Abstract
Twenty-one Salmonella and 54 Escherichia coli isolates, recovered from food animals and retail ground meats, that exhibited decreased susceptibilities to ceftiofur and ceftriaxone were shown to possess a blaCMY gene. The blaCMY-4 gene was identified in an E. coli isolate recovered from retail chicken and was further shown to be responsible for resistance to cephalothin, ampicillin, and amoxicillin-clavulanic acid and elevated MICs of ceftriaxone, cefoxitin, and ceftiofur.
Resistance to broad-spectrum cephalosporins has increased among Salmonella species over the past 2 decades (17, 20). The majority of cephalosporin-resistant Salmonella strains express an extended-spectrum β-lactamase such as TEM and SHV, that is able to hydrolyze oxyimino cephalosporins and monobactams but not cephamycins (2). However, recent reports indicate that several species of Enterobacteriaceae have acquired plasmids encoding AmpC-like β-lactamases that hydrolyze cephalosporins, as well as cephamycins such as cefoxitin and ceftriaxone (14, 20). Resistance to ceftriaxone is most commonly mediated by a cephalomycinase (CMY) encoded by the blaCMY gene (2), and 11 blaCMY sequence variants have been deposited in the GenBank database to date. Plasmid-mediated AmpC-like β-lactamases have been identified in clinical isolates of Klebsiella pneumoniae, Escherichia coli, Proteus mirabilis, and Enterobacter aerogenes in Europe and the United States and other countries (8–10, 18, 22). They have also been recently described among Salmonella isolates recovered from food animals and humans in the United States (4, 20). The source of ceftriaxone-resistant Salmonella is often not identified in human cases, but it may have been acquired through the consumption of contaminated food, particularly mishandled or undercooked foods of animal origin (5).
Ceftiofur is the only cephalosporin approved for systemic use in food-producing animals in the United States. This drug was first approved in 1988 as an injectable therapeutic agent for the treatment of acute bovine respiratory disease and has been subsequently approved for use in other food animal species, including pigs, sheep, chickens, and turkeys (4). Because ceftiofur-resistant organisms also exhibit decreased susceptibility to cephamycins and extended-spectrum cephalosporins, the use of this antimicrobial in food animals has come under increasing scrutiny as a selective agent responsible for the emergence and dissemination of ceftriaxone-resistant enteric pathogens such as Salmonella (6, 8, 20, 21). The objectives of this study were to determine the presence of cephamycinase blaCMY genes and their contribution to the decreased ceftiofur-ceftriaxone susceptibility phenotypes observed among Salmonella and E. coli isolates recovered from food animals and retail ground meats.
Eighty-one (60 E. coli and 21 Salmonella) isolates from cattle, poultry, swine, and retail meats that displayed decreased susceptibility to ceftiofur (MIC, ≥8 μg/ml) and ceftriaxone (MIC, ≥16μg/ml) were selected for study. All bacterial isolates were recovered from 1998 to 2000 in five states (Table 1). The majority of the Salmonella and E. coli isolates recovered from animals did not have a history of cephamycin or cephalosporin exposure. Primers cmy-F 5′-GACAGCCTCTTTCTCCACA-3′ and cmy-R 5′-TGGAACGAAGGCTACGTA-3′ were used in the PCR assay based on the blaCMY-2 gene sequence of K. pneumoniae (GenBank accession no. Y16784). Amplifications were carried out as described previously with 50°C as the annealing temperature (23). For each set of PCRs, cephalosporin-susceptible Salmonella enterica serotype Typhimurium CVM785 and E. coli CVM4168 were included as negative controls. Fifty-four (90%) of the E. coli isolates and all 21 of the Salmonella isolates tested possessed a blaCMY gene. The PCR-generated DNA fragments were purified and sequenced. Sequence comparisons were made using the National Center for Biotechnology Information BLAST program (1). DNA sequence analysis of 1.0-kb PCR amplicons obtained from five Salmonella and four E. coli isolates confirmed that the PCR products were blaCMY genes demonstrating 95 to 99% homology to previously reported blaCMY-2 genes in K. pneumonia and S. enterica serotype Senftenberg.
