Synopsis
During the study period, 523 pregnant or postpartum women died in Brazil due to confirmed COVID‐19 or undetermined etiology. This results in a projected COVID‐19 MMR of 17.5/100 000 or potentially even higher.
Keywords: COVID‐19, maternal death, maternal mortality
The present study is based on publicly available data obtained from the Brazilian Official Acute Respiratory Syndrome Surveillance System (ARDS‐SS). We extracted data up to November 23, 2020 and selected pregnant and postpartum women with acute respiratory distress syndrome (ARDS) and a recorded outcome (death or recovery). Cases with a confirmed COVID‐19 diagnosis or closed as “undetermined etiology” were deemed eligible. A detailed description of the methods is described elsewhere. 1
We identified 9563 eligible cases, of which 523 (5.4%) died either with a confirmed diagnosis of COVID‐19 (n = 363) or undetermined etiology (n = 160) (Table 1). The peak of COVID‐19 ARDS cases and deaths occurred between epidemiological weeks 17 and 30, while undetermined cases peaked from weeks 11 to 34 (Figure 1). The case fatality rate for COVID‐19 was 7.6%, while for undetermined etiology it was 3.3%. Postpartum deaths accounted for 41.6% (151/363) and 47.5% (76/160) of confirmed COVID‐19 and undetermined etiology deaths, respectively. Postpartum lethality was over twice the rate of pregnancy lethality regardless of etiology (9.9% vs. 4.1%) (Table 1).
TABLE 1.
ARDS cases among obstetric patients in Brazil by etiology and outcome
| Cured | Died | Total | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Postpartum | 2059 | 90.1 | 227 | 9.9 | 2286 |
| Undetermined etiology | 1207 | 94.1 | 76 | 5.9 | 1283 |
| COVID‐19 | 852 | 84.9 | 151 | 15.1 | 1003 |
| Pregnancy | 6981 | 95.9 | 296 | 4.1 | 7277 |
| Undetermined etiology | 3427 | 97.6 | 84 | 2.4 | 3511 |
| COVID‐19 | 3554 | 94.4 | 212 | 5.6 | 3766 |
| All obstetric cases | 9040 | 94.5 | 523 | 5.5 | 9563 |
| Undetermined etiology | 4634 | 96.7 | 160 | 3.3 | 4794 |
| COVID‐19 | 4406 | 92.4 | 363 | 7.6 | 4769 |
Abbreviation: ARDS, acute respiratory distress syndrome.
FIGURE 1.
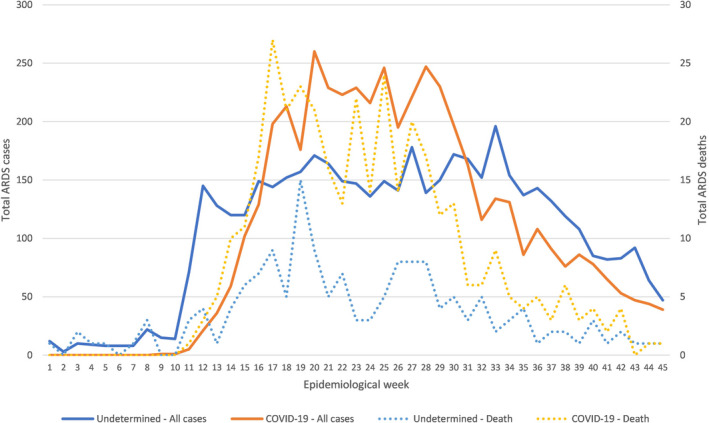
Acute respiratory distress syndrome (ARDS) cases and deaths among pregnant and postpartum women in Brazil by etiology and epidemiological week
In 2018, the Brazilian Ministry of Health officially reported 1658 maternal deaths and preliminary data for 2019 indicate 1547 maternal deaths. 2 This means that COVID‐19‐related maternal deaths so far represent approximately 20% of all maternal deaths relative to mortality statistics from 2018 and 2019. COVID‐19 maternal deaths up to November 2020 already surpass maternal deaths due to hypertension in 2018 and are six times higher than all influenza‐related maternal deaths in 2009. 2
In recent years, 2016 presented the largest maternal mortality ratio (MMR) due to respiratory causes (105 events, 3.6/100 000 live births). Live birth statistics for 2020 are not available so far; however, by extrapolating 1998–2018 data, 3 we project a COVID‐19 MMR of 17.5/100 000, five times higher than all respiratory causes of death in 2016. This figure may be even higher, as a further 160 undetermined etiology ARDS‐related deaths occurred in the same period, many of which could potentially be attributed to COVID‐19. Undetermined etiology ARDS maternal deaths represent 44% of COVID‐19 fatal cases in 2020 and are 1.5 times higher than maternal deaths due to all respiratory causes combined in 2016, raising concerns about underdiagnosis in this population. By now, the “second wave” is well documented in other countries and we are seeing evidence of the same phenomenon in Brazil. The effects on maternal outcomes remain to be understood.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
AUTHOR CONTRIBUTIONS
MNP and MLST equally contributed to study conception and design, data collection, analysis, and interpretation. MNP wrote the first draft of the paper and incorporated substantial contributions from RK, MOM, CAB and MLST after critical revision. All authors reviewed and approved the final manuscript.
ACKNOWLEDGMENTS
The authors would like to thank all members of the Brazilian Group for Studies of COVID‐19 and Pregnancy for their efforts in supporting this work.
REFERENCES
- 1. Menezes MO, Takemoto MLS, Nakamura‐Pereira M, et al.; Brazilian Group of Studies for COVID‐19, Pregnancy . Risk factors for adverse outcomes among pregnant and postpartum women with acute respiratory distress syndrome due to COVID‐19 in Brazil. Int J Gynecol Obstet. 2020;151(3):415‐423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brasil. Ministério da Saúde . Departamento de Informática. [Mortality Information System] [Internet]. SIM‐DATASUS. 2009. http://www2.datasus.gov.br/DATASUS/index.php?area=0205&id=6939&VObj=http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/mat10. Accessed December 1, 2020.
- 3. Brasil. Ministério da Saúde . Departamento de Informática. [Live Birth Information System] [Internet]. SINASC‐DATASUS. 2009. http://www2.datasus.gov.br/DATASUS/index.php?area=0205&id=6936&VObj=http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nv. Accessed December 1, 2020.


