Abstract
Objectives
The first wave of the COVID‐19 pandemic necessitated extensive infection control measures in long‐term care (LTC) and had a significant impact on staffing and services. Anecdotal reports indicate that this negatively affected LTC residents' quality of care and wellbeing, but there is scarce evidence on the effects of COVID‐19 on quality of dementia care in LTC.
Methods
From December 2020 to March 2021, we conducted a cross‐sectional online survey among staff who worked in LTC homes in Ontario, Canada. Survey questions examined staffs' perceptions of the impact of COVID‐19 on dementia quality of care during the initial wave of the COVID‐19 pandemic (beginning 1 March 2020).
Results
There were a total of 227 survey respondents; more than half reported both worsened overall quality of care (51.3%) and worsening of a majority of specific quality of care measures (55.5%). Measures of cognitive functioning, mobility and behavioural symptoms were most frequently described as worsened. Medical and allied/support staff had the highest odds of reporting overall worsened quality of care, while specialized behavioural care staff and those with more experience in LTC were less likely to. LTC home factors including rural location and smaller size, staffing challenges, higher number of outbreaks and less COVID‐19 preparedness were associated with increased odds of perceived worsening of quality of dementia care outcomes.
Conclusions
These findings suggest that COVID‐19 pandemic restrictions and related effects such as inadequate staffing may have contributed to poor quality of care and outcomes for those with dementia in LTC.
Keywords: COVID‐19, dementia, long‐term care, nursing home, quality of care
Key points
There is a lack of information on the impact of COVID‐19 on quality of dementia care in long‐term care (LTC).
In this survey of LTC staff, approximately half of respondents reported worsened overall quality of dementia care related to the COVID‐19 pandemic and infection control measures.
A majority of respondents reported worsening of specific measures of quality of care. In particular, a worsening of resident cognitive functioning, mobility and behavioural symptoms was reported.
Worsened quality of care related to the COVID‐19 pandemic may have contributed to poor outcomes for those with dementia in LTC.
1. INTRODUCTION
Globally, residential care homes were disproportionately affected by the initial wave of the COVID‐19 pandemic. In Canada, 70% of long‐term care (LTC) residents have dementia and a majority are of advanced age (mean 83 years) and frail, 1 , 2 making them particularly vulnerable to the effects of COVID‐19. Over 6000 LTC residents died during the first wave of the pandemic, accounting for 66% of total COVID‐19 related deaths in Canada. 3 The rapid spread and serious adverse health effects of COVID‐19 in LTC necessitated sustained infection control measures and exposed or magnified longstanding problems, such as chronic understaffing. 4 , 5 Visitor restrictions prevented the support from family and friend caregivers and limited access to healthcare and social services. These measures and associated consequences have undoubtedly affected LTC residents' quality of care and wellbeing.
Quality of care in Canadian LTC is closely monitored via publicly reported quality indicators, including measures of key outcomes reflecting resident functioning, safety, and quality of life. 6 , 7 , 8 At present, we have little understanding of how these quality indices may have changed and how their measurement was impacted by the pandemic. Past studies evaluating COVID‐19 and quality of care in LTC have focused on whether pre‐pandemic quality is associated with COVID‐19 outbreaks and deaths, on which evidence is mixed. 9 Thus, there is an important opportunity to examine effects related to COVID‐19 on quality of dementia care in LTC. Specific concerns include that the isolation of residents and the loss of support and advocacy from families may have resulted in a worsening of markers of quality in LTC, such as increases in the use of physical restraints or psychotropic medications such as antipsychotics, 10 , 11 which have both been widely reported among persons with dementia in other settings. 12 , 13 , 14
To address the dearth of empirical data in this area, we conducted a survey among staff who worked in LTC homes in Ontario, Canada during the initial waves of the pandemic. This reflects a period when Ontario LTC homes implemented strict measures including masking, visitor and activity restrictions, and resident isolation and testing protocols to limit the introduction and spread of the virus. 5 Our objectives were to (i) examine staff perceptions of the impact of the COVID‐19 pandemic and related restrictions on overall quality of care and specific quality of care measures for residents with dementia; and (ii) examine the associations between staff and home characteristics and perceived worsening of dementia quality of care during the initial wave of the pandemic.
2. METHODS
2.1. Study design
A cross‐sectional online survey of staff working in Ontario LTC homes was conducted during a 12‐week period from December 16, 2020 to March 12, 2021. The survey was programmed and hosted by the University of Waterloo Survey Research Centre (SRC; https://uwaterloo.ca/survey‐research‐centre/). This study was based on a larger program of research investigating the barriers and opportunities to improve the compassionate and safe isolation of LTC home residents with dementia during public health crises guided by the Dementia Isolation Toolkit (DIT; www.dementiaisolationtoolkit.com). 15 , 16 The University Health Network Research Ethics Board and a University of Waterloo Research Ethics Committee approved the study protocols and survey instruments.
2.2. Participants
LTC home staff (including administrators, front‐line health care providers and support staff) were recruited through research team stakeholder partners and relevant provincial organizations (Behavioural Supports Ontario [BSO], Regional Geriatric Programs, Ontario Long‐Term Care Association, AdvantAge Ontario, Toronto Region COVID‐19 LTC/Continuing Care Table), social media and the DIT website with an open survey link. Eligible respondents must have worked in an Ontario LTC home at any time during the first wave of the COVID‐19 pandemic (i.e., from March 1, 2020 up to their survey date), be fluent in English, and not currently working for the University Health Network (the institutional affiliation for some research team members). An initial invitation and several reminders were distributed via organizational email lists, websites, newsletters and social media platforms. A draw for one of five $100 gift cards was used as an incentive to complete the survey. Given the recruitment strategy and open survey link, accurate numbers of LTC home staff who were made aware of the survey link are unavailable and it is not possible to derive contact or response rates. Overall characteristics of LTC staff and facilities in Ontario are shown in Supplementary Table S1.
2.3. Survey measures
Staff, home, and quality of care survey items were derived based on previous LTC research team and with input from stakeholder partners and organizations. 17 , 18 , 19 These categorical measures included close‐ended standard responses (some allowing for additional free text options to specify ‘other’). Given sample size limitations, several of the categorical measures were collapsed based on data distribution, clinical considerations, and preliminary bivariate associations. Most measures had no or few (≤ 1%) missing responses.
