Abstract
BACKGROUND
The objective of the current study was to summarize current research on burnout among surgical trainees and surgeons during the COVID-19 pandemic.
METHODS
PubMed, SCOPUS, Embase, and Psych INFO were systematically searched for studies that evaluated burnout during the COVID-19 pandemic among surgical trainees and surgeons.
RESULTS
A total of 29 articles met inclusion criteria, most of which originated from the United States (n = 18, 62.1%). Rates of burnout ranged from 6.0% to 86.0%. Personal factors responsible for burnout were fear of contracting/transmitting COVID-19 (8 studies, 27.6%), female gender (8, 27.6%), and younger age (5, 17.2%). Professional factors contributing to burnout included increased COVID-19 patient clinical load (6, 20.7%), limited work experience (6, 20.7%), reduction in operative cases (5, 17.2%) and redeployment to COVID-19 wards (4, 13.8%). The COVID-19 pandemic negatively impacted surgical education due to reduced number of operative cases (11, 37.9%), decreased hands-on experience (4, 13.8%), and not being able to complete case requirements (3, 10.34%). The shift of didactics to virtual formats (3, 10.3%), increased use of telemedicine (2, 6.9%), and improved camaraderie among residents (1, 3.4%) were viewed as positive consequences.
CONCLUSION
COVID-19 related burnout was reported in as many as 1 in 2 surgical trainees and attending surgeons. Intrinsic- (i.e., gender, age), family- (i.e., family/being married/having children or being single/not having children), as well as work-related extrinsic- (i.e., work-force deployment, risk of infection/spread, changes in educational format) factors were strongly associated with risk of burnout. These factors should be considered when designing interventions to ameliorate burnout among surgical trainees and surgeons.
Key Words: Surgeons, Surgical trainees, COVID-19 pandemic, Coronavirus, Burnout and occupational stress
Competencies: Professionalism, Interpersonal and Communication Skills, Patient Care
Introduction
With over 220 million confirmed cases and 4 million deaths to date, the COVID-19 pandemic has placed a heavy burden on health care providers, trainees, and medical delivery systems worldwide. Front-line workers were expected to provide high-quality patient care despite limited resources, staffing shortages, and potential exposure to COVID-19.1 , 2 Emerging evidence suggests that these working conditions had a detrimental psychological impact on health care workers, including increased rates of depression, anxiety, and insomnia.3 In the context of surgery, a paradigm shift led to constantly evolving clinical guidelines, including the delay of non-emergent surgical procedures. For these reasons, the impact of the COVID-19 pandemic on the well-being of surgical trainees and surgeons, and the resulting occupational “burnout” (i.e., a negative psychological reaction to chronic occupational stressors), has become a matter of great concern.4
Prior to the COVID-19 pandemic, surgeons were already vulnerable to burnout due to long work hours, challenges in patient care, and difficulties with work-life balance.5 Factors associated with risk of burnout can be at the individual and/or institutional level and consequences of burnout can impact both individual providers (i.e., depression, substance abuse and suicide), as well as organizations (i.e., higher staff attrition, increased risk of medical errors).6, 7, 8 The COVID-19 pandemic, and unique circumstances associated with its various waves/phases, may have exacerbated these conditions, exposing surgeons to an even higher risk of burnout. While several studies have examined the impact of the COVID-19 pandemic on burnout among physicians in general, no attempt has been made to synthesize the findings of these studies to assess the impact on surgeons specifically. Therefore, the objective of the current study was to conduct a systematic review of the literature to summarize data on burnout among surgical trainees and attending surgeons during the COVID-19 pandemic.
Methods
A systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.9 Literature searches were performed using the following databases: PubMed/Medline, SCOPUS, Embase and Psych INFO. The search strategies are provided in Supplemental Table 1 and included the following terms and variations listed in the Medical Subject Headings index: “Surgeons'' (e.g., surgical trainee or resident), “Burnout” (e.g., occupational stress) AND “COVID-19” (e.g., coronavirus).
Selection Criteria and Eligibility
Included articles were published in English between January 1, 2020, and August 30, 2021, and had empirical qualitative and quantitative research designs. Articles related to burnout among surgical trainees and practicing surgeons during the COVID-19 pandemic with burnout mentioned in the abstract, keywords, introduction, and/or methods were included. All studies assessing burnout in surgical trainees and surgeons were included, regardless of the surgical subspecialty, as well as reports that included other healthcare providers in addition to surgeons. As the COVID-19 pandemic is a global event, articles were not excluded based on location. Summaries, reviews, commentaries, and poster presentation abstracts were excluded. Studies assessing burnout exclusively in health care providers other than surgical trainees or surgeons or including only medical students were also excluded. Table 1 includes a summary of study inclusion and exclusion criteria.
TABLE 1.
Inclusion and Exclusion Criteria
|
Selection Criteria | |
|---|---|
| Inclusion Criteria | Exclusion Criteria |
| 1. Related to burnout during the COVID-19 pandemic with the concept of burnout mentioned in the abstract, keywords, introduction and/or methods. 2. Related to burnout in surgeons in training or in practice. 3. Related to burnout in all surgical specialties (breast, hepato-pancreato-biliary, colorectal, general, orthopaedic, neuro, plastic, vascular, trauma, cardiovascular, otolaryngology and thoracic surgeons). 4. Published globally. 5. Published in English. |
1. Related to burnout in nurses and medical students, without inclusion of surgeons in training or surgeons. 2. Summaries, reviews, commentaries and poster presentation abstracts. 3. Related to burnout of physicians in non-surgical specialties. |
Burnout Assessment Scales
Studies were included in the systematic review regardless of which burnout assessment tool was used. The tool used most often was the Maslach Burnout Inventory (MBI). The MBI is a psychological assessment instrument including 22 items pertaining to occupational burnout that includes 3 subscales: emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA).10 Other tools included the Mini-Z burnout assessment scale,11 the Professional Fulfilment Index (PFI),12 the Utrecht Burnout Scale (UBOS),13 the Professional Quality of Life Measure V5,14 the Resident Fellow Well-Being Index (RSWBI),15 and the Shirom-Melamed Burnout Measure (SMBM).16 Studies were also included that utilized investigator-created assessments (ICA) tool.
Data Extraction
All articles returned from the formal search strategy were imported into Covidence, a web-based software designed to aid in systematic review management and recommended by Cochrane.17 Literature screening took place in two phases. In the first phase, two authors (CFS, AP) independently screened article titles and abstracts. In the second phase, the same authors screened full-text articles for inclusion and exclusion criteria. In both phases, a third author (EPK) resolved any conflicts or discrepancies. Full text interrater reliability was Κ = 0.87.
