Abstract
Purpose
The age-adjusted Charlson comorbidity index (ACCI) is a useful measure of comorbidity to standardize the evaluation of elderly patients and has been reported to predict mortality in various cancers. To our best knowledge, no studies have examined the relationship between the ACCI and survival of elderly patients with cancer. Therefore, the primary objective of this study was to investigate the relationship between the ACCI and survival of elderly patients with cancer.
Patients and Methods
A total of 64 elderly patients (>80 years) with cancer between 2011 and 2021 were enrolled in this study. According to the ACCI, the age-adjusted comorbidity index was calculated by weighting individual comorbidities; patients with ACCI<11 were considered the low-ACCI group, whereas those with ACCI≥11 were considered the high-ACCI group. The correlations between the ACCI score and survival outcomes were statistically analyzed.
Results
There was a significant difference in overall survival (OS) and progression-free survival (PFS) between the high-ACCI group and the low-ACCI group (P<0.001). The median OS time of the high-ACCI group and the low-ACCI group were 13.9 (10.5–22.0) months and 51.9 (34.1–84.0) months, respectively. The 2-, 3-, and 5-year survival rates of the high-ACCI group were 28.1%, 18.8%, and 4.2%, respectively, whereas the 2-, 3-, and 5-year survival rates of the low-ACCI group were 77.3%, 66.4%, and 39.1%, respectively. Multivariate analysis showed that ACCI was independently associated with OS (HR=1.402, 95% CI: 1.226–1.604, P < 0.05) and PFS (HR=1.353, 95% CI: 1.085–1.688, P = 0.0073).
Conclusion
The ACCI score is a significant independent predictor of prognosis in elderly patients with cancer.
Keywords: age-adjusted Charlson comorbidity index, comorbidity, elderly cancer patients, prognosis
Introduction
Given that the incidence of cancer rises with age and that the world population ages, the incidence of malignant cancer is increasing year by year. According to the World Health Organization (WHO), the elderly are people aged 80 years and over. The National Cancer Center released the latest cancer data from China, reporting 4.29 million new cases of cancer and 2.82 million cancer-related deaths annually, and elderly individuals comprise 36% of these numbers. Owing to the aging of the population, this proportion is expected to markedly increase in the next decades. Thus, special attention should be paid to elderly patients with cancer. Owing to the decline of the physical function in the elderly, they often have a variety of chronic diseases; two or more diseases coexisting at the same time are marked as senile comorbidity.1 Elderly patients with cancer have a high burden of chronic diseases, so it is difficult to achieve the optimal treatment results.
The age-adjusted Charlson comorbidity index (ACCI) is a measure of comorbidity, which has widely been used to measure the burden of complex comorbidities in various disease subgroups, including cardiac disease, renal disease, liver disease, and non-small cell lung cancer.2–6 The ACCI incorporates the patient’s age as a correction variable in the final CCI, and the several studies have shown that it is a useful tool for predicting both the short-term and long-term outcomes in various cancers.7,8 The ACCI has been shown to play an important role in many aspects of the care of older cancer patients, including treatment selection, response to therapy, tumor progression, morbidity, and survival outcomes.9–11 Thus far, the ACCI has been clearly reported as a prognostic factor in patients with hepatocellular carcinoma, breast cancer, gastric cancer, and colorectal cancer.12–17 However, there are limited data on the predictive value of the ACCI in elderly cancer patients older than 80 years. In this study, we aimed to evaluate the relationship between ACCI score and survival of elderly cancer patients.
Patients and Methods
Patient Population
This was a retrospective study included patients from the Geriatrics Department, Jinling Hospital, Medical School of Nanjing University. The elderly patients aged over 80 years between January 2011 and December 2021 were enrolled based on medical record assessments. Eligibility criteria include patients newly diagnosed tumors over 80 years. We collected the basic characteristics including age, gender, histology, Eastern Cooperative Oncology Group performance status (ECOG), PFS, OS, smoking status, chemotherapy, radiotherapy, and laboratory examination data were recorded. The study was approved by the ethics committee of the hospital.
The Age-Adjusted Charlson Comorbidity Index
The comorbidity score was calculated at the time of cancer diagnosis based on the clinical history. The ACCI was calculated by adding the comorbidity score and the age. The ACCI score included 19 different medical conditions and each comorbidity condition was rated from 1 to 6 points to sum an index score (Table 1). The ACCI scores were calculated with additional points added for age. Each decade over the age of 40 years was assigned a comorbidity score of 1.18 In the current study, the cutoff value for the ACCI (<11 or ≥11) was arbitrarily determined based on the median and average ACCI values of the study participants.
