Abstract
Surgery in suspected/confirmed COVID‐19 patients is a high‐risk venture. In infected patients, COVID‐19 is present in the body cavity. During surgery it could be nebulized in the spray generated by surgical instruments and could theoretically infect members of the surgical team. Nevertheless, some surgical gynecologic pathologies cannot be postponed. We present a list of the most frequent gynecologic diseases and recommendations on their surgical management during the COVID‐19 pandemic, based on expert opinion, current available information, and international scientific society recommendations to support the work of gynecologists worldwide. In brief, any kind of surgical treatment should be scrutinized and postponed if possible. Nonoperative conservative treatment including pharmacological therapies for hormone‐sensitive pathologies should be implemented. Health risk assessment by patient history and COVID‐19 test before elective surgery are pivotal to protect both patients and healthcare providers. In confirmed COVID‐19 patients or highly suspected cases, elective surgery should be postponed until full recovery.
Keywords: Cervical cancer, Coronavirus, COVID‐19, Endometrial cancer, Endometriosis, Gynecology, Laparoscopy, Myoma, Ovarian cancer, Surgery, Urogynecology, Vulvar cancer
Short abstract
The COVID‐19 pandemic required crucial reorganization of health services according to priorities. Recommendations for gynecologic surgery are presented.
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic is a global health emergency. Governments worldwide are attempting to contain the rate of infection using complete or partial lockdowns to reduce the mobility of people. Italy is one of the countries worst affected by the virus and different phases of lockdown are planned to contain virus circulation and prevent complete socioeconomic collapse. The extent of lockdown depends, as in other countries, on the epidemic situation, with three different phases: (1) total lockdown in the emergency period during the peak of the epidemic; (2) an intermediary period begun when the contagion curve starts to descend; and (3) progressive restart of all normal activities. In Italy, phase two began on May 4, 2020.
In many cases, COVID‐19 pneumonia requires hospitalization and intensive care treatment. It leads to a high mortality rate, especially peri‐ and postoperatively. Surgery is a high‐risk situation for the transmission of respiratory infections. 1 Therefore, any kind of surgical treatment should be scrutinized and postponed if possible.
At the same time however, women continue to require treatment for several gynecologic pathologies, some of which cannot be postponed. Nonoperative conservative treatment including pharmacological therapies for hormone‐sensitive pathologies should be implemented. Even if there is no Level 1 evidence, surgery in potential COVID‐19 patients represents a high‐risk challenge and various international societies recommend a nonsurgical approach when feasible.
To our knowledge, no clinical guidelines exist on surgical management of gynecologic diseases that consider COVID‐19. The aim of the present article is to present a list of the most frequent gynecologic diseases and recommendations on their surgical management during the COVID‐19 pandemic. These are based on expert opinion, current available information, and advice from international scientific societies to support the work of gynecologists worldwide.
2. GENERAL CONSIDERATIONS
The virus causing COVID‐19 is transmitted via droplets of different size and through fomites. Airborne transmission is also a mode, whereby the presence of microbes within droplet nuclei, generally considered to be particles less than 5 μm in diameter, can remain in the air for long periods of time and be transmitted to others over distances greater than 1 m. 2 Airborne transmission may be possible in specific circumstances that generate aerosols, such as endotracheal intubation, airway manipulation, and probably surgery.
In infected patients, COVID‐19 is present in the body cavity and during surgery it could be nebulized in the spray generated by surgical instruments. The aerosol generated in an operating room during surgery can contain the virus or parts of it, with some suggesting that the virus remains viable in the aerosol for at least 3 hours. 3
However, there is no available evidence from the current pandemic or from prior global influenza epidemics to conclude that respiratory viruses are transmitted via an abdominal route from patients to healthcare providers in the operating room. The risk of transmission could be increased in other types of surgery, such as head and neck surgery. 4
There is controversy regarding laparoscopy and robotic surgery during the COVID‐19 pandemic, as they are considered aerosol‐generating procedures.
The European Society for Gynaecological Endoscopy (ESGE) 5 and the American Association of Gynecologic Laparoscopists (AAGL) 6 have issued recommendations to continue performing minimally invasive surgery using particular caution measures, such as reducing surgery time, leakage of carbon dioxide from any trocars (check seals or use disposable trocars), production of plume aerosol, and blood/fluid droplet spray or spread. For these purposes it is useful to employ a smoke evacuation/filtration system with ultra‐low particulate air (ULPA) filter capability to remove surgical plume and fluids using laparoscopic and open suction, and to avoid rapid desufflation or loss of pneumoperitoneum during instrument exchange or specimen extraction.