Data was abstracted by two study team members (CFS, BM). The following data was abstracted: article title, year, journal, authors, country, abstract results, abstract conclusions, conflict of interest statement, inclusion criteria, exclusion criteria, type of study, study design, aim, recruitment procedure, impact on personal/professional life, number of providers included, number of surgical trainees/surgeons, types of providers included, surgical specialties, years in practice, age, gender, race, family composition, healthcare setting, primary and secondary outcomes, measure of burnout used, operational definition, rates of burnout, factors associated with burnout (personal or professional), risk mitigation, risk intervention, and consequences of COVID-19. Data were extracted around the variable “conflict of interest” to detect any biases in the included studies.
Results
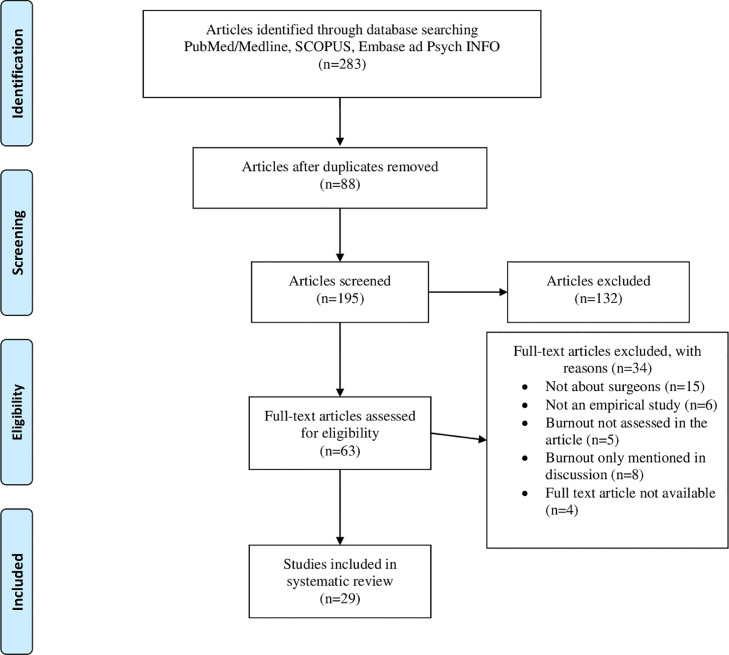
A total of 283 titles/abstracts were imported into Covidence to be considered during the initial title and abstract screening phase. Among these reports, 88 were identified as duplicates and removed. After 195 article titles and abstracts were screened, 132 were considered irrelevant based on study inclusion and exclusion criteria. The remaining 63 articles underwent the full-text screening procedure, during which articles were excluded because they were not about surgeons (n = 15), were not empirical studies (n = 6), did not explicitly assess burnout (n = 5) or only mentioned burnout in the context of the discussion (n = 4) or because the full-text article was not available (n = 4). The remaining 29 studies comprised the final sample and underwent data extraction by two members of the team. The study search and screening procedure are illustrated in Figure 1 .
FIGURE 1.
PRISMA diagram depicting search strategy.
Overall Study Characteristics
Among the 29 included studies conducted between April 2020 and December 2021, most were published in 2020 (n = 16, 55.2%),18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 whereas the remaining papers (n = 13, 44.8%) were published in 2021.4 , 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45 The majority of studies utilized cross-sectional, quantitative methods (n = 27),18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 , 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45 with only a small minority being qualitative (n = 2).4 , 34 The sample size varied widely across studies, ranging from 24 to 2040 for quantitative studies and from 16 to 870 for qualitative studies. Most of the studies were about the healthcare system in the United States (n = 17),19 , 21 , 22 , 26, 27, 28, 29 , 32, 33, 34, 35, 36, 37, 38, 39 , 42 , 43 while the remaining reports were from Singapore (n = 3),20 , 24 , 25 Egypt (n = 2),18 , 40 the United Kingdom (n = 1),4 France (n = 1),44 Brazil (n = 1),24 Pakistan (n = 1),23 the Netherlands (n = 1),45 Romania (n = 1),31 and the Czech Republic (n = 1).41 Almost all studies included surgical trainees (residents, fellows) as part of the studied population (28 studies, 96.6%). However, a minority of articles also included attendings and/or consultants in the studied population (10 studies, 34.5%).4 , 20 , 27, 28, 29 , 35 , 38 , 40 , 42 , 43 Slightly more than half of surgical trainees/surgeons involved were female (n = 5486, 54.3%), while 45.6% (n = 4599) of the total sample were male. None of the articles declared any conflicts of interest related to the studies. A brief summary of all included articles and the respective results can be found in Table 2 .
Table 2.