2.4. Staff characteristics
Respondents' role in the LTC was categorized as administrator (including director of care, manager); medical (including registered, practical or licensed practical nurse, physician); BSO team member (specialized staff who support the management of residents with dementia and behavioural symptoms); or allied healthcare or support services staff (including personal support work, physical therapy, social work, recreation, dietary and environmental services). They were asked about their age, gender, ethnic/cultural identity role in the LTC home, years of LTC experience, and average days/week providing or supporting care in the LTC home (since 1 March 2020). Responses for gender were collapsed as female versus non‐female (male, non‐binary or gender diverse, and prefer not to answer) given small cells.
2.5. LTC home characteristics and COVID‐19 related challenges
Home items captured the size (number of beds), location population size (categorized as rural/small if less than 30,000 population and urban if 30,000 or more), ownership status (government owned, not‐for‐profit, for profit) and COVID‐19 related challenges including staffing challenges since the start of the pandemic, perceived preparedness of the LTC home for COVID‐19, and reported COVID‐19 outbreaks in the home (number and size of the largest outbreak for both residents and staff). For size of COVID‐19 outbreaks, those who reported I don't know were coded as missing.
2.6. Quality of care
Respondents were also asked about their perceptions of the impact of COVID‐19 and related infection and control restrictions on the quality of care for residents with dementia. These included the impact on overall resident quality of care and on nine specific measures of quality of care including the frequency and severity of responsive behaviours, cognitive function, activities of daily living (ADL) function, mobility, food/fluid intake, presence of pressure ulcers, frequency of falls, use of medications for responsive behaviours, and use of physical restraints. These items align with indicators used for measuring quality of care in LTC in Canada. 20
The items for overall quality of care and behaviours used a five‐level Likert scale with values of significantly worse, somewhat worse, about the same, somewhat improved, and significantly improved. Cognitive function, ADL function, mobility and food/fluid intake had the same response values with the addition of I don't know. Pressure ulcers, falls, medications and physical restraints had response values of significantly increased, somewhat increased, about the same, somewhat decreased, significantly decreased and I don't know. These responses were aggregated into binary or 3‐level measures (e.g., significantly or somewhat worse, same or somewhat or significantly improved, I don't know).
2.7. Analyses
Descriptive analyses examined the distribution of staff, home and COVID‐19 related measures overall and according to two binary measures of the perceived impact of COVID‐19 and infection control measures on quality of dementia care: (i) overall quality of care (coded as significantly or somewhat worse vs. same, somewhat or significantly improved) and (ii) number of specific quality of measures considered to have worsened (coded as ≥ 5 [of 9] measures vs. ≤ 4, based on the median cut‐point). We also compared the distribution of responses on the nine‐specific quality of dementia care measures among respondents who reported that overall quality of dementia care was significantly or somewhat worse versus same, somewhat or significantly improved. Comparisons across these groups were made with chi‐square tests using an alpha of 0.05 for statistical significance.
Unadjusted and adjusted logistic regression models examined the associations between respondent and LTC home characteristics with these two quality of dementia care measures (with separate models for each outcome). Measures that were significant at an alpha of 0.1 in the unadjusted model were retained in the full multivariable model. A step‐wise selection approach was employed in deriving the final multivariable models with considerations of high correlations between independent measures (collinearity).
All data were analyzed using Stata 17 (StataCorp LLC, College Station, Texas, USA).
3. RESULTS
There were 228 completed web surveys with an average survey length of 23 min. We excluded one respondent who identified themselves (in open text field) as a family/friend caregiver, resulting in a final analytical sample size of n = 227.
3.1. Characteristics of participating staff and LTC homes
Survey respondents had a variety of professional backgrounds, representing almost all facets of LTC staffing. A majority were either BSO (30.1%) or allied healthcare or support staff (32.7%); the remainder were administrative (19.0%) or medical staff (18.1%; Table 1). Respondents were relatively evenly distributed across age categories (though with a lower proportion aged ≥55 years) and years of experience in LTC. A majority were female (89.9%), White (74.5%) and working on average at least 5 days/week in LTC (71.8%).
TABLE 1.
Distribution (% [n]) of LTC survey respondent characteristics, overall and by perceived impact of the COVID‐19 pandemic on overall quality of care for residents with dementia
| Characteristic | Perceived impact of COVID‐19 and infection control measures on quality of care a | ||
|---|---|---|---|
| Total sample (n = 227) | Significantly or somewhat worse (51.3%; n = 115) | Same/Somewhat or significantly improved (48.7%; n = 109) | |
| Respondent factors | |||
| Staff role in LTC b | |||
