To the Editor,
We were pleased to read the publication by Lan et al. 1 which included a meta‐analysis of the randomized controlled trials (RCTs) in which melatonin was used as a treatment for COVID‐19. Sixty‐two studies were considered, but only three RCTs (published before September 11, 2021) met the requirements for inclusion. 2 , 3 , 4 The primary outcome was the clinical recovery rate with secondary measures including the requirement for intensive care, level of inflammation, and mortality. The trial durations were 7–14 days with the total daily dose of melatonin being either 3, 6, or 9 mg. Eighty‐six patients were treated with melatonin and 85 received a placebo. Melatonin treatment significantly improved the recovery rate and provided evidence of a lowered requirement for intensive care, reduced mortality, and depressed inflammation (C‐reactive protein levels) compared to placebo. 2 , 3 , 4 The authors feel larger doses of melatonin maybe even more effective in combatting COVID‐19 infections.
These findings are consistent with the outcomes of observational studies. Castillo et al. 5 performed a case series study that included 10 severely‐ill COVID patients given 36–72 mg melatonin daily; the melatonin‐treated patients experienced a more rapid clinical improvement, reduced requirement for mechanical ventilation, shorter duration of hospitalization, and evidence of lower mortality. Also, Ramlall et al. 6 retrospectively examined the outcome of 112 COVID‐infected patients who required mechanical intubation as respiratory support and observed that those who received melatonin had a better clinical outcome compared to those who did not. Sanchez‐Gonzalez et al. 7 found that melatonin treatment of seriously‐ill COVID patients led to a reduced mortality rate. Since the cutoff date (September 2021) for the meta‐analysis described above, 1 an additional study was published using melatonin to treat COVID patients. This clinical trial investigated the impact of melatonin on the mortality of severely‐diseased COVID patients and reported a significantly reduced death rate. 8 The reduction in mortality of COVID patients who are treated with melatonin is a theme seen in most of the published studies. Obviously, there is no more important endpoint than survival and it reflects underlying physiological improvements.
Treatments for COVID have evolved quickly with vaccines taking center stage. These were developed against the initial severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) phenotype. With the persistent mutation of the virus, the efficacy of the vaccines has waned somewhat. Additionally, a significantly large percentage of the population has refused immunization, and in some less developed countries, the vaccines are neither affordable nor available. Repurposed drugs are used as treatments with variable success but newly‐developed medications are becoming available which may provide greater efficacy against COVID‐19. 9 The active ingredient of the newly‐developed Pfizer drug, paxlovid, is nirmatreliv, a Mpro inhibitor. Mpro is a major protease of SARS‐CoV‐2 which mediates viral replication and transcription. Melatonin also inhibits Mpro but has a more favorable pharmacological profile than nirmatreliv. 10 The use of melatonin as a countermeasure to COVID‐19 would represent a paradigm shift, since it directs treatment to the infected individual rather than against the virus.
Besides clinical trials, and so forth, which indicate that melatonin is effective in aiding the recovery of COVID patients, measured by any parameter considered, there is a vast amount of experimental information (150 publications to date) which clarifies why it is effective. 9 , 11 Melatonin is a powerful antioxidant and anti‐inflammatory molecule that modifies the innate immune system and functions as a pan‐antiviral agent. 12 Melatonin lowers virus uptake into cells and hinders their replication, inhibits sepsis, reduces phospholipase A2 levels, lowers inflammatory cytokines, and so forth, which contribute to acute respiratory disease and systemic multiorgan dysfunction (Figure 1). Thus, in contrast to what the vaccines and some of the other drugs which are recommended treatments for COVID‐19 do, melatonin greatly enhances the defensive posture of infected patients making them more resistant to infection by SARS‐CoV‐2 or any other virus.
Figure 1.
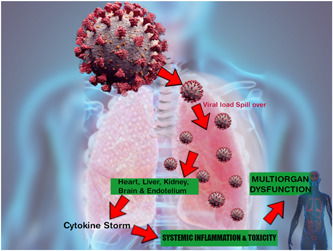
Melatonin intervenes at several levels to reduce the severity of an infection mediated by SARS‐CoV‐2. Melatonin limits the entrance of the virus into cells as well as its intracellular replication, thereby reducing the total viral load. Moreover, melatonin functions as an anti‐inflammatory molecule to lower the cytokine storm and as a potent antioxidant to curtail the cellular damage resulting from excessive free radical generation. These combined actions lead to decreased multiorgan failure and mortality. Thus, melatonin's protective actions are direct more toward improving the resistance of the individual rather than against the virus. Evidence supporting these outcomes is provided by both the results of experimental studies and of clinical trials. SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2
No single treatment will eliminate the COVID‐19 pandemic. It is imperative that all available tactics and medications be used to overcome this disease, although it will probably never totally disappear. Melatonin is inexpensive so it is affordable throughout the world, it does not require refrigeration and it has a very long shelf‐life. Melatonin has no substantial side effects even at extremely high doses, no overdose has ever occurred, and it can be self‐administered via several routes. Considering its efficacy in both experimental studies and clinical trials, the portfolio of medications used to curtail COVID‐19 infections should clearly include melatonin. Since melatonin inhibits many types of viruses, it should also be considered a potential treatment for Ebola, Zika, and hantavirus infections, and so forth.
