Abstract
Aim: This study aimed to reveal the mortality risk by age in patients undergoing femoropopliteal endovascular therapy for intermittent claudication, in comparison to the national age-specific standard value.
Methods: We analyzed 2056 patients undergoing endovascular therapy for moderate to severe intermittent claudication between 2010 and 2018, performed at five cardiovascular centers in Japan. The 3-year mortality risk by age was compared with the data from year- and sex-matched Japanese citizens, which were obtained from Japan’s national life table data. Clinical characteristics associated with age in the study patients were also explored.
Results: The mean age was 73±9 years. The 3-year mortality risk was increased with age in the patient population, from 6.4% for patients aged <65 years to 21.2% for those aged ≥ 85 years. On the contrary, its risk ratio relative to the matched citizens of the same age was decreased with age; the relative risk ratio was 3.08 for patients aged <65 years ( P =0.001) and 0.60 for those aged ≥ 85 years ( P =0.016). Current smoking, body mass index ≥ 25 kg/m 2 , hyperlipidemia, diabetes mellitus, and dialysis dependence were inversely associated with age (all P <0.05).
Conclusion: Mortality risk increased with age, but the risk ratio relative to the matched citizens decreased with age. Younger patients had a higher mortality risk relative to the matched citizens, whereas patients aged ≥ 85 years had a lower mortality risk relative to the matched citizens. Younger patients were more likely to accumulate cardiovascular risk factors.
Keywords: Intermittent claudication, Mortality, Age group, Femoropopliteal endovascular therapy
Introduction
Femoropopliteal stenosis or occlusion is the most common lesion associated with intermittent claudication 1) . The prevalence of intermittent claudication increases with age 2) . Currently, endovascular therapy is considered the first-line revascularization strategy for femoropopliteal lesions 3 , 4) . In aging societies, it has become common to perform endovascular therapy in older patients.
Age is a well-known risk factor for mortality in various populations, and there is no exception in a population with peripheral artery disease 5) . Furthermore, many previous studies have reported that the mortality risk of patients with intermittent claudication is two to three times higher than that of the general population with adjustment for age 6 , 7) . In this context, older patients with intermittent claudication are often referred as a high-risk population with poor prognosis 8 , 9) . However, the age-adjusted comparison did not mean an age-specific comparison but merely presented features that were averaged across all age groups. It remained unknown whether every age group of the population undergoing femoropopliteal endovascular therapy for intermittent claudication would have a similarly high mortality risk relative to the national age-specific standard value.
Aim
The aim of this study was to reveal the mortality risk by age in patients undergoing femoropopliteal endovascular therapy for intermittent claudication.
Methods
We used a multicenter retrospective longitudinal database of 2056 consecutive patients undergoing femoropopliteal endovascular therapy for intermittent claudication, with a median follow-up period of 3.1 years. All patients presented with moderate to severe intermittent claudication (Rutherford category 2 and 3) and underwent endovascular therapy for de novo lesions, including lesions from the superficial femoral artery to the proximal popliteal artery, between 2010 and 2018 at five cardiovascular centers in Japan.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the institutional review boards of the participating institutions. Because the study was a retrospective analysis of existing data, the need for informed consent was waived by the institutional review boards, in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.
The determination of cardiovascular risk factors was based on the clinical diagnosis according to domestic clinical guidelines. In brief, the presence of hypertension was defined for those who received antihypertensive treatments or those who presented with systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg 10) . Hyperlipidemia was defined for those that received antihyperlipidemic treatments or those who had fasting triglyceride levels ≥ 150 mg/dL, fasting low-density lipoprotein cholesterol levels ≥ 140 mg/dL, or non-high-density lipoprotein cholesterol levels ≥ 170 mg/dL 11) . Diabetes mellitus was defined for those that received antidiabetic treatment or those who had fasting plasma glucose levels ≥ 126 mg/dL, casual plasma glucose levels ≥ 200 mg/dL, or hemoglobin A1c levels ≥ 6.5% 12) . Dialysis dependence, i.e., end-stage renal disease on dialysis, included both hemodialysis and peritoneal dialysis. Chronic heart failure was determined when patients had a history of hospitalization due to heart failure or received treatments for heart failure. Body mass index (BMI) was classified into <18.5 (lean), 18.5 to 25, and ≥ 25 kg/m 2 (obese). The severity of intermittent claudication was classified as moderate (Rutherford category 2) and severe (Rutherford category 3) 4) .
