Abstract
Objective
To review what is known about COVID‐19 and highlight gaps in the context of Nigerian obstetric practice. Research data on COVID‐19 are understandably sparse in Africa. Nigeria, like most African countries, is battling a disease she is poorly equipped to fight.
Methods
The current available literature on COVID‐19 was reviewed in relation to obstetric practice in the Nigerian context, gaps were identified, and recommendations were made to improve the handling of the COVID‐19 pandemic in Nigerian obstetric practice.
Results
In and out of hospital, both the obstetrician and the obstetric patient are constantly being put at risk of exposure to the coronavirus because testing and preventive measures are either ineffective or non‐existent.
Conclusion
The pandemic has exposed the gross inadequacies in Nigeria’s healthcare system and is therefore a wake‐up call to the need for a complete overhaul of infrastructure and services. The government will do well to increase the budget allocation for health from the current paltry 4.14% to the recommended 15% of the total budget.
The Nigerian obstetrician stands a high risk of exposure due to inadequate preventive measures, and testing and diagnostic challenges.
Keywords: COVID‐19, Health workers, Nigeria, Obstetric practice
Short abstract
The Nigerian obstetrician stands a high risk of exposure due to inadequate preventive measures, and testing and diagnostic challenges.
1. INTRODUCTION
The outbreak of a completely unique 2019 coronavirus disease (COVID‐19), previously referred to as 2019‐nCoV, was first reported in Wuhan, Hubei province, China, on December 31, 2019. 1 With a case fatality rate (CFR) of 2%, the disease had quickly spread to over 20 countries in the world, including the USA and Europe by January 30, 2020. It was then declared a Public Health Emergency of International Concern. 2 WHO declared it a pandemic on March 11, 2020. 3 The disease currently affects 215 countries worldwide, with 8 871 099 cases and 465 987 deaths (Fig.1). 4
Figure 1.

World distribution of COVID‐19 as of June 26, 2020, 12:00pm ET (source: www.cdc.gov).
In Africa, 315 410 cases and 8334 deaths (CFR 2.7%) have been reported in 54 countries as of June 23, 2020. 4 This represents 3.6% of all cases recorded worldwide. 4 Sub‐Saharan Africa recorded her first confirmed case of COVID‐19 in Nigeria on February 27, 2020, 5 when an Italian expatriate who had returned to Lagos, Nigeria, from Milan, Italy, 2 days before, tested positive for the novel virus. By May 13, 2020, every country in Africa had been affected by the disease, with Lesotho being the last to record an infection. 6 This is not surprising because out of the 25 countries in the world most susceptible to a communicable disease outbreak, 22 are African. 7 In Nigeria, as of June 26, 2020, a total of 22 614 confirmed cases and 549 deaths have been recorded in 35/36 states of the country, including the Federal Capital Territory (FCT) (Table 1, Fig. 2). 8
Table 1.
Distribution of confirmed cases, active cases, discharged and deaths, and tests done in Nigeria as of June 26, 2020 (based on data from the NCDC).
| Cases | Number |
|---|---|
| Confirmed | 22 614 |
| Active | 14 243 |
| Discharged | 7822 |
| Deaths | 549 |
| Total tests | 122 155 |
Figure 2.
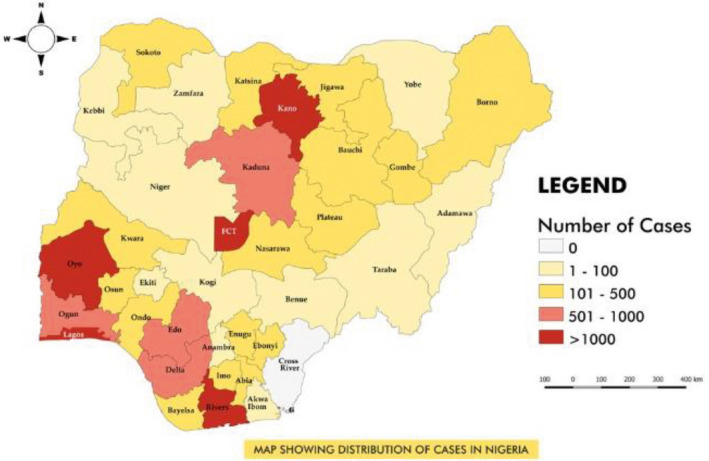
Map showing distribution of cases in Nigeria (source: Twitter, @ncdcgov, accessed June 28, 2020).
