Abstract
Background
The coronavirus disease 2019 (COVID‐19), caused by Severe Acute Respiratory Syndrome Coronavirus 2, has spread rapidly across the world.
Objective
To assess the influence of the COVID‐19 pandemic on the emergency medical service (EMS) for transportation of pregnant women by ambulance.
Methods
This study was a retrospective, descriptive study using the Osaka Emergency Information Research Intelligent Operation Network system, and included pregnant women transported by ambulance in Osaka Prefecture between January 1, 2018 and December 31, 2020. The main outcome of the study was difficulty in obtaining hospital acceptance for transfer of patients (difficult‐to‐transfer cases). We calculated the rates of difficult‐to‐transfer cases using univariate and multivariate analyses.
Results
Of the 1 346 457 total patients transported to hospitals by ambulance in Osaka Prefecture during the study period, pregnant women accounted for 2586 (909, 943, and 734, in 2018, 2019, and 2020, respectively). Logistic regression analysis revealed that pregnant women were negatively associated with difficult‐to‐transfer cases (adjusted OR 0.36, 95% CI 0.26–0.50). Compared with 2018, 2020 was significantly associated with difficult‐to‐transfer cases (adjusted OR 1.27, 95% CI 1.24–1.30).
Conclusion
Pregnant women were consistently associated with reduced odds for being difficult‐to‐transfer cases. The COVID‐19 pandemic might have influenced difficult‐to‐transfer cases in 2020.
Keywords: COVID‐19, difficult‐to‐transfer cases, pandemic, pregnant women, women of childbearing age
Short abstract
This study showed that pregnancy was consistently associated with reduced odds for difficult‐to‐transfer cases in 2020 even during the COVID‐19 outbreak.
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19), caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2), was identified in Wuhan, China in December 2019, after which a COVID‐19 outbreak spread rapidly across the world. 1 On March 11, 2020, the World Health Organization (WHO) declared COVID‐19 as a pandemic.
A previous study has reported that pregnancy was associated with significantly increased chance of hospitalization, ICU admission, and the need for mechanical ventilation due to COVID‐19, but not associated with significantly increased risk of death compared with non‐pregnant counterparts of childbearing age. 2 One retrospective cohort study of asymptomatic pregnant women showed that the COVID‐19 pandemic environment did not affect early first‐trimester miscarriage rates. 3 However, the COVID‐19 pandemic has been associated with an increased rate of stillbirth. 4
The number of hospitals with optimal volumes of deliveries and obstetricians has increased rapidly due to governmental policies to facilitate selection and concentration of obstetric hospitals in Japan. 5 , 6 However, heavy workloads and a shortage of obstetrician resources might limit the provision of comprehensive Emergency Obstetric and Neonatal Care and affect the quality of care. In 2006, 2007, and 2008, two maternal deaths and one neonatal death due to difficulty in obtaining hospital acceptance for transfer of patients were recorded in Japan. 7 , 8 These incidents provoked strong social reactions towards the emergency medical system regarding care of pregnant women. 9 Although the emergency obstetric transportation system has since been reorganized, “difficult‐to‐transfer cases” can still occur and it is possible that the COVID‐19 pandemic may additionally influence emergency obstetric transportation.
This study aimed to assess the influence of the COVID‐19 pandemic on the EMS system for pregnant women who were transported by ambulance in Osaka Prefecture.
2. METHODS
2.1. Study design and setting
This was a retrospective, descriptive study using data from the Osaka Emergency Information Research Intelligent Operation Network (ORION) system for the period January 1, 2018 to December 31, 2020. 10 Osaka Prefecture has a population of approximately 8.8 million and a total area of 1905 km2, and is the largest metropolitan community in western Japan. The ORION system was developed and introduced by the government of Osaka prefecture as an information system for managing emergency patients. It collects data via a smartphone application that is used by emergency medical service personnel for on‐scene hospital selection, and accumulates data for all ambulance records. Since January 2015, diagnostic and outcome information on the patients transported to each medical institution have been merged with the ORION ambulance record data, including the smartphone application data. To assess the influence of the COVID‐19 pandemic on the EMS system, we focused on pregnant women who were transported by ambulance in Osaka Prefecture (Figure 1). We defined “women of childbearing age” as female patients aged 15–44 years. 11 We used the presumptive diagnosis and the final diagnosis for patients who were admitted, using the International Classification of Diseases, 10th Revision (ICD‐10). 12 In the present study, we defined pregnancy‐related patients (pregnancy patients) as ICD‐10 codes O00–O99 and P00–P96. We also collected “COVID‐19” data as ICD‐10 code U07.1, and “COVID‐19 suspected” data (if the virus not identified) as U07.2.
FIGURE 1.
