Abstract
Objective
Investigate the quality of maternal and newborn care (QMNC) during childbirth in the first year of COVID‐19 pandemic in Italy, from the mothers' perspective, as key service users.
Methods
Women who gave birth in an Italian facility from March 1, 2020 to February 29, 2021 answered an online questionnaire including 40 WHO Standard‐based Quality Measures. Descriptive and multivariate quantile regression analyses were performed.
Results
In total, 4824 women were included, reporting heterogeneity of practices across regions: among 3981 women who underwent labour 78.4% (63.0%–92.0%) were not allowed a companion of choice, 44.6% (28.9%–53.3%) had difficulties in attending routine antenatal visits, 36.3% (24.9%–61.1%) reported inadequate breastfeeding support, 39.2% (23.3%–62.2%) felt not involved in medical choices, 33.0% (23.9%–49.3%) experienced unclear communication from staff, 24.8% (15.9%–39.4%) were not always treated with dignity and 12.7% (10.1%–29.3%) reported abuses. Findings in the group of women who did not experience labour were substantially similar. Multivariate analyses confirmed a significant lower QMNC index for regions in southern Italy compared to North and Central regions.
Conclusion
Mothers reported substantial inequities in the QMNC across Italian regions. Future studies should monitor QMNC over time. Meanwhile, actions to ensure high QMNC for all mothers and newborns across Italy are urgently required.
Keywords: childbirth, COVID‐19, European region, hospital, maternal, newborn, quality of care, questionnaire, survey
Short abstract
Mothers giving birth in the first year of the COVID‐19 pandemic reported substantial inequities across Italian regions in the QMNC around the time of childbirth.
Abbreviations
- CS
caesarean section
- ECS
emergency caesarean section
- GDPR
General Data Protection Regulation
- HCP
health care provider
- IQRs
interquartile ranges
- IVB
instrumental vaginal birth
- NICE
National Institute of Health and Care Excellence
- OB‐GYN
obstetrician‐gynecologist doctor
- OR
Odds ratios
- PPE
personal protective equipment
- QMNC
quality of maternal and newborn care
- SEs
Standard errors
- SVB
spontaneous vaginal birth
- WHO
World Health Organization
1. INTRODUCTION
Published studies documented a deterioration in maternal and newborn health indicators in Italy during the COVID‐19 pandemic when compared to previous periods: a decrease in access to maternal health services and breastfeeding rates, and an increase in the number of stillbirths, in the prevalence of ruptured ectopic pregnancy and induction of labour have been reported. 1 , 2 , 3 , 4 Evidence also showed higher levels of anxiety and post‐partum depression among women in Italy during the COVID‐19 pandemic compared to previous periods, albeit with variations depending on the setting. 4 , 5 , 6
Even before the COVID‐19 pandemic, evidence had highlighted gaps in the quality of maternal and newborn care (QMNC) in Italy, with heterogeneity of practices. 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 As a well‐known example, the average caesarean section (CS) rate in the country—31.8% according to the latest national estimate 7 —has been one of the highest in Europe for the last decades, and national reports 7 , 8 have consistently showed a significantly higher CS rate in private versus public facilities (79.6% vs 30.0%), and in Southern Italy compared to Norther Italy (e.g. 18.7% in Trento vs 50.9% in Campania). Significant differences across regions have also been documented for maternal and newborn mortality and breastfeeding rates. 11 , 12 , 13 , 14 However, for many indicators of the QMNC, little data, especially on women perspectives on the QMNC in Italy, are available.
The World Health Organization (WHO) developed in 2016 a set of Standards and Quality Measures for improving the QMNC. 16 The IMAgiNE EURO Study Group, a multicountry project including so far partners of 20 countries of the WHO European Region, validated a questionnaire to collect the perspectives of service users (i.e. mothers) on a key set of 40 WHO Standard‐based Quality Measures, through an online survey. 17 , 18 This study aimed at reporting detailed results of the IMAgiNE EURO Study in mothers who gave birth in Italy during the first year of the pandemic, and at comparing findings across Italian regions. We also assessed how clinical and socio‐demographic characteristics associated with a QMNC Index through multivariable regression models.
2. MATERIALS AND METHODS
This is a cross‐sectional study, it was registered in ClinicalTrials.gov (NCT04847336), and is reported according to the STROBE 19 (Table S1).
Women ≥18 years of age who gave birth in Italy from March 1, 2020 up to February 29, 2021 were invited to participate in an online survey. Women who gave birth outside the hospital setting were excluded.
Ethics approval was gained from the Institutional Review Board of the IRCCS Burlo Garofolo Trieste (IRB‐BURLO 05/2020 15.07.2020). Participation in the online survey was voluntary and anonymous. Prior to participation, women were informed of the objectives and methods of the study, including their rights to decline participation, and each provided consent before responding to the questionnaires. Anonymity in data collection during the survey was ensured by not collecting any information that could disclose participants' identity. Data transmission and storage were secured by encryption.
The process of questionnaire development, validation and previous use has been reported elsewhere, 17 , 18 , 20 , 21 and is summarized in Figure S1. The questionnaire included 40 questions (one for each single Quality Measure), equally distributed across four domains: provision of care, experience of care, availability of human and physical resources, and key organizational changes related to the COVID‐19 pandemic. The 40 Quality Measure contributed to a QMNC Index, with higher scores indicating higher adherence to WHO Standards.
Two tailored versions of the questionnaire were available, one for women who underwent labour and the other for those who did not. Each version included 40 key Quality Measures, most of which were the same.
The questionnaire was made available for this round of data collection in 23 languages (Table S2), and women were invited to join the study in their preferred language. The survey was actively promoted through a predefined dissemination plan, whose main approaches used social media, websites, and local networks (e.g. mothers' groups and Non‐Governmental Organizations).
For data analysis a minimum required sample size of 100 women for each region was calculated as adequate to detect a minimum frequency on each Quality Measure of 4% ± 4%, with a confidence level of 96%. For the primary analysis, duplicates detected as represented in Figure S1, and cases missing 20% or more answers on 45 key variables (i.e. the 40 Quality Measures and the five following key socio‐demographic variables: year of birth, age, education, parity, whether the women gave birth in the same country where she was born) were excluded. A descriptive analysis was performed, calculating absolute frequencies and percentages for each variable, in the two groups of women who underwent and died not underwent labour. Women with emergency CS were categorized based on their report of having undergone labour or not, informed by the National Institute of Health and Care Excellence (NICE) definition of labour 22 provided in the questionnaire. Odds ratios (OR) were calculated to assess differences in the 40 Quality Measures between the two groups, adjusting for sample characteristics (socio‐demographic and others). Subgroup analyses were performed to explore differences among regions.