Regardless of the type of surgery, all surgical procedures should be considered high risk as asymptomatic patients may be carrying the virus.
Similar concerns exist for vaginal and laparotomic approaches over aerosolization of viral particles with use of hand‐held electrosurgical devices and plume release directly into the operating room in an uncontrolled way. Therefore, it is important to implement measures to minimize these risks by performing dissection and vascular control using non‐electrosurgical techniques where possible; employing electrosurgical and ultrasonic devices in a manner that minimizes production of plume (with low power setting and avoidance of long desiccation times); using smoke evacuators and suction devices to remove any surgical plume; and minimizing blood/fluid droplet spray or spread.
It is important to discuss the preference for use of spinal or local anesthesia whenever possible with anesthesiologist colleagues, thus avoiding intubation and extubation procedures.
Considerations regarding choice of surgical route include patient comorbidities (such as diabetes, obesity, cardiovascular disease) that could result in higher morbidity from laparotomic procedures and prolonged hospitalization with higher risk of nosocomial infection (including COVID‐19).
Based on our experience, health risk assessment through patient history (contact within the last 14 days with suspected/confirmed cases and movements in some high‐risk places) is a necessary and cheap method to screen patients.
COVID‐19 status of every patient should also be evaluated by physical exam and patient questionnaire regarding flu‐related symptoms, defined by the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC):
Common symptoms: fever, dry cough, fatigue, shortness of breath.
Other associated symptoms: muscle aches, sore throat, diarrhea, nausea/vomiting, runny nose.
A COVID‐19 test before elective surgery is pivotal (nasopharyngeal swab or serological tests) to protect both patients and healthcare providers. 7 The type of screening will depend on the availability and priorities of the healthcare system and of the single institution. Identification of paucisymptomatic or asymptomatic patients is of paramount importance to reduce the spread of the virus in hospitals. However, the false‐negative rate of about 20% with nasopharyngeal swab must be considered.
Patients with unknown COVID‐19 status may be considered “positive until proven otherwise” in terms of mobilizing appropriate protective gear for healthcare workers.
Providers in some areas of the world that were affected early in the global pandemic have advocated for additional imaging evaluation (CT scan of the chest) prior to any surgical procedure owing to the suggestion of its superior predictive ability in early disease.
All members of the surgical team should be trained in appropriate use of personal protective equipment (PPE). 1
It is recommended that anyone working in the operating room utilize full PPE, which includes shoe covers, impermeable gowns, surgical or FFP2/3 masks, protective head covering, gloves, and eye protection. It is also important to limit the number of people inside the operating room as much as possible and to reduce entry and exit movements. 8 , 9
A dedicated operating theatre should be used in all positive cases where surgery cannot be postponed; alternatively, positive cases should be redirected to the nearest referral center.
In confirmed COVID‐19 patients or highly suspected cases, elective surgery should be postponed until the patient has fully recovered. In accordance with Italian ministry recommendations, an infected patient can be considered recovered when they are asymptomatic and have had two negative tests for COVID‐19 at 24‐hour intervals.
3. SURGICAL MANAGEMENT OF GYNECOLOGIC DISEASES
Only category 1 and some exceptional category 2 surgery should continue during the pandemic, until further notice (Table 1).
Table 1.
Surgical triage categories.
| Category | Description | Desirable maximum waiting time |
|---|---|---|
| 1. Urgent | Has the potential to deteriorate quickly to the point where it may become an emergency | Within 30 days |
| 2. Semi‐urgent |
|
Within 60 days |
| 3. Elective |
|
Within 365 days |
Based on current knowledge and our experience, we developed a list of the most frequent gynecologic diseases and recommendations on their surgical management during the COVID‐19 pandemic to guide the medical conduct of healthcare providers. A surgical flowchart is given as Figure 1.
Figure 1.
