Abstract
Background and Aim
The COVID‐19 pandemic has significantly impacted human lives across the world. In a country like India, with the second highest population in the world, impact of COVID‐19 has been diverse and multidimensional. Under such circumstances, vaccination against COVID‐19 infection is claimed to be one of the major solutions to contain the pandemic. Understanding of Knowledge, Attitude and Practice (KAP) measures are essential prerequisites to design suitable intervention programs. This paper examines the different KAP factors in Indians towards their decision of vaccine uptake.
Method
An online questionnaire was administered to Indian respondents. (Pilot study: n = 100, Main study: n = 221) to assess their existing knowledge on COVID‐19 infections and vaccination, attitude and intentions towards COVID‐19 vaccines and their decision towards COVID‐19 vaccine uptake.
Result
The findings highlighted that existing knowledge on COVID‐19 infections and vaccination directly impacted their attitude and intention towards vaccination. The attitude and intention towards COVID‐19 vaccines directly impacted their practice of undergoing COVID‐19 vaccination. Further, there was a statistically significant and considerably large indirect effect of existing knowledge on COVID‐19 infections and vaccination on the practice of undergoing COVID‐19 vaccination through attitude and intention towards the vaccine. There was no direct effect of Knowledge (existing knowledge on COVID‐19 infections and vaccination) on Practice (decision to undergo COVID‐19 vaccination). Therefore, Attitude and intention towards COVID‐19 vaccine is the primary mediator between Knowledge (existing knowledge on COVID‐19 infections and vaccination) and Practice (decision to undergo COVID‐19 vaccination).
Conclusion
Participants decision towards COVID‐19 vaccination decisions are strongly related to their attitude and intentions that confirms the strong role of attitude towards success of COVID‐19 vaccination programme. Therefore, ‘person‐centric’ attitude based positive intervention strategies that links their prior knowledge on COVID‐19 infections and vaccination must be designed for greater vaccine acceptance amongst Indians.
Keywords: attitude, COVID‐19, India, knowledge, practice, vaccination
Highlights
Knowledge is the key to successful COVID‐19 vaccination drive which is deemed to be essential for ending the global pandemic.
Knowledge positively affects attitude and attitude positively impacts COVID‐19 vaccine uptake decision.
Attitude completely mediates the relationship between respondent's knowledge and their decision of COVID‐19 vaccination.
Specific awareness campaigns towards COVID‐19 vaccination aimed at attitude restructuring are needed.
1. INTRODUCTION
The Coronavirus (CoV) belongs to a family of viruses causing illness that range from acute infection to severe pneumonia, respiratory distress and even death. 1 This group was grossly overlooked until the outbreak of Severe acute respiratory syndrome and Middle East respiratory syndrome. Research work on understanding its virulence and infectivity was underway when, in 2019, a novel strain of coronavirus was identified in Wuhan city of China and nomenclated as SARS‐COV2, COVID‐19 by World Health Organization (WHO). 2 Shortly, it spread to neighbouring cities and countries resulting in an outbreak. The WHO called it a global public health emergency and finally declared a pandemic. 3
The scale of events resulted in an international lockdown and stringent screening of travellers. Regardless of measures, the spread was significant for most countries including India. The first case of COVID‐19 was documented on 27 January 2020 in Kerala. 4 It soon spread to other states causing health complications and mortality. With a population of 1.3 billion and limited health infrastructure, the already overburdened healthcare system saw unimaginable mortality figures 5 and a high infection rate amongst frontline healthcare workers. Though health is a state subject, the central government actively worked to contain the contagious COVID‐19 infections during the first wave, resulting in controlled infection. 6
The second wave of COVID‐19 reported higher infection load, morbidity and mortality figures globally. 7 In India, the second wave of COVID‐19 infection peaked in 2021, with notable incidence and prevalence of infection, that hit many households irrespective of their financial and socio‐economic status. India is one of the top five countries in the world to be severely impacted, with the highest disease incidence being reported in the month of April 2021. Apparent lack of coordination and consensus amongst various health agencies and the current government policies contributed to significant mortality figures.
The only logical way to deal with this current menace is mass vaccination across all age groups. 8 Mass vaccination can lead to herd immunity without the requirement of a significant population being infected. 9 As relevant research on vaccine safety, efficacy, efficiency and duration of effectivity are still on, numerous roadblocks and vital linkages pertaining to herd immunity are complex and remain unanswered. Nonetheless, mass vaccination seems to be one of the most viable options to contain mortality statistics of COVID‐19 pandemic.
Vaccination process in India began with the frontline health workers receiving vaccine doses. 10 The initial rollout targeted the vulnerable population that included senior citizens (>60 years) and middle aged with comorbidities (45–60 years). Presently, anyone above 18 years can receive immunisation.
For any vaccination programme to be successful, it is recommended that the programme must be credible. Besides, higher competency of the officials responsible for securing vaccine doses, judicious vaccine distribution, effective management, convincing the common population regarding safety and efficiency, as well as motivating them for vaccine acceptance on their turn holds equal importance. 11 Since there is a growing demand for coronavirus vaccine worldwide, the question of manufacturing/procuring adequate supply and further distribution of requisite vaccines doses inevitably is a priority issue. The Indian government initiatives provide free vaccination to people, reducing the chances of misuse.
WHO has identified anti‐vaccination sentiments as a leading hurdle encountered globally during vaccine awareness and implementation. 12 Informal information overload coupled with misinformation has created a negative perception. 11 Vaccine awareness campaigns thus strive hard to win itself against the turbulent anti‐vaccination sentiments working amongst certain groups that don't want to get vaccinated. The key factor determining the success of COVID‐19 vaccination strategy in India is the effectiveness of vaccine awareness campaigns to overcome the prevailing anti‐vaccination sentiments.
On one side, while people across the world waited for an efficient vaccine to curb the menace, emergence of vaccine hesitancy during implementation is worrisome. Understanding of knowledge and attitude of the common mass regarding vaccination initiatives shall aid public health experts to create specific outcome‐based vaccine awareness strategies. 13 It will help to reduce as well as limit disease incidence.
The current study has been undertaken with the aim to explore the role of knowledge and attitude of adult Indians (>18 years) towards COVID‐19 vaccination that affects their vaccine uptake decisions.
The organization of the subsequent sections of this paper is as follows. The next section describes the hypotheses based on the underlying relationship between knowledge, attitude and practices towards COVID‐19 vaccine uptake. Subsequent sections describe the methodology, results and discussion in details. Finally, the conclusion and limitations of the study has been documented.