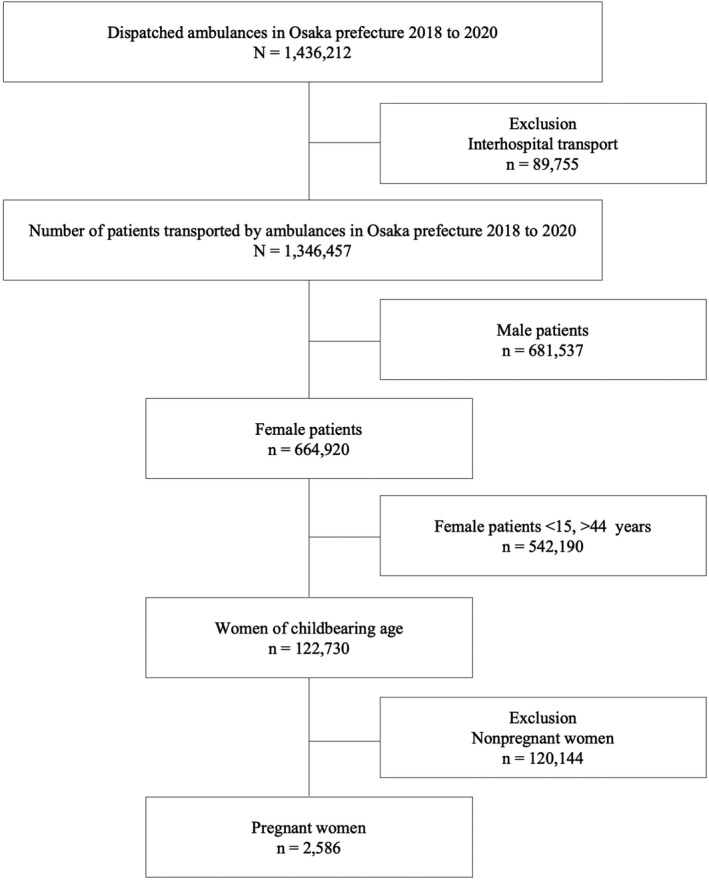
Patient flow. All female patients aged 15–44 years were selected and then divided into two groups
Patients who were not transported to a hospital were excluded from the study. The ambulance records in Osaka Prefecture are considered administrative records, and the necessity to obtain informed consent from the participants was waived because the data were anonymous. This study was approved by the Ethics Committee of Osaka Medical and Pharmaceutical University (Takatsuki City, Japan). Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines were used in the design and in reporting the results of the study.
2.2. Data collection and quality control
Data were uniformly collected using specific data collection forms and the reason for the ambulance call, the location of the accident, the time of day and day of the week, and the tools used, were included, in addition to age, sex, and ICD‐10 code. The detailed situation and patient information were recorded in text form. These data were completed by EMS personnel and then transferred to the information center at the Osaka Municipal Fire Department (OMFD). To assure the quality of the data, incomplete data sheets were returned to the relevant EMS personnel for completion.
2.3. Outcomes
The primary outcome of this study was the difficulty in obtaining hospital acceptance for transfer of a patient. According to the guidelines of the Fire and Disaster Management Agency of the Ministry of Internal Affairs and Communications, we defined “difficult‐to‐transfer cases” as those in which the time interval from arrival at the scene to departure from the scene was longer than 30 min, and those in which ambulance crews needed to make four or more phone calls to hospitals before obtaining hospital acceptance.
2.4. Data analysis
We calculated the numbers of patients transported by ambulance per year due to any cause except interhospital transport between 1 January and December 31, 2020. Patient demographics among the 3 years were compared using χ2 test for categorical variables and the Kruskal–Wallis test for continuous variables. For comparison purposes, the numbers of patients transported by ambulance for the same reasons per year between 1 January and December 31, 2018 and between 1 January and December 31, 2019 were also collected. A logistic regression analysis was used to calculate the rate of difficulty of hospital acceptance of patients for 3 years, and the crude odds ratio (OR) and 95% confidence interval (CI) were calculated for each year for difficult‐to‐transfer cases, with 2018 as the reference. The adjusted OR and 95%CI of difficult‐to‐transfer cases were calculated in all transported patients for pregnant women and for women of childbearing age as well as for other age groups (child, adult, and elderly) using multivariate analyses for month, time of transportation, day of week, and suspected COVID‐19 during transportation. The adjusted OR and 95% CI of difficult‐to‐transfer cases were also calculated in pregnant women and in women of childbearing age using multivariate analyses for month, time of transportation, day of week, and suspected COVID‐19 during transportation.
All statistical analyses were performed using SPSS version 25.0 software (IBM Corp., Armonk, NY, USA) or STATA (version 16.1; Stata Corp., College Station, TX, USA). All tests were two‐tailed, and P‐values <0.05 were considered statistically significant.