Summary of Included Articles
| Authors | Date | Country | Included Participants n/Total Sample n | Participant Type | Surgical[Sub-] Specialty | Burnout Assessment Used | Results |
|---|---|---|---|---|---|---|---|
| Abdelsattar, et al.34 |
May 2021 |
USA |
16/16 | Residents Fellows |
General | 6 focus group interview questions | Themes identified: (1) Impacts on resident education included clinical and non-clinical education; (2) Impacts on personal life included professional identity and sense of community; (3) Impacts on employee included management, communication, and personal safety. |
| Al-Ghunaim, et al.4 | Oct 2021 |
UK | 141/141 | Consultants Trainees |
General Multiple |
2 open-ended questions: ‘What challenges is the COVID-19 crisis currently presenting to you in your work and home life?’ and ‘How is this stress affecting you personally?’ | 85.8% of surgeons reported feeling negatively affected by COVID-19. Themes identified: (1) Changing and challenging environment, (2) Challenges to professional life and development, (3) Management to change and loss of personal lives, (4) Emotional and psychological impacts. |
| Al-Humadi, et al.38 |
Dec 2021 |
USA | 57/225 | Attendings Residents Fellows |
Ortho |
Single-items from EE and DP subscales of MBI | The overall burnout rate was 19.6%. History of depression/anxiety, age, and number of calls last month were significantly associated with feeling burnt out. |
| Ashry, et al.18 |
Sep 2020 |
Egypt | 50/50 | Residents | Neuro | Investigator-created assessment question; “Did you feel symptoms of burnout syndrome?” | 68% reported experiencing burnout symptoms. Unavailability of PPE, financial strains, and residents’ perception regarding the negative effect of the pandemic on their hands-on skills were associated with report of burnout symptoms. |
| Aziz, et al.19 |
Jul 2020 |
USA | 1102/1102 | Residents | General Multiple |
Investigator-created assessment | 33.1% of respondents reported more burnout than usual during COVID-19. |
| Cai, et al.26 |
Jun 2020 |
USA | 219/219 | Residents | ENT | Investigator-created assessment | Redeployed residents were more concerned about burnout than those not redeployed. |
| Chou, et al.39 |
Jan 2021 |
USA | 119/119 | Residents | ENT | Shirom-Melamed Burnout Measure |
10.9% of respondents met the criteria for clinically relevant burnout. Females and PGY-2 resident classes reported higher rates of burnout. |
| Civantos et al.27 |
May 2020 |
Brazil | 163/163 | Attendings Residents |
ENT | Single-item Mini-Z burnout assessment |
Burnout was reported in 14.7% participants. Females were more likely than males to report symptoms of burnout and more severe symptoms of burnout. |
| Civantos et al.28 |
Jul 2020 |
USA | 349/349 | Attendings Residents |
ENT | Single-item Mini-Z burnout assessment |
21.8% reported burnout. Residents (vs. attendings) and females (vs. males) more frequently reported burnout. |
| Coleman et al.29 |
Aug 2020 |
USA | 1160/1160 | Residents Early career surgeons |
General Multiple |
PHQ9 and aMBI (EE, DP) | Residents reported higher rates of DP (39%) than early-career surgeons (30%). Being female, a lack of wellness resources, reduction in case volume, and providing care to COVID-19 patients were associated with greater odds of burnout. Access to PPE was protective against burnout. |
| Cravero et al.30 |
Aug 2020 |
USA | 130/1420 | Residents Fellows |
General | Single-item measures of EE and DP | 66% of trainees who cared for >60 patients with COVID-19 reported burnout, compared with 39% of trainees who cared for no COVID-19 patients. Adequate access to PPE, country of origin, and having colleagues test positive for COVID-19 also predicted burnout. |
| Dimitriu et al.31 |
May 2020 |
Romania | 35/100 | Residents | General | MBI | 76% of residents reported burnout. Burnout rates were higher (86%) among general surgery, obstetrics/gynecology and orthopedics compared to residents in emergency or intensive care and radiology (66%). |
| Elghazally et al.40 |
Mar 2021 |
Egypt | 59/201 |
Attendings Residents |
General | MBI | The overall prevalence of burnout was 6%; 35.5% had high EE, 70.6% had high DP, and 26.4% had high PA. Younger, resident, single physicians and those working with COVID-19 patients > 8 hours/ day had higher burnout scores. |
| Fargen et al.32 |
Jun 2020 |
USA | 54/151 | Physicians | Neuro | Investigator-created assessment | 35% of participants reported a slight or great increase in career burnout, 44% reported no change and 4% reported less burnout, respectively. |
| Firew et al.33 |
Jul 2020 |
USA | 86/2040 | Multiple healthcare providers | General Multiple |
Single-item MBI | Providers that contracted COVID-19 or had a coworker contract COVID-19 reported higher levels of burnout symptoms. Isolation and asking cohabitants to move out was also associated with higher levels of burnout. |
| Guha et al.41 |
Oct 2021 |
Czech Republic | 181/181 | Physicians | ENT | Investigator-created assessment | 12.7% of physicians experienced burnout syndrome. |
| Hines et al.42 |
Dec 2021 |
USA | 9/96 | Attendings Residents fellows |
General Multiple |
MIES | Moral injury scores did not change between baseline, 1- and 3-month assessments. A supportive workplace was associated with lower moral injury. |
| Kabir et al.20 |
Sep 2020 |
Singapore | 96/96 | Consultant Residents |
General Orthopedic Urology ENT |
PFI | Overall, 34% of surgeons experienced burnout. Specifically, 42% of surgeons had evidence of work exhaustion burnout, while 33% had evidence of interpersonal disengagement burnout. |
| Khalafallah et al.21 |
Jul 2020 |
USA | 111/111 | Residents | Neuro | aMBI | Burnout was identified in 26.1% of the sample; 51.4% had low EE, 67.6% reported low DP, and 78.4% reported high PA. Alteration of clinical and vacation schedules and lower PGY level was associated with higher levels of burnout. |
| Khalafallah et al.22 |
Jul 2020 |
USA | 407/407 | Attendings | Neuro | aMBI | Burnout was identified in 20.4% of respondents. Factors associated with burnout included a hostile COVID-19 working environment, not having children, being in practice 5-15 years, increased time providing non-neurosurgical care, and feeling uncertain about future earnings. |
| Lazarides et al.43 |
Dec 2021 |
USA | 112/112 | Attendings Residents |
Ortho | PFI | The overall burnout rate was 15.9%. Specifically, 9% of trainees and 20% of experienced surgeons reported burnout. Burnout was inversely correlated with professional fulfilment. |
| Mion et al.44 |
Oct 2021 |
France | 47/1050 | Residents | General Multiple |
MBI | The total burnout rate was 55%. Burnout was associated with number of monthly calls, psychiatric history, interpersonal conflicts, and desire to quit specialty, fatigue, job satisfaction, and depression. |
| Osama et al.23 |
May 2020 |
Pakistan | 112/112 | Residents | General Multiple |
MBI | There was a significant decrease in EE, DP, and PA scores pre/post pandemic |
| Poelmann et al.45 |
Feb 2021 |
Netherlands | 313/313⁎⁎ | Residents | General Multiple |
UBOS* | The prevalence of burnout symptoms pre COVID-19 was 9.5% and 9.0% during the COVID-19 pandemic. Rates of burnout were higher in COVID-19 deployed resident (16.0% vs not 7.6%). |
| Seow et al.25 |
Apr 2020 |
Singapore | 58/117 | Multiple healthcare providers | Ortho | MBI and additional investigator-created questions | The prevalence of healthcare staff experiencing burnout increased from 38.5% before COVID-19 to 51.3% after COVID-19, with the greatest increase seen in EE. 57.3% of providers reported burnout was worse during COVID-19. |
| Tan et al.24 |
Aug 2020 |
Singapore | 45/45⁎⁎⁎ | Multiple healthcare providers | General | Professional Quality of Life Measure V5 | 48.9% of respondents screened positive for burnout including 33.3% of doctors and 59.3% of nondoctors. |
| Yao et al.35 |
Dec 2021 |
USA | 559/870 | Attendings Residents Fellows |
General Plastic surgery |
Investigator-created assessment of COVID-19 burnout symptoms. | 33.6% of participants reported EE, while 26.1% reported anxiety, and 22.1% reported general burnout. Age, gender, years in practice, taking care of COVID-19 patients, and testing positive for COVID-19 were associated with burnout. Additionally, delays in initiating therapies and consultations, and patient worry that those delays will impact patient overall survival were also associated with burnout. |
| Yu et al.36 |
Jun 2021 |
USA | 24/24 | Residents | Plastic surgery | modified MBI | 88% of residents reported feeling “always,” “very frequently,” or “occasionally” burnt out due to the number of virtual educational activities. |
| Zoorob et al.37 |
Apr 2021 |
USA | 93/1115 | Residents | General Multiple |
RSWBI | 51.5% of respondents felt burnt out during the previous month. Gender, age, and institutional support were positively associated with resident well-being. |
UBOS was adapted from MBI.