The study of this disease is new and rapidly evolving globally, and there is a paucity of research data on COVID‐19 in Africa. In light of this background, there is an urgent need to review what is known so far about the disease and highlight gaps in the context of the African continent, especially the peculiarity of the Nigerian situation. The aim of the present study was to review the current available literature on COVID‐19 in relation to obstetric practice in the Nigerian context, identify gaps, and make recommendations.
2. COVID‐19 AND HEALTHCARE IN NIGERIA
Expectedly, health workers in Nigeria have been hit by the pandemic. Currently, over 800 Nigerian healthcare workers are infected with the virus. 9 As at June 22, 2020, 910 medical doctors had been quarantined for the disease, with 239 of them testing positive for the virus. Ten Nigerian doctors have died from COVID‐19, the first being an obstetrician, who died at Lagos University Teaching Hospital (LUTH), Idi‐Araba, Lagos, on April 15, 2020, after exposure to a patient with COVID‐19 in his private clinic. 10 The above situation gives a peek into the COVID‐19 pandemic as it affects medical doctors and, by extension, healthcare workers in Nigeria.
2.1. COVID‐19 and pregnancy
A major concern for the obstetrician is the effect of COVID‐19 on the pregnant patient and her unborn baby. There is currently no evidence that pregnant women are at higher risk of the disease compared to the general population; therefore, there is also no evidence of intrauterine fetal infection and currently no data suggesting an increased risk of congenital malformation, miscarriage, or early pregnancy loss in association with COVID‐19. 11 This is reassuring, especially so for the obstetrician in Nigeria, where the baseline maternal and perinatal morbidity and mortality are already high.
However, malaria fever is endemic in Nigeria and is the commonest cause of fever in pregnant women. This underscores the diagnostic challenge of the disease in the obstetric patient, as many infections and infestations in pregnancy and the puerperium, including but not limited to respiratory and urinary tract infections, malaria, inflammatory conditions such as asthma, puerperal sepsis, pulmonary embolism, and peripartum cardiomyopathy share cardinal symptoms with COVID‐19. 12
2.2. COVID‐19 testing in Nigeria
The diagnostic dilemma of COVID‐19 in the obstetric patient is compounded by the fact that testing in Nigeria is not only limited, but also restricted. The few rapid diagnostic tests with high sensitivity and specificity are only available in high‐resource countries. 13 Testing in Nigeria is currently limited to suspected cases of COVID‐19, defined by WHO as “a patient with acute respiratory illness (fever and at least one sign/symptom of respiratory disease (e.g., cough, shortness of breath)), AND with no other etiology that fully explains the clinical presentation AND a history of travel to or residence in a country/area or territory reporting local transmission of COVID‐19 disease during the 14 days prior to symptom onset; OR a patient with any acute respiratory illness AND having been in contact with a confirmed or probable COVID‐19 case in the last 14 days prior to onset of symptoms; OR a patient with severe acute respiratory infection (fever and at least one sign/symptom of respiratory disease (e.g., cough, shortness of breath)) AND requiring hospitalization AND with no other etiology that fully explains the clinical presentation”. 14
An obstetric patient who tested positive and eventually died of COVID‐19, the first fatality from the disease in the Lagos State University Teaching Hospital (LASUTH), Lagos, the epicenter of COVID‐19 in Nigeria, did not exactly fulfil this definition and yet on testing, based on clinical suspicion, she was positive. This lends credence to calls to expand testing in Nigeria, where out of an estimated population of over 200 million, only 125 090 tests have been completed as of June 26, 2020. 8 Put more appropriately, since the first case of COVID‐19 was confirmed in Nigeria 4 months ago, on February 27, 2020, less than 1% of Nigeria’s total population had been tested. Ghana and South Africa, with far fewer citizens, have carried out over 190 000 and 560 000 tests, respectively. 15 Currently, there are only 23 COVID‐19 testing laboratories located across 14 out of 36 states of Nigeria, including the FCT, serving a population of over 200 million people. 16
2.3. Attitude and perception of Nigerians towards COVID‐19
There are cases in Nigeria of patients hiding their travel history from their managing doctors. The implication of this is that such patients who would hitherto have fulfilled the COVID‐19 suspected case definition criteria, and tested in line with the country’s testing protocol, would most probably be admitted and managed for other benign conditions without a suspicion of COVID‐19. This portends grave danger for not only the doctors but also for all other healthcare workers and patients who would come into contact with such patients.
There are also reports of persons absconding after testing positive for the coronavirus, all with a view to avoid being taken to an isolation center. Quarantine measures are being flouted, as there are cases of persons with a travel history to high‐risk countries refusing to go into the stipulated 14 days of isolation upon return from such countries. These people pose a risk to other members of the community, who, after exposure to such contacts, may present asymptomatically to the hospital, further propagating the spread of the virus.