Table 1.
The Age-Adjusted Charlson Comorbidity Index
| Point | Comorbidity |
|---|---|
| 1 | Myocardial infarction, heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disorder, peptic ulcer disease, mild liver disease, diabetes mellitus without complications |
| 2 | Diabetes mellitus with complications, moderate-to-severe renal disease, hemiplegia, leukaemia, lymphoma, tumor without metastases |
| 3 | Moderate-to-severe liver disease |
| 6 | Metastatic solid tumors, acquired immunodeficiency syndrome |
Statistical Analysis
We used descriptive statistics to illustrate patients’ demographic characteristics and clinical information. Quantitative data, such as age, carcino-embryonic antigen (CEA), glycosylated hemoglobin -type A1c (HbA1c), hemoglobin (Hb), platelets (PLT), albumin (Alb), and creatinine (Cr), were compared by Student’s t-test. Qualitative data, such as gender, ECOG, smoking, hypertension, coronary heart disease (CHD), chemotherapy, radiotherapy, and cancer type were compared by chi-square test or Fisher’s exact probability test.
The outcome measures were OS and PFS. The OS was defined as the time from random assignment to death owing to any cause or the end of the study. The PFS was defined as the time from randomization to the tumor progression, death or end of the study. A one-sided Log rank test was used to assess the OS and PFS between different ACCI groups. The Kaplan-Meier method was also used to estimate the median OS and graphically display the OS curve in each of the ACCI groups. A Cox proportional-hazard model was used to assess the hazard ratio (HR) and its 95% confidence interval (CI). The PFS was evaluated in the same way as the OS.
Results
Patient Characteristics
A total of 64 patients with ACCI score from 7 to 16 were enrolled. The mean age of the patients was 88 (±6.1) years, 54 patients (84.38%) were male and 10 patients (15.62%) were female. Patients with ACCI score <11 were classified to the low-ACCI group (N=32), whereas those with ACCI score≥11 were classified to the high-ACCI group (N=32). As shown in Table 2, there were no significant differences between the low-ACCI group and the high-ACCI group in any of the baseline characteristics (P>0.05), indicating that the baseline data were well balanced between the two groups.
Table 2.
Demographic and Clinical Characteristics of the Patients
| Characteristic | Low-ACCI (N=32) | High-ACCI (N=32) | Total (N=64) | P-value |
|---|---|---|---|---|
| Age (year) | 88.69±5.86 | 86.50±6.22 | 87.59±6.10 | 0.1527 |
| Gender | 0.1685 | |||
| Male, n (%) | 29 (90.63%) | 25 (78.13%) | 54 (84.38%) | |
| Female, n (%) | 3 (9.37%) | 7 (21.87%) | 10 (15.62%) | |
| ECOG | 0.3087 | |||
| 1–2, n (%) | 21 (65.62%) | 17 (53.13%) | 38 (59.37%) | |
| 3–4, n (%) | 11 (34.38%) | 15 (46.87%) | 26 (40.63%) | |
| Smoking | 0.4513 | |||
| Yes, n (%) | 16 (50.00%) | 13 (40.62%) | 29 (45.31%) | |
| No, n (%) | 16 (50.00%) | 19 (59.38%) | 35 (54.69%) | |
| Hypertension | 0.1306 | |||
