EAT study. Annals of Behavioral Medicine, 54(10), 738–746. 10.1093/abm/kaaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Quathamer, N. , & Joy, P. (2021). Being in a queer time: Exploring the influence of the COVID‐19 pandemic on LGBTQ+ body image. Nutrition & Dietetics. 10.1111/1747-0080.12699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar, R. P. (2020). COVID‐19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Ramalho, S. M. , Trovisqueira, A. , de Lourdes, M. , Gonçalves, S. , Ribeiro, I. , Vaz, A. R. , Machado, P. P. , & Conceição, E. (2021). The impact of COVID‐19 lockdown on disordered eating behaviors: The mediation role of psychological distress. Eating and Weight Disorders, 27, 179–188. 10.1007/s40519-021-01128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmusson, G. , Lydecker, J. A. , Coffino, J. A. , White, M. A. , & Grilo, C. M. (2019). Household food insecurity is associated with binge‐eating disorder and obesity. International Journal of Eating Disorders, 52(1), 28–35. 10.1002/eat.22990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Richardson, C. , Patton, M. , Phillips, S. , & Paslakis, G. (2020). The impact of the COVID‐19 pandemic on help‐seeking behaviors in individuals suffering from eating disorders and their caregivers. General Hospital Psychiatry, 67, 136–140. 10.1016/j.genhosppsych.2020.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Robertson, M. , Duffy, F. , Newman, E. , Bravo, C. P. , Ates, H. H. , & Sharpe, H. (2021). Exploring changes in body image, eating and exercise during the COVID‐19 lockdown: A UK survey. Appetite, 159, 105062. 10.1016/j.appet.2020.105062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. , Linardon, J. , Courtet, P. , & Guillaume, S. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53(7), 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Scharmer, C. , Martinez, K. , Gorrell, S. , Reilly, E. E. , Donahue, J. M. , & Anderson, D. A. (2020). Eating disorder pathology and compulsive exercise during the COVID‐19 public health emergency: Examining risk associated with COVID‐19 anxiety and intolerance of uncertainty. International Journal of Eating Disorders, 53(12), 2049–2054. 10.1002/eat.23395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Schlegl, S. , Maier, J. , Meule, A. , & Voderholzer, U. (2020). Eating disorders in times of the COVID‐19 pandemic—Results from an online survey of patients with anorexia nervosa. International Journal of Eating Disorders, 53(11), 1791–1800. 10.1002/eat.23374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Schlegl, S. , Meule, A. , Favreau, M. , & Voderholzer, U. (2020). Bulimia nervosa in times of the COVID‐19 pandemic—Results from an online survey of former inpatients. European Eating Disorders Review, 28(6), 847–854. 10.1002/erv.2773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider, J. , Talamonti, D. , Gibson, B. , & Forshaw, M. (2021). Factors mediating the psychological well‐being of healthcare workers responding to global pandemics: A systematic review. Journal of Health Psychology, 00(0), 1–22. 10.1177/13591053211012759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Serin, E. , & Koç, M. C. (2020). Examination of the eating behaviours and depression states of the university students who stay at home during the coronavirus pandemic in terms of different variables. Progress in Nutrition, 22(1), 3–43. 10.23751/pn.v22i1-S.9780 [DOI] [Google Scholar]
- Sideli, L. , Lo Coco, G. , Bonfanti, R. C. , Borsarini, B. , Fortunato, L. , Sechi, C. , & Micali, N. (2021). Effects of COVID‐19 lockdown on eating disorders and obesity: A systematic review and meta‐analysis. European Eating Disorders Review, 29, 826–841. 10.1002/erv.2861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Simone, M. , Emery, R. L. , Hazzard, V. M. , Eisenberg, M. E. , Larson, N. , & Neumark‐Sztainer, D. (2021). Disordered eating in a population‐based sample of young adults during the COVID‐19 outbreak. International Journal of Eating Disorders, 54(7), 1189–1201. 10.1002/eat.23505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolak, L. , & Levine, M. P. (2015). Body image, disordered eating, and eating disorders: Connections and disconnects. In Smolak L. & Levine M. P. (Eds.), The Wiley handbook of eating disorders, assessment, prevention, treatment, policy, and future directions (pp. 1–10). John Wiley & Sons. [Google Scholar]
- * Spettigue, W. , Obeid, N. , Erbach, M. , Feder, S. , Finner, N. , Harrison, M. E. , Isserlin, L. , Robinson, A. , & Norris, M. L. (2021). The impact of COVID‐19 on adolescents with eating disorders: A cohort study. Journal of Eating Disorders, 9(1), 65–72. 10.1186/s40337-021-00419-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern, C. , Lizarondo, L. , Carrier, J. , Godfrey, C. , Rieger, K. , Salmond, S. , Apóstolo, J. , Kirkpatrick, P. , & Loveday, H. (2020). Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evidence Synthesis, 18(10), 2108–2118. 10.11124/JBISRIR-D-19-00169 [DOI] [PubMed] [Google Scholar]
- * Stoddard, T. A. (2021). Eating and body image disorders in the time of COVID19: An anthropological inquiry into the pandemic's effects on the bodies [Master's thesis, University of South Florida]. ProQuest Dissertations Publishing.
