Abstract
Background
Itraconazole (ITZ) is an effective agent when used as primary invasive fungal disease (IFD) prophylaxis, but is limited by drug tolerability and variability in serum concentrations. A new formulation, SUBA-itraconazole (for “super bioavailability”; S-ITZ), addresses the limitations of conventional ITZ formulations.
Methods
We conducted a retrospective cohort study at 2 Australian centers to evaluate the safety, tolerability, and effectiveness of S-ITZ as primary antifungal prophylaxis in hematopoietic cell transplant (HCT) recipients without grade II–IV acute graft-vs-host disease, from day 1 until approximately day 100 (cohort A) or day 1 until neutrophil engraftment (cohort B). A total of 204 patients and 1410 trough plasma ITZ concentrations were assessed.
Results
The incidence of breakthrough proven/probable IFD at day 180 was 1.0% (95% confidence interval [CI], .2%–3.2%), with 1.6% in cohort A and 0% in cohort B, and overall fungal-free survival of proven/probable IFD was 82.9% (95% CI, 76.8%–87.4%). Preengraftment early permanent S-ITZ discontinuation was 3.4% overall, with no significant difference between cohorts. No patients required cessation due to gastrointestinal intolerance attributed to S-ITZ. The geometric mean trough plasma ITZ concentration was 1130ng/mL (interquartile range, 566–1801ng/mL; coefficient of variation, 56.57%) and the median time to achieve therapeutic levels was 10 days.
Conclusions
S-ITZ is a safe and well-tolerated oral formulation and is a novel alternative for primary IFD prophylaxis after HCT.
Keywords: allogeneic hematopoietic cell transplantation, antifungal prophylaxis, itraconazole, HCT, S-ITZ, SUBA, itraconazole
New formulation SUBA-itraconazole (S-ITZ) addresses the conventional formulations limitations of intolerability and variability in absorption. The incidence of breakthrough proven/probable invasive fungal disease at day 180 was 1.0%; no patients required cessation due to gastrointestinal intolerance attributed to S-ITZ.
Invasive fungal disease (IFD) in allogeneic hematopoietic cell transplant (HCT) recipients is associated with significant morbidity, mortality, and health care costs [1, 2]. Antifungal prophylaxis is known to prevent IFD in HCT, although the threshold for prophylaxis and agents of choice continue to evolve with progress in HCT and development of new antifungal agents and formulations [3–6]. There is no clear advantage between IFD prophylaxis agents that are routinely used in HCT in the absence of graft-vs-host disease (GVHD), particularly in regard to all-cause mortality [7]. Itraconazole (ITZ) has been demonstrated to be an effective primary prophylactic agent post-HCT in preventing the incidence of IFD in randomized controlled trials; however, because of consistent issues with gastrointestinal (GI) intolerance and compromised bioavailability, conventional ITZ has fallen out of favor in many HCT centers for newer triazoles such as voriconazole, posaconazole, and isavuconazole [8–12].
To address the limited bioavailability of, and intolerance to, conventional ITZ formulations, a novel formulation, SUBA (“super bioavailability”) itraconazole (S-ITZ), was recently licensed by the Food and Drug Administration in the United States and the Therapeutic Goods Administration in Australia, but as yet, not the European Medicines Agency [13, 14]. S-ITZ is a formulation containing a solid dispersion of ITZ in a pH-dependent polymeric matrix to enhance intestinal absorption, therefore increasing bioavailability [15, 16]. The first study using this novel formulation for fungal prophylaxis compared conventional ITZ oral solution in patients undergoing HCT; [17] the S-ITZ capsule formulation was associated with more rapid attainment of therapeutic ITZ levels with less interpatient variability or GI intolerance, using the same initial dosage as the oral solution of 200mg twice a day. However, the small sample size (n=27) limited the study’s findings, particularly the rate of IFD. In this multisite longitudinal cohort study, we report the use of S-ITZ prophylaxis after HCT in Australia.
METHODS
Study Design and Participants
This was a retrospective longitudinal cohort study of S-ITZ used as primary antifungal prophylaxis in HCT recipients at Royal North Shore Hospital (cohort A) and Royal Prince Alfred Hospital (cohort B) in Sydney, Australia, from June 2015 to January 2020. All consecutive patients undergoing HCT, without a documented prior IFD, were administered S-ITZ as primary antifungal prophylaxis. Patients were excluded if they had received secondary prophylaxis for a prior IFD, or if they were administered <5 uninterrupted days of S-ITZ. All patients were followed until death or at least 180 days post-HCT. Institutional databases were accessed, with a full chart review of each patient for details of antifungal prophylaxis, incidence of proven/probable and possible IFD according to the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the Mycoses Study Group Education and Research Consortium (EORTC/MSG ERC) definitions, or a suspected IFD by the treating clinician that did not meet EORTC/MSG ERC criteria for possible or proven/probable IFD [18], as well as HCT characteristics.
Primary Antifungal Prophylaxis and HCT Policies
S-ITZ was administered from day 1 of HCT except in haploidentical HCT where it was administered from day 5 due to a potential cytochrome P450 interaction with posttransplant cyclophosphamide. The initial dose was 200mg twice a day (BID, every 12 hours) in both cohorts [19]. In cohort A, S-ITZ was administered as primary prophylaxis until weaning of immunosuppression at approximately day 100. In cohort B, S-ITZ was administered as primary prophylaxis only until neutrophil engraftment (Figure 1). In both cohorts, in the event of grade II–IV acute GVHD (aGVHD; defined by a modified Glucksberg criteria [20]), prophylaxis was switched to posaconazole as per national guidelines and continued for a duration specified by the treating physician [19]. Trough plasma ITZ concentrations were measured twice weekly aiming for a therapeutic range between 500 and 2000ng/mL [21]. Hydroxyitraconazole levels were not measured as routine clinical practice and therefore were not reported. If trough ITZ concentrations were >2000ng/mL, the dose was reduced by 50mg/dose every week until steady-state concentrations returned to <2000ng/mL; doses were not increased for subtherapeutic levels. If the patient was unable to tolerate any oral medication (nil by mouth), or the trough itraconazole level was <500ng/mL after approximately 14 days of therapy, either intravenous (IV) posaconazole 300mg daily (cohort A) or IV itraconazole 200mg daily (cohort B) was given until the patient was able to take oral medication, at which point S-ITZ was restarted. Standard conditioning regimens were fludarabine-melphalan, fludarabine-busulfan, busulfan/cyclophosphamide, or cyclophosphamide/total body irradiation; standard GVHD prophylaxis consisted of cyclosporin and methotrexate, and all unrelated donors received thymoglobulin 4.5mg/kg.