Sample size changed by question due to missing data
All participants were from the surgical department, but not all were surgeons. USA, United States of America; UK, United Kingdom; Ortho, orthopedic surgery; EE, emotional exhaustion; DP, depersonalization; MBI, Maslach Burnout Inventory; Neuro, neurosurgery; PPE, personal protective equipment; ENT, ear nose throat; PGY, post-graduate year; PHQ9, Patient Health Questionnaire 9; aMBI, abbreviated Maslach Burnout Inventory; MIES, Moral Injury Event Scale; PSS, Perceived Stress Scale; PFI, Professional Fulfilment Index; PA, personal achievement; UBOS, Utrecht Burnout Scale; RSWBI, Residents Fellow Wellbeing Index.
Burnout Rates and Specialties
The overall rate of burnout among surgical trainees/surgeons across all studies ranged from as low as 6.0% to as high as 86.0%.31 , 40 Of note, the reported rates of burnout varied considerably based on the scale used to assess them. Specifically, the 10 studies using the MBI reported rates of burnout ranging from 6.0% to 86.0%.21, 22, 23 , 25 , 31 , 33 , 36 , 38 , 40 , 44 Additionally, the 2 studies that used the Mini-Z burnout assessment scale reported rates of burnout of 14.7% and 21.8%.27 , 28 Two other studies assessed burnout rates through the PFI, and reported burnout rates of 15.9% and 34.0%.20 , 43 Less commonly used tools to measure burnout included the UBOS (1 study, burnout = 9.0%),45 the Professional Quality of Life Measure V5 (1 study, burnout = 48.9%)24 and the RSWBI (1 study, burnout = 51.5%).37 However, not all studies used previously validated tools to measure rates of burnout. In 8 studies (27.6%), investigators instead opted to design and implement their own tools or investigator created assessment (ICA). Rates of burnout measured using the investigator created assessment tools varied widely, ranging from 12.7% to 68.0%.4 , 18 , 19 , 26 , 32 , 34 , 35 , 41 Chou et al. compared the rate of self-reported burnout (24.4%) with the rate of burnout assessed via SMBM (10.9%).39
Reported burnout rates varied by surgical subspecialty. Among 4 studies including only ENT trainees and attending surgeons, reported burnout rates ranged from 10.9% to 21.8% (SMBM 10.9%, ICA 12.7%, single-item Mini-Z 14.7% and 21.8%).27 , 28 , 39 , 41 Among 4 studies including only neurosurgery trainees and attending surgeons, reported burnout rates ranged from 20.4% to 68.0% (aMBI 20.4%, aMBI 26.1%, ICA 35%, ICA 68%).18 , 21 , 22 , 32 Among 3 studies including only orthopedic surgery trainees and attending surgeons, reported burnout rates ranged from 15.9% to 57.3% (PFI 15.9%, EE & DP from MBI 19.6%, MBI and ICA 57.3%).25 , 38 , 43 The highest reported rate of burnout was among a cohort of plastic surgery residents related specifically to their experience with virtual education: 88% of residents expressed being always, often or occasionally burned out and 79% were emotionally drained from videoconferencing.36
Factors Associated with Burnout
Studies included in the current review identified both personal and professional factors associated with burnout in surgical trainees/surgeons during the COVID-19 pandemic. Personal factors contributing to burnout most often were fear of a family member potentially contracting COVID-19 (8 studies, 27.6%)19 , 23, 24, 25 , 30 , 32 , 44 , 46 and female gender (8 studies, 27.6%),27, 28, 29 , 34 , 35 , 38 , 39 , 41 followed by concerns for one's own safety (6 studies, 20.7%),19 , 24 , 29 , 37 , 38 , 44 and younger age or fewer years of practice (5 studies, 17.2%).27 , 28 , 38 , 40 , 41 Other less commonly cited personal factors associated with burnout during the pandemic are noted in Table 3 . The findings from the qualitative studies by Abdelsattar et al. and Al-Ghunaim et al. were consistent with these results, as demonstrated in their thematic analysis. For example, in the study by Al-Ghunaim et al. several comments focused on anxiety about the disease, including the “fear of bringing the virus home and infecting my family.” In turn, measures aimed at avoiding transmission of COVID-19 affected communication with family: “Not being able to live with my wife [...] makes communication harder.” As one participant from the study by Abdelsattar et al. mentioned, “[the pandemic] had a major impact on my relationships, [...] it will never go back.”4 , 34
TABLE 3.
