Abstract
Background
Patients with type 2 diabetes mellitus (T2DM) are prone to develop non-alcoholic fatty liver disease (NAFLD) and cardiovascular diseases (CVD). We aimed to investigate whether the resveratrol supplementation improves novel hepatic and cardiovascular indices in these patients.
Methods
We conducted a double-blind, randomized controlled trial for 8 weeks. Seventy-six patients with T2DM were randomly assigned to receive 1000 mg/day resveratrol or placebo. Levels of lipid accumulation product (LAP), visceral adiposity index (VAI), Castelli risk index I (CRI-I), CRI-II and atherogenic coefficient (AC) were measured at the beginning and after intervention.
Results
A total of 71 participants completed the trial. After adjusting for confounding factors including medications, diabetes duration, energy intake and physical activity, no significant difference was found between the intervention group and the control group in LAP (mean change: − 2.46 ± 23.3 vs. 1.43 ± 14.3; P = 0.43), VAI (mean change: − 0.25 ± 1.1 vs. − 0.02 ± 0.6; P = 0.47), CRI-I (mean change: − 0.25 ± 0.9 vs. − 0.09 ± 0.5; P = 0.79), CRI-II (mean change: − 0.23 ± 0.7 vs. − 0.06 ± 0.6; P = 0.38) and AC (mean change: − 0.25 ± 0.9 vs. − 0.09 ± 0.5; P = 0.79).
Conclusions
Resveratrol supplementation had no effect on hepatic steatosis and cardiovascular indices. Further clinical trials, especially among subjects with dyslipidemia are needed to reach a firm conclusion. In addition, taking all medications should be controlled in future studies.
Trial registration The protocol was registered on 29/12/2017 at the Iranian clinical trials website (IRCT20171118037528N1) with URL: https://en.irct.ir/trial/27734.
Keywords: Type 2 diabetes mellitus, Resveratrol, Steatosis, Cardiovascular risk
Background
The prevalence of type 2 diabetes mellitus (T2DM) is increasing, and has become a major public health problem [1]. In 2020, the worldwide prevalence of T2DM was estimated about 6.3% among adult population [2]. The main characteristics of T2DM are elevated blood glucose and decreased insulin sensitivity [3]. Non-alcoholic fatty liver disease (NAFLD) is strongly linked to T2DM, and is more prevalent in these patients [4, 5]. Insulin resistance, inflammation, dyslipidemia, oxidative stress and obesity are involved in the pathogenesis of both T2DM and NAFLD [6–8]. Recently, new non-invasive indices including lipid accumulation product (LAP) and visceral adiposity index (VAI) have been introduced [9, 10] that can accurately assess hepatic steatosis [9–13]. It is also well established that prevalence of CVD is high among patients with T2DM, and it is known as a main cause of death among patients with T2DM [14]. Castelli risk index (CRI) and atherogenic coefficient (AC) are developed based on lipid profile to estimate cardiovascular risk [15, 16].
Resveratrol (3,5,4′-trihydroxy-trans-stilbene), as a polyphenolic compound with antioxidant and anti-inflammatory properties, is mainly found in plants such as berries, red grapes, rhubarb and peanuts [17]. Recent studies have revealed the beneficial effect of resveratrol on glycemic status, insulin sensitivity, oxidative stress and inflammation [18–22]. In addition, experimental studies have suggested that resveratrol can improve the severity of NAFLD through attenuating obesity and dyslipidemia [23–27].
There are some clinical trials that evaluated the effect of resveratrol supplementation on cardiovascular risk factors [18, 28–30]; but, their findings are inconsistent. On the other hand, the results of studies that investigated the effect of resveratrol on severity of NAFLD are not integrated [22, 31–33]. In addition, there is no study evaluating the effect of resveratrol supplementation on hepatic steatosis in patients with T2DM. Accordingly, we designed a randomized controlled trial (RCT) to investigate the effect of resveratrol supplementation (1000 mg/d) on hepatic steatosis indices (LAP and VAI) and cardiovascular indices (CRI-I, CRI-II and AC) in patients with T2DM.
Methods
Sample size
The present article is a part of our study [34] that estimated the optimal sample size (equal to or more than 36 participants in each group) based on the peroxisome proliferator-activated receptor alpha (PPARα) gene expression in the peripheral blood mononuclear cells (PBMCs) [35], using a proposed formula for parallel clinical trials [36] by considering α = 0.05, a power of 80%, and assuming a 20% of drop-out rate. However, a retrospective power analysis was performed for outcomes of this article to assure the sample size is adequate to detect statistical significance, and adequate power was observed for all the interested outcomes except for CRI-I levels (power = 44% for CRI-I).
Recruitment and eligibility screening
Endocrinologist-diagnosed patients with T2DM were identified and screened at the Diabetes Research Center affiliated with Shahid Sadoughi University of Medical sciences in Yazd, Iran. The inclusion criteria were aged 30–60 years, body mass index (BMI) ranging 25–30 kg/m2 and glycated hemoglobin (HbA1c) lower than 8%. The exclusion criteria were as follows: all types of cancer, kidney or liver failure, gastrointestinal ulcers, mental disorders, cardiovascular diseases, insulin therapy, pregnancy or lactation, consuming antioxidant supplements, fibrate lipid‐lowering agents, platelet aggregation inhibitor or anti-inflammatory medications, and also red wine consumption (for at least 6 months before the enrollment). Participants with compliance rate lower than 80%, and who were unwilling to continue the trial were dropped out from the study.