Two sensitivity analyses were conducted to assess robustness of descriptive findings: (1) including only women who answered 100% of the 45 Quality Measures; and (2) including women with up to 90% missing answers on 45 key variables, as performed by other survey authors. 23
For women providing data on all 40 Quality Measures, a QMNC Index was calculated based on the predefined criteria (Table S3). The QMNC index could range from 0 to 100 in each of the four domains, with the total ranging from 0 to 400. The QMNC indexes are presented as median and interquartile ranges (IQRs), because they were not normally distributed. The QMNC indexes of each region was compared to the QMNC index on the whole sample with Mood’s median test.
Additionally, we developed multivariable regression models with the QMNC index as the dependent variable and the following as independent variables: socio‐demographic variables, mode of birth, presence of a doctor during childbirth, macro‐regions of birth (North‐West Italy, North‐East Italy, Central Italy and South Italy and Islands). We conducted a multivariable quantile regression with robust standard errors (SEs) and we modeled the median, the 0.25th and 0.75th quantile, given the statistical evidence of heteroskedasticity for parity (Breusch‐Pagan/Cook‐Weisberg test P < 0.001, H0: homoskedasticity), newborn region of birth (P < 0.001), mode of birth (P < 0.001), and presence of an obstetrician‐gynecologist doctor (OB‐GYN) in the team who assisted the birth (P = 0.007). 24 The categories with the highest frequency were used as reference, except for regions where those with the QMNC index closer to the average QMNC index for the whole sample were chosen as reference.
A two tailed P < 0.05 was considered statistically significant. Statistical analyses were performed using stata/se version 14.0 (Stata Corporation, College Station, TX, USA).
3. RESULTS
Out of a total of 34391 women accessing the online survey of the IMAGINE EURO Study, 4824 gave birth in Italy; of these, 3981 (82.5%) underwent labour, 843 (17.5%) did not undergo labour (Figure 1).
FIGURE 1.
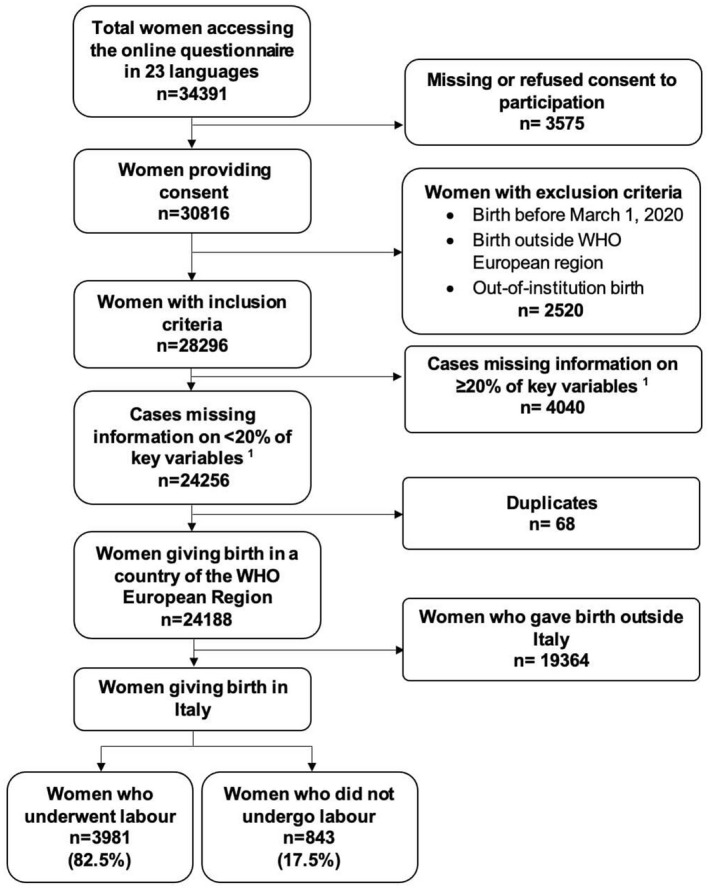
Study flow diagram. 1 40 quality measures and five key socio‐demographic variables were considered as key variables
The total sample accounted for 1.1% of the total births expected in Italy in the study period, with 14 out of the 20 Italian regions contributing with over 100 births (Table 1), and with the collected sample in most regions representing around 1% of their expected births (Table S4). 7
TABLE 1.
Characteristics of the sample
| N = 4824, n (%) | |
|---|---|
| Region of birth a | |
| North‐West Italy | |
| Lombardy | 967 (20.0) |
| Piedmont | 386 (8.0) |
| Liguria | 104 (2.2) |
| North‐East Italy | |
| Veneto | 443 (9.2) |
| Friuli Venezia Giulia | 352 (7.3) |
| Emilia‐Romagna | 333 (6.9) |
| Central Italy | |
| Lazio | 392 (8.1) |
| Tuscany | 245 (5.1) |
| The Marches | 121 (2.5) |
| South Italy and islands | |
| Campania | 309 (6.4) |
| Apulia | 295 (6.1) |
| Sicily | 279 (5.8) |
| Sardinia | 133 (2.8) |
| Calabria | 117 (2.4) |
| Other regions contributing with less than 100 births each b | 348 (7.2) |
| Year of birth | |
| 2020 | 4485 (93.0) |
| 2021 | 150 (3.1) |
| Missing | 189 (3.9) |
| Maternal age | |
| 18–24 | 104 (2.2) |
| 25–30 | 1081 (22.4) |
| 31–35 | 1980 (41.0) |
| 36–39 | 1064 (22.1) |
| ≥40 | 448 (9.3) |
| Missing | 147 (3.0) |
| Maternal educational level c | |
| None | 2 (0.0) |
| Elementary school | 3 (0.1) |
| Junior High school | 217 (4.5) |
| High School | 1867 (38.7) |
| University degree | 1381 (28.6) |
| Postgraduate degree/Master/Doctorate or higher | 1206 (25.0) |
| Missing | 148 (3.1) |
| Maternal parity | |
| 1 | 3221 (66.8) |
| >1 | 1456 (30.2) |
| Missing | 147 (3.0) |
| Type of facility where the birth occurred | |
| Public | 4289 (88.9) |
| Private | 387 (8.0) |
| Missing | 148 (3.1) |
| Mother giving birth in the same country where she was born | |
| Yes | 4456 (92.4) |
| No | 220 (4.6) |
| Missing | 148 (3.1) |
| Mode of birth | |
| Vaginal spontaneous d | 3131 (64.9) |
| Instrumental vaginal birth | 344 (7.1) |
| Emergency caesarean section during labour | 506 (10.5) |
| Emergency caesarean section before going into labour | 303 (6.3) |
| Elective caesarean section | 540 (11.2) |
| Presence of a doctor during childbirth | |
| Obstetrician‐gynecologist doctor | 2620 (54.3) |
| Obstetrics registrar/medical resident (under post‐graduation training) | 596 (12.4) |
| I do not know (healthcare providers did not introduce themselves) | 296 (6.1) |
| Other characteristics | |
| Multiple birth | 53 (1.1) |
| Newborn admitted in neonatal intensive care unit | 482 (10.0) |
| Mother admitted in intensive care unit | 5 (0.1) |
| Stillbirth | 4 (0.1) |
Regions were grouped according to the Italian National Institute of Statistics (https://www.istat.it/en/organisation‐and‐activity), combining Islands with South Italy.
