Abstract
Objective.
To describe the clinical and psychosocial characteristics, and their hypothesized inter-relations, as it pertains to risk for stimulant diversion (sharing, selling, or trading) for adolescents in pediatric primary care treatment for ADHD.
Method.
Baseline data for 341 adolescents in a cluster-randomized controlled trial of stimulant diversion prevention in pediatric primary care (NCT_03080259) were used to 1) characterize diversion and newly measured risk factors, 2) examine their associations with age and gender, and 3) test whether associations among risk factors were consistent with model-implied predictions. Data were collected via multi-informant electronic surveys from adolescents and parents.
Results.
Diversion was rare (1%) in this sample (Mage=15, SD=1.5, 74% male participants). Older age was associated with being approached to divert, r=.25, p<.001, and higher risk on variables pertinent to stimulant treatment, such as treatment disclosure, r=.12, p<.05, tolerance for stimulant misuse and diversion, r=.17, p<.05, and peer norms favorable to stimulant misuse and diversion (r’s=.15 to .34, p<.001). Gender differences were minimal. Variables from our conceptual model and specific to stimulants (e.g., perceived likelihood of negative consequences from diversion and schoolmate stimulant misuse/diversion) were related in multi-variable regressions to hypothesized immediate precursors of diversion (e.g., diversion intentions).
Conclusion.
Although diversion was rare for these primary care-treated adolescents, risk levels appear to be higher for older adolescents. Prevention may be most effective by capitalizing on current psychosocial strengths and discussing stimulant-specific attitudes, behaviors, and social norms before vulnerability to diversion increases in the final years of high school and into college.
Keywords: Stimulant diversion, pediatric primary care, Attention Deficit Hyperactivity Disorder
Introduction
Concern about the misuse (overuse and non-prescribed use) of stimulant medications for Attention Deficit Hyperactivity Disorder (ADHD) followed a rise in prescriptions for teens and young adults in the US.1 Non-prescribed use for cognitive enhancement and recreation has been well-documented for college students and, increasingly, adolescents.2–5 The most common source of stimulants for non-prescribed use is peers with prescriptions.6,7 Up to 24% of teens with stimulant prescriptions for ADHD have reported diverting (selling, sharing, or trading) their medication, although the rates are highly variable across studies.5,8,9 Unfortunately, very little is known about adolescent stimulant diversion and the demographic, psychosocial, and treatment risk factors that may be important to address in prevention. The current study directly addresses this knowledge gap by reporting newly measured risk factors and their predicted inter-relations for one sample of adolescents from a prevalent population: teenage patients prescribed stimulant medications for ADHD in pediatric primary care.
Few studies of adolescents have examined patient characteristics associated with stimulant diversion. The most consistently identified factor is being approached by peers to share, sell, or trade.7,10,11 In some studies, the significance of being approached as an immediate precursor to diversion has led to it being treated as an important outcome variable in its own right.11 Limited cross-sectional research with adolescents has suggested other variables that are associated with diversion: male gender, older age, White race, an absence of plans to attend college, stimulant use by peers, and typical adolescent health risk behaviors (e.g., substance use).7,12
Theoretical models of adolescent health risk behaviors have aided identification of factors that develop over time and that have direct, or indirect, associations with the predicted behavior of interest. For research on stimulants, this type of work has only been conducted for college student stimulant misuse. Bavarian and colleagues (2014) tested a triadic model of intrapersonal, interpersonal, and broader cultural environmental factors in relation to college student misuse. Conceptually proximal, stimulant-specific factors (e.g., self-efficacy for avoiding misuse) as well as more distal health risk behavior risk factors (e.g., sensation-seeking) were associated either directly or indirectly with misuse and intentions.12 Intent to misuse, reflecting the conceptual and empirical history of behavioral intentions as a direct driver of behavior, including adolescent health risk behaviors,13 was conceptualized as an immediate precursor.
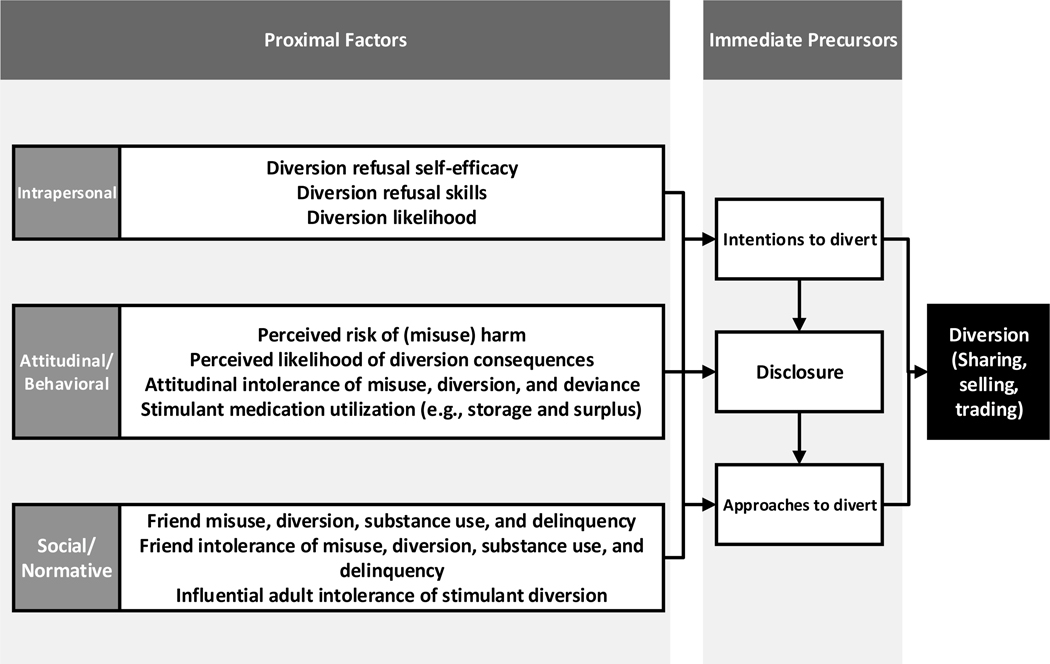
In the current study, due to the dearth of literature, we extrapolate from these findings and draw from our prior research on prevention of stimulant diversion by college students,14 to offer a conceptual model of stimulant diversion risk (see Figure 1) and associated measurement of these presumed risk factors. We make use of baseline data from a cluster-randomized clinical trial of adolescent stimulant diversion prevention to comprehensively characterize adolescent patients prescribed stimulants for ADHD with respect to hypothesized risk variables and their associations with age and gender to inform prevention timing and specificity. These variables include precursors with presumed immediate, direct influence (e.g., being approached to divert, treatment disclosure to peers, and intent to divert), and proximal risk factors in the domains of intrapersonal (e.g., refusal skill self-efficacy), attitudinal-behavioral (e.g., perceived risk of harm from misuse), and social-normative (i.e., descriptive and injunctive norms) influence. We include additional factors presumed to have distal and/or universal influences (e.g., substance use, sensation-seeking, school performance). Finally, we provide an initial test of our hypothesis that intrapersonal, attitudinal-behavioral, and social-normative proximal risk factors are related to immediate precursors of diversion behavior and examine these associations alongside those of distal/universal risk factors.
Figure 1.
