Abstract
Background:
Epithelial lacrimal gland tumours are uncommon orbital tumours and are not widely reported among African populations.
Objective:
This study aimed to describe the clinicopathological features, treatment, and outcomes of epithelial lacrimal gland tumours in Nigeria.
Design:
Retrospective case series.
Setting:
Ocular Oncology Unit, Ophthalmology Department and Pathology Department of University College Hospital, Ibadan, Nigeria.
Materials and Methods:
A review of the medical records of all patients with histopathological diagnoses of epithelial lacrimal gland tumours managed at a tertiary health facility, southwestern Nigeria over 11.5 years was carried out.
Results:
Eighteen patients with equal numbers of men and women, and mean age at presentation of 42.2 ± 15.7 years (median 42 years, range 17–70 years) were managed. All patients presented with orbital swelling and had nonaxial proptosis with palpable firm to hard mass in the superotemporal quadrant of the orbit. The mean duration of symptoms was 42.2 ± 38.6 months (median 24 months, range 3–120 months). Visual acuity was <3/60 at presentation in eight (44.4%) of the affected eyes. Thirteen (72.2%) patients underwent orbitotomy and tumour excision, while five (27.8%) patients had orbital exenteration, and two of whom (11.1%) had combined orbital exenteration and craniotomy. Histopathological examination of the specimens revealed pleomorphic adenoma in nine (50.0%) patients, low-grade mucoepidermoid carcinoma in three (16.7%) patients, high-grade mucoepidermoid carcinoma in two (11.1%) patients, adenoid cystic carcinoma in three (16.7%) patients, and adenocarcinoma “not otherwise specified” in one (5.6%) patient. Mortality was reported in four (44.4%) of nine patients with malignant tumours, while no mortality was noted in the patients with benign pleomorphic adenoma. The mean follow-up period for the patients was 28.9 months (median, 4.5 months; range, 2–140 months).
Conclusion:
The main presenting symptom of epithelial lacrimal gland tumours in our patients was an orbital mass and the most common clinical finding, in addition to the orbital mass, was nonaxial proptosis. The tumours were equally divided into benign and malignant lesions in our studied population. Pleomorphic adenoma was the only benign tumour while mucoepidermoid carcinoma was the commonest malignant lesion. Orbital exenteration was performed in a high proportion of our patients and high mortality was noted among patients with malignant tumours.
Keywords: Lacrimal tumours, mucoepidermoid carcinoma, orbital exenteration, orbitotomy, pleomorphic adenoma
Abstrait
Contexte:
Les tumeurs épithéliales des glandes lacrymales sont des tumeurs orbitales rares et ne sont pas largement rapportées parmi les populations africaines.
Objectif:
Cette étude visait à décrire les caractéristiques clinico-pathologiques, le traitement et le résultat des tumeurs épithéliales des glandes lacrymales au Nigeria.
Conception:
Série de cas rétrospectifs.
Cadre:
Unité d’oncologie oculaire, département d’ophtalmologie et département de pathologie du Collège Hospitalier Universitaire, Ibadan, Nigéria.
Méthode:
Un examen des dossiers médicaux de tous les patients présentant des diagnostics histopathologiques de tumeurs épithéliales des glandes lacrymales gérées dans un établissement de santé tertiaire du sud-ouest du Nigéria pendant 11,5 ans a été effectué.
Résultats:
Dix - huit patients avec un nombre égal d’hommes et de femmes et un âge moyen à la présentation de 42,2 ± 15,7 ans (médian de 42 ans, intervalle de 17 à 70 ans) ont été pris en charge. Tous les patients présentaient un gonflement orbital et avait l’exophtalmie non-axiale avec ferme à dur masse palpable dans le quadrant temporel supérieur de l’orbite. La durée moyenne des symptômes était de 42,2 ± 38,6 mois (médiane de 24 mois, intervalle de 3 à 120 mois). L’acuité visuelle était <3/60 à la présentation dans huit (44,4%) des yeux atteints. Treize (72,2%) patients ont subi une orbitotomie et une excision de la tumeur, tandis que cinq (27,8%) patients avaient une exentération orbitaire, dont deux (11,1%) avaient l’exentération orbitale et la craniotomie combinées. L’examen histopathologique des échantillons a révélé un adénome pléomorphe chez neuf (50,0%) patients, un carcinome muco-épidermoïde de bas grade chez trois (16,7%) patients, un carcinome muco-épidermoïde de haut grade chez deux (11,1%) patients, un carcinome adénoïde kystique chez trois (16,7%) patients et adénocarcinome “non autrement spécifié” (NOS) chez un patient (5,6%). La mortalité a été rapportée chez quatre (44,4%) des neuf patients atteints de tumeurs malignes, alors qu’aucune mortalité n’a été notée chez les patients présentant un adénome pléomorphe bénin. La période moyenne de suivi des patients était de 28,9 mois (médiane de 4,5 mois; intervalle de 2 à 140 mois).