2. PROPOSED CONCEPTUAL FRAMEWORK AND HYPOTHESIS FORMULATION
2.1. Existing knowledge on COVID ‐19 infections and vaccines
The onset of pandemic, while, crippled the world on one side, it also opened newer vistas of research. Numerous researchers working on COVID‐19 pandemic covered important thrust areas that included technical, biological, sociological, economic, psychological and a host of other interdisciplinary fields linked to COVID‐19 pandemic. A number of studies across different countries have been undertaken to understand the relationship of KAP with vaccine uptake. The importance of behavioural interventions for general public and redesigning health policy dimensions due to differential Knowledge, Attitude and Practices have been documented by researchers across different countries proposing specific campaigns affecting vaccine uptake decisions. 14 , 15 , 16 , 17 In Indian context, adequate knowledge on COVID‐19 disease affected their vaccine uptake decision. 18 From all these findings, it is thus clear that knowledge about COVID‐19 infections and its severity might contribute towards the decision of vaccine uptake.
Information from multiple sources like electronic, print, social media and other discussions have built some knowledge regarding COVID‐19 infection, its severity and vaccine efficacy. Many studies have indicated the role of social media 19 to convince people towards vaccination, that reduce the chances of infection. 20 Also, vaccinated people encounter less severity in situations of infection. Most importantly, vaccination is recommended by doctors and government agencies and it is believed that pandemic can be controlled only through vaccination measures. Therefore, it is hypothesised that existing knowledge on COVID‐19 vaccine shall significantly impact the attitude towards vaccination.
H1 Existing knowledge has an influence on the respondent's attitude to undergo COVID‐19 vaccination.
2.2. Attitude towards COVID‐19 vaccine and its uptake
Attitude, in common parlance, refers to the viewpoints of an individual towards any topic, that reflects their behavioural decision. 21 A review of literature has highlighted a relationship between attitude towards vaccine uptake and successful vaccination campaigns. 22 , 23
Current research on attitude and intention towards COVID‐19 vaccination has explored the negative predictors that create uncertainty and vaccine hesitancy. 24 They stressed on the importance of customised information for vulnerable and minority population. It needs outcome based evaluation for a successful COVID‐19 vaccination programme. Researchers in Malta and Jordan highlighted the importance of attitude on vaccine uptake and reflected on the need of group strategies with special reassurance to women and others regarding vaccine safety. 25 , 26 It is thus clear that for promoting positive attitude towards vaccination campaigns, personalised intervention addressing trust, hesitancy, efficacy, availability and transparency issues must be considered. For designing a customised public health initiative suitable for Indian people, structured intervention campaigns that highlight the benefits from vaccine uptake need to be told, based on the underlying attitude and intention of individuals. Thus the following hypotheses have been proposed.
H2 Positive attitude towards vaccine uptake influence respondent's decision to undergo COVID‐19 vaccination.
H3 Attitude mediates the relationship between respondent's knowledge and the decision to undergo COVID‐19 vaccination.
The proposed conceptual model linking the objectives has been illustrated in Figure 1A. It is hypothesized that knowledge on COVID‐19 infections and vaccination and attitude towards vaccine uptake has a relationship with the decision to participate in vaccination. The present analysis also tests the model (Figure 1A) using existing knowledge, attitude and practice (decision) as the measurement domains with a potential that attitude mediates the relationship between prior knowledge and practice of participating in vaccination drives (Figure 1B).
FIGURE 1.
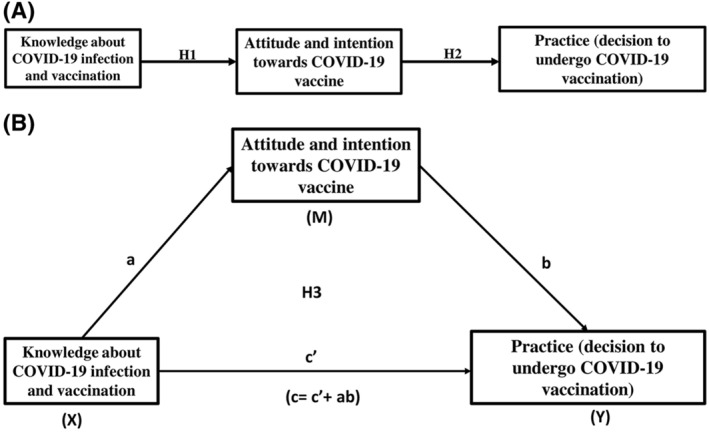
(A): The conceptual knowledge, attitude and practices Model (Source: Author's creation). (B): The proposed mediation model of knowledge, attitude and practices towards COVID‐19 vaccination (Source: Author's creation)
3. METHODOLOGY
3.1. Context
COVID‐19 infections in India during the first and second wave has created havoc in the lives of people. Due to the emergence of newer variants of COVID‐19 virus, the possibility of future waves cannot be ruled out. 27 As on today, the total number of cases stand at approximately 3,09,07,282 people, while the mortality statistics are approximately 410,784 people. Though the active rates of infection have somewhat dipped in India, the current active case load is approximately 432,778 people. Vaccination camps are being organised rigorously and till today around 381,467,646 people across varied age groups have been vaccinated. 28
3.2. Measurement instruments
A comprehensive literature review was done to explore the role of knowledge, attitude and practices on vaccine uptake amongst Indians. It was found that in Indian context, there is limited work on developing a specific scale that links knowledge, attitude and practices of individuals with vaccine uptake. Moreover, the existing scales do not operationalise the study constructs, as conceptualised by the researchers. Therefore, the questionnaire employed in the study was developed by modifying some of the items of the existing scale 29 and adding some new items on the basis of expert suggestions.
To assess the content validity of the questionnaire, a three step process was followed. 30 In the first step, the content for the items was established from reviewing available literature and discussion with domain experts. Secondly, this questionnaire was circulated to three subject matter experts that independently viewed the content of the scale and made required adjustments. Finally, the authors reviewed the content reformatted by the subject experts and made meaningful minimal changes in words to fulfil the original objective of the research question.
Initially, a pilot study with 100 participants was carried out to ensure that there was clarity in understanding the format and question/viewpoint specificity as asked in the questions. Feedback from respondents revealed that questionnaire length and choice of words/language was clear, well understood and concise.
The measurement instrument comprised of two sections. The first section consisted of a few screening questions for respondents related to information on COVID‐19 infection and vaccination in line with other studies. 29 , 31 Participants answered questions related to number of siblings in the household, COVID‐19 vaccine uptake, basic knowledge on eligibility for COVID‐19 vaccine, protective immunity and sources of information on COVID‐19 vaccination process (Table A‐1, Appendix).
The subsequent section comprised of items for measuring the constructs namely existing knowledge on COVID‐19 infections and vaccination, attitude and intention towards COVID‐19 vaccines and practice of COVID‐19 vaccine uptake. The construct of knowledge consisted of 8 items while attitude and practices construct, consisted of 5 items each. All these items were aligned to statements fulfiling requirements of Likert scale ranging from Strongly disagree (1), disagree (2), neither agree nor disagree (3), agree (4) and strongly agree (5) respectively. Details of constructs and items are mentioned in Table A‐2, Appendix.