2.4. Obstetric practice in Nigeria during the COVID‐19 pandemic
The Society of Gynaecology and Obstetrics of Nigeria (SOGON) has issued a practice guidance aimed at preventing the spread of coronavirus while delivering obstetric care during the pandemic. 17 The guidance recommends that duty rosters be reorganized to limit hospital contact of medical personnel. This has been difficult to implement in many obstetric units across the country due to a gross shortage of manpower predating the COVID‐19 pandemic. There are 39 qualified medical doctors per 100 000 people (0.4 per 1000) in Nigeria. 18 The implication of this is that aside from the elderly practitioners, especially those aged 60 years or above, who are strongly advised to work from home, all or most of the other cadres of doctors in obstetric units across the country still report for duty daily.
Telephone consultations are recommended for non‐emergency cases, to prevent patients visiting the hospital unnecessarily. 17 This is not totally realistic as there are currently 25–40 million smartphone users in Nigeria, representing less than 20% of the country’s total population. 19 The experience therefore is that the larger majority of patients who do not have phones still present to obstetric units across the country, even for non‐emergencies. Most of the patients who do have phones do not utilize the telephone consultation services due to poor dissemination of information on the availability of these services and the financial constraints of purchasing airtime. More so, the bulk of these patients are used to presenting to the hospital without having to first call hospital telephone lines, whether for emergencies or non‐emergencies.
It is also recommended by SOGON that all obstetric units organize drills for maternity staff on the management of suspected and confirmed cases of COVID‐19. 17 Nigeria, with a healthcare workforce of over 390 000 (extrapolated from the Nigerian health workforce density of 1.95 per 1000 population, 20 currently has only about 25 000 of her health workers trained on the prevention, control, and management of COVID‐19. 21 This number represents a meagre 6.4% of the total Nigerian healthcare workforce.
In line with general recommendations on social distancing, SOGON equally advises that overcrowding in waiting and consulting rooms should be avoided, and a safe distance should be maintained between/among staff and patients during waiting and consultations. 17 Clinics and consulting rooms in the tropics are mostly small, making safe social distancing difficult.
Frequent and proper handwashing with soap, as well as use of alcohol‐based hand sanitizers, by both patients and hospital staff is strongly encouraged. 17 However, one‐third of Nigeria’s population do not have access to clean water 22 and many hospitals do not have a constant supply of running water. 23 Furthermore, hand sanitizers are not readily available/restocked in hospitals, meaning that doctors and other healthcare workers have to make provision for personal hand sanitizers, which are sold at inflated prices due to an increase in demand.
Hospital units across the country do not have enough infrared thermometers, which are important for basic temperature screening. Even where there is reasonable ground for suspicion that the patient has risk factors, there are not enough holding bays in hospitals across the country, where further evaluation of such patients can be carried out to minimize exposure of other patients and healthcare workers. Worse still, there is a gross shortage of bed spaces in isolation centers, whose number is disproportionate to the number of positive cases. 21 It is also pertinent to note that the available isolation centers in the country are not equipped for the care of the obstetric patient, both in terms of facilities and manpower. Ventilators, which may be required to support the life of infected patients, are very scarce in Nigeria, as in other African countries. 24
As part of the preventive measures against COVID‐19, outpatient clinics and elective surgeries in most other medical subspecialties have been postponed. In obstetric units, however, the labor rooms have remained open, and antenatal clinics and elective cesarean sections are still being run/performed due to the fact that pregnancy is a time‐bound condition. Obstetricians have to run these clinics and perform these surgeries even in the face of scarce/barely available personal protective equipment (PPE), including appropriate surgical masks and goggles. Doctors have had to purchase these PPE kits (sold at exorbitant prices) either out of their own pockets or pass down the cost of such purchases to the mostly indigent patients. At other times, PPE is improvised.
On a positive note, the Nigerian government has recently made significant efforts in increasing the supply of PPE kits to hospital units across the country. Even though these kits are still grossly inadequate, the government has taken a step in the right direction. The government has also provided group life insurance for health workers and has commenced payments of special COVID‐19 hazard allowances to healthcare workers in the country.
3. COVID‐19 PREVENTIVE MEASURES IN NIGERIA: THE CURRENT SITUATION
The Nigerian government declared a two‐week lockdown on March 30, 2020, which was extended for another 2 weeks on April 13, 2020. 25 This had severe economic consequences on families, mostly so because the majority of Nigerians are either unemployed or work in the informal sector, depending on daily earnings for sustenance. 23 , 25 Further, nearly one‐half of Nigeria’s population live below the poverty line. 25 Expectedly, therefore, many Nigerians did not obey the “stay at home” orders. 25 This was accentuated by the government’s inability to provide adequate palliation in the form of food and cash relief to citizens, to cushion the economic effect of the lockdown. 25 The government provided support to an insignificant proportion of the population. The quest for survival in the face of economic meltdown occasioned by the lockdown saw an increase in the spate of armed robberies and other criminal activities, especially in large cities like Lagos. 25 Several jobs in the private sector were lost due to downsizing.
