Abstract
Objective
To provide a descriptive account of the challenges and administrative preparedness for establishing and sustaining safe obstetric services during the COVID‐19 pandemic at Topiwala National Medical College & BYL Nair Charitable Hospital (NH), Mumbai, India.
Methods
The management of pregnant women with COVID‐19 was implemented as per international (WHO, RCOG, ACOG) and national (Indian Council of Medical Research) recommendations and guidelines at an academic, tertiary care, COVID‐19 hospital in India.
Results
Using a multidisciplinary approach and active engagement of a multispecialty team, obstetric services were provided to over 400 women with laboratory‐confirmed COVID‐19. A sustainable model is established for providing services to pregnant women with COVID‐19 in Mumbai Metropolitan Region, India.
Conclusion
With limited resources, it is possible to set up dedicated maternity services, aligned to international guidelines, for safe pregnancy outcomes in COVID‐19 settings. This COVID‐19 hospital addressed the challenges and implemented several known and novel methods to establish and sustain obstetric services for women with COVID‐19. The model established in the present study can be replicated in other low‐ and middle‐income countries.
Keywords: Administrative challenges, Cesarean, Coronavirus, COVID‐19 disease, Dedicated COVID‐19 facility, Maternity, Personal protective equipment, SARS‐CoV‐2
Short abstract
A sustainable model is established using a multidisciplinary approach for providing obstetric services to over 400 women with COVID‐19 in Mumbai Metropolitan Region, India.
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is caused by severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2), first identified in China. 1 In India, the first confirmed case of COVID‐19 was reported in the state of Kerala on January 30, 2020. 2 On March 11, 2020 two cases were admitted to Kasturba Hospital for Infectious Diseases (KH), Mumbai. Since then, the total number of cases has increased to more than 600 000 with over 18 000 deaths at July 4, 2020, and the number continues to rise. 3 This pandemic has posed a daunting challenge to healthcare systems across the world due to its magnitude, severity, the rapidity of spread, and unavailability of any previous scientific data regarding the disease, and thereby questioning the resilience of healthcare systems. India has a population of more than 1.3 billion population and the healthcare system is currently under crisis due to the COVID‐19 pandemic. The aim of the present study was to describe the administrative challenges, solutions for establishing a dedicated COVID‐19 hospital, experiences of delivering over 400 women with COVID‐19, and a sustainable model for addressing a public health emergency such as COVID‐19 in India.
1.1. The existing public healthcare system in Mumbai Metropolitan Region (MMR), India
Public healthcare in MMR is mainly provided and maintained by the Municipal Corporation of Greater Mumbai (MCGM), Government of Maharashtra, and is based on a traditional three‐tier system with primary, secondary, and tertiary care centers. It has a network of 16 municipal general hospitals, six specialty hospitals, 29 maternity homes, 175 municipal dispensaries, and 183 health posts. Peripheral hospitals (primary and secondary care centers) are linked to tertiary care centers. There are four multispecialty tertiary care centers with their respective teaching institutes including Topiwala National Medical College & BYL Nair Charitable Hospital (NH). NH was founded in 1921 and its Obstetrics and Gynaecology Department caters to approximately 17 000 antenatal outpatients and 3500–4000 deliveries per year.
2. MATERIALS AND METHODS
Written informed consent was not needed as the present study did not involve studies of patients, patient records, or volunteers. A waiver for ethical review was obtained from the Ethics Committee.
2.1. Preparedness for handling pregnant women with COVID‐19
When the COVID‐19 pandemic hit the city of Mumbai and patients started to show up at NH, the first challenge was to manage patients with COVID‐19 amid those without COVID‐19 who had already been admitted to the same institute. To enable this, administrative teams were essentially divided into four parts: on‐site changes, personnel operations, human resources, and rendering obstetric services. The core committee managed logistic problems and patient transfer calls from all over MMR 24 hours a day.