3.3. Sampling framework
To check the research hypothesis based on the proposed conceptual model, a structured questionnaire was developed on topics linked to knowledge, attitude and practices of respondents towards COVID‐19 vaccine uptake as per availability norms in India. In view of social distancing norms and other restrictive measures, a web‐based survey was conducted spanning a period of 5 weeks from 1 May 2021. The inclusion criteria considered Indian participants who were above 18 years of age and agreed to record their observations on the subject mentioned. Non Probability convenient sampling was employed to collect data from respondents based on their availability. This technique is conventionally used by social science researchers in situations of financial and time constraints for improvisation of the resources needed for conducting research.
The minimum sample size required to detect mediation effect, depends on the test employed for detecting mediation and the magnitude of the two paths which constitute the indirect effect. In this study, accelerated biased‐ corrected Bootstrap test has been employed for examining the presence of mediated effect. In addition, the existing literature reveals that the magnitude of the paths from knowledge to attitude and attitude to behaviour is not small. For this method, a minimum sample size between 34 and 148 is deemed to be adequate 32 for various combinations of path sizes comprising the indirect effect when none of the two paths are small. Hence, a sample size of 200 was considered adequate for further data collection and analysis. The final questionnaire was administered to 300 respondents online out of which 221 respondents completed it indicating approximately 74% response rate.
Details about sociodemographic attributes of respondents are presented in Table 1.
TABLE 1.
Socio‐economic details of respondents
| Parameters | Number of respondents |
|---|---|
| Age | |
| 18–45 years | 201 |
| 45–60 years | 11 |
| >60 years | 9 |
| Gender | |
| Male | 121 |
| Female | 100 |
| Transgender | NIL |
| Education | |
| No formal education | NIL |
| High school | 15 |
| Bachelor's degree | 163 |
| Post‐ graduation/Professional degree | 43 |
| Monthly income | |
| <50,000 INR | 139 |
| 50,001–250,000 INR | 73 |
| 250,001–500,000 INR | 7 |
| >500,001 INR | 2 |
| Residence | |
| Rural | 81 |
| Urban | 140 |
| COVID‐19 vaccination status | |
| Yes (1st dose) | 34 |
| Yes (2nd dose) | 16 |
| No | 171 |
4. ETHICAL CONSIDERATION
All measures to maintain ethics were considered. Prior to undertaking the study, the research protocol was reviewed and approved by the relevant Institutional Ethics Committee. Authors also obtained official permission from the study sites. The introductory page of the questionnaire described the purpose, objectives and approximate duration of the study and had a section on informed consent from participants. Upon agreement, they could proceed for the subsequent sections. Participants' identities were accessible only to the researchers and assurances of anonymity were provided to the participants.
5. DATA ANALYSIS PROCEDURES
For the purpose of data analysis, Structural Equation Modelling (SEM) has been employed, which encompasses two models – measurement model and structural model. In the first step of this procedure, the latent constructs are measured utilising the technique of (CFA) Confirmatory Factor Analysis with the aim of assessing their unidimensionality, validity and reliability of the measurement model. Once the measurement model has attained an acceptable validity and reliability, path analysis is performed using the structural model.
- CFA : CFA has been implemented in R‐Studio to check the measurement model validity and reliability of the proposed model. The following categories of fit indices were taken into account in this study: Chisq/df, parsimony‐corrected fit (root mean square error of approximation [RMSEA]), (standardized root mean square residual [SRMR]) and comparative fit (Tucker–Lewis fit index [TLI], comparative fit index [CFI]). The following threshold values were employed to indicate model fit: Chisq/df ≤3 as mentioned by 33 TLI and CFI ≥0.95 as illustrated by, 34 , 35 RMSEA ≤0.08 and SRMR ≤0.08 as given by. 34 The prescribed cut off value of composite reliability (CR) which indicates adequate internal consistency is 0.7. 36 The internal consistency and test‐ retest reliability of the scales employed, was evaluated. For assessing the internal consistency, the CR as well as Cronbach's alpha (α) were computed. An internally consistent scale should exhibit a Cronbach's alpha (α) value of 0.6–0.7. 37 , 38 For examining the test‐ retest reliability of the measuring instrument, it was administered for a second time to a sub‐set of the 50 respondents who were part of the original survey. A gap of 2 weeks was maintained between the original and the subsequent survey since a long interval could lead to changes in degree of knowledge or attitude of the respondents that would in turn affect the behavioural practice where as a very short interval could result in recall bias. 39 Intra‐class correlation (2,1) (ICC) coefficient was calculated to judge the test‐retest reliability of the scales. 40 A minimum ICC value of 0.4 implies adequate test retest reliability. 41 , 42 Further evaluation of construct validity constituted of an appraisal of convergent validity and discriminant validity. The assessment of convergent validity is done by inspecting the item factor loadings and also their corresponding statistical significance. Furthermore, an appraisal of the factors' average variance extracted (AVE) and construct reliabilities (CRs) is undertaken. Convergent validity was implied by an item factor loading ≥0.5 and p < 0.05 as mentioned by, 36 AVE ≥0.5, and CR ≥ 0.7 as given by. 43 AVE and CR values were computed using the following formulas given by. 43
Discriminant validity has been assessed using a chi‐square difference test. 44 In this method the constructs are introduced in pairs of two. This test involves fitting two models, first one in which the two constructs under consideration are not correlated and a second one in which they are correlated. The significance of the difference of the Chi‐square statistics obtained from these two models implies the presence of discriminant validity among the constructs. For each pair of these latent constructs, this particular process is further repeated.
Models were updated on the basis of estimated values of factor loadings and modification indices (MIs) while preserving the congenericity of the measurement model within the theoretical framework. Items with factor loadings <0.5 were contemplated for removal. 36 The current study used MI values for spotting potential cross‐loading items, 36 but did not fix any specific cut‐off values.
Path Analysis: Path analysis has been carried out using Lavaan package in R‐Studio 4.0.4.
6. RESULTS
6.1. General profile of the participants
The results indicate that approximately 55% of the respondents were males while 45% females. The majority of the participants belonged to the age group of 18–45 years (approximately. 91%). Around 74% of respondents were graduates and resided in urban area (Table 1). When probed regarding vaccine uptake, a majority of respondents (78%) indicated that they have not been vaccinated yet, while about 15% of the population received the first dose of vaccine and around 7% received both the doses. An important factor towards this huge unvaccinated population can be attributed to the non‐availability of vaccines along with the priority grouping from the population by government. Vaccine hesitancy and confusions on future implications were also noted.
6.2. Basic understanding about COVID‐19 vaccination
On being probed regarding the source(s) of information for COVID‐19 vaccination process, total response analysis revealed around 68% responses mentioning social media as an important tool, followed by electronic media and government agencies (49%, 41%) respectively (Figure 2A).
FIGURE 2.