Other regions: Abruzzo (n = 96); Umbria (n = 96); Trentino‐Alto Adige (n = 84); Basilicata (n = 44); Molise (n = 17); Aosta Valley (n = 11).
Wording on education levels agreed among partners during the Delphi; questionnaire translated and back translated according to ISPOR Task Force for Translation and Cultural Adaptation Principles of Good Practice.
Spontaneous vaginal births include all non‐instrumental vaginal births independently of spontaneous or induced onset of labour.
Around three quarters (85.5%) of women were aged 25–39 years old, and most (92.3%) had at least a high school diploma, while around one third (30.2%) had a previous birth. The sample included 220 (4.6%) women who were born in another country, 387 (8.0%) who gave birth in a private hospital, 482 (10.0%) whose newborn was admitted in a neonatal intensive care unit, and 53 (1.1%) mothers of twins. Overall, 1349 (27.9%) births occurred through a CS, while about half (54.3%) of mothers reported were assisted by an obstetrician‐gynecologist. Most births (93.0%) occurred in 2020. More details are provided in Tables S5 and S6.
Figures 2, 3, 4, 5 show findings on each of 40 Quality Measures, in the groups of women who underwent labour (Panel a) and for those who did not undergo labour (Panel b). Detailed data are reported in Tables S7–S10.
FIGURE 2.
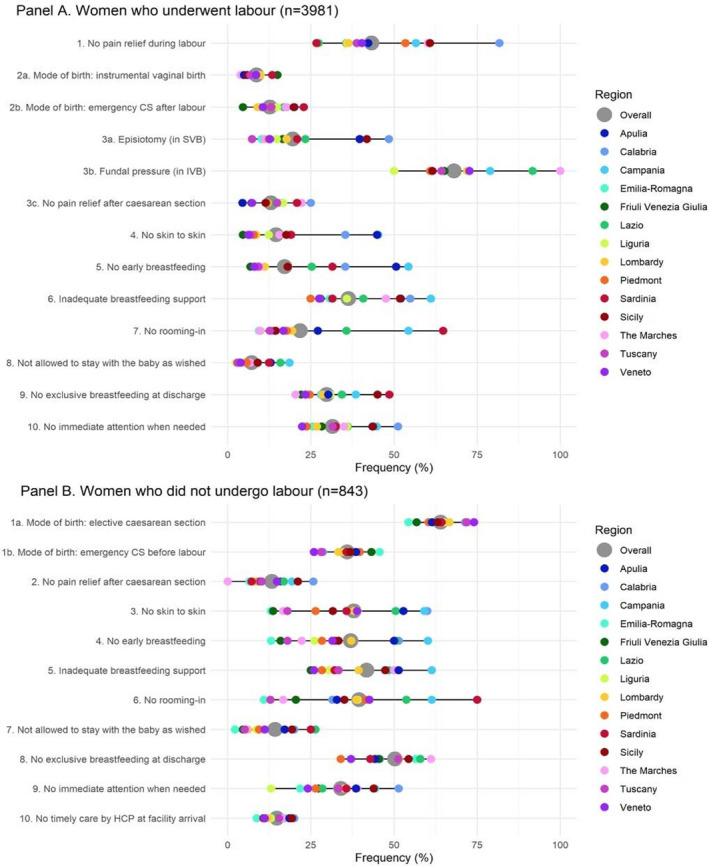
Provision of care. Data are reported as median frequency on the total sample (gray dot) and as median frequency on the same of women giving birth in each region (colored dots). All the indicators in the domain of provision of care are directly based on WHO standards. Indicators identified with letters (e.g. 3a, 3b) were tailored to take into account different mode of birth (i.e. spontaneous vaginal, instrumental vaginal, and caesarean section). These were calculated on subsamples (e.g. 3a was calculated on spontaneous vaginal births; 3b was calculated on instrumental vaginal births). CS, caesarean section; HCP, health care provider; IVB, instrumental vaginal birth; SVB, spontaneous vaginal birth
FIGURE 3.
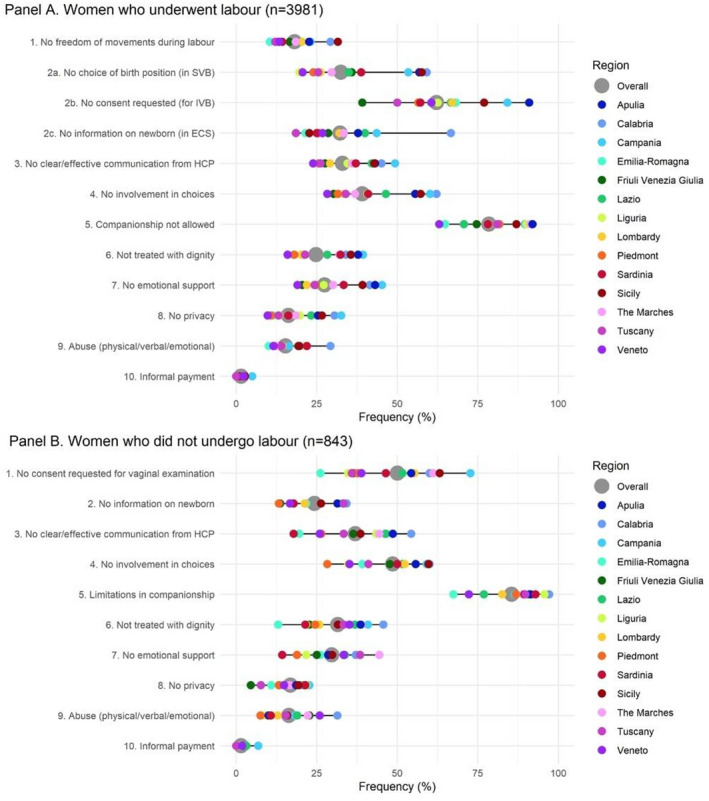
Experience of care. Data are reported as median frequency on the total sample (gray dot) and as median frequency on the same of women giving birth in each region (colored dots). All the indicators in the domain of experience of care are directly based on WHO standards. Indicators identified with letters (e.g. 2a, 2b) were tailored to take into account different mode of birth (i.e. spontaneous vaginal, instrumental vaginal, and caesarean section). These were calculated on subsamples (e.g. 2a was calculated on spontaneous vaginal births; 2b was calculated on instrumental vaginal births). ECS, emergency caesarean section; HCP, health care provider; IVB, instrumental vaginal birth; SVB, spontaneous vaginal birth
FIGURE 4.

