Abstract
COVID‐19 outbreaks appear to be related to exacerbation of psychological problems such as depression and anxiety in high‐risk population such as pregnant women and the postpartum period due to stress and life‐threatening illnesses. The aim of this study was to evaluate the prevalence of postpartum depression (PPD) during COVID‐19. This study protocol is registered in PROSPERO with CRD42021278425 code. Data sources including Google Scholar, ISC, Magiran, Scopus, PubMed, Embase, and Web of Science and reference list of included articles were used to identify related studies. Observational studies that reported the prevalence of PPD in both Persian and English during COVID‐19 between January 20, 2020 and August 31, 2021 were included. Data were collected and analyzed with a random effects model for meta‐analysis. In this study, 671 initial articles were identified and after removing duplicates, 454 studies were screened and finally 24 studies entered the meta‐analysis stage. According to this study results PPD based on Edinburgh Postnatal Depression Scale (EPDS) ≥9, EPDS ≥10, EPDS ≥11, EPDS ≥12, EPDS ≥13, Postpartum Depression Screening Scale‐Short Form (PDSS‐SF) ≥17 and total prevalence was reported 12% (95% confidence interval [CI] = 0.07–17, I 2 = 97%), 27% (95% CI = 15–39, I 2 = 99%), 44% (95% CI = 40–49, I 2 = 0.0%), 27% (95% CI = 0.06–49, I 2 = 97.4%), 28% (95% CI = 18–39, I 2 = 98.5%), 37% (95% CI = 32–42), 28% (95% CI = 23–33, I 2 = 98.5%). The findings of this study showed that the prevalence of PPD in women is relatively high during COVID‐19. Therefore, considering the psychological consequences of the COVID‐19 pandemic and the importance of pregnancy and the postpartum period in terms of the emergence of mental disorders, especially depression, it seems necessary to perform interventions and physical and psychological support.
Keywords: COVID‐19, mental health, postpartum depression, women
Short abstract
The present study found that the prevalence of postpartum depression( PPD) in women is relatively high during COVID‐19.
1. INTRODUCTION
COVID‐19 outbreaks appear to be exacerbated in all populations due to stress and life‐threatening risks. 1 The COVID‐19 pandemic is also a trigger for various types of mental health problems such as depression, anxiety and panic disorder. 2 Measures such as social distancing, reduction of religious activities, tourism, and schooling during COVID‐19 have changed people’s lifestyles and mental health outcomes, disproportionately affecting high‐risk populations. 3 , 4
Pregnancy and postpartum are challenging and are associated with disorders such as insomnia, relationship tension, and feelings of isolation, which have caused mood disorders in many women. On the other hand, environmental stressors such as natural disasters can exacerbate mood disorders during pregnancy. 5 Pregnant women experience high stress during epidemics. On the other hand, increased symptoms of depression and anxiety in pregnant women are associated with an increased risk of preterm delivery, postpartum depression (PPD) and behavioral problems in children. Therefore, pregnant women need social support during pregnancy because these measures reduce PPD. 6 , 7 According to studies, COVID‐19 has been associated with an increased risk of mental health problems in pregnant and postpartum women. 8
Postpartum depression disorder is the most common postpartum illness among women. 9 According to the DSM‐5 definition, PPD occurs 4 weeks after delivery while others define it as commencing at any time in the first year after delivery. 10 Postpartum depression threatens not only the health of mothers but also the health of infants, and infants of depressed mothers may have developmental disorders, reduced cognitive function, as well as problems pertaining to social communication with their parents and peers. 11
Approximately 10%–16% of women in the postpartum period experience a period of major depression and many of them also suffer from anxiety disorders. 12 The results of a study in China showed that the prevalence of depression in pregnant women and postpartum women was 27.43%, and women who were worried about themselves or their baby developing COVID‐19 were more prone to depression. 8 The results of other studies have shown that women who gave birth during COVID‐19 had a higher rate of PPD than other women who gave birth during the non‐COVID ‐19 period. 13
Studies have shown that several studies have been conducted to investigate the association between COVID‐19 and PPD in mothers, but a comprehensive study was not found to examine the prevalence of PPD during COVID‐19. Access to comprehensive and complete information about the rate of PPD during COVID‐19 can be used as a reference for health system decisions and policies. Therefore, the research team decided to conduct a systematic review and meta‐analysis study to assess the prevalence of PPD during COVID‐19.
