Abstract
The spread of COVID‐19 infection has changed the world. Population‐based studies of COVID‐19 are limited because it is unknown why events happen or why certain outcomes occur. An alternative approach called the patient pathway review evaluates what happens to individuals in detail. In the “ideal” pathway patients with COVID‐19 will seek medical attention and COVID‐19 will be identified and they will either be admitted to hospital, managed in the community or they will self‐care. However, in the “real‐world” pathway, patients may delay seeking medical attention and it is variable who the patient decides to seek help from and some patients may be initially misdiagnosed. The eventual outcome will be recovery from the acute infection or death but there may be a spectrum of healthcare needs for patients from those who care for themselves in the community to those who are hospitalized and require intensive care. The patients may or may not have short‐ and long‐term adverse effects. People infected with COVID‐19 can take on different paths which depend on the patient's decision making, clinical decision making, and the patient's response to the infection. Desirable pathways are those where patients have good outcomes and also limit the transmission of the virus.
Keywords: COVID‐19, pathways, patient care outcomes
1. INTRODUCTION
The spread of COVID‐19 infection has changed the world. This virus is responsible for significant morbidity and mortality, such that all aspects of life have been affected. People have had to isolate and reduce social contact. A proportion of those employed have been made redundant and some businesses have had to shut down. Health services have had to be restructured and clinical practice has had to rapidly adapt and change. Governments have had to make unforeseen policy decisions to curtail the spread of the virus. The pandemic has undoubtedly had a significant impact on the physical and mental health of the entire population.
Epidemiological evaluations of COVID‐19 infections have enabled a great understanding of the virus and how it spreads which has driven policy decisions all over the world. 1 Epidemiologists were able to model early in the pandemic that the virus case numbers were actually higher than documented. Furthermore, they were able to demonstrate the benefit of using face masks, staying at home, and other public health measures such as school closures, restricting travel, and reducing mixing within households. 1 However, this approach is not without limitations. The data accuracy are dependent on the data collection methods. For example, in the absence of testing the entire population, it is impossible to know the total burden of infection, with modeling used to provide estimates. Therefore, most reported estimates are derived from people who underwent testing, whilst many patients with COVID‐19 are asymptomatic. 2 While it is not the purpose of epidemiological studies, the more useful information that can be applied clinically and practically for decision making is the impact of COVID‐19 on individuals and understanding both why events took place and their associated outcome. An alternative approach is looking at what happens to individuals in detail. This novel approach, known as the patient pathway review, 3 has not been applied to COVID‐19 infections before. It has the distinct advantage that it considers possible paths that patients may take and then attempts to rationalize them by considering different perspectives such as that of the patient, clinician, health service, and society.
This review reports the patient pathway review with the starting point of a patient contracting COVID‐19. It explores the consequence of the acute infection and the possible key events that take place. This is done in a systematic approach whereby an initial “ideal” pathway is defined with is then modified considering events that take place in “real‐world” settings. The findings of the real‐world settings are then discussed in the contact of the patient, clinician, healthcare service, and society perspective.
2. METHODS
The first description of the patient pathway review has been published elsewhere. 3 This is described in brief below.
2.1. Starting point
The starting point of this patient pathway review is that of a patient that is infected with COVID‐19. The patient pathway review is also broken down into two aspects: the acute infection and potential short and long‐term consequences after initial recovery.
2.2. Defining the “ideal” patient pathway for acute COVID‐19 infection
The “ideal” pathway, from the patients' starting point is then developed considering the onset of symptoms, review by healthcare professionals, investigations, diagnosis, treatment, response for the acute infection, and subsequent outcomes.
2.3. Defining the “real‐world” patient pathway for acute COVID‐19 infection
From the “ideal” patient pathway, each stage will be systematically explored by considering undesirable realities in clinical practice such as patient's failure to recognize the significance of their symptoms, variability of the care delivered by healthcare professionals, and possible misdiagnosis. The systematic approach is defined by considering all stages of the pathway as opposed to just targeting certain stages of the pathway and ignoring others. This will be used to create a “real‐world” pathway.