TABLE 1.
Ceftiofur-resistant bacteria used in this study and their carriage of the blaCMY gene
| Isolate(s) | No. of isolates | No. isolates with blaCMY | Source | State(s) |
|---|---|---|---|---|
| E. coli | 15 | 12 | Avian | Georgia |
| E. coli | 34 | 31 | Bovine | Michigan, North Dakota |
| E. coli | 1 | 1 | Swine | Oklahoma |
| E. coli | 1 | 1 | Ground beef | Maryland |
| E. coli | 9 | 9 | Ground chicken | Maryland |
| All E. coli | 60 | 54 | ||
| Salmonella | 3 | 3 | Bovine | Michigan |
| Salmonella | 6 | 6 | Ground beef | Maryland |
| Salmonella | 2 | 2 | Ground chicken | Maryland |
| Salmonella | 10 | 10 | Ground turkey | Maryland |
| All Salmonella | 21 | 21 | ||
| Total | 81 | 75 |
Conjugation studies were conducted to determine whether ceftriaxone-ceftiofur resistance is transferable between bacterial strains. S. enterica serotype Agona CVM1132 (from ground beef), E. coli CVM1320 (from ground chicken), and E. coli CVM1897 (from cattle) were used as donor strains, and E. coli O157:H7 strains CVM 990 and JM263 were used as recipient strains. Ceftiofur (16 μg/ml) and ceftriaxone (64 μg/ml) were used as counterselective agents for donor strains, and kanamycin (64 μg/ml) and nalidixic acid (100 μg/ml) were used as selective agents for recipient strains CVM 990 and JM263, respectively. Transconjugants were confirmed as E. coli O157:H7 by a latex agglutination test (Unipath, Oxoid Division, Ogdensburg, N.Y.). Antimicrobial MICs were determined by using the Sensititre automated antimicrobial susceptibility system (Trek Diagnostic Systems, Westlake, Ohio) and interpreted in accordance with the NCCLS guidelines for broth microdilution methods using recommended quality control organisms (12, 13).
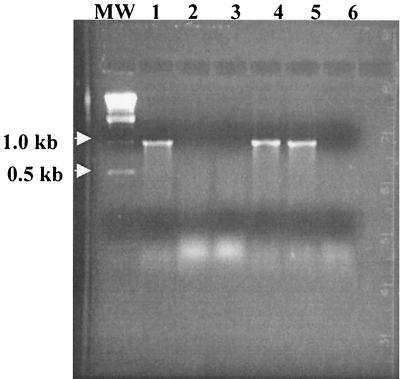
E. coli CVM1320 transferred the ceftriaxone-ceftiofur resistance phenotype to two E. coli O157:H7 strains, CVM990 and JM263. However, S. enterica serotype Agona CVM1132 and E. coli CVM1897 were not able to transfer the resistance phenotype to recipient strains. Transconjugant 1320/990 acquired resistance to ceftriaxone and ceftiofur and other β-lactams, including ampicillin, amoxicillin-clavulanic acid, cephalothin, and cefoxitin (Table 2). Transconjugant 1320/263 exhibited resistance to ceftriaxone, ceftiofur, ampicillin, and amoxicillin. Resistance to cefoxitin and cephalothin could not be measured because JM263 was resistant to these two antimicrobials prior to the conjugation experiments. Additionally, for both transconjugants, the MICs of ceftriaxone and ceftiofur were increased compared to those for the wild-type donor strains. Transfer of the blaCMY gene to the transconjugants was confirmed by PCR analysis (Fig. 1). Interestingly, the MICs of ceftiofur and ceftriaxone for the transconjugants were two- to fourfold higher than those for the donor strain. This may be due to synergism with resident β-lactamases present in the recipient strains, as chromosome-encoded β-lactamases are present in most gram-negative bacteria and these enzymes are often expressed at low levels (22). On two occasions, conjugal transfer of cephalosporin resistance could not be achieved with E. coli CVM1897 and S. enterica serotype Agona CVM1132 as donors. This may be due to integration of the blaCMY genes in the chromosome or their inclusion on nonconjugative plasmids.