2. MATERIALS AND METHODS
This systematic review and meta‐analysis was done according to PRISMA guideline. 14 This study protocol was registered in PROSPERO with CRD42021278425 code.
2.1. Search strategy
Information sources including Google Scholar, ISC, Magiran, Scopus, PubMed, Embase, and Web of Science and reference list of imported articles were used to identify related studies. Persian equivalent and English key words include: “Postnatal Depression”, “Post‐Partum Depression”, “Post‐Partum Depression”, “Postpartum Depression”, “Post‐Natal Depression”, “Post Natal Depression”, “2019 novel coronavirus disease”, COVID19, “COVID‐19 pandemic”, “SARS‐CoV‐2 infection”, “COVID‐19 virus disease”, “2019 novel coronavirus infection”, “2019‐nCoV infection”, “Coronavirus disease 2019”, “2019‐nCoV disease”, “COVID‐19 virus infection” were used. In order to compile the strategy search, keywords, search fields and operators were used. First, Pubmed syntax search was compiled and then based on Pubmed syntax search, syntax search of other databases was compiled. The searches were conducted in both Persian and English from January 20, 2020 to August 31, 2021. Table 1 lists the search strategies in the database types.
TABLE 1.
Search strategy in database types
| Database | Search syntax |
|---|---|
| PubMed | ((“Postnatal Depression” OR “Post‐Partum Depression” OR “Post‐Partum Depression” OR “Postpartum Depression” OR “Post‐Natal Depression” OR “Post Natal Depression”) AND (“2019 novel coronavirus disease” OR COVID19 OR “COVID‐19 pandemic” OR “SARS‐CoV‐2 infection” OR “COVID‐19 virus disease” OR “2019 novel coronavirus infection” OR “2019‐nCoV infection” OR “Coronavirus disease 2019” OR “2019‐nCoV disease” OR “COVID‐19 virus infection”)) |
| Scopus | (((ALL(“Postnatal Depression”) OR ALL(“Post‐Partum Depression”) OR ALL(“Post‐Partum Depression”) OR ALL(“Postpartum Depression”) OR ALL(“Post‐Natal Depression”) OR ALL(“Post Natal Depression”)) AND (ALL(“2019 novel coronavirus disease”) OR ALL(COVID19) OR ALL(“COVID‐19 pandemic”) OR ALL(“SARS‐CoV‐2 infection”) OR ALL(“COVID‐19 virus disease”) OR ALL(“2019 novel coronavirus infection”) OR ALL(“2019‐nCoV infection”) OR ALL(“Coronavirus disease 2019”) OR ALL(“2019‐nCoV disease”) OR ALL(“COVID‐19 virus infection”)))) |
| Web of science | (((TS = (“Postnatal Depression”) OR TS = (“Post‐Partum Depression”) OR TS = (“Post‐Partum Depression”) OR TS = (“Postpartum Depression”) OR TS = (“Post‐Natal Depression”) OR TS = (“Post Natal Depression”)) AND (TS = (“2019 novel coronavirus disease”) OR TS = (COVID19) OR TS = (“COVID‐19 pandemic”) OR TS = (“SARS‐CoV‐2 infection”) OR TS = (“COVID‐19 virus disease”) OR TS = (“2019 novel coronavirus infection”) OR TS = (“2019‐nCoV infection”) OR TS = (“Coronavirus disease 2019”) OR TS = (“2019‐nCoV disease”) OR TS = (“COVID‐19 virus infection”)))) |
2.2. Eligible criteria
In this study, inclusion criteria include observational studies that reported the prevalence of PPD in both Persian and English during COVID‐19 between January 20, 2020 and August 31, 2021. Exclusion criteria included mean and standard deviation of PPD, PPD reports among men, pregnant women, during epidemics other than COVID‐19, as well as systematic review studies, interventional studies, case reports, and letters to the editor.
2.3. Selection of studies
In this study, 671 studies were entered into the EndNote 7 software after the search results were completed, and after removing duplicates, titles, and abstracts, 454 studies were screened. In the next step, the two researchers independently studied 46 possible related studies in detail and selected 24 final studies.