For the purposes of this evaluation, two assumptions are made. First, patients who are tested for COVID‐19 who have the infection will test positive and we will not consider the real possibility that the test failed to detect the infection. Therefore, with the widespread availability of testing in many developed countries, all that is required for the determination of COVID‐19 status is suspicion of the infection. Furthermore, while there is variation in the exact care individual patients with COVID‐19 receive, once diagnosed the exact treatment algorithms for patients are beyond the scope of the current review but rather the approach of the patient being managed in the community, hospital, or intensive care is used with clinical severity of illness driving the transition between settings. The response is defined as either recovery from COVID‐19 or death.
2.4. Defining the long‐term patient pathway after recovery from acute COVID‐19 infection
The development of potential adverse complications associated with COVID‐19 after recovery will be discussed but a single pathway will be defined rather than first defining the “ideal” and then exploring it from a “real‐world” approach.
2.5. Explaining the “real‐world” patient pathways
Considering that one of the tenants of the patient pathway analysis is that there is usually a reason for why events take place, a systematic approach of considering the key perspectives was used to explain what and why events happen in the real‐world pathway. First, would be the patient perspective including the reasoning for the decisions they made as well as their priorities. Second, the clinician perspective is explored followed by that of the health service. Finally, the society agenda will be considered as public health measures and health policies can influence patient, clinician, and health service decision making.
3. RESULTS
3.1. “Ideal” patient pathway after acute COVID‐19 infection
From the starting point where a person contract COVID‐19 the ideal pathway is shown in Figure 1. The major decision for patients is whether to seek health care attention or remain in the community. A patient who remains in the community after contracting COVID‐19 may be unwell but the infection could resolve. Their symptoms may worsen which merits hospitalization, identification of COVID‐19, and even intensive care admission if they deteriorate. They may also seek medical attention at an early stage and COVID‐19 may be detected. The eventual outcome will either be recovery from the acute infection or death.
Figure 1.
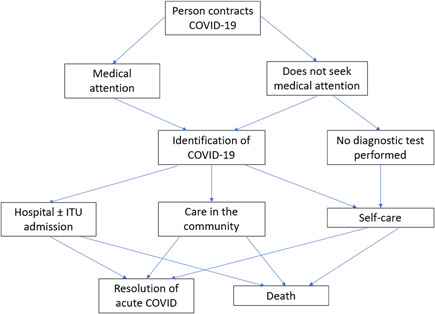
“Ideal” pathway of acute COVID‐19 infection
3.2. “Real‐world” patient pathway after acute COVID‐19 infection
The “real‐world patient pathway evaluates what happens to patients in more detail (Figure 2). After contracting COVID‐19 patients may or may not develop symptoms which may be a major driver regarding whether or not they will seek medical attention. There are also options in terms of who the person infected with COVID‐19 will see for medical help. These include the general practitioner or family doctors, outpatient hospital care, emergency care, and other professional groups such as community nurse practitioners or pharmacists. If medical attention is not sought the COVID‐19 infection may resolve or progress and if it progresses it introduces a delay to medical attention. Even at the stage of medical attention, it is important that COVID‐19 is suspected as misdiagnosis is also possible. Misdiagnosis may result in increased severity of symptoms which creates delay before the eventual identification of COVID‐19. From there, similar to the “ideal” pathway patient may be managed in the community and hospital with or without intensive care admissions. The ultimate outcome will be the resolution of COVID‐19 or death.
Figure 2.