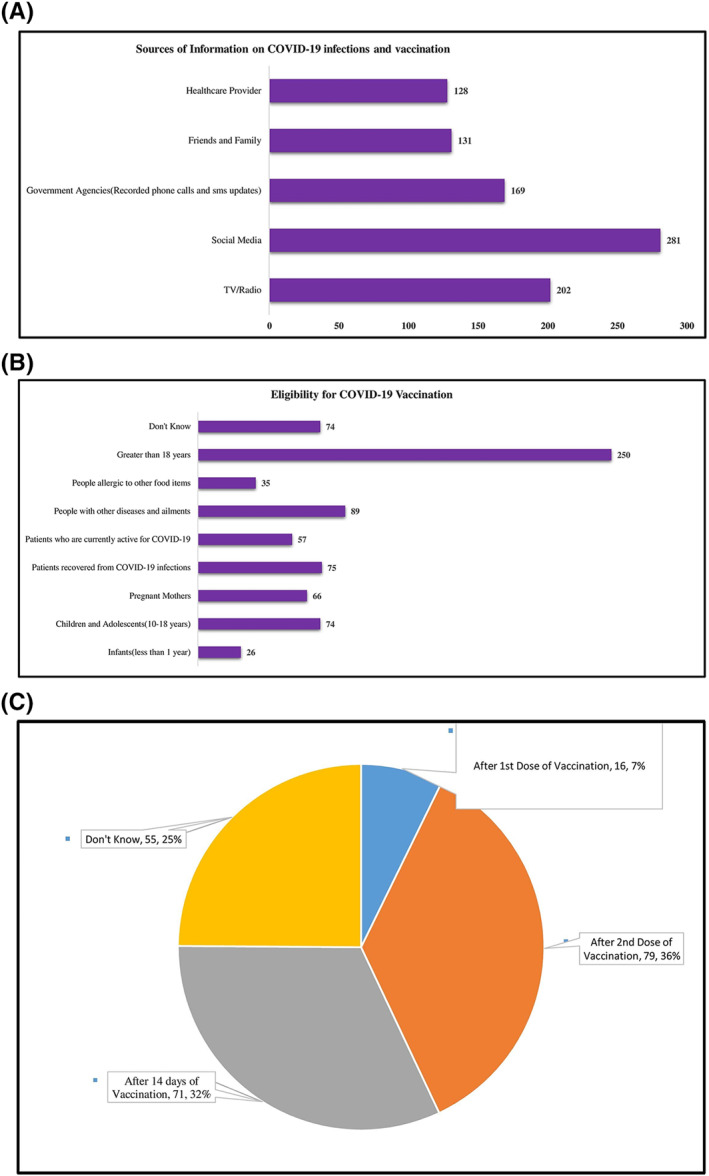
(A) (B) (C) Basic understanding about COVID‐19 vaccination. (A) Sources of information on COVID‐19 infections and vaccination. (B) Basic knowledge on eligibility for COVID‐19 vaccination. (C) Perception on immunity after COVID‐19 vaccination
In order to ascertain the basis awareness of people towards phased roll out of vaccines across different categories, opinions on vaccination eligibility age groups/categories revealed around 60% responses in favour of anyone above 18 years of age. However, about 18% of responses revealed that eligibility conditions for vaccination were unknown (Figure 2B).
Knowledge on COVID‐19 vaccination immunity revealed that 36% of respondents perceived immunity after both the doses of vaccination, although there is a quarter of population (25%) who are not aware of the same (Figure 2C).
7. MEASUREMENT MODEL OF THE CONSTRUCT
The initial model (M1) for this study was specified as a reflective measurement model that constituted of three first‐order latent constructs, 18 items and three inter‐factor correlations. M1 had a poor model fit, as demonstrated by all goodness of fit indices. To improve model fit, M1 was modified following an iterative process which is described below.
Initially, five items (K1, K2, K3, K4, K7) of knowledge construct and one item (A2) of Attitude construct were removed because the factor loadings for these items were below the thresh hold level of 0.5. 36 From the resulting model again K8 was dropped due to low factor loading. After the removal of these 7 items, A5 was found to cross‐load on Practice based on an MI value of 12.404. Therefore, A5 was dropped, leaving attitude with three items.
Overall, 8 items were removed from the three factors. The resulting model (M2) was a three‐factor model comprising of two items under knowledge, three items under attitude and five items under practice (Table 2). This model exhibits a good model fit: Chisq/df = 1.9; RMSEA = 0.061; SRMR = 0.037; CFI = 0.97; TLI = 0.958.
TABLE 2.
Final Items and constructs
| Constructs | Items |
|---|---|
| Knowledge (existing knowledge on COVID‐19 infections and vaccination) | COVID‐19 vaccines are approved and recommended by doctors and government agencies.(K5) |
| COVID‐19 vaccines reduce my chances of infection. (K6) | |
| Attitude (attitude and intention towards COVID‐19 vaccine) | When my turn of vaccination comes, I will take the COVID‐19 vaccine (A1) |
| I Am willing to take the COVID‐19 vaccine even if I am asked to pay for it (A3) | |
| According to me, COVID‐19 vaccines are an effective response to corona pandemic (A4) | |
| Practices (decision to undergo COVID‐19 vaccination) | I Believe there are many benefits of COVID‐19 vaccine(P1) |
| I Believe taking COVID‐19 vaccine is a societal responsibility (P2) | |
| I Believe there is sufficient data that favours COVID‐19 vaccination (P3) | |
| I Believe the COVID‐19 vaccine is the solution to deal in pandemic since it is recommended by doctors and scientists (P4) | |
| Death numbers are high in COVID. Taking vaccine is the only solution (P5) |
Table 3 presents the results of the confirmatory factor analysis of the final model (M2). The CR values exceed the prescribed cut off of 0.7 indicating that all the three latent constructs exhibit a satisfactory level of internal consistency. 36 Internal consistency was also assessed through Cronbach's alpha (α) and the values obtained were 0.64, 0.7 and 0.81 for knowledge, attitude and practice scales respectively which exceeds the minimum threshold value as prescribed. 37 , 38 The test‐ retest reliability of each of the three scales was established as the calculated ICC values for knowledge, attitude and practice are 0.53,0.76 and 0.89 which satisfies the adequate test‐ retest reliability criteria as specified. 39 Convergent validity is also established since all the item factor loadings were above 0.5 with statistically. significant values and the Average Variance Extracted (AVE) for each of the three latent constructs exceeded 0.5 as given by. 36
TABLE 3.
Measurement model
| Construct | Item | Factor loading | CR | AVE |
|---|---|---|---|---|
| Knowledge | K5 | 0.74 | 0.7 | 0.5 |
| K6 | 0.65 | |||
| Attitude | A1 | 0.66 | 0.7 | 0.5 |
| A3 | 0.60 | |||
| A4 | 0.78 | |||
| Practice | P1 | 0.77 | 0.7 | 0.5 |
| P2 | 0.67 | |||
| P3 | 0.61 | |||
| P4 | 0.81 | |||
| P5 | 0.59 |
The results of Chi‐square difference test for assessing discriminant validity is presented in Table 4. For each pair of constructs, the chi‐square difference between constrained and freely estimated models was high and significant at 1% level which indicates that there is discriminant validity among the scales employed for measuring the constructs.