Trial design
A double-blind, placebo-controlled, single-center, randomized clinical trial with two parallel study arms (the resveratrol and placebo groups) was conducted for 8 weeks. The study was in complete agreement with the Helsinki declaration, and the protocol approved by the medical ethics committee of Shahid Sadoughi University of Medical Sciences and Health Services, Yazd (IR.SSU.SPH.REC.1396.120). All the participants were fully aware about the study process and they were asked to signed the consent form. The protocol of trial was registered on 29/12/2017 at the Iranian clinical trials website under code number IRCT20171118037528N1, with URL: https://en.irct.ir/trial/27734.
Participants were enrolled using a stratified randomization process based on gender (male/female) and age (30–45 and 45–60 years), utilizing a random allocation software (random numbers table) [37]. Random allocation of the participants to the resveratrol and placebo groups was performed by a third person. The participants and investigators were all blinded to the intervention assignment until the end of the intervention. The intervention group received 1000 mg/d resveratrol (two capsules per day, each capsule provided 500 mg of 99.71% micronized trans‐resveratrol with particle size lower than 1.9 μm and without any inactive ingredients, fillers, flavoring agents, and additives (Mega‐Resveratrol, Danbury, USA)), and the control group received the same amount and appearance of capsules containing methylcellulose. Packaging and labeling the containers as A or B was performed by a third person. The number of capsules that were not consumed by the participants was recorded at the end of the trial, and the compliance rate of each participant was evaluated.
Dietary intake and physical activity assessments
The participants were asked to record their foods and beverages intakes at baseline and end of the trial (two weekdays and one weekend day). The Nutritionist IV software (The Hearst Corporation, San Bruno, CA) was used to analyze the collected data [38].
Moreover, using a validated questionnaire [39], the physical activity was measured at baseline and end of the trial. This questionnaire provides metabolic equivalents (METs) based on the type and intensity of activities in nine different levels from sleep/rest (0.9 METs) to high-intensity activities (> 6 METs). Calculating METs/h was performed by multiplying the time spent on each activity by the MET value, and finally, MET/h per day obtained by adding the MET/h of each activity together.
Anthropometric assessments
Anthropometric variables including height, weight, and waist circumference (WC) were measured using standard methods, before and after the study. Height of participants was assessed via a stadiometer (Seca, Hamburg, Germany) with an accuracy of 0.5 cm. Utilizing a bioelectrical impedance analyzer (Tanita BC‐418, Tokyo, Japan), weight was measured with light clothes and without shoes. Measuring WC was performed using a flexible tape with an accuracy of 0.5 cm. BMI was calculated using the following formula: weight (kg)/height squared (m2).
Laboratory evaluations
An overnight fasting venous blood sample (10 mL) was obtained from all participants. Samples were centrifuged at a speed 3000 rpm, for 10 min at 25 °C (Eppendorf AG, Hamburg), and serums were immediately frozen at −70 °C. Total cholesterol (TC), triglycerides (TG), low density lipoprotein-cholesterol (LDL-c) and high density lipoprotein-cholesterol (HDL-c) concentrations were measured by an autoanalyzer (AVIDA 1800 chemistry system; Siemens, United Kingdom) and utilizing Pars Azmoon kits (Tehran, Iran), at baseline and end of the study.
Hepatic steatosis and cardiovascular indices
The LAP [9], VAI [10], CRI-I [16], CRI-II [16] and AC [15] indices were calculated at the baseline and end of the study based on the following equations:
Statistical analysis
We used the statistical package for social science (SPSS) software (Chicago, Illinois, USA) version 24 to perform statistical analyses. Comparing the qualitative variables between two groups was performed using chi-square test. We used an independent t-test to compare the means of variables between the two groups. Within group comparisons were performed utilizing paired t-test. Analysis of covariance (ANCOVA) was carried out to adjust the effect of confounding factors (medications, diabetes duration, energy intake and physical activity). P < 0.05 was considered significant. Further details of the study protocol have been previously reported [34].
Results
Characteristics of the participants
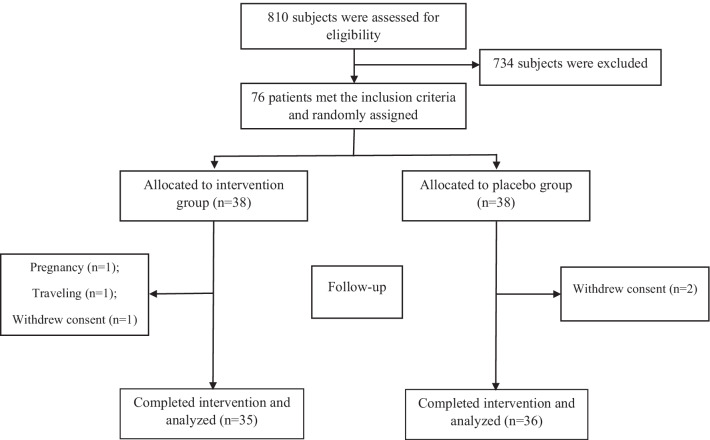
A total of seventy-six patients were enrolled and randomly assigned into the intervention and control groups. Five patients left the trial due to the pregnancy (n = 1), traveling (n = 1), and withdrawal of consent (n = 3). Finally, 71 participants including 35 patients in the intervention group and 36 patients in the control group completed the trial (Fig. 1). All variables had normal distribution, and parametric tests were used to analyze data. The participants did not report any serious adverse event during intervention.
Fig. 1.