Conceptual Model of Diversion Risk
Note. Selected universal health risk factors are included due to their presumed proximal influence: attitudinal intolerance of deviance, friend substance use and delinquency, friend intolerance of substance use and delinquency. Other distal and/or universal health risk factors (e.g., sensation-seeking, religiosity) are excluded from the figure for simplified presentation (see Supplement 1, Table 2, and Results).
Method
Overview
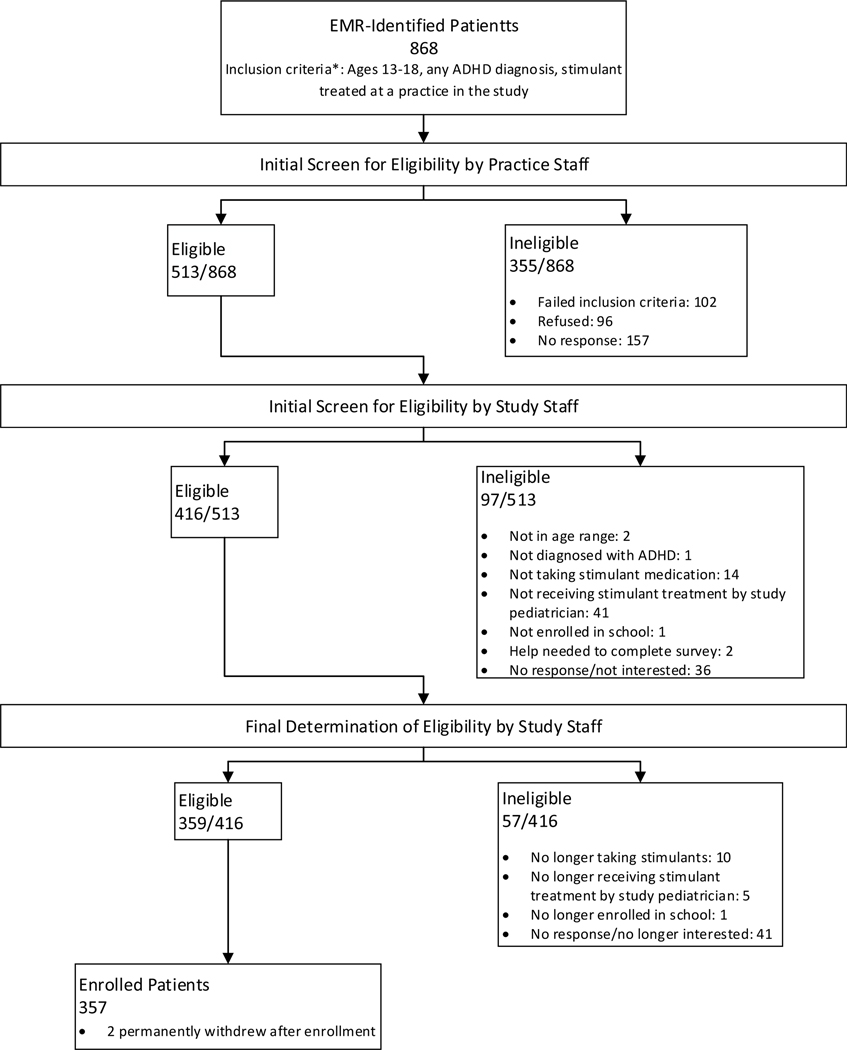
This study is based on 357 adolescent patients participating in a randomized controlled trial (RCT) of a stimulant diversion prevention workshop administered to pediatric primary care providers and their staff (ClinicalTrials.gov NCT_03080259). Analyses for this study made use of the baseline data collected from the patients and their parents prior to randomization of practices. We recruited patients from seven practices within 30 miles of the University of Pittsburgh. Figure 2 illustrates the flow of recruitment.
Figure 2.
Flow of Participant Recruitment
Note. EMR = Electronic Medical Record. In addition to confirming medical record-identified inclusion criteria (age, ADHD diagnosis, stimulant-treated for ADHD at practice), practice staff screened for the following exclusion criteria: sibling in the study, stimulant prescribed by a psychiatrist outside of the practice, home-schooled, no legal parent or guardian who could consent to participate, unable to complete survey without parent/guardian assistance.
Patient recruitment
Patients were identified from the medical records of the enrolled pediatric practices and initially contacted by practice staff. Confirmation of eligibility and enrollment was completed by research staff. Parents and patients provided informed consent to participate that emphasized confidentiality from one another’s reports and from their providers, bolstered by a NIDA-issued Certificate of Confidentiality. Parents also provided consent for the research team to communicate directly with the patient (separate emails and mobile phone numbers obtained). The study was approved by the University of Pittsburgh Human Research Protection Office.
Of the 357 enrolled adolescents, 341 provided baseline data (see Table 1). Three-quarters identified as male gender, 74%; mean (and median) age was 15 years. Two-thirds of parents were college-educated and mean (as well as median) income was $75-$99K/year. Adolescent-identified race and ethnicity mirrored regional demographics of Allegheny County (13.4% Black, 2.2% two or more races, 2.2% Hispanic) despite stimulants being less often prescribed for racial and ethnic minority children.15
Table 1.
Demographics and clinical characteristics
| All (n=341) | ||
|---|---|---|
|
| ||
| Mean/% | SD | |
|
| ||
| Age | 14.97 | (1.54) |
| Gender, % male | 75% | |
| Household educationa,c | 3.55 | (0.66) |
| 1 = Less than a high school degree | 0% | |
| 2 = High school degree | 7% | |
| 3 = Some college | 28% | |
| 4 = Bachelor’s degree or higher | 64% | |
| Annual household incomeb,c | 3.72 | (1.51) |
| 1 = Less than $35,000 | 16% | |
| 2 = $35,000 - $49,999 | 8% | |
| 3 = $50,000 - $74,999 | 13% | |
| 4 = $75,000 - $99,999 | 15% | |
| 5 = $100,000 or more | 48% | |
| Race and ethnicity | ||
| White, non-Hispanic/Latinx | 80% | |
| Black, non-Hispanic/Latinx | 10% | |
| More than one race, non-Hispanic/Latinx | 4% | |
| Hispanic or Latinx | 6% | |
| History of diagnosis and treatmentc | ||
| Grade of initial ADHD diagnosis | ||
| Preschool | 10% | |
| Elementary | 69% | |
| Middle School | 14% | |
| High School | 6% | |
| Who initially diagnosed | ||
| Pediatrician | 62% | |
| Psychiatrist | 14% | |
| Psychologist | 15% | |
| Other | 9% | |
| DSM-5 symptoms for ADHDd | ||
| Inattention | 74% | |
| Hyperactivity/Impulsivity | 47% | |
| Inattention or Hyp/Impulsivity | 76% | |
| Pediatric depressive symptoms ≥ 2 SD than published averagee | 3% | |
| Pediatric anxiety symptoms ≥ 2 SD than published averagee | 1% | |
Note.
Household education is parent report of the highest level of adult education in the adolescent’s household.
Household income was parent-reported at the 6-month follow-up assessment; median household income was the same as the mean household income.
Parent report was used, 85% biological mother.
Percent meeting DSM-5 age-specific symptom count is reported: 6+ symptoms for ages 13–16 and 5+ symptoms for ages 17 and older. For each symptom, higher rating across parent and teen report was used.
Teen self-report was used.
p < .01. Tests of gender differences were analyzed using ANCOVAs and logistic regression analyses controlling for clustering within practice.