3. RESULTS
3.1. Baseline characteristics
In the 3 years between January 1, 2018 and December 1, 2020, a total of 1 436 212 patients were transported to hospitals by ambulance in Osaka Prefecture, Japan. Of them, 1 346 457 were enrolled in this study. Excluded were 89 755 patients who were transferred to a different hospital. There were 462 773 patients in 2018, 468 697 patients in 2019, and 414 987 patients in 2020 who were transported to hospitals by ambulance (Table 1). The total number of women of childbearing age (15–44 years old) was 122 730 (43 616, 43 105, and 36 009, in 2018, 2019, and 2020, respectively, P < 0.001). In addition, the total number of pregnant women was 2586 (909, 943, and 734, in 2018, 2019, and 2020, respectively, P = 0.024). Table 1 lists all baseline characteristics of patients transported to hospitals by ambulance in Osaka Prefecture during the study period. Figure S1 shows violin plots of the age distribution for each patient category.
TABLE 1.
Demographic characteristics of transported patients
| Year | 2018 | 2019 | 2020 | Total | P‐value |
|---|---|---|---|---|---|
| Number of patients | 462 773 | 468 697 | 414 987 | 1 346 457 | <0.001 |
| Age, median (IQR) | 69.0 (38) | 70.0 (38) | 71.0 (35) | <0.001 | |
| Sex (male), % | 234 542 (50.7) | 236 661 (50.5) | 210 334 (50.7) | 681 537 (50.6) | 0.111 |
| Age, median (IQR) | 67.0 (38) | 67.0 (38) | 69.0 (34) | <0.001 | |
| Children, % | 35 314 (7.6) | 37 547 (8.0) | 24 697 (6.0) | 97 558 (7.3) | <0.001 |
| Age, median (IQR) | 3.0 (7) | 3.0 (7) | 4.0 (7) | <0.001 | |
| Adult, % | 166 402 (36.0) | 164 722 (35.1) | 143 740 (34.6) | 474 864 (35.3) | <0.001 |
| Age, median (IQR) | 43.0 (26) | 44.0 (26) | 45.0 (26) | <0.001 | |
| Elderly patients, % | 261 057 (56.4) | 266 428 (56.8) | 246 550 (59.4) | 774 035 (57.5) | <0.001 |
| Age, median (IQR) | 80.0 (12) | 80.0 (12) | 80.0 (12) | <0.001 | |
| Women of childbearing age, % | 43 616 (9.4) | 43 105 (9.2) | 36 009 (8.7) | 122 730 (9.1) | <0.001 |
| Age, median (IQR) | 29.0 (15) | 28.0 (14) | 28.0 (14) | 0.001 | |
| Pregnant women | 909 (0.2) | 943 (0.2) | 734 (0.2) | 2586 (0.2) | 0.024 |
| Age, median (IQR) | 30.0 (11) | 30.0 (10) | 30.0 (9) | 0.141 |
Note. Children, 0–14 years; adults, 15–64 years; elderly patients, ≥65 years.
Determined by the χ2 test for categorical variables and Kruskal–Wallis test for continuous variables.
Abbreviation: IQR, interquartile range.
It was difficult to obtain hospital acceptance for transfer of a total of 4578 female patients of childbearing age (1500, 1503, and 1575, in 2018, 2019, and 2020, respectively, P < 0.001). For pregnant women, the total number of difficult‐to‐transfer cases was 36 (13, 12, and 11, in 2018, 2019, and 2020, respectively, P = 0.919) (Table 2). Table S2 lists the clinical characteristics of all 36 difficult‐to‐transfer cases in pregnant women.
TABLE 2.
Annual transfer data for women of childbearing age and pregnant women
| Year | 2018 | 2019 | 2020 | Total | P‐value |
|---|---|---|---|---|---|
| Women of childbearing age | |||||
| Not difficult‐to‐transfer cases, n (%) | 42 116 (96.6) | 41 602 (96.5) | 34 434 (95.6) | 118 152 (96.3) | <0.001 |
| Difficult‐to‐transfer cases, n (%) | 1500 (3.4) | 1503 (3.5) | 1575 (4.4) | 4578 (3.7) | |
| All | 43 616 | 43 105 | 36 009 | 122 730 | |
| Pregnant women | |||||
| Not difficult‐to‐transfer cases, n (%) | 896 (98.6) | 931 (98.7) | 723 (98.5) | 2550 (98.6) | 0.919 |
| Difficult‐to‐transfer cases, n (%) | 13 (1.4) | 12 (1.3) | 11 (1.5) | 36 (1.4) | |
| All | 909 | 943 | 734 | 2586 | |
Note. Determined by the χ2 test for categorical variables.
3.2. Outcomes and adjusted analyses
Table 3 lists the results of univariate logistic regression analysis of difficult‐to‐transfer cases. The OR for difficult‐to‐transfer women of childbearing age was significantly positive in 2020 compared with 2018 and 2019, but was not significant in 2020 for pregnant women.