Availability of physical and human resources. Data are reported as median frequency on the total sample (gray dot) and as median frequency on the same of women giving birth in each region (colored dots). All the indicators in the domain of availability of physical and human resources are directly based on WHO standards. HCP, health care provider
FIGURE 5.
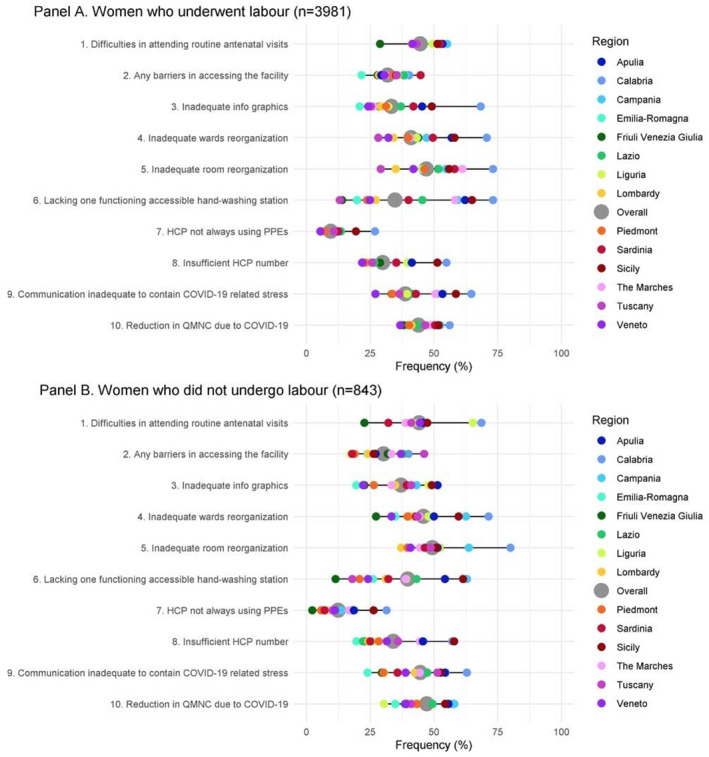
Reorganizational changes due to COVID‐19. Data are reported as median frequency on the total sample (gray dot) and as median frequency on the same of women giving birth in each region (colored dots); indicator 6 in both panels was defined as: At least one functioning and accessible hand‐washing station (near or inside the room where the mother was hospitalized) supplied with water and soap or with disinfectant alcohol solution. HCP, health care provider; PPE, personal protective equipment; QMNC, quality of maternal and newborn care
For most Quality Measures there were wide variations across regions (Figures 2, 3, 4, 5). In the domain of provision of care (Figure 2; Table S7), out of the 3981 women who underwent labour, 1722 (43.3%) did not receive pain relief during labour, with frequencies ranging from 26.7% in Sardinia to 81.7% in Calabria. Overall, 1445 (36.3%) reported an inadequate breastfeeding support (24.9% in Piedmont to 61.1% in Campania), 867 (21.8%) did not have rooming‐in (6.4% in Emilia Romagna to 64.8% in Sardinia), 1255 (31.5%) did not receive immediate attention when needed (22.4% in Veneto to 51.2% in Calabria), and 1184 (29.7%) did not exclusively breastfeed at discharge (20.4% in the Marches to 45% in Sicily). Among 3131 women who had a spontaneous vaginal birth, the median episiotomy rate was 19.6%, ranging from 7.3% in Tuscany to 48.5% in Calabria. Fundal pressure was applied in 68.0% of the 344 women who had an instrumental vaginal birth (IVB), with a reported frequency ranging from 50.0% in Emilia‐Romagna and Liguria to 100% in the Marches and Calabria.
Similarly, large variations were observed on all Quality Measures of experience of care (Figure 3; Table S8) with mothers giving birth in the South of Italy consistently reporting worst indicators than other regions: 3123 (78.4%) women had limitations imposed regarding the presence of a companion of choice (63.0% in Veneto to 92.0% in Apulia); 1559 (39.2%) did not feel involved in choices related to the medical interventions they received (23.3% in Veneto to 62.2% in Calabria); 1313 (33.0%) complained about the lack of a clear and effective communication from health workers (23.9% in Veneto to 49.3% in Campania); 988 (24.8%) felt they were not always treated with dignity (15.9% in Veneto to 39.4% in Campania); 610 (15.3%) reported abuses (10.1% in Emilia Romagna to 29.3% in Calabria).
Findings in the domain of availability of physical and human resources (Figure 4; Table S9) also showed large variations across regions: 709 (17.8%) women rated as inadequate the number of health care professionals compared to the workload (11.7% in Piedmont to 39.0% in Calabria); 578 (14.5%) complained inadequate bathroom facilities (6.2% in Veneto to 30.5% in Sardinia); 291 (7.3%) reported inadequate room cleaning (1.3% in Veneto to 18.3% in Calabria). Overall, 2621 (65.8%) women (47.7% in Emilia Romagna to 83.8% in Sardinia) felt that the visiting hours for partners/relatives were inadequate.
Key findings in the domain related to organizational changes due to the COVID‐19 pandemic (Figure 5; Table S10) revealed that 1750 (44.0%) women perceived a reduction in QMNC due to the COVID‐19 pandemic (36.8 in Veneto to 56.1% in Calabria). Difficulties in attending routine antenatal visits due to the COVID‐19 pandemic were experienced by 1776 (44.6%) women, (28.9% in Friuli to 53.3% in Puglia). Overall, 1382 (34.7%) women reported a lack of at least one functioning and easily‐accessible hand washing station near or inside the room where the mother was hospitalized (13.1% in Tuscany to 73.2% in Calabria) while 380 (9.5%) noted that health workers did not always use personal protective equipment (PPE) (5.4% in Veneto to 56.1% in Calabria).
Findings in the group of women who did not experience labour, when corrected for population characteristics were substantially similar to those of women who did experience labour, with very few differences (Table S11).