2.4. Quality assessment and data extraction
The quality evaluation of the studies was done by two researchers independently and any disagreement between them was resolved through a third person. To evaluate cross‐sectional studies from the checklist Appraisal tool for Cross‐Sectional Studies (AXIS) Tool 15 was used. This tool has a score of 0–20. The Newcastle‐Ottawa Scale (NOS) tool 16 was also used to evaluate other observational studies (cohort and case–control). This tool has eight items in cohort studies in three sections including Selection (four items), Comparability (one item) and Outcome (three items) and also in case–control studies eight items including selection (Selection (four items), Comparability (one item) and Exposure (three items). Also, to extract the required data, two researchers independently used a pre‐prepared checklist including: first author, study site, sample size, tools, and the prevalence of PPD used.
2.5. Statistical analysis
In this study, the binomial distribution formula was used to calculate the standard error of prevalence in each study. Random effects model was used to estimate pooled measures and 95% confidence interval [CI]. The I 2 index was used to examine the heterogeneity between studies and heterogeneity less than 25%, 25%–50%, 50%–75% and more than 75% indicate no heterogeneity, moderate heterogeneity, high and very high. 17 The effect of heterogeneity on the prevalence of PPD was investigated by analyzing the subgroups based on the type of tools and also the cut‐off points of the tools. Publication bias in the study was assessed using the Begg test. All analyzes were performed using STATA software, version 14 (StataCorp., College Station, TX, USA).
3. RESULTS
In this review study, 671 initial articles were identified through search and after removing duplicates, 454 studies were screened and finally 24 studies were selected and evaluated for quality and all of them entered the meta‐analysis stage (Figure 1). Also in this study, 13 169 women were examined for postpartum depression during COVID‐19. In this study, Edinburgh Postnatal Depression Scale (EPDS) and Postpartum Depression Screening Scale‐Short Form (PDSS‐SF) were used to evaluate PPD.
FIGURE 1.
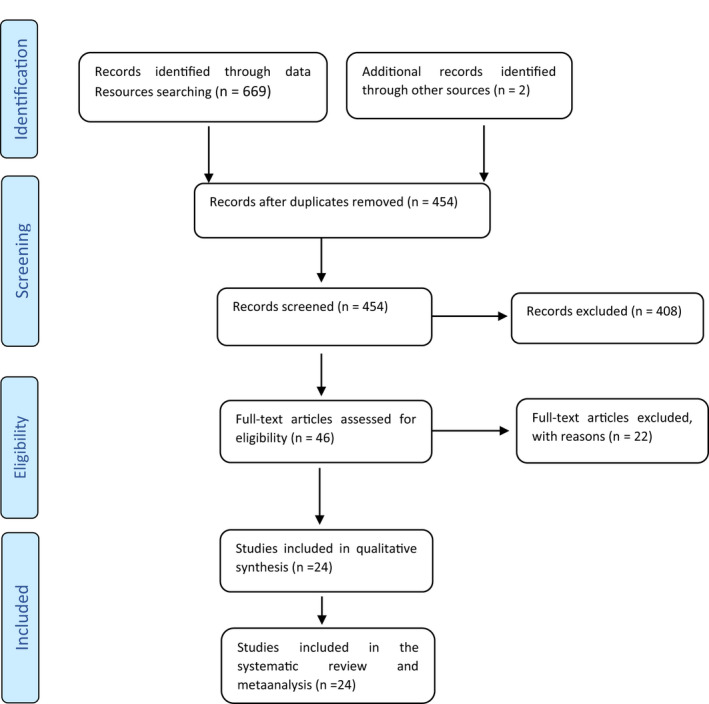
Flowchart of the selection of studies based on PRISMA
Among the selected methodology studies, 18 were cross‐sectional studies, five were retrospective cohort studies, and two were case control studies. The characteristics of other studies are also listed in Table 2. Based on the results of this study, three studies were performed based on EPDS ≥9 and PPD levels 12% (95% CI = 0.07–17, I 2 = 97%, P = 0.009) were reported. Eight studies were done based on EPDS ≥10 and PPD 27% (95% CI = 15–39, I 2 = 99%, P = < 0.001) was reported. Three study was done based on EPDS ≥11 and PPD 44% (95% CI = 40–49, I 2 = 0.0%, P = 0.436) was reported. Three studies were done based on EPDS ≥12 and PPD 27% (95% CI = 0.06–49, I 2 = 97.4%, P = < 0.001). Seven studies were done based on EPDS ≥13 and PPD 28% (95% CI = 18–39, I 2 = 98.5%, P = < 0.001) was reported. One study was done based on PDSS‐SF ≥17 and PPD 37% (95% CI = 32–42) was reported. Also, total prevalence of PPD in women during COVID‐19, 28% (95% CI = 23–33, I 2 = 98.5%, P = < 0.001) (Figure 2). Index I 2 showed that heterogeneity between studies is very high (Figure 2). Based on the Begg test results (P = 0.084), the publication bias is not significant in the present study (Figure 3).