Figure 1.
Study outline. If grade II–IV acute graft-vs-host disease was diagnosed at any timepoint, intravenous or oral posaconazole was initiated and the patient was censored at that timepoint for primary endpoint (SUBA-itraconazole [S-ITZ] breakthrough invasive fungal disease [IFD]); overall IFD, fungal-free survival, nonrelapse mortality, and overall survival continued to be measured for the entire cohorts. A minimum of 5 days of uninterrupted S-ITZ must have been given to meet inclusion criteria. *Initiated day 5 after posttransplant cyclophosphamide in haploidentical hematopoietic cell transplant. Abbreviations: GVHD, graft-vs-host disease; IFD, invasive fungal disease; IV-ITZ, intravenous itraconazole; NBM, nil by mouth; S-ITZ, SUBA-itraconazole.
Safety and Tolerability
Microbiologic assessment, radiologic procedures, and other investigations such as Aspergillus galactomannan and Aspergillus polymerase chain reaction were undertaken throughout the study period as part of standard clinical practice only if prompted by fever not responding to empirical antibacterial therapy or for clinical suspicion of infection. Routine liver function tests were performed at least weekly and used to assess for drug-attributable hepatotoxicity. Moderate to severe liver injury defined as Drug-Induced Liver Injury Network (DILIN) grade 3+ liver injury [22] that was potentially attributable to S-ITZ required initiation of an alternative antifungal. Routine electrocardiography measurements were performed at the discretion of the treating clinician.
Study Endpoints
The primary endpoint was the incidence of breakthrough proven/probable IFD (bIFD) during administration or within 7 days of cessation of S-ITZ. Secondary endpoints included (1) the incidence of overall proven/probable IFD; (2) survival analyses including fungal-free survival (FFS; alive and free from proven/probable IFD), IFD attributable mortality, overall survival, and progression-free survival of malignant disease at 180 days post-HCT; and (3) early permanent S-ITZ discontinuation and/or initiation of alternative antifungal agent due to any reason, classified as a proven/probable IFD, a possible/suspected IFD, failure to achieve therapeutic serum concentrations after 14 days of therapy, an adverse drug reaction attributed to S-ITZ or intolerance to S-ITZ, or any other reason (Figure 1). Analysis of therapeutic drug levels were also performed, including the probability over time of attaining therapeutic ITZ serum concentrations defined as >500ng/mL [21] and steady-state trough ITZ serum concentrations, which was defined by 14 days of uninterrupted therapy.
Endpoints were assessed over the preengraftment period from day 0 (day of stem cell infusion) until neutrophil recovery (>0.5×109/L absolute neutrophil count for 3 consecutive days) at the “engraftment assessment point,” then through the postengraftment period until approximately day 180, at the “final assessment point” (Figure 1).
Statistical Analyses
Endpoints were assessed from day 0 of HCT until day 180 posttransplant. Cumulative incidence functions were used for bIFD, the early permanent S-ITZ discontinuation and/or initiation of alternative antifungal agent, and attainment of therapeutic drug levels, with death as a competing risk for all analyses and grade II–IV aGVHD as a competing risk for bIFD and S-ITZ discontinuation; relapse and nonrelapse mortality were competing risks for each other. The association of outcomes with pre- and posttransplant factors were analyzed using Fine-Gray competing risk regression [23]. Survival analyses were calculated using Kaplan-Meier and Fine-Gray proportional hazard regression analysis and groups compared with the log-rank test, with the impact of pretransplant factors and GVHD as a time-dependent posttransplant factor analyzed with Cox regression. Factors with a P value of<.10 on univariable analysis were included into multivariable models. Descriptive statistics were used for therapeutic drug levels of ITZ trough serum concentrations. As the maximum quantifiable ITZ level reported was 2000ng/mL, any level >2000ng/mL was considered 2000ng/mL for the geometric mean. Statistical analyses were performed using R statistical software version 3.5.2 (R Core Development Team, Vienna, Austria) and EZR [24].
Patient Consent Statement
Institutional Human Ethics Committee approval was obtained with a patient waiver of consent (HREC/50095/PMCC-2019).
RESULTS
Demographics and Characteristics of S-ITZ Administration
A total of 204 patients met the inclusion criteria for study, 129 in cohort A, of which 27 have been previously described in a pilot study, [17] and 75 in cohort B, of which 6 were previously described [25]. Three additional patients were initiated on S-ITZ but did not meet inclusion criteria as they received <5 days of uninterrupted therapy. The median total days of S-ITZ therapy was 103 days (IQR, 58–133 days) in cohort A and 18 days (IQR, 13–21 days) in cohort B. Patient demographics and post-HCT parameters are shown in Table 1.
Table 1.