| Administrative | 19.0 (43) | 44.2 (19) | 55.8 (24) |
| Medical (nurse, physician) | 18.1 (41) | 65.9 (27) | 34.2 (14) |
| Behavioural supports Ontario | 30.1 (68) | 41.2 (28) | 58.8 (40) |
| Allied healthcare/Support | 32.7 (74) | 56.3 (40) | 43.7 (31) |
| Age | |||
| 18–34 | 26.4 (60) | 45.8 (27) | 54.2 (32) |
| 35–44 | 25.1 (57) | 55.4 (31) | 44.6 (25) |
| 45–54 | 27.3 (62) | 54.1 (33) | 45.9 (28) |
| ≥55 | 21.2 (48) | 50.0 (24) | 50.0 (24) |
| Gender | |||
| Female | 89.9 (204) | 51.0 (103) | 49.0 (99) |
| Non‐female | 10.1 (23) | 54.6 (12) | 45.5 (10) |
| Ethnicity | |||
| White | 74.5 (169) | 50.9 (85) | 49.1 (82) |
| Non‐white | 25.6 (58) | 52.6 (30) | 47.4 (27) |
| Years of experience in LTC | |||
| <5 years | 24.7 (56) | 53.7 (29) | 46.3 (25) |
| 6–10 years | 26.0 (59) | 47.5 (28) | 52.5 (31) |
| 11–20 years | 24.2 (55) | 60.0 (33) | 40.0 (22) |
| >20 years | 25.1 (57) | 44.6 (25) | 55.4 (31) |
| Average # days/week providing or supporting care in LTC | |||
| ≤4 days/week | 28.2 (64) | 58.7 (37) | 41.3 (26) |
| >4 days/week | 71.8 (163) | 48.5 (78) | 51.6 (83) |
| LTC home factors | |||
| Size (number of beds) | |||
| <100 | 26.1 (59) | 59.3 (35) | 40.7 (24) |
| 100–199 | 50.4 (114) | 44.1 (49) | 55.9 (62) |
| ≥200 | 23.5 (53) | 56.6 (30) | 43.4 (23) |
| Region b | |||
| Rural/Small (<30,000 population) | 21.7 (49) | 64.6 (31) | 35.4 (17) |
| Urban (≥30,000 population) | 78.3 (177) | 47.4 (83) | 52.6 (92) |
| Ownership | |||
| Government | 28.9 (65) | 55.4 (36) | 44.6 (29) |
| Not‐for‐profit | 32.0 (72) | 50.0 (35) | 50.0 (35) |
| For profit | 34.7 (78) | 50.7 (39) | 49.4 (38) |
| Do not know | 4.4 (10) | 40.0 (4) | 60.0 (6) |
| Ensuring adequate staffing levels since Mar 1/20 c | |||
| Significantly more challenging | 61.2 (137) | 59.6 (81) | 40.4 (55) |
| Somewhat more challenging/Same/Somewhat or significantly less challenging | 38.8 (87) | 38.6 (34) | 61.4 (54) |
| Number of outbreaks | |||
| None | 22.9 (52) | 48.1 (25) | 51.9 (27) |
| 1 | 24.7 (56) | 45.5 (25) | 54.6 (30) |
| 2–3 | 30.0 (68) | 51.5 (34) | 48.5 (32) |
| ≥4 | 22.5 (51) | 60.8 (31) | 39.2 (20) |
| Size of (largest) outbreak among residents | |||
| No outbreak among residents | 41.1 (92) | 48.4 (44) | 51.7 (47) |
| <5 residents | 17.9 (40) | 51.3 (20) | 48.7 (19) |
| 5–20 residents | 15.6 (35) | 48.6 (17) | 51.4 (18) |
| >20 residents | 25.5 (57) | 60.7 (34) | 39.3 (22) |
| Size of (largest) outbreak among staff | |||
| No outbreak among staff | 26.2 (57) | 47.4 (27) | 52.6 (30) |
| <5 staff | 33.5 (73) | 49.3 (35) | 50.7 (36) |
| 5–20 staff | 20.6 (45) | 55.6 (25) | 44.4 (20) |
| >20 staff | 19.7 (43) | 58.1 (25) | 41.9 (18) |
| Level of COVID preparedness b | |||
| Not at all or poorly prepared | 34.8 (78) | 61.5 (48) | 38.5 (30) |
| Somewhat prepared | 44.2 (99) | 49.0 (48) | 51.0 (50) |
| Well or very well prepared | 21.0 (47) | 37.0 (17) | 63.0 (29) |
Note: Table 1 shows characteristics of LTC staff who responded to the survey and LTC homes represented by participants.
Abbreviation: LTC, long‐term care.
Distribution shown as row %.
p < 0.05.
p < 0.01.
Half (50.4%) of respondents represented mid‐sized homes (100–199 beds) and most (78.3%) were from urban homes. About a third were affiliated with each of not‐for profit and for‐profit homes with slightly less from government owned homes. Ensuring adequate staffing since the onset of the pandemic was reported as significantly more challenging by 61.2% of respondents and 77.1% reported experiencing at least one COVID‐19 outbreak in their LTC home. Only 21% reported that their home was well or very well prepared for COVID‐19.
3.2. Perceived impact of COVID‐19 on overall quality of care
About half (51.3%) of respondents reported that overall quality of care for residents with dementia was somewhat or significantly worse. Staff role, home region, adequacy of staffing levels, and COVID‐19 preparedness were all significantly associated with perceived worsening of overall quality of care at the bivariate level (Table 1). All remaining respondent and LTC home factors (including outbreak characteristics) were not significantly associated with the overall quality of dementia care outcome at the bivariate level.
Findings from adjusted logistic regression models showed that staff role (Adjusted [Adj] Odds Ratio [OR] = 4.48, 95% Confidence Interval [CI] 1.79–11.21 for medical and Adj OR = 2.83, 95%CI 1.31–6.09 for allied healthcare/support vs. BSO staff), home region (Adj OR = 2.92, 95%CI 1.40–6.13 for rural/small), perceived adequacy of staffing levels (Adj OR = 3.03, 95% CI 1.63–5.65 for significantly more challenging) and level of COVID‐19 preparedness (Adj OR = 2.35, 95%CI 1.04–5.31 for not at all or poorly prepared) remained significantly associated with a perceived worsening of overall quality of dementia care (Table 2). Additionally, respondents who reported 11–20 years of experience in LTC were also more likely to report a worsening of overall quality of dementia care relative to those with >20 years of experience (Adj OR = 2.15, 95% CI 0.93–4.96).
TABLE 2.
Unadjusted and adjusted odds ratios (95% Confidence Intervals) for perceived worsening of overall quality of dementia care following the onset of COVID‐19 associated with LTC survey respondent characteristics
| Characteristic | Perceived worsening of overall quality of dementia care | |
|---|---|---|
| Unadjusted odds ratio (95% CI) | Adjusted a odds ratio (95% CI) | |
| Respondent factors | ||
| Staff role in LTC | ||
| Administrative | 1.13 (0.52–2.45) | 1.84 (0.78–4.34) |
| Medical (nurse, physician) | 2.76 (1.23–6.17) | 4.48 (1.79–11.21) |
| Behavioural supports Ontario | 1.00 | 1.00 |