Flowchart of eligibility, screening and follow-up
There were no significant differences between the intervention and control groups for the baseline measures, except for VAI which was significantly higher in the intervention group, compared to the control group (P = 0.04) (Table 1). In addition, no significant difference between two groups was observed in dietary intakes and physical activity at the baseline and during intervention (Table 2).
Table 1.
Baseline characteristics of patients with type 2 diabetes
| Variables | Intervention (n = 35) | Control (n = 36) | Pa |
|---|---|---|---|
| Age, y | 50.1 ± 7.3 | 50.0 ± 7.6 | 0.96 |
| Diabetes duration, y | 9.40 ± 7.0 | 8.11 ± 6.9 | 0.44 |
| Gender | 0.89 | ||
| Male, n (%) | 20 (57.1) | 20 (55.6) | |
| Female, n (%) | 15 (42.9) | 16 (44.4) | |
| Medications | |||
| Metformin, n (%) | 30 (85.7) | 31 (86.1) | 0.96 |
| Glibenclamide, n (%) | 11 (31.4) | 16 (44.4) | 0.25 |
| Statins, n (%) | 3 (8.6) | 4 (11.1) | 0.70 |
| Blood pressure lowering drugs, n (%) | 6 (17.2) | 5 (13.9) | 0.72 |
| Height, cm | 164.94 ± 7.2 | 162.08 ± 11.29 | 0.20 |
| Weight, kg | 73.69 ± 8.2 | 72.71 ± 10.5 | 0.66 |
| BMI | 27.10 ± 2.6 | 27.66 ± 2.7 | 0.39 |
| WC, cm | 91.75 ± 7.4 | 92.58 ± 8.5 | 0.66 |
| HDL-c, mg/dL | 42.49 ± 7.9 | 45.83 ± 9.0 | 0.1 |
| TG, mg/dL | 188.34 ± 81.8 | 159.89 ± 63.1 | 0.1 |
| TC, mg/dL | 167.74 ± 33.8 | 184.03 ± 43.3 | 0.08 |
| LDL-c, mg/dL | 95.86 ± 34.2 | 105.13 ± 48.7 | 0.36 |
| LAP | 65.62 ± 36.5 | 55.74 ± 29.4 | 0.21 |
| VAI | 3.29 ± 1.9 | 2.48 ± 1.2 | 0.04 |
| CRI-I | 4.09 ± 1.0 | 4.17 ± 1.1 | 0.78 |
| CRI-II | 2.35 ± 0.9 | 2.42 ± 1.2 | 0.79 |
| AC | 3.09 ± 1.0 | 3.17 ± 1.1 | 0.78 |
Data are expressed as mean ± SD for continuous variables, and as number (percentage) for categorical variables
aDifferences between the control and intervention groups were evaluated using the independent t-test for continuous variables and chi‐square test for categorical variables
BMI: body mass index; WC: waist circumference; HDL-c: high density lipoprotein-cholesterol; TG: triglyceride; TC: total cholesterol; LDL-c: low density lipoprotein-cholesterol; LAP: lipid accumulation product; VAI: visceral adiposity index; CRI: Castelli risk index; AC: atherogenic coefficient
Table 2.
Dietary intakes and physical activity in patients with type 2 diabetes
| Variables | Intervention (n = 35) | Control (n = 36) | Pb |
|---|---|---|---|
| Energy intake, kcal/d | |||
| Baseline | 1612.87 ± 587.87 | 1708.79 ± 515.39 | 0.47 |
| After intervention | 1544.71 ± 597.37 | 1674.16 ± 597.07 | 0.26 |
| Pa | 0.45 | 0.55 | |
| Carbohydrates, % | |||
| Baseline | 59.76 ± 12.71 | 59.82 ± 9.96 | 0.70 |
| After intervention | 60.66 ± 11.20 | 59.90 ± 8.76 | 0.48 |
| Pa | 0.43 | 0.88 | |
| Proteins, % | |||
| Baseline | 15.05 ± 4.65 | 15.48 ± 3.48 | 0.97 |
| After intervention | 15.20 ± 5.17 | 15.84 ± 4.02 | 0.56 |
| Pa | 0.47 | 0.56 | |
| Fats, % | |||
| Baseline | 25.19 ± 14.55 | 24.70 ± 10.42 | 0.81 |
| After intervention | 24.14 ± 11.02 | 24.26 ± 9.63 | 0.63 |
| Pa | 0.58 | 0.77 | |
| Physical activity, MET‐h/d | |||
| Baseline | 35.61 ± 5.22 | 37.54 ± 7.82 | 0.24 |
| After intervention | 36.33 ± 5.70 | 36.99 ± 5.87 | 0.62 |
| Pa | 0.14 | 0.31 | |
Values were presented as mean ± standard deviation (SD)
Pa: resulted from comparisons within groups by paired t-test
Pb: resulted from comparisons between two groups by independent t-test
Outcomes
The crude analyses did not show any significant change in LAP (P = 0.40), VAI (P = 0.30), CRI-I (P = 0.39), CRI-II (P = 0.34) and AC (P = 0.39) following the intervention (Table 3).
Table 3.