Cohort Demographics
| Characteristic | Overall
(N = 204) |
Cohort A
(n = 129) |
Cohort B
(n = 75) |
P Value |
|---|---|---|---|---|
| Age, y, mean (SD) | 51.13 (13.83) | 53.70 (12.65) | 46.72 (14.71) | <.001 |
| Sex | ||||
| Female | 85 (41.7) | 55 (42.6) | 30 (40.0) | .769 |
| Male | 119 (58.3) | 74 (57.4) | 45 (60.0) | |
| Primary disease | ||||
| Acute myeloid leukemia | 85 (41.7) | 57 (44.2) | 28 (37.3) | .152 |
| Myelodysplastic syndrome | 33 (16.2) | 22 (17.1) | 11 (14.7) | |
| Acute lymphocytic leukemia | 14 (6.9) | 7 (5.4) | 7 (9.3) | |
| Non-Hodgkin lymphoma | 39 (19.1) | 21 (16.3) | 18 (24.0) | |
| Multiple myeloma | 7 (3.4) | 3 (2.3) | 4 (5.3) | |
| Aplastic anemia | 3 (1.5) | 0 (0.0) | 3 (4.0) | |
| Solid organ malignancy | 1 (0.5) | 0 (0.0) | 1 (1.3) | |
| Other | 22 (10.8) | 19 (14.7) | 3 (4.0) | |
| HCT conditioning | ||||
| Myeloablative | 70 (34.3) | 28 (21.7) | 42 (56.0) | <.001 |
| Reduced intensity | 134 (65.7) | 101 (78.3) | 33 (44.0) | |
| HCT source | ||||
| Matched related donor | 67 (32.8) | 40 (31.0) | 27 (36.0) | <.001 |
| Unrelated donor | 118 (57.8) | 87 (67.4) | 31 (41.3) | |
| Haploidentical | 16 (7.8) | 2 (1.6) | 14 (18.7) | |
| Cord | 3 (1.5) | 0 (0.0) | 3 (4.0) | |
| Unrelated donor HLA mismatch | ||||
| No (matched) | 72 (61.0) | 47 (54.0) | 25 (80.6) | .010 |
| Yes (mismatched) | 46 (39.0) | 40 (46.0) | 6 (19.4) | |
| Antithymocyte globulin | ||||
| No | 94 (46.1) | 48 (37.2) | 46 (61.3) | .001 |
| Yes | 110 (53.9) | 81 (62.8) | 29 (38.7) | |
| Post-HCT parameters | ||||
| Median days to engraftment | 17 | 17 | 17 | .796 |
| Engraftment failure >30 d | 2 (1.0) | 0 | 2 (2.7) | NA |
| Relapse at day 180, % (95% CI) | 14.5 (10.0–19.7) | 13.4 (8.1–19.9) | 16.4 (8.9–25.8) | .299 |
| Grade II–IV aGVHD at day 100, % (95% CI) | 22.6 (17.1–28.5) | 17.8 (11.8–24.9) | 30.7 (20.6–41.4) | .02 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: aGVHD, acute graft-vs-host disease; CI, confidence interval; HCT, hematopoietic cell transplant; NA, not applicable; SD, standard deviation.
Incidence of IFD and FFS
The overall incidence of bIFD among patients receiving S-ITZ at day 180 posttransplant was 1.0% (95% confidence interval [CI], .2%–3.2%), with 1.6% (95% CI, .3%–5.0%) in cohort A and 0% in cohort B (P=.281) (Table 2 and Figure 2A and 2B).
Table 2.
Cumulative Incidence of Breakthrough Invasive Fungal Disease (IFD), Fungal-Free Survival, Proven/Probable IFD, and Proven/Probable IFD Combined With Possible/Suspected IFD at 180 Days
| Cohort | No. | Survival Rate/Cumulative Incidence, % (95% CI) | P Value |
|---|---|---|---|
| Breakthrough proven/probable IFD with competing risk of death | |||
| Total | 204 | 1.0 (.2–3.4) | |
| Cohort A | 129 | 1.6 (.3–5.1) | .306 |
| Cohort B | 75 | 0 | |
| Fungal-free survival (proven/probable) | |||
| Total | 204 | 83.1 (77.2–87.7) | |
| Cohort A | 129 | 85.2 (77.7–90.3) | .057 |
| Cohort B | 75 | 79.7 (68.6–87.2) | |
| Proven/probable IFD with competing risk of death | |||
| Total | 204 | 3.0 (1.2–6.0) | |
| Cohort A | 129 | 1.6 (.3–5.0) | .124 |
| Cohort B | 75 | 5.5 (1.7–12.4) | |
| Proven/probable IFD with competing risk of death and GVHD | |||
| Total | 204 | 2.0 (.7–4.7) | |
| Cohort A | 129 | 1.6 (.3–5.0) | .563 |
| Cohort B | 75 | 2.9 (.5–9.0) | |
| Proven/probable IFD combined with possible/suspected IFD with competing risk of death | |||
| Total | 204 | 5.4 (2.9–9.2) | |
| Cohort A | 129 | 1.6 (.3–5.0) | .002 |
| Cohort B | 75 | 12.2 (6.0–20.9) | |
| Proven/probable IFD combined with possible/suspected IFD with competing risk of death and GVHD | |||
| Total | 204 | 3.5 (1.5–6.7) | |
| Cohort A | 129 | 1.6 (.3–5.0) | .053 |
| Cohort B | 75 | 6.8 (2.5–14.2) |
Abbreviations: CI, confidence interval; GVHD, graft-vs-host disease; IFD, invasive fungal disease.
Figure 2.
Breakthrough proven/probable invasive fungal disease for total patients (A) and by cohort (B). Abbreviations: HCT, hematopoietic cell transplant; IFD, invasive fungal disease.
The overall incidence of proven/probable IFD was 3.0% (95% CI, 1.2%–6.1%) with no significant difference between cohorts A and B at 1.6% and 5.8%, respectively (P=.111). However, the overall incidence of proven/probable IFD combined with possible/suspected IFD was 5.4% (95% CI, 2.9%–9.2%), with a significantly higher rate in cohort B (12.2% [95% CI, 6.0%–20.9%]) compared to cohort A (1.6% [95% CI, .3%–5.0%]) (P=.002). When excluding patients who developed grade II–IV aGVHD, the overall incidence of proven/probable IFD was 2.0% (95% CI, .7%–4.7%) with no significant difference between cohorts A and B, at 1.6% and 3.0%, respectively (P=.551); and the incidence of proven/probable IFD combined with possible/suspected IFD was 3.5% (95% CI, 1.5%–6.7%) with a non–statistically significant trend between cohorts at 1.6% and 6.8%, respectively, (P=.053). On univariable analysis, only age was a risk factor for proven/probable IFD (Table 3).
Table 3.
Univariable Analysis of Risk Factors for Proven/Probable Invasive Fungal Disease
| Variable | Univariable Analysis | |||
|---|---|---|---|---|
| HR | Lower 95% CI | Upper 95% CI | P Value | |
| Age | 1.085 | 1.034 | 1.138 | .001 |
| Antithymocyte globulin | 1.72 | .3181 | 9.3 | .529 |
| Cohort B (vs A) | 3.629 | .648 | 20.33 | .143 |
| Male sex (vs female) | 1.414 | .26 | 7.686 | .689 |
| Conditioning: RIC (vs MAT) | 1.041 | .1921 | 5.643 | .963 |
| Donor source (vs MRD) | ||||
| Unrelated donor | 1.135 | .2104 | 6.123 | .883 |
| Haploidentical | 0 | NA | NA | NA |
| Cord | 0 | NA | NA | NA |
| Mismatch (vs matched) | 0.63 | .0727 | 5.459 | .675 |
| Primary disease (vs lymphoma) | ||||
| AML/MDS | 1.533 | .1732 | 13.57 | .701 |
| ALL | 0 | NA | NA | NA |
| Other | 1.783 | .1125 | 28.27 | .6816 |
| Grade II–IV aGVHD (time dependent) | 1.164 | .1249 | 10.84 | .8942 |
Abbreviations: aGVHD, acute graft-vs-host disease; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; CI, confidence interval; HR, hazard ratio; MAT, myeloablative conditioning; MDS, myelodysplastic syndrome; MRD, matched related donor; NA, not applicable; RIC, reduced intensity conditioning.