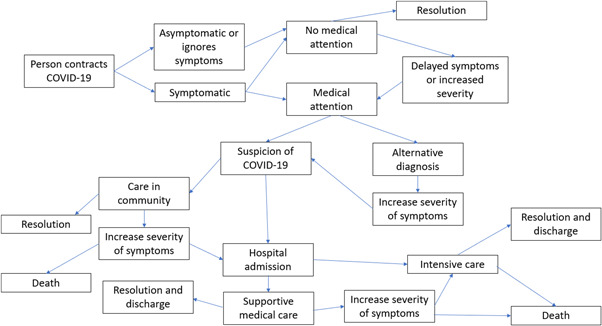
“Real‐world” pathway of acute COVID‐19 infection
3.3. Patient pathway after recovery from acute infection
The pathway for patients after recovery from acute infection is shown in Figure 3. Patients may have no short‐ or long‐term adverse effects after COVID‐19. The patient may have short‐term adverse effects with or without long terms adverse effects including prolonged COVID‐19 or no short‐term adverse effects but long‐term adverse effects. In terms of long‐term effects, an important consideration is whether patients will die before developing the long‐term adverse event.
Figure 3.
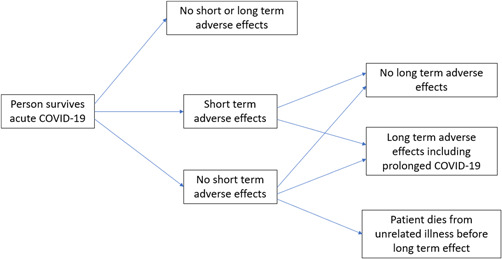
Pathway postrecovery from acute COVID‐19 infection
3.4. The patient perspective
It is well known that COVID‐19 infection is potentially life‐threatening and as such most people would aim to avoid contracting the infection. However, once they are infected the aim shifts to overcoming the infection, alleviating any suffering from symptoms, and carrying on with independent living without any long‐term adverse consequences. In the cases where patients are symptomatic understanding what the diagnosis underlying their ill‐health may be of prime concern. Once the diagnosis is suspected or confirmed, the patient will consider whether or not they have symptoms that merit seeking medical advice. If a patient had a fever and cough, they may self‐medicate with over‐the‐counter medications such as paracetamol. However, the collection of symptoms that may represent COVID‐19 is diverse which includes fatigue, shortness of breath, anosmia, loss of appetite, myalgia, headache, and the patient may even be asymptomatic. 4 While symptoms may be the main driver for seeking medical attention, there may be other factors influencing the willingness to seek medical attention including whether they have the time or have other priorities/responsibilities, medical knowledge, and other factors including any concerns about contracting COVID‐19 from seeking medical attention. One other factor which may impact decisions about seeking medical attention is the healthcare service and whether patients need to pay for care. There may be delays in seeking help in cases where there are initially mild symptoms because of the potential cost associated with healthcare in some countries.
It is not known whether delay in seeking medical attention affects the eventual outcome of acute COVID‐19 infection. Aside from cases where patients die in the community from COVID‐19 who did not receive any treatment, those patients who present to the hospital will have monitoring and treatment with appropriate escalation with clinical deterioration. Delays can also be contributed by delays in accessing diagnostic tests, delays related to misdiagnosis, and delays related to the volume of patients needing treatment. The exact care received will depend on the availability of healthcare and the extent to which it had to make adaptations to cope with COVID‐19. It is expected that most patients will survive the illness but some may die especially those who are elderly and frail. 5 , 6
The impact of COVID‐19 infection extends beyond the individual but also to everyone around them and everyone they come into contact with. The possible responses are shown in Figure 4 which influence the likelihood of transmission to others which may be related to the severity of symptoms. People may increase contact with others, carry on with usual activities, reduce but not carry out full isolation or fully isolate themselves with as limited contact as possible. Patients may have a strong desire to limit potential spread to those living with them and isolate as much as possible. Alternatively, patients especially those with very mild or no symptoms, may carry on with daily activities or increase contact with others.
Figure 4.