Statistical Analysis
Data were given as means and standard deviations for continuous variables or as frequencies and percentages for discrete variables, if not otherwise mentioned. A P value of <0.05 was considered statistically significant, and 95% confidence intervals were reported when appropriate. The Kaplan-Meier method was used to estimate the 3-year cumulative incidence rate of mortality in the overall study population, and in subgroups aged <65 years, 65 to 69 years, 70 to 74 years, 75 to 79 years, 80 to 84 years, and ≥ 85 years. The 3-year cumulative incidence rate of mortality was subsequently compared with that of the year- and sex-matched Japanese citizens, which was derived from Japan’s national life table data published by the Ministry of Health, Labor, and Welfare 13) . As a sensitivity analysis, the 3-year mortality risk by age and its comparison to the year- and sex-matched citizens was also analyzed using the smoothing spline model. A series of the analyses on mortality were also performed in the male subgroup and in the female subgroup separately. Finally, we explored the association of clinical features with age, by fitting an analysis of variance model stratified with sex. The 95% confidence intervals of the respective estimates were obtained from the 2000-time bootstrapping method. All statistical analyses were performed using R version 3.6.0 (R Development Core Team, Vienna, Austria).
Results
The clinical characteristics of the study population are shown in Table 1 . The mean age was 73±9 years old, and 72.5% were male. Within 3-year follow-ups, 213 deaths were observed. The 3-year cumulative incidence rate of all-cause mortality was 19.4% (95% confidence interval, 17.3% to 21.6%) in the overall study population. The corresponding value for the year- and sex-matched citizens was 10.1% (9.7% to 10.5%), indicating that the overall study population with intermittent claudication had a higher mortality risk than the year- and sex-matched citizens, with a relative risk ratio of 2.13 (1.86 to 2.44) ( P <0.001).
Table 1. Characteristics of the study population.
| n | 2056 |
| Age (years) | 73±9 |
| Male sex | 1490 (72.5%) |
| Current smoker | 795 (38.7%) |
| Body mass index | |
| <18.5 kg/m 2 | 228 (11.1%) |
| 18.5 to 25 kg/m 2 | 1384 (67.3%) |
| ≥ 25 kg/m 2 | 444 (21.6%) |
| Hypertension | 1769 (86.0%) |
| Hyperlipidemia | 1224 (59.5%) |
| Diabetes mellitus | 1125 (54.7%) |
| Dialysis dependence | 441 (21.4%) |
| Chronic heart failure | 293 (14.3%) |
| Coronary artery disease | 1211 (58.9%) |
| Cerebrovascular disease | 387 (18.8%) |
| Severe claudication (Rutherford 3) | 1308 (63.6%) |
Data are shown as means±standard deviations, or frequencies (percentages).