TABLE 2.
Characteristics of entered study in systematic review and meta‐analysis
| First author | Type of study | Location | Tools | Sample size | Prevalence of PPD (%) |
|---|---|---|---|---|---|
| An 18 | Cross‐sectional | China | EPDS ≥10 | 209 | 56.9 |
|
Ceulemans 19 |
Cross‐sectional | Ireland, Norway, Switzerland, Netherlands, United Kingdom | EPDS ≥13 | 5134 | 13 |
| Stojanov 20 | Cross‐sectional | Serbia | EPDS ≥10 | 108 | 14.8 |
| Fallon 21 | Cross‐sectional | UK | EPDS ≥13 | 614 | 43 |
| Guvenc 22 | Cross‐sectional | Turkey | EPDS ≥13 | 212 | 34.0 |
| Hiiragi 23 | Retrospective cohort | Japan | EPDS ≥9 | 279 | 14 |
| Baran 11 | Cross‐sectional | Poland | EPDS ≥11 | 130 | 40 |
| Liang 24 | Cross‐sectional | China | EPDS ≥10 | 864 | 30.0 |
| Loret de Mola 25 | Retrospective cohort | Brazil | EPDS ≥13 | 1042 | 29.3 |
| Mariño‐Narvaez 26 | Cross‐sectional | Spanish | EPDS ≥10 | 75 | 22.4 |
| Oskovi‐Kaplan 27 | Cross‐sectional | Turkey | EPDS ≥13 | 223 | 14.7 |
| Ostacoli 28 | Cross‐sectional | Italy | EPDS ≥11 | 163 | 44.2 |
| Pariente 29 | Retrospective cohort | Israel | EPDS ≥10 | 223 | 16.7 |
| Spinola 30 | Cross‐sectional | Italy | EPDS ≥12 | 243 | 44 |
| Suárez‐Rico 31 | Cross‐sectional | Mexico | EPDS ≥13 | 293 | 39.2 |
| Suzuki 32 | Cross‐sectional | Japan | EPDS ≥9 | 132 | 14.4 |
| Myers 33 | Cross‐sectional | United Kingdom | EPDS ≥11 | 162 | 47.5 |
| Vatcheva 34 | Cross‐sectional | Belgium | EPDS ≥13 | 34 | 26 |
| Hui 35 | Retrospective cohort | Hong Kong | EPDS ≥10 | 802 | 2.9 |
| Hui 35 | Retrospective cohort | Hong Kong | EPDS ≥10 | 925 | 14.4 |
| Miranda 4 | Cross‐sectional | Argentina | PDSS‐SF ≥17 | 305 | 37 |
| Terada 36 | Cross‐sectional | Japan | EPDS ≥9 | 461 | 7.6 |
| Zanardo 13 | Case – control | Italy | EPDS ≥12 | 91 | 26 |
| Tarabay 37 | Cross‐sectional | Saudi Arabia | EPDS ≥10 | 150 | 60.7 |
| Madera 38 | Case – control | Italy | EPDS ≥12 | 295 | 11.9 |
Abbreviations: EPDS, Edinburgh Postnatal Depression Scal; PDSS‐SF, Postpartum Depression Screening Scale‐Short Form; PPD, postpartum depression.
Bold values indicate statistically significant.
FIGURE 2.