Data collection
Adolescents and one parent each (85% mothers) completed electronic surveys programmed in Qualtrics (Provo, UT). Unique survey hyperlinks were emailed to parents and adolescents separately. The high response rate, 95.5% (n=341/357), was achieved by a combination of emailing and texting after re-iterating the importance of maintaining privacy for all participants. Data were collected over eight weeks between October and December of 2016 (Cohort 1) and 2017 (Cohort 2).
Measures
Table 2 lists all variables, response scales, and alphas calculated from current study data.
Table 2.
Hypothesized diversion risk factors, sample descriptives, associations with age, and scale characteristics.
| All (n=341) | Correlation with age | Ages 13–14 (n=157) | Ages 15+ (n=194) | Scale | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Mean/% | SD | r | Mean/% | SD | Mean/% | SD | α | ||
|
| |||||||||
| Stimulant Diversion and Immediate Precursors | |||||||||
| Diversion | 1% | .03 | |||||||
| Approached to divert | 7% | .25*** | 3% | 11% | |||||
| Disclosure: # social network types who know about prescription | 1.46 | (1.63) | .12* | 1.31 | (1.54) | 1.58 | (1.69) | Count ranging from 0–6 | |
| Intentions to diverta | 1.07 | (0.24) | .10 | 1=I definitely won’t, 4=I definitely will | .81 | ||||
| Intrapersonal Proximal Factors | |||||||||
| Diversion refusal self-efficacy | 3.53 | (0.60) | .01 | 1=Very difficult, 4=Very easy | .91 | ||||
| Diversion refusal skills | 4.00 | (0.83) | .01 | 1=Definitely not, 5=Definitely | .84 | ||||
| Likelihood of diversion | 1.17 | (0.47) | .10 | 1=I definitely wouldn’t, 4=I definitely would | .97 | ||||
| Attitudinal/Behavioral Proximal Factors | |||||||||
| Perceived risk of harm | 2.95 | (0.85) | −.10 | 1=No risk, 4=Great risk | .86 | ||||
| Perceived likelihood of negative consequences of diversion if caught | 3.45 | (0.53) | −.04 | 1=Very unlikely, 4=Very likely | .91 | ||||
| Perceived likelihood of negative social consequences of diversion | 3.09 | (0.81) | .06 | 1=Very unlikely, 4=Very likely | .71 | ||||
| Attitudinal intolerance of stimulant misuse and diversion | 3.59 | (0.55) | −.17** | 3.68 | (0.49) | 3.52 | (0.59) | 1=Not wrong, 4=Very wrong | .87 |
| Medication utilization | |||||||||
| Taking an amphetamine medicationbc | 37% | .03 | |||||||
| Medication surplus | |||||||||
| Days missed medication in last month | 4.38 | (5.28) | .02 | Count ranging from 1–31 | |||||
| # Treatment windows medicated < daily (schoolyear weeks, schoolyear weekends, summer weeks, summer weekends, up to 4) | 1.06 | (1.03) | .21*** | 0.88 | (0.93) | 1.21 | (1.08) | 0=No to limited likelihood of extra pills, 4=Highest likelihood of extra pills | |
| Medication access (unprotected/unmonitored) | 35% | −.07 | |||||||
| Social/Normative Proximal Factors | |||||||||
| Friend stimulant misuse and diversion | 0.17 | (0.42) | .25*** | 0.09 | (0.27) | 0.24 | (0.50) | .84 | |
| Friend substance use | 0.43 | (0.71) | .34*** | 0.22 | (0.47) | 0.60 | (0.81) | 0=None, | .94 |
| Friend delinquency | 0.41 | (0.61) | .08 | 5=All | .81 | ||||
| Schoolmate stimulant misuse and diversion | 0.67 | (0.80) | .35*** | 0.42 | (0.67) | 0.87 | (0.84) | .87 | |
|
| |||||||||
| Friend intolerance of stimulant misuse and diversion | 4.33 | (0.78) | −.15** | 4.41 | (0.85) | 4.26 | (0.72) | .89 | |
| Friend intolerance of substance use | 4.45 | (0.80) | −.22*** | 4.56 | (0.83) | 4.35 | (0.77) | 1=Strongly approve, | .97 |
| Friend intolerance of delinquency | 4.51 | (0.74) | −.06 | 5=Strongly disapprove | .92 | ||||
| Schoolmate intolerance of stimulant diversion | 4.28 | (0.79) | −.17** | 4.41 | (0.73) | 4.17 | (0.82) | .92 | |
| Adult intolerance of stimulant diversion | 4.86 | (0.34) | .01 | .86 | |||||
| Distal and/or Universal Risk Factors | |||||||||
| ADHD symptomsd | 1.87 | (0.66) | −.15** | 1.95 | (0.68) | 1.80 | (0.65) | 0=Not at all, 3=Very much | .94 |
| ODD symptomsd | 1.41 | (0.80) | −.13* | 1.48 | (0.81) | 1.35 | (0.80) | 0=Not at all, 3=Very much | .93 |
| Impairment from ADHDd | 3.53 | (1.62) | −.05 | 0=No problem, 6=Extreme problem | |||||
| Impairment from ODDd | 3.04 | (1.66) | −.04 | 0=No problem, 6=Extreme problem | |||||
| Treatment history | |||||||||
| Age first treated with stimulantse | 9.17 | (2.91) | .28*** | 8.65 | (2.40) | 9.59 | (3.21) | ||
| Number of years treated with stimulantse | 5.75 | (2.88) | .24*** | 4.93 | (2.45) | 6.41 | (3.04) | ||
| Ever stopped taking stimulants for 6 months+ | 14% | .17** | 8% | 18% | |||||
| UPPS-P Impulsive Personality | 1=Agree strongly, 4=Disagree strongly | ||||||||
| Negative urgency | 2.36 | (0.79) | .00 | .81 | |||||
| Positive urgency | 2.34 | (0.69) | .07 | .63 | |||||
| Sensation-seeking | 2.34 | (0.65) | .06 | .59 | |||||
| (Lack of) Premeditation | 2.09 | (0.67) | −.01 | .82 | |||||
| (Lack of) Perseverance | 2.02 | (0.58) | −.01 | .71 | |||||
| Co-occurring mental health problems | |||||||||
| Depression | 47.50 | (12.01) | .18** | 46.07 | (12.03) | 48.64 | (11.91) | T-score | .96 |
| Anxiety | 43.98 | (11.01) | .05 | T-score | .92 | ||||
| Delinquencyd | 1.75 | (2.63) | .00 | Count; ranges from 0–22 | |||||
| Substance usef | 40% | .33*** | 27% | 51% | |||||
| Problems from alcohol or drug used | 13% | .17** | 8% | 16% | |||||
| Attitudinal intolerance of deviance | 3.64 | (0.50) | −.09 | 1=Not wrong, 4=Very wrong | .92 | ||||
| Religious importance | 2.33 | (1.02) | −.14* | 2.44 | (1.03) | 2.24 | (1.01) | 1=Not important, 4=Very important | |
| General functioning | |||||||||
| Average grade in school | 6.29 | (1.96) | −.02 | 1=D (69 or below) to 9=A (93–100) | |||||
| Plans to graduate from college | 3.11 | (0.87) | .07 | 1=I definitely won’t, 4=I definitely will | |||||
| Academic demand | 2.31 | (1.01) | .25*** | 2.08 | (0.94) | 2.48 | (1.03) | 1=None, 4=A great deal | |
| Social functioningg | 41.05 | (9.29) | −.03 | T-score | .94 | ||||
|
| |||||||||
| General Life Functioningd | 2.73 | (0.52) | .02 | 1=A good bit behind, 5=A good deal further ahead | .89 | ||||
Note. Teen report presented unless otherwise noted. Due to periodic missing data, sample size ranges from 331 to 341.