TABLE 3.
Univariate logistic regression analysis of difficult‐to‐transfer cases
| Odds ratio | 95% confidence interval | P‐value | |
|---|---|---|---|
| Women of childbearing age | |||
| 2018 | Reference | ||
| 2019 | 1.01 | 0.94–1.09 | 0.701 |
| 2020 | 1.28 | 1.19–1.38 | <0.001 |
| Pregnant women | |||
| 2018 | Reference | ||
| 2019 | 0.89 | 0.40–1.96 | 0.769 |
| 2020 | 1.05 | 0.47–2.35 | 0.908 |
The OR for difficult‐to‐transfer cases of pregnant women was negative (adjusted OR 0.36, 95% CI 0.26–0.50) (Table 4). The OR of 1.27 for 2020 was significantly positive with reference to 2018 (95% CI 1.24–1.30) in all transported patients, however the OR of 0.97 for 2020 was not significant with reference to 2018 (95% CI 0.43–2.23) in pregnant women (Table 5). With reference to June, all the other months were positively associated with difficult‐to‐transfer cases. In terms of time of transportation, with reference to “9 am to 10 am”, all other times were positively associated with difficult‐to‐transfer cases. In particular, it was approximately eight times more difficult to obtain hospital acceptance for transfer during the time “2 am to 5 am” compared with ‘9 am to 10 am’. With reference to Monday, the ORs for Saturday and Sunday were significantly higher for difficult‐to‐transfer cases (adjusted OR 1.14, 95% CI 1.10–1.18 and adjusted OR 1.25, 95% CI 1.21–1.30, respectively). There was a significant association of patients who were suspected to have COVID‐19 with difficult‐to‐transfer cases (adjusted OR 2.77, 95% CI 2.49–3.09). Table S1 shows a similar positive association of female patients of childbearing age with difficult‐to‐transfer cases (adjusted OR 1.09, 95% CI 1.05–1.12) in all transported patients.
TABLE 4.
Multivariate logistic regression analysis of difficult‐to‐transfer cases in all patients (pregnant women as a variable)
| Odds ratio | 95% confidence interval | P‐value | |
|---|---|---|---|
| Year | |||
| 2018 | Reference | ||
| 2019 | 0.92 | 0.90–0.94 | <0.001 |
| 2020 | 1.27 | 1.24–1.30 | <0.001 |
| Month | |||
| June | Reference | ||
| January | 1.98 | 1.88–2.08 | <0.001 |
| February | 1.90 | 1.81–2.00 | <0.001 |
| March | 1.52 | 1.44–1.60 | <0.001 |
| April | 1.62 | 1.53–1.71 | <0.001 |
| May | 1.42 | 1.34–1.50 | <0.001 |
| July | 1.15 | 1.08–1.21 | <0.001 |
| August | 1.44 | 1.37–1.52 | <0.001 |
| September | 1.22 | 1.15–1.29 | <0.001 |
| October | 1.13 | 1.07–1.20 | <0.001 |
| November | 1.30 | 1.23–1.37 | <0.001 |
| December | 1.56 | 1.48–1.64 | <0.001 |
| Time of transportation | |||
| 9 am to 10 am | Reference | ||
| 0 am to 1 am | 6.66 | 6.10–7.27 | <0.001 |
| 1 am to 2 am | 7.75 | 7.10–8.47 | <0.001 |
| 2 am to 3 am | 8.38 | 7.67–9.16 | <0.001 |
| 3 am to 4 am | 8.07 | 7.37–8.84 | <0.001 |
| 4 am to 5 am | 8.03 | 7.33–8.80 | <0.001 |
| 5 am to 6 am | 7.16 | 6.53–7.85 | <0.001 |
| 6 am to 7 am | 5.72 | 5.21–6.27 | <0.001 |
| 7 am to 8 am | 4.09 | 3.73–4.49 | <0.001 |
| 8 am to 9 am | 2.18 | 1.98–2.40 | <0.001 |
| 10 am to 11 am | 1.25 | 1.13–1.38 | <0.001 |
| 11 am to 12 pm | 1.58 | 1.43–1.74 | <0.001 |
| 12 pm to 13 pm | 1.90 | 1.73–2.09 | <0.001 |
| 13 pm to 14 pm | 2.14 | 1.95–2.36 | <0.001 |
| 14 pm to 15 pm | 2.16 | 1.97–2.38 | <0.001 |
| 15 pm to 16 pm | 2.36 | 2.15–2.59 | <0.001 |
| 16 pm to 17 pm | 2.35 | 2.14–2.59 | <0.001 |
| 17 pm to 18 pm | 3.01 | 2.75–3.30 | <0.001 |
| 18 pm to 19 pm | 3.81 | 3.49–4.15 | <0.001 |
| 19 pm to 20 pm | 4.45 | 4.09–4.85 | <0.001 |
| 20 pm to 21 pm | 4.76 | 4.37–5.19 | <0.001 |
| 21 pm to 22 pm | 4.83 | 4.43–5.27 | <0.001 |
| 22 pm to 23 pm | 5.29 | 4.85–5.77 | <0.001 |
| 23 pm to 0 am | 5.88 | 5.39–6.42 | <0.001 |
| Day of week | |||
| Monday | Reference | ||
| Tuesday | 0.97 | 0.94–1.01 | 0.121 |
| Wednesday | 0.99 | 0.95–1.02 | 0.439 |
| Thursday | 0.95 | 0.91–0.99 | 0.007 |
| Friday | 0.90 | 0.86–0.93 | <0.001 |
| Saturday | 1.14 | 1.10–1.18 | <0.001 |
| Sunday | 1.25 | 1.21–1.30 | <0.001 |
| Pregnant women | 0.36 | 0.26–0.50 | <0.001 |
| Suspected COVID‐19 | 2.77 | 2.49–3.09 | <0.001 |
TABLE 5.