Conclusion:
Le principal symptôme de présentation des tumeurs épithéliales des glandes lacrymales chez nos patients était une masse orbitale et le résultat clinique le plus courant, en plus de la masse orbitale, était une exophtalmie non axiale. Les tumeurs étaient également divisées entre les lésions bénignes et malignes dans notre population étudiée. L’adénome pléomorphe était la seule tumeur bénigne tandis que le carcinome muco-épidermoïde était la lésion maligne la plus courante. Une exentération orbitale a été réalisée chez une forte proportion de nos patients et une mortalité élevée a été notée chez les patients atteints de tumeurs malignes.
Mots-clés: Adénome pléomorphe, carcinome muco-épidermoïde, exentération orbitale, orbitotomie, tumeur lacrymale
Introduction
Lacrimal gland swellings can be classified as inflammatory, lymphoproliferative, primary epithelial tumours, or malignant nonepithelial tumours.[1] The primary epithelial tumours include benign mixed tumour (pleomorphic adenoma), adenoid cystic carcinoma, primary adenocarcinoma, malignant mixed tumors (pleomorphic adenocarcinoma), and mucoepidermoid carcinoma.[2] Metastatic lacrimal gland carcinomas are rare and can arise from breast or lung carcinomas.[3] The prevalence of these lesions varies in different studies as they account for 7–9% of orbital tumours as reported by some authors,[4] whereas they make up 5–13% of all surgical specimens from the orbit as reported by other authors.[5] The typical presentation of patients with epithelial lacrimal gland tumours includes protrusion in the temporal superior region of the anterior orbit, displacement of the globe into the nasal inferior direction, proptosis dependent on tumour extension into the retrobulbar space, and restriction of ocular movements.[6] Specific diagnosis is at histopathological examination of the excised tumour, hence, treatment of suspected epithelial lacrimal gland tumour is surgical excision aimed at complete excision with intact capsule to avoid seeding of residual tissue that can lead to tumour recurrence or malignant transformation and poor prognosis.[6] Lacrimal gland tumours are traditionally broadly categorised as 50% epithelial and 50% nonepithelial in origin;[4] however, recent studies[1,5] have reported that the proportion of epithelial lacrimal gland tumours is lower than that previously documented. The proportion of benign epithelial tumours to malignant tumours was reported by Bernardini et al.[7] to be 55% benign and 45% malignant, whereas some authors[8,9] reported a higher proportion of benign tumours among Asians compared with Caucasians, thus, suggesting a racial variation in the pattern of epidemiological distribution of these tumours. Approximately 60% of the malignant tumours are adenoid cystic carcinoma, 20% pleomorphic adenocarcinoma, 10% primary adenocarcinoma, 5% mucoepidermoid carcinoma, and 5% miscellaneous malignant epithelial tumours.[2] There is a paucity of reports on lacrimal gland tumours among indigenous black populations. The study thus aimed to describe the clinicopathological features, treatment, and outcomes of epithelial lacrimal gland tumours among a homogenous black African population.
Patients and Methods
In this retrospective, observational case series, all patients with histopathological diagnoses of epithelial lacrimal gland tumours managed at the Oculoplasty and Ocular Oncology Unit of the Eye Clinic, University College Hospital, Ibadan, Nigeria, between October 2008 and March 2020 were studied. Records were obtained from the Eye Clinic, Ward and Theatre register, and the register at the Pathology Department. University College Hospital is the foremost tertiary institution in Nigeria with facilities for surgical and radiation treatment of orbital tumours, hence, these patients were referred from the six geopolitical zones of the country. All patients had computed tomography (CT) scan done preoperatively to evaluate the extent of the tumour and integrity of the orbital walls. Staging of malignant tumours was not done.