| Yes, n (%) | 21 (65.62%) | 15 (46.87%) | 36 (56.25%) | |
| No, n (%) | 11 (34.38%) | 17 (53.13%) | 28 (43.75%) | |
| CHD | 0.2057 | |||
| Yes, n (%) | 21 (65.62%) | 16 (50.00%) | 27 (42.19%) | |
| No, n (%) | 11 (34.38%) | 16 (50.00%) | 37 (57.81%) | |
| Chemotherapy | 0.3135 | |||
| Yes, n (%) | 16 (50.00%) | 20 (62.50%) | 36 (56.25%) | |
| No, n (%) | 16 (50.00%) | 12 (37.05%) | 28 (43.75%) | |
| Radiotherapy | 1.000 | |||
| Yes, n (%) | 6 (18.75%) | 6 (18.75%) | 12 (18.75%) | |
| No, n (%) | 26 (81.25%) | 26 (81.25%) | 52 (81.25%) | |
| Cancer type | 0.3031 | |||
| Gastrointestinal, n (%) | 12 (37.5%) | 17 (53.13%) | 29 (45.31%) | |
| Respiratory, n (%) | 10 (31.25%) | 10 (31.25%) | 20 (31.25%) | |
| Urinary, n (%) | 7 (21.88%) | 2 (6.25%) | 9 (14.06%) | |
| Other, n (%) | 3 (9.37%) | 3 (9.37%) | 6 (9.38%) | |
| CEA (ng/mL) | 9.82±24.60 | 25.08±62.03 | 17.57±47.71 | 0.2041 |
| HbA1c (%) | 6.08±0.96 | 6.77±1.46 | 6.39±1.25 | 0.0589 |
| Hb (g/L) | 117.20±22.48 | 106.70±27.38 | 111.93±25.41 | 0.0981 |
| PLT (*109/L) | 180.10±75.17 | 174.40±68.54 | 177.28±71.41 | 0.7529 |
| Alb (g/L) | 36.14±6.75 | 34.41±4.95 | 35.28±5.94 | 0.2458 |
| Cr (umol/L) | 84.37±36.21 | 103.50±86.53 | 93.92±66.50 | 0.2539 |
Note: Data are expressed as mean ± SD or n (%).
Abbreviations: ACCI, the age-adjusted Charlson comorbidity index; ECOG, Eastern Cooperative Oncology Group Performance Status; CHD, coronary heart disease; CEA, carcino-embryonic antigen; HbA1c, glycosylated hemoglobin type A1c; Hb, hemoglobin; PLT, platelet; Alb, albumin; Cr, creatinine.
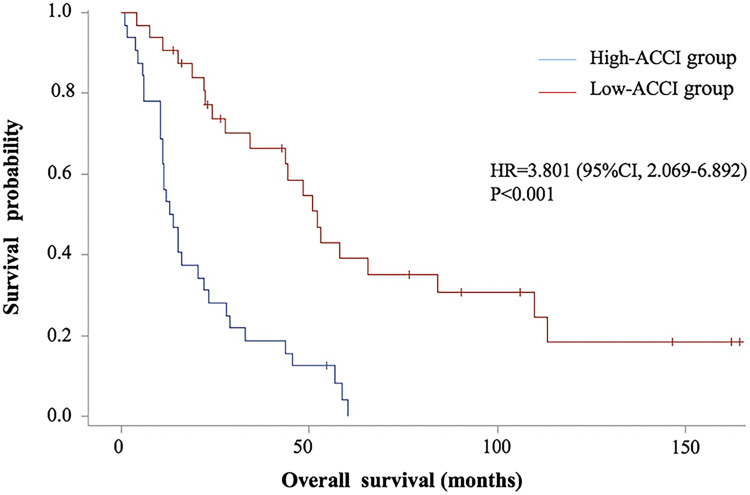
Analysis of Overall Survival Time
The one-sided Log rank test revealed a significant difference in the OS between the high-ACCI group and the low-ACCI group cancer patients (P<0.001). The median OS time of the high-ACCI group and the low-ACCI group were 13.9 (10.5–22.0) months and 51.9 (34.1–84.0) months, respectively. Additionally, the 2-, 3-, and 5-year survival rates of the high-ACCI group were 28.1%, 18.8%, and 4.2% respectively, whereas the 2-, 3-, and 5-year survival rates of the low-ACCI group were 77.3%, 66.4%, and 39.1% respectively (Table 3). The survival rate of the high-ACCI group was significantly higher than that of the low-ACCI group. The OS curves in all of the patients are shown in Figure 1.
Table 3.
Analysis of Overall Survival Time
| Variables | Parameter | Low-ACCI (N=32) | High-ACCI (N=32) |
|---|---|---|---|
| Events | |||
| Death | n (%) | 11 (65.62) | 31 (96.87) |
| Censor | n (%) | 21 (34.38) | 1 (3.13) |
| Overall survival (month) | Median (95% CI) | 51.9 (34.1–84.0) | 13.9 (10.5 −22.0) |
| Log rank p-value | <0.001 | ||
| HR (95% CI) | 3.801 (2.069 −6.982) | ||
| Survival rate | |||
| 2 years (95% CI) | 0.773 (0.581–0.885) | 0.281 (0.140–0.441) | |
| 3 years (95% CI) | 0.664 (0.464–0.804) | 0.188 (0.076–0.337) | |
| 5 years (95% CI) | 0.391 (0.211–0.567) | 0.042 (0.003–0.169) |
Abbreviations: ACCI, the age-adjusted Charlson comorbidity index; HR, hazard ratio.
