Abstract
Background
Uninsured people who use drugs (PWUD) require extended parenteral antibiotic therapy when diagnosed with complex infections such as osteomyelitis. They are ineligible to enroll in our self-administered outpatient antimicrobial therapy (S-OPAT) program and instead sent to a skilled nursing facility (SNF). We aim to retrospectively assess clinical outcomes of PWUD discharged from our safety net hospital to complete OPAT in an SNF.
Methods
Using our hospital electronic medical record, PWUD discharged to an SNF for extended antibiotic therapy were identified for the study period, 1/1/17–4/30/18. Demographics, drug use, discharge diagnosis, antibiotic therapy, discharge disposition from SNF (AMA, early non-AMA, completed), 30-day emergency department (ED) utilization, and 30-day readmission were collected for the study cohort. ED utilization and 30-day readmission rates were analyzed by disposition group.
Results
While the majority of patients completed treatment (83), a sizeable number left AMA (26) or early non-AMA (20). Patients who left early, AMA or non-AMA, had increased rates of 30-day readmission or ED utilization (P=.01) and increased rates of 30-day readmission alone (P=.01), but not ED utilization alone (P=.43), compared with patients who completed treatment.
Conclusions
In our cohort, many PWUD discharged to an SNF to receive parenteral antibiotics did not complete treatment. These patients were observed to have increased health care utilization compared with patients completing therapy.
Keywords: drug use, OPAT
Substance use disorders (SUDs) are a costly public health problem that pose a significant challenge in planning for postacute care of hospitalized patients across the United States [1, 2]. While the opioid epidemic is a well-recognized crisis [3], geographic variations exist for substance use patterns, including increased frequency of methamphetamine and cocaine use among patients in the Southeast United States [4]. People who use drugs (PWUD) are often hospitalized with complicated infections requiring long courses of intravenous (IV) antimicrobial therapy. Outpatient parenteral antimicrobial therapy (OPAT) is an established transition-of-care model for medically stable patients to complete a planned treatment course in the outpatient setting [5]. PWUD and uninsured patients have limited options for OPAT. Stigmatization within the medical community is a well-studied barrier to health care for PWUD and is associated with worse clinical outcomes [6]. In regards to OPAT, biases within the medical community serve as major barriers for PWUD, specifically fear of nonadherence, concerns about patient and staff safety, and legality [7]. Further, there is a lack of guidance in the literature on OPAT use in PWUD [8].
Parkland Health and Hospital System (PHHS) is an 882-bed safety-net hospital serving a largely uninsured and underinsured patient population residing in Dallas, Texas. A self-administered OPAT (S-OPAT) program was developed in 2009 to address the needs of patients unable to access standard forms of OPAT due to lack of insurance coverage. Previously published data demonstrate the safety and efficacy of the program, including improved resource utilization, cost of care, and clinical outcomes [9]. PWUD with a history of active drug use within the past 12 months are currently ineligible to participate in S-OPAT at our institution. Historically, PWUD have been excluded due to concern for treatment adherence and adverse outcomes such as catheter misuse. Instead, they are required to finish their IV antibiotic course in the hospital or, more commonly, in a skilled nursing facility (SNF). These options burden both patients and health systems due to inconvenience and higher cost of care [10]. There is scant literature evaluating clinical outcomes, efficacy, and adverse events associated with OPAT in the SNF setting for PWUD. OPAT has been successfully used in at least 1 US health care system with a decrease in hospital length of stay (LOS) and health care cost in patients with opioid use disorder (OUD) and injection-related infections when addiction was concurrently treated with buprenorphine therapy [11]. Internationally, a Singaporean study found OPAT in patients with nonopioid and opioid injection drug use to be safe and effective, with decreased hospital LOS [12]. Further, patients leaving against medical advice (AMA) either fail to complete their antibiotic course or are switched to a less ideal oral regimen and have increased morbidity associated with inadequate treatment of an underlying infection.
While infections in PWUD that require long-term IV antibiotic therapy are frequently encountered in clinical practice, few studies have described clinical outcomes and health care utilizations for PWUD requiring long-term IV antibiotics. We retrospectively reviewed clinical outcomes for a cohort of PWUD discharged from our safety-net hospital to SNF for OPAT therapy.