2.2. On‐site changes
2.2.1. Triage system and special screening for outpatient department (OPD)
Efficient triage of patients with COVID‐19 at the entrance to the hospital helped the hospital administration cope with patient inflow, direct necessary medical resources to efficiently manage the critically ill, and protect the safety of frontline healthcare workers (HCW) (Fig. 1). 4 It was also necessary to have a special screening area for those suspected of having COVID‐19 at the entrance of the hospital to guide patients to further management pathways. Therefore, a special screening OPD (SSO) was set up near the entrance of the hospital. All the referred patients with confirmed or suspected COVID‐19 were assessed at SSO (Fig. 2) which also has eight beds for emergency care and an ambulance bay for stabilizing critical patients. From here, patients are then directed as per the triage system. A separate path, called “Corona Path,” was created for transporting patients to the wards.
Figure 1.
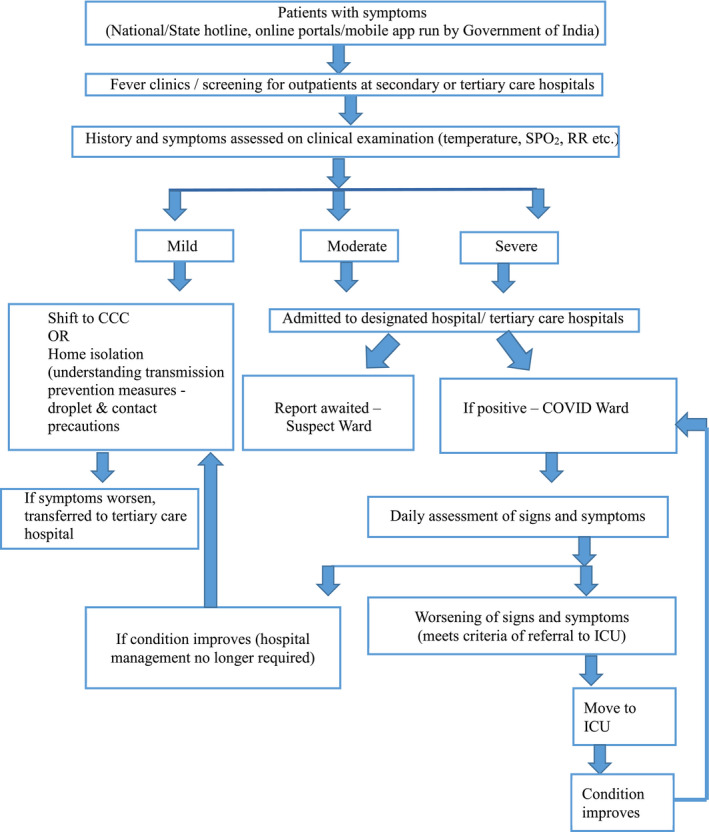
Triage system in Mumbai. Abbreviations: CCC, COVID Care Center; ICU, intensive care unit; RR, respiratory rate; SPO2, oxygen saturation.
Figure 2.
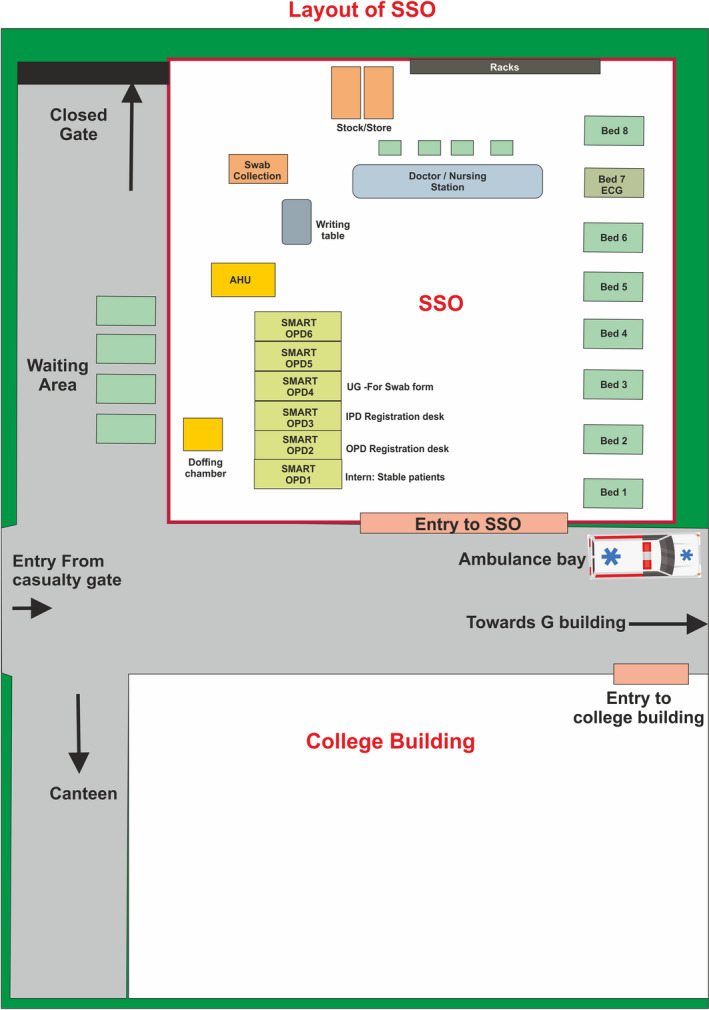
Layout of SSO. Abbreviation: SSO, special screening for outpatients.
2.2.2. Increase in beds and local Standard Operating Procedures (SOP)
NH was soon converted to a dedicated COVID‐19 facility with more than 1000 beds, including 120 maternity beds. This was done by increasing the number of beds and creating COVID‐19–compliant wards (Table 1). While managing the first few cases, there was no clarity due to the lack of pre‐existing scientific data about SARS‐CoV‐2, hence it was difficult to formulate SOPs in the beginning. The management of the disease in pregnancy was solely dependent on recently published data and experience of previous outbreaks such as SARS and Middle East respiratory syndrome (MERS). Care was provided by a multidisciplinary team including obstetricians, neonatologists, obstetrical anesthesiologists, intensivists, virologists, microbiologists, and