Figure 1.
Overall survival curve of high-ACCI vs low-ACCI group.
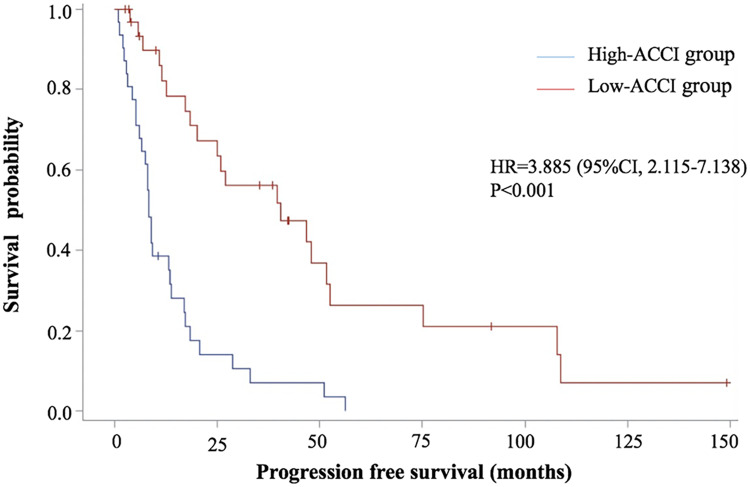
Analysis of Progression-Free Survival
The one-sided Log rank test revealed a significant difference in the PFS between the high-ACCI group and low-ACCI group cancer patients (P<0.001). The median PFS of the high-ACCI group and the low-ACCI group were 8.5 (6.1 −13.6) months and 40.6 (20.1–52.4) months, respectively (Table 4). The PFS curves in all of the patients are shown in Figure 2.
Table 4.
Analysis of Progression-Free Survival Time
| Variables | Parameter | Low-ACCI (N=32) | High-ACCI (N=32) |
|---|---|---|---|
| Events | |||
| Death | n (%) | 11 (65.62) | 31 (96.87) |
| Censor | n (%) | 21 (34.38) | 1 (3.13) |
| PFS (month) | Median (95% CI) | 40.6 (20.1–52.4) | 8.5 (6.1–13.6) |
| Log rank p value | <0.001 | ||
| HR (95% CI) | 3.885 (2.115–7.138) |
Abbreviations: ACCI, the age-adjusted Charlson comorbidity index; HR, hazard ratio.
Figure 2.
Progression free survival curve of high-ACCI vs low-ACCI group.
Predictive Risk Factors for OS
Univariate analysis was conducted to determine the predictors of OS using univariate Cox model regression. ACCI (HR=1.402, 95% CI: 1.226–1.604, P < 0.05) and CEA (HR=1.006, 95% CI: 1.001–1.011, P = 0.0234) were independently associated with overall survival. Other factors had no significant association with the OS (P > 0.05).
Multivariate analysis was conducted to determine the predictors of OS using multivariate Cox model regression. ACCI score (HR=1.456, 95% CI: 1.162–1.824, P = 0.0234) was independently associated with overall survival. Other factors had no significant association with the OS (P > 0.05) (Table 5).
Table 5.