Multivariate logistic regression analysis of difficult‐to‐transfer cases in pregnant women
| Odds ratio | 95% confidence interval | P‐value | |||
|---|---|---|---|---|---|
| Year | |||||
| 2018 | Reference | ||||
| 2019 | 0.83 | 0.37–1.86 | 0.650 | ||
| 2020 | 0.97 | 0.43–2.23 | 0.951 | ||
| Month | |||||
| June | Reference | ||||
| January | 1.69 | 0.30–9.60 | 0.552 | ||
| February | 1.76 | 0.28–10.92 | 0.545 | ||
| March | 1.02 | 0.14–7.52 | 0.981 | ||
| April | 1.63 | 0.26–10.08 | 0.599 | ||
| May | 1.00 | (empty)−(empty) | (empty) | ||
| July | 2.85 | 0.58–14.09 | 0.200 | ||
| August | 2.00 | 0.36–11.24 | 0.430 | ||
| September | 1.08 | 0.15–7.85 | 0.942 | ||
| October | 2.16 | 0.41–11.45 | 0.365 | ||
| November | 2.04 | 0.36–11.59 | 0.420 | ||
| December | 1 | (omitted)–(omitted) | (omitted) | ||
| Time of transportation | |||||
| 9 am to 10 am | Reference | ||||
| 0 am to 1 am | 0.67 | 0.06–7.50 | 0.743 | ||
| 1 am to 2 am | 3.51 | 0.66–18.82 | 0.143 | ||
| 2 am to 3 am | 0.66 | 0.06–7.42 | 0.735 | ||
| 3 am to 4 am | 2.43 | 0.39–15.05 | 0.339 | ||
| 4 am to 5 am | 2.00 | 0.27–14.76 | 0.498 | ||
| 5 am to 6 am | 2.07 | 0.28–15.19 | 0.475 | ||
| 6 am to 7 am | 1.07 | 0.09–12.18 | 0.955 | ||
| 7 am to 8 am | 1.00 | (empty)–(empty) | (empty) | ||
| 8 am to 9 am | 1.00 | (empty)–(empty) | (empty) | ||
| 10 am to 11 am | 1.00 | (empty)–(empty) | (empty) | ||
| 11 am to 12 pm | 1.00 | (empty)–(empty) | (empty) | ||
| 12 pm to 13 pm | 0.93 | 0.08–10.59 | 0.952 | ||
| 13 pm to 14 pm | 0.99 | 0.09–11.23 | 0.992 | ||
| 14 pm to 15 pm | 2.48 | 0.40–15.32 | 0.327 | ||
| 15 pm to 16 pm | 0.85 | 0.07–9.64 | 0.894 | ||
| 16 pm to 17 pm | 2.38 | 0.38–14.78 | 0.353 | ||
| 17 pm to 18 pm | 0.92 | 0.08–10.35 | 0.944 | ||
| 18 pm to 19 pm | 1.30 | 0.18–9.44 | 0.797 | ||
| 19 pm to 20 pm | 1.53 | 0.25–9.42 | 0.649 | ||
| 20 pm to 21 pm | 1.35 | 0.19–9.88 | 0.765 | ||
| 21 pm to 22 pm | 0.62 | 0.06–7.02 | 0.701 | ||
| 22 pm to 23 pm | 0.56 | 0.05–6.35 | 0.640 | ||
| 23 pm to 0 am | 1.00 | (omitted)–(omitted) | (omitted) | ||
| Day of week | |||||
| Monday | Reference | ||||
| Tuesday | 1.62 | 0.50–5.27 | 0.420 | ||
| Wednesday | 1.12 | 0.31–3.99 | 0.860 | ||
| Thursday | 1.34 | 0.40–4.51 | 0.638 | ||
| Friday | 0.74 | 0.17–3.20 | 0.690 | ||
| Saturday | 0.89 | 0.23–3.42 | 0.865 | ||
| Sunday | 1.19 | 0.35–4.01 | 0.779 | ||
| Suspected COVID‐19 | 1 | (omitted)–(omitted) | (omitted) | ||
To investigate why it was more difficult for female patients of childbearing age to obtain hospital acceptance for transfer compared with pregnant women in the same age group (Table 4 and Table S1), we compared patients' vital signs during transportation between these two groups (Figure 2). Statistically significant differences were found for all vital signs (respiratory rate, blood pressure, temperature, pulse rate, oxygen saturation [SpO2], and level of consciousness with Glasgow Coma Scale [GCS, not shown]) between female patients of childbearing age and pregnant women (P < 0.001 for all).