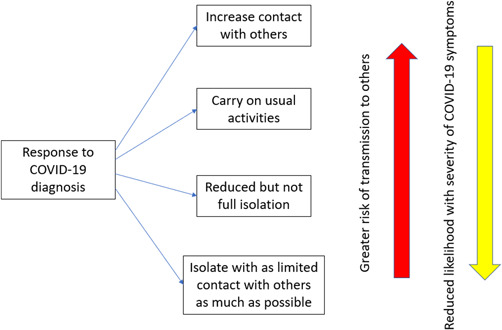
Options of patient activity in response to acute infection
3.5. The clinician perspective
From the clinician's perspective, it is important to protect themselves from being infected while also carrying out their duty to identify and treat the COVID‐19 infection. In the efforts to minimize the chance of contracting COVID‐19 many clinicians seeing patients in the community have reduced face‐to‐face appointments. Unlike emergency hospital visits where patients will be reviewed in person, assessments of symptoms can only be undertaken via the telephone but physical examinations are not possible. Nevertheless, the information from telephone assessments can be used to risk stratify and advise patients to have COVID‐19 testing when they have not done so already. It is particularly important that the personnel at the front lines including paramedics and emergency room doctors have adequate personal protective equipment. There should also be pathways within hospitals to have designed potential COVID‐19 infected patients and areas where patients do not have COVID‐19.
As not detecting COVID‐19 can have disastrous consequences with the spread of infection, the tests used to identify COVID‐19 have become widespread such that all patients in hospital and community settings can be tested. Nevertheless, no test is perfect and some patients may not be detected initially but go one to have COVID‐19. Because of how common infections with COVID‐19 are in most hospitals there are protocols in place for Treatment protocols, including advice on the use of dexamethasone and oxygen and when to escalate patients to intensive care are commonplace in secondary care and rapidly evolving as new evidence emerges.
Especially worse at the height of the pandemic, many clinicians have been psychologically affected by COVID. Patients with COVID‐19 infections were dying and colleagues were frequently victims of the virus. In some places there was mass staff redeployment to care for COVID‐19 patients and the type of work specialist doctors and surgeons were doing was radically different from their usual clinical activity. Clinicians were concerned about having the right skills to care for these patients while being concerned about rising waiting lists for routine work.
3.6. The healthcare service perspective
The healthcare service perspective is complex. COVID‐19 pandemic created an additional burden of managing infected patients in most healthcare systems on top of the usual patient workload in the community or hospital settings. In places where there was a high volume of hospitalized COVID‐19 cases, routine services such as elective surgery and procedures had to be canceled and medical and surgical wards were converted to COVID‐19 wards. Also, there are changes in physical delivery of care where patient care may be divided into those who may be exposed to COVID‐19 and a separate area for those who have tested negative. Furthermore, healthcare services need to secure personal protective equipment including gloves, aprons, and masks. During the early part of the pandemic, there were concerns about not having enough or the correct supplies.
COVID‐19 has had a different impact on the different areas of the healthcare system, whether public or private. In public healthcare systems, the effect of finite resources is greater as there is no additional monetary support provided to care for more patients. This is particularly important as resources had to be diverted to manage the burden of COVID‐19 patients. In private settings, patients pay for the cost of health care so there may be more resources available for clinicians to care for patients. However, in such settings, there may be a reluctance to seek healthcare professionals because of the associated cost. Avoidance of seeking help can translate into the greater spread of infection in the community.
The effect of COVID‐19 infections on staff and workers in care settings having to isolate because of exposure because of potential COVID‐19 exposure is a serious problem to health services. The morale of staff may be impacted by seeing the devastating effect of COVID‐19 on patients and society and now some have had to take up additional responsibilities and be put under additional pressure because of their colleagues' COVID‐related absences.
3.7. Society
The impact of COVID‐19 on society is significant. The priority is to stop the infection from spreading and alleviating the burden of those affected by the illness and its consequences on society.
A worldwide problem, drastic measures have been taken by different governments to reduce the transmission of infection. These have significant downstream consequences on healthcare services, clinicians, patients, and the public. While public health measures were implanted for the recent infectious outbreaks such as the severe acute respiratory syndrome (SARS), Avian influenza, and Zika virus, the measures taken have never been as drastic as those implemented for COVID‐19. These measures include lockdowns restricting social contact, social isolation policies, and vaccination programs. While in theory, these large‐scale interventions should be of benefit, the key is that for them to work they must be adhered to and the extent of compliance with these measures is uncertain. This is particularly challenging when trying to demonstrate robust evidence regarding the extent to which these measures reduce transmission. More than likely, these interventions potentially can modify the proportion of patients in different pathways.