| Allied healthcare/Support | 1.84 (0.94–3.61) | 2.83 (1.31–6.09) |
| Age | ||
| 18–34 (ref) | 1.00 | |
| 35–44 | 1.47 (0.70–3.06) | |
| 45–54 | 1.40 (0.68–2.86) | |
| ≥55 | 1.19 (0.55–2.54) | |
| Gender | ||
| Female (ref) | 1.00 | |
| Non‐female | 1.15 (0.48–2.79) | |
| Ethnicity | ||
| White (ref) | 1.00 | |
| Non‐white | 1.07 (0.59–1.96) | |
| Years of experience in LTC | ||
| <5 years | 1.44 (0.68–3.05) | 1.49 (0.64–3.44) |
| 6–10 years | 1.12 (0.54–2.33) | 1.20 (0.53–2.71) |
| 11–20 years | 1.86 (0.88–3.95) | 2.15 (0.93–4.96) |
| >20 years (ref) | 1.00 | 1.00 |
| Average # days/week providing or supporting care in LTC | ||
| ≤4 days/week | 1.51 (0.84–2.73) | |
| >4 days/week (ref) | 1.00 | |
| LTC home factors | ||
| LTC size (number of beds) | ||
| <100 | 1.85 (0.97–3.50) | |
| 100–199 | 1.00 | |
| ≥200 | 1.65 (0.85–3.19) | |
| Region | ||
| Rural/Small (<30,000 population) | 2.02 (1.04–3.92) | 2.92 (1.40–6.13) |
| Urban (≥30,000 population) (ref) | 1.00 | 1.00 |
| Ownership | ||
| Government (ref) | 1.00 | |
| Not‐for‐profit | 0.81 (0.41–1.59) | |
| For profit | 0.83 (0.43–1.60) | |
| Do not know | 0.54 (0.14–2.08) | |
| Ensuring adequate staffing levels since Mar 1/20 | ||
| Significantly more challenging | 2.49 (1.43–4.33) | 3.03 (1.63–5.65) |
| Somewhat more challenging/Same/Somewhat or significantly less challenging (ref) | 1.00 | 1.00 |
| Number of outbreaks | ||
| None (ref) | 1.00 | |
| 1 | 0.90 (0.42–1.92) | |
| 2–3 | 1.15 (0.55–2.37) | |
| ≥4 | 1.67 (0.77–3.66) | |
| Size of (largest) outbreak among residents | ||
| No outbreak among residents (ref) | 1.00 | |
| <5 residents | 1.12 (0.53–2.38) | |
| 5–20 residents | 1.01 (0.46–2.20) | |
| >20 residents | 1.65 (0.84–3.24) | |
| Size of (largest) outbreak among staff | ||
| No outbreak among staff (ref) | 1.00 | |
| <5 staff | 1.08 (0.54–2.17) | |
| 5–20 staff | 1.39 (0.63–3.04) | |
| >20 staff | 1.54 (0.69–3.43) | |
| Level of COVID preparedness | ||
| Not at all or poorly prepared | 2.73 (1.29–5.79) | 2.35 (1.04–5.31) |
| Somewhat prepared | 1.64 (0.80–3.36) | 1.58 (0.73–3.44) |
| Well or very well prepared (ref) | 1.00 | 1.00 |
Note: Table 2 shows the association between LTC staff respondent characteristics and perceived worsening of overall quality of dementia care. Medical and allied healthcare/support staff type years of experience in LTC, rural/small home region, significantly more challenging perceived adequacy of staffing levels, and lesser level of COVID‐19 preparedness were significantly associated with a perceived worsening of overall quality of dementia care following the onset of the pandemic in adjusted models.
Abbreviations: CI, Confidence Intervals, LTC, long‐term care.
Final logistic regression model adjusted for staff role in LTC, years of experience in LTC, region of LTC home, adequacy of staffing levels, and level of COVID preparedness.
3.3. Perceived impact of COVID‐19 on specific quality of care measures
At least half of staff respondents reported that residents' status had worsened in relation to their behaviours, cognition, daily functioning, mobility, and food/fluid intake following the onset of the pandemic (Figure 1; Supplementary Table S2). Residents' cognitive functioning was the area most frequently reported by respondents as being significantly or somewhat worse (81.9%), followed by mobility (71.2%) and frequency/severity of responsive behaviours (66.1%). Almost half (48.7%) reported that the frequency of falls had increased among residents with dementia. For the remaining specific quality measures (presence of pressure ulcers, use of medications for behaviours, physical restraint use), relatively fewer respondents noted an increase (worsening) following the pandemic, though there was also a relative increase in those responding ‘I don't know’ for these measures. Respondents who reported that overall quality of care for residents with dementia had worsened following the pandemic were also significantly more likely to report a worsening of all specific quality of care measures, with the exception of physical restraint use (Supplementary Table S2).
FIGURE 1.
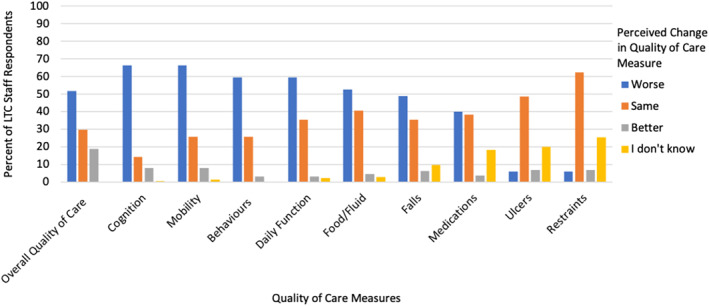
Long‐term care (LTC) staff perceived Impact of the COVID‐19 pandemic on overall and specific quality of care measures
Worsening of a majority (≥5) of individual quality of care measures was reported by 55.5% of respondents (Figure 2). The bivariate associations between respondent and home characteristics and number of quality of care measures perceived to have worsened (comparing those reporting a worsening of ≥5 quality measures vs. ≤4) are shown in Supplementary Table 3. After adjusting for other relevant covariates, perceived worsening on a majority (≥5) of individual quality measures was significantly more likely to be reported by staff respondents with fewer years of experience working in LTC (Adj OR = 2.80, 95% CI 1.23–6.39 for those with 6–10 years vs. those with >20 years), from smaller LTC homes (Adj OR = 2.09, 95% CI 1.04–4.23 for <100 beds vs. 100–199 beds), those reporting greater challenges in ensuring adequate staffing since the pandemic onset (Adj OR = 2.27, 95% CI 1.24–4.15), a higher number of COVID‐19 outbreaks (Adj OR = 3.36, 95% CI 1.29–8.73 for 4+ outbreaks vs. none), and a relatively low level of COVID‐19 preparedness in the LTC home (Adj OR = 3.34, 95% CI 1.46–7.63 for not at all or poorly prepared and Adj OR = 2.52, 95% CI 1.15–5.50 for somewhat prepared; Table 3).
FIGURE 2.
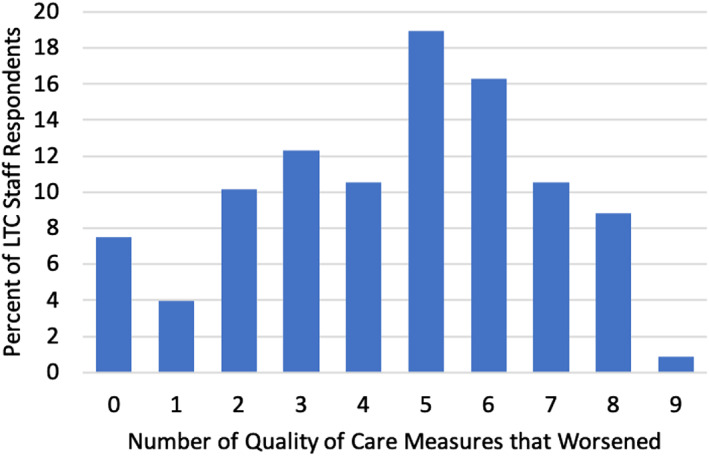
Distribution of the number of specific quality of care measures perceived by long‐term care (LTC) staff to have worsened since the onset of the COVID‐19 pandemic
TABLE 3.