FFS at day 180 was 82.9% (95% CI 76.8%–87.4%), with no significant difference between cohorts A and B at 85.2% and 78.6%, respectively (P=.139). On univariable and multivariable analysis, only the incidence of grade II–IV aGVHD was significantly associated with poorer FFS (Table 4; and Figure 3A and 3B).
Table 4.
Univariable and Multivariable Analysis of Risk Factors for Fungal-Free Survival (Alive Without Proven/Probable Invasive Fungal Disease)
| Variable | Univariable | Multivariable | ||||||
|---|---|---|---|---|---|---|---|---|
| HR | Lower 95% CI | Upper 95% CI | P Value | HR | Lower 95% CI | Upper 95% CI | P Value | |
| Age | 1.013 | .993 | 1.033 | .213 | … | … | … | |
| Antithymocyte globulin | 1.386 | .826 | 2.327 | .217 | … | … | … | |
| Cohort B (vs A) | 1.630 | .981 | 2.708 | .060 | 1.520 | .868 | 2.663 | .143 |
| Male sex (vs female) | 0.978 | .585 | 1.634 | .932 | … | … | … | |
| Conditioning: RIC (vs MAT) | 1.189 | .689 | 2.050 | .534 | … | … | … | |
| Donor source (vs MRD) | ||||||||
| Unrelated donor | 1.721 | .946 | 3.132 | .075 | 1.669 | .912 | 3.052 | .097 |
| Haploidentical | 1.589 | .577 | 4.378 | .370 | 1.558 | .539 | 4.509 | .413 |
| Cord | 2.416 | .317 | 18.390 | .394 | 1.954 | .248 | 15.380 | .525 |
| Mismatch (vs matched) | 1.154 | .630 | 2.113 | .643 | … | … | … | |
| Primary disease (vs lymphoma) | ||||||||
| AML/MDS | 1.596 | .768 | 3.315 | .210 | 1.567 | .745 | 3.297 | .236 |
| ALL | 1.666 | .511 | 5.425 | .397 | 1.497 | .455 | 4.923 | .507 |
| Other | 2.148 | .890 | 5.185 | .089 | 2.275 | .924 | 5.601 | .074 |
| Grade II–IV GVHD (time dependent) | 2.291 | 1.336 | 3.929 | .003 | 2.035 | 1.155 | 3.587 | .014 |
Outcome events: death or proven/probable invasive fungal disease.
Abbreviations: ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; CI, confidence interval; GVHD, acute graft-vs-host disease; HR, hazard ratio; MAT, myeloablative conditioning; MDS, myelodysplastic syndrome; MRD, matched related donor; RIC, reduced intensity conditioning.
Figure 3.
Fungal-free survival for total patients (A) and by cohort (B). Abbreviation: HCT, hematopoietic cell transplant.
Characteristics of IFD
There were 2 (2/204) bIFDs, both Nakaseomyces glabrata (Candida glabrata) fungemia and both in cohort A. The first bIFD was identified on day 12, with an ITZ trough serum concentration of 1607ng/mL on day 13; antifungal sensitivities were not available for the isolate. The second bIFD was identified on day 15, after the patient achieved a ITZ trough serum concentration of 256ng/mL on day 5, then was changed to IV posaconazole on day 12 due to nil by mouth; minimum inhibitory concentrations (MICs) of the isolate were 8.0mg/L for ITZ and 2.0mg/L for posaconazole. Both patients were successfully treated with anidulafungin (MIC = 0.060mg/L for the second case). Four (4/202) other proven/probable IFDs were identified overall, all in cohort B after routine cessation of S-ITZ (postengraftment). These included 2 further N glabrata fungemias on day 90 post-HCT in remission and day 140 post-HCT after acute myeloid leukemia relapse, as well as 2 probable invasive pulmonary aspergilloses, identified on computed tomography, with positive galactomannan on bronchoalveolar lavage on days 69 and 82 post-HCT; 1 was in the context of grade II–IV aGVHD. No deaths were attributable to IFD.
Overall Survival, Progression-Free Survival, and Incidence of GVHD
The overall survival was 89.7% (95% CI, 84.6%–93.2%) at day 100, 84.6% (95% CI, 78.9%–88.9%) at day 180, and 74.9% (95% CI, 67.9%–80.6%) at 1 year. At day 180, cohorts A and B had similar rates of overall survival (85.2% vs 83.8%, P=.187), progression-free survival (76.5% vs 71.5%, P=.141), and nonrelapse mortality (10.1% vs 12.1%, P=.464). The incidence of grade II–IV aGVHD was 18.1% (95% CI, 13.2%–23.7%) at day 50 and 22.6% (95% CI, 17.1%–28.5%) at day 100, with a lower rate reported in cohort A compared to cohort B (14.0% vs 25.3% at day 50 and 17.8% vs 30.7% at day 100; P=.018).
Early Permanent Discontinuation of S-ITZ and/or Initiation of Alternative Antifungal Agent
Preengraftment early permanent S-ITZ discontinuation and initiation of an alternative antifungal agent in the absence of grade II–IV aGVHD was 3.4% (7/204; 95% CI, 1.5%–6.6%) overall, with no significant difference between cohorts (Table 5 and Figure 4A). Reasons for overall preengraftment S-ITZ discontinuations are shown in Table 6.
Table 5.
Overall Early Permanent SUBA-Itraconazole Discontinuation and/or Initiation of Alternative Antifungal Agent for Any Reason in the Absence of Graft-vs-Host Disease
| Cohort | No. | Cumulative Incidence, % (95% CI) | P Value |
|---|---|---|---|
| Preengraftmenta | |||
| Total | 204 | 3.4 (1.5–6.6) | |
| Cohort A | 129 | 3.1 (1.0–7.2) | .750 |
| Cohort B | 75 | 4.0 (1.1–10.3) | |
| Postengraftmentb | |||
| Total | 197 | 2.5 (1.0–5.5) | |
| Cohort A | 125 | 0.8 (.1–4.0) | .016 |
| Cohort B | 72 | 7.1 (2.6–14.6) |
Abbreviation: CI, confidence interval.