They were all operated on by a single ophthalmic plastic surgeon in conjunction with neurosurgeons when indicated. Patients who presented with orbital tumours and had normal orbital anatomic structure underwent orbitotomy with tumuor excision, whereas those with large tumuors, prolapsed globe with keratinised ocular surface, and distorted orbital anatomy underwent orbital exenteration, and patients with intracranial extension of the tumour had orbital exenteration in combination with craniotomy. They were subsequently reviewed by the radiation oncologist and offered adjuvant therapy based on their histological diagnoses. Data retrieved from the medical records included patients’ age, gender, presenting symptoms and their duration, clinical features, radiological investigation findings, operative findings, histopathological diagnoses, postoperative management, and outcomes. Patients found to have defaulted their postoperative treatment and clinic visits were contacted via calls to their mobile phones or those of their next of kin to ascertain their treatment outcomes and current status. For the histopathological analyses, slides of hematoxylin and eosin-stained sections of the specimen were retrieved and reviewed by a single histopathologist. The classification used in this study was the WHO histological classification of tumours of the lacrimal gland.[10] Ethical approval was obtained from the Institutional Ethical Review Committee of the hospital and the study adhered to the tenets of the Helsinki Declaration.
Statistical analysis was performed using Statistical Package for Social Sciences version 21 software (SPSS Inc, Chicago, IL, USA). Descriptive statistics such as means and SDs were used to summarise quantitative variables (with the student t-test being used to compare them), whereas categorical variables were presented as proportions and percentages.
Results
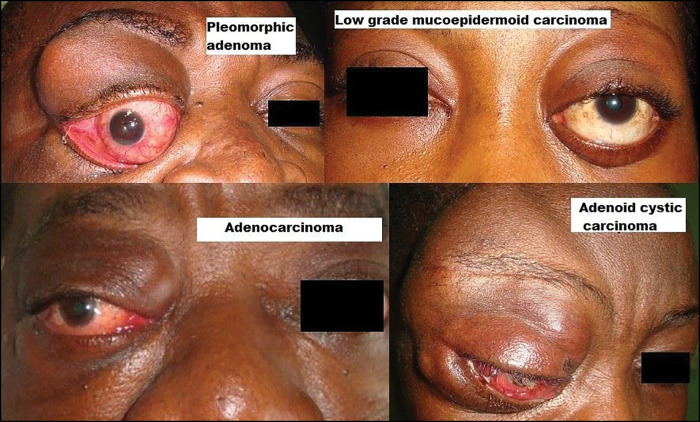
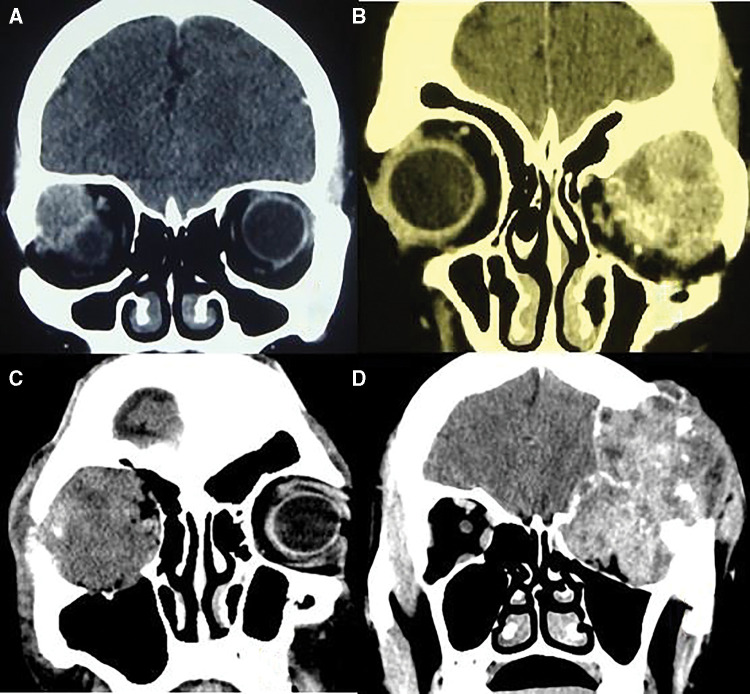
