Abstract
Studies conducted during the pandemic revealed strong associations between gender and COVID-19 related fear and anxiety. Females perceive coronavirus as a greater threat to personal health and population than males. The aim of the current meta-analysis is to estimate gender difference in COVID-19 related fear and anxiety. The second purpose of this study is to clarify the role of potential moderators in COVID-19 fear and anxiety. For these reasons, studies published between March 2020 and October 2021 were searched in various databases (Web of Science, SCOPUS, PubMed, and Google Scholar). In total, 315 studies met the inclusion criteria, and 60 studies for COVID-19 related fear and 23 studies for COVID-19 related anxiety were included in the current study. Cohen's d effect size values were calculated based on these individual studies showing the difference between males and females in terms of COVID-19 related fear and anxiety. Results revealed that gender has a moderate and statistically significant effect on COVID-19 related fear (ES = 0.307) and anxiety (ES = 0.316) in favor of females. Moderator analyses showed that continent variable was a statistically significant moderator of gender difference in COVID-19 related fear and anxiety. The highest effect size of gender differences in COVID-related fear and anxiety were obtained from the studies conducted in Europe. However, other moderators (the average age of sample, culture, timing, and population) were not statistically significant. Although this meta-analysis has a few limitations, the findings showed that COVID-19 outbreak negatively affected females more.
Keywords: The fear of COVID-19, COVID-19 anxiety, Gender, Meta-analysis
1. Introduction
Although the COVID-19 disease has been considered a global epidemic since March 2020, it was seen at the end of 2019 (WHO, 2021a). Over 246 million cases and approximately 5 million deaths have been reported worldwide (WHO, 2021b) since the day it was first seen. Many countries had to take various measures to prevent the spread of the virus. Some of these measures are quarantine, restriction, wearing masks, avoiding public areas, and physical distancing. Although 2020 passed with these measures, the vaccines developed in 2021 allowed some measures to be stretched. Vaccines have started to prevent hospitalizations (WHO, 2021c). On the other hand, the rapid spread of SARS-CoV-2 has led to the development of various variants, and this has begun to limit the effectiveness of vaccines. People have been trying to cope with the pandemic process for about two years. The pandemic has affected human life in many ways. One of these effects is the psychological factor. Studies, especially when quarantine measures were taken in 2020, reported that individuals were mentally affected (Metin et al., 2021; Santabárbara et al., 2021a, Santabárbara et al., 2021b). In addition, many uncertainties during the pandemic process have caused anxiety and fear (Santabárbara et al., 2021a, Santabárbara et al., 2021b). Anxiety and fear are related emotions to each other. Fear is the primary reaction of human beings in the face of danger or threat (Ekman, 2007), and it mediates the survival of humans (Matsumoto & Hwang, 2013). It is claimed that there is a difference between the two affects, although anxiety also performs similar functions. Anxiety is about the dangers in the inner world; fear is also a reaction to the threat in the outside world (Akhtar, 2018).
The limited information about COVID-19, especially in the early stages of the pandemic, is one of the factors that cause increased COVID-19 related fear and anxiety. Meta-analysis studies on this issue showed that COVID-19 related anxiety and fear have a negative effect on people (Erbiçer et al., 2021; Lasheras et al., 2020; Santabárbara et al., 2021a, Santabárbara et al., 2021b; Wang et al., 2021). It is seen that COVID-19 anxiety and fear are positively correlated with depression, addiction, PTSD, insomnia, mood swing, and stress (Dubey et al., 2020; Kira et al., 2020; Özdin and Bayrak Özdin, 2020; Şahin et al., 2020), while negatively correlated with resilience, life satisfaction, and well-being (Alyami et al., 2021; Karataş and Tagay, 2021; Özmen et al., 2021; Satici et al., 2020). This negative situation may differ according to gender.
1.1. Gender and COVID-19 related fear and anxiety
Studies conducted during the pandemic found strong associations between gender and COVID-19 related fear and anxiety (Evren et al., 2020; Hossain et al., 2020; Padovan-Neto et al., 2021; Reznik et al., 2020; Sakib et al., 2020; Tsipropoulou et al., 2020). Females perceive coronavirus as a greater threat to personal health and population than males (Niño et al., 2021; Pérez-Fuentes et al., 2020). This is also the case for both COVID-19 related fear and anxiety. Many studies reported higher fear of COVID-19 and threat perception in females (Nguyen et al., 2020; Reznik et al., 2020; Sakib et al., 2020). Similar results were obtained in studies for COVID-19 anxiety (Akyildiz and Durna, 2021; Bhattacharya et al., 2021; Orrù et al., 2021). On the other hand, some studies showed that males have higher COVID-19 anxiety levels (Ashoor et al., 2021; Curtis et al., 2021; Saravanan et al., 2020; Srivastava et al., 2020). Also, many studies revealed males have higher fear of COVID-19 levels than females (Abdelgwad and Abdelaziz, 2021; Alnazly et al., 2021; Ghaderi et al., 2021; Osagiator Ariyo et al., 2021). In addition, Parlak and Akgün Şahin (2021) and Wakashima et al. (2020) found no gender difference in COVID-19 related fear and anxiety. Therefore, it would be useful to clarify gender differences on this matter. To our knowledge, the current study is the first and most extensive meta-analysis to estimate the effect size of gender difference in COVID-19 related fear and anxiety. Also, providing an overview of gender difference on COVID-19 related fear and anxiety can be an important guide in prevention and intervention programs to reduce the mental health effects of the COVID-19 outbreak.
1.2. Potential moderators
Various variables may have affected gender differences in COVID-19 related fear and anxiety. Target population was considered in this meta-analysis as a potential moderator. Studies have revealed inconsistent findings regarding gender differences in COVID-19 related fear and anxiety across different populations. For instance, according to Osagiator Ariyo et al. (2021), males had higher fear of COVID-19 than females in healthcare professionals. In contrast, Morales-Rodríguez (2021) found that females had higher fear of COVID-19 than males in university students. However, Parlak and Akgün Şahin (2021) found no gender differences in fear of COVID-19 level among the general population. In addition, studies conducted with different populations to determine COVID-19 related anxiety levels by gender revealed that males had higher levels of COVID-19 anxiety than females among the university students (Saravanan et al., 2020), whereas Lee et al. (2020) found that females had a higher level of COVID-19 anxiety in the general population. Yet, Ashoor et al. (2021) revealed no difference according to gender in hospital staff. Hence, target population was added as a categorical moderator in this meta-analysis to assess moderating effect of different populations. During the first wave of the COVID-19 outbreak, as we have misconceptions on how to prevent infection, individuals exhibit a stronger threat perception to disease. Especially, threat perception to COVID-19 was higher in females than males (Pérez-Fuentes et al., 2020). Threat perception plays an essential role in the psychological adjustment of individuals (Cui et al., 2020). First wave studies during the COVID-19 outbreak revealed that COVID-19 related fear and anxiety levels were higher in females (Sakib et al., 2020; Broche-Pérez et al., 2020; Evren et al., 2020; Srivastava et al., 2020). However, as individuals' knowledge level about preventing and controlling the COVID-19 disease has increased, gender differences may have changed in COVID-19 related fear and anxiety. Indeed, some recent studies revealed that there was no difference between the levels of COVID-19 related fear and anxiety in terms of gender (Magano et al., 2021; Mahmoud et al., 2021). Therefore, data collection time (timing) could be one of the moderators affecting gender differences in COVID-19 related fear and anxiety. Another potential moderator of the meta-analysis was the average age of the sample. The immune system weakens, and health problems increase with aging. This leads to more deaths related to COVID-19 as age increase (WHO, 2021d). Global data shows that death rates related to COVID-19 are higher in males than in females (The Sex, Gender, and COVID-19 Project, 2021). In addition, females live longer than males due to genetic structure, chromosomes, hormones, and other ecological factors (Austad, 2006; Eskes and Haanen, 2007; Vina and Borras, 2010; Zarulli et al., 2018). For that reason, age may moderate gender difference in COVID-19 related fear and anxiety. In addition, cultural factors might influence individuals' psychological responses to diseases or epidemics (Fincher et al., 2008; Kim et al., 2016). One of the most important cultural factors is the categorization of collectivism and individualism (Schimmack et al., 2005; Triandis et al., 1988). While a desire for self-sufficiency and independence characterizes individualistic orientation, collectivistic orientation emphasizes the traditional understanding of males as masculine and females as feminine (Chun et al., 2006; Kim et al., 1994; Shafiro et al., 2003; Williams and Best, 1990). The cultural orientation of the country in which the study was conducted may lead to gender differences in COVID-19 related fear and anxiety. Therefore, culture (individualism vs. collectivism) was added in the meta-analysis as a categorical moderator. Finally, continent was added in the meta-analysis as a potential moderator to assess the moderating effect of different countries. In most studies conducted in North America, females had higher levels of COVID-19 related fear and anxiety than males (Barbosa-Camacho et al., 2021; Grande and Doyle-Baker, 2021; García-Reyna et al., 2021; Gélinas et al., 2021; Landa-Blanco et al., 2021; Lee et al., 2020; Pérez-Fuentes et al., 2020; Ojalehto et al., 2021). In addition, studies conducted in Europe, female's COVID-19 related fear and anxiety levels were higher (Bakioğlu et al., 2020; Kaçoğlu et al., 2021; Morales-Rodríguez, 2021; Orrù et al., 2021; Tsipropoulou et al., 2020; Ypsilanti et al., 2021). On the other hand, some studies conducted in Middle East countries showed that males had higher levels of COVID-19 related fear and anxiety than females (Abdelgwad and Abdelaziz, 2021; Alnazly et al., 2021; Ashoor et al., 2021; Ghaderi et al., 2021; Saravanan et al., 2020). These studies revealed inconsistent findings regarding gender differences in COVID-19 related fear and anxiety across different continents. To clarify this, it would be useful to add continent as a categorical moderator. Overall, the average age of sample, culture, continent, timing, and target population were considered potential moderators as these variables were treated as moderators in the studies included in this meta-analysis (e.g., Alothman et al., 2021; Chorwe-Sungani, 2021; Gélinas et al., 2021; Ojalehto et al., 2021; Saravanan et al., 2020; Wakashima et al., 2020; Yalçın et al., 2022; Ypsilanti et al., 2021).
Based on all these, the second purpose of the current research is to examine the effect of the potential moderators on gender difference in COVID-19 related fear and anxiety. For these purposes, the following questions were addressed:
Research Question 1: Is there a statistically significant gender difference in COVID-19 related fear and anxiety?
Research Question 2: How do gender differences in COVID-19 related fear and anxiety change as a function of moderators?
2. Method
The PRISMA statement was followed in reporting this meta-analysis (Page et al., 2021).