METHODS
The electronic medical record was used to identify PWUD requiring extended courses of IV antibiotic therapy and discharged to an SNF between 1/1/17 and 4/30/18 from PHHS. Data were reviewed for demographics including age, gender, ethnicity, funding status, and specific drug use, including both intravenous and nonintravenous drugs. Data were collected for discharge diagnosis (ie, source of infection) as well as treatment plan, including antibiotic choice and duration of therapy. Measured outcomes include completion of planned treatment course, AMA discharge, ED utilization, and 30-day readmission rates. Clinical outcomes were compared between patients who completed treatment and those who left before the completion of treatment (non-AMA) or left AMA. Patients who left AMA were required to sign paperwork given their medical need for IV antibiotic therapy, while patients who left early were able to safely terminate their therapy early or switch to oral antibiotics as determined by their health care provider. ED utilization was calculated as total number of ED visits within 1 month of initial discharge from the hospital to SNF. The 30-day readmission rate was calculated as the total number of hospitalizations within 1 month of discharge from the hospital to an SNF. Demographic and outcome variables are summarized with percentages, means and standard deviations, and medians (interquartile ranges). The chi-square test was used to compare the 3 groups for categorical variables with Bonferroni correction for the pair-wise comparison. Each subscript letter denotes a subset of the 3 groups that do not differ significantly from each other at the .05 level. Analysis of variance and the Kruskal-Wallis rank-sum test were used to compare the continuous variables depending on data distribution. All statistical tests used .05 as the significance level.
Lastly, we estimated the cost of SNF stay (not including the antibiotic cost itself) for the entire cohort using the Department of Health and Human Services’ estimate of $225 per night. Our institution has existing contracts with local SNFs for uninsured patients who require prolonged time in a health care setting but do not meet criteria for an inpatient hospitalization. As such, patients were not personally responsible for the cost of an SNF stay.
Patient Consent
The study was approved by our Institutional Review Board with a waiver of consent given the retrospective, encrypted, and de-identified nature of the data collected.
RESULTS
A total of 129 PWUD were discharged to an SNF on extended courses of antibiotics for complicated infections (Table 1). More than one-third (n = 46; 35%) left before completing their treatment course (57% AMA and 43% non-AMA). Women were more likely to complete their treatment course compared with men (12.0% vs 41.3%; P<.01). There was no statistical difference in race/ethnicity and age between patients who completed their treatment course and those who did not. Cocaine use was observed to be more frequently reported among patients completing a prescribed treatment course. There was no difference in planned length of antibiotic course between each group (completed 28, AMA 31, non-AMA early discharge 32; P=.36). Patients discharged with AMA status completed an average of 3 days of antibiotic treatment. Patients with early discharge status from SNF (non-AMA) averaged 21 days of treatment compared with the average complete treatment course of 28 days. Of patients who discharged AMA or who were discharged early non-AMA, 43% received prescriptions for oral antibiotics (45% of non-AMA vs 42% of AMA). All patients who were discharged early (non-AMA) filled their oral antibiotic prescriptions, while 72% of those who left AMA filled their antibiotic prescriptions.
Table 1.
Demographic Variables
| AMA (n=26) | Non-AMA (n=20) | Treatment Complete (n=83) | P Value | |
|---|---|---|---|---|
| Female | 3 (12)a,b | 0 (0)b | 22 (27)a | .01 |
| Race/ethnicity | .22 | |||
| White non-Hispanic | 12 (46) | 12 (60) | 27 (33) | |
| Hispanic | 10 (39) | 6 (30) | 41 (49) | |
| Black non-Hispanic | 4 (15) | 2 (10) | 15 (18) | |
| Age, y | 41 ± 12 | 43 ± 8 | 45 ± 10 | .15 |
| Drug of choice | ||||
| Cocaine | 7 (27)a | 8 (40)a,b | 45 (54)b | .04 |
| Heroin | 9 (35) | 3 (15) | 26 (31) | .29 |
| Methamphetamines | 14 (54) | 10 (50) | 41 (49) | .46 |
| Phencyclidine | 2 (8) | 1 (5) | 1 (1) | .22 |
| Prescription drugs | 1 (4) | 2 (10) | 1 (1) | .12 |
| Discharge diagnosis | ||||
| Endocarditis | 7 (27) | 1 (5) | 8 (10) | .05 |
| Bacteremia | 6 (23) | 6 (30) | 31 (37) | .38 |
| Bone and joint | 13 (50) | 10 (50) | 35 (42) | .69 |
| Skin and soft tissue | 0 (0) | 0 (0) | 4 (5) | .32 |
| Diabetic foot infection | 5 (19) | 4 (20) | 14 (17) | .93 |
| Pulmonary | 0 (0) | 2 (10) | 5 (6) | .31 |
| GI/GU | 0 (0) | 0 (0) | 2 (2) | .57 |
| CNS/ENT | 0 (0) | 2 (10) | 4 (5) | .28 |
| Antibiotic at discharge | ||||
| Cephalosporin | 16 (62) | 8 (40) | 48 (58) | .29 |
| Vancomycin | 0 (0) | 10 (50) | 23 (28) | .16 |
| Carbapenem | 0 (0) | 1 (5) | 7 (8) | .29 |
| Penicillin | 2 (8) | 4 (20) | 12 (15) | .48 |
| Daptomycin | 0 (0) | 0 (0) | 1 (1) | .76 |
| Duration of planned antibiotic treatment, d | 31 (22–34) | 32 (18–35) | 28 (15–33) | .36 |
| Duration of actual antibiotic treatment, d | 3 (2–11) | 21 (9–31) | 28 (20–35) | <.01 |
Table 1 demonstrates demographic and clinical variables including drug of choice, final diagnosis, and details regarding antibiotic treatment and duration among people who use drugs discharged to short-term nursing facilities for extended courses of intravenous antibiotics (n=129). Data are presented as No. (%), median (IQR), or mean ± SD.