The QMNC index (Figure S3) varied among regions, with mothers giving birth in Emilia Romagna, Veneto, Piedmont, Tuscany, Friuli Venezia Giulia and Lombardy (regions in North Italy) reporting a significantly higher median QMNC index than the total sample (P < 0.001 in all comparisons except for Friuli Venezia Giulia and Tuscany, P = 0.002 and P = 0.015 respectively). Mothers giving birth in the South of Italy and Islands reported a lower median value than the whole sample (P < 0.001), while data on Central Italy were not significantly different from that of the overall sample (P = 0.272) (Table S12).
Findings of the sensitivity analyses were substantially similar to findings of the primary analysis (Figures S4 and S5; Tables S13–S16).
In the multivariate analysis (Table S17), when adjusted for other variables, compared to the reference region (Central Italy), mothers giving birth in the South Italy reported a significantly lower QMNC index at the 25%, 50% and 75% quantile with increasing coefficients for lower quantiles (−45.0, −39.0, −35.0 respectively); the North‐East Italy had significantly higher QMNC index either at all or at lower quantiles (+25.0, +18.0, +5.0 for the North‐West; +35.0, 24.0, +10.0 for the North‐East) (Figure 6; Table S17).
FIGURE 6.
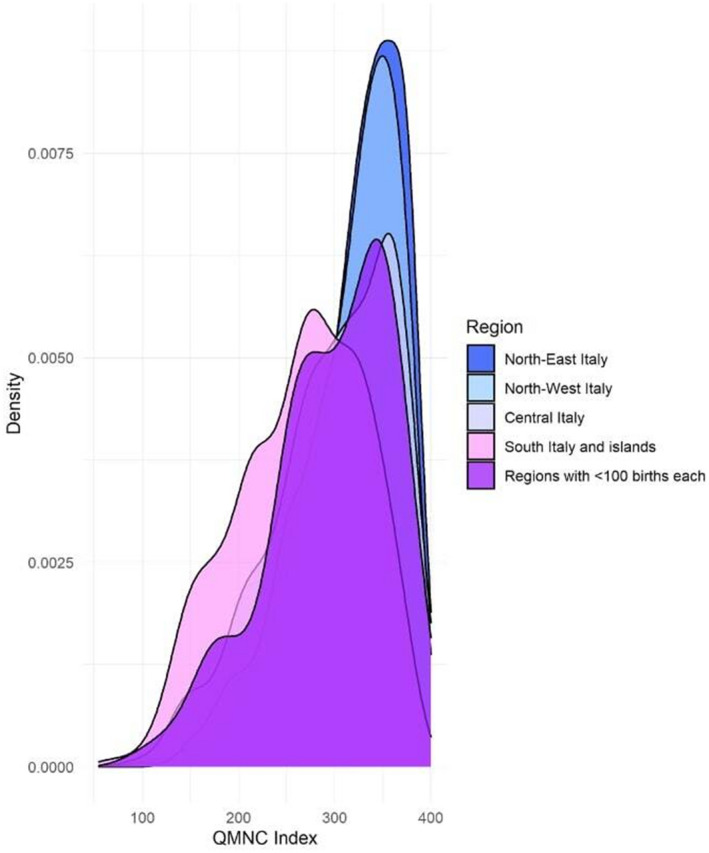
QMNC index by major socio‐economic regions. QMNC, quality of maternal and newborn care
When corrected for other variables (Table S17; Figure 7), multiparous women, women who gave birth in a private facility, or who were assisted by an OB‐GYN reported a significant higher QMNC Index (+20.0, +14.0, 10.0 at the 0.25th, 0.50th and 0.75th quantile for multiparous women; +20.0, +17.0, +15.0 for private hospital; +15.0, +11.0, +5.0 for women with an OB‐GYN in the team who assisted delivery). Women with a junior high school or high school educational level reported a significant higher QMNC Index for 0.50th and 0.75th quantiles compared to women with a university degree or higher educational level (+8.0, +10.0; and +5.0, +5.0 respectively).
FIGURE 7.
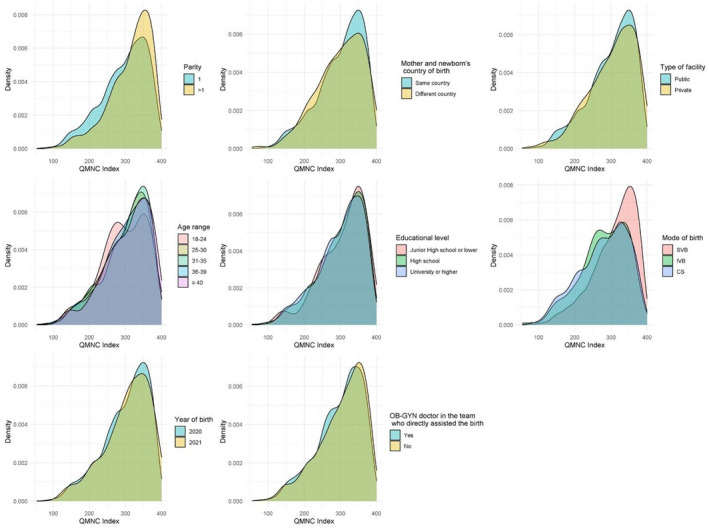
QMNC index by other variables used in quantile regression analysis. CS, caesarean section; IVB, instrumental vaginal birth; OB‐GYN, obstetrics and gynecology; QMNC, quality of maternal and newborn care; SVB, spontaneous vaginal birth
Mother experiencing IVB and CS had a significant lower QMNC Index with increasing coefficients for lower quantiles (−35.0, −34.0, −15.0; and − 35.0, −27.0, −15.0 respectively). Young mothers aged 18–24 years had a significant lower QMNC Index at the 0.25th quantile (−20.0) compared to mothers aged 31–35.
4. DISCUSSION
This study investigated service user’s perceptions of the QMNC around childbirth in Italy across different regions, during the first year of the COVID‐19 pandemic, using a set of 40 Quality Measures based on WHO Standards. Study findings highlights that during the first year of the COVID‐19 pandemic, many aspects of the QMNC—especially those related to patient‐centred respectful care but also availability of resources—were substandard according to mothers. Despite the existence of a national guidance on COVID‐19 and pregnancy, childbirth and breastfeeding 25 large inequalities across regions were reported, with mothers from the South of Italy and Islands reporting lower QMNC indexes than mothers giving birth in North and Central Italy. These inequalities were systematic in their distribution and are in principle preventable, therefore should be called “inequities”. 26
Results of this study are in line with previous evidence, showing gaps in the QMNC, although with major heterogeneity across different settings within Italy, as well as existing example of very good practices in the country. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 20 , 21 The geographical trend with regions in the South of Italy showing significantly worse maternal and newborn indicators compared to regions in the North of Italy has been reported by many other studies. 7 , 8 , 9 , 11 , 12 , 13 , 14 This study did not aim at understanding the underlying reasons for these differences, but rather at documenting the maternal perceptions on the QMNC.