Intentions to divert were measured as intentions within the next 6 months.
Teen and parent report were compared; parent report was used in discrepancies.
Eight adolescents, confirmed by parent report, reported no longer taking stimulant medication at the baseline assessment.
Combined teen and parent report; higher of the two reports was used.
Parent report was used, 85% biological mother.
Ever had a drink of alcohol, been drunk, used marijuana, used tobacco, misused a prescription medication, or misused a stimulant medication.
Combined teen and parent report, lower of the two reports was used.
p < .05,
p < .01,
p < .001. Associations with age were tested with partial correlations controlling for clustering within practice.
Stimulant diversion and immediate precursors.
1) Diversion and approached to divert were assessed with a series of questions about occurrence (no/yes) in the lifetime (>6 months ago) and recently (in the last 6 months); lifetime rates (no/yes) are reported. 2) As an indicator of treatment disclosure to peers, adolescents indicated the number of social network types who knew about their prescription (6 categories, e.g., best friend, small circle of friends, classmates). 3) Intentions to divert were modeled after substance use intentions from the Monitoring the Future Study (MTF).16 Three questions asked “Do you think you will share/trade/sell ADHD prescription stimulants in the next six months (1=I definitely will not, 4=I definitely will).
Intrapersonal proximal factors
1) Diversion refusal self-efficacy and 2) skills: Adolescents rated the difficulty and likelihood of using 11 responses to diversion requests (e.g., Tell them you don’t want to, Tell them no). Items were adapted from research13,17,18 demonstrating the importance of similarly measured self-efficacy and refusal skills predicting adolescent health behaviors and intentions. 3) Likelihood of diversion was based on measures designed to capture situational specificity of intentions.19 Adolescents rated “How likely would you be to give away (9 items)/sell (9 items) your ADHD medication…” in nine situations (e.g., To a classmate who needed it to study).” One overall scale mean was used, reflecting the high intercorrelation between the “give away” and “sell” subscales, r=.90.
Attitudinal/behavioral proximal factors.
1) Perceived risk of harm, measured in the MTF to track trends in substance use attitudes,16 was adapted for non-prescribed use of stimulants once or twice, occasionally, and regularly (3 items). 2) Perceived likelihood of diversion consequences was measured with two subscales: a) Likelihood of negative consequences of diversion if caught was the mean of 18 items asking “What is the likelihood of the following things happening if you got caught sharing, selling, trading, or loaning your ADHD medication… in school? At home? In general?” (e.g. Suspension, lose scholarship opportunities); b) Likelihood of negative social consequences of diversion was measured with three items, “What is the likelihood of the following things happening if you share, sell, trade, or loan your ADHD medication?” (People I don’t know or like will ask for my medication; My reputation will be negatively affected; People will take advantage of me). 3) Attitudinal intolerance of stimulant misuse and diversion was 6 items added to the Attitudinal Intolerance of Deviance measure,20 and asked “how wrong” misuse and diversion are).20 4) Medication utilization: a) Taking amphetamine medication, versus methylphenidate, was measured with adolescent and parent report from a menu of ADHD-indicated medications. Responses were coded as taking any amphetamines (1) or taking only methylphenidate (0). In the case of discrepancies, parent report was used; b) ADHD medication surplus was two variables. The first, Days missed medication in last month, was reported by adolescents with an open-ended response. For # Treatment windows medicated, adolescents reported how they typically take their medication during the school year (2 questions) and summer (2 questions) during the week and on weekends. A count of responses across the four questions indicating pill consumption less than daily was calculated; c) Medication access was coded, based on research team consensus, as (1) potentially unprotected/unmonitored (e.g. out in the open, top of the fridge) versus (0) based on responses to one question asking the adolescent where their medication is usually kept (please check all that apply).
Social/normative proximal factors.
1) Friend misuse and diversion, delinquency, and substance use: a) Four questions were added to the Peer Substance Use Questionnaire16 asking how many of your friends would you estimate use ADHD medication without a prescription for studying, for partying, and how many share or sell their ADHD medication. b) Four items addressed perceived friend delinquency. c) 10 items assessed perceived friend substance use. 2) Schoolmate misuse and diversion. Three questions asked the adolescent to estimate how many students at their school use ADHD medication for studying, for partying, and how many share or sell their ADHD medication. 3) Friend intolerance of misuse and diversion, delinquency, and substance use. As an expansion of the Peer Tolerance of Substance Use Questionnaire,16 adolescents were asked how their close friends would feel about their (the adolescent) doing the behaviors listed above. 4) Schoolmate intolerance of diversion. Four questions asked how their classmates and teammates would feel about their (the adolescent) engaging in sharing and selling stimulant medication. 5) Adult intolerance of stimulant diversion: eight items asked how parents, coaches, teachers, and the adolescent’s doctor would feel about the adolescent sharing, loaning, selling, or trading) their stimulant medication.
Distal and/or universal factors.
Source and reliability for these variables, listed in Table 2, may be found in Supplement 1. These factors are hypothesized to have less proximal influence and/or have been shown in multiple studies to be pertinent to multiple adolescent health risk behaviors.
Statistical analysis plan
A fixed-effects approach, treating practice as a nominal covariate, was used in all analyses to address clustering within practice. Due to the narrow range of working correlations for provider effects, from −.046 to .044, there was no need to address clustering within physicians. Analyses examining associations with gender were tested with ANCOVAs and logistic regressions, and associations with age were tested with partial correlations. Regressions (linear and logistic, as appropriate) were used to examine associations among the hypothesized proximal and distal risk factors with the three hypothesized immediate precursors. As in similar work evaluating multiple variables grouped in conceptual domains,21 predictor variables with bivariate correlations significant at p<.05 were tested first for all three immediate precursors, within conceptually grouped blocks, and only those significant at p<.05 were entered simultaneously into final regressions (one regression for each immediate precursor). The Benjamini-Hochberg procedure, with a false discovery rate of .05, was used to determine threshold alphas against which p-values in final regression analyses were compared (see Table 3). Zero order correlations among the regression predictors and immediate precursors are in Supplement 2.
Table 3.