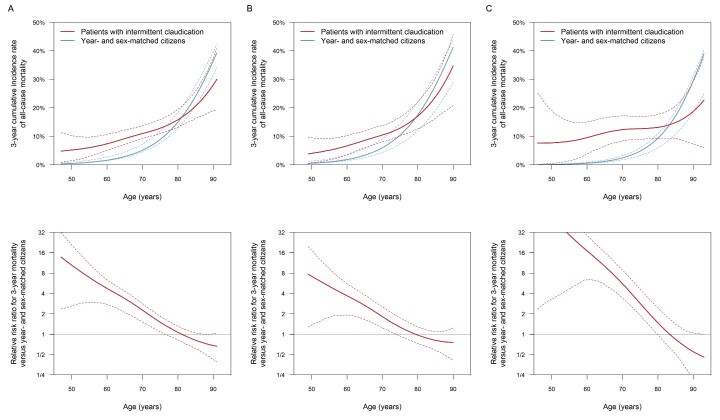
As summarized in Table 2 , the 3-year mortality risk increased with age in overall patients with intermittent claudication, from 6.4% (3.6% to 9.4%) for the subgroups aged <65 years to 21.2% (13.6% to 29.1%) for those aged ≥ 85 years. On the contrary, when compared with the year- and sex-adjusted citizens of the same age group, its relative risk ratio decreased with age. Patients aged <65 years had a higher mortality risk than the year- and sex-matched citizens (relative risk ratio, 3.08 [1.67 to 4.69]; P =0.001), whereas those aged ≥ 85 years had a lower mortality risk (relative risk ratio, 0.60 [0.35 to 0.90]; P =0.016). The corresponding relative risk ratios were 2.69 (1.34 to 4.30) ( P =0.010) for age <65 years and 0.64 (0.34 to 1.09) ( P =0.10) for age ≥ 85 years in the male subgroup, and 6.03 (1.25 to 13.8) ( P =0.037) for age <65 years and 0.52 (0.15 to 1.05) ( P =0.071) for age ≥ 85 years in the female subgroup ( Table 2 ). Similar findings were observed when analyzing with the smoothing spline ( Fig.1 ) .
Table 2. Age and 3-year mortality risk.
| Population | Age group | n of study patients | 3-year mortality incidence rate of study patients | 3-year mortality incidence rate of year- and sex-matched citizens | Relative risk ratio versus year- and sex-matched citizens |
|---|---|---|---|---|---|
| Overall | <65 years | 303 | 6.4% [3.6% to 9.4%] | 2.2% [2.0% to 2.3%] | 3.08 [1.67 to 4.69] ( P = 0.001) |
| 65 to 69 years | 338 | 10.9% [7.2% to 14.7%] | 4.1% [3.9% to 4.2%] | 2.88 [1.82 to 4.09] ( P <0.001) | |
| 70 to 74 years | 476 | 11.4% [8.3% to 14.7%] | 6.2% [6.1% to 6.4%] | 1.93 [1.36 to 2.60] ( P <0.001) | |
| 75 to 79 years | 435 | 14.3% [10.6% to 18.2%] | 10.3% [10.0% to 10.6%] | 1.46 [1.03 to 1.93] ( P = 0.034) | |
| 80 to 84 years | 331 | 19.4% [14.8% to 24.4%] | 18.1% [17.5% to 18.7%] | 1.09 [0.79 to 1.46] ( P = 0.65) | |
| ≥ 85 years | 173 | 21.2% [13.6% to 29.1%] | 31.0% [29.6% to 32.4%] | 0.60 [0.35 to 0.90] ( P = 0.016) | |
| Male | <65 years | 228 | 6.5% [3.4% to 10.0%] | 2.5% [2.4% to 2.6%] | 2.69 [1.34 to 4.30] ( P = 0.010) |
| 65 to 69 years | 262 | 9.0% [5.3% to 13.4%] | 4.7% [4.6% to 4.8%] | 2.00 [1.14 to 3.12] ( P = 0.018) | |
| 70 to 74 years | 358 | 11.1% [7.6% to 15.0%] | 7.2% [7.1% to 7.3%] | 1.61 [1.05 to 2.28] ( P = 0.024) | |
| 75 to 79 years | 306 | 14.8% [10.2% to 19.8%] | 12.2% [11.9% to 12.4%] | 1.25 [0.83 to 1.77] ( P = 0.27) | |
| 80 to 84 years | 233 | 21.6% [15.4% to 27.9%] | 20.9% [20.5% to 21.3%] | 1.04 [0.70 to 1.46] ( P = 0.83) | |
| ≥ 85 years | 103 | 25.9% [15.4% to 37.8%] | 35.4% [34.1% to 36.7%] | 0.64 [0.34 to 1.09] ( P = 0.10) | |
| Female | <65 years | 75 | 5.9% [1.3% to 12.6%] | 1.0% [0.9% to 1.1%] | 6.03 [1.25 to 13.8] ( P = 0.037) |
| 65 to 69 years | 76 | 17.7% [8.5% to 28.3%] | 1.9% [1.9% to 2.0%] | 11.0 [4.78 to 20.2] ( P <0.001) | |
| 70 to 74 years | 118 | 12.0% [5.6% to 18.5%] | 3.3% [3.2% to 3.4%] | 4.05 [1.79 to 6.78] ( P = 0.002) | |
| 75 to 79 years | 129 | 13.4% [6.9% to 20.6%] | 5.9% [5.7% to 6.1%] | 2.47 [1.18 to 4.14] ( P = 0.026) | |