infectious‐disease specialists, constantly adapting management protocols with respect to rapidly evolving national and international guidelines. This updated scientific information was disseminated among all the HCWs by regular meetings via videoconferencing, webinars, and sharing information on the hospital’s closed social media groups. Training sessions are carried out regularly for all HCWs to ensure that they not only receive adequate information about clinical management, but are also trained in using personal protective equipment (PPE) and undertaking infection prevention and control (IPC) measures correctly (Table 2).
Table 1.
Logistic challenges for establishing a dedicated COVID‐19 facility
| Challenges | Solutions |
|---|---|
| Managing non‐COVID‐19 patients already admitted when NH was declared a dedicated COVID‐19 facility |
|
| Shifting of resident medical doctors out of campus |
|
| OPDs needed to be moved outside the building to avoid exposure to non‐COVID‐19 patients already admitted |
|
| Preparing for infrastructure compatible with the management of COVID‐19 |
|
| Establishing a dedicated COVID‐19 facility with an increasing demand for beds |
|
| Increased demand for oxygen |
|
| Difficulty taking FHS and taking temperature |
|
| Difficulties operating or delivering while wearing PPE, such as misting on eyewear/face shields |
|
| Increased sweating and dehydration |
|
Abbreviations: BiPAP, bi‐level positive airway pressure; FHS, Fetal heart sound; HCW, healthcare worker; HFNO, high‐flow nasal oxygen; OPD, outpatient department; PPE, personal protective equipment; SSO, special screening for outpatients.
Table 2.
Challenges with human resources and training of HCWs
| Challenges | Solutions |
|---|---|
|
Keeping adequate number of treating doctors Many HCWs being quarantined due to exposure |
|
| Resident doctors’ hostel was inside the campus on the top floor where COVID‐19 patients were to be admitted |
|
| Caring for HCWs |
|
| Training frontline workers |
|
Abbreviations: HCW, healthcare worker; IPC, infection prevention and control; PPE, personal protective equipment.