The COX Proportional Hazards Model Analyses Predictors for OS
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Age | 0.974 (0.926–1.024) | 0.2986 | 1.046 (0.930–1.177) | 0.4506 |
| Gender | ||||
| Male | 1.003 (0.469–2.144) | 0.9949 | 0.784 (0.200–3.068) | 0.7267 |
| Female | ||||
| ECOG | ||||
| 1–2 | ||||
| 3–4 | 1.228 (0.700–2.155) | 0.4730 | 0.984 (0.307–3.154) | 0.9777 |
| Smoking | ||||
| Yes | 1.155 (0.667–2.000) | 0.6063 | 1.660 (0.743–3.705) | 0.2163 |
| No | ||||
| Hypertension | ||||
| Yes | 0.636 (0.365–1.107) | 0.1091 | 0.612 (0.279–1.341) | 0.2200 |
| No | ||||
| CHD | ||||
| Yes | 0.628 (0.357–1.104) | 0.1061 | 0.401 (0.108–1.482) | 0.1705 |
| No | ||||
| Chemotherapy | ||||
| Yes | 1.031 (0.591–1.798) | 0.9148 | 0.967 (0.463–2.016) | 0.9279 |
| No | ||||
| Radiotherapy | ||||
| Yes | 0.893 (0.457–1.742) | 0.7389 | 1.801 (0.629–5.152) | 0.2728 |
| No | ||||
| ACCI | 1.402 (1.226–1.604) | <0.001 | 1.456 (1.162–1.824) | 0.0011 |
| HbA1c | 1.009 (0.756–1.346) | 0.9540 | 0.805 (0.567–1.143) | 0.2248 |
| CEA | 1.006 (1.001–1.011) | 0.0234 | 1.008 (0.992–1.024) | 0.3192 |
| Alb | 0.992 (0.945–1.042) | 0.7529 | 1.008 (0.944–1.076) | 0.8097 |
Abbreviations: ACCI, the age-adjusted Charlson comorbidity index; ECOG, Eastern Cooperative Oncology Group Performance Status; CHD, coronary heart disease; CEA, carcino-embryonic antigen; HbA1c, glycosylated hemoglobin type A1c; Alb, albumin.
Predictive Risk Factors for PFS
Univariate analysis was conducted to determine the predictors of PFS using univariate cox model regression. ACCI score (HR=1.387, 95% CI: 1.212–1.587, P < 0.05) was independently associated with the PFS. Other factors had no significant association with the PFS (P > 0.05).
Multivariate analysis was conducted to determine the predictors of OS using multivariate cox model regression. ACCI (HR=1.353, 95% CI: 1.085–1.688, P = 0.0073) was independently associated with PFS. Other factors had no significant association with the PFS (P > 0.05) (Table 6).
Table 6.
The COX Proportional Hazards Model Analyses Predictors for PFS
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Age | 0.963 (0.914–1.016) | 0.1693 | 1.027 (0.908–1.162) | 0.6667 |
| Gender | ||||
| Male | 0.920 (0.430–1.965) | 0.8290 | 0.576 (0.142–2.339) | 0.4404 |
| Female | ||||
| ECOG | ||||
| 1–2 | ||||
| 3–4 | 1.220 (0.687–2.166) | 0.4967 | 1.181 (0.376–3.712) | 0.7757 |
| Smoking | ||||
| Yes | 1.191 (0.683–2.077) | 0.5376 | 1.691 (0.776–3.683) | 0.1862 |
| No | ||||
| Hypertension | ||||
| Yes | 0.619 (0.352–1.091) | 0.0971 | 0.641 (0.292–1.411) | 0.2695 |
| No | ||||
| CHD | ||||
| Yes | 0.597 (0.335–1.065) | 0.0807 | 0.440 (0.132–1.468) | 0.1816 |
| No | ||||
| Chemotherapy | ||||
| Yes | 1.092 (0.621–1.921) | 0.7600 | 1.052 (0.499–2.218) | 0.8944 |
| No | ||||
| Radiotherapy | ||||
| Yes | 0.904 (0.461–1.772) | 0.7680 | 1.587 (0.538–4.680) | 0.4027 |
| No | ||||
| ACCI | 1.387 (1.212–1.587) | <0.001 | 1.353 (1.085–1.688) | 0.0073 |
| HbA1c | 1.062 (0.800–1.410) | 0.6769 | 0.917 (0.664–1.306) | 0.6325 |
| CEA | 1.004 (0.999–1.010) | 0.1465 | 1.006 (0.988–1.024) | 0.5241 |
| Alb | 0.994 (0.944–1.045) | 0.8022 | 1.004 (0.942–1.071) | 0.8960 |
Abbreviations: ACCI, the age-adjusted Charlson comorbidity index; ECOG, Eastern Cooperative Oncology Group Performance Status; CHD, coronary heart disease; HR, hazard ratio; CI, confidence interval; CEA, carcino-embryonic antigen; HbA1c, glycosylated hemoglobin type A1c; Hb, hemoglobin; Alb, albumin.