Abbreviations: AMA, against medical advice; CNS/ENT, Central Nervous System/Ear Nose and Throat; GI/GU, Gastroenterology/Genitourinary; IQR, interquartile range.
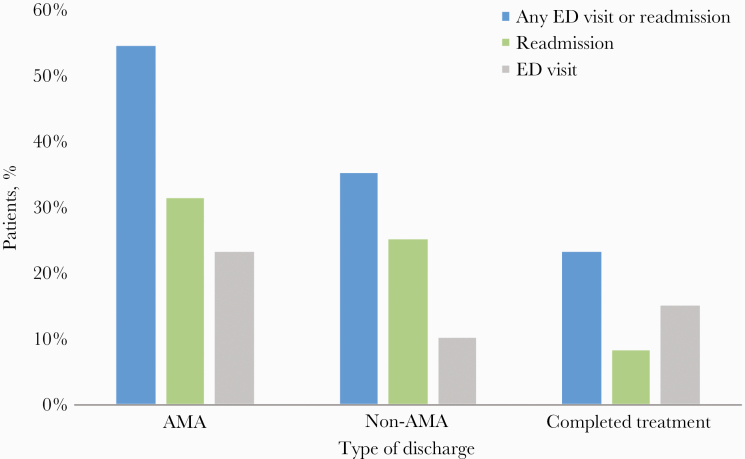
Patients who failed to complete a prescribed treatment course (AMA and non-AMA) were found to have a significantly higher inpatient readmission rate and combined ED visit/inpatient readmission rate (Table 2; Figure 1). Most of the ED visits (76.1%) and hospital readmissions (71.4%) were related to treatment failure of the original infection. However, patients who left AMA or left early (non-AMA) did not experience any difference in 30-day ED visits. Patients with reported injection drug use were found to have the same treatment completion rate as patients reporting noninjection drug use (Table 2). Estimated cumulative cost for SNF stay for the entire cohort was $692550.00. The estimated cost per patient was $5338.60 (Table 3).
Table 2.
Outcome Variables
| AMA (n=26), No. (%) | Non-AMA (n=20), No. (%) | Treatment Complete (n=83), No. (%) | P Value | |
|---|---|---|---|---|
| Any inpatient readmission or ED visits within 30 d | 14 (54) | 7 (35) | 19 (23) | .01 |
| Inpatient readmission within 30 da | 8 (31) | 5 (25) | 7 (8) | .01 |
| ED utilization within 30 db | 6 (23) | 2 (10) | 12 (15) | .43 |
| Injection drug use | 12 (46) | 4 (20) | 27 (33) | .17 |
| Noninjection drug use | 14 (54) | 16 (80) | 56 (67) |
Table 2 demonstrates the primary outcomes of health care resource utilization, defined as 30-day ED visits and 30-day hospital readmissions. There was a statistically significant increase in the composite hospital readmission or ED visit rates in the AMA and early non-AMA groups vs the treatment complete group (P=.01), as well as increased readmissions alone in the AMA and early non-AMA groups vs the treatment complete group (P=.01). There was no significant difference in ED visits alone (P=.43).
Abbreviations: AMA, against medical advice; ED, emergency department.
Readmission through ED counted as readmission.
ED visit only (no readmission).
Figure 1.