2.2.3. Separate maternity space and services for COVID‐19
In the initial phase, a separate maternity space (for both confirmed and suspected cases) and a smaller neonatal intensive care unit for patients with COVID‐19 was also created in a building located at the perimeter of the hospital campus. A makeshift labor room was created by moving labor tables, oxygen cylinders, and portable lamps. With an increasing number of obstetric patients, this arrangement was upgraded to a separate maternity ward with 50 beds and an independent operation theater (OT) in the same building. Neonates were kept with the mother to ensure exclusive breastfeeding. Problems relating to infrastructure during this installation, including equipment outsourcing, logistics, engineering modifications, etc., were dealt with efficiently by the hospital administration (Table 1).
A quality check of all PPE was done regularly after noticing a tear in one of the PPE kits and seepage of blood through it during the first few deliveries. The team working with donor liaison was the bridge between clinicians’ needs and donors, which helped in preparing for infrastructure that was compatible with managing COVID‐19 (Table 1).
2.2.4. Infrastructure preparedness
In view of increased consumption of oxygen during the COVID‐19 pandemic, the oxygen capacity of the hospital was increased. Non‐invasive options, such as high‐flow nasal oxygen (HFNO) and bi‐level positive airway pressure (BiPAP), assist patients with COVID‐19 experiencing mild or moderate respiratory distress and reduce the numbers of patients requiring intubation, mechanical ventilation, and admission to the intensive care unit (ICU) for some severely ill patients. 5 These respiratory support devices were procured and were successfully used to treat patients with COVID‐19. As both BIPAP and HFNO are aerosol‐generating procedures (AGP), HCWs were trained to take the utmost care while administering either therapy.
2.3. Managing human resources and personnel operations
Since the main mode of transport, the trains, had been suspended due to a lockdown, the transport of around 1500–2000 employees was arranged by collaborating with the Brihanmumbai Electricity Supply and Transport (BEST) who dedicated their buses, in three shifts, over a period of 3 months. Fourteen bus routes were mapped exclusively for NH. Off‐site accommodation for 500 resident doctors and 300 paramedical staff staying in hospital campus was arranged to align to the rota designed to protect HCWs from continual exposure to the hospital viral load. The total number of frontline doctors was increased in collaboration with other hospitals by mobilizing their doctors to NH, giving HCWs incentives, such as pay rises, and calling back resident doctors on preparatory exam leave to resume duty (Table 2).
2.4. Rendering obstetric services
In the initial phase, the outpatient services were functional, adhering to IPC measures and transmission‐based precautions (social distancing, wearing face masks mandatory for all, allowing only one accompanying person with each patient, etc.) and keeping antenatal visits to a minimum. 6 , 7 However, as the national lockdown rules were made stringent, the outpatient service was stopped and only emergency services were continued. All elective surgical procedures were delayed in an attempt to make available the maximum ventilatory support for critical patients with COVID‐19.
2.4.1. Delivering the first mother with COVID‐19
The first two parturients with COVID‐19 were attended in one of the peripheral hospitals affiliated to NH on April 14, 2020, and subsequently admitted to NH. Before coming to NH, both were denied admission at four private hospitals due to the unavailability of a COVID‐19 infrastructure. Both delivered vaginally in a makeshift labor room. With the rise in cases of COVID‐19, NH was soon converted into a dedicated COVID‐19 facility on April 18, 2020, managing only patients with COVID‐19 with all specialties, including maternity. This mandated discharging non‐COVID‐19 patients who had already been admitted or moving them to another hospital which was an organized task between the administrative heads of NH and those of neighboring hospitals.