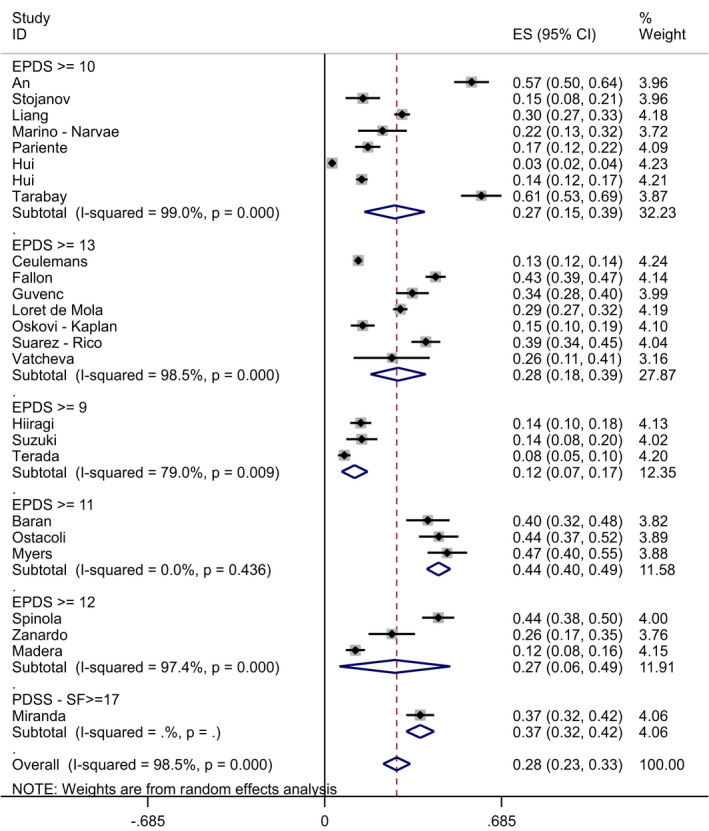
Forest plot of the prevalence of PPD among women during COVID‐19 in general and separately with 95% confidence interval. PPD, postpartum depression
FIGURE 3.
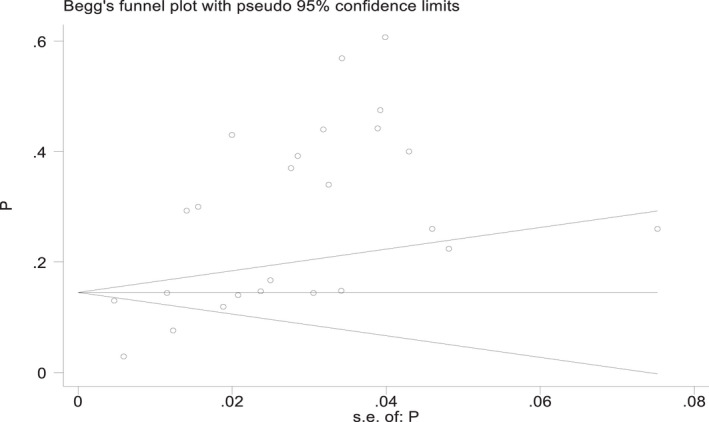
Publication bias based on Begg test
4. DISCUSSION
Based on the results of this review study, 24 articles were reviewed and meta‐analyzed and the overall prevalence of PPD in the COVID‐19 pandemic was reported to be 28%. Also, the results of index I 2 (98.5%) showed that the heterogeneity between studies is very high. In another systematic review and meta‐analysis study, the overall prevalence of depression in pregnant women during COVID‐19 was 29% and PPD in the three reviewed articles was 22% with an I 2 index (85.7%). 39 In other meta‐analysis studies, the prevalence of depression in pregnant and or lactating women during COVID‐19 was reported to be 27%. 40 The results of the studies were consistent with the present study, so it can be concluded that COVID‐19 can play an important role in the development of depression both during pregnancy and after delivery. Therefore, health care providers should screen mothers for depression during the COVID‐19 pandemic from early pregnancy to the postpartum period. On the other hand, in the study of heterogeneity between studies, it was shown that in all studies that have examined the prevalence of PPD, they have a very high degree of heterogeneity, which can be due to the use of different sample sizes as well as the use of tools and cut‐off points. Different points in prevalence studies.