Unadjusted and adjusted odds ratios (95% Confidence Intervals) for perceived worsening of ≥5 quality of care measures (following the onset of COVID‐19) associated with LTC survey respondent characteristics
| Characteristic | Perceived worsening of ≥5 dementia quality of care measures (vs. ≤4) | |
|---|---|---|
| Unadjusted odds ratio (95% CI) | Adjusted a odds ratio (95% CI) | |
| Respondent factors | ||
| Staff role in LTC | ||
| Administrative | 0.86 (0.40–1.84) | |
| Medical (nurse, physician) | 1.60 (0.71–3.62) | |
| Behavioural supports Ontario (ref) | 1.00 | |
| Allied healthcare/Support | 0.67 (0.34–1.29) | |
| Age | ||
| 18–34 (ref) | 1.00 | |
| 35–44 | 0.48 (0.23–1.02) | |
| 45–54 | 0.41 (0.20–0.86) | |
| ≥55 | 0.83 (0.38–1.84) | |
| Gender | ||
| Female (ref) | 1.00 | |
| Non‐female | 0.48 (0.20–1.15) | |
| Ethnicity | ||
| White (ref) | 1.00 | |
| Non‐white | 0.81 (0.45–1.48) | |
| Years of experience in LTC | ||
| <5 years | 1.59 (0.76–3.34) | 1.55 (0.68–3.56) |
| 6–10 years | 2.51 (1.18–5.34) | 2.80 (1.23–6.39) |
| 11–20 years | 1.24 (0.59–2.60) | 1.09 (0.48–2.49) |
| >20 years (ref) | 1.00 | 1.00 |
| Average # days/week providing or supporting care in LTC | ||
| ≤4 days/week | 1.25 (0.69–2.24) | |
| >4 days/week (ref) | 1.00 | |
| LTC home factors | ||
| Size (number of beds) | ||
| <100 | 1.75 (0.91–3.34) | 2.09 (1.04–4.23) |
| 100–199 (ref) | 1.00 | 1.00 |
| ≥200 | 1.17 (0.61–2.24) | 0.91 (0.42–1.96) |
| Region | ||
| Rural/Small (<30,000 population) | 1.70 (0.88–3.28) | |
| Urban (≥30,000 population) (ref) | 1.00 | |
| Ownership | ||
| Government (ref) | 1.00 | |
| Not‐for‐profit | 0.76 (0.39–1.49) | |
| For profit | 1.36 (0.70–2.66) | |
| Do not know | 0.54 (0.14–2.08) | |
| Ensuring adequate staffing levels since Mar 1/20 | ||
| Significantly more challenging | 2.17 (1.26–3.76) | 2.27 (1.24–4.15) |
| Somewhat more challenging/Same/Somewhat or significantly less challenging (ref) | 1.00 | 1.00 |
| Number of outbreaks | ||
| None (ref) | 1.00 | 1.00 |
| 1 | 1.16 (0.54–2.47) | 1.12 (0.47–2.67) |
| 2–3 | 1.15 (0.56–2.36) | 1.08 (0.48–2.46) |
| ≥4 | 2.85 (1.26–6.49) | 3.36 (1.29–8.73) |
| Size of (largest) outbreak among residents | ||
| No outbreak among residents (ref) | 1.00 | |
| <5 residents | 1.14 (0.54–2.40) | |
| 5–20 residents | 1.52 (0.69–3.33) | |
| >20 residents | 3.19 (1.56–6.54) | |
| Size of (largest) outbreak among staff | ||
| No outbreak among staff (ref) | 1.00 | |
| <5 staff | 0.90 (0.45–1.81) | |
| 5–20 staff | 1.71 (0.77–3.78) | |
| >20 staff | 3.01 (1.28–7.12) | |
| Level of COVID preparedness | ||
| Not at all or poorly prepared | 3.74 (1.75–8.01) | 3.34 (1.46–7.63) |
| Somewhat prepared | 2.21 (1.08–4.51) | 2.52 (1.15–5.50) |
| Well or very well prepared (ref) | 1.00 | 1.00 |
Note: Table 3 shows perceived worsening on a majority (≥5) of individual quality measures after adjusting for relevant covariates (see Supplementary Table 1 for the bivariate distribution of characteristics for this outcome). In adjusted models, staff respondents with fewer years of experience working in LTC, from smaller LTC homes, reporting greater challenges in ensuring adequate staffing since the pandemic onset, from LTC homes with a higher number of COVID‐19 outbreaks, or a relatively low level of COVID‐19 preparedness in the LTC homes were all significantly more likely to report perceived worsening of a majority of quality measures.
Abbreviations: CI, Confidence Intervals, LTC, long‐term care.
Final logistic regression model adjusted for years of experience in LTC, LTC home size, adequacy of staffing levels, number of outbreaks and level of COVID preparedness.
4. DISCUSSION
A large impact of the COVID‐19 pandemic on quality of care for residents with dementia was reported in this survey of LTC staff, with over half of respondents reporting declines in overall quality of care and in a majority of specific quality of care measures. Measures of cognitive functioning, mobility and behavioural symptoms were most frequently described as worsened. Medical and allied healthcare/support staff were most likely to report overall worsened quality of care, while specialized behavioural care staff and those with more experience in LTC were least likely to. LTC home factors including rural location and smaller size, greater staffing challenges, higher number of outbreaks and less COVID‐19 preparedness were all associated with increased odds of perceived worsening of quality of dementia care outcomes.