TABLE 4.
Discriminant validity: Chi‐square difference fest
| Construct 1 | Construct 2 | Chi‐square of constrained model | Df | Chi‐square of free model | df | Chi‐square difference |
|---|---|---|---|---|---|---|
| Knowledge | Attitude | 108.09 | 5 | 3.22 | 4 | 104.87 a |
| Knowledge | Practice | 111.2 | 14 | 16.21 | 13 | 94.99 a |
| Attitude | Practice | 229.22 | 20 | 40.57 | 19 | 188.65 a |
Statistical significance at 1% level.
8. STRUCTURAL MODEL
The analysis that has been presented in the previous section has successfully established the validity, reliability and unidimensionality of the constructs. Therefore, at this stage(SEM) Structural Equation Model has been implemented for testing the hypotheses. In Structural Equation Modelling, adjusted R 2 of an outcome variable is the percentage of variance in that outcome variable which is explained by the entire set of predictors included in the SEM model under consideration. The adjusted R 2 values of the two endogenous variables in the proposed SEM model, namely, attitude and practice are 0.783 and 0.989 respectively. This indicates that approximately 78% and 99% of variances of the two dependent variables (attitude and practice) are explained by the predictor variables under consideration. As at the time of the study, the vaccination drives were intensively initiated in the country, people having positive attitude towards vaccination were more inclined towards vaccine uptake which may have resulted in a higher adjusted R 2 value for the construct ‘practice’. The results of hypothesis testing are shown in Table 5.
TABLE 5.
Hypothesis testing
| Construct | Path | Construct | Estimate | S.E. | C.R. | p | Result |
|---|---|---|---|---|---|---|---|
| Attitude | <‐‐‐ | Knowledge | 0.612 | 0.090 | 6.818 | 0.000 | Significant |
| Practice | <‐‐‐ | Attitude | 1.828 | 0.569 | 3.211 | 0.001 | Significant |
From the results in Table 5 it is evident that the first two hypotheses are supported because the regression path coefficients are significant at 1% level in each case.
9. MEDIATION ANALYSIS
Mediation analysis has been performed using the bootstrap method. 45 , 46 The magnitude and confidence interval of the effect size has been computed using a bootstrap sample of 1000 and a bias corrected and accelerated 95% confidence interval (Figure 3). The results obtained are presented in Table 6 .
FIGURE 3.
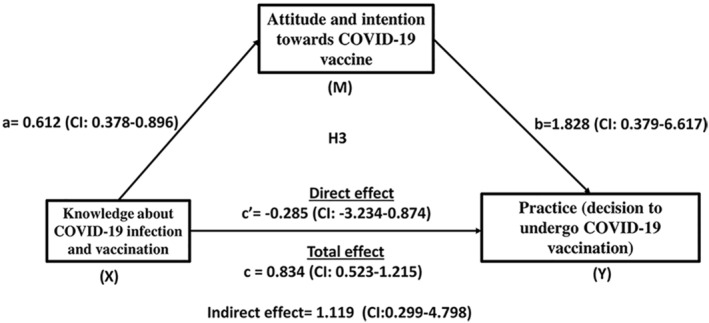
Mediation analysis of attitude in relation to knowledge and practice towards COVID‐19 vaccine. Bootstrap sample of 1000 has been used to calculate the magnitude and confidence interval. The confidence interval has been accelerated to 95%. The X to M path denotes the effect of knowledge about COVID‐19 infection and vaccination on attitude towards COVID‐19 vaccine. The M to Y path denotes the effect of attitude on their decision of COVID‐19 vaccine uptake. The direct effect refers to the effect of knowledge about COVID‐19 infections and vaccination on decision for vaccination uptake by adjusting for attitude. The total effect is the sum total of the direct effect of existing knowledge about COVID‐19 infection and vaccination on practice (decision of COVID‐19 vaccine uptake) and indirect effect of existing knowledge about COVID‐19 infection and vaccination on practice (decision of COVID‐19 vaccine uptake) via attitude and intention towards COVID‐19 vaccine
TABLE 6.
Mediation effects
| Indirect effect | Direct effect | |
|---|---|---|
| Effect size | 1.119 | −0.285 |
| Lower confidence interval | 0.299 | −3.234 |
| Upper confidence interval | 4.798 | 0.874 |
From the results shown in Table 6, it is evident that the indirect effect is significant because zero is not included in the 95% confidence interval of the estimate. Therefore, attitude mediates the relationship between knowledge about COVID‐19 vaccine and the decision to take the vaccine. Furthermore, apart from testing the indirect effect significance, 47 the categorisation of the effect sizes into small, medium and large was done following the usual standards. 48 As the effect size of the indirect effect has exceeded the value of 0.5, the indirect effect magnitude is thus considered to be large. In contrast, the direct effect cannot be considered to be statistically significant because zero is already included in the 95% confidence interval. 47 Therefore, it can be concluded that there is presence of complete mediation. It means that there is no sufficient evidence to prove that knowledge related to COVID‐19 vaccine is associated with people's decision to take the vaccine independent of its association with attitude.
10. DISCUSSION
In the absence of proven and tested treatment regimen, mass vaccination remains pivotal to control COVID‐19 infection. 8 Successful vaccination campaign is directly dependent upon two factors‐ adequate availability of vaccines and the acceptance of vaccine amongst general population. Optimization of vaccine production and supply depends on a gamut of factors such as nationalistic drive, political willingness, economic strength and a strong scientific as well as research base, coupled with levels of production capabilities. The focus on vaccine outreach activities is important in relation to a definite timeframe of delivery keeping in mind the anticipation of ‘‘waves” and population involvement. A number of vaccine candidates have been researched upon and identified to have potential efficacy. Many of them have been approved by countries to be used in their vaccination regimen. In India, the government has currently approved Covishield, Covaxin and Sputnik V. A few others are in the process of finalisation and implementation in vaccination programs. Although the conventional vaccines and vaccination drives are operational as a part of the greater vaccination strategy, in India, the prevalence of a completely new disease such as COVID with lesser known cause and poor prognosis have created apprehensiveness and anxiety amongst common people. Moreover, vaccine availability, roll out process, distribution modes and channels have posed serious questions on the mind‐set of respondents that are interlinked with vaccine acceptance. 49 It is thus imperative to gauge the general population's knowledge, attitude and practices on taking up COVID‐19 vaccine.
The current research intends to identify the different underlying concepts related to knowledge and attitude that determines the practical decision of people towards acceptance of COVID‐19 vaccines. To explore and further progress on the research question of this study, the conceptual model has been specifically aligned to that of theory of planned behaviour and trans‐theoretical model.
