Short abstract
Description of the emergency approach used for management of an abdominal pregnancy during the COVID‐19 pandemic.
Keywords: Abdominal pregnancy, COVID‐19, Decidual tissue, Ectopic pregnancy, Hemoperitoneum, Methotrexate
Abdominal pregnancy is a rare type of ectopic pregnancy with an incidence of 1:10 000 to 1:30 000 women. 1 Several different locations have been reported, including the pouch of Douglas, pelvic sidewall, bowel, broad ligament, omentum, and spleen. 2 , 3 Most abdominal pregnancies are diagnosed after presenting with various complications; however, in a few cases it may remain asymptomatic and is rarely established before surgery. 4 Institutional Review Board approval was not required for this case report; written informed consent was obtained.
A 33‐year‐old primigravida presented at 14 weeks of pregnancy with persistent abdominal pain lasting 15 days. The patient had not attended hospital sooner for fear of coronavirus disease 2019 (COVID‐19) infection. The patient’s history was unremarkable. On admission, hemoglobin serum level was 6 g/dL, blood pressure was 80/50 mm Hg, and serum beta‐hCG level was 88 000 IU/L. The patient’s lower abdomen was significantly tender at palpation. Ultrasonography revealed an empty uterus; however, a fetus with cardiac activity was evident posterior to the uterus between the intestinal loops. Massive blood clots appeared to be present in the pouch of Douglas. The patient was hospitalized at leopoldo mandic hospital.
Laparoscopy was performed and around 2000 mL of blood was drained. The fetus was located behind the posterior wall of the uterus, close to the rectosigmoid junction (Fig. 1). The placental tissue was strictly adherent to the sigmoid mesocolon, pouch of Douglas, perimetrium and left adnexa. Decidual tissue could not be removed completely. Owing to neovascularization invading the sigmoid mesocolon and omental vessels, a delicate approach with forceps and bipolar scissors caused significant blood loss and a drain was placed. Three units of packed red blood cells and one unit of plasma were transfused. Postoperative methotrexate was given to treat incomplete resection of the decidual tissue.
Figure 1.
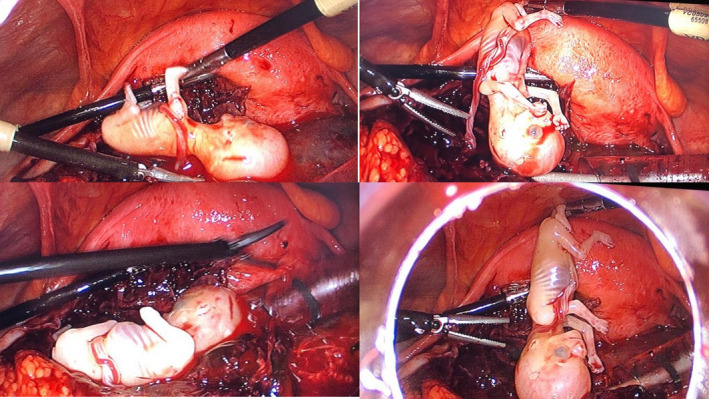
Fetus located behind the posterior wall of the uterus, close to the rectosigmoid junction.
Given the risk of COVID‐19 infection, the patient underwent chest X‐ray and nasopharyngeal swab before surgery. As both test results were negative, the patient received 50 mg/m2 methotrexate intramuscularly within 24 hours after surgery. The patient was discharged after 3 days (serum beta‐hCG 2900 IU/L). Serum beta‐hCG had decreased to less than 5 IU/L at 21 days. No residual lesion was detected with ultrasonography at the 6‐week follow‐up.
In general, image magnification during laparoscopy allows complete removal of placental cotyledons from the peritoneal surface, thereby avoiding possible postoperative bleeding, infection, and sepsis resulting from retention of placental remnants. However, given the tenaciously adherent decidual tissue in the present case and the negative test result for COVID‐19, the patient was managed with methotrexate rather than removing all of the placenta, with the aim of preventing possible complications of infection during the pandemic, when availability of operating rooms and packed red blood cells was limited.
AUTHOR CONTRIBUTIONS
GRD was responsible for conception of the study and writing the manuscript. AB was responsible for performing the surgery and data collection. GDB was responsible for the surgery, case management, literature review, and reviewing the manuscript. FA revised the manuscript. FA wrote also the paper and make photos.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
REFERENCES
- 1. Yoder N, Tal R, Martin JR. Abdominal ectopic pregnancy after in vitro fertilization and single embryo transfer: A case report and systematic review. Reprod Biol Endocrinol. 2016;14:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cosentino F, Rossitto C, Turco L, et al. Laparoscopic management of abdominal pregnancy. J Minim Invasive Gynecol. 2017;24:724–725. [DOI] [PubMed] [Google Scholar]
- 3. Hailu FG, Yihunie GT, Essa AA, Tsega WK. Advanced abdominal pregnancy, with live fetus and severe preeclampsia: Case report. BMC Pregnancy Childbirth. 2017;17:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rahaman J, Berkowitz R, Mitty H, Gaddipati S, Brown B, Nezhat F. Minimally invasive management of advanced abdominal pregnancy. Obstet Gynecol. 2004;103:1064–1068. [DOI] [PubMed] [Google Scholar]