These survey results are consistent with the small number of previous studies and numerous anecdotal reports about issues of quality of care and the negative impact on well‐being for people with dementia in LTC during the pandemic. 21 , 22 , 23 Past studies showed similar concerns of cognitive and functional decline, and worsened behavioural and psychological symptoms in LTC residents as reported by both family caregivers of residents with dementia and staff. 24 , 25 While there is a lack of observational studies directly demonstrating resident‐level changes in specific areas of dementia quality care, several studies have shown increases in psychotropic medication use in LTC, 10 , 11 , 26 believed to be a response to increases in depression and behavioural symptoms from reductions in essential care and limited prioritization of non‐pharmacological treatment approaches due to reduced staffing. 10 , 11 , 27 Social isolation resulting from infection control measures and visitor restrictions may also be responsible for the negative effects of COVID‐19 on persons with dementia in LTC, given the known benefits of social contact in dementia. 22 , 23 , 28 Functional decline has occurred in LTC residents without dementia regardless of COVID‐19 infection status, suggesting that factors beyond those due to COVID‐19 infection are partly responsible for the negative impact of the pandemic in residential care settings. 29 Our findings that nearly half of respondents did not perceive any worsening of overall quality of dementia care and the minimal perceived increase in physical restraint use during the pandemic are encouraging. The latter may be a result of longstanding quality improvement efforts aimed at limiting the use of restraints in LTC in Canada. 30 In an Italian study, higher rates of physical restraint use alongside more frequent psychotropic medication use were reported. 31
We found some important respondent‐ and home‐related factors associated with staff respondent perceptions of poorer quality of care for LTC residents with dementia during the initial wave of the COVID‐19 pandemic. In general, those in specialized roles supporting care for behavioural symptoms in dementia were less likely to report poorer overall quality of care and medical staff were most likely to. These findings may reflect differences in attitudes towards and skill in dementia care based on experience and role in dementia care among staff types. BSO staff are typically nurses or personal support workers (PSWs) with additional training. Previous research has shown that those with better training in dementia care have higher job satisfaction, motivation, and self‐efficacy in their roles. 32 , 33 , 34 While we did not examine these factors, they may influence staff perceptions of quality of care provided (e.g. a sense of competence in providing high quality care despite the pandemic). A more skilled staff mix is associated with higher care quality and better resident outcomes in LTC, and more training and experience may also affect the ability to provide high quality care regardless of the circumstances. 35 The medical staff category in our survey included both physicians and nurses, whose experience and involvement in day to day, direct care are varied, which may have affected their perception of the care provided.
At the home level, the association between home factors such as challenges ensuring adequate staffing, smaller size and less COVID‐19 preparedness and worsened perceived quality of care may reflect the relationship of these factors with COVID‐19 outbreak severity. LTC homes with higher staffing were better able to contain COVID‐19 spread 36 , 37 and thus may have been better able to reduce its overall impact including on quality of care. Others have found that COVID‐19 outbreaks in smaller homes affect a great number of residents, 38 possibly owing to challenges in implementing infection control measures such as physical distancing in smaller homes. In Ontario, more crowded homes were more likely to experience more severe outbreaks. 39 The impact of COVID‐19 preparedness on outcomes has not been examined in other studies, though adequate staffing has been identified as a key aspect of pandemic preparedness in LTC. 40
Our study was not designed to identify why quality of care may have been negatively affected by COVID‐19, though open‐ended responses to our survey shed some light on possible reasons. Respondents frequently described difficulty communicating verbally and non‐verbally while wearing personal protective equipment. Effectively isolating residents with dementia who may lack the ability to understand or recall the reasons for infection control measures, such as masking or physical distancing, was also identified as challenging.
While many issues underlying poor quality of dementia care and related outcomes due to COVID‐19 may be related to exacerbations of longstanding, systemic problems, others associated with worsened quality of care in our study, such as COVID‐19 preparedness and staffing challenges, may be more amenable to change. Several reports since the pandemic first wave have outlined clear strategies for improving pandemic preparedness, such as staff training, better access to personal protective equipment and more flexible visitation policies, 3 , 5 , 41 and guidelines for the ethical and effective isolation of residents with dementia that emphasise minimizing associated harms are now available. 16 Policies that promote higher and more skilled staffing, including personal support workers, recreation staff and dedicated infection control practitioners, will be important in lessening the negative impact of COVID‐19 or other outbreaks on dementia quality of care in the future. 5 , 37 , 42 , 43
This is one of few studies to evaluate post‐pandemic quality of dementia care in LTC and used established markers of quality of care. Respondents included a variety of LTC staff well positioned to speak to the quality of dementia care during the pandemic's first wave. Our study is limited by the subjective and retrospective nature of the survey data. Recall bias and a lack of resident‐level outcome and quality indicator data, or other perspectives on quality of care (such as those from family caregivers) may limit the validity of the findings. Though we are unable to characterize non‐respondents, a broad range of staff were represented among survey respondents, representing all major categories of LTC staff types involved in day‐to‐day resident care. Personal support workers (included in the allied/support staff group) make up the majority (58%) of LTC staff in Ontario 44 and were underrepresented among survey respondents compared to the overall LTC workforce, while administrative and BSO staff were overrepresented. BSO staff were less likely than other staff types to report a perceived worsening on overall quality of care, consequently, our study may underestimate the impact of COVID‐19 on quality of dementia care. Some observed differences, such as that between smaller home size and perceived worsening of overall quality of care, may have not reached statistical significance due to the small sample size and require further exploration. Finally, effects of COVID‐19 in LTC varied greatly across Canadian provinces—Ontario had higher rates of severe COVID‐19 infection and mortality compared to other provinces in the early pandemic. 45 Thus, impacts of COVID‐19 on quality of dementia care in LTC may differ in other areas.
There is a need for studies to examine the impact of COVID‐19 on outcomes beyond those directly related to COVID‐19 infections (e.g., mortality) in dementia residential care settings. Though COVID‐19 outbreaks in LTC have decreased in frequency and severity in subsequent waves of the pandemic owing to high vaccination rates, many LTC homes continue to have intermittent restrictions on visitation and social activities and ongoing staffing issues that may impact dementia quality of care. Studies examining longer term changes in LTC quality indicators will be helpful in characterizing areas of quality most substantially impacted by COVID‐19, with a goal of mitigating the risk that future outbreaks result in worsened quality of dementia care.
5. CONCLUSION
Our survey of LTC staff found that COVID‐19 was associated with worsened perceived overall quality of dementia care and worsening on a majority of specific quality measures. Although the impact of the COVID‐19 pandemic beyond mortality in LTC is yet to be well described, this study suggests that poorer quality of care may be one factor mediating the observed negative effects of COVID‐19 in individuals with dementia in LTC.
CONFLICT OF INTEREST
The authors have no relevant conflicts of interest to disclose.
ETHICS STATEMENT
This study was reviewed and received ethics clearance by the University Health Network Research Ethics Board (REB#20‐5866) and University of Waterloo Research Ethics Committee (ORE#42803).
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank Ontario long‐term care stakeholder partners for their involvement in developing and disseminating the survey, study participants for their engagement and time responding to the survey, and the Survey Research Centre at the University of Waterloo for the expert administration and coordination of the online survey. This study was supported with funds from the Neuropsychiatric Symptoms Team (Team 11) of the Canadian Consortium on Neurodegeneration in Aging (CCNA), which is supported by a grant from the Canadian Institutes of Health Research (CIHR) with funding from several partners, and by funds from the Province of Ontario Rapid Access COVID‐19 research grant.