Effect of resveratrol supplementation on indices in patients with type 2 diabetes
| Indices | Intervention | Control | Pa | Pb | Pc | Pd | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male (n = 20) | Female (n = 15) | Total (n = 35) | Male (n = 20) | Female (n = 16) | Total (n = 36) | |||||
| LAP | ||||||||||
| Baseline | 53.37 ± 24.4 | 83.13 ± 44.1 | 65.62 ± 36.5 | 50.74 ± 22.0 | 61.68 ± 36.1 | 55.74 ± 29.4 | 0.72 | 0.15 | 0.21 | |
| After intervention | 50.83 ± 25.3 | 80.76 ± 40.3 | 63.16 ± 35.1 | 50.08 ± 21.9 | 65.60 ± 41.4 | 57.17 ± 32.7 | 0.92 | 0.32 | 0.46 | |
| P | 0.39 | 0.79 | 0.54 | 0.81 | 0.36 | 0.55 | ||||
| Mean change of LAP | − 2.54 ± 12.2 | − 2.37 ± 34.0 | − 2.46 ± 23.3 | − 0.65 ± 12.0 | 3.92 ± 16.8 | 1.43 ± 14.3 | 0.63 | 0.51 | 0.40 | 0.43 |
| VAI | ||||||||||
| Baseline | 2.36 ± 1.1 | 4.62 ± 2.0 | 3.29 ± 1.9 | 2.08 ± 0.9 | 2.96 ± 1.4 | 2.48 ± 1.2 | 0.40 | 0.01 | 0.04 | |
| After intervention | 2.15 ± 1.1 | 4.32 ± 1.8 | 3.04 ± 1.8 | 1.99 ± 0.8 | 3.01 ± 1.5 | 2.46 ± 1.2 | 0.62 | 0.04 | 0.12 | |
| P | 0.01 | 0.52 | 0.20 | 0.39 | 0.77 | 0.82 | ||||
| Mean change of VAI | − 0.21 ± 0.3 | − 0.30 ± 1.7 | − 0.25 ± 1.1 | − 0.09 ± 0.4 | 0.05 ± 0.7 | − 0.02 ± 0.6 | 0.39 | 0.45 | 0.30 | 0.47 |
| CRI-I | ||||||||||
| Baseline | 3.89 ± 1.0 | 4.39 ± 0.9 | 4.09 ± 1.0 | 3.92 ± 1.0 | 4.45 ± 1.2 | 4.17 ± 1.1 | 0.92 | 0.86 | 0.78 | |
| After intervention | 3.64 ± 1.0 | 4.12 ± 1.1 | 3.84 ± 1.0 | 3.87 ± 1.0 | 4.33 ± 1.2 | 4.08 ± 1.1 | 0.49 | 0.65 | 0.38 | |
| P | 0.31 | 0.29 | 0.14 | 0.68 | 0.36 | 0.35 | ||||
| Mean change of CRI-I | − 0.25 ± 1.0 | − 0.27 ± 0.8 | − 0.25 ± 0.9 | − 0.05 ± 0.5 | − 0.12 ± 0.5 | − 0.09 ± 0.5 | 0.49 | 0.62 | 0.39 | 0.79 |
| CRI-II | ||||||||||
| Baseline | 2.32 ± 0.8 | 2.40 ± 0.9 | 2.35 ± 0.9 | 2.12 ± 0.9 | 2.78 ± 1.4 | 2.42 ± 1.2 | 0.50 | 0.41 | 0.79 | |
| After intervention | 2.07 ± 0.8 | 2.20 ± 1.3 | 2.12 ± 1.0 | 2.07 ± 1.0 | 2.69 ± 1.2 | 2.36 ± 1.1 | 0.98 | 0.31 | 0.40 | |
| P | 0.20 | 0.34 | 0.10 | 0.74 | 0.58 | 0.53 | ||||
| Mean change of CRI-II | − 0.25 ± 0.8 | − 0.20 ± 0.7 | − 0.23 ± 0.7 | − 0.05 ± 0.6 | − 0.09 ± 0.6 | − 0.06 ± 0.6 | 0.38 | 0.69 | 0.34 | 0.38 |
| AC | ||||||||||
| Baseline | 2.89 ± 1.0 | 3.39 ± 0.9 | 3.09 ± 1.0 | 2.92 ± 1.0 | 3.45 ± 1.2 | 3.17 ± 1.1 | 0.92 | 0.86 | 0.78 | |
| After intervention | 2.64 ± 1.0 | 3.12 ± 1.1 | 2.84 ± 1.0 | 2.87 ± 1.0 | 3.33 ± 1.2 | 3.08 ± 1.1 | 0.49 | 0.65 | 0.38 | |
| P | 0.31 | 0.29 | 0.14 | 0.68 | 0.36 | 0.35 | ||||
| Mean change of AC | − 0.25 ± 1.0 | − 0.27 ± 0.8 | − 0.25 ± 0.9 | − 0.05 ± 0.5 | − 0.12 ± 0.5 | − 0.09 ± 0.5 | 0.49 | 0.62 | 0.39 | 0.79 |
Values of total CRI-I, CRI-II and AC were presented as mean ± standard deviation (SD), while for LAP and VAI were presented as median and quartile range
LAP: lipid accumulation product; VAI: visceral adiposity index; CRI: Castelli risk index; AC: atherogenic coefficient
P: resulted from comparisons within groups by paired t-test
Pa: resulted from comparisons between two groups (males) by independent t-test
Pb: resulted from comparisons between two groups (females) by independent t-test
Pc: resulted from comparisons between two groups (total) by independent t-test
Pd: resulted from comparisons mean changes of variables between two groups after adjusting for medications, diabetes duration, energy intake and physical activity by univariate analysis of covariance (ANCOVA)
After adjusting for confounding variables (medications, diabetes duration, energy intake and physical activity), no significant difference was also revealed in mean changes of LAP (− 2.46 ± 23.3 vs. 1.43 ± 14.3; P = 0.43), VAI (− 0.25 ± 1.1 vs. − 0.02 ± 0.6; P = 0.47), CRI-I (− 0.25 ± 0.9 vs. − 0.09 ± 0.5; P = 0.79), CRI-II (− 0.23 ± 0.7 vs. − 0.06 ± 0.6; P = 0.38) and AC (− 0.25 ± 0.9 vs. − 0.09 ± 0.5; P = 0.79) between groups (Table 3). In addition, a split-sample analysis by gender was performed, and results of all comparisons remained non-significant (Table 3).