2.1. Literature search
Literature search was conducted between September and October 2021. PubMed, Web of Science, SCOPUS, and Google Scholar databases were used to locate all relevant studies. To estimate gender difference in COVID-19 related fear, the studies cited The Fear of COVID-19 Scale (FCV-19-S; Ahorsu et al., 2020) were examined in these databases. In addition, references of the studies included were reviewed to identify the studies that might be relevant. Keywords used for the search were: “Fear of COVID-19 Scale”, “COVID-19 Related Fear”, “Fear of COVID-19”, and “COVID-19 Fear”. The FCV-19S (Ahorsu et al., 2020) is the only tool used in the meta-analysis to assess gender differences in fear of COVID-19. The FCV-19S was developed by Ahorsu et al. (2020) to measure individuals' fear of COVID-19. The scale consists of 7 items of 5-point Likert type. The lowest score that can be achieved from the scale is 7; the highest score is 35. The higher score on the scale means that the fear of COVID-19 is high. Some of the scale items are: “I am most afraid of coronavirus-19”; “It makes me uncomfortable to think about coronavirus-19”.
To evaluate gender differences in COVID-19 related anxiety, studies cited Coronavirus Anxiety Scale (CAS; Lee, 2020) were also examined in these databases. In addition, references of included studies were reviewed to find the studies that might be relevant. Keywords used for the search were: “Coronavirus Anxiety”, “Coronavirus Anxiety Scale”, “COVID-19 Related Anxiety”, “COVID-19 Anxiety”, and “COVID-19 Anxiety Scale”. CAS (Lee, 2020) is the only tool used in the meta-analysis to assess gender differences in COVID-19 related anxiety. CAS was developed by Lee et al. (2020) to assess individuals' COVID-19 related anxiety. The scale consists of five items of 5-point Likert type, ranging from never (0) to almost every day (4). The lowest and highest scores can be obtained from the scale is zero and twenty, respectively. A higher score on the scale means higher COVID-19 related anxiety. Some of the scale items are: “I had trouble falling or staying asleep because I was thinking about the coronavirus”, “I lost interest in eating when I thought about or was exposed to information about the coronavirus”.
Although there are other measures to assess COVID-19 related fear and anxiety (e.g., COVID-19 Anxiety Syndrome Scale – Nikčević and Spada, 2020; Brief Coronavirus Threat Scale – Chiacchia et al., 2022; COVID-19 Phobia Scale – Arpaci et al., 2020) the more well-established and most frequently reported scales (FCV-19S and CAS) were selected in this meta-analysis. In addition, these scales have robust psychometric properties and are reliable and valid in assessing COVID-19 related fear and anxiety (Ahorsu et al., 2020; Lee, 2020). As we conducted a meta-analysis of the means produced from these two scales, combining the average scores from different scales with different metrics may not be meaningful. Thus, we decided not to include the studies where the COVID-19 related fear and anxiety were assessed with other scales.
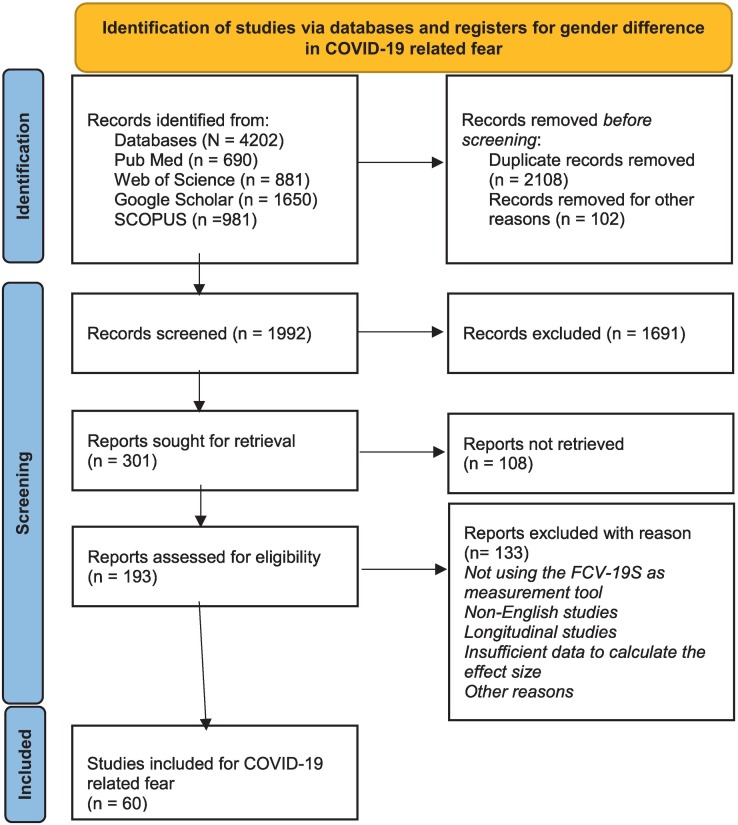
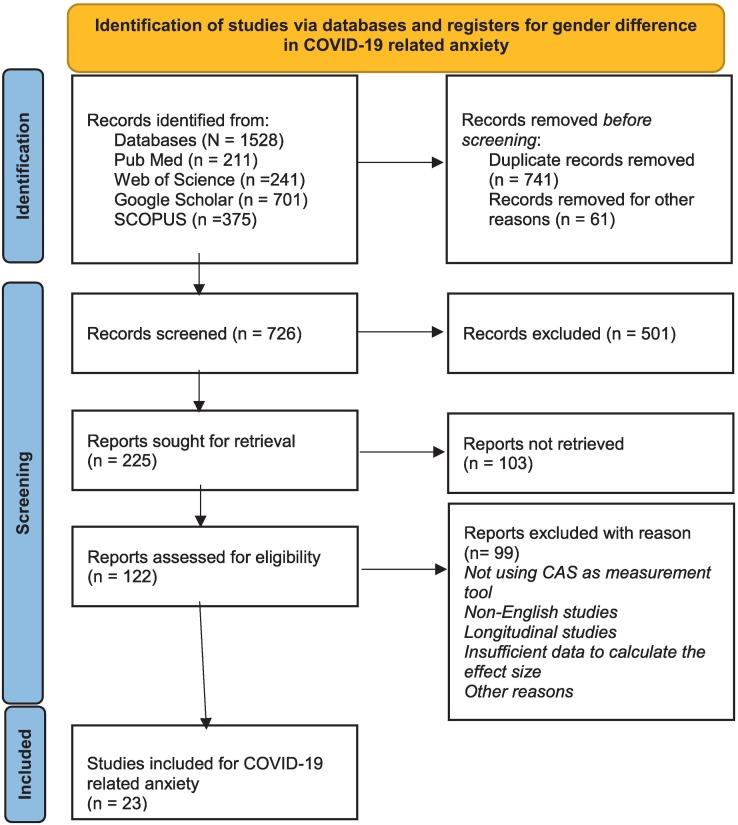
The criteria used to determine which article to include were: 1) Examining COVID-19 related fear or anxiety during COVID-19 pandemic, 2) using The FCV-19S or CAS as the measurement tool, 3) studies adapting the FCV-19S or CAS to different languages, 4) cross-sectional studies, 5) quantitative studies, 6) studies published in English, 7) the mean and standard deviation of COVID-19 related fear or anxiety were calculated by gender. Exclusion criteria: 1) Studies did not use the FCV-19S or CAS, 2) longitudinal studies, 3) non-English studies, 4) reports, 5) case reports, 6) qualitative studies, 7) dissertation/thesis, 8) conference paper, 9) school project 10) books or e-books 11) experimental studies, and 12) insufficient data to calculate the effect size. Sixty studies were determined for COVID-19 related fear and 23 studies for COVID-19 related anxiety based on the inclusion and exclusion criteria included in the meta-analysis. Results of the literature review are shown in Fig. 1, Fig. 2 .
Fig. 1.
PRISMA flow diagram for literature search.
Fig. 2.
PRISMA flow diagram for literature search.
2.2. Quality assessment and coding
Quality Appraisal Tool for Cross-Sectional Studies (AXIS) was used to evaluate the quality of the studies included in this meta-analysis (Downes et al., 2016). Critical appraisal (CA) was developed for use in assessing observational cross-sectional studies. There are many key areas to CA including study design, sample size justification, target population, sampling frame, sample selection, measurement validity and reliability, and overall methods. These key areas need to be identified in CA for good reporting of the study, making it difficult to assess relevance and bias if the study is under-reported. Appraisal of Cross-sectional Studies consisted of 20 items. CA has areas to record a “Yes”, “No” or “Unclear/Not known” answer for each question. The items were coded as Unclear/Not known “0”, No “0”, and Yes “1”. A higher score obtained indicated a better quality of the study. The scores obtained from the studies included in the meta-analysis were 75% and above (see Appendix 1). Quality Assessment was performed by two different authors. It is also recommended that at least two independent reviewers conduct the quality assessment process and increase inter-rater reliability and study validity. Afterward, quality assessments done by two independent raters were compared with a Kappa coefficient (0.84), and disagreements were resolved by consensus.
A coding key was created to identify studies to be included in the meta-analysis and to facilitate data analysis. The first author's name, publication year, sample size (n), data collection time, country, female proportion, quality of the studies and to estimate gender difference in COVID-19 related fear and anxiety, calculated values for two genders (mean, SD, and n for females and males) were entered into the coding sheet. In addition, potential moderators including the average age of sample, culture, continent, timing, and target population were also collected from the studies included in this meta-analysis. The coding key was coded by two independent researchers. Then, the coding sheets were compared to avoid errors in data entry. To establish intercoder reliability, an agreement index was calculated between the codes done by two independent raters (first two authors). An intercoder reliability of 0.95 was achieved. Disagreements between two raters were resolved before proceeding to analyses.
2.3. Data analysis
A random effects meta-analysis model was used to estimate overall effect size value in this study. Cohen's d coefficient was calculated for each included study to estimate gender difference in COVID-19 related fear and anxiety. Positive effect size values indicate that there is an effect in favor of females, and negative values indicates that there is an effect in favor of males in terms of both fear and anxiety variables. The confidence level was taken as 95% in all calculations regarding the effect size. The effect sizes were interpreted as follow: 0.20 = small; 0.50 = medium; and 0.80 = large (Cohen, 1988).
Q test was used to assess heterogeneity between studies included in the meta-analysis (Borenstein et al., 2011). I 2 value was used as another criterion for heterogeneity in the meta-analysis. I 2 value was interpreted as follows: 25% low heterogeneity; 50% medium heterogeneity; and 75% high heterogeneity (Cooper et al., 2009). Restricted maximum likelihood was used as a heterogeneity variance estimator (Langan et al., 2015).