Social distancing, another preventive measure, has been difficult to maintain because of the many slums, overcrowded settlements, and internally displaced persons (IDP) camps in the country. It is noteworthy that 62% of the urban population in sub‐Saharan Africa (including Nigeria) are slum‐dwellers, the highest in the world. 26 Public places in the country have therefore remained congested. There is no doubt that Nigeria faces a high risk of rapid transmission of the disease. There are already reports of widespread community transmission of the virus across the country. 27
Due to majorly economic considerations, the government recently relaxed the lockdown in the country. The result has been an astronomical rise in the number of COVID‐19 cases. From 1337 cases and 49 deaths on April 27, 2020, when easing of the lockdown began, the country has witnessed more than a 1500% increase in the COVID‐19 case count and 13‐fold rise in case fatalities. At this rate, it will not be long before the already underequipped and underfunded public healthcare system in the country becomes overwhelmed. 28
4. CONCLUSION
The obstetrician in Nigeria has not only an underequipped and underfunded healthcare system to contend with, but also stringent working conditions and poor physical infrastructure, with little or no motivation, and barely being provided with appropriate PPE to work with during this pandemic. In and out of hospital, both the obstetrician and the obstetric patient are constantly being put at risk of exposure to the coronavirus because preventive measures are either ineffective or non‐existent. It is a constant battle to deliver a healthy baby to a happy and satisfied mother. Even more, it is an uphill battle for the obstetrician to stay alive and uninfected in the process.
5. RECOMMENDATIONS
Prevention remains the cornerstone in the fight against COVID‐19. Intense and continuous public health education on the need to strictly adhere to preventive measures, including the use of face masks/shields, social distancing, frequent hand washing, and use of alcohol‐based hand sanitizers, is recommended.
There is an urgent need to increase the country’s capacity for testing and decentralize it in order to improve access to tests. Secondary and tertiary hospitals will need to seek alternative sources of funding to establish their own testing centers instead of waiting on the government. Rapid test kits should be made available and used to screen all women in labor. Women in labor often hyperventilate and scream/shout, thereby aerosolizing the viral droplets in asymptomatic cases. This increases the risk of infection to the obstetrician and other staff in the labor room.
Local manufacturers should be incentivized by the government to produce PPE that meets safety standards using locally available materials and appropriate technology. This will also help to provide jobs and boost the economy. The pandemic has exposed the gross inadequacies in Nigeria’s healthcare system and is therefore a wake‐up call to the need for a complete overhaul of infrastructure and services. The government will do well to increase the budget allocation for health from the current paltry 4.14% to the recommended 15% of the total budget. Private sector investment in the health sector should be encouraged. A revamped and functioning health system through public–private partnership will reduce the need for overseas medical tourism and loss of valuable foreign exchange.
The government should provide palliatives for the citizens in terms of tax waivers, suspension of utility bills and mortgage payments, soft loans for small and medium scale enterprises, and incentives and improved working conditions for healthcare workers. The telecommunications industry can help to facilitate the use of telemedicine for outpatient consultations by their subscribers. Most importantly, as citizens of the world, we must remember that we are in this together, sink or swim.
AUTHOR CONTRIBUTIONS
IO conceptualized and designed the study; IO and UA developed and wrote the manuscript; OB, KT, EO, and IJ assisted with manuscript review. All the authors have read and agreed to the final manuscript.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
Acknowledgments
IO was supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No–B 8606.RO2), Sida (Grant No: 54100029), the DELTAS Africa Initiative (Grant No: 107768/Z/15/Z). The DELTAS Africa initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa's Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (UK) and the UK Government. The statements made and views expressed are solely the responsibility of the Fellow.
REFERENCES
- 1. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID‐19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wilder‐Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: Pivotal role for old‐style public health measures in the novel coronavirus (2019‐nCoV) outbreak. Journal of Travel Medicine. 2020;27:taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patrizi A, Bardazzi F, Filippi F, Abbenante D, Piraccini BM. The covid‐19 outbreak in Italy: Preventive and protective measures adopted by the dermatology unit of bologna university hospital. Dermatol Ther. 2020. 10.1111/dth.13469 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Africa Centre for Disease Control . Outbreak Brief 23: COVID‐19 Pandemic. 2020. www.africacdc.org. Accessed June 26, 2020.
