Dear Editor,
Increasing pool of evidence consistently links increased red‐cell‐distribution‐width (RDW) with unfavorable clinical outcomes in cardiovascular, 1 malignant, 2 and chronic inflammatory diseases, 3 as well as in COVID‐19 patients. 4 However, uncertainties regarding the prognostic role of this parameter in anemic and non‐anemic COVID‐19 patients exist, 5 prompting us to evaluate RDW prognostic associations in these two groups of patients.
We retrospectively investigated a total of 5872 consecutive hospitalized COVID‐19 patients treated in our tertiary‐level institution (University Hospital Dubrava) in the period from 3/2020 to 6/2021 during the period of complete repurpose of the hospital solely for treatment of COVID‐19 patients. All patients were adults of white race and had confirmed COVID‐19 infection. Data used for this analysis were obtained by analysis of written and electronic medical records and are a part of the hospital registry project. RDW was assessed at the time of hospital admission. Anemia was defined as <130 g/L in males and <120 g/L in females per World Health Organization (WHO) definition. MedCalc statistical program version 20.014 was used for presented analyses (MedCalc Software Ltd). The Mann–Whitney U‐test, the Jonckheere–Terpstra test for trend, the Χ 2 test, the ROC curve analysis, and the logistic regression were used. p values <0.05 were considered statistically significant.
Among 5872 analyzed patients, there were 3297 (56.1%) males, median age was 72 years, median Charlson comorbidity index (CCI) was four points. At the time of hospital admission, a total of 4167 (71%) had severe and 897 (15.3%) patients had critical severity of COVID‐19 symptoms, respectively. Median RDW was 14%, IQR (13.3–15.1). A total of 2466 (42%) of patients were anemic per WHO definition, whereas 3405 (58%) were not. Anemic patients had significantly higher RDW levels (median 14.8 vs. 13.6%; p < 0.001).
Gradual increase in in‐hospital mortality was present with each increasing RDW percentage point in both non‐anemic and anemic patients (p for trend <0.001 for both subgroups; Figure 1A). There was a statistically significant interaction between RDW, anemia, and death (p < 0.001), however, no significant differences in in‐hospital mortality could be shown between non‐anemic and anemic patients in any of the particular RDW subgroups (p > 0.05 for all comparisons). Nevertheless, anemic patients had overall worse survival (38.2% vs. 30.7%; p < 0.001). Using the ROC‐curve analysis, optimal RDW cutoff level for in‐hospital mortality differed for non‐anemic (>13.7%, AUC 0.658) and anemic patients (>15%, AUC 0.630). Higher risk for death could be shown with RDW stratified at these specific cutoff points in both non‐anemic (odds ratio [OR] 3.65, 95% CI [2.28–3.08], p < 0.001) and anemic patients (OR 2.24, 95% CI [1.9–2.65], p < 0.001). In two separate logistic regression models for in‐hospital mortality shown in Table 1, association of increasing RDW with mortality persisted in both non‐anemic and anemic patients after adjustments for age, sex, CCI, and WHO COVID‐19 severity on admission.
Figure 1.
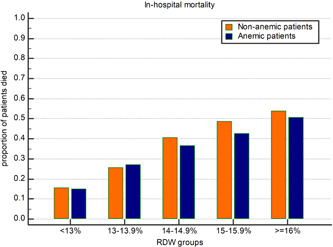
Association of increasing red cell distribution width (RDW) percentage points with in‐hospital mortality stratified according to the presence of anemia.
Table 1.
The logistic regression models for in‐hospital mortality presented separately for non‐anemic and anemic patients
| Non‐anemic patients | Anemic patients | |
|---|---|---|
| OR with 95% CI and p | OR with 95% CI and p | |
| RDW | ||
| <13% | Reference group | Reference group |
| 13%–13.9% | 1.27 (0.97–1.66); p = 0.085 | 1.66 (0.97–2.81); p = 0.059 |
| 14%–14.9% | 1.81 (1.35–2.43); p < 0.001 | 2.08 (1.22–3.53); p = 0.006 |
| 15%–15.9% | 2.61 (1.82–3.74); p < 0.001 | 2.72 (1.58–4.69); p < 0.001 |
| ≥16% | 3.26 (2.06–5.17); p < 0.001 | 3.87 (2.28–6.55); p < 0.001 |
| Age(years) | 1.05 (1.04–1.06); p < 0.001 | 1.03 (1.02–1.04); p < 0.001 |
| Male sex | 1.71 (1.43–2.04); p < 0.001 | 1.31 (1.08–1.58); p = 0.006 |
| Charlson comorbidity index | 1.15 (1.09–1.21); p < 0.001 | 1.16 (1.11–1.21); p < 0.001 |
| Severe or critical COVID‐19 | 25.54 (12.45–52.36); p < 0.001 | 19.77 (11.93–32.77); p < 0.001 |
Abbreviations: CI, confidence interval; OR, odds ratio; RDW, red cell distribution width.