Factors Associated With Increased Burnout
| Personal Factors | n | Professional Factors | n |
|---|---|---|---|
| Having a covid positive family member, scared of bringing it home/transmitting it to a loved one/losing a loved one | 8 | Increased COVID-19 patients in clinical load | 6 |
| Being female | 8 | Limited work experience* | 6 |
| Getting the disease, losing life | 6 | Redeployment to COVID-19 wards | 4 |
| Young age | 5 | Increased workload or stressful environment | 4 |
| Having a family/being married/having children | 3 | Limited availability of PPE | 4 |
| Being single | 3 | Long duty hours | 2 |
| Financial strain | 3 | Increased number of monthly calls | 2 |
| not having children | 2 | Hands-on experience compromised | 2 |
| Having a psychiatric history | 1 |
Note. n= number of studies; *=surgeons in PGY1-2
Several professional factors also contributed to the risk of burnout. In particular, having to care for a larger number of COVID-19-positive patients and having fewer years of clinical experience were the two most commonly reported professional factors associated with burnout (both mentioned in 6 separate studies, 20.7%).19 , 20 , 27 , 29 , 30 , 34 , 37 , 39 , 40 Additionally, redeployment to COVID-19 wards, an increased workload and limited availability of personal protective equipment were cited by 4 studies each (13.8%).18 , 22 , 25 , 26 , 29 , 30 , 34 , 41 , 42 , 45 These and other professional factors associated with higher burnout rates are noted in Table 3. The qualitative themes highlighted by Abdelsattar et al. and Al-Ghunaim et al. echoed these results. Al-Ghunaim et al. identified a “changing and challenging work environment” as one of the most prevalent subthemes in their analysis. For example, respondents commented on the “reduced capacity for operative surgery,” the “increased workload,” and the “lack of PPE”. Similarly, participants in the study by Abdelsattar et al. complained about being “in charge of 10 to 20 intubated COVID-19 patients on a daily basis,” “[not knowing] when I would return to the OR,” “[being] pulled away from my education [that is] operating to manage these COVID-19 patients,” and “[reusing] PPE for 20 to 30 days.”4 , 34
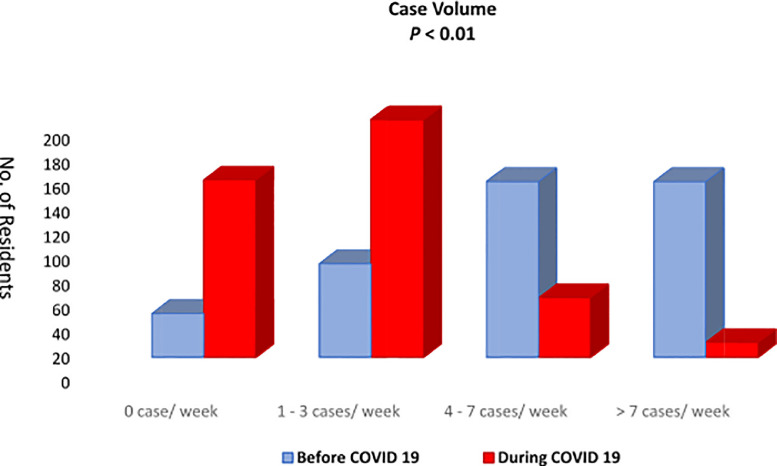
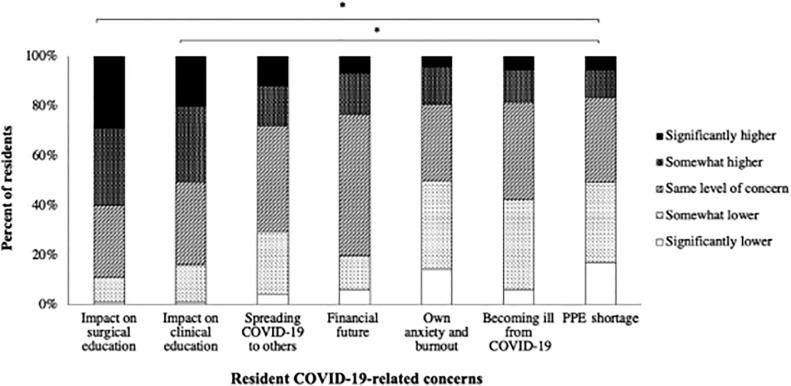
Impact on Surgical Education
Almost all studies involved surgical trainees (i.e., residents and fellows; 28 studies, 96.6%), and several commented on the impact of the COVID-19 pandemic on surgical education. Eleven out of 29 (38.0%) articles mentioned a marked reduction in the elective and emergent operative cases.4 , 18, 19, 20 , 23 , 26 , 29 , 32 , 34 , 39 , 45 The decrease in surgical case volume became a matter of great concern for the residents (FIGURE 2, FIGURE 3 ).19 While surgical personnel were redeployed (4 studies, 13.8%)18 , 20 , 26 , 45 to other areas of COVID-19 care within the hospitals, hands-on experience (4 studies, 13.8%)4 , 18 , 23 , 45 was also felt to be compromised. Furthermore, 3 out of 29 studies (10.3%) highlighted that the residents in their program were worried about not fulfilling the minimum requirements for Accreditation Council for Graduate Medical Education (ACGME) certification.19 , 22 , 29 Of note, surgical and clinical education were rated to be of higher concern than worries about PPE shortage (p < 0.00001).26
FIGURE 2.
Surgical case volume before and during COVID-19. Used with permission Aziz et al.19
FIGURE 3.
Changes in resident concerns during COVID-19. Used with permission Cai et al.26
Due to implementation of public health policies, didactics were shifted to virtual platforms. Residents in 5 (17.2%) of the studies noted that the virtual format had a markedly negative impact on surgical education.18 , 26 , 29 , 36 , 39 In contrast, 3 studies (10.3%) suggested that the move to a virtual education format was one of the successes pertaining to the COVID-19 pandemic.19 , 29 , 34 Additional factors that were considered positive included use of telehealth (2 studies, 7.0%),26 , 34 flexibility in schedules (1 study, 3.4%),34 work from home (1 study, 3.4%)4 and increased comradery among residents (1 study, 3.4%).34
Discussion
The COVID-19 pandemic has created unprecedented challenges across a vast array of areas both inside and outside the field of medicine. These challenges have generated significant stress and strain on physicians and health care professionals. In fact, one survey of 20,947 physicians and other healthcare workers reported that 43% suffered from work overload and 49% had burnout.47 Burnout can be associated with extreme physical and emotional exhaustion.48 While traditionally burnout among healthcare workers is not a newly recognized crisis, and has been associated with higher rates of anxiety, depression, and substance abuse,49 COVID-19 has presented unique challenges, leading to increased mental health issues among healthcare workers. Although several previous publications have reported on the prevalence of stress and burnout among US healthcare workers, to our knowledge, the current study is the first systematic review to examine burnout specifically among surgical trainees and surgeons during the COVID-19 pandemic. We defined burnout rates among surgeons and identified personal and professional factors associated with burnout relative to the COVID-19 pandemic. Of note, reported burnout rates among surgical trainees and attending surgeons varied widely in the literature, likely due to the different study populations and the varied burnout assessment tools used. The most commonly reported personal factors contributing to burnout included fear of contracting/transmitting COVID-19 and being female whereas professional factors related to increased COVID-19 patient clinical load, limited work experience, reduction in operative cases and redeployment to COVID-19 wards. The COVID-19 pandemic was also noted to have a negative impact on surgical education including reduced hands-on experience and concern about completing case requirements.