2.4.2. Dedicated COVID‐19 maternity facility
NH became the only tertiary care hospital designated solely for the management of pregnant patients with COVID‐19 and all their emergency care. The obstetric unit was soon functional with capacity for 120 beds, including three wards and a labor room with eight beds, stringently following the protocols set by the hospital’s IPC committee, which were consistent with guidelines given by the Ministry of Health and Family Welfare (MoHFW) as well as WHO and Centers for Disease Control and Prevention (CDC). 8 , 9 , 10 , 11
All beds were kept at a minimum distance of 1.5 m from each other, three‐layered surgical masks were given to all admitted patients, and engineering controls (installing physical barriers, curtains, or partitions) were undertaken to reduce or eliminate exposure by shielding HCWs. Environmental cleaning and disinfection procedures were followed, adhering to IPC guidelines. 9
2.4.3. Admission policy
As the pandemic evolved, the admission policy needed to be updated regularly, taking into consideration the increased inflow of patients. Therefore, the initial policy of admitting all pregnant patients with confirmed COVID‐19 was changed to admitting only those with moderate to severe symptoms and those with high‐risk pregnancies or requiring active obstetric management. This approach was endorsed by MoHFW in their home isolation guidelines, that mild cases can be managed at COVID Care Centers (CCCs), First Referral Units, Community Health Centers, sub‐district and district hospitals, or at home. 12
Severity‐based stratification of inpatients was done on detailed history and clinical examination. With the help of a multidisciplinary approach, patients with moderate to severe disease were moved to the high dependency unit/ICU, while those with mild disease were managed in the wards (Fig. 3).
Figure 3.
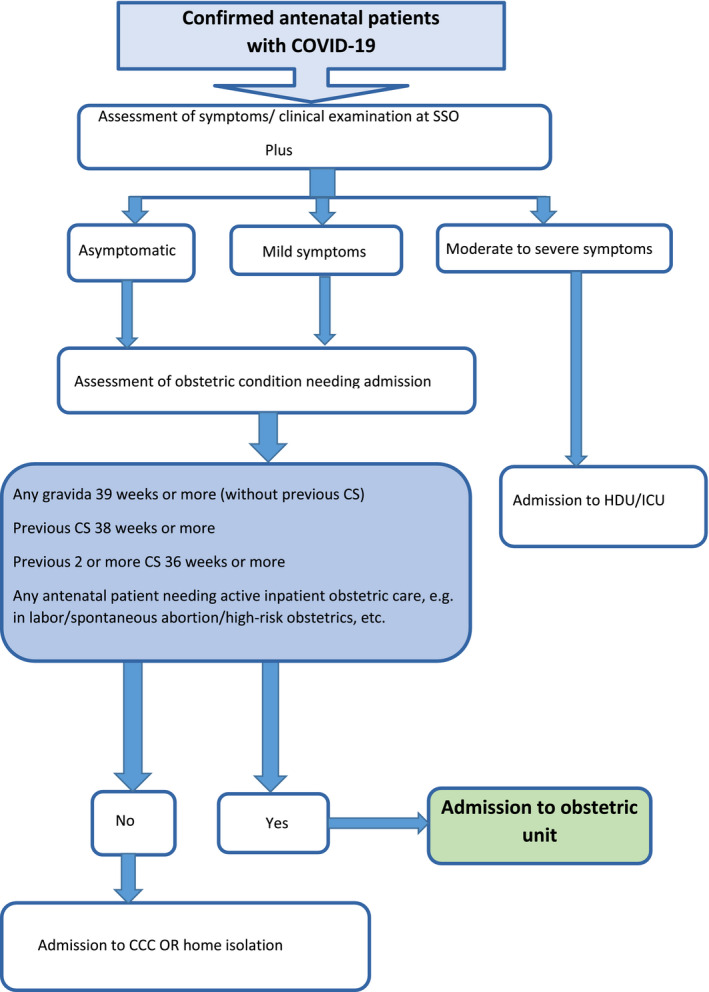
Admission policy for obstetric patients at Topiwala National Medical College & BYL Nair Charitable Hospital. Abbreviations: CCC, COVID Care Center; CS, cesarean section; HDU, high dependency unit; ICU, intensive care unit; SSO, special screening for outpatients
2.4.4. Inpatient care
Inpatient management protocols for antenatal as well as intrapartum patients were formulated and timely updated as per national 6 , 8 and international (International Federation of Gynecology and Obstetrics [FIGO], CDC, and WHO) 7 , 13 , 14 guidelines. OT protocols, including communication pathways and transport protocols, were also formulated adhering to these guidelines. 9 , 10 , 11 , 15 Although all the preparations were in place for operative intervention of patients with COVID‐19 if needed, nothing was foolproof until it was experienced first‐hand. Operating in PPE was inconvenient due to the constant misting of eyewear/face shields and the extreme heat/dehydration. Subsequently, users learned how to avoid misting and to carry on without feeling giddy. The use of electrocautery during surgery was limited and was only used with suction when required (Table 2).