- * Swami, V. , Horne, G. , & Furnham, A. (2021). COVID‐19‐related stress and anxiety are associated with negative body image in adults from the United Kingdom. Personality and Individual Differences, 170, 110426. 10.1016/j.paid.2020.110426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Swami, V. , Todd, J. , Robinson, C. , & Furnham, A. (2021). Self‐compassion mediates the relationship between COVID‐19‐related stress and body image disturbance: Evidence from the United Kingdom under lockdown. Personality and Individual Differences, 183, 111130. 10.1016/j.paid.2021.111130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Tabler, J. , Schmitz, R. M. , Charak, R. , & Dickinson, E. (2021). Perceived weight gain and eating disorder symptoms among LGBTQ+ adults during the COVID‐19 pandemic: A convergent mixed‐method study. Journal of Eating Disorders, 9, 115. 10.21203/rs.3.rs-587552/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Taquet, M. , Geddes, J. R. , Luciano, S. , & Harrison, P. J. (2021). Incidence and outcomes of eating disorders during the COVID‐19 pandemic. The British Journal of Psychiatry, 1–3. 10.1192/bjp.2021.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Termorshuizen, J. D. , Watson, H. J. , Thornton, L. M. , Borg, S. , Flatt, R. E. , MacDermod, C. M. , Harper, L. E. , van Furth, E. F. , Peat, C. M. , & Bulik, C. M. (2020). Early impact of COVID‐19 on individuals with self‐reported eating disorders: A survey of ~1,000 individuals in the United States and The Netherlands. International Journal of Eating Disorders, 53(11), 1780–1790. 10.1002/eat.23353 [DOI] [PubMed] [Google Scholar]
- Thomas, B. , Ciliska, D. , Dobbins, M. , & Micucci, S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews on Evidence‐Based Nursing, 1(3), 176–184. 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- Touyz, S. , Lacey, H. , & Hay, P. (2020). Eating disorders in the time of COVID‐19. Journal of Eating Disorders, 8, 19–21. 10.1186/s40337-020-00295-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Trott, M. , Johnstone, J. , Pardhan, S. , Barnett, Y. , & Smith, L. (2021). Changes in body dysmorphic disorder, eating disorder, and exercise addiction symptomology during the COVID‐19 pandemic: A longitudinal study of 319 health club users. Psychiatry Research, 298, 113831. 10.1016/j.psychres.2021.113831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Vall‐Roqué, H. , Andrés, A. , & Saldaña, C. (2021). The impact of COVID‐19 lockdown on social network sites use, body image disturbances and self‐esteem among adolescent and young women. Progress in Neuro‐Psychopharmacology and Biological Psychiatry, 110, 110293. 10.1016/j.pnpbp.2021.110293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Vitagliano, J. A. , Jhe, G. , Milliren, C. E. , Lin, J. A. , Spigel, R. , Freizinger, M. , Woods, E. R. , Forman, S. F. , & Richmond, T. K. (2021). COVID‐19 and eating disorder and mental health concerns in patients with eating disorders. Journal of Eating Disorders, 9(1), 80–87. 10.1186/s40337-021-00437-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Vuillier, L. , May, L. , Greville‐Harris, M. , Surman, R. , & Moseley, R. L. (2021). The impact of the COVID‐19 pandemic on individuals with eating disorders: The role of emotion regulation and exploration of online treatment experiences. Journal of Eating Disorders, 9(1), 10. 10.1186/s40337-020-00362-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman, R. S. , Bauer, S. , & Thomas, J. J. (2020). Access to evidence‐based care for eating disorders during the COVID‐19 crisis. International Journal of Eating Disorders, 53(5), 639–646. 10.1002/eat.23279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White III, J. * (2021). Examining physical activity behaviors and psychometric beliefs of college students before and after the COVID‐19 shutdown [Winthrop University].
- World Health Organization . (2021). The true death toll of COVID‐19: Estimating global excess mortality . https://www.who.int/data/stories/the-true-death-toll-of-covid-19-estimating-global-excess-mortality
- * Zeiler, M. , Wittek, T. , Kahlenberg, L. , Gröbner, E.‐M. , Nitsch, M. , Wagner, G. , Truttmann, S. , Krauss, H. , Waldherr, K. , & Karwautz, A. (2021). Impact of COVID‐19 confinement on adolescent patients with anorexia nervosa: A qualitative interview study involving adolescents and parents. International Journal of Environmental Research and Public Health, 18(8), 4251. 10.3390/ijerph18084251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Zhou, Y. , & Wade, T. D. (2021). The impact of COVID‐19 on body‐dissatisfied female university students. International Journal of Eating Disorders, 54(7), 1283–1288. 10.1002/eat.23521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zickgraf, H. F. , Hazzard, V. M. , & O'Connor, S. M. (2022). Food insecurity is associated with eating disorders independent of depression and anxiety: Findings from the 2020–2021 healthy minds study. International Journal of Eating Disorders, 55, 354–361. 10.1002/eat.23668 [DOI] [PubMed] [Google Scholar]
- Zidouemba, P. R. , Kinda, S. R. , & Ouedraogo, I. M. (2020). Could COVID‐19 worsen food insecurity in Burkina Faso? The European Journal of Development Research, 32(5), 1379–1401. 10.1057/s41287-020-00324-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