We performed the analog to the ANOVA and meta-regression analyses to detect the possible sources of heterogeneity between the studies. It is recommended to have two or more studies in each subgroup to perform analog to the ANOVA, and ten or more studies to perform meta-regression analysis (Borenstein et al., 2011). Moderator analyses were performed with the variables meeting these criteria. Possible moderators were: the average age of sample, culture, continent, timing, and target population. The primary moderator was the average age of the sample. Typically, the average age of sample was used and if the age range of the sample was not available, coded as Not Available (N.A.). Culture was coded as individualism or collectivism. Hofstede's classification (Hofstede's Insights, 2021) was used to identify whether the country from which the sample was collected was characterized by individualistic or collectivistic orientation (e.g., Turkey, Iran, China, Brazil, Mexico coded as collectivism; Canada, Spain, USA, Portugal coded as individualism). The studies included in the meta-analysis collected data from nearly all continents except for Oceania. Effect sizes were coded into five categories of continents (Africa, Asia, Europe, North America, and South America) and one region (Middle East). For example, Portugal, Spain, UK, and Turkey were categorized as Europe; India, China, Malaysia, and Philippines were categorized as Asia; Canada, USA, Mexico, and Cuba were categorized as North America; Peru, and Brazil were categorized as South America; and United Arab Emirates, Saudi Arabia, Egypt, and Iran were categorized as Middle East. As SARS-CoV-2 firstly was reported in Wuhan, Hubei province, China on December 2019 (Wang and Zhang, 2020), we included the studies from January 2020 onwards. Data collection time (timing) was coded chronologically (e.g., January 2020 coded as “1”; February 2020 “2”; March 2020 “3”; January 2021 “13”). If data were collected over two or more months, the average of the numbers given to each month was calculated (i.e., between March and April 2020 coded as “3.5”). The studies included in the meta-analysis consisted of different populations. Target population was coded into nine categories (general population, hospital staff, mental health professionals, medical, healthcare students, academics, university students, high school personnel, older adults). For instance, doctor, nurse, and other hospital worker samples were categorized as hospital staff; psychologist, counselor, social worker samples were categorized as mental health professionals; and college students' sample except medical and nursing students were categorized as university students.
In this meta-analysis, possibility of publication bias was assessed using several methods including fail-safe N, Funnel plot, Egger's regression test and Begg and Mazumdar's rank correlation test. The calculated Fail-safe N value < 5k +10 (k = the number of observed effect sizes) indicates that the meta-analysis result may be susceptible to publication bias (Rosenthal, 1979). Nonsignificant p-values obtained from two tests indicate the lack of publication bias. In the funnel plot, an asymmetrical distribution is expected in case of publication bias (Borenstein et al., 2011). All the analyses were conducted using the Comprehensive Meta-Analysis (CMA Version 3.0) software package in this study.
3. Results
3.1. Study characteristics
Eighty-three studies having 86,167 participants were included in the meta-analysis. Of these studies, 75,176 participants were used for the FCV-19S, 10,991 participants were used for CAS. The FCV-19S was used as the data collection tool in sixty of these studies (87.2%), while CAS was used in twenty-three studies (12.8%).
Eighteen (30%) studies were conducted in Europe, twenty (33.33%) in Asia, twelve (20%) in North and South America, eight (13.33%) in the Middle East, and two (0.33%) in Africa for the FCV-19S. In addition, twelve of the studies (20%) were published in 2020 and forty-eight (80%) in 2021. It has been reported that data from fifty-eight studies (96.67%) were collected in 2020, and two studies (3.33%) in 2021. Data from thirty studies (50%) were collected from the general population, twelve studies (20%) from hospital staff, three studies (5%) from healthcare workers and students, three studies (5%) from medical, one study (1.66%) from high school personnel, ten studies (16.66%) from university students, and one study (1.66%) from elderly individuals. The average age range of the participants was between 20 and 48. Finally, the cultures of the participants in the four studies (6.66%) were individualistic, while those of the fifty-six studies (93.33%) were collectivist.
Ten (43.47%) studies were conducted in Europe, three (13.04%) in Asia, six (26.08%) in North and South America, two (8.69%) in the Middle East, and two (8.69%) in Africa for the CAS. In addition, four of the studies (17.39%) were published in 2020, and nineteen (82.61%) in 2021. It has been reported that data from fifteen studies (65.21%) were collected in 2020, and one study (4.34%) in 2021. No information was reported regarding the time of data collection in seven studies (30.43%). Data from twelve studies (52.17%) were collected from the general population, six studies (26.08%) from hospital staff, one study (4.34%) from healthcare students, one study (4.34%) from medical professionals, one study (4.34%) from mental health professionals, one study (4.34%) from university students, and one study (4.34%) from academia. The average age range of the participants was between 29 and 65. Finally, the cultures of the participants in six studies (26.08%) were individualistic, while those of seventeen studies (73.91%) were collectivist. Detailed information about the studies included is presented in Table 1 .
Table 1.
Study characteristics.
| Author | Sample size | Timing of COVID-19 | Country | Continent | Target population | Sample age (mean) |
|---|---|---|---|---|---|---|
| Studies included in the meta-analysis for gender and COVID-19 related fear | ||||||
| Nguyen et al., 2020 | 5423 | 4 | Vietnam | Asia | University students | 22.00 |
| Sakib et al., 2020 | 8550 | 4 | Bangladesh | Asia | General population | 25.50 |
| Doshi et al., 2020 | 1499 | 4 | India | Asia | General population | N.A. |
| Pérez-Fuentes et al., 2020 | 772 | 4.5 | Cuba | North America | General population | 36.00 |
| García-Reyna et al., 2020 | 2860 | N.A. | Mexico | North America | Hospital staff | N.A. |
| Tsipropoulou et al., 2020 | 2970 | N.A. | Greece | Europe | General population | N.A. |
| Hossain et al., 2020 | 2157 | 3.5 | Bangladesh | Asia | General population | 33.48 |
| Haktanir et al., 2020 | 668 | N.A. | Turkey | Europe | General population | 31.04 |
| Bakioğlu et al., 2020 | 960 | 3.5 | Turkey | Europe | General population | 29.74 |
| Abdelgwad and Abdelaziz, 2021 | 382 | N.A. | Egypt | Middle East | University students | 21.93 |
| Aksoy et al., 2021 | 1060 | 7.5 | Turkey | Europe | General population | 29.76 |
| Alnazly et al., 2021 | 365 | 8 | Jordan | Middle East | Hospital staff | N.A. |
| Alothman et al., 2021 | 554 | 5.5 | Saudi Arabia | Middle East | General population | 34.5 |
| Antonio and Elizabeth, 2021 | 438 | N.A. | Mexico | North America | General population | N.A. |
| Aslam et al., 2021 | 250 | N.A. | Pakistan | Asia | General population | 24.02 |
| Aslan and Dinç, n.d. | 845 | 8 | Turkey | Europe | Hospital staff | N.A. |
| Barbosa-Camacho et al., 2021 | 1216 | 5 | Mexico | North America | General population | 37.5 |
| Broche-Pérez et al., 2020 | 772 | 4.5 | Cuba | North America | General population | 36 |
| Bukhari et al., 2021 | 200 | N.A. | Pakistan | Asia | General population | N.A. |
| Cervantes-Guevara et al., 2021 | 1529 | 7 | Mexico | North America | High school personnel | N.A. |
| De los Santos and Labrague, 2021 | 385 | 6 | Philippines | Asia | Hospital staff | 32.65 |
| De Los Santos et al., 2021 | 261 | 6 | Philippines | Asia | Healthcare students | 20.7 |
| Doğan et al., 2021 | 135 | N.A. | Turkey | Europe | Medical | 47.39 |
| Elsayed and Ghazi, 2021 | 275 | 6.5 | Egypt | Middle East | Healthcare students | N.A. |
| Ghaderi et al., 2021 | 457 | 4.5 | Iran | Middle East | General population | 37.86 |
| Grande and Doyle-Baker, 2021 | 680 | 13.5 | Canada | North America | University students | 23 |
| Green et al., 2021 | 608 | 9 | Pakistan | Asia | University students | 24.76 |
| Gélinas et al., 2021 | 1517 | N.A. | Canada | North America | Hospital staff | 41.11 |
| Jafari-Oori et al., 2021 | 350 | N.A. | Iran | Middle East | General population | N.A. |
| Jan et al., 2021 | 530 | 4 | Pakistan | Asia | General population | N.A. |
| Kaçoğlu et al., 2021 | 176 | 12 | Turkey | Europe | University students | 22.6 |
| Kakodkar et al., 2021 | 198 | 4.5 | India | Asia | University students | N.A. |
| Karadem et al., 2021 | 527 | N.A. | Turkey | Europe | Hospital staff | 35.7 |
| Karahan et al., 2021 | 138 | 12.5 | Turkey | Europe | Hospital staff | 37.6 |
| Kardaş, 2021 | 679 | 9 | Turkey | Europe | General population | 26.7 |
| Krägeloh et al., 2021 | 1029 | 4.5 | Saudi Arabia | Middle East | General population | 33.7 |
| Landa-Blanco et al., 2021 | 595 | N.A. | Honduras | North America | General population | 25.1 |
| Mahmoud et al., 2021 | 382 | 11.5 | Egypt | Middle East | Hospital staff | 33.83 |
| Malik et al., 2021 | 421 | 4.5 | Pakistan | Asia | Hospital staff | 30.81 |
| Mamun, 2021 | 10,052 | 4 | Bangladesh | Asia | General population | 26.95 |
| Mistry et al., 2021 | 1032 | 10 | Bangladesh | Asia | Older adults | N.A. |
| Montag et al., 2021 | 932 | N.A. | China | Asia | University students | 21.1 |
| Osagiator Ariyo et al., 2021 | 413 | N.A. | Nigeria | Africa | Hospital staff | 38.7 |
| Öztürk Altınayak and Yılar Erkek, 2021 | 1749 | 11 | Turkey | Europe | General population | 32.9 |
| Parlak and Akgün Şahin, 2021 | 70 | N.A. | Turkey | Europe | Medical | N.A. |
| Siddique et al., 2021 | 521 | N.A. | Bangladesh | Asia | General population | 24.78 |
| Sotomayor-Beltran et al., 2021 | 449 | 9 | Peru | South America | General population | 40.75 |
| Sürme et al., 2021 | 639 | 11 | Turkey | Europe | Medical | 46.12 |
| Tan et al., 2021 | 352 | N.A. | Turkey | Europe | University students | 20.04 |
| Ünver and Yeniğün, 2021 | 202 | N.A. | Turkey | Europe | Hospital staff | 35.54 |
| Wakashima et al., 2020 | 450 | 4 | Japan | Asia | General population | 48.13 |
| Yaşar Can and Dilmen Bayar, 2021 | 171 | N.A. | Turkey | Europe | Hospital staff | N.A. |
| Midorikawa et al., 2021 | 6750 | 8 | Japan | Asia | General population | N.A. |
| Morales-Rodríguez, 2021 | 180 | 4.5 | Spain | Europe | University students | 20.76 |
| Giordani et al., 2021a | 4638 | 7 | Brazil | South America | General population | 41.50 |
| Kassim et al., 2021 | 255 | 5.5 | Malaysia | Asia | General population | N.A. |
| Giordani et al., 2021b | 387 | 9.5 | Mozambic | Africa | General population | 34.50 |
| Ahammed et al., 2021 | 1317 | 4 | Bangladesh | Asia | University students | N.A. |
| Yalçın et al., 2022 | 588 | 6.5 | Turkey | Europe | General population | 30.42 |
| Studies included in the meta-analysis for gender and COVID-19 related anxiety | ||||||
| Magano et al., 2021 | 1122 | 10.5 | Portugal | Europe | General population | 31.90 |
| van de Venter et al., 2021 | 248 | N.A. | South Africa | Africa | Hospital staff | N.A. |
| Ypsilanti et al., 2021 | 101 | 5.5 | UK | Europe | General population | 29.10 |
| Sarıgedik and Bahar Ölmez, 2021 | 407 | 13.5 | Turkey | Europe | General population | 29.54 |
| Guzel et al., 2021 | 370 | 12 | Turkey | Europe | Healthcare students | N.A. |
| Öztekin et al., 2021 | 479 | N.A. | Turkey | Europe | General population | N.A. |
| Ojalehto et al., 2021 | 438 | N.A. | USA | North America | General population | 30.29 |
| Eşkut et al., 2021 | 247 | N.A. | Turkey | Europe | Medical | 45.95 |
| Chorwe-Sungani, 2021 | 102 | 8 | Malawi | Africa | Hospital staff | 36.70 |
| García-Reyna et al., 2021 | 2140 | 5.5 | Mexico | North America | Hospital staff | 36.10 |
| Curtis et al., 2021 | 281 | 7.5 | USA | North America | General population | 64.69 |
| Çakmak and Öztürk, 2021 | 162 | N.A. | Turkey | Europe | Hospital staff | 36.9 |
| Ashoor et al., 2021 | 129 | 6 | Saudi Arabia | Middle East | Hospital staff | N.A. |
| Bhattacharya et al., 2021 | 154 | N.A. | India | Asia | Mental health workers | 33.89 |
| Broche-Pérez et al., 2021 | 373 | 8 | Cuban | North America | General population | 32.1 |
| Akyildiz and Durna, 2021 | 290 | 8 | Turkey | Europe | Academics | N.A. |
| Padovan-Neto et al., 2021 | 505 | 8 | Brazil | South America | General population | N.A. |
| Srivastava et al., 2020 | 66 | 6.5 | India | Asia | General population | N.A. |
| Orrù et al., 2021 | 697 | 10 | Italy | Europe | General population | N.A. |
| Labrague and De Los Santos, 2021 | 736 | 9.5 | Philippines | Asia | Hospital staff | 31.9 |
| Saravanan et al., 2020 | 433 | 5 | UAE | Middle East | University students | 21 |
| Lee et al., 2020 | 398 | N.A. | USA | North America | General population | 35.91 |
| Evren et al., 2020 | 1113 | 5 | Turkey | Europe | General population | 43.32 |
3.2. Publication bias
Before proceeding to the main findings of meta-analyses, possibility of publication bias was assessed using the methods mentioned above. First, the fail-safe N number was calculated to be 1074 and 7831 for anxiety and fear, respectively. Such large values indicated a lack of publication bias. This finding was also confirmed by the results of the two tests based on regression and rank correlation. Both of Egger's regression test and Begg and Mazumdar's rank correlation test produced non-significant p-values (p > .05) for anxiety and fear analyses. So, we have additional evidence for the lack of publication bias. In addition, visual inspections were conducted using funnel plot of anxiety and fear. As shown in Figs. S1 and S2, the funnel plot for the standard error vs. Cohen's d values showed that a weak publication bias was detected. Overall, we can conclude that publication bias would not be a concern for the present study.