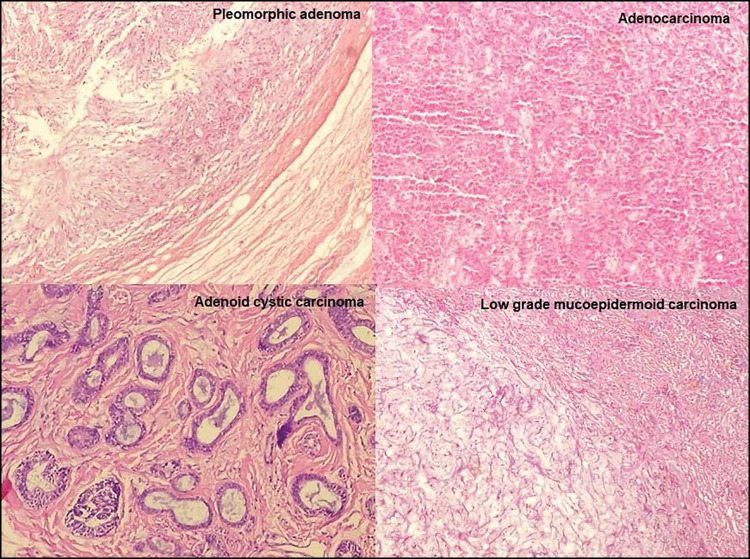
Eighteen patients, with equal numbers of men and women, were seen with epithelial lacrimal gland tumours during the study period. The mean age at presentation was 42.2 ± 15.7 years (range, 17–70 years); the mean age of patients with malignant tumours was 36.3 ± 15.0 years, while that of patients with pleomorphic adenoma was 47.8 ± 16.0 years, the difference not being statistically significant (P = 0.564) [Table 1]. The commonest clinical presentation was nonaxial proptosis, with a palpable firm to hard mass in the superotemporal quadrant of the orbit in all the patients, while four patients with malignant tumours had complaints of pain [Figure 1 and Table 2]. The mean duration of symptoms was 42.2 ± 38.6 months, (median 24 months, range 3–120 months). The right orbit was affected in 13 (72.2%) patients and the left orbit in 5 (27.8%); no bilateral cases were seen. At presentation, eight (44.4%) patients were blind (visual acuity <3/60) in the affected eye and were noted to have severe proptosis with ocular surface keratinisation and corneal haziness which precluded detailed fundal examination [Table 1]. CT scan done showed the sizes and extent of the tumours, the integrity of the orbital walls, and intracranial tumour extension in two patients [Figure 2]. Thirteen (72.2%) patients underwent orbitotomy which was combined with craniotomy in one patient, whereas five (27.8%) patients had orbital exenteration which was combined with craniotomy in one patient [Table 1]. Histopathological examination of the specimens revealed pleomorphic adenoma in nine (50.0%) patients, low-grade mucoepidermoid carcinoma in three (16.7%) patients, adenoid cystic carcinoma in three (16.7%) patients, high-grade mucoepidermoid carcinoma in 2 (11.1%) patients, and adenocarcinoma “not otherwise specified” (NOS) in one (5.6%) patient. Histopathology photomicrographs are shown in Figure 3.
Table 1.