TABLE 2.
Antimicrobial susceptibility profiles of E. coli strains used in conjugation and expression experimentsa
| Strain | Designation | MIC (μg/ml)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amo | Amp | Cef | Cet | Cep | Fox | Cml | Kan | Nal | Str | Sul | Tet | ||
| CVM1320 | Donor | >32 | >32 | 8 | 16 | >32 | >32 | ≤4 | ≤16 | ≤4 | 128 | ≤128 | >32 |
| CVM990 | Recipient | 4 | 4 | ≤0.5 | ≤0.25 | 8 | ≤4 | ≤4 | >64 | ≤4 | >256 | >512 | >32 |
| 1320/990 | Transconjugant | >32 | >32 | >16 | 64 | >32 | >32 | 8 | >64 | ≤4 | >256 | >512 | >32 |
| JM263 | Recipient | 8 | 8 | 1 | ≤0.25 | 32 | 32 | 32 | ≤16 | >256 | ≤32 | ≤128 | 8 |
| 1320/263 | Transconjugant | >32 | >32 | >16 | 64 | >32 | 32 | ≤16 | >256 | ≤32 | ≤128 | 8 | |
| BL21(DE3)pLysS | Host cell | 2 | ≤2 | ≤0.5 | ≤0.25 | 2 | ≤4 | >32 | ≤16 | ≤4 | ≤32 | ≤128 | ≤4 |
| BL21(DE3)pLysS + pET34b | Host cell + vector | 2 | ≤2 | ≤0.5 | ≤0.25 | 2 | ≤4 | >32 | >64 | ≤4 | ≤32 | ≤128 | ≤4 |
| BL21 (DE3)pLysS + pET34b-cmy | Transformant | >32 | >32 | 8 | 4 | >32 | 16 | >32 | >64 | ≤4 | ≤32 | ≤128 | ≤4 |
Amo, amoxicillin-clavulanic acid; Amp, ampicillin; Cef, ceftiofur; Cet, ceftriaxone; Cep, cephalothin; Fox, cefoxitin; Cml, chloramphenicol; Kan, kanamycin; Nal, nalidixic acid; Str, streptomycin; Sul, sulfamethoxazole; Tet, tetracycline. All isolates were susceptible to amikacin, apramycin, ciprofloxacin, gentamicin, and trimethoprim-sulfamethoxazole. β-Lactam antimicrobials are bolded and italicized. MICs were determined via broth microdilution methods in accordance with NCCLS guidelines (12, 13). Resistance is indicated by boldface values.
FIG. 1.
PCR amplifications of the blaCMY gene in donor E. coli CVM1320 (lane 1), recipients E. coli O157: H7 CVM990 and JM263 (lanes 2 and 3), transconjugants 1320/990 and 1320/263 (lanes 4 and 5), and negative control S. enterica serotype Typhimurium CVM785 (lane 6), which were used in conjugation experiments. Lane MW contained molecular size standards.
Conjugation experiments showed that two transconjugants (1320/990 and 1320/263) acquired resistance to all six of the β-lactam antimicrobials tested. Cloning and expression experiments were then performed in order to determine if the blaCMY gene was solely responsible for the resistance phenotype observed in the transconjugants. The entire 1,146-bp blaCMY gene from CVM1320 was amplified with primers cmy-F-exp (5′-KpnI- BamHI-GGATCCTAGGATCCATGATGAAAAAATCGT-3′) and cmy-R-exp, (5′-SacI-HindIII-EcoRI-GAGCTCAAGCTTGAATTCTTATTGCAGCTTTTC-3′) by PCR. The underlined sequences indicate restriction sites. The PCR product was digested with BamHI and EcoRI, purified, and cloned into expression vector pET34b+ (Novagen, Inc., Madison, Wis.). Recombinants were then introduced into E. coli BL21(DE3)pLysS (Novagen), and transformants were selected on tryptic soy agar supplemented with kanamycin (30 μg/ml) and either ceftriaxone (16 μg/ml) or ceftiofur (8 μg/ml).