3.3. Heterogeneity and meta-analyses of effect sizes
The mean effect size estimates under the random-effects model and heterogeneity statistics for anxiety and fear variables are presented in Table 2 . Under the random-effects model, the mean ES value for anxiety was found to be 0.316, with a 95% confidence interval of 0.183–0.449. The test of the null (when the mean ES is 0.0) yielded a Z-value of 4.664 and a corresponding p-value of <.001. The Q-statistics was found to be significant (p < .001, Q = 208.325 with df = 22) and failed to reject the hypothesis of homogeneity at α = 0.05. In addition, I 2 percentage was calculated as 89.440. Thus, these findings provided evidence for heterogeneity. Similarly, the mean ES value for fear was found to be 0.307, with a 95% confidence interval of 0.255–0.359 under the random-effects model. The test of the null produced a Z-value of 11.622 and a corresponding p-value of <.001. The Q-statistics was found to be significant (p < .001, Q = 578.342 with df = 59) and I 2 percentage was calculated as 89.798 which indicated the heterogeneity between studies. Besides, forest plots (Figs. S3 and S4) presented can be examined to see the distribution of effect sizes obtained from each study included in the meta-analysis.
Table 2.
Results of the random effects meta-analyses.
| Measures | k | N | ESr | 95% CI | Z | pz | Cochran's Q | pQ | I2 (%) |
|---|---|---|---|---|---|---|---|---|---|
| Anxiety | 23 | 10,991 | 0.316 | [0.183, 0.449] | 4.664 | <.001 | 208.325 | <.001 | 89.440 |
| Fear | 60 | 75,176 | 0.307 | [0.255, 0.359] | 11.622 | <.001 | 578.342 | <.001 | 89.798 |
Note. k = number of studies, Cochran's Q = tests of heterogeneity, N = number of participants in all studies, CI = confidence interval.
3.4. Moderator analyses
Possible sources of heterogeneity can be examined with analog to the ANOVA and meta-regression approaches in the presence of heterogeneity (Lipsey and Wilson, 2001). Thus, these approaches were used for anxiety and fear variables in this study. First, the analog to the ANOVA method was used to examine whether the categorical moderators (continent, culture, and target population) can be responsible for the heterogeneity between studies. Second, meta-regression was used for the analyses with continuous moderators (i.e., age, and timing).
Results of the analog to the ANOVA method for anxiety and fear variables are presented in Table 3 . The Q-Between (Q B) line tells us that the difference between groups is statistically significant in terms of average effect size. To investigate the effect of continent, we divided the continent variable into five categories for anxiety variable: Africa (k = 2), Asia (k = 3), Europe (k = 10), Middle East (k = 2), and North America (k = 5). The moderator analysis showed that the combined effect size values between five continents were statistically significantly different (Q = 12.815, df = 4, p = .012). The statistically significantly p-value indicated significant heterogeneity in effect sizes among five continents. The estimated mean effect size was the highest (i.e., 0.478) for Europe while the lowest (i.e., 0.189) for North America. The other postulated categorical moderators (culture and target population) did not influence the effect of gender on anxiety. To investigate the effect of culture on anxiety, we divided the culture variable into two categories for anxiety variable: Collectivism (k = 17), and individualism (k = 6). Similarly, we divided the target population variable into two categories for anxiety variable: General (k = 12), and hospital staff (k = 6) to investigate the effect of population. The moderator analysis showed that there were no differences in terms of culture (Q = 0.208, df = 1, p = .648) and target population (Q = 0.137; df = 1; p = .711). The statistically nonsignificant p-values indicate the lack of significant heterogeneity in effect sizes among the subgroups.
Table 3.
Results of categorical moderator analyses.
| Outcome | Predictors | Categories | k | d | 95% CI | Q-between |
|---|---|---|---|---|---|---|
| COVID-19 anxiety | Continent | Africa | 2 | 0.370⁎ | [0.071, 0.699] | 12.815⁎ |
| Asia | 3 | 0.360 | [−0.004, 0.725] | |||
| Europe | 10 | 0.478⁎⁎⁎ | [0.319, 0.637] | |||
| Middle East | 2 | −0.392 | [−1.099, 0.314] | |||
| North America | 5 | 0.189⁎⁎⁎ | [0.083, 0.295] | |||
| Culture | Collectivism | 17 | 0.326⁎⁎⁎ | [0.149, 0.504] | 0.208 | |
| Individualism | 6 | 0.274⁎⁎⁎ | [0.132, 0.415] | |||
| Population | General | 12 | 0.331⁎⁎⁎ | [0.228, 0.434] | 0.137 | |
| Hospital staff | 6 | 0.296⁎⁎⁎ | [0.140, 0.352] | |||
| COVID-19 fear | Continent | Asia | 20 | 0.288⁎⁎⁎ | [0.226, 0.351] | 9.050⁎ |
| Europe | 18 | 0.390⁎⁎⁎ | [0.255, 0.525] | |||
| Middle East | 8 | 0.048 | [−0.157, 0.254] | |||
| North America | 10 | 0.367⁎⁎⁎ | [0.258, 0.476] | |||
| Culture | Collectivism | 56 | 0.296⁎⁎⁎ | [0.243, 0.349] | 2.128 | |
| Individualism | 4 | 0.466⁎⁎⁎ | [0.244, 0.688] | |||
| Population | General | 30 | 0.316⁎⁎⁎ | [0.246, 0.387] | 1.593 | |
| Hospital staff | 13 | 0.248⁎⁎⁎ | [0.121, 0.375] | |||
| Medical | 3 | 0.357⁎⁎⁎ | [0.123, 0.591] | |||
| University | 10 | 0.360⁎⁎⁎ | [0.220, 0.501] |
Note. k = number of studies, Cochran's Q = tests of heterogeneity, CI: confidence interval.
p < .05.
p < .001.
Similar analyses were also conducted for fear variable. To investigate the effect of continent, we divided the continent variable into four categories: Asia (k = 20), Europe (k = 18), Middle East (k = 8), and North America (k = 10). The moderator analysis showed that the combined effect size values between four continents were statistically significantly different (Q = 9.050, df = 3, p = .029). The statistically significantly p-value indicated significant heterogeneity in effect sizes among four continents. The estimated mean effect size was the highest (i.e., 0.390) for Europe while the lowest (i.e., 0.048) for Middle East. The other postulated categorical moderator (i.e., culture and target population) did not influence the effect of gender on fear. To investigate the effect of type of culture, we divided the examined culture variable into two major categories: Collectivism (k = 56) and individualism (k = 4). Similarly, we divided the target population variable into four categories for fear variable: General (k = 30), hospital staff (k = 13), medical (k = 3), and university students (k = 10). The moderator analysis showed that there were no statistically significant differences in terms of culture (Q = 2.128, df = 1, p = .145) and target population (Q = 1.593; df = 3; p = .661). The statistically nonsignificant p-values indicated the lack of significant heterogeneity in effect sizes among the subgroups. It should be noted that non-significant results in this study may occur due to unevenly distributed cells.
To investigate the effect of continuous moderators (i.e., age and timing) on anxiety and fear variables, we conducted meta-regression analyses. Two separate meta-regression models with a random effects model using unrestricted maximum likelihood estimation were analyzed with these two continuous moderators for both anxiety and fear outcomes. Results of the meta-regression analyses for anxiety and fear variables are presented in Table 4 . As shown in Table 4, no significant effect was found for two continuous moderators (age and timing) in terms of anxiety and fear outcomes (p < .05).
Table 4.
Results of meta regression analyses for anxiety and fear.
| Predictors | COVID-19 anxiety |
COVID-19 fear |
||||
|---|---|---|---|---|---|---|
| B | S.E. | z | B | S.E. | z | |
| Average age of sample | 0.002 | 0.008 | 0.232 | −0.002 | 0.005 | −0.523 |
| Timing | 0.058 | 0.038 | −0.594 | 0.012 | 0.014 | 0.382 |
Note. β = regression coefficient; S.E. = standard error; z = Significance of moderator.