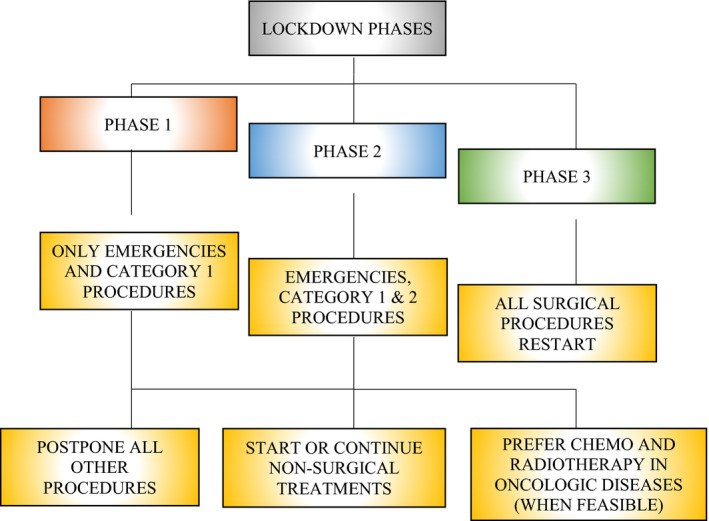
Flowchart of gynecologic surgical priorities during the three lockdown phases of the COVID‐19 pandemic.
3.1. Emergencies
Emergencies such as ovarian torsions, ectopic pregnancies, and hemorrhagic cysts cannot be postponed; however, following previous reports, COVID‐19 testing and risk assessment are advised, always dependent on the degree of urgency. 10
3.2. Hysteroscopic surgery
The risk of viral transmission at time of hysteroscopy, particularly with bipolar electrosurgical devices and normal saline solution, is theoretically low given that it is not an aerosol‐generating procedure. 11 The “see and treat” approach in an outpatient setting is advisable. 11 Depending on hospital resources, it is reasonable to submit to outpatient office procedures patients with polyps and symptomatic myomas not responding to medical treatments. Furthermore, infertile women with intrauterine pathologies who want to conceive quickly could be treated with an office procedure. Resectoscopic surgery should be postponed, except for endometrial ablation in endometrial cancer for fertility‐sparing purposes.
3.3. Myomas
Maintain all effective pharmacological treatments, change ineffective medical treatments, and start an effective medical treatment in newly diagnosed patients. Depending on hospital resources, it is possible to submit to surgery all symptomatic myomas in which pharmacological therapies are not effective (category 2 surgery). Minilaparotomy is preferred to laparoscopy when possible.
3.4. Endometriosis
Maintain all effective pharmacological treatments, change ineffective medical treatments, using GnRH analogues if necessary, and start an effective medical treatment in newly diagnosed patients. Depending on hospital resources, it is possible to submit to surgery symptomatic patients in which pharmacological therapies are not effective, but only when the risk of transmission decreases (phase 2). Laparoscopic access is more effective in these patients, with strict adherence to ESGE guidelines.
3.5. Ovarian lesions
An accurate vaginal ultrasound examination performed by an expert sonographer is recommended, in association with CA 125 and HE4 serum levels, to calculate the risk of malignancy following the International Ovarian Tumor Analysis (IOTA) models. 12 Patients with a risk of malignancy of 5% or greater should not have surgery postponed and should be referred to an oncologic COVID‐free center. Young (<30 years) asymptomatic patients with large (≥10 cm) benign adnexal masses must be submitted to surgery. Medical therapy is recommended in patients with apparently functional cysts unless it is contraindicated.
3.6. Urogynecology
The risk of COVID‐19 infection during urogynecologic surgery is unknown, but theoretically low. Urogynecologic procedures are considered category 3 surgery and therefore may be postponed without problems during the “hot” phase of the epidemic. It is important to implement nonsurgical management for urinary incontinence, as advised by the International Urogynecological Association (IUGA). 13 Depending on the local situation, the procedure can be performed in highly symptomatic patients when the risk of transmission decreases (phase 2).
3.7. Conization
Large conization or trachelectomy for fertility‐sparing surgery in cervical cancer patients is recommended. According to the American Society for Colposcopy and Cervical Pathology, 14 patients with high‐grade cervical lesions should have a procedure scheduled within 3 months. However, when a cervical cancer is highly suspicious with a negative cervical biopsy, it is not wise to postpone conization more than 4 weeks. The risks related to laser vaporization and conization procedures are also unknown, and it is important to apply the above recommendations concerning minimization and evacuation of surgical plume.
3.8. Atypical hyperplasia
Multiple hysteroscopic biopsies in an outpatient setting and transvaginal ultrasound or MRI are recommended to exclude a synchronous cancer. Whether an endometrial carcinoma is excluded, surgery could be delayed, considering a systemic hormonal treatment or a medicated intrauterine device, if not contraindicated.
