Abstract
Objectives:
To examine age differences in the association between discrimination and depressive symptoms among urban American Indians and Alaska Natives (AI/AN).
Methods:
A sample of 303 urban AI/AN (18–78 years old) reported on lifetime and past-week experiences of racial discrimination and depressive symptoms. Depressive symptoms were regressed on racial discrimination, age, and their interaction, adjusting for demographic factors and other life stressors.
Results:
Lifetime and past-week discrimination were significantly associated with depressive symptoms, and these associations were stronger among younger than older adult AI/AN.
Discussion:
The results are consistent with prior reports in other populations, but this is the first such study to focus on AI/AN, and it highlights the importance of considering life course perspectives. Conclusions are limited by the cross-sectional nature of the data. Longitudinal and qualitative work is needed to understand why discrimination may have a stronger effect on mental health for younger than older AI/AN.
Keywords: American Indians and Alaska Natives, depression, discrimination, life course perspective
American Indians and Alaska Natives (AI/AN)1 numbered in the millions prior to the arrival of Europeans (Stannard, 1992). Following exposure to foreign diseases and hundreds of years of colonization—including forced removal from traditional lands, the separation of families, and government policies of “Indian Termination”—AI/AN are now one of the smallest (2%) racial/ethnic groups in the United States (Bear Chief, 2016; Brave Heart & Debruyn, 1998; Brown, 1970; Sellars, 2013; Stannard, 1992) and report high rates of discrimination (Blair et al., 2020; Gonzales et al., 2016; NPR et al., 2018; Thayer et al., 2017), which may be traumatizing (Evans-Campbell, 2008).
Consistent with theoretical models of the adverse health effects of racial discrimination (Brondolo et al., 2018; Williams & Mohammed, 2013), research shows a robust link between reports of perceived racial discrimination and depression or depressive symptoms in AI/AN (Gonzales et al., 2016; Kading et al., 2015; Matheson et al., 2019; Tucker et al., 2016; Whitbeck et al., 2002), as found in other racialized and stigmatized groups (de Freitas et al., 2018; Paradies et al., 2015; Schmitt et al., 2014). Less clear, however, is whether this association varies over the life course. Links between discrimination and depressive symptoms have been observed among AI/AN children (Yoder et al., 2006), adolescents (Yasui et al., 2015), and adults (Tucker et al., 2016), but potential differences by age (or life stage) have not been systematically investigated. Instead, age is typically viewed as a confounder to be statistically controlled (e.g., Whitbeck et al., 2002). Yet, age and experience define one’s role within AI/AN communities, affecting personal and relational well-being within those communities (Howell & Peterson, 2017; Lewis & Allen, 2017; Rowe et al., 2020). For instance, Elders’ traditional roles as repositories of knowledge contribute both to their own personal health and well-being as well as that of the entire community. Thus, a life course perspective on discrimination and depressive symptoms within AI/AN communities may be particularly relevant.
Gee et al. (2012) argue eloquently that a full understanding of the association between discrimination and health requires a consideration of how discrimination manifests across the life course (NIMHD, n.d.). Age is not merely of biological or developmental relevance, rather as people age, they leave some social institutions and enter new ones (e.g., transitioning from secondary to tertiary education, to the work force, and then retirement). These life changes can result in “age-patterned” exposures to discrimination that vary in frequency, type, and intensity, potentially affecting the nature and extent of depressive symptoms over the life course. Moreover, certain stressors may have a more profound effect on people depending on their “life task.” For instance, the task of developing a coherent identity is a major challenge for emerging adults (Phinney, 1990) and appears related to psychological distress in AI/AN (Chandler & Lalonde, 1998). Related to the above, processes of colonization—both past and present—may have disrupted certain age-related cultural norms or practices, such as the transmission of cultural knowledge from Elders to other community members (Pace & Grenier, 2017), leaving younger AI/AN more vulnerable to the harms of colonization and discrimination. Indeed, the loss of these holistic intergenerational practices, as well as the removal of AI/AN from traditional lands and into urban settings, may all impinge on health and well-being of AI/AN across the life course.
Existing research on age differences in the association between discrimination and depressive symptoms has yielded mixed results. In one meta-analysis involving eight different ethnic and racial groups, age did not modify this association (Paradies et al., 2015). But two other meta-analyses (de Freitas et al., 2018; Schmitt et al., 2014) with a wider range of intergroup contexts (e.g., racism, heterosexism, and sexism) suggested that the association is stronger in younger individuals. Direct tests have yielded mixed findings. In a sample of African American men, the association between depressive symptoms and the everyday slights and hassles of discrimination was strongest among middle-aged men and weakest among older men (Wheaton et al., 2018). However, older men in this sample were more likely to report depressive symptoms with major discrimination—discrete instances of unfair treatment tied to livelihood, success, and upward mobility.