FIGURE 2.
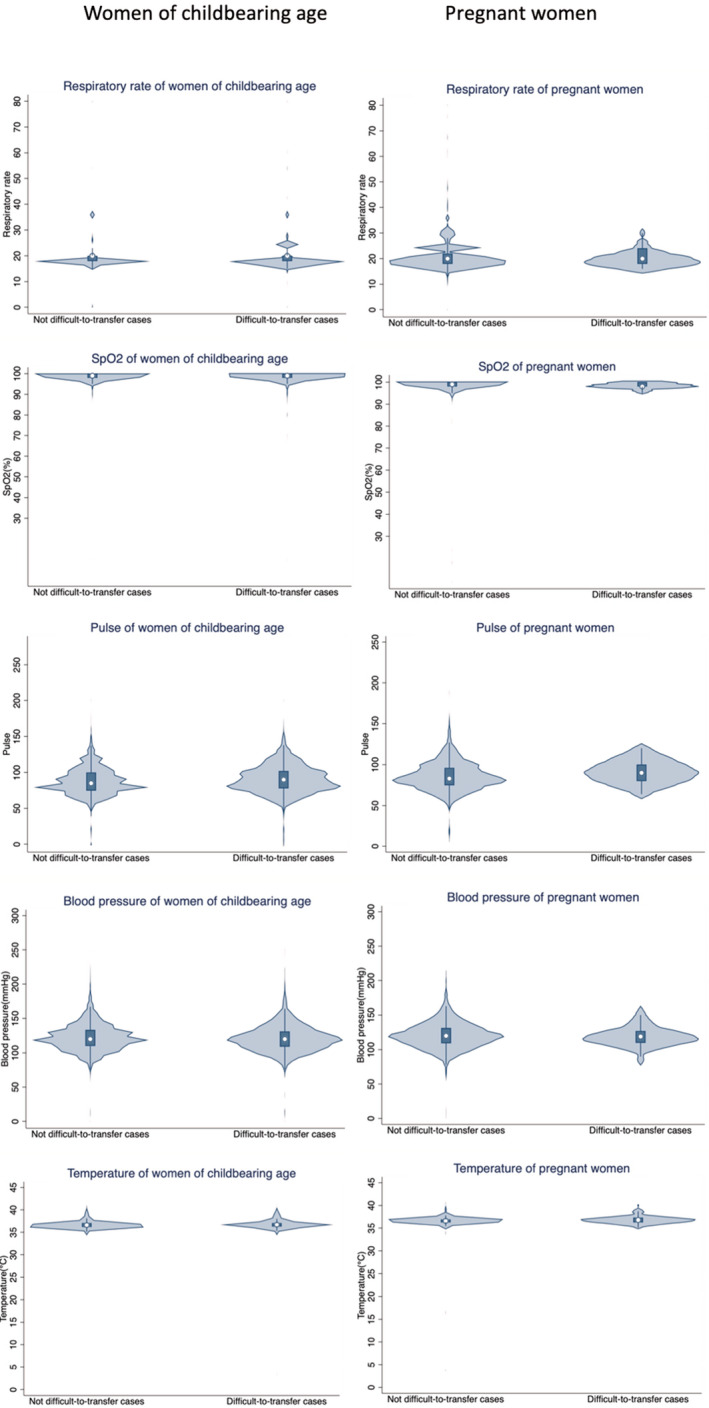
Violin plots of vital signs in women of childbearing age and pregnant women. Glasgow Coma Scale (GCS) is not shown because GCS score was 15 in all 36 difficult‐to‐transfer pregnant women
A total of 234 female patients of childbearing age died at the emergency department (77, 66, and 88 in 2018, 2019, and 2020, respectively). No deaths of pregnant women were reported.