| 80 to 84 years | 98 | 14.1% [6.8% to 23.0%] | 11.4% [11.0% to 11.9%] | 1.27 [0.56 to 2.28] ( P = 0.51) | |
| ≥ 85 years | 70 | 14.6% [4.7% to 25.8%] | 24.6% [22.7% to 26.9%] | 0.52 [0.15 to 1.05] ( P = 0.071) |
Data are estimates [95% confidence intervals].
Fig.1. Mortality risk by age in the study patients and comparison with year- and sex-matched citizens.
Data are estimates (bold lines) and 95% confidence intervals (dashed lines) in the overall population (A), male population (B), and female population (C). Upper panels show the 3-year cumulative incidence rate of all-cause mortality corresponding to ages in the study patients with intermittent claudication (red lines) and the year- and sex-matched citizens derived from the life table data of the Japanese citizens (blue lines). Lower panels show the risk ratio for the 3-year mortality relative to the year- and sex-adjusted citizens of the same age in the study patients with intermittent claudication.
Table 3 demonstrates the association of clinical features with age. Smoking, BMI ≥ 25 kg/m 2 , hyperlipidemia, diabetes mellitus, and dialysis dependence were inversely associated with age. The association of these clinical features with age was independent of one another, suggesting that their effect on age was additive. Indeed, patients with more of the clinical features were younger (upper panel in Fig.2 ), and younger age groups accumulated more of the clinical features (lower panel in Fig.2 ).
Table 3. Clinical features associated with age.
| Crude regression coefficient | Adjusted regression coefficient | |
|---|---|---|
| Current smoker | -2.6 [-3.4 to -1.9] ( P <0.001) | -3.1 [-3.8 to -2.4] ( P <0.001) |
| Body mass index | ||
| <18.5 kg/m 2 | 0.0 (Reference) | 0.0 (Reference) |
| 18.5 to 25 kg/m 2 | -0.6 [-1.7 to 0.6] ( P = 0.32) | -0.9 [-2.0 to 0.3] ( P = 0.12) |
| ≥ 25 kg/m 2 | -2.5 [-3.8 to -1.1] ( P <0.001) | -2.8 [-4.1 to -1.5] ( P <0.001) |
| Hypertension | 0.6 [-0.5 to 1.7] ( P = 0.32) | 1.0 [-0.1 to 2.1] ( P = 0.070) |
| Hyperlipidemia | -0.4 [-1.2 to 0.3] ( P = 0.26) | -0.9 [-1.7 to -0.2] ( P = 0.011) |
| Diabetes mellitus | -2.9 [-3.7 to -2.2] ( P <0.001) | -2.4 [-3.1 to -1.7] ( P <0.001) |
| Dialysis dependence | -4.7 [-5.7 to -3.8] ( P <0.001) | -5.1 [-6.1 to -4.2] ( P <0.001) |
| Chronic heart failure | -1.1 [-2.2 to 0.0] ( P = 0.060) | -0.6 [-1.7 to 0.5] ( P = 0.25) |
| Coronary artery disease | -0.6 [-1.4 to 0.2] ( P = 0.14) | 0.3 [-0.5 to 1.0] ( P = 0.52) |
| Cerebrovascular disease | 0.7 [-0.2 to 1.6] ( P = 0.13) | 0.6 [-0.3 to 1.4] ( P = 0.17) |
| Rutherford 3 versus 2 | -0.8 [-1.6 to -0.1] ( P = 0.020) | -0.5 [-1.2 to 0.2] ( P = 0.18) |
Data are regression coefficients and 95% confidence intervals ( P values). Crude regression coefficients were derived from the respective univariate analysis of variance models stratified by sex, whereas adjusted regression coefficients were from the multivariate analysis of variance model in which all explanatory variables listed in the table were entered.