Other studies have highlighted that the COVID‐19 pandemic has negatively impacted several aspects of the QMNC, including both experience of care, and health outcomes. 1 , 2 , 3 , 4 It is plausible that the pandemic has negatively affected some of the Quality Measures that we have reported in this study, such companionship in labour, access to routine antenatal visits, breastfeeding support, rooming‐ in, number of health care professionals compared to the workload. However, for other aspects of care‐ for example measures of provision of care such as pain management, episiotomies, or measures of experience of care, such as adequate communication and respect—a role of the pandemic is less plausible, or would otherwise suggest inappropriate practices. Given the lack of previous studies investigating comprehensively maternal perceptions of the QMNC with the same WHO Quality Measures used in this study, it’s impossible to further assess to which extend the study findings may be associated with the pandemic. The IMAgiNE EURO study will perform other rounds of data collection, and will further explore to what extent gaps in the QMNC reported in this study were associated to the COVID‐19 pandemic, or will persist beyond it. Standardized systems to routinely measure and compare all domains relevant to QMNC over time and across regions, focusing especially but not exclusively on variables related to the experience of care, are still lacking in Italy as in many other countries, and comprehensive data on QMNC are currently not readily available to inform policy and practice in a timely manner. 27 , 28
A strength of the study was the use of a standardized validated questionnaire, which allowed a comparison across regions for the first time, on a set of 40 prioritized Quality Measures based on the WHO Standards and other WHO guidance. 16 , 17 , 18 The questionnaire explored all domains of the WHO QMNC framework, 16 including several measures of respectful maternal care and the additional domain of organizational changes due to COVID‐19. The study aimed at collecting the perspectives of key service users (i.e. mothers), in line with what WHO considers a crucial strategy to monitor QMNC. 29 The sample collected accounted for about the 1% of the about 450,000 total births expected during the study period in Italy, which is not negligible when considering also the peculiar period of the COVID‐19 pandemic and the related practical constrains in data collection. Many of the characteristics of the sample included in this study were substantially aligned with those of the overall sample of mothers giving birth in Italy, as reported by national statistics, thus suggesting that the population is representative of the average population of mothers giving birth in Italy. Specifically, the following key characteristics were fairly similar among mothers enrolled in this study compared to national statistics 7 : age (63% of birth occurring in mothers between 30 to 39 years of age both in our survey and in the national statistics), birth mode (CS rate 28.0% vs 31.3%), type of facility (8.0% of births in a private facility vs 11.0%).
On the other hand, this study included more highly educated mothers and fewer foreign mothers compared to national statistics. 7 , 8 It is difficult to estimate how this may have affected results, whether toward better or worst reported QMNC. The study questionnaire was anonymous and made available in 23 languages, but several factors (e.g. language barriers, digital poverty, interest in the study) may explain population selection. A stratified sampling was difficult to roll‐out in the pandemic period. In the future, if pandemic condition will permit, we will aim at a sample even more representative of the average population of women giving birth in Italy.
Most of the 40 key Quality Measures included in this survey were dichotomous and relatively easy to recall (e.g. skin to skin yes/no, early breastfeeding yes/no) thus increasing reliability and comparability of finding. Nevertheless, some of the measures (e.g. those on experience of care, or the report of better care in the presence of a doctor) may have been affected by women’s subjective judgment, individual culture and expectations, 30 , 31 , 32 which however are impossible to measure in a quantitative way. Notably, most indicators of QMNC used by high level institutions, such as WHO, UNICEF and USAID, lack validation in different cultural settings and are open to subjectivity and recall bias. 28 , 30 As a matter of a fact, findings of the survey represent perceptions of key service users on QMNC around the time of childbirth, and should be valued as such. However, with the multivariate analyses, we corrected findings on QMNC Index for maternal characteristics (such as age, education, type of birth etc). Additionally, the high heterogeneity in QMNC across regions reported by mothers in this study is in line with previous evidence 7 , 8 , 9 , 11 , 12 , 13 , 14 suggesting that quality of health care around the time of childbirth in Italy need further attention to achieve equitable outcomes. This study therefore suggests that the WHO Standards should be monitored and upheld in Italy. Decision makers at all level of the health system and service providers should take action actions to ensure high QMNC for all mothers and newborns in Italy.
IMAgiNE EURO Study Group
Bosnia‐Herzegovina: Amira Ćerimagić, NGO Baby Steps, Sarajevo, Bosnia‐Herzegovina; Croatia: Daniela Drandić, Roda – Parents in Action, Zagreb, Croatia; Magdalena Kurbanović, Faculty of Health Studies, University of Rijeka, Rijeka, Croatia; France: Rozée Virginie and Elise de La Rochebrochard, Sexual and Reproductive Health and Rights Research Unit, Institut National d’Études Démographiques (INED), Paris, France; Kristina Löfgren, Baby‐friendly Hospital Initiative (IHAB), France; Germany: Céline Miani, Stephanie Batram‐Zantvoort, Lisa Wandschneider, Department of Epidemiology and International Public Health, School of Public Health, Bielefeld University, Bielefeld, Germany; Italy: Giuseppa Verardi, Beatrice Zanin, Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy; Sandra Morano, Medical School and Midwifery School, Genoa University, Genoa, Italy; Israel: Ilana Chertok, Ohio University, School of Nursing, Athens, Ohio, USA and Ruppin Academic Center, Department of Nursing, Emek Hefer, Israel, Rada Artzi‐Medvedik, Department of Nursing, The Recanati School for Community Health Professions, Faculty of Health Sciences at Ben‐Gurion University (BGU) of the Negev, Israel, Latvia: Elizabete Pumpure, Dace Rezeberga, and Agnija Vaska, Riga Stradins University Department of Obstetrics and Gynecology, Rīga, Latvia Dārta