Discussion
The currently recognized adverse prognostic factors for cancer patients include the type, size, and TNM staging of the tumor.19 In elderly patients, non-tumor factors such as comorbidities and nutritional status are also affect the prognosis.20,21 The ACCI takes into account 19 comorbidities, including cardiovascular disease, diabetes, liver disease, and pulmonary disease, to classify comorbidities that may change the risk of death for longitudinal research.22
To the best of our knowledge, this is the first report demonstrating the correlation between the clinical significance of ACCI score and the survival outcomes of elderly cancer patients (≥80 years). In this study, there were significant differences in the OS and PFS between the high-ACCI group and the low-ACCI group (P<0.001). Multivariate analysis showed that ACCI score was independently associated with OS (HR=1.402, 95% CI 1.226–1.604, P < 0.05) and PFS (HR=1.353, 95% CI 1.085–1.688, P = 0.0073).
Our findings support the previous reports that showed the usefulness of ACCI score for predicting mortality of patients with cancer.23–25 Qu et al evaluated the clinical impact of the ACCI in 268 patients who treated with curative surgery for intrahepatic cholangiocarcinoma. Multivariate analysis showed that ACCI score was associated with the OS, and higher scores were associated with poorer prognosis (HR=1.134, 95% CI 1.015–1.267, P=0.026).26 Tominaga et al retrospectively collected data on 250 patients with colorectal cancer aged over 75 years. Multivariate analysis showed that CCI ≥ 2 (HR=5.2, 95% CI 1.30–12.1, P=0.01) was an important determinant of postoperative outcome. Patients with high CCI scores tended to have lower OS (P = 0.03). The CCI helped to predict postoperative outcomes in elderly patients with colorectal cancer. Lin et al27 evaluated data on 1476 patients with gastric cancer who underwent radical gastrectomy. In univariate analysis, ACCI score and age were statistically significant prognostic factors in patients with gastric cancer. Multivariate analysis showed ACCI score remained the independent prognostic factor for patients with gastric cancer, while age and CCI were not independent prognostic factors. These result show that as a comprehensive index with age and complications, the ACCI provides better prognostic evaluation for patients. Although the effects of age and comorbidities should be assessed separately in univariate, bivariate, or multivariate analyses. The index is intended to be a simple, crude, comprehensive risk assessment used by clinicians.28
There is another important result of our study. In the univariate analysis and multivariate analysis, ECOG score did not prolong the OS and PFS in elderly patients with cancer. Performance status of elderly cancer patients defined by using ECOG score is commonly used in younger (<65 years) patients with cancer. However, ECOG score cannot estimate the functional limitations of incidence rate and mortality in elderly patients.29 Elderly patients with good ECOG performance status scores are generally considered appropriate and can receive standard intensive treatment comparable to younger patients. However, these elderly cancer patients are heterogeneous. Some patients, even with ECOG performance status scores, have a low survival rate. ECOG does not always reflect the functional status of elderly cancer patients.30 This is consistent with our results. Therefore, we believe that ACCI score can better evaluate the functional status of elderly cancer patients.
There are some major limitations in our study. First, this is a retrospective study from a single center. Retrospective clinical data from medical records for the elderly population are not conducive to controlling all potential confounding biases that may affect the OS. Second, due to more restrictive conditions, the number of patients is small (N=64). Third, the tumor staging standards of each system are different, and the data were collected retrospectively. Thus, it was impossible to stage the cancer and collect the toxicity data after therapy including chemotherapy and radiotherapy.
Despite these limitations, ACCI score is a prognostic indicator independent of the treatment benefits of elderly cancer patients. Therefore, we believe that ACCI score can help doctors to predict mortality and prognosis in the routine clinical environment of elderly cancer patients. Further randomized prospective studies are needed to verify the effects of ACCI score on the survival in elderly cancer patients.
Conclusion
In conclusion, in patients aged 80 years or more, long term-prognosis is independently influenced by ACCI score and CEA. Thus, ACCI score is a valuable prognostic indicator for physicians to evaluate elderly cancer patients for optimal treatment.
Acknowledgments
This study was supported primarily by grants from the Health Project Foundation (19BJZ10 and 17BJZ17).
Ethics Statement
This retrospective study was approved by the Research Ethics Committee of Jinling Hospital of Nanjing University. We promise that all the data of the participants was maintained with confidentiality. The study protocol abided by the principles of the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
No conflict of interest was declared by the authors.