4. Discussion
The findings of the meta-analysis showed that COVID-19 related fear and anxiety was higher in females. These findings are consistent with previous studies, reporting that female is more anxious than males (Robichaud et al., 2003; Stavosky & Borkovec, 1987). In addition, it is known that females have higher rates than males in other psychological disorders related to anxiety and fear (Kessler, 2003; Pigott, 1999). In the pandemic, the female gender was significantly associated with higher stress, anxiety, and depression. In addition, the psychological effects of the epidemic were greater in females. Although some studies showed that males had more COVID-19 anxiety than females (e.g., Ashoor et al., 2021; Curtis et al., 2021; Saravanan et al., 2020), it was found that females had more in this meta-analysis.
Females have more anxiety and fears than males is a situation observed pre-pandemic (e.g., McLean et al., 2011; Pigott, 1999; Wenjuan et al., 2020). Various reasons have been reported for females to be more anxious than males (Rossi et al., 2020; Wang et al., 2020). One of these reasons for the higher fear and anxiety scores of females may be due to their relationship with gender roles (Block, 1983; Zalta & Chambless, 2012). Females' anxiety reactions may have been higher because expressing distress is more encouraged (Chambless & Mason, 1986). Studies showed that females had a higher perception of COVID-19 risk and saw this pandemic as more dangerous for the population (Niño et al., 2021; Nguyen et al., 2020; Reznik et al., 2020; Sakib et al., 2020). Besides, females express their emotions easily, whereas males tend to suppress them and appear strong (Bakioğlu et al., 2020). Another reason females have high levels of fear and anxiety may be related to biological factors. In other words, hormonal factors and reproductive cycles may mediate increasing females' anxiety-related feelings (Pigott, 1999). These biological differences between males and females seem to be significant in explaining the difference in anxiety-related feelings. Our results are consistent with these pre-pandemic findings-females more anxious than males. COVID-19 related fear and anxiety as a new phenomenon may be related to the emergence of existing anxiety and fear. In other words, COVID-19 outbreak may have played a triggering role. For example, information about the pandemic may have exacerbated anxiety and fear in individuals who are more prone to anxiety and fear.
The moderator analyses revealed the highest effect size of gender differences in COVID-19 related fear, and anxiety obtained from the studies conducted in Europe. Also, contrary to what we expected, Middle East samples surprisingly revealed no gender difference in COVID-19 related fear and anxiety. Considering the higher risk perception of females in individualistic societies, their greater awareness of danger, maladaptation in facing threats, and more negative perceptions about the health risks of the pandemics (Alsharawy et al., 2021; Bengtsson et al., 2005; Magano et al., 2021; Morales-Rodríguez, 2021; Niño et al., 2021; Orrù et al., 2021; Tsipropoulou et al., 2020; Ypsilanti et al., 2021), and some cultural factors, the highest effect size in favor of females is expected in European samples. In addition, the effect size of gender difference in COVID-19 related fear was higher in individualistic orientation than collectivistic, while in COVID-19 related anxiety was higher in collectivistic orientation than individualistic, but there were no statistically significant differences. Finally, other moderators, the average age of the sample, timing, and target population, were not significant moderators for gender differences in COVID-19 related fear and anxiety. Overall, the continent variable provided partial evidence for gender difference in COVID-19 related fear and anxiety. However, the findings of other moderators revealed that the source of heterogeneity is not the characteristic of sample or the study characteristic. Other sources such as lockdown and social isolation period, economic growth (GDP), COVID-19 death rate, Gini index, and data availability may result in heterogeneity in this meta-analysis.
4.1. Implications and future research
Results of this study highlighted the need for prevention and intervention programs. Considering the relationship between COVID-19 related fear and anxiety and depression, stress, mood swings, general irritability, insomnia, attention deficit, suicide, addiction, and PTSD, it is a threat to the well-being of individuals. Therefore, psycho-education programs on coping skills and adverse thoughts about the virus implemented by mental health professionals and more explicit and accurate information about COVID-19 provided by decision-makers is necessary. It should be considered that COVID-19 related fear and anxiety were higher in females while applying these programs and information. The results of this study also showed that females in Europe had higher fear and anxiety related to COVID-19 than females in Middle East. Therefore, cultural factors such as gender roles should be considered when designing prevention and intervention programs. In addition, the reasons for these intercontinental differences could be investigated in future research. In this study, we only estimated the effect of gender on COVID-19 related fear and anxiety. In future studies, the effect of gender on COVID-19 related phobia, perceived risk, and stress would be examined to find evidence for convergent validity. Finally, there may be various reasons for the higher fear and anxiety associated with COVID-19 in females, such as gender equality, gender roles, and some cultural factors which could be examined in future studies.
4.2. Limitations
The current study has a few limitations. First, only articles written in English were included. Thus, studies conducted in other languages (i.e., Spanish, German, Arabic) were not included in this meta-analysis. Second, articles using the FCV-19S (Ahorsu et al., 2020) and CAS (Lee, 2020) screening tools for the assessment of COVID-19 fear and anxiety were included. Other screening tools assessing COVID-19 related fear and anxiety were not included in the current study. Third, there was a high level of heterogeneity among the studies included in this meta-analysis. As a result of the moderator analyses to explain the heterogeneity, it was observed that only continent variable partially explained the heterogeneity. Therefore, this situation should be considered when interpreting the study results. Fourth, we considered culture, continent, the average age of the sample, timing, and target population as potential moderators. However, to determine heterogeneity between the studies, we could not include other potential moderators (e.g., lockdown period, COVID-19 death rate, Gini index) because details were not available for these moderators in the studies included in the current meta-analysis. Finally, gender is not always divided along the binary lines of female and male. But we could not address other identities as there were insufficient data to calculate the mean and SD of other gender identities in the studies included in this meta-analysis.
5. Conclusion
COVID-19 outbreak has negatively affected individuals in many ways such as psychological, economics, sociological etc. To our knowledge, this meta-analysis is the most extensive and the first study to estimate gender difference in COVID-19 related fear and anxiety. Although this study has some limitations, our study showed that COVID-19 related fear and anxiety was higher in females. Also, in this current study we found additional evidence to the higher COVID-19 related fear and anxiety, those who are females in Europe. In conclusion, COVID-19 outbreak negatively affected females more.
Financial disclosure
This study has not been done within any project.
Funding
No funds were used.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
CRediT authorship contribution statement
Eyüp Sabır Erbiçer: Writing, methodology, theoretical basis, literature review, and data analysis.
Ahmet Metin: Writing, methodology, theoretical basis, and literature review.
Sedat Şen: Writing and data analysis.
Ali Çetinkaya: Literature review.
Conflict of interest
The authors do not report any conflicts of interest.
Acknowledgments
None. No funding to declare.
Footnotes
References for the studies included in the meta-analysis are marked with asterisks.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.05.036.
Appendix A. Supplementary data
The quality of the studies.
Funnel plots.
Forest plots.
References1
- *Abdelgwad M.A.Z., Abdelaziz A.F.A. Fear of COVID-19 and its Relationship to Wisdom of University Students. Psychol. Educ. J. 2021;58(3):1342–1353. doi: 10.17762/pae.v58i3.3866. [DOI] [Google Scholar]
- *Ahammed B., Jahan N., Seddeque A., Hossain M.T., Khan B., Mamun M.A., Islam M.N. Exploring the association between mental health and subjective sleep quality during the COVID-19 pandemic among Bangladeshi university students. Heliyon. 2021;7(5) doi: 10.1016/j.heliyon.2021.e07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The Fear of COVID-19 Scale: development and initial validation. Int. J. Ment. Heal. Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. (Advance online publication) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhtar S. Routledge; 2018. Sources of Suffering: Fear, Greed, Guilt, Deception, Betrayal, and Revenge. [Google Scholar]
- *Aksoy A., Abiç A., Değirmenci F., Vefıkuluçay Yılmaz D. The relationship between quality of life and fear of Turkish individuals during the COVID-19 pandemic: A cross-sectional study. Arch. Psychiatr. Nurs. 2021;35:472–478. doi: 10.1016/j.apnu.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Akyildiz D., Durna S. Determining the research status and coronavirus anxiety scores of academics during the flexible working arrangements initiated after the COVID-19 pandemic. J. Taibah Univ. Med. Sci. 2021;16(3):336–343. doi: 10.1016/j.jtumed.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Alnazly E., Khraisat O.M., Al-Bashaireh A.M., Bryant C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Alothman S.A., Alghannam A.F., Almasud A.A., Altalhi A.S., Al-Hazzaa H.M. Lifestyle behaviors trend and their relationship with fear level of COVID-19: cross-sectional study in Saudi Arabia. PLoS One. 2021;16(10) doi: 10.1371/journal.pone.0257904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsharawy A., Spoon R., Smith A., Ball S. Gender differences in fear and risk perception during the COVID-19 pandemic. Front. Psychol. 2021;12(689):467. doi: 10.3389/fpsyg.2021.689467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alyami M., de Albuquerque J.V., Krägeloh C.U., Alyami H., Henning M.A. Effects of fear of COVID-19 on mental well-being and quality of life among Saudi adults: a path analysis. Saudi J. Med. Med. Sci. 2021;9(1):24–30. doi: 10.4103/sjmms.sjmms_630_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Antonio M.T.L., Elizabeth V.A.C. Transcultural adaptation and validation of the fear of COVID-19 Scale into Mexican-Spanish. Med. Clin. Res. 2021;6(5):512–515. https://medclinres.org/pdfs/2021/transcultural-adaptation-and-validation-of-the-fear-of-covid-19-scale-into-mexican-spanish-mcr-21.pdf (ISSN, 2577, 8005) [Google Scholar]