Table 5 revealed no significantly greater OR for pregnant women, whereas women of childbearing age showed similar results to the general population (Table S3). In addition, sensitivity analyses for children and elderly patients were negatively associated with difficult‐to‐transfer cases in all transported patients, whereas adult was positively associated with difficult‐to‐transfer cases (Tables S4–S6).
4. DISCUSSION
Pregnant women were associated with reduced odds for difficulty in obtaining hospital acceptance for transfer of a patient (difficult‐to‐transfer cases) (adjusted OR 0.36, 95% CI 0.26–0.50) (Table 4). In contrast, women of childbearing age had greater odds for difficult‐to‐transfer cases than the general population (OR 1.09, 95% CI 1.05–1.12) (Table S1).
During the 3‐year study period, only 36 pregnant women were difficult‐to‐transfer cases (13, 12, and 11 women in 2018, 2019, and 2020, respectively). However, it is important to reduce difficult‐to‐transfer cases, with or without the COVID‐19 pandemic. There was a strong association with difficult‐to‐transfer cases with patients suspected to have COVID‐19. Hospitals were most likely to accept patients in the morning (9 am to 10 am), on Fridays, and in the month of June.
We did not know the exact reason why young women had greater odds of being difficult‐to‐transfer cases than pregnant women in the same age group. One of the reasons for this finding might be the difference in age distribution between these two categories for all years between 2018 and 2020, as shown in the violin plots in Figure S1. Vital signs including respiratory rate, blood pressure, temperature, pulse rate, SpO2, and GCS were significantly different between female patients aged 15–44 and pregnant women (Figure 2). Another reason might be that the Obstetric and Gynecologic Cooperative System (OGCS) for pregnant women and the Neonatal Mutual Cooperative System for newborns had been established in Osaka prefecture. 13 When emergency maternal events due to obstetric diseases occur, the OGCS allows obstetricians and gynecologists to directly contact the obstetricians and gynecologists at the higher‐care facility for smooth transport. OGCS could manage for smooth transport in pregnant women effectively.
A meta‐analysis of pregnant women with COVID‐19 found that 76.5% of pregnant patients had mild disease, 15.9% had severe disease, and 7.7% had critical disease at the time of admission. 14 Critical disease is reported to be rare in pregnant patients but slightly increased when compared with the general population. 15 In the present study, there were no deaths of pregnant women, and univariate logistic regression analysis failed to show any greater OR for difficult‐to‐transfer cases in pregnant women in 2020. This result suggests that the emergency obstetric transportation system of Osaka Prefecture (OGCS) had been established effectively, and continues to function well even during the COVID‐19 pandemic. It also should be noted that the reduced OR for difficult‐to‐transfer cases for pregnant women might have been affected by the fact that most of these women were already registered with a hospital for their routine prenatal checkups. A previous study conducted in Osaka City showed a negative OR of 0.234 for difficult‐to‐transfer cases in gynecological disease. 16 The OR was higher than 0.18 in the present study that included only obstetric patients.
There are several limitations in this study. First, COVID‐19 is a new disease identified in Japan only in 2020, and the ICD‐10 code “U07.2”, which was used when COVID‐19 was suspected, also included acute upper respiratory tract infection and gastroenteritis. Second, the exact gestations of pregnancy were not available. Third, as this study was a retrospective, observational study, there might be some confounding factors that are unknown. Fourth, this study defined difficult‐to‐transfer cases uniformly regardless of the patient’s condition, and assessed differences only by demographic factors and the reasons for the ambulance call. Finally, in the logistic regression analysis, we could not adjust for factors such as past medical history, medications, and health status because this information was not available.
5. CONCLUSION
The results of this study showed that pregnancy was consistently associated with reduced odds for difficult‐to‐transfer cases. Specifically, when compared with women of childbearing age in the same age group, pregnant women had lower odds of being difficult‐to‐transfer cases in 2020 even during the COVID‐19 outbreak. Hospitals are more likely to accept patients between 9 am and 10 am in the morning, on Fridays, and in the month of June.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
AUTHOR CONTRIBUTIONS
K.O. designed the study and wrote the initial draft of the manuscript. Ka.O., D.N., T.K., Y.K., M.N., T.M., and A.T. contributed to analysis and interpretation of the data and assisted in the preparation of the manuscript. All authors contributed to data collection and interpretation and critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work, including ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors meet the International Committee of Medical Journal Editors (ICMJE) authorship criteria.
Supporting information
Figure S1
Table S1
Table S2
Table S3
Table S4
Table S5
Table S6
ACKNOWLEDGMENTS
The authors thank the EMS providers, nurses, emergency physicians and administrators for their cooperation in the ORION. We thank all the members of The Working Group to Analyze the Emergency Medical Care System in Osaka Prefecture for their kind support.