In another study, the mitigating effects of age depended on whether discrimination or discrimination-related threat appraisals were examined, and further differed by group (Matheson et al., 2019). Specifically, age diminished the association between discrimination and depressive symptoms among Black and Jewish Canadians. But for Indigenous peoples in Canada, age diminished the relationship between discrimination-related threat appraisals and depressive symptoms, but not discrimination itself. Taken together, whether age moderates the association between discrimination and depressive symptoms remains equivocal. For AI/AN, age can represent unique experiences and perspectives, such as traumatizing memories of boarding school among older AI/AN or, conversely, older AI/AN may hold different resources, including wisdom, traditional values, or roles in community that mitigate the harms of discrimination.
The goal of the present study was to examine the extent to which age moderates the association between discrimination and depressive symptoms in a sample of urban-dwelling AI/AN, ranging in age from 18 to 78 years old. In doing so, we looked at both lifetime experiences of discrimination and past-week discrimination, and we tested these associations before and after adjusting for demographic variables (e.g., gender, education, and household income) and other significant life stressors for which there may be generational differences in exposure (e.g., childhood adversity and major life events).
Methods
Participants and Procedure
The data analyzed in the current study were drawn from a broader project known as the American Indian Stress and Health study, a community-based, cross-sectional, observational study of discrimination and health conducted between November 2016 and April 2019 among urban-dwelling AI/AN in the Denver, Colorado area. Approximately 71% of AI/AN live in urban areas (US Census Bureau, 2010), where opportunities for contact between AI/AN and non-AI/AN are numerous. All data collected were in accordance with the ethical standards for research including human subjects as per the Colorado Multiple Institutional Review Board (University of Colorado) and with the guidance of an AI/AN community advisory council as well as AI/AN members of the research team. Further details on recruitment, informed consent, study procedures, and a comprehensive list of measures obtained as part of the 2-day study protocol can be found on the Open Science Framework (Blair et al., 2019).
Measures
Lifetime discrimination
Participants indicated how often over their lifetimes they experienced different forms of discrimination attributable to their AI/AN identity using the 17-item Brief Perceived Ethnic Discrimination Questionnaire–Community Version (PEDQ-CVB; Brondolo et al., 2005). The PEDQ-CVB was validated for use with American Indians in a prior study (Blair et al., 2020) and assesses multiple forms of discrimination: social exclusion, stigmatization, threats/harm to self and property, and discrimination at work or school. Items were rated on a 5-point scale (0 = never, 1 = rarely, 2 = sometimes, 3 = often, and 4 = very often), with higher scores reflecting more frequent lifetime discrimination exposure. Consistent with prior use of this scale, lifetime discrimination was scored as the average rating across items (α = .94 in this sample).
Past-week discrimination
Participants reported experiences with discrimination in the past 7 days using a 10-item scale similar to the PEDQ-CVB, which assessed social exclusion, stigmatization, threat, and harassment (Brondolo et al., 2009). Consistent with prior use of this scale, participants’ responses were averaged across items (α = .95 in this sample).
Other significant life stressors
Given the cross-sectional nature of our data, two additional measures of major life stressors were included as covariates to better isolate the unique association between discrimination and depressive symptoms. Adverse childhood experiences were assessed with five questions on childhood abuse and deprivation (response options: 0 = never, 1 = rarely, 2 = sometimes, and 3 = often) and scored according to standard practice (Felitti et al., 1998), with higher scores reflecting greater adversity in childhood. Participants were also asked whether each of 10 stressful life experiences had occurred in the past year (e.g., divorce, death of a loved one, and serious financial problems), and “yes” responses were summed, with higher scores reflecting more experiences of significant life stressors (Holmes & Rahe, 1967).
Depressive symptoms
Participants reported their depressive symptoms over the prior 2-week period using 18 items from the Center for Epidemiologic Studies Depression Scale–Revised (CESD-R; Eaton et al., 2004; Van Dam & Earleywine, 2011). Items assess agitation, anhedonia, appetite, dysphoria, fatigue, sleep, thinking/concentration, and worthlessness, using a 5-point scale (0 = 0 or <1 day last week; 1 = 1–2 days last week; 2 = 3–4 days last week; 3 = 5–7 days last week; and 4 = nearly everyday for 2 weeks). Two CESD-R questions on suicidality were eliminated because study staff were not trained to address this with participants. Given that depression cannot be diagnosed without these two questions, we averaged responses across items to reflect average depressive symptoms over the prior 2 weeks (α = .94 in this sample).