Jakovicka, Paula Rudzīte, Riga Stradins University Faculty of Medicine, Rīga, Latvia; Elīna Ērmane, Katrīna Paula Vilcāne, Riga Stradins University, Rīga, Latvia; Luxembourg: Maryse Arendt, Neonatal intensive care unit, KannerKlinik, Centre Hospitalier de Luxembourg, Luxembourg, Luxembourg; Barbara Tasch, Neonatal intensive care unit, KannerKlinik, Centre Hospitalier de Luxembourg, Luxembourg, Luxembourg and Neonatal intensive care unit, KannerKlinik, Centre Hospitalier de Luxembourg, Luxembourg, Luxembourg; Norway: Ingvild Hersoug Nedberg, Department of community medicine, UiT The Arctic University of Norway; Sigrun Kongslien, Department of health and care sciences, UiT The Arctic University of Norway; Eline Skirnisdottir Vik, Department of health and caring sciences, Western Norway University of Applied Sciences, Norway; Poland: Barbara Baranowska, Urszula Tataj‐Puzyna, Maria Węgrzynowska, Department of Midwifery, Centre of Postgraduate Medical Education, Warsaw, Poland; Portugal: Raquel Costa, EPIUnit, Institute of Public Health, University of Porto, Porto, Portugal; Laboratory for Integrative and Translational Research in Population Health (ITR), Porto, Portugal; Hei‐Lab:Digital Human‐Environment Interaction Lab. Faculty of Psychology, Education and Sports, Lusófona University, Porto, Portugal; Catarina Barata, Instituto de Ciências Sociais, Universidade de Lisboa, Lisboa, Portugal, Teresa Santos, Hei‐Lab:Digital Human‐Environment Interaction Lab. Faculty of Psychology, Education and Sports, Lusófona University, Porto, Portugal; Centro de Investigação Interdisciplinar em Saúde (CIIS) da Universidade Católica Portuguesa, Lisbon, Portugal; Carina Rodrigues, EPIUnit, Institute of Public Health, University of Porto, Porto, Portugal; Laboratory for Integrative and Translational Research in Population Health (ITR), Porto, PortugalHeloísa Dias, Administração Regional de Saúde do Algarve, Algarve, Portugal; Romania: Marina Ruxandra Otelea, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania, SAMAS Association, Bucharest, Romania; Russia: Ekaterina Yarotskaya, Department of International Cooperation National Medical Research Center for Obs., Gyn. & Perinatology, Moscow, Russia; Serbia: Jelena Radetić and Jovana Ružičić, Centar za mame, Belgrade, Serbia; Slovenia: Zalka Drglin, Barbara Mihevc Ponikvar, and Anja Bohinec, National Institute of Public Health, Ljubljana, Slovenia; Spain: Serena Brigidi, Department of Anthropology, Philosophy and Social Work. Medical Anthropology Research Center (MARC). Rovira i Virgili University (URV), Tarragona, Spain; Lara Martín Castañeda, Institut Català de la Salut, Generalitat de Catalunya, Spain; Ana Canales Viver, Institut Català d'Antropologia (ICA), Barcelona, Spain; Sweden: Helen Elden, Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; Department of Obstetrics and Gynecology, Region Västra Götaland, Sahlgrenska University Hospital, Gothenburg, Sweden; Karolina Linden35, Mehreen Zaigham, Obstetrics and Gynecology, Department of Obstetrics and Gynecology, Institution of Clinical Sciences Lund, Lund University, Lund and Skåne University Hospital, Malmö, Sweden; Verena Sengpiel, Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; Department of Obstetrics and Gynecology, Region Västra Götaland, Sahlgrenska University Hospital, Gothenburg, Sweden; Switzerland: Claire De Labrusse, Alessia Abderhalden, Anouck Pfund, Harriet Thorn, Haute École De Santé Vaud (HESAV), Lausanne, Switzerland.
CONFLICT OF INTEREST
The authors have no conflicts of interest.
AUTHOR CONTRIBUTIONS
ML conceived the study, with major inputs from EPV, BC, IM, AG. EPV and BC supported the process of data collection, with inputs from ML. IM analyzed data, with major inputs from ML, BC, EPV. ML wrote the first draft, which major inputs from all authors.
Supporting information
Table S1
ACKNOWLEDGEMENT
We would like to thank all women who took their time to respond to this survey despite the burden of COVID‐19 pandemic. We also would like to thank Enrico Marchetto from Nozia, an expert in digital marketing, who helped promote the survey via social media. We also wish to acknowledge to help provided by Elise Chapin with English language review. A special thanks to the IMAgiNE EURO study group for their contribute to the development of this project and support for this manuscript.
Lazzerini M, Covi B, Mariani I, Giusti A, Pessa Valente E; for the IMAgiNE EURO Study Group . Quality of care at childbirth: Findings of IMAgiNE EURO in Italy during the first year of the COVID‐19 pandemic. Int J Gynecol Obstet. 2022;157:405–417. doi: 10.1002/ijgo.14119
Members of the IMAgiNE EURO Study Group are listed at the end of the document.
Funding informationThis research was funded by the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste Italy.
DATA AVAILABILITY STATEMENT
Data are available upon reasonable request to the corresponding author.
REFERENCES
- 1. Dell’Utri C, Manzoni E, Cipriani S, et al. Effects of SARS Cov‐2 epidemic on the obstetrical and gynecological emergency service accesses. What happened and what shall we expect now? Eur J Obstet Gynecol Reprod Biol. 2020;254:64‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Casadio P, Youssef A, Arena A, Gamal N, Pilu G, Seracchioli R. Increased rate of ruptured ectopic pregnancy in COVID‐19 pandemic: analysis from the north of Italy. Ultrasound Obstet Gynecol. 2020;56(2):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. De Curtis M, Villani L, Polo A. Increase of stillbirth and decrease of late preterm infants during the COVID‐19 pandemic lockdown. Arch Dis Child Fetal Neonatal Ed. 2021;106(4):456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zanardo V, Tortora D, Guerrini P, et al. Infant feeding initiation practices in the context of COVID‐19 lockdown. Early Hum Dev. 2021;152:105‐286. [Google Scholar]
- 5. Bartick MC, Valdés V, Giusti A, et al. Maternal and infant outcomes associated with maternity practices related to COVID‐19: the COVID mothers study. Breastfeed Med. 2021;16(3):189‐199. [DOI] [PubMed] [Google Scholar]
- 6. Bua J, Mariani I, Girardelli M, Tomadin M, Tripani A, Travan L, Lazzerini M. Parental stress, depression, and participation in care before and during the COVID‐19 pandemic: a prospective observational study in an Italian Neonatal Intensive Care Unit. Frontiers in Pediatrics. 2021;9:737089. 10.3389/fped.2021.737089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Directorate‐General for Digitisation, Health Information System and Statistics . Statistical Office. Certificate of childbirth assistance (CeDAP). Analysis of the birth event ‐Year 2019. Rome, 2021. C_17_pubblicazioni_3076_allegato.pdf (salute.gov.it). Accessed August 25, 2021.