Discussion
The present study found no significant improvement in hepatic and cardiovascular indices following an 8-week 1000 mg/d resveratrol supplementation in patients with T2DM.
It has been confirmed that LAP and VAI can accurately estimate the severity of visceral adiposity and hepatic steatosis [9, 10]. The equations of these validated tools are based on the anthropometric variables and lipid profile [9, 10]. The study of Timmers et al. [40] was the only clinical trial that investigated the effect of resveratrol supplementation on hepatic steatosis among patients with T2DM, and reported that intrahepatic lipid content did not change after resveratrol supplementation (150 mg/d) for 30 days. Some studies have evaluated the effect of resveratrol supplementation in patients with NAFLD. The study of Chachay et al. [31] reported no significant effect of resveratrol supplementation for 8 weeks on hepatic steatosis in patients with NAFLD. However, the study of Faghihzadeh et al. [32], found that 500 mg/d resveratrol supplementation for 12 weeks could reduce the grade of hepatic steatosis in patients with NAFLD. In addition, another study demonstrated a beneficial effect of resveratrol supplementation for 3 months on features of NAFLD [22]. The inconsistence results may be partly related to the wide variation in intervention duration. Clinical trials with longer intervention durations reported the beneficial effect of resveratrol supplementation on hepatic steatosis [22, 32]. Based on the experimental evidence, resveratrol can improve hepatic steatosis through regulating inflammatory pathways, increasing antioxidant capacity and insulin sensitivity, decreasing lipogenic gene expression, de novo lipogenesis and intracellular lipids in the liver, upregulating carnitine/palmitoyl transferase 1 as well as Acyl-CoA oxidase, and subsequent increasing fatty acid (FA) oxidation [25–27, 41].
Resveratrol supplementation could not improve cardiovascular indices such as CRI-I, CRI-II and AC in the present study. These indices are developed based on lipid profile [15, 16]. Some investigations have examined the effect of resveratrol supplementation on cardiovascular indices. The study of Farzin et al. [42] found no significant effect of 12-week resveratrol supplementation (600 mg/d) on CRI-II and AIP in patients with NAFLD. However, the study of Hoseini et al. [30] reported that 500 mg/d resveratrol supplementation can improve TC/HDL-c ratio in patients with T2DM and coronary heart disease. The study of Bo et al. [43] found that resveratrol supplementation has no lipid-modifying effect in patients with T2DM. Another study demonstrated that resveratrol supplementation for 2 months leads to a significant reduction of TC and TG in subjects with dyslipidemia; however, resveratrol had no effect on HDL-C and LDL-c [44]. Consistent with our findings, a recent meta-analysis of RCTs concluded that resveratrol has no impact on dyslipidemia [45]. However, as an important limitation, most of the previous studies did not measure the level of resveratrol in the blood or its metabolites in the urine to assess the bioavailability of the resveratrol. Therefore, the findings must be interpreted with more caution. The experimental investigations suggested that resveratrol can exert its beneficial effects on cardiovascular risk factors by activating adenosine monophosphate kinase (MAPK), increasing fatty acids oxidation, downregulating lipogenic genes, regulating glucose homeostasis, activating the Akt pathway, stimulating intracellular glucose transport, and increasing insulin sensitivity [18, 46–48]. Previously, we reported the effect of resveratrol supplementation on PPARα, p16, p53, p21 gene expressions, and cluster of differentiation 163 (CD163)/ TNF-like weak inducer of apoptosis (TWEAK) ratio in serum [49]. In addition, we reported the findings of anthropometric parameters, lipid profile, atherogenic index of plasma, serum levels of asymmetric de-methyl-arginine and paraoxonase 1 activity [20, 29]. To follow the ethical principals in research, we declare that we used the same data for the present article. To proper understanding and interpretation, Fig. 1 and some important information (baseline characteristics, dietary intakes and physical activity) of our previous articles (20, 29) were added to the present article.
To the best of our knowledge, this is the first study that evaluated the effect of resveratrol supplementation on non-invasive and simple indices such as LAP and VAI in patients with T2DM. In addition, we used micronized trans‐resveratrol, which has higher bioavailability compared to the normal form of resveratrol. However, we conducted a short-term intervention, which is an important limitation of our study. In addition, indices of the present article are the secondary outcomes of our original study, and as mentioned, the optimal sample size was calculated according to a primary outcome. Moreover, we did not measure the level of resveratrol in the blood or its metabolites in the urine to assess the bioavailability of the resveratrol.