Socio-demographics
Participants indicated their age (in years), gender, education level, and annual household income (calculated relative to poverty level). To protect confidentiality for transgender/nonbinary participants, gender is analyzed as female versus other. Excluding transgender/nonbinary or using a 3-level categorical variable made no difference in the results.
Analytic Approach
Bivariate correlations and t-tests were used to test sample characteristics. Discrimination and depressive symptoms were then each regressed on age in terms of its linear, quadratic, and cubic effects, to determine whether and how age is related to these primary variables of interest. Depressive symptoms were then regressed on discrimination (lifetime or past-week), the linear effect of age, and the interaction of both terms. We also explored whether models including interactions between discrimination and nonlinear effects of age predicted depressive symptoms. In these models, only the linear effect of age was a significant moderator of the association between discrimination and depressive symptoms.
Additional models included background and other significant life stressors as covariates. Because depressive symptoms showed moderate skew (1.22), a square-root transformation was applied to meet assumptions of normality (skew reduced to 0.02); poverty level had more substantial skew (2.12) and was log-transformed (skew reduced to 0.44). Multiple post hoc linear regressions, stratified by age in decades, were conducted to better understand the relation between discrimination and depressive symptoms at different age periods. All analyses were conducted with R statistical software (version 3.6.1; R Core Team, 2019), and missing data were handled using full information maximum likelihood procedures from the lavaan package (Oberski, 2014).2
Results
Sample Characteristics
Participant characteristics are shown in Table 1. Bivariate correlations among continuous and ordinal variables are shown in Table 2. T-tests revealed that gender was significantly associated with age (Mfemale = 45.38, Mother = 40.71; p = .006) and adverse childhood experiences (Mfemale = 2.64, Mother = 2.03; p = .002).
Table 1.
Sample Characteristics (N = 303)
| Age M (SD) | 43.62 (14.74) |
| Female gender | 188 (63%) |
| Education | |
| < High school diploma | 64 (21%) |
| High school diploma or GED | 93 (31%) |
| 1–3 yrs college | 118 (39%) |
| 4 yrs college or advanced degree | 23 (8%) |
| N/A | 4 (1%) |
| Household poverty level | |
| Below poverty level | 169 (56%) |
| At poverty level | 16 (5%) |
| 1.25–4 × poverty level | 98 (32%) |
| > 4 × poverty level | 17 (6%) |
| N/A | 2 (1%) |
| Adverse childhood experiences M (SD) | 2.41 (1.73) |
| Past-year major life events M (SD) | 3.71 (2.35) |
| Lifetime discrimination M (SD) | 1.48 (0.80) |
| Past-week discrimination M (SD) | 1.23 (0.96) |
| Depressive symptoms M (SD) | 0.91 (0.82) |
Note: Categories with <10 participants are collapsed to protect confidentiality. N = 303. GED = General Educational Development Test.
Table 2.
Pearson’s Correlations among Continuous and Ordinal Variables using Full Information Maximum Likelihood
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Depressive symptoms (square root) | — | |||||||
| 2. Lifetime discrimination | 0.344*** | — | ||||||
| 3. Past-week discrimination | 0.337*** | 0.763*** | — | |||||
| 4. Age | −0.012 | 0.201*** | 0.251*** | — | ||||
| 5. Education | −0.051 | 0.141* | 0.050 | 0.134* | — | |||
| 6. Poverty threshold (log) | −0.108 | −0.084 | −0.148** | −0.028 | 0.294*** | — | ||
| 7. Adverse childhood experiences | 0.317*** | 0.395*** | 0.290*** | 0.058 | 0.168** | −0.035 | — | |
| 8. Major life stressors | 0.293*** | 0.243*** | 0.204*** | −0.061 | 0.108 | −0.042 | 0.239*** | — |
p ≤ .05,
p ≤ .01,
p ≤ .001.
Nonlinear Effects of Age
Regression models examining linear, quadratic, and cubic effects of age showed significant quadratic effects for both discrimination (lifetime, b = −0.134, 95% CI [−0.225, −0.044]; past-week, b = −0.124, 95% CI [−0.232, −0.016]) and depressive symptoms, b = −0.059, 95% CI [−0.113, −0.006]. In this sample of urban AI/AN, those at mid-life (approximately 48 years old) reported higher levels of discrimination and depressive symptoms than those in early adulthood or in later life. These patterns remained unchanged after controlling for gender, education, and poverty level. The quadratic effect of age was also significant for adverse childhood experiences, b = −0.275, 95% CI [−0.476, −0.074], and major life events, b = −0.340, 95% CI [−0.614, −0.066], with mid-life AI/AN reporting more events than either younger or older adults.