Transformants from the expression experiments displayed resistance or decreased susceptibility to the six β-lactams tested compared to the host strain, BL21(DE3)pLysS, or the host strain possessing expression vector pET34b+ alone (Table 2). For transformants, the MICs of cefoxitin increased 4-fold and those of ceftriaxone, ceftiofur, amoxicillin-clavulanic acid, ampicillin, and cephalothin increased up to 16-fold. The MICs of amoxicillin-clavulanic acid, ampicillin, ceftiofur, and cephalothin for the transformants were similar to those for wild-type donor strain CVM1320; however, the MICs of cefoxitin and ceftriaxone were two- to fourfold lower (Table 2). This interesting observation, which has also been reported by other investigators (3), may be due, in part, to the dissimilar genetic backgrounds of the recipient and cloning host strains, resulting in decreased β-lactamase expression and activity relative to that of the wild-type strain.
The blaCMY gene insert of the expression experiments was sequenced by using flanking primers (pET34F [5′-ATCTGGGTACCGATGACGACGACAA-3] and pET34R [5′-ATCAATTAGTGGTGGTGGTGGTGGT-3′]) derived from the pET34b+ vector DNA sequence. DNA sequence analysis revealed that the 1,146-bp DNA insert was 100% homologous to the blaCMY-4 gene described in E. coli (16). The sequence of the retail meat E. coli blaCMY-4 gene has been assigned GenBank accession number AF420597. This gene has previously been identified in an E. coli strain from stool specimens of a leukemia patient in the United Kingdom (16) and a P. mirabilis strain from a urine sample collected from a woman in Tunisia (18). Using BLAST, it was determined that the cloned blaCMY gene also demonstrated 99.9% similarity to the blaCMY-2 gene identified in K. pneumoniae and S. enterica serotype Senftenberg and 99% similarity to the blaCMY-3 gene identified in P. mirabilis (2, 18).
The extended-spectrum cephalosporin ceftiofur has been approved in the United States for therapeutic use in animals beginning with cattle in 1988. Since its approval, ceftiofur has commonly been used for treatment of respiratory tract infections, metritis, and foot rot (20). Our findings confirm those of other investigators that Salmonella and E. coli isolates of animal and food origin that possess blaCMY genes display decreased susceptibility to ceftiofur, as well as to ceftriaxone (21). Such an association may have been a contributing factor in the development of ceftriaxone-resistant Salmonella phenotypes. Indeed, the isolation of extended-spectrum cephalosporin-resistant E. coli and Salmonella from retail ground meats presents compelling evidence for potential food-borne transmission of these resistant pathogens. Interestingly, resistance to extended-spectrum β-lactams was not associated with one particular chromosomal genotype and is most likely due to horizontal dissemination of the blaCMY genes via large, broad-host-range plasmids and/or a mobile transposon(s) (11, 21). This suggests the possibility that ceftriaxone resistance in E. coli and Salmonella arose from intraspecies transfer of broad-host-range plasmids, which has been observed for other antimicrobial resistance phenotypes (15, 19). This is in contrast to a recent report attributing aminoglycoside resistance in S. enterica serotype Typhimurium DT104 to clonal dissemination of this pathogen (7). Additionally, since the isolates in our study displayed resistance to other β-lactams, including ampicillin, amoxicillin-clavulanic acid, cephalothin, and cefoxitin, the use of any of these antimicrobials may contribute to the overall selective pressures involved in maintaining these resistance genes within enteric pathogens that are present in the animal production environment.