Personal factors associated with burnout during COVID-19 were complex and multifactorial. Interestingly, data on the impact of having family/children were somewhat conflicting. Specifically, in the pre-pandemic setting, “having children” (especially older children) was associated with decreased rates of burnout.7 , 50 Several studies similarly noted that “having children” was a protective factor against burnout during COVID-19.21 , 22 , 27 , 28 Specifically, Khalafallah and colleagues reported that neurosurgeons who did not have children were at 3-times higher odds of burnout versus individuals who did have children.21 In contrast, other studies highlighted the additional stress associated with finding childcare, inconsistent schooling schedules, and worries about virus transmission among young children.4 , 25 These data highlight how the COVID-19 specific context impacted the relative effect of children/family on individual risk of burnout among different individuals. In addition to children/family, female sex was also associated with a higher risk of COVID-19 related burnout across several medical subspecialties. Females may experience higher rates of burnout due to gender- related pay gap inequities, a lack of female role models, less advancement opportunities, sexual harassment, and poor work-life balance.51 The unique challenges experienced by providers and patients on COVID-19 wards, including the experience of illness and death without visitation from friends and family members, may put female surgeons at higher risk of emotional exhaustion and occupational burnout. Interestingly, Purvanova and Muros argued that it may be the expression of burnout, not the incidence of burnout itself that is different between genders.52 According to the authors, women are more likely to suffer from emotional exhaustion whereas men are more likely to describe depersonalization.
Burnout may be especially pervasive among physicians who are concerned about their work-place environment, as well as dissatisfied with their work-life balance.53, 54, 55 Contributors to burnout may include excessive workload, loss of autonomy, poor job satisfaction, as well as concerns for patient- and self-safety.56 , 57 In the current study, several specific work-based factors were associated with an increased risk of burnout. For, excessive example patient workload, as well as fear of acquiring or transmitting the COVID-19 virus were significant contributors to burnout.50 , 58 The need to redeploy surgical personnel from surgical services to COVID-19 wards was also an important factor associated with burnout among surgical trainees/surgeons, as was the cancellation of elective surgical cases.4 , 18 , 19 , 34 Utilization of virtual didactic sessions dramatically increased, which had a varied impact on resident education.59 In addition, decreased time in the OR and more limited exposure to hands-on surgical training generated concern among trainees about meeting case requirements, graduation, and fellowship opportunities. To assuage these concerns, several national organizations made changes to accommodate surgical trainees. Specifically, for the 2019 to 20 academic year, the American Board of Surgery (ABS) lowered the minimum requirement to 44 weeks of clinical time and decreased the minimum case requirement by 10% (i.e., 850-765).34 , 60 The American Board of Orthopedic Surgery (ABOS) gave the option to defer the written board exam if residents felt uncertain of a successful examination and modified the approach for the practice based oral examination.61 Longitudinal follow-up is needed to determine how these changes impact the global surgical workforce.
While no studies tested or aimed to develop interventions, several studies suggested ways to mitigate COVID-19 related burnout secondary to the COVID-19 pandemic, including formal PPE training, familiarization with pandemic protocols, and careful workload management.20 , 24 Other recommendations to reduce or prevent burnout included spending time with family and friends, doing exercise or yoga, keeping pets and listening to music or painting.37 Within the context of training programs providing meals, residency mentorship and seeking support with increased mental breaks were suggested to alleviate burnout symptoms.37 , 43 While helpful, these are individual-level interventions, whereas a comprehensive approach to mitigating burnout would also include organizational-level supports. Providing resources for providers mental health support and emergency childcare could be vital steps to maintaining a healthy workforce through the remainder of the pandemic.62 Additional qualitative research assessing specific needs of healthcare providers by role, specialty and other demographic/occupational factors would provide some much-needed insight.
Several limitations should be considered when interpreting results of the current study. As noted, the heterogeneity of tools used to measure burnout limited the ability to compare burnout rates across different publications and specialties. Additionally, while burnout was assessed in virtually every study with a validated tool, these measures have not been validated within the context of the COVID-19 pandemic. This manuscript aimed to reflect on the global experience of COIVD-19 on surgery, yet most publications included in the systematic review were also from high-income countries. As such, lower/middle-income countries, which had a very different experience with the COVID-19 pandemic due to more limited resources and inadequate PPE, were likely under-represented. In turn, data from the current study cannot be extrapolated to surgeons in those countries/clinical settings. Of note, the current review included studies performed between April 2020 and December 2021, during drastically different phases of disaster as originally defined by Zunin and Myers.63 The varying phases of the COVID-19 pandemic relative to the timing of any given study undoubtedly contributed to some heterogeneity in the data. Lastly, longitudinal data remain unavailable and therefore the long-term implications of burnout experienced by surgical trainees and surgeons during the COVID-19 pandemic remain unknown.
In conclusion, while there was variation among surgical trainees and surgeons across various studies, reported burnout associated with COVID-19 was high. In fact, numerous studies reported that as many as 1 in 2 surgical trainees and attending surgeons experienced COVID-19 related burnout. Intrinsic- (i.e., gender, age), family- (i.e., family/being married/having children or being single/not having children), as well as work-related extrinsic- (i.e., work-force deployment, risk of infection/spread, changes in educational format) factors were strongly associated with risk of burnout. As the threat of COVID-19 persists, it is important to note that health care workers continue to struggle with burnout and suffering. Interventions to ameliorate burnout among surgical trainees and surgeons should be informed by the factors identified in the current study and focus on those individuals most at risk including women and surgeons-in-training.
Funding
None.
Conflicts of interest
None.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jsurg.2022.04.015.