- 5. Adepoju P. Nigeria responds to COVID‐19; first case detected in sub‐Saharan Africa. Nat Med. 2020;26:444–448. [DOI] [PubMed] [Google Scholar]
- 6. Oxford Analytica . Africa remains in a precarious COVID‐19 position. Emerald Expert Briefings. (oxan‐db).
- 7. Ayebare RR, Flick R, Okware S, Bodo B, Lamorde M. Adoption of COVID‐19 triage strategies for low‐income settings. Lancet Respir Med. 2020;8:e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nigeria Centre for Disease Control . COVID‐19 Nigeria. 2020. www.covid19.ncdc.gov.ng. Accessed June 26, 2020.
- 9. Anadolu Agency . Nigeria: 800 health workers infected with COVID‐19. 2020. ww.aa.com.tr. Accessed June 26, 2020.
- 10. Sahara Reporters . Lagos Doctor Dies of COVID‐19 After Treating Infected Patient. 2020. www.saharareporters.com. Accessed May 10, 2020.
- 11. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID‐19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020;395:809–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS‐CoV‐2 infection: A single arm meta‐analysis. J Med Virol. 2020;92:612–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kavanagh MM, Erondu NA, Tomori O, et al. Access to lifesaving medical resources for African countries: COVID‐19 testing and response, ethics, and politics. Lancet. 2020;395:1735–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . Coronavirus Disease 2019 (COVID‐19) Situation Report‐61. Geneva, Switzerland: World Health Organization; 2020. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200322‐sitrep‐62‐covid‐19.pdf. Accessed 26 June, 2020. [Google Scholar]
- 15. Vanguard (Lagos) . Nigeria: COVID‐19‐With Fewer Tests, Nigeria Ties With Ghana, Algeria in Death Burden. 2020. www.allafrica.com. Accessed June 26, 2020.
- 16. Nigeria Centre for Disease Control . Facebook, 10 May 2020. Accessed May 10, 2020.
- 17. Society of Gynaecology and Obstetrics of Nigeria (SOGON) . SOGON Advice on SARS‐COV‐19 (COVID‐19) Infection‐ Practice Guidance for Members. Published 2020.
- 18. Akinyemi AI, Isiugo‐Abanihe UC. Demographic dynamics and development in Nigeria: Issues and perspectives. Afr Popul Stud. 2014;27:239–248. [Google Scholar]
- 19. Abner IP, Samuel UE, Jack AE, Kanu C. Current and potential users adoption of mobile payment technology in Nigeria. Int J Recent Technol Eng. 2019;8:4983–4991. [Google Scholar]
- 20. World Health Organization. Nigeria. Global Health Workforce Alliance. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 21. Business Day . Many COVID‐19 patients not in isolation centres due to shortage of bed space‐NCDC. 2020. www.businessday.ng. Accessed May 10, 2020.
- 22. National Bureau of Statistics and United Nations Children’s Fund . 2017 Multiple Indicator Cluster Survey 2016–2017, Survey Findings Report. Abuja, Nigeria: NBS and UNICEF; 2017. https://www.unicef.org/nigeria/sites/unicef.org.nigeria/files/2018‐09/Nigeria‐MICS‐2016‐17.pdf. Accessed June 26,2020. [Google Scholar]
- 23. Fosu GO, Edunyah G. Flattening The Exponential Growth Curve of COVID‐19 in Ghana and Other Developing Countries; Divine Intervention Is A Necessity. SSRN Electronic Journal. Published 2020. [Google Scholar]
- 24. Bowale A, Abayomi A, Idris J, et al. Clinical presentation, case management and outcomes for the first 32 COVID‐19 patients in Nigeria. Pan Afr Med J. 2020;35:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kalu B. COVID‐19 in Nigeria: A disease of hunger. Lancet Respir Med. 2020;8:556–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Habitat UN. State of The World Cities 2012/2013: Prosperity of Cities. Abingdon, UK: Routledge; 2013. https://sustainabledevelopment.un.org/content/documents/745habitat.pdf. Accessed June 26, 2020. [Google Scholar]
- 27. Okunade KS, Makwe CC, Akinajo OR, et al. Good clinical practice advice for the management of pregnant women with suspected or confirmed COVID‐19 in Nigeria. Int J Gynecol Obstet. 2020. 10.1002/ijgo.13278 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Quartz Africa . Nigeria is easing its coronavirus lockdown at what could be the worst possible time. 2020. www.qz.com. Accessed May 10, 2020.