Early permanent SUBA-itraconazole discontinuation and initiation of alternative antifungal.
Early permanent SUBA-itraconazole discontinuation and initiation of alternative antifungal in cohort A and initiation of an antifungal agent in cohort B.
Figure 4.
A, Preengraftment, early permanent SUBA-itraconazole (S-ITZ) discontinuation and initiation of alternative antifungal agent for any reason by cohort. B, Postengraftment, early permanent S-ITZ discontinuation, and initiation of alternative antifungal agent (cohort A) or initiation of an antifungal agent (cohort B). Abbreviation: HCT, hematopoietic cell transplant.
Table 6.
Early Permanent SUBA-Itraconazole Discontinuation and/or Initiation of Alternative Antifungal Agent for Any Reason in the Absence of Graft-vs-Host Disease by Numbers of Patients
| Cohort | Preengraftmenta | Postengraftmentb |
|---|---|---|
| Total | 204 | 197 |
| Cohort A | 129 | 125 |
| Cohort B | 75 | 72 |
| Proven/probable IFD | ||
| Total | 2 (1.0) | 3 (1.5) |
| Cohort A | 2 (1.6) | 0 |
| Cohort B | 0 | 3 (2.4) |
| Possible/suspected IFD | ||
| Total | 2 (1.0) | 3 (1.5) |
| Cohort A | 0 | 1 (0.8) |
| Cohort B | 2 (2.7) | 2 (2.8) |
| Failure to achieve therapeutic serum ITZ concentrations after 14 d of therapy | ||
| Total | 1 (0.5) | 0 |
| Cohort A | 1 (0.8) | 0 |
| Cohort B | 0 | NA |
| Adverse drug reactions attributed to S-ITZ | ||
| Total | 1 (0.5) | 0 |
| Cohort A | 0 | 0 |
| Cohort B | 1 (1.3) | NA |
| Intolerance to S-ITZ | ||
| Total | 0 | 0 |
| Cohort A | 0 | 0 |
| Cohort B | 0 | NA |
| Any other reason | ||
| Total | 1 (0.5) | 0 |
| Cohort A | 1 (0.8) | 0 |
| Cohort B | 0 | NA |
Data are presented as No. (%).
Abbreviations: IFD, invasive fungal disease; ITZ, itraconazole; NA, not applicable; S-ITZ, SUBA-itraconazole.
Early permanent S-ITZ discontinuation and initiation of alternative antifungal.
Early permanent S-ITZ discontinuation and initiation of alternative antifungal in cohort A and initiation of an antifungal agent in cohort B.
Postengraftment early permanent S-ITZ discontinuation and/or the initiation of an alternative antifungal agent in the absence of grade II–IV aGVHD was 2.5% (6/197; 95% CI, 1.0%–5.5%) overall. In cohort A, where S-ITZ was used as primary prophylaxis until weaning of immunosuppression (~day 100), an alternative antifungal agent was initiated in 0.8% (1/125; 95% CI, .1%–4.0%) of patients. In cohort B, where no routine primary prophylaxis after engraftment was used, 7.1% (5/72; 95% CI, 2.6%–14.6%) of patients were initiated on an antifungal agent (P=.016) (Tables 5 and 6 and Figure 4B).
Safety and Tolerability
One patient (0.5%) developed DILIN grade 3+ liver injury potentially attributable to S-ITZ, no patients were reported having a prolonged QTc, and no patients required cessation due to GI intolerance attributed to S-ITZ.
Sixty-four patients (31%) required temporary substitution of an IV alternative antifungal as per institutional policy—22.4% (29/129) in cohort A to IV posaconazole, and 46.7% (35/75) in cohort B to IV itraconazole. The most common reason for temporary substitution was nil by mouth due to mucositis (92.2%), followed by nil by mouth due to any other reason (6.3%), liver dysfunction not attributed to S-ITZ (1.6%), or omitted in error (1.6%). The median day post-HCT for substitution was day 8 (range, 1–39). In cohort A, 82.7% (24/29) of patients restarted S-ITZ, with the remaining patients developing aGVHD and remaining on posaconazole. In cohort B, 40.0% (14/35) patients restarted S-ITZ; the remaining patients were discharged postengraftment without an antifungal or developed aGVHD and were changed to posaconazole as per policy. The median duration of substitution was 11 days (range, 5–25 days). The median day post-HCT for cohort B to cease S-ITZ on engraftment as per policy was 18 (range, 10–47).
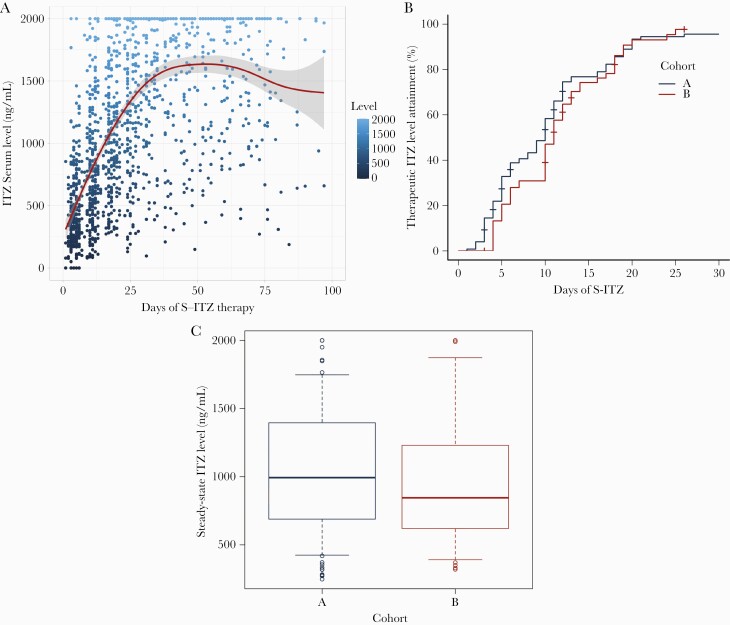
Therapeutic Drug Levels of S-ITZ
A total of 1410 trough plasma ITZ concentrations from 193 (94.6%) patients are shown in Figure 5A. The geometric mean trough plasma concentration was 1130ng/mL (IQR, 566–1801ng/mL; coefficient of variation [CV], 56.57%). Therapeutic ITZ level attainment is shown in Figure 5B; the median time to achieve therapeutic levels was 10 days (95% CI, 10–11 days), with no significant difference between cohorts (P=.27). By day 14 and day 21 of S-ITZ therapy, 75.8% (95% CI, 69.0%–82.0%) and 94.0% (95% CI, 89.3%–97.1%) of patients achieved therapeutic levels. Overall, the geometric mean of first ITZ trough concentration after steady state was 1037ng/mL (range 248–2000ng/mL; IQR, 651–1370ng/mL; CV, 56.71%) and there was no significant difference between cohorts (Figure 5C).