Depressive Symptoms Regressed on Discrimination
In unadjusted models, both lifetime and past-week discrimination were significantly associated with depressive symptoms (lifetime, b = 0.198, 95% CI [0.137, 0.259]; past-week, b = 0.162, 95% CI [0.111, 0.214]; see also Table 2). These associations remained significant when controlling for gender, poverty level, education, age, and other life stressors (lifetime, b = 0.138, 95% CI [0.071, 0.204]; past-week, b = 0.120, 95% CI [0.066, 0.173]) and, adjusted for covariates, respectively accounted for 21.4% and 21.9% of the variance in depressive symptoms.
Tests of the age × discrimination interaction, reported in Table 3, showed that age modified the relation of both types of discrimination to depressive symptoms, controlling for all covariates (lifetime, b = −0.007, 95% CI [−0.011, −0.003], R2 = .243; past-week, b = −0.006, 95% CI [−0.009, −0.002], R2 = .247). To better understand the modifying effects of age on the association between discrimination and depressive symptoms, we estimated the strength of the association at specific age points using the approach suggested by Aiken and West (1991). The associations between discrimination and depressive symptoms represented medium to large effects at 40 years of age and younger (lifetime: βs ≥ 0.29; Figure 1, top panel; past-week: βs ≥ 0.31; Figure 1, bottom panel). The magnitude of these associations attenuated with increased age, becoming nonsignificant at approximately 60 years and older (lifetime: βs ≤ 0.06; past-week: βs ≤ 0.07). Predicted values of the association between discrimination and depressive symptoms (square-root transformed) at different ages (top panel: lifetime discrimination; bottom panel: past-week discrimination). Plotted values are estimated from their respective statistical models. Error bars represent one standard error above and below estimated values. ***p < .001, **p < .01.
Table 3.
Estimates and 95% Confidence Intervals of Adjusted Linear Regressions predicting Depressive Symptoms by Age × Discrimination Exposure
| Lifetime discrimination as predictor of depressive symptoms (N = 303) | Past-week discrimination as predictor of depressive symptoms (N = 303) | |||||||
|---|---|---|---|---|---|---|---|---|
| Std. Est. | Est. | CI lower | CI upper | Std. Est. | Est. | CI lower | CI upper | |
| Intercept | 0.000 | 0.842 | 0.783 | 0.901 | 0.000 | 0.852 | 0.793 | 0.912 |
| Gender (female = 0, other = 1) | 0.029 | 0.027 | −0.071 | 0.126 | 0.011 | 0.010 | −0.088 | 0.109 |
| Education | −0.120 | −0.056 | −0.106 | −0.005 | −0.112 | −0.052 | −0.103 | −0.001 |
| Household poverty level | −0.045 | −0.025 | −0.085 | 0.035 | −0.030 | −0.017 | −0.077 | 0.043 |
| Adverse childhood experiences | 0.214 | 0.057 | 0.027 | 0.087 | 0.215 | 0.057 | 0.028 | 0.086 |
| Major life events | 0.179 | 0.035 | 0.015 | 0.055 | 0.195 | 0.038 | 0.018 | 0.058 |
| Age | −0.070 | −0.002 | −0.005 | 0.001 | −0.080 | −0.002 | −0.006 | 0.001 |
| Discrimination | 0.252 | 0.145 | 0.080 | 0.211 | 0.264 | 0.127 | 0.074 | 0.180 |
| Age × discrimination | −0.173 | −0.007 | −0.011 | −0.003 | −0.169 | −0.006 | −0.009 | −0.002 |
Note. Income level was adjusted according to poverty threshold. Education was treated as a continuous variable. Std. Est. = standardized estimate. CI = the lower and upper bounds of the 95% confidence interval.
Figure 1.