In summary, the present study indicates that blaCMY genes are commonly present in E. coli and Salmonella isolates of animal origin that display decreased susceptibility to ceftiofur and ceftriaxone. Additionally, blaCMY genes were shown to be transferred between bacteria through conjugation. To our knowledge, this is the first report of blaCMY-4 being detected in E. coli recovered from retail ground meats. This significant finding warrants continued surveillance for blaCMY variants in bacterial pathogens isolated from animals and animal-derived foods. Of particular importance is the fact that many of these isolates possessing blaCMY genes were recovered from animals that had no history of exposure to cephamycins and extended-spectrum cephalosporins. As the presence and expression of this gene in a bacterium result in decreased susceptibility to penicillins, cephalosporins, and cephamycin, its dissemination in E. coli and Salmonella may present future therapeutic challenges in animal and human health care.
Nucleotide sequence accession number. The sequence of the retail meat E. coli blaCMA−4 gene has been assigned GenBank accession number AF420597.
REFERENCES
- 1.Altschul S F, Madden T L, Schaffer A A, Zhang J, Zhang Z, Miller W, Lipman D J. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauernfeind A, Stemplinger I, Jungwirth R, Giamarellou H. Characterization of the plasmidic beta-lactamase CMY-2, which is responsible for cephamycin resistance. Antimicrob Agents Chemother. 1996;40:221–224. doi: 10.1128/aac.40.1.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauernfeind A, Stemplinger I, Jungwirth R, Wilhelm R, Chong Y. Comparative characterization of the cephamycinase blaCMY-1 gene and its relationship with other β-lactamase genes. Antimicrob Agents Chemother. 1996;40:1926–1930. doi: 10.1128/aac.40.8.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradford P A, Petersen P J, Fingerman I M, White D G. Characterization of expanded-spectrum cephalosporin resistance in E. coli isolates associated with bovine calf diarrhoeal disease. J Antimicrob Chemother. 1999;44:607–610. doi: 10.1093/jac/44.5.607. [DOI] [PubMed] [Google Scholar]
- 5.Dunne E F, Fey P D, Kludt P, Reporter R, Mostashari F, Ribot E, Iwen P C, Bradford P A, Angulo F J. Emergence of domestically acquired ceftriaxone-resistant Salmonella infections associated with ampC beta-lactamase. JAMA. 2000;284:3151–3156. doi: 10.1001/jama.284.24.3151. [DOI] [PubMed] [Google Scholar]
- 6.Fey P D, Safranek T J, Rupp M E, Dunne E F, Ribot E, Iwen P C, Bradford P A, Angulo F J, Hinrichs S H. Ceftriaxone-resistant Salmonella infection acquired by a child from cattle. N Engl J Med. 2000;342:1242–1249. doi: 10.1056/NEJM200004273421703. [DOI] [PubMed] [Google Scholar]
- 7.Frana T S, Carlson S A, Griffith R W. Relative distribution and conservation of genes encoding aminoglycoside-modifying enzymes in Salmonella enterica serotype Typhimurium phage type DT104. Appl Environ Microbiol. 2001;67:445–448. doi: 10.1128/AEM.67.1.445-448.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gazouli M, Sidorenko S V, Tzelepi E, Kozlova N S, Gladin D P, Tzouvelekis L S. A plasmid-mediated beta-lactamase conferring resistance to cefotaxime in a Salmonella typhimurium clone found in St Petersburg, Russia. J Antimicrob Chemother. 1998;41:119–121. doi: 10.1093/jac/41.1.119. [DOI] [PubMed] [Google Scholar]
- 9.Gazouli M, Tzelepi E, Sidorenko S V, Tzouvelekis L S. Sequence of the gene encoding a plasmid-mediated cefotaxime-hydrolyzing class A beta-lactamase (CTX-M-4): involvement of serine 237 in cephalosporin hydrolysis. Antimicrob Agents Chemother. 1998;42:1259–1262. doi: 10.1128/aac.42.5.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kesah C N, Coker A O, Alabi S A, Olukoya D K. Prevalence, antimicrobial properties and beta-lactamase production of haemolytic enterobacteria in patients with diarrhoea and urinary tract infections in Lagos, Nigeria. Cent Afr J Med. 1996;42:147–150. [PubMed] [Google Scholar]