The societal perspective is complex. If a patient with COVID‐19 dies, it is a tragic event. As most patients recover from the infection, the difficulty in understanding how transmission of the virus occurs on the individual and then the populational level. While partly influenced by the severity of the symptoms, people who contract COVID‐19 make key decisions regarding their health about whether they should ignore symptoms, self‐treat, or seek medical attention. A significant problem occurs if patients are actually contracting the virus from seeking medical attention. At present, it is not absolutely clear how the virus is spread but the danger is if patients who do not have the virus contract it from ambulance drivers, professionals in hospital, or even from inanimate objects in the hospital or transport environment.
The downstream consequence of COVID‐19 infection is significant affecting the workforce and healthcare. Countries who used strategies to support people financially during periods of lockdown (such as the UK “furlough” scheme) have incurred large financial debts. Investments have also been required to support patient care. Some patients with COVID‐19 may develop complications and we are still trying to understand these long‐term outcomes.
4. DISCUSSION
Human factors, whether it is the patient and clinician, are a major contributor to deviations from the “ideal” pathway. The COVID‐19 pandemic has created significant uncertainty which has caused anxiety for the public and healthcare professionals. As highlighted in the patient pathway review, after one is infected with the virus the possible outcomes for patients are diverse and there is currently insufficient knowledge to reliably predict the eventual outcome for most patients. In the pathway review, we show how it can become increasingly complex due to multifactorial human factors such as decisions to seek medical attention and the ability of clinicians to recognize the infection. A key challenge is heterogeneity in clinical response to infection. Some patients will have no or mild symptoms, while others may develop life‐threatening symptoms. In the absence of extensive clinical experience handling the infection, no one really knows how to identify those who will be unwell until they deteriorate. This is further compounded by the fact that there are different variants of the virus which have different pathogenicity. The key is to recognize that there are potentially nonavoidable reasons for deviations from the pathway, such as the strain of the virus and patient variability in response to infection, but there are also modifiable factors such as the degree to which the public who are infected agree to measures recommended by government as well as areas such as healthcare professional's willingness to follow the guidance.
The priorities and vigilance of the patient, clinician, healthcare service, and society integrate to influence the proportion of patients who undergo the identified pathways. There are two important considerations regarding the implications of the patient pathway and that is the outcome of the patient and the degree to which there is transmission as a consequence of the infected patient. The consideration of transmission is important as it separates COVID‐19 from other clinically significant noncommunicable diseases such as ischaemic heart disease, chronic lung disease, diabetes mellitus, and cancer.
The aim of the patient, in general, is to overcome the infection and minimize and potential long‐term adverse effects. Some patients may also feel that it is important not to spread it to others, especially family members. Among mild cases which resolve, ideally the patient is able to isolate at home which minimizes the spread to other members of the public. While challenging to control especially when patients are asymptomatic, the risk of spreading the infection is expected to be high for patients who have COVID‐19 but carry on doing the same level or increased levels of social contact. Isolation and not seeking medical attention can place the patient in danger of a poor outcome and even death in the community. In most cases, however, patients who deteriorate will call for help, and for some medical treatment may reverse the course of the illness. Nevertheless, for some patients, mortality will be the outcome regardless of intervention but it may place those looking after the patient and transporting the patient at risk of infection.
Clinicians and those involved in the care of patients who may have COVID‐19 must be vigilant when it comes to use of protective equipment from infection. While some clinicians may have had the vaccine or had the infection, they should not assume they are immune as they may not contract the same strain of virus again but also, they could indirectly transmit the infection indirectly via fomites, surfaces, and objects. 7 This can have serious implications as viral infections can grow exponentially if frontline staff are infecting patients and other staff members. The priority from the clinician point of view is to protect oneself and other members of staff while carrying out the best management for patients. It is, therefore, important that the clinicians themselves are cautious minimizing unnecessary contact with patients and discouraging potentially high‐risk practices.