Results of regression analyses predicting hypothesized immediate precursors of diversion
| Approached to divert | Disclosure | Intention to divert | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Models 1 – 8 | Model 9 | Models 1 – 8 | Model 9 | Models 1 – 8 | Model 9 | |||||||
|
| ||||||||||||
| b | p | b | p | b | p | b | p | b | p | b | p | |
| Practice | −0.01 | 0.903 | −0.06 | 0.615 | 0.06 | 0.218 | 0.05 | 0.343 | −0.01 | 0.449 | 0.00 | 0.609 |
| Demographics | ||||||||||||
| Age | 0.65 | 0.000 | 0.37 | 0.037 | 0.13 | 0.083 | 0.01 | 0.919 | 0.01 | 0.081 | −0.01 | 0.385 |
| Male | −0.40 | 0.408 | −0.76 | 0.173 | 0.14 | 0.590 | 0.17 | 0.545 | 0.01 | 0.810 | −0.03 | 0.317 |
| Intrapersonal Proximal Factors | ||||||||||||
| Diversion refusal self-efficacy | −0.28 | 0.455 | −0.02 | 0.911 | −0.00 | 0.959 | ||||||
| Diversion refusal skills | −0.50 | 0.050 | −0.19 | 0.191 | −0.05 | 0.000 | −0.02 | 0.135 | ||||
| Likelihood of diversion | 0.10 | 0.824 | 0.39 | 0.164 | 0.16 | 0.000 | 0.09 | 0.001 | ||||
| Attitudinal/Behavioral Proximal Factors | ||||||||||||
| Perceived risk of harm | −0.21 | 0.457 | 0.05 | 0.711 | 0.00 | 0.850 | ||||||
| Perceived likelihood of negative consequences of diversion if caught | −0.40 | 0.451 | −0.79 | 0.009 | −0.77 | 0.004 | −0.10 | 0.001 | −0.08 | 0.002 | ||
| Perceived likelihood of negative social consequences of diversion | 0.68 | 0.082 | 0.16 | 0.339 | −0.02 | 0.262 | ||||||
| Attitudinal intolerance of stimulant misuse and diversion | −0.82 | 0.021 | −0.24 | 0.506 | −0.40 | 0.116 | −0.12 | 0.000 | −0.06 | 0.033 | ||
| Social/Normative Proximal Factors | ||||||||||||
| Friend stimulant misuse and diversion | 0.68 | 0.192 | −0.10 | 0.795 | 0.08 | 0.042 | 0.04 | 0.189 | ||||
| Friend substance use | 0.46 | 0.374 | 0.00 | 0.994 | 0.04 | 0.192 | ||||||
| Friend delinquency | 0.39 | 0.440 | −0.01 | 0.977 | −0.05 | 0.130 | ||||||
| Schoolmate stimulant misuse and diversion | 0.67 | 0.025 | 0.84 | 0.003 | 0.71 | 0.000 | 0.72 | 0.000 | 0.00 | 0.883 | ||
| Friend intolerance of stimulant misuse and diversion | −0.54 | 0.314 | −0.16 | 0.555 | −0.04 | 0.204 | ||||||
| Friend intolerance of substance use | −0.08 | 0.891 | 0.13 | 0.711 | −0.02 | 0.638 | ||||||
| Friend intolerance of delinquency | 0.43 | 0.440 | 0.05 | 0.877 | 0.02 | 0.633 | ||||||
| Schoolmate intolerance of stimulant diversion | 0.00 | 0.994 | −0.22 | 0.223 | −0.04 | 0.043 | −0.01 | 0.465 | ||||
| Adult intolerance of stimulant diversion | −0.30 | 0.691 | −0.20 | 0.616 | −0.04 | 0.366 | ||||||
| Distal and/or Universal Risk Factors | ||||||||||||
| Age first treated with stimulants | 0.23 | 0.46 | 0.13 | 0.263 | 0.02 | 0.064 | ||||||
| Number of years treated with stimulants | 0.15 | 0.555 | 0.17 | 0.127 | 0.02 | 0.080 | ||||||
| Ever stopped taking stimulants for 6 months+ | 1.46 | 0.004 | 0.71 | 0.184 | 0.23 | 0.507 | 0.20 | 0.000 | 0.11 | 0.003 | ||
| Negative urgency | 0.31 | 0.458 | 0.37 | 0.066 | 0.02 | 0.502 | ||||||
| Positive urgency | −0.54 | 0.264 | 0.30 | 0.254 | 0.00 | 0.980 | ||||||
| Sensation-seeking | 0.91 | 0.096 | −0.11 | 0.700 | 0.01 | 0.866 | ||||||
| (Lack of) Premeditation | 0.81 | 0.065 | 0.26 | 0.251 | 0.03 | 0.269 | ||||||
| (Lack of) Perseverance | −0.08 | 0.867 | 0.06 | 0.813 | 0.03 | 0.347 | ||||||
| Depression | 0.05 | 0.092 | 0.01 | 0.305 | 0.00 | 0.561 | ||||||
| Anxiety | −0.01 | 0.832 | 0.00 | 0.830 | 0.00 | 0.095 | ||||||
| Delinquency | 0.04 | 0.583 | 0.08 | 0.098 | 0.01 | 0.011 | 0.01 | 0.308 | ||||
| Substance use | 1.45 | 0.019 | 1.49 | 0.016 | 0.39 | 0.147 | 0.06 | 0.033 | 0.03 | 0.327 | ||
| Problems from alcohol or drug use | 0.34 | 0.548 | −0.81 | 0.036 | −0.73 | 0.049 | 0.13 | 0.001 | 0.11 | 0.004 | ||
| Attitudinal intolerance of deviance | −0.67 | 0.061 | −0.59 | 0.021 | −0.35 | 0.215 | −0.13 | 0.000 | 0.01 | 0.779 | ||
| Religious importance | −0.26 | 0.264 | −0.21 | 0.060 | 0.01 | 0.348 | ||||||
Note. Ever approached to divert was analyzed using logistic regression, disclosure was analyzed using logistic regression as appropriate for a count variable with a binomial distribution, and intention to divert was analyzed using continuous regression. Models 1 through 8 tested each block of variables separately in regression analyses; results are presented in a single column for ease of viewing. All five UPPS-P variables were included to identify any unique effects amongst them despite non-significant zero-order correlations for some. Model 9 included age, sex, and all significant predictors from Models 1 through 8. Bolded p-values for Model 9 indicate that the hypothesis test remained significant after computing a Benjamini-Hochberg adjusted alpha.
Results
Overview
Sample characteristics are detailed in Tables 1 and 2 with additional description provided in text. Associations with gender were minimal and are mentioned in text. Significant associations with age are shown in Table 2 alongside descriptive statistics by age group (sample split roughly in half by age).
Clinical characteristics of the sample
As shown in Table 1, most adolescents were initially diagnosed in elementary school; more male (n=31/255, 12%) than female (n=2/84, 2%) participants were first diagnosed at preschool age. A majority were initially diagnosed by a pediatrician. Most (76%) adolescents met DSM-5 symptom count criteria for ADHD based on parent and teen rating scale report (see Table 1 footnote for variable construction). Clinically significant depression and anxiety, as indicated by t-scores more than two standard deviations from published norms, was rare.
Diversion and immediate precursors
Diversion.
As shown in Table 2, diversion was rare (1%, n=3). (See Supplement 3 for additional details.)
Approached to divert was reported by seven percent of the sample (n=25). Specifically, 14 teens (9 male, 5 female) were approached to share their medication, three were approached to sell their medication (all male), and eight were approached for selling and sharing (6 male, 2 female). Teens were most frequently asked to share by an acquaintance (n=10/22) or close friend (n=6/22), at school (n=8/22), and for studying or test-taking (n=12/22). Teens were most frequently asked to sell by an acquaintance (n=7/11), at school (n=5/11), and for partying (n=4/11) or studying/test-taking (n=3/11). Older teens were more often approached to divert than younger teens – at nearly four times the rate (11% vs. 3%, respectively).
Treatment disclosure to peers.