- 11.Liebert C A, Hall R M, Summers A O. Transposon Tn21, flagship of the floating genome. Microbiol Mol Biol Rev. 1999;63:507–522. doi: 10.1128/mmbr.63.3.507-522.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NCCLS. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard. NCCLS document M7–A4. 4th ed. Wayne, Pa: NCCLS; 1997. [Google Scholar]
- 13.NCCLS. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals; approved standard. NCCLS document M31-A. 4th ed. Wayne, Pa: NCCLS; 1999. [Google Scholar]
- 14.Nordmann P. Trends in beta-lactam resistance among Enterobacteriaceae. Clin Infect Dis. 1998;27(Suppl. 1):S100–S106. doi: 10.1086/514905. [DOI] [PubMed] [Google Scholar]
- 15.Salyers A A, Amabile-Cuevas C F. Why are antibiotic resistance genes so resistant to elimination? Antimicrob Agents Chemother. 1997;41:2321–2325. doi: 10.1128/aac.41.11.2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stapleton P D, Shannon K P, French G L. Carbapenem resistance in Escherichia coli associated with plasmid-determined CMY-4 β-lactamase production and loss of an outer membrane protein. Antimicrob Agents Chemother. 1999;43:1206–1210. doi: 10.1128/aac.43.5.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Threlfall E J, Skinner J A, Graham A, Ward L R, Smith H R. Resistance to ceftriaxone and cefotaxime in non-typhoidal Salmonella enterica in England and Wales, 1998–99. J Antimicrob Chemother. 2000;46:860–862. doi: 10.1093/jac/46.5.860. [DOI] [PubMed] [Google Scholar]
- 18.Verdet C, Arlet G, Ben Redjeb S, Ben Hassen A, Lagrange P H, Philippon A. Characterisation of CMY-4, an AmpC-type plasmid-mediated beta-lactamase in a Tunisian clinical isolate of Proteus mirabilis. FEMS Microbiol Lett. 1998;169:235–240. doi: 10.1111/j.1574-6968.1998.tb13323.x. [DOI] [PubMed] [Google Scholar]
- 19.White D G, Hudson C, Maurer J J, Ayers S, Zhao S, Lee M D, Bolton L, Foley T, Sherwood J. Characterization of chloramphenicol and florfenicol resistance in Escherichia coli associated with bovine diarrhea. J Clin Microbiol. 2000;38:4593–4598. doi: 10.1128/jcm.38.12.4593-4598.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winokur P L, Brueggemann A, DeSalvo D L, Hoffmann L, Apley M D, Uhlenhopp E K, Pfaller M A, Doern G V. Animal and human multidrug-resistant, cephalosporin-resistant Salmonella isolates expressing a plasmid-mediated CMY-2 AmpC β-lactamase. Antimicrob Agents Chemother. 2000;44:2777–2783. doi: 10.1128/aac.44.10.2777-2783.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Winokur P L, Vonstein D L, Hoffman L J, Uhlenhopp E K, Doern G V. Evidence for transfer of CMY-2 AmpC β-lactamase plasmids between Escherichia coli and Salmonella isolates from food animals and humans. Antimicrob Agents Chemother. 2001;45:2716–2722. doi: 10.1128/AAC.45.10.2716-2722.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu S W, Dornbusch K, Kronvall G, Norgren M. Characterization and nucleotide sequence of a Klebsiella oxytoca cryptic plasmid encoding a CMY-type β-lactamase: confirmation that the plasmid-mediated cephamycinase originated from the Citrobacter freundii AmpC β-lactamase. Antimicrob Agents Chemother. 1999;43:1350–1357. doi: 10.1128/aac.43.6.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao S, White D G, Ge B, Ayers S, Friedman S, English L, Wagner D, Gaines S, Meng J. Identification and characterization of integron-mediated antibiotic resistance among Shiga toxin-producing Escherichia coli isolates. Appl Environ Microbiol. 2001;67:1558–1564. doi: 10.1128/AEM.67.4.1558-1564.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]