In conclusion, 1000 mg/d resveratrol supplementation could not improve hepatic steatosis indices and had no impact on cardiovascular indices; however, it is not mean that resveratrol has no beneficial effect on liver or cardiovascular health. In general, demonstrating the real effect of nutraceuticals on health problems is difficult, especially if the participants are being treated with various medications for their health problems. Moreover, based on the means of lipid profile, most participants in the present study had normal values for serum lipid profile that can complicate the resveratrol's ability to demonstrate efficacy. It is recommended to conduct clinical trials among individuals with higher lipid profile values to reach a definitive conclusion. Furthermore, taking all medications should be monitored and controlled in future clinical trials.
Acknowledgements
We acknowledge the contribution of the patients and co-researchers.
Abbreviations
- AC
Atherogenic coefficient
- ANCOVA
Analysis of covariance
- CRI
Castelli risk index
- CVD
Cardiovascular disease
- HbA1c
Glycated haemoglobin
- HDL-c
High-density lipoprotein cholesterol
- LAP
Lipid accumulation product
- LDL-c
Low-density lipoprotein cholesterol
- METs
Metabolic equivalents
- NAFLD
Non-alcoholic fatty liver disease
- PPARα
Peroxisome proliferator-activated receptor alpha
- PBMCs
Peripheral blood mononuclear cells
- SPSS
Statistical package for social science
- T2DM
Type 2 diabetes mellitus
- TC
Total cholesterol
- TG
Triglyceride
- VAI
Visceral adiposity index
Author contributions
H.M–K: designed the research; S.A: conducted the research; A.S: analyzed the data; A.S: wrote the manuscript; H.M–K: critically revised the manuscript. All authors reviewed the manuscript.
Funding
This study was supported by Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran, as a financial support for student thesis process.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, Hassan Mozaffari-Khosravi, upon reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Declarations
Ethics approval and consent to participate
The ethical committee of Shahid Sadoughi University of Medical Sciences and Health Services in Yazd, confirmed the study protocol, and approved the written informed consent that obtained from all participants at the beginning of the study (IR.SSU.SPH.REC.1396.120).
Consent for publication
Not applicable.
Competing interests
The authors have declared no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 2.Abdul M, Khan B, Hashim MJ, King JK, Govender RD, Mustafa H, et al. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10:107–111. doi: 10.2991/jegh.k.191028.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diabetes AA. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;36(Suppl 1):S67–74. doi: 10.2337/dc13-S067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leite NC, Villela-Nogueira CA, Cardoso CRL, Salles GF. Non-alcoholic fatty liver disease and diabetes: from physiopathological interplay to diagnosis and treatment. World J Gastroenterol. 2014;20(26):8377–8392. doi: 10.3748/wjg.v20.i26.8377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Portillo-Sanchez P, Bril F, Maximos M, Lomonaco R, Biernacki D, Orsak B, et al. High prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus and normal plasma aminotransferase levels. J Clin Endocrinol Metab. 2015;100(6):2231–2238. doi: 10.1210/jc.2015-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sangouni AA, Ghavamzadeh S, Jamalzehi A. A narrative review on effects of vitamin D on main risk factors and severity of Non-Alcoholic Fatty Liver Disease. Diabetes Metab Syndr Clin Res Rev. 2019;13(3):2260–2265. doi: 10.1016/j.dsx.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Sangouni AA, Ghavamzadeh S. A review of synbiotic efficacy in non-alcoholic fatty liver disease as a therapeutic approach. Diabetes Metab Syndr Clin Res Rev. 2019;13(5):2917–2922. doi: 10.1016/j.dsx.2019.07.063. [DOI] [PubMed] [Google Scholar]
- 8.Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, et al. Pathophysiology of type 2 diabetes mellitus. Int J Mol Sci. 2020;21(17):1–34. doi: 10.3390/ijms21176275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bedogni G, Kahn HS, Bellentani S, Tiribelli C. A simple index of lipid overaccumulation is a good marker of liver steatosis. BMC Gastroenterol. 2010;10:98. doi: 10.1186/1471-230X-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–922. doi: 10.2337/dc09-1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sangouni AA, Sangsefidi ZS, Yarhosseini F, Hosseinzadeh M, Akhondi-Meybodi M, Ranjbar A, et al. Effect of Cornus mas L. fruit extract on lipid accumulation product and cardiovascular indices in patients with non-alcoholic fatty liver disease: a double-blind randomized controlled trial. Clin Nutr ESPEN. 2021 doi: 10.1016/j.clnesp.2021.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Sangouni AA, Orang Z, Mozaffari-Khosravi H. Effect of omega-3 supplementation on fatty liver and visceral adiposity indices in diabetic patients with non-alcoholic fatty liver disease: a randomized controlled trial. Clin Nutr ESPEN. 2021;44:130–135. doi: 10.1016/j.clnesp.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 13.Sangouni AA, Sasanfar B, Ghadiri-Anari A, Hosseinzadeh M. Effect of L-carnitine supplementation on liver fat content and cardiometabolic indices in overweight/obese women with polycystic ovary syndrome: a randomized controlled trial. Clin Nutr ESPEN. 2021;46:54–59. doi: 10.1016/j.clnesp.2021.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):1–19. doi: 10.1186/s12933-018-0728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sujatha R, Kavitha S. Atherogenic indices in stroke patients: a retrospective study. Iran J Neurol. 2017;16(2):78–82. [PMC free article] [PubMed] [Google Scholar]