Appendix. SUPPLEMENTARY INFORMATION
References
- 1.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among healthcare workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. Published 2020 Mar 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. World Health Organization . World Health Organization; 2021. WHO Coronavirus Disease (COVID-19) Dashboard.https://covid19.who.int/ Published. [Google Scholar]
- 3.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis [published correction appears in Brain Behav Immun. 2021 Feb;92:247] Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdulaziz Al-Ghunaim T, Johnson J, Shekhar Biyani C. Psychological and occupational impact of the COVID-19 pandemic on UK surgeons: a qualitative investigation. BMJ Open. 2021;11:45699. doi: 10.1136/bmjopen-2020-045699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Burn-out an “occupational phenomenon”: International Classification of Diseases. Int Classif Dis. 2019 Published online. [Google Scholar]
- 6.Balasubramanian A, Paleri V, Bennett R, Paleri V. Impact of COVID-19 on the mental health of surgeons and coping strategies. Head Neck. 2020;42(7):1638–1644. doi: 10.1002/hed.26291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol. 2012;30(11):1235–1241. doi: 10.1200/JCO.2011.39.7380. [DOI] [PubMed] [Google Scholar]
- 8.Patti MG, Schlottmann F, Sarr MG. The problem of burnout among surgeons. JAMA Surg. 2018;153(5):403–404. doi: 10.1001/jamasurg.2018.0047. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2016;4(1):1. doi: 10.1186/2046-4053-4-1. Published 2015 Jan 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaufeli WB, Maslach C, Leiter MP, Jackson SE. Maslach Burnout Inventory - General Survey (MBI-GS) MBI Man. 1996 Published online. [Google Scholar]
- 11.Linzer M, Visser MRM, Oort FJ, et al. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001;111(2):170–175. doi: 10.1016/S0002-9343(01)00814-2. [DOI] [PubMed] [Google Scholar]
- 12.Trockel M, Bohman B, Lesure E, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. 2018;42(1):11–24. doi: 10.1007/s40596-017-0849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schaufeli W, Van Dierendonck D. Utrechtse Burnout Schaal (UBOS) De Psycholoog. 2001 Published online. [Google Scholar]
- 14.Stamm BH. Professional Quality of Life: Compassion Satisfaction and Fatigue Version 5 (ProQOL. ProQOL. 2009 Published online. [Google Scholar]
- 15.Dyrbye LN, Satele D, Sloan J, Shanafelt TD. Ability of the physician well-being index to identify residents in distress. J Grad Med Educ. 2014;6(1):78–84. doi: 10.4300/jgme-d-13-00117.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shirom A. Burnout in work organizations. Int Rev Industr Org Psychol. 1989;5(6):25–48. [Google Scholar]
- 17.Kellermeyer L, Harnke B, Knight S. Covidence and Rayyan. J Med Libr Assoc. 2018;106(4):580–583. doi: 10.5195/JMLA.2018.513. [DOI] [Google Scholar]
- 18.Ashry AH, Soffar HM, Alsawy MF. Neurosurgical education during COVID-19: challenges and lessons learned in Egypt. Egypt J Neurol Psychiatry Neurosurg. 2020;56(1):110. doi: 10.1186/s41983-020-00242-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aziz H, James T, Remulla D, et al. Effect of COVID-19 on Surgical Training Across the United States: A National Survey of General Surgery Residents. J Surg Educ. 2021;78(2):431–439. doi: 10.1016/j.jsurg.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kabir T, Tan AYH, Koh FHX, Chew MH. Burnout and professional fulfilment among surgeons during the COVID-19 pandemic. Br J Surg. 2021;108(1):e3–e5. doi: 10.1093/bjs/znaa001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khalafallah AM, Lam S, Gami A, et al. A national survey on the impact of the COVID-19 pandemic upon burnout and career satisfaction among neurosurgery residents. J Clin Neurosci. 2020;80:137–142. doi: 10.1016/j.jocn.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khalafallah AM, Lam S, Gami A, et al. Burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic. Clin Neurol Neurosurg. 2020;198:106193. doi: 10.1016/j.clineuro.2020.106193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osama M, Zaheer F, Saeed H, et al. Impact of COVID-19 on surgical residency programs in Pakistan; A residents’ perspective. Do programs need formal restructuring to adjust with the “new normal”? A cross-sectional survey study. Int J Surg. 2020;79:252–256. doi: 10.1016/j.ijsu.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tan YQ, Chan MT, Chiong E. Psychological health among surgical providers during the COVID-19 pandemic: a call to action. Br J Surg. 2020;107(11):e459–e460. doi: 10.1002/bjs.11915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seow JW, Lin S, Khor YP, Hey DH, Kagda FH. Stress and strain in an orthopaedic department on the frontlines during the COVID-19 pandemic: an analysis of burnout and the factors influencing it. Ann Acad Med Singapore. 2020;49(10):814–816. doi: 10.47102/annals-acadmedsg.2020289. [DOI] [PubMed] [Google Scholar]
- 26.Cai Y, Gulati A, Jiam NT, et al. Evolving otolaryngology resident roles and concerns at the peak of the US COVID-19 pandemic. Head Neck. 2020;42(12):3712–3719. doi: 10.1002/hed.26438. [DOI] [PubMed] [Google Scholar]
- 27.Civantos AM, Bertelli A, Gonçalves A, et al. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: a national study. Am J Otolaryngol. 2020;41(6):102694. doi: 10.1016/j.amjoto.2020.102694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Civantos AM, Byrnes Y, Chang C, et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head and Neck. 2020;42(7):1597–1609. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coleman JR, Abdelsattar JM, Glocker RJ, RAS-ACS COVID-19 Task Force COVID-19 pandemic and the lived experience of surgical residents, fellows, and early-career surgeons in the American College of Surgeons. J Am Coll Surg. 2021;232(2):119–135. doi: 10.1016/j.jamcollsurg.2020.09.026. e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cravero AL, Kim NJ, Feld LD, et al. Impact of exposure to patients with COVID-19 on residents and fellows: an international survey of 1420 trainees. Postgrad Med J. 2021;97(1153):706–715. doi: 10.1136/postgradmedj-2020-138789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dimitriu MCT, Pantea-Stoian A, Smaranda AC, et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. 2020;144:109972. doi: 10.1016/j.mehy.2020.109972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fargen KM, Leslie-Mazwi TM, Klucznik RP, et al. The professional and personal impact of the coronavirus pandemic on US neurointerventional practices: a nationwide survey. J Neurointerv Surg. 2020;12(10):927–931. doi: 10.1136/neurintsurg-2020-016513. [DOI] [PubMed] [Google Scholar]