Kirkham J, Shorey CL, Iaboni A, et al. Staff perceptions of the consequences of COVID‐19 on quality of dementia care for residents in Ontario long‐term care homes. Int J Geriatr Psychiatry. 2022;1‐13. 10.1002/gps.5725
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Hsu AT, Lane N. Impact of COVID‐19 on Residents of Canada’s Long‐Term Care Homes — Ongoing Challenges and Policy response. 2020. Accessed September 12, 2021. https://ltccovid.org/2020/04/15/impact‐of‐covid‐19‐on‐residents‐of‐canadas‐long‐term‐care‐homes‐ongoing‐challenges‐and‐policy‐response/ [Google Scholar]
- 2. Long‐Term Care in Ontario: Sector Overview. Health Analytics Branch, Ministry of Health and Long‐Term Care. 2015. Accessed March 28, 2022. http://longtermcareinquiry.ca/wp‐content/uploads/Exhibit‐169‐Long‐Term‐Care‐in‐Ontario‐Sector‐overview.pdf [Google Scholar]
- 3. Canadian Institute for Health Information . The Impact of COVID‐19 on Long‐Term Care in Canada: Focus on the First 6 Months; 2021. Accessed April 5, 2022. https://www.cihi.ca/sites/default/files/document/impact‐covid‐19‐long‐term‐care‐canada‐first‐6‐months‐report‐en.pdf [Google Scholar]
- 4. Bakerjian D, Boltz M, Bowers B, et al. Expert nurse response to workforce recommendations made by the coronavirus commission for safety and quality in nursing homes. Nurs Outlook. 2021;69(5):735‐743. 10.1016/j.outlook.2021.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ontario’s LTC Covid‐19 Commission: Final Report. 2021. Accessed September 10, 2021. http://www.ltccommission‐commissionsld.ca/report/pdf/20210623_LTCC_AODA_EN.pdf [Google Scholar]
- 6. Canadian Institute for Health Information . Your Health System. Accessed April 18, 2022. https://yourhealthsystem.cihi.ca/hsp/indepth?lang=en#/ [Google Scholar]
- 7. Health Quality Ontario . LTC Indicator Review Report: the Review and Selection of Indicators for Long‐Term Care Public Reporting. 2015. Accessed October 2, 2021. https://www.hqontario.ca/Portals/0/documents/system‐performance/ltc‐indicator‐review‐report‐november‐2015.pdf [Google Scholar]
- 8. Health Quality Ontario . Looking for Balance: Antipsychotic Medication Use in Ontario Long‐Term Care Homes. Queen's Printer for Ontario; 2015. [Google Scholar]
- 9. Ochieng N, Chiambaram P, Garfield R, Neuman T. Factors Associated With COVID‐19 Cases and Deaths in Long‐Term Care Facilities: Findings from a Literature Review. Kaiser Family Foundation (KFF). Accessed November 4, 2021. https://www.kff.org/coronavirus‐covid‐19/issue‐brief/factors‐associated‐with‐covid‐19‐cases‐and‐deaths‐in‐long‐term‐care‐facilities‐findings‐from‐a‐literature‐review/ [Google Scholar]
- 10. Campitelli MA, Bronskill SE, Maclagan LC, et al. Comparison of medication prescribing before and after the COVID‐19 pandemic among nursing home residents in Ontario, Canada. JAMA Netw Open. 2021;4(8):e2118441. 10.1001/jamanetworkopen.2021.18441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stall NM, Zipursky JS, Rangrej J, et al. Assessment of psychotropic drug prescribing among nursing home residents in Ontario, Canada, during the COVID‐19 pandemic. JAMA Intern Med. 2021;181(6):861. 10.1001/jamainternmed.2021.0224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Suarez‐Gonzalez A. Detrimental Effects of Confinement and Isolation on the Cognitive and Psychological Health of People living With Dementia During COVID‐19: Emerging Evidence. International Long‐Term Care Policy Network. Accessed September 12, 2021. https://ltccovid.org/wp‐content/uploads/2020/07/LTCcovid‐1‐July‐Detrimental‐effects‐confinement‐on‐people‐with‐dementia.pdf [Google Scholar]
- 13. Suárez‐González A, Rajagopalan J, Livingston G, Alladi S. The effect of COVID‐19 isolation measures on the cognition and mental health of people living with dementia: a rapid systematic review of one year of quantitative evidence. EClinicalMedicine. 2021;39:101047. 10.1016/j.eclinm.2021.101047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Okuno T, Itoshima H, Shin J‐H, Morishita T, Kunisawa S, Imanaka Y. Physical restraint of dementia patients in acute care hospitals during the COVID‐19 pandemic: a cohort analysis in Japan. PLoS One. 2021;16(11):e0260446. 10.1371/journal.pone.0260446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Iaboni A, Quirt H, Engell K, et al. Barriers and facilitators to person‐centred infection prevention and control: results of a survey about the Dementia Isolation Toolkit. BMC Geriatr. 2022;22(1):74. 10.1186/s12877-022-02759-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iaboni A, Cockburn A, Marcil M, et al. Achieving safe, effective, and compassionate quarantine or isolation of older adults with dementia in nursing homes. Am J Geriatric Psychiatry. 2020;28(8):835‐838. 10.1016/j.jagp.2020.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Strain L, Maxwell CJ, Wanless D, Gilbart E. Designated Assisted Living (DAL) and Long‐Term Care (LTC) in Alberta: Selected Highlights from the Alberta Continuing Care Epidemiological Studies (ACCES). 2011. Accessed November 18, 2021. http://hdl.handle.net/10402/era.23779 [Google Scholar]
- 18. White EM, Wetle TF, Reddy A, Baier RR. Front‐line nursing home staff experiences during the COVID‐19 pandemic. J Am Med Dir Assoc. 2021;22(1):199‐203. 10.1016/j.jamda.2020.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Institute for the Advancement of Senior Care . COVID‐19 Survey for Senior Care LTC Facilities Q4; 2020. Accessed November 18, 2021. https://www.iadvanceseniorcare.com/covid‐19‐survey‐senior‐care‐ltc‐facilities‐results‐download‐4Q2020 [Google Scholar]
- 20. Canadian Institute for Health Information . Dementia in Canada: Dementia in Long‐Term Care. Accessed April 18, 2022. https://www.cihi.ca/en/dementia‐in‐canada/dementia‐care‐across‐the‐health‐system/dementia‐in‐long‐term‐care [Google Scholar]