Daily rounds were taken twice, assessing the symptoms and clinical findings of patients, including temperature, heart rate, respiratory rate, and oxygen saturation, thus constantly updating the discharge list of patients who can be released to CCC or into the home setting.
2.4.5. Testing strategy
Pregnant asymptomatic women with COVID‐19 are not only at risk of infecting their newborns but also pose a risk to HCWs. Considering this, the Indian Council of Medical Research (ICMR) on April 20, 2020, recommended testing for SARS‐CoV‐2 in all pregnant women residing in clusters/containment area or in large migration gatherings/evacuee centers from hotspot districts in India and presenting in labor or likely to deliver in the next 5 days. 16 This increased the rate of testing tremendously and therefore increased the number of referrals of obstetric patients with confirmed COVID‐19 and the rate of admission to NH maternity unit. In its recent testing strategy, ICMR advocates testing only symptomatic patients (symptoms of influenza‐like illness) and asymptomatic direct or high‐risk contacts of confirmed cases. It also advises not to delay emergency procedures, such as delivery, due to lack of test and to apply the same criteria while sending their samples for testing. 17
The testing strategy for inpatients was also updated accordingly. Where the oropharyngeal swabs for reverse transcription polymerase chain reaction (RT‐PCR) were initially sent every 48 hours for all patients, this then changed to sending them only on a case‐by‐case basis where repeat swabs were sent for critically ill or immunocompromised patients before discharging them from hospital. 18
Sample collection, packaging, and transport of all specimens obtained from all wards were strictly supervised for adherence to the guidelines set by MoHFW. 19
2.4.6. Discharge policy
The decision to discharge was taken on symptom‐ and test‐based criteria, where initially, as per MoHFW and WHO guidelines, the patient was only discharged after receiving two consecutive negative RT‐PCR tests done on oropharyngeal swabs, sent 24 hours apart. These recommendations were based on the knowledge and experience with similar coronaviruses, including those that caused SARS and MERS. 20 , 21
This approach burdened the testing capacity. Hence the decision to discharge was then modified to only symptom‐based criteria, where asymptomatic patients and those with mild to moderate disease were discharged after being asymptomatic for 10 days from the onset of first symptoms, and were advised to self‐isolate and take transmission‐based precautions at home for a further 14 days, which later changed to 7 days as per the MoHFW revised discharge policy after 08.05.2020. 21 An undertaking to this effect was signed by all patients. 12 Patients for whom it was not possible to follow those precautions at home were discharged to a CCC.
Asymptomatic antenatal inpatients were retested by RT‐PCR at day 9 of admission or 10 days after onset of symptoms. If the result was negative, they were transferred to another non‐COVID‐19 facility in the city. This is being practiced with the understanding that the documented report of negative RT‐PCR would be needed for admission to non‐COVID‐19 hospitals.
CDC describes symptom‐based strategies (similar to WHO), test‐based strategies (still requiring at least two consecutive negative results from respiratory specimens collected at least 24 hours apart), and time‐based strategies (at least 10 days have passed since the date of their first positive COVID‐19 diagnostic test) to decide discontinuation of isolation and transmission‐based precautions. 22 , 23 The Department of Health and Social Care in the UK, with the NHS, has also accepted a rapid discharge policy to ensure capacity to support patients with acute healthcare needs. 24
2.5. The yield
NH is the only tertiary care hospital in MMR that has been converted into a dedicated COVID‐19 specialty hospital. The impact of the pandemic was so high that the number of COVID‐19 deliveries at NH reached 100 within a month of it starting its dedicated COVID‐19 maternity services. NH has successfully managed more than 600 obstetric patients, conducting 412 deliveries including seven pairs of twins and one set of triplets so far. There were no maternal mortalities among those delivered; however, there were four maternal mortalities due to unrelated causes. In this battle against the COVID‐19 pandemic, since the day NH became a dedicated COVID‐19 facility, only two frontline HCWs contracted COVID‐19. Thus, NH has managed to keep its HCWs safe, with the lowest rate of COVID‐19 infection among them. Thus, handling operations of this magnitude was more of a lesson in management than just a lesson in medicine.