Numerous findings identifying relationships on KAP factors linked with COVID‐19 vaccination has been instrumental in proposing public health initiatives that provide community based strategic behavioural interventions and better protection from such pandemics in future. 50 , 51 Identification of barriers towards vaccine hesitancy and addressing trust are integral for mass acceptance. 52 Vaccine literacy directly affects vaccine acceptance. 29 It is especially important and relevant in current circumstance where the country is undergoing the crisis of a second wave and possibly awaits another spike of cases in the ‘third’ wave of COVID‐19 infections. Therefore, knowledge has a crucial role towards successful vaccination programs.
The major findings of this research highlighted that existing knowledge on COVID‐19 infections and vaccination process significantly impacted the attitude and intention of participants concerning COVID‐19 vaccination. The prior knowledge and foresight of respondents are decisive factors for vaccination. Our results identified a considerable population being not aware of vaccination criteria. Previous studies have also reported KAP measures being used to study vaccination outcomes. 53 Knowledge discrepancies in general population on COVID‐19 infection and vaccination has also been reported. 16 , 17 Additionally, under reporting of mortality cases coupled with wrong information, misinterpretation, ambiguity and ignorance lessen disease concern, vaccine safety and increase reluctance for vaccination. 54 This demands knowledge dissemination backed by scientific evidence and use of language that is easily understood by all.
Attitude and intention are reflected in behavioural outcomes. 55 Awareness, foresight and belief system on vaccine efficacy impacts attitude which is reflected in the practice of preventive behaviours. Previous studies have identified the relationship between attitude and individual's choice to participate in vaccination drives. 22 , 24 Factors influencing attitude influence equitable vaccine uptake. 25 A strong relationship is thus highlighted between respondent's attitude towards COVID‐19 vaccination drives and these results support the previous research findings. 56 , 57 In consistent with these studies, we have also reported that positive attitude is directly related to the decision to vaccinate against COVID‐19 infection. Therefore, positively motivated participants are willing to participate in COVID‐19 vaccination drives.
A relationship of KAP factors associated with COVID‐19 vaccination is well established. 58 However, how prior knowledge on COVID‐19 infections and vaccines could affect the practice, that is vaccination decisions indirectly via attitude is still not commonly known. 14 In our study, knowledge on COVID‐19 infection and vaccination has been found to considerably affect the intention to take COVID‐19 vaccine through attitude, but prior knowledge on COVID‐19 infection and vaccination directly does not impact the vaccination decisions independent of its association with attitude. Attitude, therefore, can be considered to be the primary mediator between existing knowledge and practice of vaccination for COVID‐19. These outcomes are cornerstone to public health awareness programs that must aim at bringing about a positive transformation of attitude amongst the general population. In this regard, a deeper understanding of the KAP measures associated with COVID‐19 vaccination intention shall help the public health scientists and officials to design personalised key strategic initiatives that will bring about positivity towards vaccination campaigns.
11. CONCLUSION
During any public healthcare emergency or pandemic, it is important to practice behavioural decisions that are precautionary in nature. Successful vaccination programme outcomes are reflected in the form of herd immunity at the population level. The rate of transmission can be controlled through vaccination strategies involving the greater community. For the success of the same, a strong understanding of knowledge, attitude and practice measures of the general public towards vaccination uptake, needs to be understood. Our study has observed that people with knowledge about COVID‐19 infections understand the effectivity and importance of vaccines. Furthermore, this study has identified an important relationship between knowledge and attitude that is reflected in practice. Though knowledge on COVID vaccination directly does not affect the preventive practice measures and vaccination participation, it indirectly affects the practice via attitude that has a mediating role in this relationship. These findings shall be pivotal for healthcare officials and public health experts to work on community based intervention strategies.
12. RECOMMENDATIONS
Vaccination against COVID‐19 infection is a time consuming, resource driven project which has its own challenges as it percolates within the larger population. It is prudent to thus incorporate vaccination oriented goals within our healthcare planning objectives. Furthermore, there is also a need to develop effective outreach programmes in the public domain through strategic initiatives. Use of local language and integration of traditional customs and practices can help overcome the issues of vaccine hesitancy.
13. SUGGESTIVE ACTIONS
India, with its huge population and overstretched health system needs efficient public health initiatives to enhance vaccination numbers and curtail the burden of pandemic that is directly affecting treatment regimen of conventional diseases. It is important to explore the causes of vaccine hesitancy or refusal amongst general people. Recognising them shall help to overcome such hesitancy barriers. The differential vaccine acceptance rate can also be attributed to ground knowledge about COVID‐19 infection, vaccination schedule, eligibility and all other associated information which affects their attitude regarding vaccination. It will be prudent if specific vaccine awareness programs and intervention strategies be designed based upon attitude clusters with specific focus to people belonging to negative and sikken attitude regarding vaccination drives. With emergence of newer waves and variants, it is difficult to know about transmission rate, severity or fatality prospects in a population. It is thus imperative to constantly monitor the immune system of people, especially the immune‐compromised individuals and vaccination seems to be the only solution. India needs a specific vaccination management strategy, more so, with the recent signs of vaccine hesitancy and complacency setting in.
14. LIMITATIONS
Though we tried our best to address all possible rooms for biases, this study has a few limitations, aiding in further research. The study design is cross sectional in nature. With the ongoing spell of COVID‐19 infection and eligibility criteria for vaccination, the response of vaccine acceptance shall be varied. Thus, information on exact cause of vaccine hesitancy is difficult to conclude. Secondly, while we tried our best to include respondents from all socio‐economic sections, but a stratified random sampling technique was not utilised. Thus, it is difficult to claim that the sample under study is a representative of the Indian population. Our study has observed the strength or direction of the indirect effect of COVID‐19 vaccine related knowledge on vaccine intention through attitude. This relationship may however vary across educational levels, income levels, geographical location etc. However, this study has not examined such conditional indirect effects. Future studies may conduct such moderated mediation analyses to gain further insights into the interrelationship between knowledge, attitude and practice towards COVID‐19 vaccination. This will help in identifying the various dimensions and variables associated with vaccine hesitancy and refusal.
CONFLICT OF INTEREST
No conflict of interest declared.
ETHICAL STATEMENT
This research has been carried out considering the appropriate ethical framework and as per internationally accepted standards for research practice. The participants were explained regarding the aim of the study and purpose of data collection and only those were considered that agreed to the same.
AUTHOR CONTRIBUTIONS
Ms. Mitali Sengupta, Dr. Arijit Roy and Dr. Indraneel Mukhopadhyay significantly contributed towards conceptualisation and designing of the study. Data analysis was done by Mitali Sengupta and Dr. Smita Dutta. Interpretation of results and discussions were done by Mitali Sengupta, Dr. Smita Dutta, Dr. Arijit Roy, Dr. Indraneel Mukhopadhyay and Dr. Satyajit Chakrabarti. Manuscript preparation was done by Ms. Mitali Sengupta and critical revisions and addition of intellectual content was done by Dr. Satyajit Chakrabarti, Dr. Indraneel Mukhopadhyay and Dr. Arijit Roy.