On average, one social network type knew about the teen’s prescription (most commonly, 51% reporting a small circle of friends). For a substantial minority, most of the teen’s friends (29%), and a small circle of classmates (26%), knew. Older age was associated with more disclosure.
Intentions to divert were generally low with the mean response being “I definitely will not.” Ten percent had mean scores above 1 indicating less certainty about refraining from diversion.
Intrapersonal proximal factors
Diversion refusal self-efficacy and skills.
On average, adolescents reported that it was somewhat to very easy to turn down requests to share or sell their medication. Responses most commonly endorsed as “very easy” were direct: “tell them no” (81%) and “I don’t give out my pills” (82%). The refusal skill techniques most commonly endorsed were the same and included: “tell them no” (87%) and “I don’t give out my pills” (80%).
Likelihood of diversion.
On average, adolescents indicated a high likelihood of not giving away or selling their medication with the mean response rounding to “I definitely would not.” Percentages of adolescents endorsing “I definitely would not” ranged from 81% for sharing with a friend or family member who needed it to study or take a test to 96% for sharing with a classmate who wanted to use the medication for fun. The situation with the greatest likelihood of diversion was “to a friend or family member who ran out of their medication” (14% endorsing “I probably would” or “I definitely would”).
Attitudinal/behavioral proximal factors
Perceived risk of harm.
On average, adolescents perceived moderate risk associated with taking an ADHD medication without a prescription. The numbers perceiving moderate-to-great risk increased with higher frequency of use (i.e., 83% reported moderate-to-great risk when people take ADHD medication “regularly” without a prescription).
Perceived likelihood of diversion consequences.
On average, adolescents reported that negative consequences were “somewhat likely” to occur if they were caught diverting their medication. For example, 91% thought it very likely that they would lose privileges or be grounded and 79% thought it very likely they would be suspended. On average, adolescents reported that negative social consequences were “somewhat likely” to occur if they diverted their medication.
Attitudinal intolerance of stimulant misuse and diversion.
On average, adolescents rated stimulant misuse and diversion as “somewhat wrong” to “very wrong.” Older adolescents were less intolerant than younger adolescents.
Medication utilization. Taking amphetamine.
Fewer than half of the adolescents were taking an amphetamine preparation versus methylphenidate. Thirty-four percent of those taking amphetamines (n=41/119) were taking lisdexamfetamine. Medication surplus. On average, adolescents missed 4 days of medication in the prior month (which extrapolates to about 12 days in a 90 day supply). Across four treatment windows (schoolyear weekdays, schoolyear weekends, summer weekdays, summer weekends), adolescents took their medications less than daily for an average of one window. Similar to prophylactic medication use for other chronic conditions,22 age was related to adherence, with younger adolescents reporting more fully medicated treatment windows. Medication access. One-third (35%) of the adolescents reported that their medication is stored in a potentially unprotected/unmonitored location (e.g., out in the open, on top of the fridge).
Social/normative proximal factors
Friend substance use, misuse and diversion, and delinquency.
On average, adolescents reported little non-prescribed use or diversion of ADHD medication by their friends. However, 23% and 13% reported having any friends (“a few” or more) who used the medication non-prescribed or who shared or sold their own medication, respectively. The modal non-zero response was “a few” across both misuse and diversion. Perceived delinquency and substance use by friends were distributed similarly. Older adolescents reported more friend misuse, diversion, and substance use than younger adolescents.
Schoolmate misuse and diversion.
On average, adolescents reported “a few” students at their school use ADHD medication non-prescribed or divert. Fifty-four percent and 39% of adolescents reported having any schoolmates who used the medication non-prescribed or shared/sold their own medication, respectively. Older adolescents reported more schoolmate misuse and diversion than younger adolescents. Schoolmate misuse and diversion was significantly higher than friend misuse and diversion, t (df=336) = 12.04, p<.001.
Friend intolerance of stimulant misuse and diversion, substance use, and delinquency.
On average, adolescents reported that their close friends would disapprove of them using ADHD medication without a prescription or diverting it. Female participants reported more perceived disapproval than male participants, p<.01 (see Supplement 4 for gender differences statistics). Perceived intolerance of substance use and delinquency by friends was distributed similarly, including female participants reporting more disapproval than male participants, both p<.05. Older adolescents reported less friend intolerance of misuse, diversion, and substance use than younger adolescents.
Schoolmate intolerance of diversion.
On average, adolescents reported that their classmates and teammates would disapprove of them sharing or selling their ADHD medication. Older adolescents reported less intolerance of diversion.
Adult intolerance of stimulant diversion.
On average, adolescents reported strong disapproval of diversion by adults.
Distal and/or universal risk factors
Findings are selectively described. See Table 2 for details.
ADHD and ODD symptoms.
Older adolescents had lower ADHD and ODD symptom scores than younger adolescents. Average Impairment from ADHD was above normative mean levels for adolescents.23
Treatment history.
On average, adolescents were treated for nearly six years without significant interruption. Girls were treated for fewer years than boys, p<.05. As expected, all treatment history variables were positively correlated with age.
Impulsive personality characteristics.
On average, adolescents “agree(d) somewhat” with statements reflecting their tendency to act rashly when in a negative or positive mood, to be sensation-seeking, and to lack premeditation and perseverance. Boys self-rated positive urgency (acting rashly when in a positive mood) higher than girls, p<.001.
Co-occurring mental health problems.
Relative to published norms, adolescents self-rated their depression and anxiety symptoms at average (depression) or slightly below average (anxiety) levels. t-scores for both scales were higher for girls than boys, p<.01 for depression, p<.001 for anxiety, although as shown in Table 1, endorsement of clinically high symptoms was rare. Older adolescents reported higher depression symptom scores than younger adolescents.
Delinquency.
On average, adolescents engaged in fewer than two delinquent acts.
Substance use and problems.
Forty percent reported ever using any substances, with more male than female participants reporting use, p<.05. Problems from alcohol or drug use were infrequently endorsed. Older adolescents reported more substance use and problems than younger adolescents.
Attitudinal intolerance of deviance.
On average, adolescents rated deviant behaviors as “very wrong.”
Religious importance.
On average, adolescents indicated that religion was “a little important.” Older adolescents rated religion as less important in their lives than did younger adolescents.
General functioning.
The average adolescent-reported grade in school was B, with most (81%) endorsing between B- and A. Only 2% endorsed D or failing. The average academic plan was to graduate from college, with female participants having greater intentions to graduate than male participants, p<.05. Academic demand. On average, adolescents reported “a little” competition for grades at their school. Female participants reported more competition than male participants, p<.05. Older adolescents reported more competition than younger adolescents. Average social functioning was approximately one SD below T-score average. The average level of functioning across 18 life domains approached 3 = ”about where I should be.”
Regression results
Correlations were first examined. The magnitude and significance of the associations among the three immediate precursors supported studying them as separate variables (approaches to divert with treatment disclosure, r=.11, p<.05; approaches to divert with intent to divert, r=.05, ns; treatment disclosure with intent to divert, r=.04, ns). Up to one-half of the correlations between the predictors and immediate precursors were significant at p<.05 (15/43 or 35% for approached to divert; 17/43 or 40% for treatment disclosure to peers; 23/43 or 53% for intentions to divert) and included two or more variables in each hypothesized domain for testing in the regressions (see Supplement 2 for correlation matrix).