In this study, in addition to reporting the overall prevalence of PPD, a subgroup analysis was used to report the prevalence of PPD based on the type of instrument and cut‐point. The results showed that according to EPDS ≥ 10 tool, the prevalence of PPD was 27% and according to EPDS ≥ 13, the prevalence of PPD was 28%. The results of another meta‐analysis study that examined the prevalence of PPD in women in the Middle East without considering the effect of COVID‐19 showed that according to the EPDS tool> = 10 PPD prevalence of 18%, based on EPDS ≥ 13 PPD prevalence 25%. 41 The results of another study that predicted PPD in earthquake survivors showed that based on EPDS ≥ 13, the PPD rate is 13. 42 According to studies, COVID‐19 causes stress due to factors such as unpredictability, uncertainty about disease control, and serious life‐threatening risks. 1 COVID‐19 also exacerbates mental illness, feelings of hopelessness, anxiety, and social isolation. 43 On the other hand, pregnancy and childbirth have been two important events in a woman’s life and the birth of a baby causes sudden and drastic changes in a woman’s roles and responsibilities. Therefore, the postpartum period indicates the time of onset of PPD. 44 In reviewing the results of studies and the present study, it can be concluded that the prevalence of PPD during COVID‐19 was higher than other disasters as well as non‐COVID‐19 conditions, and based on what was said, it can be concluded that mothers during COVID‐19, in addition to experiencing important events such as pregnancy and childbirth, are exposed to severe psychological consequences, especially stress and anxiety, which can increase the risk of PPD. Therefore, in order to prevent or reduce the rate of PPD, it is recommended that mothers, as a vulnerable group, receive special physical and psychological care and support during COVID‐19, and in case of depressive symptoms, special measures and interventions are needed, as well as frequent follow‐ups performed by health centers and hospitals because PPD may affect mothers’ social behaviors and may lead to persistent depression.
The COVID‐19 outbreak has had significant effects on vulnerable groups, especially pregnant women. Additionally, the pregnancy and postpartum periods are vulnerable periods that can increase the level of distress in many women. 45 According to other studies, factors such as economic and social factors, history of childbirth, lifestyle and history of mental illness, level of education, gestational diseases, family dissatisfaction and limited communication and interaction with others are important predictors of PPD. 46 , 47 Studies show that several factors play a role in the occurrence of PPD, for example, COVID‐19 as a stressor can accelerate the occurrence of PPD, so mothers should be under close monitoring during pregnancy and after childbirth by families and health care workers. Also, it is recommended that government officials, psychologists and health managers provide stress management training to identify and diagnose women with a history of mental disorders and develop programs and protocols for mental health support for women during and after pregnancy.
5. CONCLUSION
The findings of this study showed that the prevalence of PPD in women was relatively high during COVID‐19. Since PPD can lead to major depression and dangerous behaviors such as suicide and other life‐threatening behaviors and have impacts on social behaviors, considering the psychological consequences of the COVID‐19 pandemic in this period is important. Psychological interventions are necessary in pregnancy and after childbirth for prevention of mental disorders, especially depression. Prevention, reduction, diagnosis, treatment and rehabilitation of PPD require screening, frequent follow‐ups, training, interventions and physical and psychological support from health care centers and hospitals. It is also recommended that studies should be undertaken to identify the challenges of pregnant and postpartum women in disasters to provide preventive solutions, formulate strategies and appropriate responses and rehabilitation solutions.
AUTHOR CONTRIBUTIONS
MS‐K and AS conceived the study. Meysam Safi‐Keykaleh, Hamid Safarpour and Ali Sahebi designed the study. Meysam Safi‐Keykaleh, Fatemeh Aliakbari, Mehdi Safari, Hojjat Sheikhbardsiri and Azadeh Tahernejad screened the abstracts for inclusion in the study. Ali Sahebi and Hamid Safarpour analyzed the data. Meysam Safi‐Keykaleh and Ali Sahebi drafted the manuscript, which was then critically revised by all authors. All authors approved the final manuscript.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
Safi‐Keykaleh M, Aliakbari F, Safarpour H, et al. Prevalence of postpartum depression in women amid the COVID‐19 pandemic: A systematic review and meta‐analysis. Int J Gynecol Obstet. 2022;157:240–247. doi: 10.1002/ijgo.14129