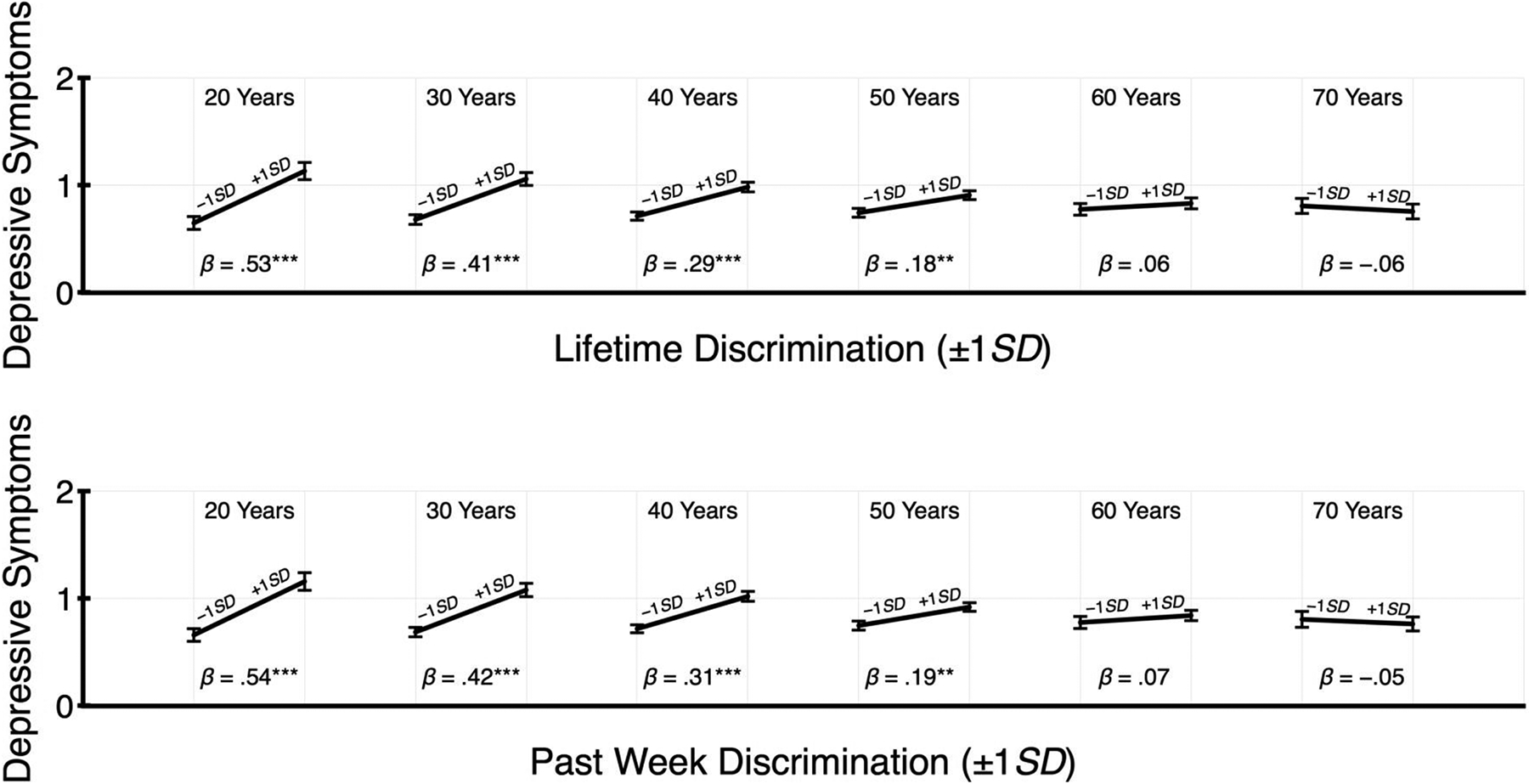
Predicted values of the association between discrimination and depressive symptoms (square-root transformed) at different ages (top panel: lifetime discrimination; bottom panel: past-week discrimination). Plotted values are estimated from their respective statistical models. Error bars represent one standard error above and below estimated values. ***p < .001, **p < .01.
Discussion
The current study demonstrated a robust association between discrimination and depressive symptoms in urban AI/AN, as has been shown by others (Gonzales et al., 2016; Kading et al., 2015; Matheson et al., 2019; Tucker et al., 2016; Whitbeck et al., 2002). More importantly, we found that this association varied by age and was significantly stronger for younger than older AI/AN adults.
In this sample, older AI/AN were more likely to be female and have higher education, and middle-aged AI/AN also reported higher levels of depressive symptoms, discrimination, and other significant life stressors. Yet, controlling for these background variables and other life stressors, we still found that discrimination was more strongly associated with depressive symptoms in younger than older adults. Indeed, our analyses suggested that the association diminishes to non-significance for AI/AN over 60 years of age.
The self-report, cross-sectional nature of our data does not allow us to claim that experiences of discrimination caused depressive symptoms in this sample of AI/AN. The reverse causal pathway is plausible: depressive symptoms may lead to heightened perceptions of hardship in life, discrimination included. This alternative explanation is weakened, however, by our finding that inclusion of other self-reported hardships—adverse childhood experiences and major stressors in the past year—did not change the results: discrimination remained uniquely associated with depressive symptoms, and this association was stronger for younger than older AI/AN.
The similarity in findings with lifetime and past-week discrimination is intriguing. One might imagine that older adults have had more time for accumulated exposure to discrimination—as measured by the lifetime scale—making age and lifetime discrimination inevitably confounded. But all age groups had the same amount of time with past-week discrimination, and this measure showed the same result. These findings suggest that the older AI/AN in this sample had greater resiliency (or less vulnerability) to discrimination that occurred recently, as well as in the past.