- 16.Sasikala T, Goswami K. Castelli risk index-1 and atherogenic coefficient are better predictors of cardiometabolic risk in patients with hypothyroidism. Int J Clin Biochem Res. 2020;7(2):254–259. doi: 10.18231/j.ijcbr.2020.055. [DOI] [Google Scholar]
- 17.Burns J, Yokota T, Ashihara H, Lean MEJ, Crozier A. Plant foods and herbal sources of resveratrol. J Agric Food Chem. 2002;50(11):3337–3340. doi: 10.1021/jf0112973. [DOI] [PubMed] [Google Scholar]
- 18.Brasnyó P, Molnár GA, Mohás M, Markó L, Laczy B, Cseh J, et al. Resveratrol improves insulin sensitivity, reduces oxidative stress and activates the Akt pathway in type 2 diabetic patients. Br J Nutr. 2011;106(3):383–389. doi: 10.1017/S0007114511000316. [DOI] [PubMed] [Google Scholar]
- 19.Zhu X, Wu C, Qiu S, Yuan X, Li L. Effects of resveratrol on glucose control and insulin sensitivity in subjects with type 2 diabetes: systematic review and meta-analysis. Nutr Metab. 2017;14(1):1–10. doi: 10.1186/s12986-017-0217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tabatabaie M, Abdollahi S, Salehi-Abargouei A, Clark CCT, Karimi-Nazari E, Fallahzadeh H, et al. The effect of resveratrol supplementation on serum levels of asymmetric de-methyl-arginine and paraoxonase 1 activity in patients with type 2 diabetes: a randomized, double-blind controlled trial. Phyther Res. 2020;34(8):2023–2031. doi: 10.1002/ptr.6655. [DOI] [PubMed] [Google Scholar]
- 21.Bagul PK, Deepthi N, Sultana R, Banerjee SK. Resveratrol ameliorates cardiac oxidative stress in diabetes through deacetylation of NFkB-p65 and histone 3. J Nutr Biochem. 2015;26(11):1298–1307. doi: 10.1016/j.jnutbio.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Faghihzadeh F, Adibi P, Rafiei R, Hekmatdoost A. Resveratrol supplementation improves inflammatory biomarkers in patients with nonalcoholic fatty liver disease. Nutr Res. 2014;34(10):837–843. doi: 10.1016/j.nutres.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Sharma R, Sharma NK, Thungapathra M. Resveratrol regulates body weight in healthy and ovariectomized rats. Nutr Metab. 2017;14(1):4–9. doi: 10.1186/s12986-017-0183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rašković A, Ćućuz V, Torović L, Tomas A, Gojković-Bukarica L, Ćebović T, et al. Resveratrol supplementation improves metabolic control in rats with induced hyperlipidemia and type 2 diabetes. Saudi Pharm J. 2019;27(7):1036–1043. doi: 10.1016/j.jsps.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gómez-Zorita S, Fernández-Quintela A, MacArulla MT, Aguirre L, Hijona E, Bujanda L, et al. Resveratrol attenuates steatosis in obese Zucker rats by decreasing fatty acid availability and reducing oxidative stress. Br J Nutr. 2012;107(2):202–210. doi: 10.1017/S0007114511002753. [DOI] [PubMed] [Google Scholar]
- 26.Ahn J, Cho I, Kim S, Kwon D, Ha T. Dietary resveratrol alters lipid metabolism-related gene expression of mice on an atherogenic diet. J Hepatol. 2008;49(6):1019–1028. doi: 10.1016/j.jhep.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 27.Bujanda L, Hijona E, Larzabal M, Beraza M, Aldazabal P, García-Urkia N, et al. Resveratrol inhibits nonalcoholic fatty liver disease in rats. BMC Gastroenterol. 2008;8:1–8. doi: 10.1186/1471-230X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Poulsen MM, Vestergaard PF, Clasen BF, Radko Y, Christensen LP, Stødkilde-Jørgensen H, et al. High-dose resveratrol supplementation in obese men an investigator-initiated, randomized, placebo-controlled clinical trial of substrate metabolism, insulin sensitivity, and body composition. Diabetes. 2013;62(4):1186–1195. doi: 10.2337/db12-0975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdollahi S, Salehi-Abargouei A, Toupchian O, Sheikhha MH, Fallahzadeh H, Rahmanian M, et al. The effect of resveratrol supplementation on cardio-metabolic risk factors in patients with type 2 diabetes: a randomized, double-blind controlled trial. Phyther Res. 2019;33(12):3153–3162. doi: 10.1002/ptr.6487. [DOI] [PubMed] [Google Scholar]
- 30.Hoseini A, Namazi G, Farrokhian A, Reiner Ž, Aghadavod E, Bahmani F, et al. The effects of resveratrol on metabolic status in patients with type 2 diabetes mellitus and coronary heart disease. Food Funct. 2019;10(9):6042–6051. doi: 10.1039/C9FO01075K. [DOI] [PubMed] [Google Scholar]
- 31.Chachay VS, Macdonald GA, Martin JH, Whitehead JP, O’Moore-Sullivan TM, Lee P, et al. Resveratrol does not benefit patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2014;12(12):2092–2103.e6. doi: 10.1016/j.cgh.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 32.Faghihzadeh F, Adibi P, Hekmatdoost A. The effects of resveratrol supplementation on cardiovascular risk factors in patients with non-alcoholic fatty liver disease: a randomised, double-blind, placebo-controlled study. Br J Nutr. 2015;114(5):796–803. doi: 10.1017/S0007114515002433. [DOI] [PubMed] [Google Scholar]