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Adibi A, Golitaleb M, Farrahi‐Ashtiani I, et al. The prevalence of generalized anxiety disorder among health care workers during the COVID‐19 pandemic: a systematic review and meta‐analysis. Front Psychiatry. 2021;12(645):658846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID‐19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2):e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not OK: COVID‐19 and maternal mental health. Front Glob Womens Health. 2020;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miranda AR, Scotta AV. Triggering of postpartum depression and insomnia with cognitive impairment in Argentinian women during the pandemic COVID‐19 social isolation in relation to reproductive and health factors. Midwifery. 2021;102:103072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Farewell CV, Jewell J, Walls J, Leiferman JA. A mixed‐methods pilot study of perinatal risk and resilience during COVID‐19. J Prim Care Community Health. 2020;11:2150132720944074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jago CA, Singh SS, Moretti F. Coronavirus disease 2019 (COVID‐19) and pregnancy: combating isolation to improve outcomes. Obstet Gynecol. 2020;136(1):33‐36. [DOI] [PubMed] [Google Scholar]
- 7. Lebel C, MacKinnon A, Bagshawe M, Tomfohr‐Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID‐19 pandemic. J Affect Disord. 2020;277:5‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bo H‐X, Yang Y, Chen J, et al. Prevalence of depressive symptoms among pregnant and postpartum women in China during the COVID‐19 pandemic. Psychosom Med. 2021;83(4):345‐350. [DOI] [PubMed] [Google Scholar]
- 9. Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. Am J Psychiatry. 2006;163(8):1443‐1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hamami H, Sheiner E, Wainstock T, et al. The association between delivery during the COVID‐19 pandemic and immediate postpartum maternal cognitive function. J Clin Med. 2020;9(11):3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baran J, Leszczak J, Baran R, et al. Prenatal and postnatal anxiety and depression in mothers during the COVID‐19 pandemic. J Clin Med. 2021;10(14):3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Misri S, Reebye P, Corral M, Milis L. The use of paroxetine and cognitive‐behavioral therapy in postpartum depression and anxiety: a randomized controlled trial. J Clin Psychiatry 2004;65(9):0‐, 1236, 1241. [DOI] [PubMed] [Google Scholar]
- 13. Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID‐19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynecol Obstet. 2020;150(2):184‐188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross‐sectional studies (AXIS). BMJ Open. 2016;6(12):e011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wells GA, Shea B, O’Connell D, et al. The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. 2014.
- 17. Sahebi A, Abdi K, Moayedi S, Torres M, Golitaleb M. The prevalence of insomnia among health care workers amid the COVID‐19 pandemic: an umbrella review of meta‐analyses. J Psychosom Res. 2021;149:110597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. An R, Chen X, Wu Y, et al. A survey of postpartum depression and health care needs among Chinese postpartum women during the pandemic of COVID‐19. Arch Psychiatr Nurs. 2021;35(2):172‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ceulemans M, Foulon V, Ngo E, et al. Mental health status of pregnant and breastfeeding women during the COVID‐19 pandemic—a multinational cross‐sectional study. Acta Obstet Gynecol Scand. 2021;100:1219‐1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stojanov J, Stankovic M, Zikic O, Stankovic M, Stojanov A. The risk for nonpsychotic postpartum mood and anxiety disorders during the COVID‐19 pandemic. Int J Psychiatry Med. 2021;56(4):228‐239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fallon V, Davies SM, Silverio SA, Jackson L, De Pascalis L, Harrold JA. Psychosocial experiences of postnatal women during the COVID‐19 pandemic. A UK‐wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J Psychiatr Res. 2021;136:157‐166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guvenc G, Yesilcinar İ, Ozkececi F, et al. Anxiety, depression, and knowledge level in postpartum women during the COVID‐19 pandemic. Perspect Psychiatr Care. 2021;57(3):1449‐1458. [DOI] [PubMed] [Google Scholar]