3. Conclusion
A sustainable model was established using a multidisciplinary approach and active engagement of a multispecialty team, and obstetric services were provided to more than 600 pregnant women with COVID‐19 in MMR, India. The COVID‐19 facility addressed the challenges and implemented several known and novel methods to establish and sustain obstetric services for women with COVID‐19. Based on this experience, it is recommended that the model is implemented in other low‐ and middle‐income countries with low‐resource settings.
Author Contributions
NM, RP, and SP designed the study. NM, RP, AS, SP, PK, SR, and SM wrote the manuscript. SP, SR, AS, SCM, SM, GS, and MJ supervised the study and were administrators. PK, AT, PL, and SS collected the data. NM, RP, and AS analyzed the data and information and wrote the first draft. All the authors revised the manuscript.
Conflicts of Interest
The authors have no conflicts of interest.
Acknowledgments
The authors thank Commissioner MCGM and other administrative officials from MCGM and TNMC for administrative support in establishing a dedicated COVID‐19 facility. The authors acknowledge the network of National Registry of Pregnant women with COVID‐19 in India (PregCovid Registry, CTRI/2020/05/025423). The authors acknowledge Rahul Gajbhiye, ICMR‐NIRRH, Mumbai, for his guidance on the design of the study, critical review of the drafts, and revision of the manuscript; Henal Shah and Seema Kini from the HR team at TNMC; and Omkar Khandkar and Sanjay Swami for their help with data and images, respectively.
References
- 1. World Health Organization . Novel coronavirus – China. Jan 12, 2020. http://www.who.int/csr/don/12‐january‐2020‐novel‐coronavirus‐china/en/. Accessed July 02, 2020.
- 2. World Health Organization, India . Novel Coronavirus (2019‐nCoV); Situation report 2. February 6, 2020. https://www.who.int/docs/default‐source/wrindia/india‐situation‐report‐2.pdf?sfvrsn=962f294b_0. Accessed July 02, 2020.
- 3. COVID‐19 India ‐ Statewise Status . Ministry of Health and Family Welfare, Government of India. 2020. https://www.mohfw.gov.in/. Accessed July 04, 2020.
- 4. World Health Organization, Regional Office for the Western Pacific . Algorithm for COVID‐19 triage and referral: patient triage and referral for resource‐limited settings during community transmission. Manila: WHO, Regional Office for the Western Pacific; 2020. https://apps.who.int/iris/handle/10665/331915. Accessed June 29, 2020. [Google Scholar]
- 5. Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID‐19). Intensive Care Med. 2020;46:854–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. The Indian Council for Medical Research . Guidance for Management of Pregnant Women in COVID‐19 Pandemic. April 2020. https://www.icmr.gov.in/pdf/covid/techdoc/Guidance_for_Management_of_Pregnant_Women_in_COVID19_Pandemic_12042020.pdf. Accessed June 29, 2020.
- 7. Poon LC, Yang H, Kapur A, et al. Global interim guidance on coronavirus disease 2019 (COVID‐19) during pregnancy and puerperium from FIGO and allied partners: Information for healthcare professionals. Int J Gynecol Obstet. 2020;149:273–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Government of India Ministry of Health and Family Welfare, Directorate General of Health Services (EMR Division) . Clinical Management Protocol: COVID‐19, Version 3. June 13, 2020. https://www.mohfw.gov.in/pdf/ClinicalManagementProtocolforCOVID19.pdf. Accessed June 29, 2020.
- 9. Government of India Ministry of Health and Family Welfare . National guidelines for infection prevention and control in healthcare facilities. January 2020. https://www.mohfw.gov.in/pdf/National%20Guidelines%20for%20IPC%20in%20HCF%20‐%20final%281%29.pdf. Accessed June 29, 2020.