- 8. Directorate‐General for Digitisation, Health Information System and Statistics . Statistical Office. Certificate of childbirth assistance (CeDAP). Analysis of the birth event ‐Year 2018. Rome, 2021. https://www.salute.gov.it/imgs/C_17_pubblicazioni_3034_allegato.pdf. Accessed August 25, 2021.
- 9. Lauria L, Lamberti A, Buoncristiano M, Bonciani M & Andreozzi S Pre‐and post‐natal assistance: promotion and assessment of operational models quality. The 2008–2009 and 2010–2011 surveys (in Italian). Rome: Italian National Institutes of Health; 2012. (ISTISAN repots 12/39). https://www.dors.it/documentazione/testo/201301/12_39_web.pdf. Accessed August 25, 2021.
- 10. Lazzerini M, Valente EP, Covi B, Semenzato C, Ciuch M. Use of WHO standards to improve quality of maternal and newborn hospital care: a study collecting both mothers' and staff perspective in a tertiary care hospital in Italy. BMJ Open Qual. 2019;8(1):e000525. [Google Scholar]
- 11. Lauria L, Spinelli A, Buoncristiano M, Bucciarelli M, Pizzi E. Breastfeeding prevalence at time of vaccination: results of a pilot study in 6 Italian regions. J Hum Lact. 2019;35(4):774‐781. [DOI] [PubMed] [Google Scholar]
- 12. Donati S, Maraschini A, Lega I, et al. Maternal mortality in Italy: results and perspectives of record‐linkage analysis. Acta Obstet Gynecol Scand. 2018;97(11):1317‐1324. [DOI] [PubMed] [Google Scholar]
- 13. Lauria L, Saporito M. Comparison of stillbirth and neonatal mortality in two Italian regions: Lombardia and Campania. Epidemiol Prev. 2004;28(4–5):217‐224. [PubMed] [Google Scholar]
- 14. Dallolio L, Lenzi J, Fantini MP. Temporal and geographical trends in infant, neonatal and post‐neonatal mortality in Italy between 1991 and 2009. Ital J Pediatr. 2013;39:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ravaldi C, Skoko E, Battisti A, Cericco M, Vannacci A. Abuse and disrespect in childbirth assistance in Italy: a community‐based survey. Eur J Obstet Gynecol Reprod Biol. 2018;224:208‐209. [DOI] [PubMed] [Google Scholar]
- 16. World Health Organization . Standards for Improving Quality of Maternal and Newborn Care in Health Facilities. World Health Organization, 2016. https://www.who.int/docs/default‐source/mca‐documents/advisory‐groups/quality‐of‐care/standards‐for‐improving‐quality‐of‐maternal‐and‐newborn‐care‐in‐health‐facilities.pdf?sfvrsn=3b364d8_2. [Google Scholar]
- 17. Lazzerini M, Argentini G & Mariani I et al. A WHO standards‐based tool to measure women’s views on the quality of care around the time of childbirth at facility level in the WHO European Region: development and validation in Italy. Accepted for publication in BMJ Open, 2021 (not published yet)
- 18. Lazzerini M, Covi B, Mariani I, et al. Quality of facility‐based maternal and newborn care around the time of childbirth during the COVID‐19 pandemic: online survey investigating maternal perspectives in 12 countries of the WHO European Region. Lancet Reg Health Eur. 2022;13:100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344‐349. [DOI] [PubMed] [Google Scholar]
- 20. Lazzerini M, Mariani I, Semenzato C, Valente EP. Association between maternal satisfaction and other indicators of quality of care at childbirth: a cross‐sectional study based on the WHO standards. BMJ Open. 2020;10(9):e037063. [Google Scholar]
- 21. Lazzerini M, Semenzato C, Kaur J, Covi B, Argentini G. Women’s suggestions on how to improve the quality of maternal and newborn hospital care: a qualitative study in Italy using the WHO standards as framework for the analysis. BMC Pregnancy Childbirth. 2020;20(1):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Institute of Health and Care Excellence (NICE) . Intrapartum care for healthy women and babies. (NICE clinical guideline 190). Published: 01/12/2014. https://www.nice.org.uk/guidance/cg190/resources/intrapartum‐care‐for‐healthy‐women‐and‐babies‐pdf‐35109866447557. Accessed August 25, 2021.
- 23. Semaan A, Audet C, Huysmans E, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID‐19 pandemic. BMJ Glob Health. 2020;5(6):e002967. [Google Scholar]
- 24. Koenker R. Quantile Regression. Cambridge University Press; 2005. [Google Scholar]
- 25. Giusti A, Zambri F, Marchetti F, Corsi E, Preziosi J, Sampaolo L, Pizzi E, Taruscio D, Salerno P, Chiantera A, Colacurci N, Davanzo R, Mosca F, Petrini F, Ramenghi L, Vicario M, Villani A, Viora E, Zanetto F, Chapin EM, Donati S. COVID‐19 and pregnancy, childbirth, and breastfeeding: the interim guidance of the Italian National Institute of Health. Epidemiol Prev. 2021;45(1‐2):14‐16. https://doi.org/10.19191/EP21.1‐2.P014.030. [DOI] [PubMed] [Google Scholar]
- 26. Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Larson E, Sharma J, Nasiri K, Bohren MA, Tunçalp Ö. Measuring experiences of facility‐based care for pregnant women and newborns: a scoping review. BMJ Glob Health. 2020;5(11):e003368. [Google Scholar]
- 28. Afulani PA, Buback L, McNally B, Mbuyita S, Mwanyika‐Sando M, Peca E. A rapid review of available evidence to inform indicators for routine monitoring and evaluation of respectful maternity care. Glob Health Sci Pract. 2020;8(1):125‐135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization Global Strategy for Women's, Children's and Adolescents' Health, 2016‐2030. 2015. https://www.who.int/life‐course/partners/global‐strategy/globalstrategyreport2016‐2030‐lowres.pdf. Accessed August 25, 2021
- 30. Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, Aguiar C, Saraiva Coneglian F, Diniz ALA, Tunçalp Ö, Javadi D, Oladapo OT, Khosla R, Hindin MJ, Gülmezoglu AM The mistreatment of women during childbirth in health facilities globally: a mixed‐methods systematic review. PLoS Med 2015;12(6):e1001847, discussion e1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rishard M, Fahmy FF, Senanayake H, et al. Correlation among experience of person‐centered maternity care, provision of care and women’s satisfaction: cross sectional study in Colombo, Sri Lanka. PLoS One. 2021;16(4):e0249265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tocchioni V, Seghieri C, De Santis G, Nuti S. Socio‐demographic determinants of women’s satisfaction with prenatal and delivery care services in Italy. Int J Qual Health Care. 2018;30(8):594‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Data Availability Statement
Data are available upon reasonable request to the corresponding author.