3.9. Endometrial cancer
Patients should be referred to an oncologic COVID‐free center. Conservative medical and surgical approaches in women with low‐risk endometrial cancer who wish to preserve fertility are recommended. The standard of care is type A radical hysterectomy with bilateral salpingo‐oophorectomy. 15 Except for low‐risk patients, sentinel lymph node biopsy with indocyanine green is recommended. Strictly following ESGE recommendations mentioned above, the minimally invasive approach should be preferred to reduce hospital stay. Lymphadenectomy should be reserved for patients with enlarged lymph nodes at the preoperative work‐up or for high‐risk patients when the sentinel lymph node is undetectable (FIGO stage IB G3, FIGO stage II). In advanced stages of disease, consider surgery just to confirm diagnosis and then start a systemic treatment as soon as possible. 16
3.10. Cervical cancer
Patients with early‐stage cervical cancer with no fertility‐sparing desire should be referred to an oncologic COVID‐free center for surgical management, according to international guidelines. 17 After conization without residual tumor and in tumors smaller than 2 cm, radical hysterectomy type B with a minimally invasive approach is reasonable, but without any uterine manipulator and, preferably, by adopting preventive surgical maneuvers. 18 , 19 , 20 Tumors with a large diameter of 2 cm or greater require a laparotomic approach. 18 Sentinel lymph node biopsy using indocyanine green is the technique of choice in this pandemic period for the evaluation of lymph node status. Refer locally advanced disease to an oncologist and radiotherapist for definitive chemoradiation. Pretreatment positron emission tomography–computed tomography (PET‐CT) is advisable to assess the eventual presence of distant metastases and to define the application field. Surgical nodal staging in advanced stages must be avoided to save resources.
3.11. Vulvar cancer
Surgery for early‐stage vulvar cancer and small local recurrence cannot be delayed. It is unreasonable to omit inguinofemoral lymphadenectomy in FIGO stages IB or higher. Sentinel lymph node biopsy should be used when indicated. 21 Advanced and unresectable diseases should be referred for definitive chemoradiation. Small precancerous lesions and noninvasive Paget disease can be postponed.
3.12. Ovarian cancer
In highly suspicious early‐stage ovarian cancer there is no need to postpone surgery. It is recommended that the patient is referred to an oncologic COVID‐free center after a complete evaluation that includes PET‐CT, MRI, vaginal examination, transvaginal ultrasound, and serum markers (CA 125, HE4 with ROMA test). Intraoperative frozen section analysis is mandatory to confirm the diagnosis. Surgical treatment of early‐stage ovarian cancer is the standard recommended by international guidelines. 22 , 23 In patients without histologic confirmation of advanced stage disease that cannot be submitted to primary debulking surgery, consider laparoscopy to obtain a tissue biopsy and then start a neoadjuvant treatment. In patients who have already started chemotherapy, consider continuing the therapy for six cycles and then submit to interval debulking surgery if possible.
3.13. Recurrences
Recurrent diseases should be discussed by a multidisciplinary team in an oncologic center to tailor the correct treatment and take into consideration hospital resources, therapeutic options, and disease prognosis.
4. CONCLUSION
The decision to postpone elective operations for benign, asymptomatic gynecologic diseases is determined by the crucial need to reduce virus circulation among the population and the importance of focusing health resources on COVID‐19 and surgery for unpostponable diseases. In histologically confirmed malignant diseases, the guarantee of care is always dependent on the pandemic situation, the resource availability of the hospital, and a benefit/risk assessment of the cases on the surgical waiting list.
AUTHOR CONTRIBUTIONS
BC was responsible for review design and manuscript writing. EB, EM, SB, VB, and GC were responsible for literature data research and discussion of different gynecological pathologies. GV, CV, and RM oversaw literature data analysis. VB revised the article. EV coordinate the research work.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
Acknowledgments
To G. Chiofalo and all those who died during this pandemic ‐ who passed away without proper commemoration.