References
- 1.Zemedikun DT, Gray LJ, Khunti K, Davies MJ, Dhalwani NN. Patterns of multimorbidity in middle-aged and older adults: an analysis of the UK biobank data. Mayo Clin Proc. 2018;93(7):857–866. doi: 10.1016/j.mayocp.2018.02.012 [DOI] [PubMed] [Google Scholar]
- 2.Zhao L, Leung LH, Wang J, et al. Association between Charlson comorbidity index score and outcome in patients with stage IIIB-IV non-small cell lung cancer. BMC Pulm Med. 2017;17(1):112. doi: 10.1186/s12890-017-0452-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myers RP, Quan H, Hubbard JN, Shaheen AA, Kaplan GG. Predicting in-hospital mortality in patients with cirrhosis: results differ across risk adjustment methods. Hepatology. 2009;49(2):568–577. doi: 10.1002/hep.22676 [DOI] [PubMed] [Google Scholar]
- 4.Lee DS, Donovan L, Austin PC, et al. Comparison of coding of heart failure and comorbidities in administrative and clinical data for use in outcomes research. Med Care. 2005;43(2):182–188. doi: 10.1097/00005650-200502000-00012 [DOI] [PubMed] [Google Scholar]
- 5.Hemmelgarn BR, Manns BJ, Quan H, Ghali WA. Adapting the Charlson comorbidity index for use in patients with ESRD. Am J Kidney Dis. 2003;42(1):125–132. doi: 10.1016/S0272-6386(03)00415-3 [DOI] [PubMed] [Google Scholar]
- 6.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 7.Wu CC, Hsu TW, Chang CM, Yu CH, Lee CC. Age-adjusted Charlson comorbidity index scores as predictor of survival in colorectal cancer patients who underwent surgical resection and chemoradiation. Medicine. 2015;94(2):e431. doi: 10.1097/MD.0000000000000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tian Y, Jian Z, Xu B, Liu H. Age-adjusted Charlson comorbidity index score as predictor of survival of patients with digestive system cancer who have undergone surgical resection. Oncotarget. 2017;8(45):79453–79461. doi: 10.18632/oncotarget.18401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulcahy CF, Mohamed ASR, Kanwar A, et al. Age-adjusted comorbidity and survival in locally advanced laryngeal cancer. Head Neck. 2018;40(9):2060–2069. doi: 10.1002/hed.25200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gimeno-Hernandez J, Iglesias-Moreno MC, Gomez-Serrano M, Carricondo F, Gil-Loyzaga P, Poch-Broto J. The impact of comorbidity on the survival of patients with laryngeal squamous cell carcinoma. Acta Otolaryngol. 2011;131(8):840–846. doi: 10.3109/00016489.2011.564651 [DOI] [PubMed] [Google Scholar]
- 11.Fuller CD, Mohamed AS, Garden AS, et al. Long-term outcomes after multidisciplinary management of T3 laryngeal squamous cell carcinomas: improved functional outcomes and survival with modern therapeutic approaches. Head Neck. 2016;38(12):1739–1751. doi: 10.1002/hed.24532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouellette JR, Small DG, Termuhlen PM. Evaluation of Charlson-age comorbidity index as predictor of morbidity and mortality in patients with colorectal carcinoma. J Gastrointest Surgery. 2004;8(8):1061–1067. doi: 10.1016/j.gassur.2004.09.045 [DOI] [PubMed] [Google Scholar]
- 13.Huguet F, Mukherjee S, Javle M. Locally advanced pancreatic cancer: the role of definitive chemoradiotherapy. Clin Oncol. 2014;26(9):560–568. doi: 10.1016/j.clon.2014.06.002 [DOI] [PubMed] [Google Scholar]
- 14.Morgan JL, Richards P, Zaman O, et al. The decision-making process for senior cancer patients: treatment allocation of older women with operable breast cancer in the UK. Cancer Biol Med. 2015;12(4):308–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bauschke A, Altendorf-Hofmann A, Mothes H, Rauchfuß F, Settmacher U. Partial liver resection results in a significantly better long-term survival than locally ablative procedures even in elderly patients. J Cancer Res Clin Oncol. 2016;142(5):1099–1108. doi: 10.1007/s00432-016-2115-6 [DOI] [PubMed] [Google Scholar]
- 16.Nagata T, Adachi Y, Taniguchi A, et al. [Impact of the age-adjusted Charlson comorbidity index on postoperative complications after gastric cancer surgery]. Gan To Kagaku Ryoho. 2021;48(13):1567–1569. Japanese. [PubMed] [Google Scholar]