Figure 5.
SUBA-itraconazole (S-ITZ) levels among study cohorts. A, Total S-ITZ levels with mean and 95% confidence interval indicated (n=1414). B, Proportion of patients to attain therapeutic itraconazole (ITZ) levels (defined by >500ng/mL; cohort A, n=124; cohort B, n=69). C, Steady-state levels (defined by first level taken >14 days of S-ITZ; cohort A, n=99; cohort B, n=33).
A total of 119 patients in cohort A continued S-ITZ postengraftment without clinical failure. To maintain a therapeutic ITZ level between 1000 and 2000ng/mL, 68 of these patients (57.1%) maintained a dose of 200mg BID, 35 patients (29.4%) required a dose adjustment to 150mg BID (median day post-HCT, 41 [range, 7–78]), and 15 of 32 patients required a further dose adjustment to 100mg BID (median day post-HCT, 61 [range, 12–105]); the remaining 16 patients (13.4%) developed grade II–IV aGVHD and were changed to posaconazole.
DISCUSSION
In this multisite longitudinal cohort study, S-ITZ as primary IFD prophylaxis after HCT appeared effective and well tolerated, with low levels of bIFD or early discontinuations due to GI intolerability or adverse effects.
ITZ is well described as an effective primary IFD prophylaxis choice post-HCT; however, routine use has been limited by GI tolerability and variation in absorption and therefore has fallen out of favor in many HCT centers [10, 11, 26, 27]. In 2004, Marr et al demonstrated that ITZ oral solution 2.5mg/kg 3 times daily showed no survival advantage over fluconazole despite being more effective in preventing molds in HCT recipients; however, 36% of patients were discontinued from ITZ because of toxicities or GI intolerance and approximately 20% of patients dose-reduced ITZ due to GI intolerance [10]. The largest randomized controlled trial in this setting using ITZ by Marks et al failed to demonstrate a survival or proven/probable IFD difference compared to voriconazole; however, early discontinuation of ITZ due to intolerance or adverse effects including vomiting, nausea, and diarrhea was significant [11]. With improvements to the formulation maximizing tolerability and absorption, S-ITZ may be a potentially advantageous choice of agent for primary IFD prophylaxis in HCT.
The utility of conventional ITZ for primary prophylaxis has also been restricted by high individual pharmacokinetic variability [21, 28, 29]. We found that therapeutic levels of S-ITZ were achieved at a median of 10 days, with 75% of patients achieving therapeutic levels by 14 days, and that the overall mean S-ITZ level was 1130ng/mL. Serum ITZ trough concentrations <1000ng/mL are predictive of therapeutic failure, with individuals with concentrations <500ng/mL significantly more likely to develop IFD [21, 29]. With the achievement of higher serum trough levels than previous studies of conventional formulations [10, 11], and improved tolerability, S-ITZ may also be a potentially useful agent for primary IFD prophylaxis during GVHD, with further studies using the S-ITZ formulation in this population warranted [27]. Recently, there has been a report of using a 3-day loading dose to achieve therapeutic levels more rapidly, which may be a potential strategy to further improve its use in clinical practice [16].
Despite achieving higher trough ITZ serum concentrations than previous studies, we did not identify any safety issues. Documented toxicity was minimal, with 1 patient demonstrating liver injury potentially attributable to S-ITZ and no patients reported to have a prolonged QTc or GI intolerance; however, routine QTc measurements were at the discretion of the treating physician only.
Drug–drug interactions are a major consideration with the use of triazole antifungals for antifungal prophylaxis in HCT [30–32]. Many centers that use triazoles as standard prophylaxis have specific dosing and therapeutic drug monitoring protocols for concomitant drugs such as calcineurin inhibitors, taking into consideration these interactions. One advantage of continuing prophylaxis with a triazole until weaning of immunosuppression, such as the cohort A policy, is the stable CYP3A4 inhibition throughout the first 100 days post-HCT, which leads to less variation in calcineurin or mTOR inhibitor levels, which could potentially impact toxicity or rates of GVHD. S-ITZ also has the advantage of less interpatient variability in trough serum levels compared to other formulations of ITZ, which in turn results in more stable CYP3A4 inhibition [13, 17].
The results of this study are limited by the retrospective, noninterventional design. In addition, the study included 2 antifungal prophylaxis strategies, with differing durations of S-ITZ therapy. We did not demonstrate a significant difference in survival or proven/probable IFD but noted there were more cases of possible/suspected IFD combined with proven/probable IFD after engraftment in cohort B with a shorter duration of prophylaxis; however, as addressed above, this result was not statistically significant in the absence of GVHD. There is currently no consensus for the duration or agent of choice for primary antifungal prophylaxis after HCT in the absence of GVHD [5]. Local prevalence of IFD, drug–drug interactions, tolerability, and the cost-to-benefit ratio result in varied practices. In low-IFD-risk, non-GVHD HCT recipients, Candida prophylaxis alone with fluconazole is used in centers with historically low rates of mold infections, whereas mold-active agents such as voriconazole, posaconazole, and isavuconazole are also often chosen [5, 33]. Mold-active prophylaxis has been reported to be marginally more effective for preventing IFD compared to empiric or preemptive therapy, but at a higher cost [34]. Further studies assessing the most appropriate postengraftment antifungal strategy are therefore warranted.
Overall, this study has demonstrated that S-ITZ is a safe and well-tolerated formulation and overcomes many of the limitations seen with the older oral ITZ formulation. It is a novel alternative for primary IFD prophylaxis after HCT.