- 33.Poulsen MK, Nellemann B, Bibby BM, Stødkilde-Jørgensen H, Pedersen SB, Grønbæk H, et al. No effect of resveratrol on VLDL-TG kinetics and insulin sensitivity in obese men with nonalcoholic fatty liver disease. Diabetes Obes Metab. 2018;20(10):2504–2509. doi: 10.1111/dom.13409. [DOI] [PubMed] [Google Scholar]
- 34.Abdollahi S, Salehi-Abargouei A, Tabatabaie M, Sheikhha MH, Fallahzadeh H, Rahmanian M, et al. The effect of resveratrol supplementation on the expression levels of factors associated with cellular senescence and sCD163/sTWEAK ratio in patients with type 2 diabetes mellitus: study protocol for a double-blind controlled randomised clinical trial. BMJ Open. 2019;9(7):1–6. doi: 10.1136/bmjopen-2018-026337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D’Amore S, Vacca M, Graziano G, D’Orazio A, Cariello M, Martelli N, et al. Nuclear receptors expression chart in peripheral blood mononuclear cells identifies patients with Metabolic Syndrome. Biochim Biophys Acta Mol Basis Dis. 2013;1832(12):2289–2301. doi: 10.1016/j.bbadis.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 36.Kirby A, Gebski V, Keech AC. Determining the sample size in a clinical trial. Med J Aust. 2002;177(5):256–257. doi: 10.5694/j.1326-5377.2002.tb04759.x. [DOI] [PubMed] [Google Scholar]
- 37.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4:26. doi: 10.1186/1471-2288-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pehrsson PR, Haytowitz DB, Holden JM, Perry CR, Beckler DG. USDA’s national food and nutrient analysis program: food sampling. J Food Compos Anal. 2000;13(4):379–389. doi: 10.1006/jfca.1999.0867. [DOI] [Google Scholar]
- 39.Aadahl M, Jørgensen T. Validation of a new self-report instrument for measuring physical activity. Med Sci Sports Exerc. 2003;35(7):1196–1202. doi: 10.1249/01.MSS.0000074446.02192.14. [DOI] [PubMed] [Google Scholar]
- 40.Timmers S, De Ligt M, Phielix E, Van De Weijer T, Hansen J, Moonen-Kornips E, et al. Resveratrol as add-on therapy in subjects with well-controlled type 2 diabetes: a randomized controlled trial. Diabetes Care. 2016;39(12):2211–2217. doi: 10.2337/dc16-0499. [DOI] [PubMed] [Google Scholar]
- 41.Shang J, Chen LL, Xiao FX, Sun H, Ding HC, Xiao H. Resveratrol improves non-alcoholic fatty liver disease by activating AMP-activated protein kinase. Acta Pharmacol Sin. 2008;29(6):698–706. doi: 10.1111/j.1745-7254.2008.00807.x. [DOI] [PubMed] [Google Scholar]
- 42.Farzin L, Asghari S, Rafraf M, Asghari-Jafarabadi M, Shirmohammadi M. No beneficial effects of resveratrol supplementation on atherogenic risk factors in patients with nonalcoholic fatty liver disease. Int J Vitam Nutr Res. 2020;90(3–4):279–289. doi: 10.1024/0300-9831/a000528. [DOI] [PubMed] [Google Scholar]
- 43.Bo S, Ponzo V, Ciccone G, Evangelista A, Saba F, Goitre I, et al. Six months of resveratrol supplementation has no measurable effect in type 2 diabetic patients. A randomized, double blind, placebo-controlled trial. Pharmacol Res. 2016;111:896–905. doi: 10.1016/j.phrs.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 44.Simental-Mendía LE, Guerrero-Romero F. Effect of resveratrol supplementation on lipid profile in subjects with dyslipidemia: a randomized double-blind, placebo-controlled trial. Nutrition. 2019;58:7–10. doi: 10.1016/j.nut.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 45.Akbari M, Tamtaji OR, Lankarani KB, Tabrizi R, Dadgostar E, Haghighat N, et al. The effects of resveratrol on lipid profiles and liver enzymes in patients with metabolic syndrome and related disorders: a systematic review and meta-analysis of randomized controlled trials. Lipids Health Dis. 2020;19(1):1–12. doi: 10.1186/s12944-020-1198-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang H, Yang YJ, Qian HY, Zhang Q, Xu H, Li JJ. Resveratrol in cardiovascular disease: what is known from current research? Heart Fail Rev. 2012;17(3):437–448. doi: 10.1007/s10741-011-9260-4. [DOI] [PubMed] [Google Scholar]
- 47.Abbasi Oshaghi E, Goodarzi MT, Higgins V, Adeli K. Role of resveratrol in the management of insulin resistance and related conditions: mechanism of action. Crit Rev Clin Lab Sci. 2017;54(4):267–293. doi: 10.1080/10408363.2017.1343274. [DOI] [PubMed] [Google Scholar]
- 48.Knutson MD, Leeuwenburgh C. Resveratrol and novel potent activators of SIRT1: effects on aging and age-related diseases. Nutr Rev. 2008;66(10):591–596. doi: 10.1111/j.1753-4887.2008.00109.x. [DOI] [PubMed] [Google Scholar]
- 49.Toupchian O, Abdollahi S, Salehi-Abargouei A, Heshmati J, Clark CCT, Sheikhha MH, et al. The effects of resveratrol supplementation on PPARα, p16, p53, p21 gene expressions, and sCD163/sTWEAK ratio in patients with type 2 diabetes mellitus: a double-blind controlled randomized trial. Phyther Res. 2021;35(6):3205–3213. doi: 10.1002/ptr.7031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Hassan Mozaffari-Khosravi, upon reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of research participants.