Ota KP, Nishioka D, Katayama Y. Influence of the COVID‐19 outbreak on transportation of pregnant women in an emergency medical service system: Population‐based, ORION registry. Int J Gynecol Obstet. 2022;157:366–374. doi: 10.1002/ijgo.14128
Funding informationNo funding was received for the study.
DATA AVAILABILITY STATEMENT
The datasets used in the current study are available from the corresponding author on reasonable request.
CODE AVAILABILITY: All data were statistically analyzed using SPSS version 25.0 software (IBM Corp., Armonk, NY, USA) or STATA (version 16.1; StataCorp, College Station, TX, USA).
REFERENCES
- 1. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID‐19): a review. JAMA ‐ J Am Med Assoc. 2020;324(8):782‐793. [DOI] [PubMed] [Google Scholar]
- 2. Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory‐confirmed SARS‐CoV‐2 infection by pregnancy status ‐ United States, January 22‐June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:769‐775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rotshenker‐Olshinka K, Volodarsky‐Perel A, Steiner N, Rubenfeld E, Dahan MH. COVID‐19 pandemic effect on early pregnancy: are miscarriage rates altered, in asymptomatic women? Arch Gynecol Obstet. 2021;303(3):839‐845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Khalil A, von Dadelszen P, Draycott T, Ugwumadu A, O’Brien P, Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID‐19 pandemic. JAMA. 2020;369(7):2020‐2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ide H, Yasunaga H, Kodama T, Koike S, Taketani Y, Imamura T. The dynamics of obstetricians and gynecologists in Japan: a retrospective cohort model using the nationwide survey of physicians data. J Obstet Gynaecol Res. 2009;35(4):761‐766. [DOI] [PubMed] [Google Scholar]
- 6. Matsumoto M, Koike S, Matsubara S, Kashima S, Ide H, Yasunaga H. Selection and concentration of obstetric facilities in Japan: longitudinal study based on national census data. J Obstet Gynaecol Res. 2015;41(6):919‐925. [DOI] [PubMed] [Google Scholar]
- 7. Kobayashi H, Akasaki M, Tsunemi T, Akasaka J, Naruse K, Sado T. Impact of reorganized interfacility transfer on emergency obstetric care in Nara prefecture, Japan. World Acad Sci J. 2019;1(4):192‐200. [Google Scholar]
- 8. Aizawa M, Itabasi K, Matsuoka R. Super maternal transport system. J Child Heal. 2010;69(6):742‐745. [Google Scholar]
- 9. Takaoka S, Obana N, Hamada M, Uehara K, Imamura T. The experiment and the comparative study of the quantitative analysis of the social reaction by incidents with health and medical risks, utilizing newspaper reporting index. Japan J Med Informatics. 2010;29(6):255‐264. [Google Scholar]
- 10. Okamoto J, Katayama Y, Kitamura T, et al. Profile of the ORION (Osaka emergency information research intelligent operation network system) between 2015 and 2016 in Osaka, Japan: a population‐based registry of emergency patients with both ambulance and in‐hospital records. Acute Med Surg. 2019;6(1):12‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Amyx M, Xiong X, Xie Y, Buekens P. Racial/ethnic differences in sleep disorders and reporting of trouble sleeping among women of childbearing age in the United States. Matern Child Health J. 2017;21(2):306‐314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. WHO . International Statistical Classification of Diseases and Related Health Problems, 10th Revision ICD‐10: Tabular List. World Health Organization, vol. 1, pp. 332–345, 2016. [Google Scholar]
- 13. Kanagawa T, Yoshimatsu J, Mitsuda N. Need for annual survey of severe maternal morbidity: the Osaka action agenda. J Obstet Gynaecol Res. 2016;42(7):906. [DOI] [PubMed] [Google Scholar]
- 14. Turan O, Hakim A, Dashraath P, Jeslyn WJL, Wright A, Abdul‐Kadir R. Clinical characteristics, prognostic factors, and maternal and neonatal outcomes of SARS‐CoV‐2 infection among hospitalized pregnant women: a systematic review. Int J Gynecol Obstet. 2020;151(1):7‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boushra MN, Koyfman A, Long B. Covid‐19 in pregnancy and puerpurium: a review for emergency physicien. Am J Emerg Med. 2020;40(January):193‐198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Katayama Y, Kitamura T, Kiyohara K, et al. Factors associated with the difficulty in hospital acceptance at the scene by emergency medical service personnel: a population‐based study in Osaka City, Japan. BMJ Open. 2016;6(10):3‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Table S1
Table S2
Table S3
Table S4
Table S5
Table S6
Data Availability Statement
The datasets used in the current study are available from the corresponding author on reasonable request.
CODE AVAILABILITY: All data were statistically analyzed using SPSS version 25.0 software (IBM Corp., Armonk, NY, USA) or STATA (version 16.1; StataCorp, College Station, TX, USA).