Demographic characteristics, clinical and histological features in the 18 cases
| Cases | Age (years) | Sex | Laterality | VA | Procedure | Histological diagnosis | Adjuvant treatment | Outcomes |
|---|---|---|---|---|---|---|---|---|
| 1 | 25 | M | Right | NLP | Exenteration | Pleom adenoma | Not Ind | No recurrence |
| 2 | 25 | M | Right | 6/5 | Orbitotomy | Pleom adenoma | Not Ind | No recurrence |
| 3 | 56 | M | Right | 6/5 | Orbitotomy | Pleom adenoma | Not Ind | No recurrence |
| 4 | 45 | M | Right | 6/18 | Orbitotomy | Pleom adenoma | Not Ind | Recurrent tumour |
| 5 | 57 | M | Right | HM | Exenteration | Pleom adenoma | Not Ind | Recurrent tumour |
| 6 | 52 | F | Right | HM | Orbitotomy | Pleom adenoma | Not Ind | No recurrence |
| 7 | 37 | F | Right | 6/12 | Orbitotomy | Pleom adenoma | Not Ind | No recurrence |
| 8 | 46 | M | Right | NLP | Exenteration | High-grade MEC | Not completed | Dead |
| 9 | 18 | M | Left | 6/5 | Orbitotomy | Low-grade MEC | Nil | No recurrence |
| 10 | 17 | F | Left | 6/5 | Orbitotomy | Low-grade MEC | Completed | No recurrence |
| 11 | 50 | F | Right | NLP | Exenteration + craniotomy | Adenoid cystic Ca | Abandoned | Dead |
| 12 | 30 | M | Right | NLP | Exenteration | Adenoid cystic Ca | Abandoned | Dead |
| 13 | 59 | M | Right | LP | Orbitotomy + craniotomy | Adenocarcinoma “NOS” | Completed | Dead |
| 14 | 38 | F | Left | 6/9 | Orbitotomy | Low-grade MEC | Nil | No recurrence |
| 15 | 70 | F | Left | 6/6 | Orbitotomy | Pleom adenoma | Not Ind | No recurrence |
| 16 | 63 | F | Right | 6/12 | Orbitotomy | Pleom adenoma | Not Ind | No recurrence |
| 17 | 32 | F | Left | CF | Orbitotomy | High-grade MEC | Yet to start | No recurrence |
| 18 | 39 | F | Right | 6/60 | Orbitotomy | Adenoid cystic Ca | On treatment | Recurrent tumour |
Yrs = years, VA = visual acuity, M = male, F = female, NLP =nil light perception, HM = hand motion, LP = light perception, CF = counting finger, Pleom = pleomorphic, MEC = mucoepidermoid carcinoma, Ca = carcinoma, NOS = not otherwise specified, Not Ind = not indicated
Figure 1.
Clinical pictures of some patients with different epithelial lacrimal gland tumours. Pleomorphic adenoma: Clinical picture of a 45-year-old man presenting with superotemporal mass in the right orbit and nonaxial proptosis with inferonasal globe displacement. Low-grade mucoepidermoid carcinoma: Clinical picture of a 38-year-old woman presenting with left firm superotemporal orbital mass and nonaxial proptosis. Adenocarcinoma: Clinical picture of a 59-year-old man presenting with right superotemporal orbital fullness and palpable mass extending to superonasal orbit and nonaxial proptosis. Adenoid cystic carcinoma: Clinical picture of a 50-year-old woman presenting with right superotemporal orbital mass with intracranial extension
Table 2.
Presenting features in the 18 cases*
| Presenting clinical features | Frequency | Percent |
|---|---|---|
| Symptoms | ||
| Orbital mass | 18 | 100 |
| Loss of vision | 8 | 44.4 |
| Pain | 4 | 22.2 |
| Bleeding | 1 | 5.6 |
| Signs | ||
| Proptosis | 18 | 100 |
| Blindness | 8 | 44.4 |
| Corneal opacity | 4 | 22.2 |
| Ptosis | 1 | 5.6 |
*Some patients had more than one symptom or sign
Figure 2.
Computed tomography scan slides of some patients with epithelial lacrimal gland tumours. A: Coronal slide of a patient with pleomorphic adenoma showing a circumscribed isodense soft tissue mass in the right superotemporal orbit with inferomedial globe displacement and no bony changes. B: Coronal slide of a patient with high-grade mucoepidermoid carcinoma showing a circumscribed mixed density soft tissue mass in the left superotemporal orbit and no bony destruction. C: Coronal slide of a patient with adenoid cystic carcinoma showing a circumscribed mixed density soft tissue mass filling the right orbit with and erosion of the lateral orbital wall. D: Coronal slide of a patient with adenoid cystic carcinoma showing a mixed density mass filling the left orbit with destruction of the orbital roof and intracranial tumour extension
Figure 3.