Fig.2. Age and accumulation of clinical factors associated with younger age.
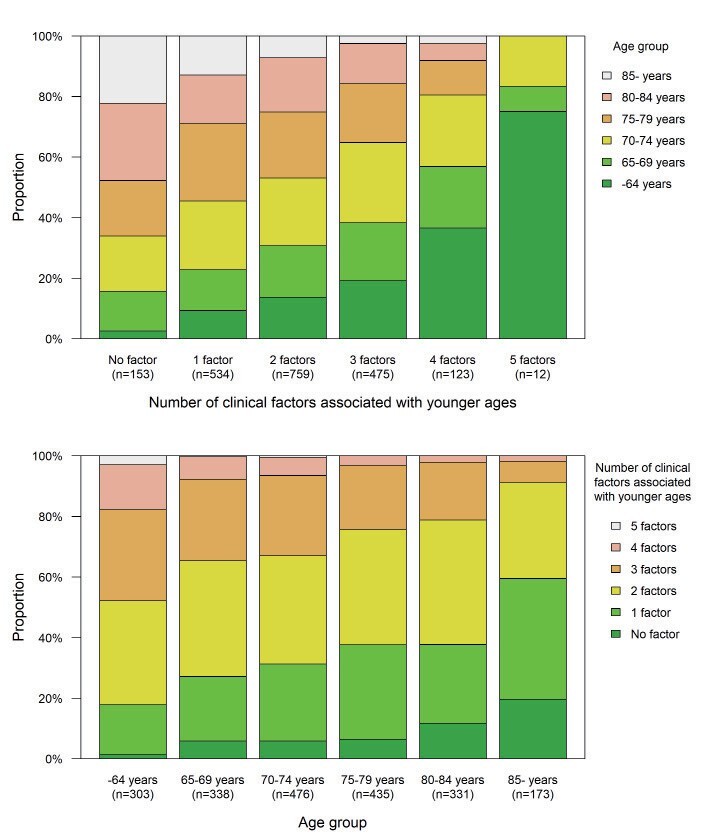
Data are the proportion of respective age categories according to the number of clinical factors associated with younger ages (upper panel) and that of respective numbers of clinical factors associated with younger ages according to the age categories (lower panel). The clinical factors associated with younger age were 1) current smoking, 2) body mass index ≥ 25 kg/m 2 , 3) hyperlipidemia, 4) diabetes mellitus, and 5) dialysis-dependent renal failure (see Table 3).
Discussion
This study demonstrated the mortality risk by age for patients undergoing femoropopliteal endovascular therapy due to intermittent claudication, in comparison to year- and sex-matched citizens. The mortality risk was increased with age within the patient population, but its risk ratio relative to the year-, sex-, and age-matched citizens was decreased with age. Younger patients had a higher mortality risk than the matched citizens, whereas patients aged ≥ 85 years had a lower mortality risk than the matched citizens. These trends were similar regardless of sex, although the relative risk ratios in each sex group had wide 95% confidence intervals and did not reach statistical significance for age ≥ 85 years, probably due to insufficient sample size. Younger patients were more likely to accumulate cardiovascular risk factors.