Our findings suggest a number of interesting possibilities for future work, particularly the notion that older individuals (or maybe older AI/AN, specifically) may build resiliency against the effects of discrimination, both lifetime and recent. One possibility is that older adults, with more experience dealing with discrimination, may have developed personalized or perhaps more automatic approaches to handling discrimination and are better prepared for coping with new instances of discrimination. Younger, less experienced individuals may be less prepared to defend themselves, resulting in feelings of guilt and shame and increased rumination, each of which are associated with depressive symptoms (Kim et al., 2011; Olatunji et al., 2013). Age-related differences in coping and emotion regulation may also explain the resiliency of older AI/AN in the current study (Carstensen et al., 2011; Thomas et al., 2006; Whitehead & Bergeman, 2013). For instance, psychological vulnerabilities specific to early adulthood may render discrimination more difficult to navigate as younger urban AI/AN try to “fit in” with the majority culture as they pursue education and employment (Chandler & Lalonde, 1998; Kirmayer, 1994). As AI/AN become older, they may focus their attention to more positive life experiences and give less attention to experiences with discrimination (Thomas et al., 2006).
It is, of course, also possible that the age differences observed in this study are the result of different social cohorts, rather than age or experience more generally. For instance, older AI/AN in our study may have been personally exposed to the trauma of being forced into government- and church-run boarding schools where abuse was rampant (Bear Chief, 2016; Sellars, 2013). Such experiences may have “hardened” these AI/AN to new experiences of discrimination or, conversely, may have resulted in a stronger cultural identity, imbuing them and their peers with greater resilience. Younger adult AI/AN today could also have other vulnerabilities that were not present in younger AI/AN of the past (Brault et al., 2012). Future work with qualitative and longitudinal designs and samples from multiple cohorts are necessary to better pinpoint the reasons why discrimination may be more strongly linked to depressive symptoms in younger than older AI/AN.
Limitations and Conclusions
As noted already, the cross-sectional data limit our conclusions. An additional limitation of the current study is that our sample consists of urban AI/AN; it is unclear whether these findings would generalize to AI/AN living on reservation lands. Further, we acknowledge the high degree of overlap between our two measures of discrimination. It is possible that reports of lifetime discrimination are colored by more recent experiences (or vice versa). Yet other work has shown these constructs to differentially predict health outcomes (Brondolo et al., 2015). Thus, another reason for the high overlap could be that some people experience more discrimination than others, due to social context or appearance, and this would be reflected in both lifetime and past-week discrimination exposure. Finally, we note that this urban AI/AN community sample was obtained by convenience and, thus, we do not claim to have representative results for urban AI/AN more generally.
In conclusion, the present findings demonstrate that the association between discrimination and depressive symptoms among urban AI/AN is robust, especially for those in younger adulthood. Future work aimed at developing interventions to build Indigenous resilience or provide support against the harms of discrimination should pay close attention to these experiences and to the lifespan changes that may contribute to resiliency in older urban AI/AN. Indeed, AI/AN Elders’ roles as intergenerational transmitters of knowledge coupled with their desire to transmit cultural knowledge and values to younger generations may be of critical value in fostering personal and relational well-being within their communities, particularly among younger generations who continue to confront discrimination and colonization as they build their families and lives.
Acknowledgments
We would like to thank Jacqueline Gardner, Alexandria Meyer, Rebeca Elizondo, and Blythe Muth for their help collecting data.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research is supported by the American Heart Association [15SFDRN24180024], the National Institute on Aging [P30AG059295, P30AG15297], and the National Center on Minority Health and Health Disparities [P60MD000507].
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
We use the term AI/AN in accordance with the 1977 joint resolution of the National Congress of American Indians and the National Tribal Chairmen’s Association, that in the absence of a specific tribal designation, “American Indian and/or Alaska Native (AI/AN)” is the preferred term of reference. Our study includes individuals from many different tribal groups across the United States, making the general term appropriate in this context.
Approximately 2% of participants had incomplete cases. For models with linear, quadratic, and cubic effects of age, age had to be standardized to ensure that the observed variances of these effects did not substantially differ from each other. Otherwise, the FIML procedures could not be implemented in these models. For the remaining models, age was treated in its raw but centered form to aid interpretation.
References
- Aiken LS, West SG (1991). Multiple regression: Testing and interpreting interactions. Sage Publications Inc. [Google Scholar]
- Bear Chief A (2016). My decade at Old Sun, my lifetime of hell. Athabasca University Press. [Google Scholar]
- Blair IV, Brondolo E, Laudenslager ML, Danyluck CM, Daugherty SL, Correll J, Manson SM (2019). American Indian Stress and Health Study. Open Science Framework. https://osf.io/jnp64/?view_only=c1f21f2757bd40598b4198bbeb3fa01b.
