Abstract
Pulmonary pseudoaneurysms have various causes and typically arise from the main pulmonary artery. Surgical and endovascular options may be considered for treatment. We report the case of a man with a pseudoaneurysm arising from the right pulmonary artery, treated with a septal occlusion device and percutaneous thrombin injection. (Level of Difficulty: Advanced.)
Key Words: catheterization, endovascular repair, pulmonary angiogram, pulmonary artery pseudoaneurysm, thrombin injection
Abbreviations and Acronyms: CT, computed tomography
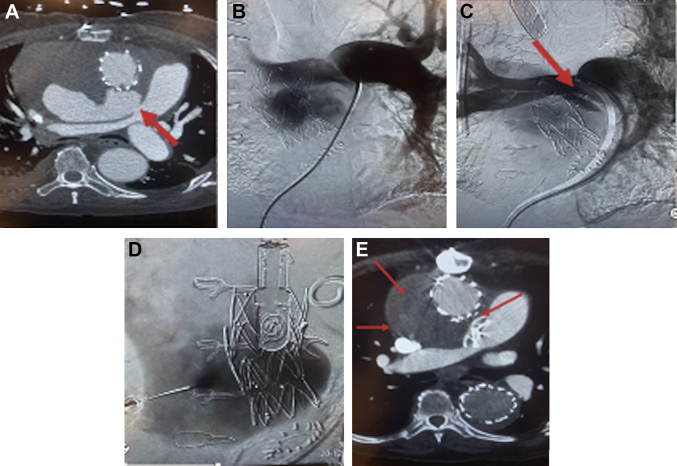
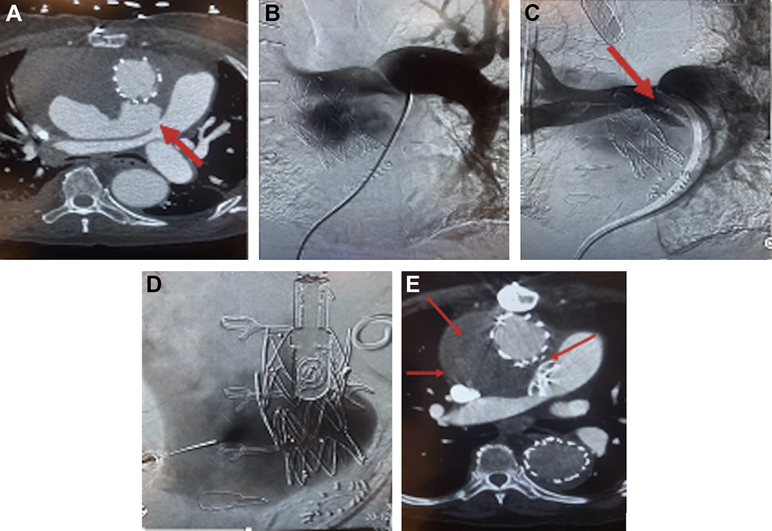
Central Illustration
A pseudoaneurysm of the pulmonary artery is an uncommon complication of pulmonary artery catheterization or aortic surgery. High mortality rates are associated with pseudoaneurysms because of the risk of rapid enlargement and rupture, necessitating prompt intervention.1 A surgical or endovascular approach may be used for successful treatment.2 We report the case of a large mediastinal pseudoaneurysm arising from the proximal right pulmonary artery.
Learning Objectives
-
•
To understand the diagnosis and treatment of pulmonary pseudoaneurysms.
-
•
To understand the role of endovascular therapy in the repair of pulmonary pseudoaneurysms.