Discharge status vs complication rates. Patients who left AMA or early non-AMA were more likely than patients who completed treatment to have either an ED visit or hospital readmission (blue bars; 54%, 35%, 23%, respectively; P=.01) and readmission alone (green bars; 31%, 25%, 8%, respectively; P=.01), but not ED visit alone (gray bars; 23%, 10%, 15%, respectively; P=.41). Abbreviations: AMA, against medical advice; ED, emergency department.
Table 3.
Cost of SNF Stay
| Cumulative Cost | Cost per Patient |
|---|---|
| $692 550.00 | $5338.60 |
Table 3 demonstrates the estimated cost associated with SNF stay for all 129 patients, as estimated by the Department of Health estimation of $225 per night, not including medications or antibiotics.
Abbreviation: SNF, skilled nursing facility.
DISCUSSION
In this single-site retrospective review, we conduct the first study of clinical outcomes and health care cost for PWUD discharged from a safety net setting to SNF for OPAT. Over one-third of PWUD discharged to an SNF in our cohort failed to complete a planned IV antibiotic treatment course (Table 1). Among those patients with incomplete treatment, >50% were discharged AMA and experienced increased rates of health care utilization (Table 2). Finally, the cost of SNF stay for the average treatment course was exceedingly high: >$5000 per patient (Table 3), although our patients did not incur any charges themselves. Our findings show that the current system of postacute care with SNF-administered antibiotics for PWUD results in low rates of treatment completion and high rates of health care utilization and is expensive to the health care system.
Our findings argue for continued efforts to develop more effective care delivery models for PWUD to complete OPAT successfully. Data regarding OPAT in PWUD are limited but encouraging. Ho et al. performed a single-center prospective observational study in which they placed 29 people who inject drugs (PWID) on OPAT, with provisions of adequate housing, a reliable guardian, and signature of a contract. The authors reported no cases of central access use for nonprescription drug use and no change in readmission rates in the study population compared with patients without a history of drug use or concurrent IV drug use [12]. In a second study, Fanucchi et al. performed a pilot randomized trial in which 20 patients with opioid use disorder (OUD) were prescribed buprenorphine and randomized to complete an IV antibiotic course inpatient or via OPAT. Unsurprisingly, the OPAT group had decreased hospital LOS by 23 days. Interestingly, the 1 patient in the hospital group who was discharged AMA went on to complete their course of IV antibiotics via OPAT outside of the study [11]. Another study describes the use of a multidisciplinary group including the patient themselves to formulate unique, patient-centered solutions to long-term antibiotics for PWUD. Options for antibiotic treatment included IV, long-acting injectables or oral antibiotics. They discharged 40% home with antibiotics, and only 12% of patients left prematurely [13]. These findings demonstrate the safety and efficacy of OPAT among selected PWUD (ie, patients with both strong insight and social support), as well as decreased health care utilization in OPAT. However, in a third study, a single-center retrospective study of 118 patients, Buehrle et al. found OPAT failure (ie, readmission, nonadherence, missed appointments, treatment failure, etc.) in 61% of PWUD [14].
Taken with our findings, these studies suggest the importance of increasing provider and patient choice regarding the location of extended antibiotic administration and of a nuanced, patient-centered approach to determining OPAT candidates. Collaboration with Addiction Psychiatry to assist in patient identification, psychiatric clearance, and concurrent management of SUD is vital to patient success. For instance, a recent analysis established reduced 1-month mortality associated with prescriptions for medications for OUD among patients hospitalized for endocarditis [15]. Further, careful attention to the patient’s social determinants of health and barriers to care is crucial in developing a patient-centered approach.
Attention to gender and the societal barriers faced by women is also paramount to a patient-centered approach. Prior studies have shown that women who use drugs (WWUD) experience faster evolution from initial substance use to addiction, more psychiatric comorbidities, more functional impairment, and worse health outcomes compared with men [16, 17]. Of note, in our study, women were >3 times as likely to complete their treatment course as men (Table 1). While WWUD access treatment less frequently [18], they maintain equal success once in treatment [19]. Perhaps SNFs provided a stabilizing environment for women, as drug use is entangled with social instability, including intimate partner violence [20, 21], substance use with sexual partners, and lack of autonomy over substance use for WWUD [19]. However, WWUD often struggle to complete treatment outside the home due to lack of childcare and fear of losing custody of their children [21]. As OPAT programs for PWUD evolve, we must develop programming that incorporates the unique needs of WWUD.