Supporting information
Supporting Information
ACKNOWLEDGEMENTS
The authors would like to thank University of Engineering and Management, Kolkata for the necessary infrastructure for conducting the research. MS would like to thank the other team members for constructive feedback and discussions.
Sengupta M, Dutta S, Roy A, Chakrabarti S, Mukhopadhyay I. Knowledge, attitude and practice survey towards COVID‐19 vaccination: a mediation analysis. Int J Health Plann Mgmt. 2022;37(4):2063‐2080. 10.1002/hpm.3449
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Pal M, Berhanu G, Desalegn C, Kandi V. Severe acute respiratory syndrome Coronavirus‐2 (SARS‐CoV‐2): an update. Cureus. 2020;12(3):e7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Srivastava S, Banu S, Singh P, Sowpati DT, Mishra RK. SARS‐CoV‐2 genomics: an Indian perspective on sequencing viral variants. J Biosci. 2021;46(1):1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The Best Time to Prevent the Next Pandemic Is Now: Countries Join Voices for Better Emergency Preparedness [Internet]. 2021. Who.int. 2021. Last accessed 13 July 2021. https://www.who.int/news/item/01‐10‐2020‐the‐best‐time‐to‐prevent‐the‐next‐pandemic‐is‐now‐countries‐join‐voices‐for‐better‐emergency‐preparedness [Google Scholar]
- 4. Andrews MA, Areekal B, Rajesh KR, et al. First confirmed case of COVID‐19 infection in India: a case report. Indian J Med Res. 2020;151(5):490‐492. 10.4103/ijmr.IJMR_2131_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sengupta M, Roy A, Ganguly A, Baishya K, Chakrabarti S, Mukhopadhyay I. Challenges encountered by healthcare providers in COVID‐19 times: an exploratory study. J Health Manag. 2021;23(2):339‐356. 10.1177/09720634211011695 [DOI] [Google Scholar]
- 6. Kar SK, Ransing R, Arafat SY, Menon V. Second wave of COVID‐19 pandemic in India: barriers to effective governmental response. EClinicalMedicine. 2021:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Worldometer . COVID‐19 Coronavirus Pandemic. 2021; COVID Live Update: 182,230,706 Cases and 3,946,518 Deaths from the Coronavirus ‐ Worldometer [Internet]. 2021. Worldometers.info. 2021. Last accessed 13 July 2021. https://www.worldometers.info/coronavirus [Google Scholar]
- 8. Goralnick E, Kaufmann C, Gawande A. Mass‐vaccination sites — an essential innovation to curb the Covid‐19 pandemic. N. Engl J Med. 2021;384(18):e67. 10.1056/nejmp2102535 [DOI] [PubMed] [Google Scholar]
- 9. Giubilini A. The Ethics of Vaccination [Internet]. Palgrave Pivot; 2019. Chapter 1, Vaccination: Facts, Relevant Concepts, and Ethical Challenges. 2018. Last accessed 13 July 2021. 10.1007/978-3-030-02068-2_1 https://www.ncbi.nlm.nih.gov/books/NBK538379/ [DOI] [Google Scholar]
- 10. Thiagarajan K. Covid‐19: India is at centre of global vaccine manufacturing, but opacity threatens public trust. BMJ. 2021;372:n196. 10.1136/bmj.n196 [DOI] [PubMed] [Google Scholar]
- 11. Kumar D, Chandra R, Mathur M, Samdariya S, Kapoor N. Vaccine hesitancy: understanding better to address better. Isr J Health Policy Res. 2016;5(1):1‐8. 10.1186/s13584-016-0062-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sonawane K, Troisi C, Deshmukh A. COVID‐19 vaccination in the UK: addressing vaccine hesitancy. Lancet Regional Health ‐ Eur. 2021;1:100016. 10.1016/j.lanepe.2020.100016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karlsson L, Soveri A, Lewandowsky S, et al. Fearing the disease or the vaccine: the case of COVID‐19. Pers Individ Dif. 2021;172:110590. 10.1016/j.paid.2020.110590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee M, Kang B, You M. Knowledge, attitudes, and practices (KAP) toward COVID‐19: a cross‐sectional study in South Korea. BMC Publ Health. 2021;21(1):1‐10. 10.1186/s12889-021-10285-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Papagiannis D, Malli F, Raptis D, et al. Assessment of knowledge, attitudes, and practices towards new coronavirus (SARS‐CoV‐2) of health care professionals in Greece before the outbreak period. Int J Environ Res Public Health. 2020;17(14):4925. 10.3390/ijerph17144925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Afzal M, Khan A, Qureshi U, et al. Community‐based assessment of knowledge, attitude, practices and risk factors regarding COVID‐19 among Pakistanis residents during a recent outbreak: a cross‐sectional survey. J Community Health. 2020;46(3):476‐486. 10.1007/s10900-020-00875-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lau L, Hung N, Go D, et al. Knowledge, attitudes and practices of COVID‐19 among income‐poor households in the Philippines: a cross‐sectional study. J Glob Health. 2020;10(1). 10.7189/jogh.10.011007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gupta M, Goyal R, Aggarwal S, Singh M, Gupta V, Garg N. Demographic and KAP determinants of COVID‐19 vaccine hesitancy and vaccine refusal: a cross‐sectional study in Indian population. Int J Community Med Public Health. 2021;8(10):4776. 10.18203/2394-6040.ijcmph20213664 [DOI] [Google Scholar]
- 19. Al‐Marshoudi S, Al‐Balushi H, Al‐Wahaibi A, et al. Knowledge, attitudes, and practices (KAP) toward the COVID‐19 vaccine in Oman: a pre‐campaign cross‐sectional study. Vaccines (Basel). 2021;9(6):602. 10.3390/vaccines9060602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mallapaty S. Can COVID vaccines stop transmission? Scientists race to find answers. Nature. 2021. Epub ahead of print. PMID: 33608683. 10.1038/d41586-021-00450-z [DOI] [PubMed] [Google Scholar]
- 21. Buchari I, Rafiki A, Qassab M. Awareness and attitudes of employees towards Islamic banking products in Bahrain. Procedia Econ Finance. 2015;30:68‐78. 10.1016/s2212-5671(15)01256-3 [DOI] [Google Scholar]
- 22. Lameris M, Schmidt C, Gleberzon B, Ogrady J. Attitudes toward vaccination: a cross‐sectional survey of students at the Canadian Memorial Chiropractic College. J Can Chiropr Assoc. 2013;57(3):214‐220. [PMC free article] [PubMed] [Google Scholar]
- 23. Yaqub O, Castle‐Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1‐11. 10.1016/j.socscimed.2014.04.018 [DOI] [PubMed] [Google Scholar]