Histopathological micrographs of hematoxylin and eosin slides (x40) of epithelial lacrimal gland tumours. Pleomorphic adenoma: Section shows benign proliferating cells surrounded by an apparent intact capsule and background chondromyxoid stroma. Adenocarcinoma: Section shows focus of tumour cells in sheets, each cell having fairly enlarged pleomorphic nuclei. Adenoid cystic carcinoma: Comedo type adenoid cystic carcinoma section shows clusters of cells forming the comedo pattern with tubules containing mucin. Low-grade mucoepidermoid carcinoma: Section shows predominantly mucin producing, clear and intermediate cells
Two (22.2%) of the nine patients with pleomorphic adenoma developed tumour recurrence 5 and 6 years, respectively, after their primary surgical tumour excision, and the excised recurrent tumours were confirmed to be pleomorphic adenoma with no malignant transformation on histopathological examination. All nine patients were alive at a mean follow-up period of 82.4 ± 34.5 months.
Mortality was reported in four (44.4%) of the nine patients with malignancies (two patients with adenoid cystic carcinoma, and one patient each with high-grade mucoepidermoid carcinoma and adenocarcinoma “NOS”) [Table 1]. One of the two patients with high-grade mucoepidermoid carcinoma died from metastatic disease while undergoing adjuvant treatment, whereas the second patient had not commenced adjuvant treatment because of financial constraints and she had no tumour recurrence 6 months after surgery. One of the three patients with low-grade mucoepidermoid carcinoma received adjuvant treatment at the instance of the radiation oncologist, whereas the other two patients did not receive any adjuvant treatment, and all three patients were alive with no recurrent tumour at a mean follow-up of 58.7 ± 33.8 months (range, 30–96 months). The three patients with adenoid cystic carcinoma presented to our facility after an average of 48 months of noticing gradual protrusion of the eyeball with one patient having intracranial tumour extension on CT scan at presentation. He subsequently underwent orbital exenteration and craniotomy, whereas the other two patients had orbitotomy with tumour excision and orbital exenteration, respectively. Postoperatively, two of the three patients abandoned further adjuvant treatment and reportedly died from the recurrent metastatic disease within 1 year of surgery, whereas the third patient had a 4-month delay before the start of chemotherapy because of financial constraints, and developed gradual tumour recurrence. She is currently undergoing chemotherapy with 5-fluorouracil and cisplatin.
The mean follow-up period for all the patients was 28.9 months (median, 4.5 months; range, 2–140 months).
Discussion
Epithelial lacrimal gland tumours occur less frequently than inflammatory and lymphoid lesions of the gland.[1,5] The mean age of the patients in our series is similar to the findings of Shields et al.,[2] and the mean age of patients with malignant tumours (36.3 ± 15.0 years) was noted to be lower than those with pleomorphic adenoma (47.8 ± 16.0 years), though the difference was not statistically significant. There are variations in the reports on gender distribution of patients with epithelial lacrimal gland tumours in different studies. Equal gender distribution of patients was noted in our series similar to some studies,[11,12] whereas a male preponderance was reported by Wright et al.[13] and female preponderance by Shields et al.[2]
Typically, patients with benign epithelial lacrimal gland tumours present with slow-growing, painless, palpable superotemporal orbital mass with inferonasal nonaxial proptosis, as observed in our patients.[11,12,13] Occurrence of pain with a lacrimal gland swelling has been associated with clinical suspicion of malignancy[11,13] and it is noted that the four patients with complaints of pain in this series had malignant tumours (one patient each with high-grade mucoepidermoid carcinoma, low-grade mucoepidermoid carcinoma, adenoid cystic carcinoma, and adenocarcinoma). About half of our patients were blind (acuity <3/60) in the affected eye at presentation and this was noted to be due to ocular surface keratinisation and corneal haziness in the proposed globe and presumably optic nerve compromise in those with severe proptosis. Also, about a quarter of our patients underwent orbital exenteration (two patients had pleomorphic adenoma, two patients had adenoid cystic carcinoma, and one patient had high-grade mucoepidermoid carcinoma). Orbital exenteration was indicated in this group of patients due to the severe proptosis, grossly distorted orbital anatomic structure, and nil potential for vision. The delay in presentation of our patients (average duration of symptoms, 42.2 ± 38.6 months) presumably contributed to the observed morbidity.