Endovascular therapy for peripheral artery disease has been widely spread in recent years 14 - 22) . In the aging societies, it has become common to perform endovascular therapy in older patients for intermittent claudication in clinical practice. It is of clinical importance to clarify their clinical features and prognosis.
Age was inversely associated with smoking, obesity, hyperlipidemia, diabetes mellitus, and dialysis-dependent renal failure in the study population. All these clinical features are well known as major accelerators of atherosclerosis, i.e., vascular aging. The inverse correlations indicate that patients with accumulated cardiovascular risk factors will develop peripheral atherosclerosis and present with intermittent claudication earlier (i.e., at a younger age), whereas those with fewer risk factors will develop the disease later (i.e., at an older age) 23) .
A number of previous studies have reported that age was a major risk factor for mortality in patients with peripheral artery disease 5) . In this sense, the current finding that the mortality risk was linearly increased with age within the patient population is not surprising. However, the subsequent comparison with the national standard value revealed that younger patients had a higher risk ratio of mortality relative to citizens of the same age. Patients developing intermittent claudication at a younger age could suffer more greatly from the survival disparity than the same generation of citizens. One possible explanation for this paradoxical finding would be the accumulation of cardiovascular risk factors. Younger patients were more likely to excessively accumulate cardiovascular risk factors, which could lead to a poorer prognosis, than the same generation of citizens. They could have more room for improvement in terms of survival.
This study additionally found that patients aged ≥ 85 years had a lower mortality risk than the matched citizens. Although the true mechanisms remained unknown, a pathophysiological feature of intermittent claudication might be involved. Intermittent claudication is characterized as leg discomfort and pain that is accompanied by walking and is resolved with rest 1) . In other words, patients will not complain of intermittent claudication unless they walk around. The complaint of intermittent claudication is an indicator of dynamic activities in daily life. In general, non-ambulatory people who live a sedentary life are more common in the elderly population, and they are at a high risk of mortality 24) . Old patients with intermittent claudication, living an active or at least non-sedentary life, could be above average in vitality and survival among the citizens of the same age. In addition, among patients with intermittent claudication, older patients carried a relatively light burden of cardiovascular risk factor clustering, which might also work favorably for their prognosis.
This study had several limitations. First, the study population was limited to patients undergoing endovascular therapy for intermittent claudication and did not include those who received conservative treatment without revascularization. In clinical practice, revascularization will not be indicated when patients are very frail or have more severe comorbidities. Patients undergoing revascularization could be more energetic and have a lower mortality risk than those patients. Patients undergoing revascularization might be also more likely to receive optimal medical therapy at hospitals, which might lower the mortality risk. Second, the analysis only demonstrated a cross-sectional relationship between clinical features and age. Although the association of clinical profiles with age is suggestive of mechanisms of the disease onset, the causal relationships between these clinical profiles and disease onset remain unclear. Third, detailed information about comorbidities was limited. Data about past smoking and control of cardiovascular risk factors were not available. Fourth, this study analyzed Japanese patients. It remains unknown whether similar findings would be observed in other ethnic populations. Future studies in other countries are necessary to validate the current findings.
Conclusion
The mortality risk increased with age in patients undergoing femoropopliteal endovascular therapy due to intermittent claudication, but the risk ratio relative to the year-, sex-, and age-matched citizens decreased with age. Younger patients had a higher mortality risk than the matched citizens, whereas patients aged ≥ 85 years had a lower mortality risk than the matched citizens. Younger patients were more likely to accumulate cardiovascular risk factors.
Acknowledgements and Notice of Grant Support
This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Number JP18K16199.