Notes
Financial support. J. L. is supported by a Leukaemia Foundation/Haematology Society of Australia and New Zealand New Investigator PhD Scholarship. M. S. is supported by National Health and Medical Research Council Centres of Research Excellence Grant (1116876) and Investigator Grant (1173791).
Potential conflicts of interest. J. L. has served on advisory boards for Mayne Pharma, Merck Sharp & Dohme (MSD), Amgen, and Bristol-Myers Squibb. D. C. M. K. has served on advisory boards for Becton Dickinson and MSD, and has received financial support from MSD and F2G, all unrelated to the current work. S. A. P. receives research support from Global Life Technologies; participated in research trials with Chimerix and Merck & Co; and participated in a clinical trial sponsored by the National Institute of Allergy and Infectious Diseases (grant number U01-AI132004). All other authors report no potential conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Contributor Information
Julian Lindsay, National Centre for Infection in Cancer, Peter MacCallum Cancer Centre, Melbourne, Australia; Haematology Department, Royal North Shore Hospital, Sydney, Australia; Vaccine and Infectious Disease and Clinical Research Division, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA.
Jad Othman, Haematology Department, Royal North Shore Hospital, Sydney, Australia.
Yvonne Kong, Institute of Haematology, Royal Prince Alfred Hospital, Sydney, Australia.
Annie Yip, Institute of Haematology, Royal Prince Alfred Hospital, Sydney, Australia.
Sebastiaan Van Hal, Infectious Diseases Department, Royal Prince Alfred Hospital, Sydney, Australia.
Stephen Larsen, Institute of Haematology, Royal Prince Alfred Hospital, Sydney, Australia.
Christian Bryant, Institute of Haematology, Royal Prince Alfred Hospital, Sydney, Australia.
John Gibson, Institute of Haematology, Royal Prince Alfred Hospital, Sydney, Australia.
Ian Kerridge, Haematology Department, Royal North Shore Hospital, Sydney, Australia; Northern Blood Research Centre, Kolling Institute of Medical Research, University of Sydney, Sydney, New South Wales, Australia.
Keith Fay, Haematology Department, Royal North Shore Hospital, Sydney, Australia.
William Stevenson, Haematology Department, Royal North Shore Hospital, Sydney, Australia; Northern Blood Research Centre, Kolling Institute of Medical Research, University of Sydney, Sydney, New South Wales, Australia.
Chris Arthur, Haematology Department, Royal North Shore Hospital, Sydney, Australia.
Sharon C A Chen, National Centre for Infection in Cancer, Peter MacCallum Cancer Centre, Melbourne, Australia; Centre for Infectious Diseases and Microbiology Laboratory Services, Institute of Clinical Pathology and Medical Research, New South Wales Health Pathology, Westmead Hospital, and Marie Bashir Institute for Infectious Diseases and Biosecurity, University of Sydney, Sydney, Australia.
David C M Kong, National Health and Medical Research Council National Centre for Antimicrobial Stewardship at the Peter Doherty Institute for Infections and Immunity, Parkville, Victoria, Australia; Centre for Medicine Use and Safety, Monash Institute of Pharmaceutical Sciences, Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, Parkville, Victoria, Australia; Pharmacy Department, Ballarat Health Services, Ballarat, Victoria, Australia.
Matthew Greenwood, Haematology Department, Royal North Shore Hospital, Sydney, Australia; Northern Blood Research Centre, Kolling Institute of Medical Research, University of Sydney, Sydney, New South Wales, Australia.
Steven A Pergam, Vaccine and Infectious Disease and Clinical Research Division, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA; Division of Allergy and Infectious Diseases, University of Washington, Seattle, Washington, USA.
Catherine Liu, Vaccine and Infectious Disease and Clinical Research Division, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA; Division of Allergy and Infectious Diseases, University of Washington, Seattle, Washington, USA.
Monica A Slavin, National Centre for Infection in Cancer, Peter MacCallum Cancer Centre, Melbourne, Australia; Department of Infectious Diseases, Peter MacCallum Cancer Centre, Melbourne, Australia; Sir Peter MacCallum Department of Oncology, University of Melbourne, Parkville, Australia.
References
- 1. Neofytos D, Horn D, Anaissie E, et al. Epidemiology and outcome of invasive fungal infection in adult hematopoietic stem cell transplant recipients: analysis of Multicenter Prospective Antifungal Therapy (PATH) Alliance registry. Clin Infect Dis 2009; 48:265–73. [DOI] [PubMed] [Google Scholar]
- 2. Menzin J, Meyers JL, Friedman M, et al. Mortality, length of hospitalization, and costs associated with invasive fungal infections in high-risk patients. Am J Health Syst Pharm 2009; 66:1711–7. [DOI] [PubMed] [Google Scholar]
- 3. Perfect JR, Hachem R, Wingard JR. Update on epidemiology of and preventive strategies for invasive fungal infections in cancer patients. Clin Infect Dis 2014; 59(Suppl 5):S352–5. [DOI] [PubMed] [Google Scholar]
- 4. Taplitz RA, Kennedy EB, Bow EJ, et al. Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J Clin Oncol 2018; 36:3043–54. [DOI] [PubMed] [Google Scholar]
- 5. Maertens JA, Girmenia C, Brüggemann RJ, et al. European Conference on Infections in Leukaemia (ECIL), a joint venture of the European Group for Blood and Marrow Transplantation (EBMT), the European Organization for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS), and European Conference on Infections in Leukaemia (ECIL), a joint venture of the European Group for Blood and Marrow Transplantation (EBMT), the European Organization for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS) and the European LeukemiaNet (ELN). European guidelines for primary antifungal prophylaxis in adult haematology patients: summary of the updated recommendations from the European Conference on Infections in Leukaemia. J Antimicrob Chemother 2018; 73:3221–30. [DOI] [PubMed] [Google Scholar]
- 6. Corzo-León DE, Satlin MJ, Soave R, et al. Epidemiology and outcomes of invasive fungal infections in allogeneic haematopoietic stem cell transplant recipients in the era of antifungal prophylaxis: a single-centre study with focus on emerging pathogens. Mycoses 2015; 58:325–36. [DOI] [PubMed] [Google Scholar]