- Blair IV, Danyluck C, Judd CM, Manson SM, Laudenslager ML, Daugherty SL, Ratliff EL, Gardner JA, Brondolo E (2021). Validation of the Brief Perceived Ethnic Discrimination Questionnaire-Community Version in American Indians. Cultural Diversity & Ethnic Minority Psychology, 27(1), 47–59. [DOI] [PubMed] [Google Scholar]
- Brault M-C, Meuleman B, Bracke P (2012). Depressive symptoms in the Belgian population: Disentangling age and cohort effects. Social Psychiatry and Psychiatric Epidemiology, 47, 903–915. [DOI] [PubMed] [Google Scholar]
- Brave Heart M, Debruyn LM (1998). The American Indian Holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research, 8(2), 60–82. [PubMed] [Google Scholar]
- Brondolo E, Beatty DL, Cubbin C, Pencille M, Saegert S, Wellington R, Tobin J, Cassells A, Schwartz J (2009). Sociodemographic variations in self-reported racism in a community sample of Blacks and Latino(a)s. Journal of Applied Social Psychology, 39(2), 407–429. https://psycnet.apa.org/doi/10.1111/j.1559-1816.2008.00444.x. [Google Scholar]
- Brondolo E, Blair IV, Kaur A (2018). Biopsychosocial mechanisms linking discrimination to health: A focus on social cognition. In Major B, Dovidio JF, Link BG (Eds.), Oxford Handbook of Stigma, Discrimination and Health. New York: Oxford University Press. [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Cassells A, Tobin JN, Sweeney M, Contrada RJ (2005). The Perceived Ethnic Discrimination Questionnaire: Development and preliminary validation of a community version. Journal of Applied Social Psychology, 35(2), 335–365. [Google Scholar]
- Brondolo E, Monge A, Agosta J, Tobin JN, Cassells A, Stanton C, Schwartz J (2015). Perceived ethnic discrimination and cigarette smoking: Examining the moderating effects of race/ethnicity and gender in a sample of Black and Latino urban adults. Journal of Behavioral Medicine, 38, 689–700. [DOI] [PubMed] [Google Scholar]
- Brown D (1970). Bury my heart at Wounded Knee: An Indian history of the American west. MacMillan. [Google Scholar]
- Carstensen LL, Turan B, Scheibe S, Ram N, Ersner-Hershfield H, Samanez-Larkin GR, Brooks KP, Nesselroade JR (2011). Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychology and Aging, 26(1), 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler MJ, Lalonde C (1998). Cultural continuity as a hedge against suicide in Canada’s First Nations. Transcultural Psychiatry, 35(2), 191–219. [Google Scholar]
- de Freitas DF, Fernandes-Jesus M, Ferreira PD, Coimbra S, Teixeira PM, de Moura A, Gato J, Marques SC, Fontaine AM (2018). Psychological correlates of perceived ethnic discrimination in Europe: A meta-analysis. Psychology of Violence, 8(6), 712–725. [Google Scholar]
- Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A (2004). Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R). In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults (pp. 363–377). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Evans-Campbell T (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23(3), 316–338. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Gee GC, Walsemann KM, Brondolo E (2012). A life course perspective on how racism may be related to health inequities. American Journal of Public Health, 102(5), 967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales KL, Noonan C, Goins RT, Henderson WG, Beals J, Manson SM, Acton KJ, Roubideaux Y (2016). Assessing the Everyday Discrimination Scale among American Indians and Alaska Natives. Psychological Assessment, 28(1), 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NPR, , the Robert Wood Johnson Foundation, and the Harvard T. H. Chan School of Public Health (2018). Discrimination in America: Final Summary. Robert Wood Johnson Foundation. https://www.rwjf.org/content/dam/farm/reports/surveys_and_polls/2018/rwjf443620. [Google Scholar]
- Holmes TH, Rahe RH (1967). The Social Readjustment Rating Scale. Journal of Psychosomatic Research, 11(2), 213–218. [DOI] [PubMed] [Google Scholar]
- Howell BM, Peterson JR (2017). “With age comes wisdom”: A qualitative review of Elder perspectives on healthy aging in the Circumpolar North. Journal of Cross-Cultural Gerontology, 35, 113–131. [DOI] [PubMed] [Google Scholar]
- Kading ML, Hautala DS, Palombi LC, Aronson BD, Smith RC, Walls ML (2015). Flourishing: American Indian positive mental health. Society and Mental Health, 5(3), 203–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S, Thibodeau R, Jorgensen RS (2011). Shame, guilt, and depressive symptoms: A meta-analytic review. Psychological Bulletin, 137(1), 68–96. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ (1994). Suicide among Canadian Aboriginal peoples. Transcultural Psychiatric Research Review, 31(1), 3–58. https://psycnet.apa.org/doi/10.1177/136346159403100101. [Google Scholar]
- Lewis JP, Allen J (2017). Alaska Native Elders in recovery: Linkages between Indigenous cultural generativity and sobriety to promote successful aging. Journal of Cross-Cultural Gerontology, 32, 209–222. [DOI] [PubMed] [Google Scholar]
- Matheson K, Foster MD, Bombay A, McQuaid RJ, Anisman H (2019). Traumatic experiences, perceived discrimination, and psychological distress among members of various socially marginalized groups. Frontiers in Psychology, 10, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIMHD (n.d.). NIMHD Research Framework Adaptation. https://www.nimhd.nih.gov/about/overview/research-framework/adaptation-framework.html.