The priorities of the health service are to carry on treating patients and protecting its staff. Lack of care in protecting the healthcare professionals can translate to serious problems if the workforce is infected and unable to work. To reduce spread many hospitals have the capacity to test all patients that are admitted. This can help identify high‐risk and low‐risk areas for risk of transmission. Current literature suggests that COVID‐19 can be spread by both direct and indirect contact. Person‐to‐person spread of COVID‐19 is reported to be mainly via respiratory droplets which typically traverse up to 6 feet and can remain suspended in the air for up to 3 h while spread can also be mediated via contaminated objects and airborne contagion. 8 This has huge implications in attempting to break the cycle of infection as we have previously suggested that the virus can be on any part of the hospital including telephones, patient notes, keyboards, and so on, and some of the most important workers in COVID‐19 exposed areas are the cleaners as they have a key role in reducing transmission. 9 It remains challenging to determine how exactly COVID‐19 is transmitted on an individual level.
As a society, there are significant consequences on infection rates depending on government policies. Decisions to implement and stop lockdowns or restrictive measures can limit social contact but the use of a vaccine to achieve herd immunity is frequently acknowledged as the approach to combat the infection in the community. 10 However, a significant problem is a knowledge regarding the degree of protection of a vaccine. While mostly mild or asymptomatic, even fully vaccinated health care workers can have breakthrough infections. 11 The impact of vaccination and social restriction can alter the patient pathway so that fewer have severe symptoms and more will isolate and reduce contact with others when they have the infection.
There are clear pathways that are more desirable than others. First is the patient who develops COVID‐19 and decides to isolate in the community with minimal contact to others. Ideally, this patient recovers and does not transmit the infection and suffers no long‐term consequences related to COVID‐19, and is immune to subsequent exposure to infection. The next pathway that is to a degree favorable is that where a patient develops COVID‐19 but requires supportive treatment in hospital or will die from the infection. While it is impossible to know whether a patient will need support to overcome the infection, there will be differences the extent to which this patient does or does not expose the public or healthcare professionals to the infection. Patients who minimize the risk of transmission to others are ideal which would mean seeking medical attention and there being rapid suspicion and confirmation of COVID‐19 and urgent treatment to alleviate any deterioration. Those who have multiple contacts with various health professionals and carry on with ongoing daily activities that involve social contact with others is undesirable from a COVID‐19 transmission perspective.
There are measures that may be taken that could promote more desirable and reduce less unfavorable pathways. While it is not always straightforward and often challenging, the use of clinical judgment to establish the ceiling of care for patients that are infected with COVID‐19. The COVID‐19 infection can rapidly spread and overwhelm health services such that there may not be sufficient resources to care for patients including the need for ventilators, oxygen, and intensive care beds. These resources should be reserved for patients who stand to most benefit from them.
Management algorithms can help prioritize care and these are developed based on the availability of local resources and existing evidence. These include policies to screen for COVID‐19 in certain individuals who have symptoms that are deemed to be high risk such as cough or fever in the community. Education has an important role both in terms of the public in recognizing how to protect themselves with measures such as handwashing, protective equipment, and avoiding close contact with others but also when they should seek medical attention. Another important aspect is educating the healthcare professionals about how to avoid contracting the infection and how patients may present with atypical symptoms to avoid misdiagnosis. Prevention can be helpful with vaccination provided that the vaccine is effective. Vaccinating people with a safe vaccine that has proven efficacy in theory only brings benefits to the population.
The COVID‐19 pandemic at different stages has evolved in infection, spread, and disease. In addition, patients, clinicians, healthcare services, and society have learned lessons at every stage and devised appropriate responses. Therefore, it is important to be aware that the patient pathway might also evolve accordingly.