Unique to our patient population was the widespread use of stimulants (cocaine and methamphetamines) compared with other published studies (Table 1). This finding reflects the epidemiology of drug use across the United States, with more stimulant use in the South and West compared with frequent opioid use in the North and East [22]. Interestingly, patients whose drug of choice was cocaine had a statistically significant difference in disposition, being more likely to complete treatment than not. For patients using other drugs, there was no statistically significant difference in disposition (Table 1). The cause behind this finding is likely multifactorial and influenced by the severity of addiction, which could not be measured in this study. In 1 study utilizing the Barratt Impulsiveness Scale to measure impulsiveness, cocaine use was associated with decreased baseline impulsiveness when compared with methamphetamine use [23]. The shorter half-life of cocaine (~90 minutes) vs methamphetamine (~11 hours) predisposes people who use cocaine to more significant binge use [24]. It is possible that the patients in our study using cocaine had decreased baseline impulsivity when not actively engaging in binge use (when compared with those who used the most similar drug, methamphetamine), making it easier for them to repel cravings and complete treatment without early discharge.
However, attributing early discharge to drug use alone is misguided and unfair to patients. Patients leave early, both AMA and non-AMA, for a variety of nonmedical and non–drug use reasons, including child care and familial obligations, paying bills, and employment [25, 26]. In our study, patients who left AMA left at an average of 3 out of a planned 31 days, while patients who discharged non-AMA left at an average of 21 out of a planned 32 days (Table 1). One possibility as to why the latter group left so late in the course is unpredictable life events requiring discharge, albeit with a modified oral antibiotic plan. The opportunity to complete OPAT at home provides patients with greater flexibility to address competing priorities and continue optimal treatment. The potential benefits of OPAT in this population are magnified at safety net hospitals such as ours, where minimizing length of stay and readmission improves resource utilization. Additionally, SNF-administered antibiotic therapy is expensive (Table 3), and safety net hospitals would also greatly benefit from the cost-savings associated with OPAT therapy [10].
The limitations of the current study include the design of an observational, single-site retrospective review. Our largely uninsured patient population with low socioeconomic status is also reflective of a safety net hospital system and not necessarily generalizable to other populations. Additionally, our hospital system uniquely pays for SNF placement for uninsured patients. The majority of patients in our cohort were male and Hispanic, and patterns of drug use varied within this population. Lastly, the distribution of drugs of choice in our population differs from other published studies with higher rates of methamphetamine and cocaine use compared with opioid use.
Our study highlights the need to improve and expand post–acute care options for patients with SUD who require extended IV antibiotic therapy. Innovative models of care that acknowledge the role of social determinants of health and addiction must be developed to address the multifaceted needs of this population with the goal of completing treatment, decreasing medical complications, and avoiding excess health care utilization. Future research efforts include analysis of larger cohorts of patients to identify specific risk factors associated with incomplete therapy and AMA discharge. Future program efforts include a collaborative pilot with Addiction Psychiatry to assist in selecting and supporting patients with SUD to safely and effectively complete OPAT in our home-based model with caregiver/family engagement.
Acknowledgements
The authors would like to acknowledge Dr. Monal Shah, Dr. Ank Nijhawan, and Norman Mang for their support of this project. The authors would also like to acknowledge the support of the Hirsch Foundation for the Parkland Center for Innovation and Value at Parkland.