- 24. Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID‐19: implications for public health communications. Lancet Reg Health Eur. 2021;1:100012. 10.1016/j.lanepe.2020.100012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cordina M, Lauri MA, Lauri J. Attitudes towards COVID‐19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract. 2021;19(1):2317. 10.18549/PharmPract.2021.1.2317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. El‐Elimat T, AbuAlSamen M, Almomani B, Al‐Sawalha N, Alali F. Acceptance and attitudes toward COVID‐19 vaccines: a cross‐sectional study from Jordan. PLoS One. 2021;16(4):e0250555. 10.1371/journal.pone.0250555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Charumilind S, Craven M, Lamb J, Sabow A, Singhal S, Wilson M. When Will the COVID‐19 Pandemic End? 2021. Mckinsey.com. Published 2021. Accessed December 9, 2021. https://www.mckinsey.com/industries/healthcare‐systems‐and‐services/our‐insights/when‐will‐the‐covid‐19‐pandemic‐end [Google Scholar]
- 28. Ministry of Health and Family Welfare . [Internet]. 2021. Last accessed 13 July 2021. https://www.mygov.in/covid‐19 [Google Scholar]
- 29. Kumari A, Ranjan P, Chopra S, et al. Development and validation of a questionnaire to assess knowledge, attitude, practices, and concerns regarding COVID‐19 vaccination among the general population. Diabetes Metab Syndr. 2021;15(3):919‐925. 10.1016/j.dsx.2021.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hord SM, Meehan ML, Orletsky S, Sattes B. Issues… About change: assessing a school staff as a community of professional learners. Southwest Educational Development Laboratory. 1999;7(1):n1. https://files.eric.ed.gov/fulltext/ED439490.pdf [Google Scholar]
- 31. Goodman JL, Grabenstein JD, Braun MM. Answering key questions about COVID‐19 vaccines. JAMA. 2020;324(20):2027‐2028. 10.1001/jama.2020.20590 [DOI] [PubMed] [Google Scholar]
- 32. Fritz M, MacKinnon D. Required sample size to detect the mediated effect. Psychol Sci. 2007;18(3):233‐239. 10.1111/j.1467-9280.2007.01882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kline R. Principles and Practice of Structural Equation Modeling. Guilford publications; 1998. [Google Scholar]
- 34. Brown T. In: Kenny DA, ed. Confirmatory Factor Analysis For Applied Research. Guilford publications; 2006. http://kharazmi‐statistics.ir/Uploads/Public/book/Methodology%20in%20the%20Social%20Sciences.pdf [Google Scholar]
- 35. Schreiber J, Nora A, Stage F, Barlow E, King J. Reporting structural equation modeling and confirmatory factor Analysis results: a review. J Educ Res. 2006;99(6):323‐338. 10.3200/joer.99.6.323-338 [DOI] [Google Scholar]
- 36. Hair JF, Black WC, Babin BJ, Anderson RE, Tatham R. Multivariate Data Analysis. Pearson Prentice Hall; 2009. [Google Scholar]
- 37. Watson R. SPSS survival manual by Julie pallant, open university press, Buckingham, 2001, 286 pages, f16.99, ISBN 0 335 20890 8. J Adv Nurs. 2001;36(3):478. 10.1046/j.1365-2648.2001.2027c.x [DOI] [Google Scholar]
- 38. Nunnally J, Bernstein I. Psychometric Theory 3E. 3rd ed. Tata McGraw‐hill education; 1994:11‐67. [Google Scholar]
- 39. De Vet H, Terwee C, Mokkink L, Knol D. Measurement in Medicine: A Practical Guide. Cambridge university press; 2011:96‐135. [Google Scholar]
- 40. Koo T, Li M. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155‐163. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fless. The Design and Analysis of Clinical Experiments. Willey and Sons; 1986:1‐15. [Google Scholar]
- 42. Cicchetti D. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284‐290. 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- 43. Fornell C, Larcker D. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39‐50. 10.1177/002224378101800104 [DOI] [Google Scholar]
- 44. Segars A. Assessing the unidimensionality of measurement: a paradigm and illustration within the context of information systems research. Omega (Westport). 1997;25(1):107‐121. 10.1016/s0305-0483(96)00051-5 [DOI] [Google Scholar]
- 45. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers. 2004;36(4):717‐731. [DOI] [PubMed] [Google Scholar]
- 46. Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879‐891. 10.3758/brm.40.3.879 [DOI] [PubMed] [Google Scholar]
- 47. Shrout P, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7(4):422‐445. 10.1037/1082-989x.7.4.422 [DOI] [PubMed] [Google Scholar]
- 48. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic press; 1988. [Google Scholar]
- 49. Syed Alwi S, Rafidah E, Zurraini A, Juslina O, Brohi I, Lukas S. A survey on COVID‐19 vaccine acceptance and concern among Malaysians. BMC Publ Health. 2021;21(1):1‐12. 10.1186/s12889-021-11071-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Islam S, Emran GI, Rahman E, et al. Knowledge, attitudes and practices associated with the COVID‐19 among slum dwellers resided in Dhaka City: a Bangladeshi interview‐based survey. J Public Health (Oxf). 2021;43(1):13‐25. 10.1093/pubmed/fdaa182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Elhadi M, Alsoufi A, Alhadi A, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID‐19 vaccine: a cross‐sectional study. BMC Publ Health. 2021;21(1):1‐21. 10.1186/s12889-021-10987-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Al‐Qerem W, Jarab A. COVID‐19 vaccination acceptance and its associated factors among a middle Eastern population. Front Public Health. 2021;9:1‐11. 10.3389/fpubh.2021.632914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dharmalingam A, Raghupathy N, Sowmiya M, Amudharaj D, Jehangir H. Immunization knowledge, attitude and practice among mothers of children from 0 to 5 years. Int J Contemp Pediatrics. 2017;4(3):783‐789. 10.18203/2349-3291.ijcp20171488 [DOI] [Google Scholar]
- 54. Dodd RH, Pickles K, Nickel B, et al. Concerns and motivations about COVID‐19 vaccination. Lancet Infect Dis. 2021;21(2):161‐163. 10.1016/S1473-3099(20)30926-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ajzen I. The theory of planned behavior: frequently asked questions. Hum Behav Emerg Technol. 2020;2(4):314‐324. 10.1002/hbe2.195 [DOI] [Google Scholar]
- 56. Chu H, Liu S. Integrating health behavior theories to predict American's intention to receive a COVID‐19 vaccine. Patient Educ Couns. 2021;104(8):1878‐1886. 10.1016/j.pec.2021.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Editor's Choice: influenza vaccine uptake, COVID‐19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. 10.1016/j.ijnurstu.2020.103854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zhang Y, Luo X, Ma ZF. Willingness of the general population to accept and pay for COVID‐19 vaccination during the early stages of COVID‐19 pandemic: a nationally representative survey in mainland China. Hum Vaccin Immunother. 2021;17(6):1622‐1627. 10.1080/21645515.2020.1847585 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