- 17.Aoyama T, Yamamoto N, Kamiya M, et al. The age-adjusted Charlson comorbidity index is an independent prognostic factor in pancreatic cancer patients who receive curative resection followed by adjuvant chemotherapy. J Cancer Res Ther. 2020;16(Supplement):S116–S121. doi: 10.4103/jcrt.JCRT_440_18 [DOI] [PubMed] [Google Scholar]
- 18.Chang CM, Yin WY, Wei CK, et al. Adjusted age-adjusted Charlson comorbidity index score as a risk measure of perioperative mortality before cancer surgery. PLoS One. 2016;11(2):e0148076. doi: 10.1371/journal.pone.0148076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girotra M, Hansen A, Farooki A, et al. The current understanding of the endocrine effects from immune checkpoint inhibitors and recommendations for management. JNCI Cancer Spectrum. 2018;2(3):pky021. doi: 10.1093/jncics/pky021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yamana I, Takeno S, Shimaoka H, et al. Geriatric Nutritional Risk Index as a prognostic factor in patients with esophageal squamous cell carcinoma -retrospective cohort study. Int J Surg. 2018;56:44–48. doi: 10.1016/j.ijsu.2018.03.052 [DOI] [PubMed] [Google Scholar]
- 21.Koseki Y, Hikage M, Fujiya K, et al. Utility of a modified age-adjusted Charlson Comorbidity Index in predicting cause-specific survival among patients with gastric cancer. Eur J Surg Oncol. 2021;47(8):2010–2015. doi: 10.1016/j.ejso.2021.01.026 [DOI] [PubMed] [Google Scholar]
- 22.Park JW, Koh DH, Jang WS, et al. Age-adjusted Charlson Comorbidity Index as a prognostic factor for radical prostatectomy outcomes of very high-risk prostate cancer patients. PLoS One. 2018;13(6):e0199365. doi: 10.1371/journal.pone.0199365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim S, Kim DH, Park SY, et al. Association between Charlson comorbidity index and complications of endoscopic resection of gastric neoplasms in elderly patients. BMC Gastroenterol. 2020;20(1):213. doi: 10.1186/s12876-020-01360-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pule L, Buckley E, Niyonsenga T, Banham D, Roder D. Developing a comorbidity index for comparing cancer outcomes in Aboriginal and non-Aboriginal Australians. BMC Health Serv Res. 2018;18(1):776. doi: 10.1186/s12913-018-3603-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jørgensen TL, Hallas J, Friis S, Herrstedt J. Comorbidity in elderly cancer patients in relation to overall and cancer-specific mortality. Br J Cancer. 2012;106(7):1353–1360. doi: 10.1038/bjc.2012.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qu WF, Zhou PY, Liu WR, et al. Age-adjusted Charlson Comorbidity Index predicts survival in intrahepatic cholangiocarcinoma patients after curative resection. Ann Transl Med. 2020;8(7):487. doi: 10.21037/atm.2020.03.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin JX, Huang YQ, Xie JW, et al. Age-adjusted Charlson Comorbidity Index (ACCI) is a significant factor for predicting survival after radical gastrectomy in patients with gastric cancer. BMC Surg. 2019;19(1):53. doi: 10.1186/s12893-019-0513-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JY, Kang HW, Rha KH, et al. Age-adjusted Charlson comorbidity index is a significant prognostic factor for long-term survival of patients with high-risk prostate cancer after radical prostatectomy: a Bayesian model averaging approach. J Cancer Res Clin Oncol. 2016;142(4):849–858. doi: 10.1007/s00432-015-2093-0 [DOI] [PubMed] [Google Scholar]
- 29.Hurria A. We need a geriatric assessment for oncologists. Nat Clin Pract Oncol. 2006;3(12):642–643. doi: 10.1038/ncponc0662 [DOI] [PubMed] [Google Scholar]
- 30.Takahashi M, Takahashi M, Komine K, et al. The G8 screening tool enhances prognostic value to ECOG performance status in elderly cancer patients: a retrospective, single institutional study. PLoS One. 2017;12(6):e0179694. doi: 10.1371/journal.pone.0179694 [DOI] [PMC free article] [PubMed] [Google Scholar]