Table 3 shows which of these variables, when tested together within domain, remained significant at p<.05 (Models 1–8). Two or more variables in each domain were significant at p<.05 for one or more of the immediate precursors. When these variables were entered in the final regressions (Model 9 for each immediate precursor), with Benjamini-Hochberg thresholds, more schoolmate stimulant misuse and diversion was associated with ever having been approached to divert, and lower perceived likelihood of negative consequences of diversion and schoolmate stimulant misuse and diversion were associated with treatment disclosure. Greater likelihood of diversion, lower perceived likelihood of negative consequences, ever having stopped taking stimulant medication for 6 or more months, and problems from alcohol or drug use were associated with greater intent to divert.
Discussion
This study provides the first characterization, pertinent to stimulant diversion risk, of a sample of adolescents prescribed stimulants for ADHD in pediatric primary care. Given the absence of data describing this population with respect to stimulant diversion risk and even more generally (clinical and health behavior risk characteristics), these findings provide important new information. In this initial examination of baseline characteristics among adolescents participating in an RCT on stimulant diversion prevention, little actual diversion was reported, but adolescents were increasingly approached to divert as they aged. We also found variability in, and higher vulnerability with older age, for selected psychosocial characteristics that we also hypothesize are pertinent to emerging diversion risk. Few gender differences were identified in risk variables specific to stimulants, suggesting that in adolescence, gender-specific prevention programming may not be necessary. Multiple zero-order correlations between the diversion risk factors and three immediate precursors, up to 53% of the correlations tested, were consistent with our conceptual model (Figure 1). When tested together in regressions, one variable from each of the model domains remained significantly associated with at least one of the immediate precursors to diversion, even after including universal health risk factors (e.g., substance use, delinquency). Results set the stage for future hypothesis testing of diversion predictors and prevention in this and in other samples.
Only three adolescents reported diversion, which may reflect the young age of the sample. Comparison to other studies is difficult because few report adolescent diversion. McCabe and colleagues provides perhaps the best comparison with 16.4% of 146 middle and high school students from two Detroit-area school districts ever diverting stimulant medication prescribed in their lifetimes.24 Aside from obvious differences (e.g., school- vs. primary care-recruited sample; current vs. lifetime prescription; geographic location), it is unclear why the rates differ. Our observed low rate may reflect increasing awareness among adolescents of the dangers of stimulant diversion and misuse. The McCabe et al. data, collected 7 years prior, reported comparable marijuana use (11.3% vs. 10.5% in the current study). As suggested by McCabe et al., treatment history may be important but this information was not available for comparison to the current sample. Despite our procedures to assure confidentiality, adolescents may have withheld reports of diversion for fear of their pediatricians finding out.
The variables that we hypothesize to be immediate precursors to diversion revealed potentially important variability at this age and, (see below), associations with other presumed risk factors. Although average intent to divert was low, as in substance use prevention research,25 10% did not commit to refrain. A substantial minority reported that friends and classmates beyond a small circle of friends knew about their medication, potentially increasing the likelihood of being approached (indeed, these two immediate precursors were correlated). Also reported by McCabe and colleagues,7 older adolescents were more often approached to divert than younger adolescents. Educating adolescents to disclose their treatment information selectively may be an important prevention strategy. We include this in our stimulant diversion prevention training – in the current RCT and in the college student study where disclosure decreased post-training.14
Regarding the intrapersonal domain of diversion risk factors, adolescents felt (on average) that refusing requests for their medication was easy. This high self-efficacy may explain why requests to divert are more common than diversion. Teens endorsed as easy, and most likely to use, direct responses to diversion requests such as “tell them no” and “I don’t give out my pills”. Refusal skill training is a common ingredient in adolescent substance use prevention programs and refusal assertiveness predicts adolescent alcohol use,26 suggesting that the confidence conveyed by most teens in our study bodes well for their future diversion risk. Maintaining this confidence as they age, and increasing confidence among those who have low self-efficacy, may be important. In the regression analyses, adolescents’ likelihood of giving away or selling their medication across various social scenarios was the surviving variable associated with intent to share/trade/sell in the next six months. Thus, some teens remain at-risk, above and beyond adjustment for other variables. Discussion of these scenarios may be useful to consider, especially given our finding that social functioning was low relative to published norms.
Regarding the attitudinal/behavioral domain of diversion risk factors, adolescents perceived a moderate degree of risk, to themselves for diversion and to others for non-prescribed use. This level of perceived harm is slightly lower than that associated with use of conventional cigarettes (3.25–3.60)27 and tracks with our findings that most of the teens in the current study do not expect serious adverse physical or psychological events from use of stimulants.28 On average, they rated misuse and diversion as wrong, but this attitude was lessened for older adolescents, suggesting that diversion risk may increase with age and that continued monitoring will be important. Perceived likelihood of negative consequences if caught diverting stood out amongst the other variables for its association with treatment disclosure to peers and intent to divert, suggesting that educating patients about these possibilities may have some merit.
Amphetamines were reported less often than methylphenidate preparations which may reflect prescriber concerns about its misuse given that amphetamines are misused more often than methylphenidate medications by college students.29 Moreover, long-acting controlled release methylphenidate has been on the market longer and pediatricians may feel more experienced with its use. Although this prescribing pattern may dissuade future diversion, the storing of these medications in open-access locations by a third of the participants may unwittingly increase peer approaches to divert or steal as the teens grow older. A history of medication cessation was higher for older adolescents and was associated in the regressions with greater intent to divert. As ADHD symptoms were also lower for older adolescents, decreased perceived need for medication, as well as supply and storage of medications, may need to be routinely monitored with increasing age.
Regarding the social/normative domain, perceived misuse and diversion of stimulants by peers was low overall, but it was positively correlated with age. The highest expected levels across the four descriptive norms variables was for schoolmate misuse and diversion, suggesting that adolescents are more likely to perceive the behavior as occurring outside of their immediate social circles. Schoolmate misuse and diversion was also the one social/normative domain variable (and in fact the only regression predictor) that survived the regression analyses for being approached to divert. Thus, attention to the larger social climate may need to be considered for its impact on diversion risk. Older teens perceived more peer approval for stimulant misuse/diversion and substance use than younger teens, and these injunctive norms were the only proximal risk variables with any gender differences (female participants reporting more peer intolerance than males, which aligns with greater misuse by college student male participants.29). Given the strong associations between injunctive norms and adolescent substance use,30 it is not surprising that we also found significantly more substance use by males in the sample.
Completely independent of age and gender, teens perceive strong disapproval of diversion by the adults in their lives. This variable did not stand out in the regression analyses, but it was correlated with other predictors (e.g., perceived likelihood of negative consequences if caught) and may suggest an indirect route to diversion risk management via education and socialization by key adults. Other factors not included in the current study, such as parental monitoring and parent/provider-teen discussions, should be considered for their potential moderating influences on diversion risk.
Overall, we found few differences between male and female participants in levels of presumed diversion risk. Most were for variables applicable to health risk behavior in general (e.g., substance use). Female compared to male participants had been treated for slightly shorter durations, they had higher college aspirations, and they reported being immersed in more competitive academic environments. Thus, although ADHD and ODD symptom levels were not different, the clinical presentation of the female participants appeared to be slightly higher functioning with later-emerging treatment initiation. Whether these characteristics ultimately affect diversion risk is unclear and should be studied, as previous research has suggested that female participants are more likely to be approached to divert.7
Study limitations.