AUTHOR CONTRIBUTIONS
After an integrated online discussion, all co‐authors (Russel J. Reiter, Ramaswamy Sharma, Dun‐Xian Tan, Richard L. Neel, Fedor Simko, Walter Manucha, Sergio Rosales‐Corral, and Daniel P. Cardinali) agreed that a letter should be submitted that would further amplify the importance of the information related to melatonin/COVID. All authors had comments concerning what should be included in the correspondence and all read and approved the submission. The figure was prepared by Sergio Rosales‐Corral.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Contributor Information
Russel J. Reiter, Email: reiter@uthscsa.edu.
Ramaswamy Sharma, Email: sharmar3@uthscsa.edu.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- 1. Lan SH, Lee HZ, Chao CM, Chang SP, Lu LC, Lai CC. Efficacy of melatonin in the treatment of patients with COVID‐19: a systematic review and meta‐analysis of randomized controlled trials. J Med Virol. 2022;94:2102‐2107. 10.1002/jmv.27595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alizadeh Z, Keyhanian N, Ghaderkhani S, Dashti‐Khavidaki S, Shokouhi Shoormasti R, Pourpak Z. A pilot study on controlling coronavirus disease 2019 (COVID‐19) inflammation using melatonin supplement. Iran J Allergy Asthma Immunol. 2021;20(4):494‐499. [PubMed] [Google Scholar]
- 3. Farnoosh G, Akbariqomi M, Badri T, et al. Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID‐19: a randomized, double‐blind clinical trial. Arch Med Res. 2022;53:79‐85. 10.1016/j.arcmed.2021.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mousavi SA, Heydari K, Mehravaran H, et al. Melatonin effects on sleep quality and outcomes of COVID‐19 patients: an open‐label, randomized, controlled trial. J Med Virol. 2021;94(1):263‐271. 10.1002/jmv.27312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Castillo RR, Quizon GRA, Juco MJM, et al. Melatonin as adjuvant treatment for coronavirus disease 2019 pneumonia patients requiring hospitalization (MAC‐19 PRO): a case series. Melatonin Res. 2020;3:297‐310. 10.32794/mr11250063 [DOI] [Google Scholar]
- 6. Ramlall V, Zucker J, Tatonetti N. Melatonin is significantly associated with survival of intubated COVID‐19 patients. MedRxiv. 2020. 10.1101/2020.10.15.20213546 [DOI] [Google Scholar]
- 7. Sanchez‐Gonzalez MA, Mahilla‐Fernandez I, Villar‐lvarez F, Llanos L. What if melatonin could help patients with severe COVID‐19? J Clin Sleep Med. 2022;18(1):335‐336. 10.5664/jcsm.9554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hasan ZT, Al Atrakji MQYMA, Mehuaiden AK. The effect of melatonin on thrombosis, sepsis and mortality rate in COVID‐19 patients. Int J Infect Dis. 2022;114:79‐84. 10.1016/j.ijid.2021.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reiter RJ, Sharma R, Simko F, et al. Melatonin: highlighting its use as a potential treatment for SARS‐CoV‐2 infection. Cell Mol Life Sci. 2022;79:143. 10.1007/s00018-021-04102-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Feitosa EL, Dos S S Júnior FT, De O Nery Neto JA, et al. COVID‐19: rational discovery of the therapeutic potential of melatonin as a SARS‐CoV‐2 main protease inhibitor. Int J Med Sci. 2020;17(14):2133‐2146. 10.7150/ijms.48053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tan DX, Hardeland R. Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID‐19. Molecules. 2020;25(19):4410. 10.3390/molecules25194410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boga JA, Coto‐Montes A, Rosales‐Corral SA, Tan DX, Reiter RJ. Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”? J Med Virol. 2012;22(5):323‐338. 10.1002/rmv.1714 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.