REFERENCES
- 1. Brindle M, Gawande A. Managing COVID‐19 in surgical systems. Ann Surg. 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Setti L, Passarini F, De Gennaro G, et al. Airborne transmission route of COVID‐19: why 2 meters/6 feet of inter‐personal distance could not be enough. Int. J. Environ. Res. Public Health. 2020;17:E2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N. Engl. J. Med. 2020;382:1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Day AT, Sher DJ, Lee RC, et al. Head and neck oncology during the COVID‐19 pandemic: Reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020;105:104684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. European Society for Gynaecological Endoscopy . ESGE Recommendations on Gynaecological Laparoscopic Surgery during Covid‐19 Outbreak. https://esge.org/wp‐content/uploads/2020/03/Covid19StatementESGE.pdf. Accessed on May 04, 2020.
- 6. Association of Gynecologic Laparoscopists . COVID‐19: Joint Statement on Minimally Invasive Gynecologic Surgery. https://www.aagl.org/news/covid‐19‐joint‐statement‐on‐minimally‐invasive‐gynecologic‐surgery/?fbclid=IwAR1BIiattvez0PxnJLsGFea75dgksuSFlJAWgqcRspZM3JfqkKs6wUsbNQc. Accessed May 04, 2020.
- 7. Steward J, Kitley WR, Schmidt CM, Sundaram CP. Urologic surgery and COVID‐19: How the pandemic is changing the way we operate. J Endourol. 2020;34:541–549. [DOI] [PubMed] [Google Scholar]
- 8. Chen N, Zhou M. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Radonovich LJ, Simberkoff MS, Bessesen MT, et al. N95 Respirators vs medical masks for preventing influenza among health care personnel: A randomized clinical trial. JAMA. 2019;322:824–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brücher B, Nigri G, Tinelli A, et al. COVID‐19: Pandemic surgery guidance. 4Open. 2020;3:1. [Google Scholar]
- 11. Carugno J, Di Spiezio SA, Alonso L, et al. COVID‐19 pandemic. Impact on hysteroscopic procedures. A consensus statement from the Global Congress of Hysteroscopy Scientific Committee. J Minim Invasive Gynecol. 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nunes N, Ambler G, Foo X, et al. Prospective evaluation of IOTA logistic regression models LR1 and LR2 in comparison with subjective pattern recognition for diagnosis of ovarian cancer in an outpatient setting. Ultrasound Obstet Gynecol. 2018;51:829–835. [DOI] [PubMed] [Google Scholar]
- 13. International Urogynecological Association . Guidance for the management of urogynecological conditions during the Coronavirus (COVID‐19) pandemic. https://www.iuga.org/publications/covid‐19‐guidance‐for‐urogynecological‐conditions. Accessed May 04, 2020.
- 14. American Society for Colposcopy and Cervical Pathology . ASCCP Interim Guidance for timing of diagnostic and treatment procedures for patients with abnormal cervical screening tests. https://www.asccp.org/covid‐19. Accessed May 04, 2020.
- 15. Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008;9:297–303. [DOI] [PubMed] [Google Scholar]
- 16. Ramirez PT, Chiva L, Eriksson AGZ, et al. COVID‐19 global pandemic: Options for Management of Gynecologic Cancers. Int J Gynecol Cancer. 2020;30:561–563. [DOI] [PubMed] [Google Scholar]
- 17. Koh WJ, Abu‐Rustum NR, Bean S, et al. Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019;17:64–84. [DOI] [PubMed] [Google Scholar]
- 18. Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895–1904. [DOI] [PubMed] [Google Scholar]
- 19. Cusimano MC, Baxter NN, Gien LT, et al. Impact of surgical approach on oncologic outcomes in women undergoing radical hysterectomy for cervical cancer. Am J Obstet Gynecol. 2019;221:619.e1–619.e24. [DOI] [PubMed] [Google Scholar]
- 20. Greggi S, Casella G, Scala F, et al. Surgical Management of Early Cervical Cancer: When is laparoscopic appropriate? Curr Oncol Rep. 2020;22:7. [DOI] [PubMed] [Google Scholar]
- 21. Querleu D, Rychlik A, Guyon F, et al. Management of the nodal disease in vulvar cancers. The ESGO guidelines [in French]. Bull Cancer. 2019. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22. Colombo N, Sessa C, du Bois A, et al.; Ovarian Cancer Consensus Conference Working Group . ESMO‐ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Ann Oncol. 2019;30:672–705. [DOI] [PubMed] [Google Scholar]
- 23. Armstrong DK, Alvarez RD, Bakkum‐Gamez JN, et al. Guidelines insights: Ovarian cancer, version 1.2019. J Natl Compr Canc Netw. 2019;17:896–909. [DOI] [PubMed] [Google Scholar]


