SARS‐CoV‐2 (COVID‐19) infection in pregnancy increases the likelihood of hospitalization, admission to intensive care, and receipt of mechanical ventilation as compared with nonpregnancy. 1 On June, 21, 2020, a 33‐year‐old pregnant woman (274 weeks of gestation) with SARS‐CoV‐2 infection presented to Hospital San José Tec Salud, Monterrey, México, with respiratory distress and oxygen saturation below 90% (room oxygen). She had developed fever, asthenia, adynamia, myalgia, dry cough, anosmia, and diarrhea 7 days prior to admission. Her past medical history was significant for smoking, which she had stopped at 4 weeks of gestation.
On admission, the woman was treated with oxygen therapy (8 L/min) via a nasal cannula; chest X‐ray showed bilateral interstitial infiltrates. Laboratory data revealed leukopenia with lymphopenia, raised interleukin‐6 and C‐reactive protein, and compensated respiratory alkalosis (Fig. 1).
Figure 1.
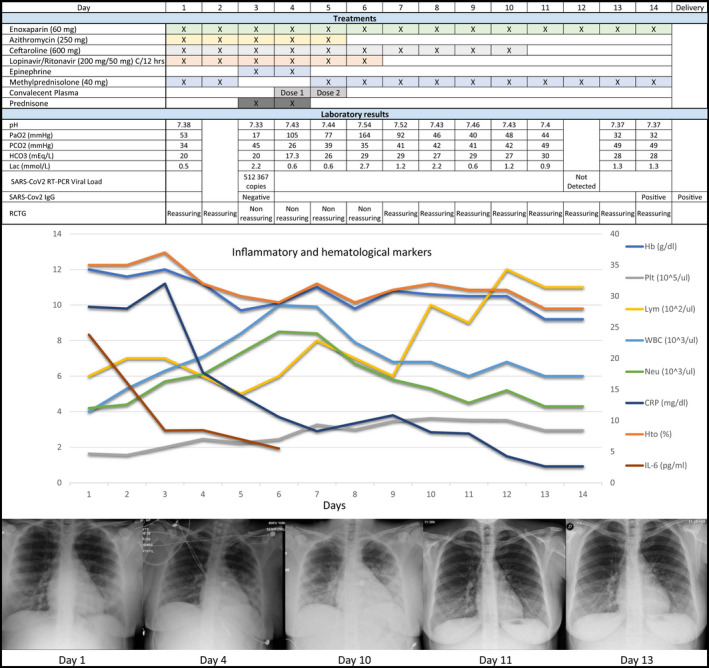
Clinical progress of a critically ill obstetric patient with SARS‐CoV‐2 infection after administration of convalescent plasma. A 33‐year‐old pregnant patient (274 weeks of gestation) with SARS‐CoV‐2 infection developed acute respiratory deterioration despite administration of antiviral, antibiotic, and corticosteroid therapy. She was treated with two doses of convalescent plasma, resulting in an improvement in respiratory parameters and inflammation markers, and a consecutive radiologic improvement in lung appearance
Therapy was initiated with enoxaparin (60 mg), azithromycin (250 mg), ceftaroline (600 mg), lopinavir/ritonavir (400 mg/100 mg), methylprednisolone (40 mg), and supportive care (antipyretics, analgesics, fluids, and nutrition). On hospital day 2 (HD2), saturation decreased and chest X‐ray showed an extension and worsening density of interstitial infiltrates. On HD3, the woman was intubated and placed on mechanical ventilation; intermittent pressure support with intravenous ephedrine was provided as needed owing to intermittent periods of hypotension and bradycardia. Continuous fetal heart rate monitoring was non‐reassuring. Serum IgG against SARS‐Cov‐2 was undetectable. Despite medical treatment, her condition continued to deteriorate. A multidisciplinary team discussed the case and the possible therapeutic interventions. We sent a request to the hospital Bioethics Committee for compassionate use of convalescent plasma. The request was approved. Methylprednisolone was discontinued and prenatal corticosteroid therapy was initiated. The treatment plan and options were discussed with the patient's legally authorized representative who consented to proceed with the administration of convalescent plasma.
Two doses of convalescent plasma from a compatible donor with confirmed anti‐SARS‐CoV‐2‐IgG were transfused (24‐h interval, HD4–HD5). Prepartum testing for fetal well‐being was reassuring both before and after each transfusion, and no adverse effects were identified. An improvement in oxygen requirement was noted on HD6. On HD7, the woman passed a trial of spontaneous breathing and was placed on non‐invasive positive pressure ventilation; ritonavir/lopinavir and azithromycin were discontinued. She was placed on supplemental oxygen via a nasal cannula on HD9, and successfully transitioned to room air on HD12. On HD14, she was discharged from the hospital. A week later, chest X‐ray showed absence of bilateral interstitial infiltrates and anti‐SARS‐CoV‐2 IgG was detected. At 39 weeks of gestation, a female neonate with growth restriction was delivered vaginally; growth restriction has been previously associated with SARS‐CoV‐2 infection in pregnancy. 2
Administration of convalescent plasma is associated with maternal survival. 3 , 4 Convalescent plasma may be a safe alternative for pregnant women who have rapid deterioration of respiratory function and a seronegative state in which the fetus shows distress parameters.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
AUTHOR CONTRIBUTIONS
The patient in this case study was supervised by GM, CV, SC, MM, JC, and SS. DD and SC were involved in recruitment of the convalescent plasma donor. CV, GM, and DD wrote the final manuscript.
ACKNOWLEDGMENTS
The authors acknowledge the multidisciplinary team of the COVID‐19 task force at Hospital San José Tec Salud, Mexico, for their continuous support and input into patient treatment. The authors thank the Blood Bank and the convalescent plasma donor for their contribution.
REFERENCES
- 1. Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory‐confirmed SARS‐CoV‐2 infection by pregnancy status – United States, January 22–June 7, 2020. MMWR. 2020;69(25):769‐775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dashraath P, Wong JLJ, Lim MXK, et al. Coronavirus disease 2019 (COVID‐19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222:521‐531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson J, Schauer J, Bryant S, Graves CR. The use of convalescent plasma therapy and remdesivir in the successful management of a critically ill obstetric patient with novel coronavirus 2019 infection: a case report. Case Rep Women’s Heallth. 2020;27:e00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grisolia G, Franchini M, Glingani C, et al. Convalescent plasma for coronavirus disease 2019 in pregnancy: a case report and review. Am J Obstet Gynecol MFM. 2020;2(3):100174. [DOI] [PMC free article] [PubMed] [Google Scholar]