While the patient pathway approach provides a framework of what might happen to patients, it is limited because there is no understanding of how common each pathway is. However, the current approach has the value that it can be applied in any country, setting, or healthcare system. Another limitation of this approach is the defined ideal pathway. It may be argued that the pathway presented may not be the same if multiple clinicians with different experiences and practices were asked to define the ideal pathway. However, most developed countries will have patients cared for in different settings including hospitals and community care. The interesting thing about COVID‐19 compared to other chronic conditions is that some patients will only have mild or no symptoms so they may not even know they had the infection so awareness of the group who do not seek medical attention is important. The consideration of guidelines may be of relevance to the ideal pathway however, the problem is that guidelines are only relevant to the countries which developed them. The other key limitation is that while we explore the possible outcomes in terms of long‐ and short‐term effects or no effects of COVID‐19 infection, there is insufficient data to comment yet on long‐term effects as the virus spreading in humans have only been around for less than 2 years.
5. CONCLUSIONS
In conclusion, we have shown in this patient pathway review that people infected with COVID‐19 can take on different paths which depend on factors related to the patient's decision making, clinical decision making and patient's response to the infection. Desirable pathways are those where patients have good outcomes and also limit the transmission of the virus. Consideration of the patient, clinician, healthcare service, and society perspective can be used in attempts to rationalize possible pathways that patients take. More studies are needed to identify those who require more aggressive management as well as the potential long‐term complications related to COVID‐19 infection.
AUTHOR CONTRIBUTIONS
Chun Shing Kwok conceptualized the review and wrote the original draft of the manuscript. Elena‐Andra Muntean and Christian D. Mallen reviewed the manuscript and revised it critically for important intellectual content.
ACKNOWLEDGMENT
Keele School of Medicine has received funds from Bristol Myer Squibb for academic support for a nonpharmacological atrial fibrillation screening trial but this is not related to this study.
Kwok CS, Muntean E‐A, Mallen CD. The impact of COVID‐19 on the patient, clinician, healthcare services and society: A patient pathway review. J Med Virol. 2022;94:3634‐3641. 10.1002/jmv.27758
DATA AVAILABILITY STATEMENT
Data sharing is not applicable.
REFERENCES
- 1. How epidemiology has shaped the COVID pandemic. Nature. 2021;589:491‐492. [DOI] [PubMed] [Google Scholar]
- 2. Nikolai LA, Meyer CB, Kremsner PG, Velavan TP. Asymptomatic SARS coronavirus 2 infection: invisible yet invincible. Int J Infect Dis. 2020;100:112‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kwok CS, Muntean EA, Mallen CD. The patient pathway review: a new method of evaluating clinical practices to understand the complexities of real‐world care. Crit Pathways in Cardiol. 2021;20:213‐219. [DOI] [PubMed] [Google Scholar]
- 4. Bennett S, Tafuro J, Mayer J, et al. Clinical features and outcomes of adults with COVID‐19: a systematic review and pooled analysis of the literature. Int J Clin Pract. 2020;75:13725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tehrani S, Killander A, Astrand P, Jakobsson J, Gille‐Johnson P. Risk factors for death in adult COVID‐19 patients: frailty predicts fatal outcome in older patients. Int J Infect Dis. 2021;102:415‐421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chinnadurai R, Ogedengbe O, Agarwal P, et al. Older age and frailty are the chief predictors of mortality in COVID‐19 patients admitted to an acute medical unit in a secondary care setting—a cohort study. BMC Geriatric. 2020;20:409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Karia R, Gupta I, Khandait H, Yadav A, Yadav A. COVID‐19 and its modes of transmission. SN Compr Clin Med. 2020: 1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lotfi M, Hamblin MR, Rezaei N. COVID‐19: Transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kwok CS, Dashti M, Tafuro J, et al. Methods to disinfect and decontaminate SARS‐CoV‐2: a systematic review of in vitro studies. Ther Adv Infect Dis. 2021;8:2049936121998548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Randolph HE, Barreiro LB. Herd immunity: understanding COVID‐19. Immunity. 2020;52:737‐741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bergwerk M, Gonen T, Lustig Y, et al. COVID‐19 breakthrough infections in vaccinated healthcare workers. N Engl J Med. 2021;385:1474‐1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable.