A strength of the sample described herein is also a limitation to generalizability. It is unclear whether our findings would generalize to patients treated by psychiatrists or to populations in other regions of the country including those less proximal to a major medical center. The adolescent patients in our study were from well-educated families and only 20% were from racial or ethnic minority groups. Although we took steps to protect privacy, we cannot confirm that all participants answered their surveys in this manner, and some variables may under-estimate risk.
Conclusions.
Collectively, our findings indicate that adolescents treated with stimulants at their pediatric practices have, on average, a clinical profile characterized by low risk for stimulant diversion. However, older age was associated with more disclosure and approaches to divert, and in regression analyses several variables stood out for their associations with these presumed immediate precursors to diversion (including intent to divert): likelihood of diverting in social scenarios, perceived negative consequences if caught diverting, perceived schoolmate misuse and diversion, previous treatment cessation, and problems with alcohol and other drugs. Prevention may be most effective in adolescence before diversion begins, and discussion of social diversion scenarios and negative consequences may be important. Longitudinally examining model-based prediction of diversion at older ages, including unfolding of these risk factors over time, will ultimately aide determination of which risk factors are most important to target and when.
Supplementary Material
Acknowledgments
Funding for this study was provided by the National Institute on Drug Abuse U01DA040213. Additional support was provided by DA035464, DA049721, MH018951-26, TR001856, MH121585. The authors have no conflicts of interest to declare. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Geetha Subramaniam is an employee of the National Institute on Drug Abuse (NIDA), which is the funding agency for the study; her participation in this publication arises from her role as a scientific officer on a cooperative agreement for this study.
References
- 1.Johansen ME, Matic K, McAlearney AS. Attention Deficit Hyperactivity Disorder Medication Use Among Teens and Young Adults. Journal of Adolescent Health. 2015;57(2):192–197. [DOI] [PubMed] [Google Scholar]
- 2.DeSantis AD, Anthony KE, Cohen EL. Illegal college ADHD stimulant distributors: characteristics and potential areas of intervention. Subst Use Misuse. 2013;48(6):446–456. [DOI] [PubMed] [Google Scholar]
- 3.McCabe SE, West BT, Teter CJ, et al. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addict Behav. 2014;39(7):1176–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry. 2013;52(12):1272–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21–31. [DOI] [PubMed] [Google Scholar]
- 6.Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCabe SE, Teter CJ, Boyd CJ. The use, misuse and diversion of prescription stimulants among middle and high school students. Subst Use Misuse. 2004;39(7):1095–1116. [DOI] [PubMed] [Google Scholar]
- 8.Cottler LB, Striley CW, Lasopa SO. Assessing prescription stimulant use, misuse, and diversion among youth 10–18 years of age. Current opinion in psychiatry. 2013;26(5):511–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poulin C Medical and nonmedical stimulant use among adolescents: from sanctioned to unsanctioned use. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2001;165(8):1039–1044. [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein-Ngo QM, McCabe SE, Veliz PT, et al. Diversion of ADHD Stimulants and Victimization Among Adolescents. Journal of Pediatric Psychology. 2016;41(7):786–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lasopa SO, Striley CW, Cottler LB. Diversion of prescription stimulant drugs among 10–18-year-olds. Current opinion in psychiatry. 2015;28(4):292–298. [DOI] [PubMed] [Google Scholar]
- 12.Bavarian N, Flay BR, Ketcham PL, et al. Using structural equation modeling to understand prescription stimulant misuse: a test of the Theory of Triadic Influence. Drug Alcohol Depend. 2014;138:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malmberg M, Kleinjan M, Vermulst AA, et al. Do substance use risk personality dimensions predict the onset of substance use in early adolescence? A variable- and person-centered approach. J Youth Adolesc. 2012;41(11):1512–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molina BSG, Kipp HL, Joseph HM, et al. Stimulant diversion risk among college students treated for ADHD: Primary care provider prevention training. Acad Pediatr. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zuvekas SH, Vitiello B. Stimulant medication use in children: a 12-year perspective. Am J Psychiatry. 2012;169(2):160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnston LD, O’Malley PM, Miech RA, et al. Monitoring the Future National Survey Results on Drug Use, 1975–2015: Overview, key findings on adolescent drug use. In: Research IfS, ed. Ann Arbor, MI: The University of Michigan; 2016. [Google Scholar]
- 17.de Vries H, Dijkstra M, Kuhlman P. Self-efficacy: the third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health education research. 1988;3(3):273–282. [Google Scholar]
- 18.Epstein JA, Botvin GJ. Media resistance skills and drug skill refusal techniques: What is their relationship with alcohol use among inner-city adolescents? Addict Behav. 2008;33(4):528–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farrelly MC, Duke JC, Crankshaw EC, et al. A Randomized Trial of the Effect of E-cigarette TV Advertisements on Intentions to Use E-cigarettes. American journal of preventive medicine. 2015;49(5):686–693. [DOI] [PubMed] [Google Scholar]
- 20.Jessor R, Donovan JE, Costa FM. Health Behavior Questionnaire. Boulder, CO: Institute of Behavioral Science, University of Colorado;1989. [Google Scholar]
- 21.Kaplow JB, Curran PJ, Dodge KA. Child, parent, and peer predictors of early-onset substance use: A multisite longitudinal study. Journal of abnormal child psychology. 2002;30(3):199–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaplan A, Price D. Treatment Adherence in Adolescents with Asthma. Journal of asthma and allergy. 2020;13:39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evans SW, Brady CE, Harrison JR, et al. Measuring ADHD and ODD symptoms and impairment using high school teachers’ ratings. J Clin Child Adolesc Psychol. 2013;42(2):197–207. [DOI] [PubMed] [Google Scholar]
- 24.McCabe SE, West BT, Teter CJ, et al. Characteristics associated with the diversion of controlled medications among adolescents. Drug Alcohol Depend. 2011;118(2–3):452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kovach Clark H, Ringwalt CL, Hanley S, et al. Project ALERT’s effects on adolescents’ prodrug beliefs: a replication and extension study. Health education & behavior : the official publication of the Society for Public Health Education. 2010;37(3):357–376. [DOI] [PubMed] [Google Scholar]
- 26.Epstein JA, Griffin KW, Botvin GJ. Risk Taking and Refusal Assertiveness in a Longitudinal Model of Alcohol Use Among Inner-City Adolescents. Prevention Science. 2001;2(3):193–200. [DOI] [PubMed] [Google Scholar]
- 27.Owotomo O, Maslowsky J, Loukas A. Perceptions of the Harm and Addictiveness of Conventional Cigarette Smoking Among Adolescent E-Cigarette Users. Journal of Adolescent Health. 2018;62(1):87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Molina BSG, Lindstrom RA, Kipp HL, et al. Expectancies for the effects of stimulant medication by adolescents in pediatric primary care treatment for ADHD. American Professional Society of ADHD and Related Disorders; January 2019, 2019; Washington, DC. [Google Scholar]
- 29.Benson K, Flory K, Humphreys KL, et al. Misuse of Stimulant Medication Among College Students: A Comprehensive Review and Meta-analysis. Clinical Child and Family Psychology Review. 2015;18(1):50–76. [DOI] [PubMed] [Google Scholar]
- 30.Pedersen ER, Osilla KC, Miles JNV, et al. The role of perceived injunctive alcohol norms in adolescent drinking behavior. Addictive behaviors. 2017;67:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.