- 7. Bow EJ, Vanness DJ, Slavin M, et al. Systematic review and mixed treatment comparison meta-analysis of randomized clinical trials of primary oral antifungal prophylaxis in allogeneic hematopoietic cell transplant recipients. BMC Infect Dis 2015; 15:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ziakas PD, Kourbeti IS, Mylonakis E. Systemic antifungal prophylaxis after hematopoietic stem cell transplantation: a meta-analysis. Clin Ther 2014; 36:292–306.e1. [DOI] [PubMed] [Google Scholar]
- 9. Stern A, Su Y, Lee YJ, et al. A single-center, open-label trial of isavuconazole prophylaxis against invasive fungal infection in patients undergoing allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2020; 26:1195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marr KA, Crippa F, Leisenring W, et al. Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Blood 2004; 103:1527–33. [DOI] [PubMed] [Google Scholar]
- 11. Marks DI, Pagliuca A, Kibbler CC, et al. IMPROVIT Study Group. Voriconazole versus itraconazole for antifungal prophylaxis following allogeneic haematopoietic stem-cell transplantation. Br J Haematol 2011; 155:318–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fontana L, Perlin DS, Zhao Y, et al. Isavuconazole prophylaxis in patients with hematologic malignancies and hematopoietic cell transplant recipients. Clin Infect Dis 2020; 70:723–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mayne Pharma International Pty Ltd. TOLSURA (itraconazole capsules) [prescribing information]. Greenville, NC: Mayne Pharma International Pty Ltd; 2018. [Google Scholar]
- 14. Mayne Pharma. Lozanoc (itraconazole capsules) [prescribing information]. Salisbury, South Australia: Mayne Pharma; 2014. [Google Scholar]
- 15. Abuhelwa AY, Foster DJ, Mudge S, et al. Population pharmacokinetic modeling of itraconazole and hydroxyitraconazole for oral SUBA-itraconazole and Sporanox capsule formulations in healthy subjects in fed and fasted states. Antimicrob Agents Chemother 2015; 59:5681–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thompson GR, 3rd, Lewis P, Mudge S, et al. Open-label crossover oral bioequivalence pharmacokinetics comparison for a 3-day loading dose regimen and 15-day steady-state administration of SUBA-itraconazole and conventional itraconazole capsules in healthy adults. Antimicrob Agents Chemother 2020; 64:e00400-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lindsay J, Sandaradura I, Wong K, et al. Serum levels, safety and tolerability of new formulation SUBA-itraconazole prophylaxis in patients with haematological malignancy or undergoing allogeneic stem cell transplantation. J Antimicrob Chemother 2017; 72:3414–9. [DOI] [PubMed] [Google Scholar]
- 18. Donnelly JP, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis 2020; 71:1367–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fleming S, Yannakou CK, Haeusler GM, et al. Consensus guidelines for antifungal prophylaxis in haematological malignancy and haemopoietic stem cell transplantation, 2014. Intern Med J 2014; 44:1283–97. [DOI] [PubMed] [Google Scholar]
- 20. Przepiorka D, Weisdorf D, Martin P, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15:825–8. [PubMed] [Google Scholar]
- 21. Glasmacher A, Hahn C, Leutner C, et al. Breakthrough invasive fungal infections in neutropenic patients after prophylaxis with itraconazole. Mycoses 1999; 42:443–51. [DOI] [PubMed] [Google Scholar]
- 22. National Institute of Diabetes and Digestive and Kidney Diseases. Severity grading in drug induced liver injury. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury 2012. Available at: livertox.nih.gov. Accessed 1 February 2021. [PubMed] [Google Scholar]
- 23. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94:496–509. [Google Scholar]
- 24. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 2013; 48:452–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nield B, Larsen SR, van Hal SJ. Clinical experience with new formulation SUBA®-itraconazole for prophylaxis in patients undergoing stem cell transplantation or treatment for haematological malignancies. J Antimicrob Chemother 2019; 74:3049–55. [DOI] [PubMed] [Google Scholar]
- 26. Winston DJ, Maziarz RT, Chandrasekar PH, et al. Intravenous and oral itraconazole versus intravenous and oral fluconazole for long-term antifungal prophylaxis in allogeneic hematopoietic stem-cell transplant recipients. A multicenter, randomized trial. Ann Intern Med 2003; 138:705–13. [DOI] [PubMed] [Google Scholar]
- 27. Grigg AP, Brown M, Roberts AW, et al. A pilot study of targeted itraconazole prophylaxis in patients with graft-versus-host disease at high risk of invasive mould infections following allogeneic stem cell transplantation. Bone Marrow Transplant 2004; 34:447–53. [DOI] [PubMed] [Google Scholar]
- 28. Andes D, Pascual A, Marchetti O. Antifungal therapeutic drug monitoring: established and emerging indications. Antimicrob Agents Chemother 2009; 53:24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cartledge JD, Midgely J, Gazzard BG. Itraconazole solution: higher serum drug concentrations and better clinical response rates than the capsule formulation in acquired immunodeficiency syndrome patients with candidosis. J Clin Pathol 1997; 50:477–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Girmenia C, Iori AP. Safety and interactions of new antifungals in stem cell transplant recipients. Expert Opin Drug Saf 2012; 11:803–18. [DOI] [PubMed] [Google Scholar]
- 31. Glotzbecker B, Duncan C, Alyea E 3rd, et al. Important drug interactions in hematopoietic stemcell transplantation: what every physicianshould know. Biol Blood Marrow Transplant 2012; 18:989–1006. [DOI] [PubMed] [Google Scholar]
- 32. Lempers VJ, Martial LC, Schreuder MF, et al. Drug-interactions of azole antifungals with selected immunosuppressants in transplant patients: strategies for optimal management in clinical practice. Curr Opin Pharmacol 2015; 24:38–44. [DOI] [PubMed] [Google Scholar]
- 33. Bogler Y, Stern A, Su Y, et al. Efficacy and safety of isavuconazole compared with voriconazole as primary antifungal prophylaxis in allogeneic hematopoietic cell transplant recipients [manuscript published online ahead of print 24 May 2021]. Med Mycol 2021. doi:10.1093/mmy/myab025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Walker BS, Schmidt RL, Tantravahi S, et al. Cost-effectiveness of antifungal prophylaxis, preemptive therapy, or empiric treatment following allogeneic hematopoietic stem cell transplant. Transpl Infect Dis 2019; 21:e13148. [DOI] [PubMed] [Google Scholar]