- Arpaci I., Karataş K., Baloğlu M. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S) Personal. Individ. Differ. 2020;164(110):108. doi: 10.1016/j.paid.2020.110108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ashoor M.M., Almulhem N.J., AlMubarak Z.A., Alrahim A.A., Alshammari S.M., Alzahrani F.S.…Alardhi A. The psychological impact of the COVID-19 pandemic on otolaryngologists: Should we be concerned? Laryngoscope Invest. Otolaryngol. 2021:576–585. doi: 10.1002/lio2.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Aslam N., Shafique K., Ahmed A. Exploring the impact of COVID-19-related fear, obsessions, anxiety and stress on psychological well-being among adults in Pakistan. J. Ment. Health Train. Educ. Pract. 2021;16(4):313–321. doi: 10.1108/JMHTEP-10-2020-0074. [DOI] [Google Scholar]
- *Aslan, S., & Dinç, M. Examining the relationship between nurses' fear levels and insomnia during the COVID-19 pandemic in Turkey. Perspect. Psychiatric Care, 10, 1–7. doi: 10.1111/ppc.12927. [DOI] [PMC free article] [PubMed]
- Austad S.N. Why women live longer than men: sex differences in longevity. Gender Med. 2006;3(2):79–92. doi: 10.1016/s1550-8579(06)80198-1. [DOI] [PubMed] [Google Scholar]
- *Bakioğlu F., Korkmaz O., Ercan H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int. J. Ment. Heal. Addict. 2020;1–14 doi: 10.1007/s11469-020-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Barbosa-Camacho F.J., García-Reyna B., Cervantes-Cardona G.A., Cervantes-Pérez E., Chavarria-Avila E., Pintor-Belmontes K.J.…Cervantes-Guevara G. Comparison of Fear of COVID-19 in Medical and Nonmedical Personnel in a Public Hospital in Mexico: a Brief Report. Int. J. Ment. Heal. Addict. 2021;1–12 doi: 10.1007/s11469-021-00600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtsson C., Persson M., Willenhag P. Gender and overconfidence. Econ. Lett. 2005;86(2):199–203. doi: 10.1016/j.econlet.2004.07.012. [DOI] [Google Scholar]
- *Bhattacharya D., Rai A.K., Singh N.K., Koushal V., Mahajan S.S., Mahajan P. Psychological impact of COVID-19 on Mental Health Professionals working in different tertiary level healthcare setups of India. J. Adv. Med. Dent. Sci. Res. 2021;9(4):1–8. doi: 10.21276/jamdsr. [DOI] [Google Scholar]
- Block J.H. Differential premises arising from differential socialization of the sexes: some conjectures. Child Dev. 1983;54(6):1335–1354. doi: 10.2307/1129799. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. John Wiley & Sons; United Kingdom: 2011. Introduction to Meta-analysis. [Google Scholar]
- *Broche-Pérez Y., Fernández-Fleites Z., Jiménez-Puig E., Fernández-Castillo E., Rodríguez-Martin B.C. Gender and fear of COVID-19 in a Cuban population sample. Int. J. Ment. Heal. Addict. 2020;1–9 doi: 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Broche-Pérez Y., Fernández-Fleites Z., Fernández-Castillo E., Jiménez-Puig E., Vizcaíno-Escobar A.E., Ferrer-Lozano D.M.…Martín-González R. Anxiety, health self-perception, and worry about the resurgence of COVID-19 predict fear reactions among genders in the Cuban population. Front. Glob. Women's Health. 2021;2:14–23. doi: 10.3389/fgwh.2021.634088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bukhari F.K., Fahd S., Firdos S., Kaleem H., Waseem A. Perceived emotional distress and fear of Covid-19 among young adults during pandemic. J. Pak. Psychiatric Soc. 2021;18(2) https://www.jpps.pk/index.php/journal/article/view/93 [Google Scholar]
- *Çakmak G., Öztürk Z.A. Being both a parent and a healthcare worker in the pandemic: who could be exhausted more? Healthcare. 2021;9(5):564–573. doi: 10.3390/healthcare9050564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Cervantes-Guevara G., Maciel-Saldierna M., Elizondo-Hernández E., Cervantes-Pérez L.A., Cervantes-Cardona G.A., García-Reyna B.…González-Ojeda A. Fear of COVID-19 in high school personnel: a survey study in Western Mexico. Int. J. Ment. Heal. Addict. 2021;1–8 doi: 10.1007/s11469-020-00473-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless D.L., Mason J. Sex, sex-role stereotyping and agoraphobia. Behav. Res. Ther. 1986;24(2):231–235. doi: 10.1016/0005-7967(86)90098-7. [DOI] [PubMed] [Google Scholar]
- Chiacchia D., Greenglass E., Antoniou A.S., Begic P., Buchwald P., Chrousos G.…Marjanovic Z. Psychometric validation of the Brief Coronavirus Threat Scale (BCTS) across nine countries. J. Stress Trauma Anxiety Resilience (J-STAR) 2022;1(1) doi: 10.55319/js.v1i1.1. [DOI] [Google Scholar]
- *Chorwe-Sungani G. Assessing COVID-19-related anxiety and functional impairment amongst nurses in Malawi. Afr. J. Prim. Health Care Fam. Med. 2021;13(1) doi: 10.4102/phcfm.v13i1.2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun C.A., Moos R.H., Cronkite R.C. Handbook of Multicultural Perspectives on Stress and Coping. Springer; Boston: 2006. Culture: a fundamental context for the stress and coping paradigm. [Google Scholar]
- Cohen J. (2nd ed.). Erlbaum; 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Cooper H., Hedges L.V., ve Valentine J.C., editors. The Handbook of Research Synthesis and Meta-analysis. Sage; New York: 2009. [Google Scholar]
- Cui T., Yang G., Ji L., Zhu L., Zhen S., Shi N.…Jin H. Chinese residents' perceptions of COVID-19 during the pandemic: online cross-sectional survey study. J. Med. Internet Res. 2020;22(11) doi: 10.2196/21672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Curtis A.F., Rodgers M., Miller M.B., McCrae C.S. Impact of sex on COVID-19 media exposure, anxiety, perceived risk, and severity in middle-aged and older adults. J. Aging Health. 2021;1–9 doi: 10.1177/08982643211025383. [DOI] [PubMed] [Google Scholar]
- *De los Santos J.A.A., Labrague L.J. The impact of fear of COVID-19 on job stress, and turnover intentions of frontline nurses in the community: a cross-sectional study in the Philippines. Traumatology. 2021;27(1):52–59. doi: 10.1037/trm0000294. [DOI] [Google Scholar]
- *De Los Santos J.A.A., Labrague L.J., Falguera C.C. Fear of COVID-19, poor quality of sleep, irritability, and intention to quit school among nursing students: a cross-sectional study. Perspect. Psychiatric Care. 2021;1–8 doi: 10.1111/ppc.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Doğan R., Serin E.K., Bağci N. Fear of COVID 19 and social effects in liver transplant patients. Transpl. Immunol. 2021;69(101):479. doi: 10.1016/j.trim.2021.101479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Doshi D., Karunakar P., Sukhabogi J.R., Prasanna J.S., Mahajan S.V. Assessing coronavirus fear in Indian population using the fear of COVID-19 scale. Int. J. Ment. Heal. Addict. 2020;1–9 doi: 10.1007/s11469-020-00332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downes M.J., Brennan M.L., Williams H.C., Dean R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 2016;6(12) doi: 10.1136/bmjopen-2016-011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey M.J., Ghosh R., Chatterjee S., Biswas P., Chatterjee S., Dubey S. COVID-19 and addiction. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14(5):817–823. doi: 10.1016/j.dsx.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekman P. 2 ed. St. Martin's Griffin; 2007. Emotions Revealed: Recognizing Faces and Feelings to Improve Communication and Emotional Life. [Google Scholar]
- *Elsayed M.M., Ghazi G.A. Fear of COVID-19 pandemic, obsessive-compulsive traits and sleep quality among first academic year nursing students, Alexandria University, Egypt. Egypt. J. Health Care. 2021;12(2):224–241. doi: 10.21608/ejhc.2021.150261. [DOI] [Google Scholar]
- Erbiçer E.S., Metin A., Çetinkaya A., Şen S. The relationship between fear of COVID-19 and depression, anxiety, and stress: a meta-analysis. Eur. Psychol. 2021;26(4) doi: 10.1027/1016-9040/a000464. [DOI] [Google Scholar]
- Eskes T., Haanen C. Why do women live longer than men? Eur. J. Obstet. Gynecol. Reprod. Biol. 2007;133(2):126–133. doi: 10.1016/j.ejogrb.2007.01.006. [DOI] [PubMed] [Google Scholar]
- *Eşkut N., Ataç Uçar C., Köşkderelioğlu A., Ünsal Bilgin Y.Ö. Evaluation of Corona Virus disease-19 related fear and anxiety in patients admitted to neurology outpatient clinic. Osmangazi Tıp Dergisi. 2021 doi: 10.20515/otd.948805. [DOI] [Google Scholar]
- *Evren C., Evren B., Dalbudak E., Topcu M., Kutlu N. Measuring anxiety related to COVID-19: a Turkish validation study of the Coronavirus Anxiety Scale. Death Stud. 2020;1–7 doi: 10.1080/07481187.2020.1774969. [DOI] [PubMed] [Google Scholar]
- Fincher C.L., Thornhill R., Murray D.R., Schaller M. Pathogen prevalence predicts human cross-cultural variability in individualism/collectivism. Proc. Biol. Sci. 2008;275(1640):1279–1285. doi: 10.1098/rspb.2008.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *García-Reyna B., Castillo-García G.D., Barbosa-Camacho F.J., Cervantes-Cardona G.A., Cervantes-Pérez E., Torres-Mendoza B.M.…Cervantes-Guevara G. Fear of COVID-19 scale for hospital staff in regional hospitals in mexico: a survey study. Res. Square. 2020;1–10 doi: 10.21203/rs.3.rs-34,065/v1. [DOI] [Google Scholar]
- *García-Reyna B., Castillo-García G.D., Barbosa-Camacho F.J., Cervantes-Cardona G.A., Cervantes-Pérez E., Esparza-Estrada I.…Cervantes-Guevara G. Anxiety and COVID-19: Coronavirus Anxiety Scale scores in medical and non-medical personnel in urban hospitals in Guadalajara. A cross-sectional survey study. Death Stud. 2021;1–9 doi: 10.1080/07481187.2021.1936297. [DOI] [PubMed] [Google Scholar]
- *Gélinas C., Maheu C., Lavoie-Tremblay M., Richard-Lalonde M., Gallani M., Gosselin É.…Côté J. Translation of the Fear of COVID-19 Scale into French-Canadian and English-Canadian and validation in the nursing staff of Quebec. Sci. Nurs. Health Pract./Science infirmière et pratiques en santé. 2021;4(1):1–23. doi: 10.7202/1077985ar. [DOI] [Google Scholar]
- *Ghaderi E., Mahmoodi H., Sharifi Saqqezi P., Ghanei Gheshlagh R., Moradi G., Shokri A.…Ahmadi A. Knowledge, attitudes, practices and fear of COVID-19 among Iranians: a quick online survey. Health Soc. Care Commun. 2021:1–10. doi: 10.1111/hsc.13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Giordani R.C., Giolo S.R., Muhl C., Zanoni da Silva M. Psychometric evaluation of the Portuguese version of the FCV-19 scale and assessment of fear of COVID-19 in a Southern Brazilian population. J. Hum. Behav. Soc. Environ. 2021;31(1–4):145–153. doi: 10.1080/10911359.2020.1854142. [DOI] [Google Scholar]