Potential conflicts of interest. All authors listed on this manuscript do not report any conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Cartwright WS, Ingster LM.. A patient-based analysis of drug disorder diagnoses in the Medicare population. Health Care Financ Rev 1993; 15:89–101. [PMC free article] [PubMed] [Google Scholar]
- 2.Fox K, Merrill JC, Chang HH, Califano JA Jr. Estimating the costs of substance abuse to the Medicaid hospital care program. Am J Public Health 1995; 85:48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Florence CS, Zhou C, Luo F, Xu L.. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care 2016; 54:901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maxwell J.National Drug Early Warning System State of Texas sentinel community site drug use patterns and trends. 2018. Available at: https://ndews.org/wordpress/files/2020/07/SCS-Report-2018-Texas-FINAL.pdf. Accessed 8 November 2021. [Google Scholar]
- 5.Rich JD, Allen SA, Williams BA.. The need for higher standards in correctional healthcare to improve public health. J Gen Intern Med 2015; 30:503–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF.. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 2013; 131:23–35. [DOI] [PubMed] [Google Scholar]
- 7.Fanucchi L, Leedy N, Li J, Thornton AC.. Perceptions and practices of physicians regarding outpatient parenteral antibiotic therapy in persons who inject drugs. J Hosp Med 2016; 11:581–2. [DOI] [PubMed] [Google Scholar]
- 8.Tice AD, Rehm SJ, Dalovisio JR, et al. ; IDSA. Practice guidelines for outpatient parenteral antimicrobial therapy. IDSA guidelines. Clin Infect Dis 2004; 38:1651–72. [DOI] [PubMed] [Google Scholar]
- 9.Bhavan KP, Brown LS, Haley RW.. Self-administered outpatient antimicrobial infusion by uninsured patients discharged from a safety-net hospital: a propensity-score-balanced retrospective cohort study. PLoS Med 2015; 12:e1001922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chapman AL, Dixon S, Andrews D, et al. Clinical efficacy and cost-effectiveness of outpatient parenteral antibiotic therapy (OPAT): a UK perspective. J Antimicrob Chemother 2009; 64:1316–24. [DOI] [PubMed] [Google Scholar]
- 11.Fanucchi LC, Walsh SL, Thornton AC, et al. Outpatient parenteral antimicrobial therapy plus buprenorphine for opioid use disorder and severe injection-related infections. Clin Infect Dis 2020; 70:1226–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho J, Archuleta S, Sulaiman Z, Fisher D.. Safe and successful treatment of intravenous drug users with a peripherally inserted central catheter in an outpatient parenteral antibiotic treatment service. J Antimicrob Chemother 2010; 65:2641–4. [DOI] [PubMed] [Google Scholar]
- 13.Sikka MK, Gore S, Vega T, et al. “OPTIONS-DC”, a feasible discharge planning conference to expand infection treatment options for people with substance use disorder. BMC Infect Dis 2021; 21:772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buehrle DJ, Shields RK, Shah N, et al. Risk factors associated with outpatient parenteral antibiotic therapy program failure among intravenous drug users. Open Forum Infect Dis 2017; 4:XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kimmel SD, Walley AY, Li Y, et al. Association of treatment with medications for opioid use disorder with mortality after hospitalization for injection drug use-associated infective endocarditis. JAMA Netw Open 2020; 3:e2016228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Back SE, Payne RL, Wahlquist AH, et al. Comparative profiles of men and women with opioid dependence: results from a national multisite effectiveness trial. Am J Drug Alcohol Abuse 2011; 37:313–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hernandez-Avila CA, Rounsaville BJ, Kranzler HR.. Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend 2004; 74:265–72. [DOI] [PubMed] [Google Scholar]
- 18.Greenfield SF, Brooks AJ, Gordon SM, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend 2007; 86:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi S, Adams SM, Morse SA, MacMaster S.. Gender differences in treatment retention among individuals with co-occurring substance abuse and mental health disorders. Subst Use Misuse 2015; 50:653–63. [DOI] [PubMed] [Google Scholar]
- 20.Cohn A, Najavits LM.. Differences between U.S. substance abuse treatment facilities that do and do not offer domestic violence services. Psychiatr Serv 2014; 65:504–10. [DOI] [PubMed] [Google Scholar]
- 21.Cronholm PF, Fogarty CT, Ambuel B, Harrison SL.. Intimate partner violence. Am Fam Physician 2011; 83:1165–72. [PubMed] [Google Scholar]
- 22.2019 National Survey of Drug Use and Health (NSDUH) Releases. 2020. Available at: https://www.samhsa.gov/data/release/2019-national-survey-drug-use-and-health-nsduh-releases. Accessed 18 January 2021. [Google Scholar]
- 23.Winhusen T, Lewis D, Adinoff B, et al. Impulsivity is associated with treatment non-completion in cocaine- and methamphetamine-dependent patients but differs in nature as a function of stimulant-dependence diagnosis. J Subst Abuse Treat 2013; 44:541–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newton TF, De La Garza R 2nd, Kalechstein AD, Nestor L.. Cocaine and methamphetamine produce different patterns of subjective and cardiovascular effects. Pharmacol Biochem Behav 2005; 82:90–7. [DOI] [PubMed] [Google Scholar]
- 25.Arora R, Warrier I, Baptist AP.. Reasons why patients leave against medical advice (AMA) following an asthma hospitalization. J Allergy Clin Immunol 2007; 119:S285. [DOI] [PubMed] [Google Scholar]
- 26.Onukwugha E, Saunders E, Mullins CD, et al. Reasons for discharges against medical advice: a qualitative study. Qual Saf Health Care 2010; 19:420–4. [DOI] [PMC free article] [PubMed] [Google Scholar]