Conflict of Interests
The authors declare that they have no conflicts of interest regarding this manuscript.
References
- 1).White C: Clinical practice. Intermittent claudication. N Engl J Med, 2007; 356: 1241-1250 [DOI] [PubMed] [Google Scholar]
- 2).Meijer WT, Hoes AW, Rutgers D, Bots ML, Hofman A and Grobbee DE: Peripheral arterial disease in the elderly: The Rotterdam Study. Arterioscler Thromb Vasc Biol, 1998; 18: 185-192 [DOI] [PubMed] [Google Scholar]
- 3).Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FG, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin JW, Patel RA, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D and Walsh ME: 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 2017; 135: e726-e779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Aboyans V, Ricco JB, Bartelink MEL, Bjorck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Rother J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I and Group ESCSD: 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J, 2018; 39: 763-816 [Google Scholar]
- 5).Feringa HH, Bax JJ, Hoeks S, van Waning VH, Elhendy A, Karagiannis S, Vidakovic R, Schouten O, Boersma E and Poldermans D: A prognostic risk index for long-term mortality in patients with peripheral arterial disease. Arch Intern Med, 2007; 167: 2482-2489 [DOI] [PubMed] [Google Scholar]
- 6).Jelnes R, Gaardsting O, Hougaard Jensen K, Baekgaard N, Tonnesen KH and Schroeder T: Fate in intermittent claudication: outcome and risk factors. Br Med J (Clin Res Ed), 1986; 293: 1137-1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Dormandy J, Mahir M, Ascady G, Balsano F, De Leeuw P, Blombery P, Bousser MG, Clement D, Coffman J, Deutshinoff A, Turpie AGG, Urai L and Verstraete M: Fate of the patient with chronic leg ischaemia. A review article. J Cardiovasc Surg (Torino), 1989; 30: 50-57 [PubMed] [Google Scholar]
- 8).Boccalon H: Intermittent claudication in older patients. Practical treatment guidelines. Drugs Aging, 1999; 14: 247-259 [DOI] [PubMed] [Google Scholar]
- 9).Aronow WS: Peripheral arterial disease in the elderly. Clin Interv Aging, 2007; 2: 645-654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H and Hirawa N: The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res, 2019; 42: 1235-1481 [DOI] [PubMed] [Google Scholar]
- 11).Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, Umemoto S, Egusa G, Ohmura H, Okamura T, Kihara S, Koba S, Saito I, Shoji T, Daida H, Tsukamoto K, Deguchi J, Dohi S, Dobashi K, Hamaguchi H, Hara M, Hiro T, Biro S, Fujioka Y, Maruyama C, Miyamoto Y, Murakami Y, Yokode M, Yoshida H, Rakugi H, Wakatsuki A, Yamashita S and Committee for Epidemiology and Clinical Management of Atherosclerosis.: Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. J Atheroscler Thromb, 2018; 25: 846-984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, Osawa H, Taguchi A, Tanizawa Y, Tobe K and Yoshioka N: Japanese Clinical Practice Guideline for Diabetes 2019. Diabetol Int, 2020; 11: 165-223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Japan’s Ministry of Health, Labor and Welfare. Life tables. https://www.mhlw.go.jp/toukei/saikin/hw/seimei/list54-57-02.html [in Japanese] (Accessed November 20, 2020). [Google Scholar]