- 33.Firew T, Sano ED, Lee JW, et al. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open. 2020;10(10):e042752. doi: 10.1136/bmjopen-2020-042752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abdelsattar JM, Coleman JR, Nagler A, et al. Lived experiences of surgical residents during the COVID-19 pandemic: a qualitative assessment. J Surg Educ. 2021;78(6):1851–1862. doi: 10.1016/j.jsurg.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao KA, Attai D, Bleicher R, et al. Covid-19 related oncologist's concerns about breast cancer treatment delays and physician well-being (the CROWN study) Breast Cancer Res Treat. 2021;186(3):625–635. doi: 10.1007/s10549-021-06101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu JL, Cho DY, DeSanti RL, Kneib CJ, Friedrich JB, Colohan SM. Resident experiences with virtual education during the COVID-19 crisis. J Plast Reconstr Aesthetic Surg. 2021;74(8):1931–1971. doi: 10.1016/j.bjps.2021.05.037. [DOI] [PubMed] [Google Scholar]
- 37.Zoorob D, Shah S, La Saevig D, Murphy C, Aouthmany S, Brickman K. Insight into resident burnout, mental wellness, and coping mechanisms early in the COVID-19 pandemic. PLoS One. 2021;16(4):e0250104–965. doi: 10.1371/journal.pone.0250104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al-Humadi S, Bronson B, Muhlrad S, Paulus M, Hong H, Cáceda R. Depression, suicidal thoughts, and burnout among physicians during the COVID-19 pandemic: a survey-based cross-sectional study. Acad Psychiatry. 2021;45(5):557–565. doi: 10.1007/s40596-021-01490-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chou DW, Staltari G, Mullen M, Chang J, Durr M. Otolaryngology resident wellness, training, and education in the early phase of the COVID-19 pandemic. Ann Otol Rhinol Laryngol. 2021;130(8):904–914. doi: 10.1177/0003489420987194. [DOI] [PubMed] [Google Scholar]
- 40.Elghazally SA, Alkarn AF, Elkhayat H, Ibrahim AK, Elkhayat MR. Burnout impact of covid- 19 pandemic on health-care professionals at Assiut University Hospitals, 2020. Int J Environ Res Public Health. 2021;18(10):5368. doi: 10.3390/ijerph18105368. Published 2021 May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guha A, Plzak J, Schalek P, Chovanec M. Extremely wicked, shockingly evil and undoubtedly COVID-19: the silent serial killer. Eur Arch Oto-Rhino-Laryngology. 2021;278(6):2101–2106. doi: 10.1007/s00405-020-06537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hines SE, Chin KH, Glick DR, Wickwire EM. Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the covid-19 pandemic. Int J Environ Res Public Health. 2021;18(2):488. doi: 10.3390/ijerph18020488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lazarides AL, Belay ES, Anastasio AT, Cook CE, Anakwenze OA. Physician burnout and professional satisfaction in orthopedic surgeons during the COVID-19 Pandemic. Work. 2021;69(1):15–22. doi: 10.3233/WOR-205288. [DOI] [PubMed] [Google Scholar]
- 44.Mion G, Hamann P, Saleten M, Plaud B, Baillard C. Psychological impact of the COVID-19 pandemic and burnout severity in French residents: A national study. Eur J Psychiatry. 2021;35:173–180. doi: 10.1016/j.ejpsy.2021.03.005. [DOI] [Google Scholar]
- 45.Poelmann FB, Koëter T, Steinkamp PJ, Vriens MR, Verhoeven B, Kruijff S. The immediate impact of the coronavirus disease 2019 (COVID-19) pandemic on burn-out, work-engagement, and surgical training in the Netherlands. Surgery. 2021;170(3):719–726. doi: 10.1016/j.surg.2021.02.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Casar Harris R, Amanda Dew M, Lee A, et al. The role of religion in heart-transplant recipients’ longterm health and well-being. J Relig Health. 1995;34(1):17–32. doi: 10.1007/BF02248635. [DOI] [PubMed] [Google Scholar]
- 47.Prasad K, McLoughlin C, Stillman M, et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine. 2021;35:100879. doi: 10.1016/j.eclinm.2021.100879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brera AS, Arrigoni C, Dellafiore F, et al. Burnout syndrome and its determinants among healthcare workers during the first wave of the covid-19 outbreak in italy: a cross-sectional study to identify sex-related differences. Med del Lav. 2021;112(4):306–319. doi: 10.23749/mdl.v112i4.11316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dzau VJ, Kirch D, Nasca T. Preventing a parallel pandemic - A National Strategy to Protect Clinicians’ Well-Being. N Engl J Med. 2020;383(6):513–515. doi: 10.1056/nejmp2011027. [DOI] [PubMed] [Google Scholar]
- 50.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 51.Robinson GE. Stresses on women physicians: consequences and coping techniques. Depress Anxiety. 2003;17(3):180–189. doi: 10.1002/da.10069. [DOI] [PubMed] [Google Scholar]
- 52.Purvanova RK, Muros JP. Gender differences in burnout: a meta-analysis. J Vocat Behav. 2010;77(2):168–185. doi: 10.1016/j.jvb.2010.04.006. [DOI] [Google Scholar]
- 53.Guest RS, Baser R, Li Y, Scardino PT, Brown AE, Kissane DW. Cancer surgeons’ distress and well-being, II: modifiable factors and the potential for organizational interventions. Ann Surg Oncol. 2011;18(5):1236–1242. doi: 10.1245/s10434-011-1623-5. [DOI] [PubMed] [Google Scholar]
- 54.Dyrbye LN, Varkey P, Boone SL, Satele DV., Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367. doi: 10.1016/j.mayocp.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 55.Dyrbye LN, Freischlag J, Kaups KL, et al. Work-home conflicts have a substantial impact on career decisions that affect the adequacy of the surgical workforce. Arch Surg. 2012;147(10):933–939. doi: 10.1001/archsurg.2012.835. [DOI] [PubMed] [Google Scholar]
- 56.Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Heal. 2019;35(2):157–175. doi: 10.1002/smi.2849. [DOI] [PubMed] [Google Scholar]
- 57.Bender A, Farvolden P. Depression and the workplace: a progress report. Curr Psychiatry Rep. 2008;10(1):73–79. doi: 10.1007/s11920-008-0013-6. [DOI] [PubMed] [Google Scholar]
- 58.Galaiya R, Kinross J, Arulampalam T. Factors associated with burnout syndrome in surgeons: a systematic review. Ann R Coll Surg Engl. 2020;102(6):401–407. doi: 10.1308/rcsann.2020.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lazaro T, Srinivasan VM, Rahman M, et al. Virtual education in neurosurgery during the COVID-19 pandemic. Neurosurg Focus. 2020;49(6):E17. doi: 10.3171/2020.9.FOCUS20672. [DOI] [PubMed] [Google Scholar]
- 60.Surgery TAB of. No Title. Modifications to training requirements. Published 2020. https://www.absurgery.org/default.jsp?news_covid19_trainingreq
- 61.Wright RW, Armstrong AD, Azar FM, et al. The American Board of Orthopaedic Surgery Response to COVID-19. J Am Acad Orthop Surg. 2020;28(11):e465–e468. doi: 10.5435/JAAOS-D-20-00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharifi M, Asadi-Pooya AA, Mousavi-Roknabadi RS. Burnout among healthcare providers of COVID-19; a systematic review of epidemiology and recommendations. Arch Acad Emerg Med. 2020;90(1):e7. doi: 10.22037/aaem.v9i1.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.DeWolfe DJ.Training manual for mental health and human service workers in major disasters.; 2000.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.