- Oberski D (2014). lavaan.survey: An R Package for complex survey analysis of structural equation models. Journal of Statistical Software, 57(1), 1–27. http://www.jstatsoft.org/v57/i01/.25400517 [Google Scholar]
- Olatunji BO, Naragon-Gainey K, Wolitzky-Taylor KB (2013). Specificity of rumination in anxiety and depression: A multimodal meta‐analysis. Clinical Psychology: Science and Practice, 20(3), 225–257. [Google Scholar]
- Pace JE, Grenier A (2017). Expanding the circle of knowledge: Reconceptualizing successful aging among North American older Indigenous peoples. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 72(2), 248–258. [DOI] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G (2015). Racism as a determinant of health: A systematic review and meta-analysis. PLoS One, 10, 1–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phinney JS (1990). Ethnic identity in adolescents and adults: Review of research. Psychological Bulletin, 108(3), 499–514. [DOI] [PubMed] [Google Scholar]
- R Core Team (2019). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.r-project.org/. [Google Scholar]
- Rowe G, Straka S, Hart M, Callahan A, Robinson D, Robson G (2020). Prioritizing Indigenous Elders’ knowledge for intergenerational well-being. Canadian Journal on Aging/La Revue canadienne du vieillissement, 39(2), 156–168. [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, Garcia A (2014). The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin, 140(4), 921–948. [DOI] [PubMed] [Google Scholar]
- Sellars B (2013). They called me number one. Singapore Books. [Google Scholar]
- Stannard DE (1992). Genocide in the Americas. The Nation, 255, 430–434. [Google Scholar]
- Thayer ZM, Blair IV, Buchwald DS, Manson SM (2017). Racial discrimination associated with higher diastolic blood pressure in a sample of American Indian adults. American Journal of Physical Anthropology, 163, 122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE (2006). The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychology, 25(5), 635–642. [DOI] [PubMed] [Google Scholar]
- Tucker RP, Wingate LR, O’Keefe VM (2016). Historical loss thinking and symptoms of depression are influenced by ethnic experience in American Indian college students. Cultural Diversity & Ethnic Minority Psychology, 22(3), 350–358. [DOI] [PubMed] [Google Scholar]
- US Census Bureau (2010). Census 2010 American Indian and Alaska native summary file. https://www.census.gov/data/datasets/2010/dec/aian-summary-file.html.
- Van Dam NT, Earleywine M (2011). Validation of the Center for Epidemiologic Studies Depression Scale-Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Research, 186(1), 128–132. [DOI] [PubMed] [Google Scholar]
- Wheaton FV, Thomas CS, Roman C, Abdou CM (2018). Discrimination and depressive symptoms among African American men across the adult lifecourse. The Journals of Gerontology: Series B, 73(2), 208–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitbeck LB, McMorris BJ, Hoyt DR, Stubben JD, LaFromboise T (2002). Perceived discrimination, traditional practices, and depressive symptoms among American Indians in the Upper Midwest. Journal of Health and Social Behavior, 43(4), 400–418. https://psycnet.apa.org/doi/10.2307/3090234. [PubMed] [Google Scholar]
- Whitehead BR, Bergeman CS (2013). Ups and downs of daily life: Age effects on the impact of daily appraisal variability on depressive symptoms. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(3), 387–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA (2013). Racism and health I: Pathways and scientific evidence. American Behavioral Scientist, 57(8), 1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasui M, Dishion TJ, Stormshak E, Ball A (2015). Socialization of culture and coping with discrimination among American Indian families: Examining cultural correlates of youth outcomes. Journal of the Society for Social Work and Research, 6(3), 317–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder KA, Whitbeck LB, Hoyt DR, LaFromboise T (2006). Suicidal ideation among American Indian youths. Archives of Suicide Research, 10(2), 177–190. [DOI] [PubMed] [Google Scholar]