There are several important points that we would like to emphasize. Negative prognostic properties of higher RDW values seem to be present both in patients with and without anemia and increase with each rising RDW percentage point regardless of anemia status. These phenomena persist in both non‐anemic and anemic subgroups of patients after adjusting analyses for clinically important parameters. Since anemia is associated with increase in anisocytosis, same degree of elevation in RDW in non‐anemic patients is probably achieved due to more pronounced inflammation and comorbidities burden (among other possible causes of increased RDW). This is probably the reason why prognostic impact of increasing RDW was more pronounced in non‐anemic than anemic patients in unadjusted analyses. Optimal RDW cutoff levels for survival discrimination seem to be higher in anemic patients (>15%) and optimized stratification among non‐anemic patients is achieved with cutoff below the upper limit of normal (>13.7%). Multivariate analyses reveal that after accounting for age, sex, comorbidities, and COVID‐19 severity, increase in RDW seems to affect anemic patients a bit more strongly since distribution of these characteristics differs among patients with different levels of RDW. Also, differences in profile of these characteristics could also explain different conclusions regarding RDW and anemia status by different author groups. 5 Mechanisms behind anisocytosis and worse survival in patients with various diseases and COVID‐19 remain elusive. In difference to other markers of inflammation, RDW seems to be strongly affected by chronic and acute comorbidities and not only by severity of COVID‐19 6 and its elevation might represent worse overall health status at the start of the SARS‐CoV‐2 infection. Integration of RDW into prognostic scores for COVID‐19 might greatly improve prognostication and should not be discarded in anemic patients since they in particular suffer from comorbidities.
AUTHOR CONTRIBUTIONS
All authors fulfilled ICMJE authorship criteria and agree to be accountable for all aspects of the work. Marko Lucijanic participated in the study design, data acquisition, statistical analysis, data interpretation, drafting of the manuscript, revising it critically for important content, and approved the final version. Ena Soric, Martina Sedinic Lacko, Anica Sabljic, Ivan Krecak, Petra Bistrovic, Ana Jordan, Sime Manola, Ozren Jaksic, Tomo Lucijanic, Lovorka Derek, and Rajko Kusec participated in data acquisition and interpretation, critically revising the manuscript for important content, and approved the final version.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
DATA AVAILABILITY STATEMENT
Data are available on reasonable request.
ETHICS STATEMENT
The study was approved by the University Hospital Dubrava Review Board.
ACKNOWLEDGMENTS
This paper is a part of the project “Registar hospitalno liječenih bolesnika u Respiracijskom centru KB Dubrava”/“Registry of hospitalized patients in University Hospital Dubrava Respiratory center.”
REFERENCES
- 1. Ćatić J, Jurin I, Lucijanić M, Jerkić H, Blažeković R. High red cell distribution width at the time of ST segment elevation myocardial infarction is better at predicting diastolic than systolic left ventricular dysfunction: a single‐center prospective cohort study. Medicine. 2018;97(18):e0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kust D, Lucijanic M, Urch K, et al. Clinical and prognostic significance of anisocytosis measured as a red cell distribution width in patients with colorectal cancer. QJM. 2017;110(6):361‐367. [DOI] [PubMed] [Google Scholar]
- 3. Lucijanic M, Krecak I, Verstovsek S, et al. Higher red blood cell distribution width predicts thrombosis risk in primary and secondary myelofibrosis. Ann Hematol . 2021. [DOI] [PubMed]
- 4. Lee JJ, Montazerin SM, Jamil A, et al. Association between red blood cell distribution width and mortality and severity among patients with COVID‐19: a systematic review and meta‐analysis. J Med Virol. 2021;93(4):2513‐2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rapp JL, Tremblay D, Alpert N, et al. Red cell distribution width is associated with mortality in non‐anemic patients with COVID‐19. J Med Virol. 2021;93(7):4130‐4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lucijanić M, Jordan A, Jurin I, et al. Red cell distribution width is a potent prognostic parameter for in‐hospital and post‐discharge mortality in hospitalized coronavirus disease 2019 patients: a registry‐based cohort study on 3941 patients. Croat Med J. 2022;63(1):44‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.