- 10. World Health Organization . Cleaning and disinfection of environmental surfaces in the context of COVID‐19. May 16, 2020. https://www.who.int/publications/i/item/cleaning‐and‐disinfection‐of‐environmental‐surfaces‐inthe‐context‐of‐covid‐19. Accessed June 29, 2020.
- 11. Centers for Disease Control and Prevention . Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID‐19) in Healthcare Settings. May 22, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/infection‐control‐recommendations.html. Accessed June 29, 2020.
- 12. Government of India Ministry of Health and Family Welfare . Revised guidelines for Home Isolation of very mild/pre‐symptomatic COVID‐19 cases. May 10, 2020. https://www.mohfw.gov.in/pdf/RevisedguidelinesforHomeIsolationofverymildpresymptomaticCOVID19cases10May2020.pdf. Accessed June 29, 2020.
- 13. World Health Organization . Clinical management of COVID‐19, Interim guidance. May 27, 2020. https://www.who.int/publications/i/item/clinical‐management‐of‐covid‐19. Accessed June 29, 2020.
- 14. Centers for Disease Control and Prevention . Coronavirus Disease 2019 (COVID‐19) Considerations for Inpatient Obstetric Healthcare Settings. May 20, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/inpatient‐obstetric‐healthcare‐guidance.html. Accessed June 29, 2020.
- 15. Centers for Disease Control and Prevention . Guidelines for Environmental Infection Control in Health‐Care Facilities (2003). Updated July 2019. https://www.cdc.gov/infectioncontrol/guidelines/environmental/index.html. Accessed June 29, 2020.
- 16. ICMR . Strategy for COVID‐19 testing for pregnant women in India (Version 1, dated 20/04/2020). Published online April 20, 2020. https://www.icmr.gov.in/pdf/covid/strategy/archive/COVID19_Testing_Strategy_for_Pregnant_Women.pdf. Accessed June 29, 2020.
- 17. ICMR . Strategy for COVID‐19 testing in India (Version 5, dated 18/05/2020) https://www.icmr.gov.in/pdf/covid/strategy/Testing_Strategy_v5_18052020.pdf. Accessed June 29, 2020.
- 18. World Health Organization . Criteria for releasing COVID‐19 patients from isolation. Scientific brief. June 17, 2020. https://www.who.int/news‐room/commentaries/detail/criteria‐for‐releasing‐covid‐19‐patients‐from‐isolation. Accessed June 29, 2020.
- 19. Government of India Ministry of Health and Family Welfare . Guidance on specimen collection, processing, transportation, including related biosafety procedures. January, 2020. https://www.mohfw.gov.in/pdf/5Sample%20collection_packaging%20%202019‐nCoV.pdf. Accessed June 29, 2020.
- 20. Government of India Ministry of Health and Family Welfare . Old discharge policy. March 17, 2020. https://www.mohfw.gov.in/pdf/Corona%20Discharge‐Policy.pdf. Accessed June 29, 2020.
- 21. Government of India Ministry of Health and Family Welfare . Revised discharge policy for COVID‐19. May 8, 2020. https://www.mohfw.gov.in/pdf/ReviseddischargePolicyforCOVID19.pdf. Accessed June 29, 2020.
- 22. Centers for Disease Control and Prevention . Symptom‐Based Strategy to Discontinue Isolation for Persons with COVID‐19. May, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/community/strategy‐discontinue‐isolation.html. Accessed June 29, 2020.
- 23. Centers for Disease Control and Prevention . Discontinuation of Transmission‐Based Precautions and Disposition of Patients with COVID‐19 in Healthcare Settings (Interim Guidance). May, 2020. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/disposition‐hospitalized‐patients.html. Accessed June 29, 2020.
- 24. Public Health England . COVID‐19 Hospital Discharge Service Requirements. March 19 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/880288/COVID‐19_hospital_discharge_service_requirements.pdf. Accessed June 29, 2020.