- 21. Alzheimer’s Society. Thousands of People With Dementia Dying or Deteriorating – Not Just from Coronavirus as Isolation Takes Its Toll. 2020. Accessed September 12, 2021. https://www.alzheimers.org.uk/news/2020‐06‐05/thousands‐people‐dementia‐dying‐or‐deteriorating‐not‐just‐coronavirus‐isolation [Google Scholar]
- 22. Abbasi J. Social isolation—the other COVID‐19 threat in nursing homes. JAMA. 2020;324(7):619. 10.1001/jama.2020.13484 [DOI] [PubMed] [Google Scholar]
- 23. AARP . Is Extended Isolation Killing Older Adults in Long‐Term Care? Accessed August 23, 2021. https://www.aarp.org/caregiving/health/info‐2020/covid‐isolation‐killing‐nursing‐home‐residents.html [Google Scholar]
- 24. Van Der Roest HG, Prins M, Van Der Velden C, et al. The impact of COVID‐19 measures on well‐being of older long‐term care facility residents in The Netherlands. J Am Med Dir Assoc. 2020;21(11):1569‐1570. 10.1016/j.jamda.2020.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O'Caoimh R, O'Donovan MR, Monahan MP, et al. Psychosocial impact of COVID‐19 nursing home restrictions on visitors of residents with cognitive impairment: a cross‐sectional study as part of the Engaging Remotely in Care (ERiC) project. Front Psychiatr. 2020;11(1115). 10.3389/fpsyt.2020.585373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Howard R, Burns A, Schneider L. Antipsychotic prescribing to people with dementia during COVID‐19. Lancet Neurol. 2020;19(11):892. 10.1016/s1474-4422(20)30370-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cagnin A, Di Lorenzo R, Marra C, et al. Behavioral and psychological effects of coronavirus disease‐19 quarantine in patients with dementia. Front Psychiatr. 2020;11(916). 10.3389/fpsyt.2020.578015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bethell J, O'Rourke HM, Eagleson H, Gaetano D, Hykaway W, McAiney C. Social connection is essential in long‐term care homes: considerations during COVID‐19 and beyond. Can Geriatrics J. 2021;24(2):151‐153. 10.5770/cgj.24.488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cortés Zamora EB, Mas Romero M, Tabernero Sahuquillo MT, et al. Psychological and functional impact of COVID‐19 in long‐term care facilities: the COVID‐A study. Am J Geriatric Psychiatry. 2022;30(4):431‐443. 10.1016/j.jagp.2022.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Health Quality Ontario . Measuring up 2015: A Yearly Report on How Ontario’s Health System is Performing. Accessed May 2, 2022. http://www.hqontario.ca/portals/0/documents/pr/measuring‐up‐2015‐en.pdf [Google Scholar]
- 31. Lombardo FL, Salvi E, Lacorte E, et al. Adverse events in Italian nursing homes during the COVID‐19 epidemic: a national survey. Front Psychiatry. 2020;11:578465. 10.3389/fpsyt.2020.578465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mackenzie CS, Peragine G. Measuring and enhancing self‐efficacy among professional caregivers of individuals with dementia. Am J Alzheimer's Dis Other Dementias. 2003;18(5):291‐299. 10.1177/153331750301800507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gurnik M, Hollis‐Sawyer LA. Empowering assisted living front‐line care staffs to better care for Alzheimer’s and dementia residents. Ageing Int. 2003;28(1):82‐97. 10.1007/s12126-003-1017-5 [DOI] [Google Scholar]
- 34. Zimmerman S, Williams CS, Reed PS, et al. Attitudes, stress, and satisfaction of staff who care for residents with dementia. Gerontologist. 2005;45(suppl_1):96‐105. 10.1093/geront/45.suppl_1.96 [DOI] [PubMed] [Google Scholar]
- 35. Institute of Medicine (US) . Committee on the adequacy of nursing staff in hospitals and nursing homes. Staffing and quality of care in nursing homes. In: Wunderlich GSSF, Davis CK, eds. Nursing Staff in Hospitals and Nursing Homes: Is It Adequate? National Academies Press; 1996. [PubMed] [Google Scholar]
- 36. Li Y, Temkin‐Greener H, Shan G, Cai X. COVID‐19 infections and deaths among Connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68(9):1899‐1906. 10.1111/jgs.16689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Figueroa JF, Wadhera RK, Papanicolas I, et al. Association of nursing home ratings on health inspections, quality of care, and nurse staffing with COVID‐19 cases. JAMA. 2020;324(11):1103‐1105. 10.1001/jama.2020.14709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Abrams HR, Loomer L, Gandhi A. Characteristics of U.S. nursing homes with COVID‐19 cases. J Am Geriatr Soc. 2020;68(8):1653‐1656. 10.1111/jgs.16661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Brown KA, Jones A, Daneman N, et al. Association between nursing home crowding and COVID‐19 infection and mortality in Ontario, Canada. JAMA Intern Med. 2021;181(2):229. 10.1001/jamainternmed.2020.6466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Quigley DD, Dick A, Agarwal M, Jones KM, Mody L, Stone PW. COVID‐19 preparedness in nursing homes in the midst of the pandemic. J Am Geriatr Soc. 2020;68(6):1164‐1166. 10.1111/jgs.16520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bergman C, Stall NM, Haimowitz D, et al. Recommendations for welcoming back nursing home visitors during the COVID‐19 pandemic: results of a Delphi panel. J Am Med Dir Assoc. 2020;21(12):1759‐1766. 10.1016/j.jamda.2020.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ouslander JG, Grabowski DC. COVID‐19 in nursing homes: calming the perfect storm. J Am Geriatr Soc. 2020;68(10):2153‐2162. 10.1111/jgs.16784 [DOI] [PubMed] [Google Scholar]
- 43. Estabrooks CA, Straus SE, Flood CM, et al. Restoring trust: COVID‐19 and the future of long‐term care in Canada. FACETS. 2020;5(1):651‐691. 10.1139/facets-2020-0056 [DOI] [Google Scholar]
- 44. Ontario Ministry of Long‐Term Care . Long‐Term Care Staffing Study. 2020. Accessed March 28, 2022. https://files.ontario.ca/mltc‐long‐term‐care‐staffing‐study‐en‐2020‐07‐31.pdf [Google Scholar]
- 45. Liu M, Maxwell CJ, Armstrong P, et al. COVID‐19 in long‐term care homes in Ontario and British Columbia. Can Med Assoc J. 2020;192(47):E1540‐E1546. 10.1503/cmaj.201860 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