Half of the patients in this series had pleomorphic adenoma similar to the report of Wright et al.[13] Other authors[1,7,14] have reported pleomorphic adenoma as the most common epithelial lacrimal gland tumour. However, possibly because of referral bias Santos et al.[12] reported a higher proportion of malignant tumours in their study. About one-fifth of the patients with pleomorphic adenoma in this series developed tumour recurrence. Recurrence following excision of pleomorphic adenoma has been associated with incomplete excision of the tumour, breach of its pseudocapsule at primary surgery, or gross attenuation of the pseudocapsule observed at histopathological examination of the mass.[15,16] Recurrences have been documented up to 15 years after excision hence, a long-term follow-up of patients with pleomorphic adenoma has been recommended.[16] The recurrences noted in our patients probably resulted from a breach in the pseudocapsule of the tumour at primary surgery.
Font et al.[1] in their study among Caucasians reported mucoepidermoid carcinoma as a rare tumour in comparison with other malignant lacrimal gland tumours. The higher proportion seen in this series may represent a racial variation in the distribution of lacrimal gland tumours or possibly be attributed to the small number of cases seen. The three patients with low-grade mucoepidermoid carcinoma remained tumour-free about 5 years after surgery, whereas one of the two patients with high-grade mucoepidermoid carcinoma died within a year of treatment. Eviatar and Hornblass[17] also reported that low-grade mucoepidermoid carcinomas have a good prognosis with or without adjuvant radiation, while high-grade tumours have a poor prognosis despite extensive excision and adjuvant therapy.
Adenoid cystic carcinoma is reported as the most common malignant epithelial lacrimal gland tumour.[1,18] The three patients in our series presented after about 48 months of symptomatology with one patient already having intracranial tumour extension. Postoperatively, the two patients who abandoned further adjuvant treatment reportedly died from recurrent metastatic disease and the third patient developed tumour recurrence before the start of delayed chemotherapy. Poor outcomes had been reported in patients with adenoid cystic carcinoma irrespective of the treatment received.[1,18]
Adenocarcinomas occur less commonly than other malignant epithelial tumours of the lacrimal gland.[1,19] Patients with adenocarcinomas reportedly have a better prognosis compared to those with adenoid cystic carcinoma;[1] however, the only patient in our series presented late with a large orbital tumour and intracranial extension necessitating a craniotomy, and he died from metastatic disease despite receiving adjuvant chemotherapy and external beam irradiation.
Limitation
The challenges encountered in the treatment of a number of our patients, mostly financial constraints and distance to the facility, together with a short follow-up period make the determination of the outcome of these tumours difficult to draw conclusions on. The relatively small number of patients is also noted; however, these were referrals from different zones in the country and thus, might give a fair representation of the occurrence of these tumours in the country.
Conclusion
The main presenting symptom of epithelial lacrimal gland tumours in our patients was an orbital mass and the most common clinical finding, in addition to the orbital mass, was nonaxial proptosis. Benign pleomorphic adenoma was the most common tumour accounting for half of the cases and mucoepidermoid carcinoma was the commonest malignancy. Most patients with pleomorphic adenoma underwent orbitotomy with tumour excision, whereas orbital exenteration was more common among patients with malignant tumours. There was high mortality in patients with malignant tumours; tumour recurrence postexcision for pleomorphic adenoma also occurred.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Font RL, Smith SL, Bryan RG. Malignant epithelial tumors of the lacrimal gland: A clinicopathologic study of 21 cases. Arch Ophthalmol. 1998;116:613–6. doi: 10.1001/archopht.116.5.613. [DOI] [PubMed] [Google Scholar]