- 14).Abola MTB, Golledge J, Miyata T, Rha SW, Yan BP, Dy TC, Ganzon MSV, Handa PK, Harris S, Zhisheng J, Pinjala R, Robless PA, Yokoi H, Alajar EB, Bermudez-Delos Santos AA, Llanes EJB, Obrado-Nabablit GM, Pestano NS, Punzalan FE and Tumanan-Mendoza B: Asia-Pacific Consensus Statement on the Management of Peripheral Artery Disease: A Report from the Asian Pacific Society of Atherosclerosis and Vascular Disease Asia-Pacific Peripheral Artery Disease Consensus Statement Project Committee. J Atheroscler Thromb, 2020; 27: 809-907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Tsujimura T, Takahara M, Iida O, Kohsaka S, Soga Y, Fujihara M, Mano T, Ohya M, Shinke T, Amano T, Ikari Y, J EVT, investigators JP, Japanese Association of Cardiovascular I and Therapeutics: In-Hospital Outcomes after Endovascular Therapy for Acute Limb Ischemia: A Report from a Japanese Nationwide Registry [J-EVT Registry]. J Atheroscler Thromb, 2021; 28: 1145-1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Takahara M, Iida O, Kohsaka S, Soga Y, Fujihara M, Shinke T, Amano T, Ikari Y, J EVT and investigators JP: Presentation Pattern of Lower Extremity Endovascular Intervention versus Percutaneous Coronary Intervention. J Atheroscler Thromb, 2020; 27: 761-768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Ko T, Higashitani M, Uemura Y, Utsunomiya M, Yamaguchi T, Matsui A, Ozaki S, Tobita K, Kodama T, Morita H and Komuro I: Clinical Outcome and Diverse Risk Factors for Different Therapeutic Target Locations of Peripheral Artery Disease. J Atheroscler Thromb, 2020; 27: 769-779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Iida O, Takahara M, Yamauchi Y, Shintani Y, Sugano T, Yamamoto Y, Kawasaki D, Yokoi H, Miyamoto A, Mano T, Nakamura M and investigators O: Impact of Hospital Volume on Clinical Outcomes after Aortoiliac Stenting in Patients with Peripheral Artery Disease. J Atheroscler Thromb, 2020; 27: 516-523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Matsuo Y, Kumakura H, Kanai H, Iwasaki T and Ichikawa S: The Geriatric Nutritional Risk Index Predicts Long-Term Survival and Cardiovascular or Limb Events in Peripheral Arterial Disease. J Atheroscler Thromb, 2020; 27: 134-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Kozuki A, Takahara M, Shimizu M, Kijima Y, Nagoshi R, Fujiwara R, Shibata H, Suzuki A, Soga F, Miyata T, Sakamoto Y, Seo H, Asada H, Isawa K, Higuchi K and Shite J: Outcomes of Dissection Angles as Predictor of Restenosis after Drug-Coated Balloon Treatment. J Atheroscler Thromb, 2021; 28: 954-962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Utsunomiya M, Takahara M, Fujihara M, Shiraki T, Kozuki A, Fukunaga M, Tan M, Yoshioka R, Tomoi Y, Mori S, Iwasaki Y, Sasaki S and Nakamura M: Effect of Target Lesion Revascularization on Restenosis Lesions of the Superficial Femoral Artery without Recurred Symptoms after Endovascular Therapy. J Atheroscler Thromb, 2021; 28: 643-655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Hata Y, Iida O, Asai M, Masuda M, Okamoto S, Ishihara T, Nanto K, Kanda T, Tsujumura T, Okuno S, Matsuda Y, Takahara M and Mano T: Risk Stratification for 2-Year Mortality in Patients with Chronic Limb-Threatening Ischemia Undergoing Endovascular Therapy. J Atheroscler Thromb, 2021; 28: 477-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).Takahara M, Iida O, Kohsaka S, Soga Y, Fujihara M, Shinke T, Amano T, Ikari Y and J- EVT and J-PCI investigators.: Diabetes mellitus and other cardiovascular risk factors in lower-extremity peripheral artery disease versus coronary artery disease: an analysis of 1,121,359 cases from the nationwide databases. Cardiovasc Diabetol, 2019; 18: 155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Clegg A, Young J, Iliffe S, Rikkert MO and Rockwood K: Frailty in elderly people. Lancet, 2013; 381: 752-762 [DOI] [PMC free article] [PubMed] [Google Scholar]