- 23. Hiiragi K, Obata S, Misumi T, Miyagi E, Aoki S. Psychological stress associated with the COVID‐19 pandemic in postpartum women in Yokohama, Japan. J Obstet Gynaecol Res. 2021;47(6):2126‐2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liang P, Wang Y, Shi S, Liu Y, Xiong R. Prevalence and factors associated with postpartum depression during the COVID‐19 pandemic among women in Guangzhou, China: a cross‐sectional study. BMC Psychiatry. 2020;20(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Loret de Mola C, Martins‐Silva T, Carpena MX, et al. Maternal mental health before and during the COVID‐19 pandemic in the 2019 Rio Grande birth cohort. Braz J Psychiatry. 2021;43:402‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mariño‐Narvaez C, Puertas‐Gonzalez JA, Romero‐Gonzalez B, Peralta‐Ramirez MI. Giving birth during the COVID‐19 pandemic: the impact on birth satisfaction and postpartum depression. Int J Gynecol Obstet. 2021;153(1):83‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Oskovi‐Kaplan ZA, Buyuk GN, Ozgu‐Erdinc AS, Keskin HL, Ozbas A, Tekin OM. The effect of COVID‐19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr Q. 2021;92(2):675‐682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ostacoli L, Cosma S, Bevilacqua F, et al. Psychosocial factors associated with postpartum psychological distress during the COVID‐19 pandemic: a cross‐sectional study. BMC Pregn Childbirth. 2020;20(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pariente G, Broder OW, Sheiner E, et al. Risk for probable post‐partum depression among women during the COVID‐19 pandemic. Arch Womens Ment Health. 2020;23(6):767‐773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Spinola O, Liotti M, Speranza AM, Tambelli R. Effects of COVID‐19 epidemic lockdown on postpartum depressive symptoms in a sample of Italian mothers. Front Psychiatry. 2020;11:1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Suárez‐Rico BV, Estrada‐Gutierrez G, Sánchez‐Martínez M, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID‐19 lockdown. Int J Environ Res Public Health. 2021;18(9):4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Suzuki S. Psychological status of postpartum women under the COVID‐19 pandemic in Japan. J Matern Fetal Neonatal Med. 2020;1‐3. [DOI] [PubMed] [Google Scholar]
- 33. Myers S, Emmott EH. Communication across maternal social networks during England’s first national lockdown and its association with postnatal depressive symptoms. Front Psychol. 2021;12:1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vatcheva T, Mostaert A, Van Ingelgem V, Henrion E, Legros L. Impact of COVID‐19 pandemic on postpartum depression among mothers of extreme and early preterm infants. Int J Gynecol Obstet. 2021;155:490‐495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hui P, Ma G, Seto T, Cheung K. Effect of COVID‐19 on delivery plans and postnatal depression scores of pregnant women. Hong Kong Med J. 2020;27:113‐117. [DOI] [PubMed] [Google Scholar]
- 36. Terada S, Kinjo K, Fukuda Y. The relationship between postpartum depression and social support during the COVID‐19 pandemic: a cross‐sectional study. Journal of Obstetrics and Gynaecology Research. 2021;47:3524‐3531. [DOI] [PubMed] [Google Scholar]
- 37. Tarabay AI, Boogis D, Tabbakh AT, et al. Prevalence and factors associated with postpartum depression during the COVID‐19 Pandemic among Women in Jeddah, Saudi Arabia: a cross‐sectional study. Open Journal of Obstetrics and Gynecology. 2020;10(11):1644‐1657. [Google Scholar]
- 38. Madera P, Romagnolo C, Zanetti S, Dal Maso F, Turro M, De Marco C. Effects of the COVID‐19 pandemic on postpartum depression: a retrospective case‐control study on a significant sample of mothers in northern Italy. J Prenat Perinat Psychol Health. 2021;35:589916. [Google Scholar]
- 39. Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta‐analysis. Front Psychol. 2020;11:3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Demissie DB, Bitew ZW. Mental health effect of COVID‐19 pandemic among women who are pregnant and/or lactating: a systematic review and meta‐analysis. SAGE Open Med. 2021;9:20503121211026195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alshikh Ahmad H, Alkhatib A, Luo J. Prevalence and risk factors of postpartum depression in the Middle East: a systematic review and meta–analysis. BMC Pregn Childbirth. 2021;21(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Demirchyan A, Petrosyan D, Armenian HK. Rate and predictors of postpartum depression in a 22‐year follow‐up of a cohort of earthquake survivors in Armenia. Arch Womens Ment Health. 2014;17(3):229‐237. [DOI] [PubMed] [Google Scholar]
- 43. Sahebi A, Nejati‐Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID‐19 pandemic: an umbrella review of meta‐analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Slomian J, Honvo G, Emonts P, Reginster J‐Y, Bruyère O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health. 2019;15:1745506519844044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Boekhorst MG, Muskens L, Hulsbosch LP, et al. The COVID‐19 outbreak increases maternal stress during pregnancy, but not the risk for postpartum depression. Arch Womens Ment Health. 2021;24(6):1037‐1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Do TKL, Nguyen TTH, Pham TTH. Postpartum depression and risk factors among Vietnamese women. Biomed Res Int. 2018;2018:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: a narrative review. J Educ Health Promot. 2017;6:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