- 2.Shields CL, Shields JA, Eagle RC, Rathmell JP. Clinicopathologic review of 142 cases of lacrimal gland lesions. Ophthalmology. 1989;96:431–5. doi: 10.1016/s0161-6420(89)32873-9. [DOI] [PubMed] [Google Scholar]
- 3.Ferry AP, Font RL. Carcinoma metastatic to the orbit. Mod Probl Ophthalmol. 1975;14:377–81. [PubMed] [Google Scholar]
- 4.Goder GJ. Tumours of the lacrimal gland. Orbit. 1982;1:91–6. [Google Scholar]
- 5.Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 montgomery lecture, part 1. Ophthalmology. 2004;111:997–1008. doi: 10.1016/j.ophtha.2003.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Guo S, Song Q. The clinical and pathological development of lacrimal gland epithelial neoplasms. Rec Adv Ophthalmol. 2001;21:138–40. [Google Scholar]
- 7.Bernardini FP, Devoto MH, Croxatto JO. Epithelial tumors of the lacrimal gland: An update. Curr Opin Ophthalmol. 2008;19:409–13. doi: 10.1097/ICU.0b013e32830b13e1. [DOI] [PubMed] [Google Scholar]
- 8.Zeng J, Shi JT, Li B, Sun XL, An YZ, Li LQ, et al. Epithelial tumors of the lacrimal gland in the Chinese: A clinicopathologic study of 298 patients. Graefes Arch Clin Exp Ophthalmol. 2010;248:1345–9. doi: 10.1007/s00417-010-1349-2. [DOI] [PubMed] [Google Scholar]
- 9.Chawla B, Kashyap S, Sen S, Bajaj MS, Pushker N, Gupta K, et al. Clinicopathologic review of epithelial tumors of the lacrimal gland. Ophthalmic Plast Reconstr Surg. 2013;29:440–5. doi: 10.1097/IOP.0b013e31829f3a0c. [DOI] [PubMed] [Google Scholar]
- 10.Grossniklaus HE, Ebelhart CG, Kivela TT. Tumors of the lacrimal gland. In: Grossniklaus HE, Eberhart CG, Kivela TT, editors. WHO Classification of Tumors of the Eye. 4th ed. Lyon: IARC; 201. pp. 148–65. [Google Scholar]
- 11.Perez DE, Pires FR, Almeida OP, Kowalski LP. Epithelial lacrimal gland tumors: A clinicopathological study of 18 cases. Otolaryngol Head Neck Surg. 2006;134:321–5. doi: 10.1016/j.otohns.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Santos RR, Damasceno RW, de Pontes FS, Cursino SR, Nishiwaki-Dantas MC, Vital Filho J, et al. Ten-year follow-up of a case series of primary epithelial neoplasms of the lacrimal gland: Clinical features, surgical treatment and histopathological findings. Arq Bras Oftalmol. 2010;73:33–9. doi: 10.1590/s0004-27492010000100006. [DOI] [PubMed] [Google Scholar]
- 13.Wright JE, Rose GE, Garner A. Primary malignant neoplasms of the lacrimal gland. Br J Ophthalmol. 1992;76:401–7. doi: 10.1136/bjo.76.7.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mallen-St Clair J, Arshi A, Tajudeen B, Abemayor E, St John M. Epidemiology and treatment of lacrimal gland tumors: A population-based cohort analysis. JAMA Otolaryngol Head Neck Surg. 2014;140:1110–6. doi: 10.1001/jamaoto.2014.2846. [DOI] [PubMed] [Google Scholar]
- 15.Rose GE, Wright JE. Pleomorphic adenoma of the lacrimal gland. Br J Ophthalmol. 1992;76:395–400. doi: 10.1136/bjo.76.7.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Currie ZI, Rose GE. Long-term risk of recurrence after intact excision of pleomorphic adenomas of the lacrimal gland. Arch Ophthalmol. 2007;125:1643–6. doi: 10.1001/archopht.125.12.1643. [DOI] [PubMed] [Google Scholar]
- 17.Eviatar JA, Hornblass A. Mucoepidermoid carcinoma of the lacrimal gland: 25 cases and a review and update of the literature. Ophthalmic Plast Reconstr Surg. 1993;9:170–81. doi: 10.1097/00002341-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Esmaeli B, Ahmadi MA, Youssef A, Diba R, Amato M, Myers JN, et al. Outcomes in patients with adenoid cystic carcinoma of the lacrimal gland. Ophthalmic Plast Reconstr Surg. 2004;20:22–6. doi: 10.1097/01.IOP.0000105518.72611.4F. [DOI] [PubMed] [Google Scholar]
- 19.Heaps RS, Miller NR, Albert DM, Green WR, Vitale S. Primary adenocarcinoma of the lacrimal gland. A retrospective study. Ophthalmology. 1993;100:1856–60. doi: 10.1016/s0161-6420(93)31385-0. [DOI] [PubMed] [Google Scholar]