- *Giordani R.C.F., Giolo S.R., Muhl C., Estavela A.J., Gove J.I.M. Validation of the FCV-19 Scale and assessment of fear of COVID-19 in the population of Mozambique, East Africa. Psychol. Res. Behav. Manag. 2021;14:345–354. doi: 10.2147/PRBM.S298948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Grande M., Doyle-Baker P. Fear of COVID-19 effects on university student’s health behaviours: the FRESH Study. Int. J. Kinesiol. Sports Sci. 2021;9(3):52–59. doi: 10.7575/aiac.ijkss.v.9n.1p.52. [DOI] [Google Scholar]
- *Green Z.A., Noor U., Ahmed F., Himayat L. Validation of the Fear of COVID-19 Scale in a sample of Pakistan’s university students and future directions. Psychol. Rep. 2021;1–24 doi: 10.1177/00332941211016754. [DOI] [PubMed] [Google Scholar]
- *Guzel H., Guzel H.I., Dogan I. Anxiety levels of medical students during COVID-19 outbreak. Med. Sci. Int. Med. J. 2021;10(3):918–923. doi: 10.5455/medscience.2021.04.109. [DOI] [Google Scholar]
- *Haktanir A., Seki T., Dilmaç B. Adaptation and evaluation of Turkish version of the fear of COVID-19 scale. Death Stud. 2020;1–9 doi: 10.1080/07481187.2020.1773026. [DOI] [PubMed] [Google Scholar]
- Hofstede Insights Cultural Compass Report Studies included in this current study. 2021. https://www.hofstede-insights.com/product/compare-countries/
- *Hossain M.A., Jahid M.I.K., Hossain K.M.A., Walton L.M., Uddin Z., Haque M.O.…Hossain Z. Knowledge, attitudes, and fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS One. 2020;15(9):1–22. doi: 10.1101/2020.06.17.20133611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jafari-Oori M., Ebadi A., Moradian S.T., Jafari M., Dehi M., Fard F.G. Psychiatric distress in family caregivers of patients with COVID-19. Arch. Psychiatr. Nurs. 2021 doi: 10.1016/j.apnu.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jan F., Qureshi M.A., Hussain M.M. Depression, anxiety and fear due to COVID-19 in Pakistan: a study based on learning perspective. Int. J. Innov. Teach. Learn. 2021;7(1):106–120. doi: 10.35993/ijitl.v7i1.1816. [DOI] [Google Scholar]
- *Kaçoğlu C., Çobanoğlu H.O., Şahin E. An investigation of fear of COVID-19 status in university student athletes from different sports associated with contact. Phys. Educ.. Stud. 2021;25(2):117–128. doi: 10.15561/20755279.2021.0207. [DOI] [Google Scholar]
- *Kakodkar P., Kale S., Bhonde R., Pawar N.J. Fear of COVID-19 and its impact on quality of life during the lockdown situation among the teaching faculty of a health university in India. Med. J. Dr. DY Patil Vidyapeeth. 2021;14(5):502–507. doi: 10.4103/mjdrdypu.mjdrdypu_284_20. [DOI] [Google Scholar]
- *Karadem F.B., Demirdaş A., Işık Ü., Kılıç F. Investigation of the psychiatric factors that determine the fear of COVID-19 in healthcare workers and hospital staff in a university hospital in Turkey. J. Commun. Psychol. 2021;1–13 doi: 10.1002/jcop.22657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Karahan S., Agadayi E., Yilmaz I.G. Problems experienced by family physicians in Sivas during the pandemic period and its relationship with COVID-19 fear. Euras. J. Fam. Med. 2021;10(2):74–83. doi: 10.33880/ejfm.2021100205. [DOI] [Google Scholar]
- Karataş Z., Tagay Ö. The relationships between resilience of the adults affected by the covid pandemic in Turkey and Covid-19 fear, meaning in life, life satisfaction, intolerance of uncertainty and hope. Personal. Individ. Differ. 2021;172 doi: 10.1016/j.paid.2020.110592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kardaş F. The fear of COVID-19 raises the level of depression, anxiety and stress through the mediating role of intolerance of uncertainty. Stud. Psychol. 2021;63(3):291–306. doi: 10.31577/sp.2021.03.828. [DOI] [Google Scholar]
- *Kassim M.A.M., Pang N.T.P., Mohamed N.H., Kamu A., Ho C.M., Ayu F.…Jeffree M.S. Relationship between fear of COVID-19, psychopathology and sociodemographic variables in Malaysian population. Int. J. Ment. Heal. Addict. 2021;1–8 doi: 10.1007/s11469-020-00444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C. Epidemiology of women and depression. J. Affect. Disord. 2003;74(1):5–13. doi: 10.1016/S0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Kim U.E., Triandis H.C., Kâğitçibaşi Ç.E., Choi S.C.E., Yoon G.E. Sage Publications, Inc.; 1994. Individualism and Collectivism: Theory, Method, and Applications. [Google Scholar]
- Kim H.S., Sherman D.K., Updegraff J.A. Fear of Ebola: the influence of collectivism on xenophobic threat responses. Psychol. Sci. 2016;27(7):935–944. doi: 10.1177/0956797616642596. [DOI] [PubMed] [Google Scholar]
- Kira I.A., Shuwiekh H.A., Rice K.G., Ashby J.S., Elwakeel S.A., Sous M.S.F., Jamil H.J. Measuring COVID-19 as traumatic stress: initial psychometrics and validation. J. Loss Trauma. 2020 doi: 10.1080/15325024.2020.1790160. [DOI] [Google Scholar]
- *Krägeloh C.U., Alyami M., Alyami H., Alwaily M., Alhuwaydi A.M., Henning M.A. Physical distancing and hand washing during the COVID-19 pandemic among Saudi adults: the role of fear, perceived seriousness, and health knowledge. Int. J. Ment. Heal. Addict. 2021;1–14 doi: 10.1007/s11469-021-00674-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Labrague L.J., De Los Santos J.A.A. Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nurs. 2021;38(3):382–389. doi: 10.1111/phn.12841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Landa-Blanco M., Santos-Midence C., Landa-Blanco A.L., Andino-Rodriguez E., Cortés-Ramos A. The relationship between fear of COVID-19 and anxiety in Honduran population. Psyarxiv. 2021 doi: 10.31234/osf.io/zyw6c. [DOI] [Google Scholar]
- Langan D., Higgins J.P.T., Simmonds M. An empirical comparison of heterogeneity variance estimators in 12894 meta-analyses. Res. Synth. Methods. 2015;6(2):195–205. doi: 10.1002/jrsm.1140. [DOI] [PubMed] [Google Scholar]
- Lasheras I., Gracia-García P., Lipnicki D.M., Bueno-Notivol J., López-Antón R., de la Cámara C., Lobo A., Santabárbara J. Erratum: Lasheras, I.; et al. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. Int. J. Environ. Res. Public Health. 2020;17(24):9353. doi: 10.3390/ijerph17249353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus Anxiety Scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44(7):393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- *Lee S.A., Mathis A.A., Jobe M.C., Pappalardo E.A. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the Coronavirus Anxiety Scale. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey M.W., Wilson D.B. SAGE; Thousand Oaks, CA: 2001. Practical Meta-analysis. [Google Scholar]
- *Magano J., Vidal D.G., Dinis M.A.P., Leite Â. Psychological factors explaining perceived impact of COVID-19 on travel. Eur. J. Inv. Health Psychol. Educ. 2021;11(4):1120–1133. doi: 10.3390/ejihpe11040083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mahmoud N., Zeid W., Alsabahy K., Ezzeldeen E. Fear of coronavirus disease (COVID-19) among Egyptian physicians. Suez Canal Univ. Med. J. 2021;24(2):193–200. doi: 10.21608/SCUMJ.2021.196531. [DOI] [Google Scholar]
- *Malik S., Ullah I., Irfan M., Ahorsu D.K., Lin C.Y., Pakpour A.H.…Minhas R. Fear of COVID-19 and workplace phobia among Pakistani doctors: a survey study. BMC Public Health. 2021;21(1):1–9. doi: 10.1186/s12889-021-10873-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mamun M.A. Exploring factors in fear of COVID-19 and its GIS-based nationwide distribution: the case of Bangladesh. Br. J. Psych. Open. 2021;7(5):1–8. doi: 10.1192/bjo.2021.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto D., Hwang H.S. In: Nonverbal communication: Science and applications. Matsumoto D., Frank M.G., Hwang H.S., editors. Sage; 2013. Facial expressions; pp. 15–52. [Google Scholar]
- McLean C.P., Asnaani A., Litz B.T., Hofmann S.G. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metin A., Çetinkaya A., Erbiçer E.S. Subjective well-being and resilience during COVID-19 pandemic in Turkey. Eur. J. Health Psychol. 2021;28(4):152–160. doi: 10.1027/2512-8442/a000081. [DOI] [Google Scholar]
- *Midorikawa H., Aiba M., Lebowitz A., Taguchi T., Shiratori Y., Ogawa T.…Tachikawa H. Confirming validity of The Fear of COVID-19 Scale in Japanese with a nationwide large-scale sample. PLoS One. 2021;16(2):1–13. doi: 10.1371/journal.pone.0246840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mistry S.K., Ali A.M., Akther F., Yadav U.N., Harris M.F. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob. Health. 2021;17(1):1–9. doi: 10.1186/s12992-021-00698-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Montag C., Sindermann C., Rozgonjuk D., Yang S., Elhai J.D., Yang H. Investigating links between fear of COVID-19, neuroticism, social networks use disorder, and smartphone use disorder tendencies. Front. Psychol. 2021;12:1–9. doi: 10.3389/fpsyg.2021.682837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Morales-Rodríguez F.M. Fear, stress, resilience and coping strategies during COVID-19 in Spanish university students. Sustainability. 2021;13(11):5824. doi: 10.3390/su13115824. [DOI] [Google Scholar]
- *Nguyen H.T., Do B.N., Pham K.M., Kim G.B., Dam H.T., Nguyen T.T.…Duong T.V. Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health. 2020;17(11):4164. doi: 10.3390/ijerph17114164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikčević A.V., Spada M.M. The COVID-19 anxiety syndrome scale: development and psychometric properties. Psychiatry Res. 2020;292(113):322. doi: 10.1016/j.psychres.2020.113322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niño M., Harris C., Drawve G., Fitzpatrick K.M. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: evidence from two national data sources. SSMPopulation. Health. 2021;13 doi: 10.1016/j.ssmph.2020.100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ojalehto H.J., Abramowitz J.S., Hellberg S.N., Butcher M.W., Buchholz J.L. Predicting COVID-19-related anxiety: the role of obsessive-compulsive symptom dimensions, anxiety sensitivity, and body vigilance. J. Anxiety Disord. 2021;83 doi: 10.1016/j.janxdis.2021.102460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Orrù G., Bertelloni D., Diolaiuti F., Conversano C., Ciacchini R., Gemignani A. A psychometric examination of the Coronavirus Anxiety Scale and the Fear of Coronavirus Disease 2019 Scale in the Italian population. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.669384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Osagiator Ariyo J., Olutope Akinnawo E., Chinonye Akpunne B., Oluwasanmi Kumuyi D., Foluke Onisile D. An investigation of associations and incidence of anxiety, depression, perceived vulnerability to diseases, and fear of COVID-19 among nigerian health care workers. Arch. Pediatr. Inf. Dis. 2021 doi: 10.5812/pedinfect.114746. (in press) [DOI] [Google Scholar]
- Özdin S., Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry. 2020;66(5):504–511. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özmen S., Özkan O., Özer Ö., Yanardağ M.Z. Investigation of COVID-19 fear, well-being and life satisfaction in Turkish society. Social Work Public Health. 2021;36(2):164–177. doi: 10.1080/19371918.2021.1877589. [DOI] [PubMed] [Google Scholar]
- *Öztekin A., Keskin E., Açil H., Durak S., Dündar M., Yılmaz İ. Evaluation of anxiety levels linked to experienced coronavirus epidemic: the example of Turkey. Eval. Educ. Soc. Sci. J. 2021;28:219–232. doi: 10.17121/ressjournal.3011. [DOI] [Google Scholar]
- *Öztürk Altınayak S., Yılar Erkek Z. Comparison of individuals’ fear of COVID-19 pandemic and perceived control in Turkey. J. Contemp. Med. 2021;11(6) doi: 10.16899/jcm.940872. (forthcoming issue) [DOI] [Google Scholar]
- *Padovan-Neto F.E., Lee S.A., Guimarães R.P., Godoy L.D., Costa H.B., Zerbini F.L.S., Fukusima S.S. Brazilian adaptation of the Coronavirus Anxiety Scale: a psychometric investigation of a measure of coronaphobia. OMEGA J. Death Dying. 2021;1–19 doi: 10.1177/2F0030222821991325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A.…Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Parlak A.G., Akgün Şahin Z. The effect of COVID-19 fear on quality of life in hemodialysis patients: a correlation study in Turkey. Samsun Sağlık Bilimleri Dergisi. 2021;6(2):367–382. doi: 10.47115/jshs.882164. [DOI] [Google Scholar]
- Pérez-Fuentes M.D.C., Molero Jurado M.D.M., Oropesa Ruiz N.F., Martos Martínez Á., Simón Márquez M.D.M., Herrera-Peco I., Gázquez Linares J.J. Questionnaire on perception of threat from COVID-19. J. Clin. Med. 2020;9(4):1196. doi: 10.3390/jcm9041196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigott T.A. Gender differences in the epidemiology and treatment of anxiety disorders. J. Clin. Psychiatry. 1999;60:4–15. https://www.psychiatrist.com/wp-content/uploads/2021/02/13682_gender-differences-epidemiology-treatment-anxiety.pdf [PubMed] [Google Scholar]
- Reznik A., Gritsenko V., Konstantinov V., Khamenka N., Isralowitz R. COVID-19 fear in Eastern Europe: validation of the fear of COVID-19 scale. Int. J. Ment. Heal. Addict. 2020 doi: 10.1007/s11469-020-00283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robichaud M., Dugas M.J., Conway M. Gender differences in worry and associated cognitive-behavioral variables. J. Anxiety Disord. 2003;17(5):501–516. doi: 10.1016/S0887-6185(02)00237-2. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979;86(3):638. doi: 10.1037/0033-2909.86.3.638. [DOI] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di MArco A., Rossi A., Siracusano A., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N=18147 web-based 2 survey. medRxiv. 2020 doi: 10.1101/2020.04.09.20057802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin M.K., Aker S., Şahin G., Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J. Community Health. 2020;45(6):1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sakib N., Bhuiyan A.I., Hossain S., Al Mamun F., Hosen I., Abdullah A.H.…Mamun M.A. Psychometric validation of the Bangla Fear of COVID-19 Scale: confirmatory factor analysis and Rasch analysis. Int. J. Ment. Heal. Addict. 2020;1–12 doi: 10.1007/s11469-020-00289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Bueno-Notivol J., Lipnicki D.M., Olaya B., Pérez-Moreno M., Gracia-García P., Idoiaga-Mondragon N., Ozamiz-Etxebarria N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107(110):244. doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Lasheras I., Lipnicki D.M., Bueno-Notivol J., Pérez-Moreno M., López-Antón R., De la Cámara C., Lobo A., Gracia-García P. Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;109(110):207. doi: 10.1016/j.pnpbp.2020.110207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Saravanan C., Mahmoud I., Elshami W., Taha M.H. Knowledge, anxiety, fear, and psychological distress about COVID-19 among university students in the United Arab Emirates. Front. Psychiatry. 2020;11:1–10. doi: 10.3389/fpsyt.2020.582189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sarıgedik E., Bahar Ölmez S. The investigation of the relationships among coronavirus anxiety, cyberchondria, and online shopping. Konuralp Med. J. 2021;13(S1):446–454. doi: 10.18521/ktd.928468. [DOI] [Google Scholar]
- Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the Fear of COVID-19 Scale: its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Heal. Addict. 2020:1–9. doi: 10.1007/s11469-020-00294-0. (Advance online publication) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimmack U., Oishi S., Diener E. Individualism: a valid and important dimension of cultural differences between nations. Personal. Soc. Psychol. Rev. 2005;9(1):17–31. doi: 10.1207/s15327957pspr0901_2. [DOI] [PubMed] [Google Scholar]
- Shafiro M.V., Himelein M.J., Best D.L. Ukrainian and US American females: differences in individualism/collectivism and gender attitudes. J. Cross-Cult. Psychol. 2003;34(3):297–303. doi: 10.1177/0022022103034003004. [DOI] [Google Scholar]
- *Siddique R.F., Ahmed O., Hossain K.N. Relationship between the fear of COVID-19 disease and sleep quality: the mediating role of stress. Heliyon. 2021;7(5) doi: 10.1016/j.heliyon.2021.e07033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotomayor-Beltran C., Matta-Solis H., Perez-Siguas R., Matta-Solis E., Matta-Zamudio L. Fear of COVID-19 among Peruvian people living in disadvantaged communities: a cross-sectional study. Clin. Pract. Epidemiol. Ment. Health. 2021;17:19–25. doi: 10.2174/1745017902117010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Srivastava A., Bala R., Srivastava A.K., Mishra A., Shamim R., Sinha P. Anxiety, obsession and fear from coronavirus in Indian population: a web-based study using COVID-19 specific scales. Int. J. Commun. Med. Public Health. 2020;7(11):4570–4577. doi: 10.18203/23946040.ijcmph20204763. [DOI] [Google Scholar]
- Stavosky J.M., Borkovec T.D. The phenomenon of worry: theory, research, treatment and its implications for women. Women Ther. 1987;6(3):77–95. doi: 10.1300/J015V06N03_07. [DOI] [Google Scholar]
- *Sürme Y., Özmen N., Ertürk Arik B. Fear of COVID-19 and related factors in emergency department patients. Int. J. Ment. Heal. Addict. 2021;1–9 doi: 10.1007/s11469-021-00575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tan B., Ay B., Ozdemir J., Caliyurt O. Fear of COVID-19 among medical students and associated factors. Turk. Med. Stud. J. 2021:13–16. http://tmsj.trakya.edu.tr [Google Scholar]
- The Sex, Gender, and COVID-19 Project The COVID-10 sex-disaggregated data tracker. 2021. https://globalhealth5050.org/the-sex-gender-and-covid-19-project/
- Triandis H.C., Bontempo R., Villareal M.J., Asai M., Lucca N. Individualism and collectivism: cross-cultural perspectives on self-ingroup relationships. J. Pers. Soc. Psychol. 1988;54(2):323–338. doi: 10.1037/0022-3514.54.2.323. [DOI] [Google Scholar]
- *Tsipropoulou V., Nikopoulou V.A., Holeva V., Nasika Z., Diakogiannis I., Sakka S.…Parlapani E. Psychometric properties of the Greek version of FCV-19S. Int. J. Ment. Heal. Addict. 2020;1–10 doi: 10.1007/s11469-020-00319-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ünver S., Yeniğün S.C. COVID-19 fear level of surgical nurses working in pandemic and surgical units. J. Perianesthesia Nurs. 2021 doi: 10.1016/j.jopan.2021.04.014. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- *van de Venter R., Williams R., Stindt C., ten Ham-Baloyi W. Coronavirus-related anxiety and fear among South African diagnostic radiographers working in the clinical setting during the pandemic. J. Med. Imaging Radiat. Sci. 2021 doi: 10.1016/j.jmir.2021.09.016. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vina J., Borras C. Women live longer than men: understanding molecular mechanisms offers opportunities to intervene by using estrogenic compounds. Antioxid. Redox Signal. 2010;13(3):269–278. doi: 10.1089/ars.2009.2952. [DOI] [PubMed] [Google Scholar]
- *Wakashima K., Asai K., Kobayashi D., Koiwa K., Kamoshida S., Sakuraba M. The Japanese version of the Fear of COVID-19 scale: reliability, validity, and relation to coping behavior. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0241958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F.S., Zhang C. What to do next to control the 2019-nCoV epidemic? Lancet (London, England) 2020;395(10222):391–393. doi: 10.1016/S0140-6736(20)30300-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Wen W., Zhang H., Ni J., Jiang J., Cheng Y., Zhou M., Ye L., Feng Z., Ge Z., Luo H., Wang M., Zhang X., Liu W. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: a systematic review and meta-analysis. J. Am. Coll. Heal. 2021:1–8. doi: 10.1080/07448481.2021.1960849. (Advance online publication) [DOI] [PubMed] [Google Scholar]
- Wenjuan G., Siqing P., Xinqiao L. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J. Affect. Disord. 2020;263:292–300. doi: 10.1016/j.jad.2019.11.121. [DOI] [PubMed] [Google Scholar]
- WHO WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2021. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- WHO COVID-19 weekly epidemiological update. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---2-november-2021
- WHO Vaccine efficacy, effectiveness and protection. 2021. https://www.who.int/news-room/feature-stories/detail/vaccine-efficacy-effectiveness-and-protection
- WHO WHO Coronavirus (COVID-19) Dashboard. 2021. https://covid19.who.int/
- Williams J.E., Best D.L. Sage Publications, Inc.; 1990. Sex and Psyche: Gender and Self Viewed Cross-culturally. [Google Scholar]
- *Yalçın M., Erbiçer E.S., Akın E. Facilitating and complicating factors in coping with fear of COVID-19. Psychiatr. Danub. 2022 doi: 10.24869/psyd.2022.758. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Yaşar Can S., Dilmen Bayar B. Determining levels of fear of COVID-19 in 112 Healthcare professionals. Hastane Öncesi Dergisi. 2021;6(2):175–185. https://dergipark.org.tr/en/pub/hod/issue/64854/834260 [Google Scholar]
- *Ypsilanti A., Mullings E., Hawkins O., Lazuras L. Feelings of fear, sadness, and loneliness during the COVID-19 pandemic: findings from two studies in the UK. J. Affect. Disord. 2021;295:1012–1023. doi: 10.1016/j.jad.2021.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta A.K., Chambless D.L. Understanding gender differences in anxiety: the mediating effects of instrumentality and mastery. Psychol. Women Q. 2012;36(4):488–499. doi: 10.1177/0361684312450004. [DOI] [Google Scholar]
- Zarulli V., Jones J.A.B., Oksuzyan A., Lindahl-Jacobsen R., Christensen K., Vaupel J.W. Women live longer than men even during severe famines and epidemics. Proc. Natl. Acad. Sci. 2018;115(4):E832–E840. doi: 10.1073/pnas.1701535115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The quality of the studies.
Funnel plots.
Forest plots.