History of Presentation
A 78-year-old man was admitted to the hospital with an incidentally noted mediastinal pseudoaneurysm arising from the right pulmonary artery during follow-up surveillance 3 months after surgical repair of an ascending thoracic type A aortic dissection (Figure 1A). Given the patient’s comorbidities and high risk for a repeated sternotomy, the initial endovascular approach at treatment was determined to be the best course of action. The patient’s vital signs on admission were as follows: temperature 99.3 °F, pulse 82 beats/min, oxygen saturation 100%, and blood pressure 123/72 mm Hg from the right arm. Otherwise, the patient’s vital signs and physical examination results were unremarkable. On examination, the patient was cooperative, alert and oriented, well dressed, and well nourished, in no acute distress. Jugular vein pressure was <5 cm. The cardiovascular examination revealed a regular rhythm, without any rubs or gallops, and a 2-3 out of 6 systolic murmur at the left upper sternal border. The patient had full equal carotid pulses, with bilateral carotid bruits. The lungs were clear to auscultation, with no wheezes, rales, or rhonchi, and his breathing was nonlabored. The patient had no abdominal masses or pulsatile masses. The patient had strong 2+ dorsalis pedis and posterior tibialis pulses bilaterally.
Figure 1.
Diagnostic Imaging of Large Mediastinal Pseudoaneurysm Arising From Proximal Right Pulmonary Artery
(A) Contrast-enhanced axial computed tomography scan of the chest demonstrates a large defect (arrow) in the proximal right pulmonary artery leading into a large mediastinal pseudoaneurysm. (B) Pulmonary angiogram through a 6-F pigtail catheter demonstrates contrast material filling the sac through the defect in the proximal right pulmonary artery. (C) Pulmonary angiogram after placement of a septal occluder device (arrow) demonstrates diminished flow in the pseudoaneurysm sac. (D) Fluoroscopic image demonstrates a biopsy needle placed via a transsternal approach opacifying the pseudoaneurysm sac. (E) Follow-up computed tomography angiogram of the chest demonstrates complete occlusion of the pseudoaneurysm sac (arrows). The septal occluder device is also seen.
Medical History
The patient’s medical history was significant for hypertension and hyperlipidemia.
Differential Diagnoses
The differential diagnoses for the patient included mycotic, iatrogenic, autoimmune, and congenital aneurysms.
Investigations
An initial pulmonary arteriogram confirmed a defect in the origin of the right pulmonary artery with a large mediastinal pseudoaneurysm (Figure 1B).
Management
The defect in the origin of the right pulmonary artery, as seen on pulmonary arteriogram (Video 1), was crossed with a catheter and wire, and a 17-mm septal occluder device was placed across the defect (Figure 1C). The septal occluder was sized based on the defect size of the pulmonary artery as measured on the CT angiogram of the chest. The pseudoaneurysm demonstrated significantly reduced flow in the sac on follow-up angiograms after the device was placed (Figure 1D). At a 1-week follow-up examination, a CT angiogram demonstrated decreased but continued filling of the sac with contrast material (Figure 1E). A decision was made to pursue further treatment in an attempt to achieve complete sac thrombosis. Under guidance by intercostal and transsternal ultrasound, transesophageal echocardiogram, and fluoroscopy, the sac was accessed from a transthoracic approach with an 18-gauge Chiba needle. Blood return was achieved, and the residual pseudoaneurysm sac was slowly injected with an overall amount of 1,000 U of thrombin under assistance with real-time color Doppler ultrasound (Video 2).
Discussion
Because of the patient’s past 2 sternotomies, a repeated third sternotomy to surgically repair the pulmonary artery was determined to be high risk. A covered stent graft to the pulmonary artery was also considered; however, the pseudoaneurysm was too close to the main pulmonary artery bifurcation to be able to achieve adequate seal, and it might have compromised flow to the left pulmonary artery. The Amplatzer septal occluder device (Abbott) has been approved for the treatment of atrial septal defects. Given the size of the hole in the pulmonary artery, and the relatively similar thickness of the vessel wall to that of the interatrial septum, a decision was made to treat the defect with a septal occluder device. The flow substantially decreased after placement of the device, and the expectation was that it would thrombose over time. On serial imaging, the flow persisted; therefore, further treatment with percutaneous thrombin injection was pursued, which successfully thrombosed and treated the pseudoaneurysm.
Follow-up
A follow-up CT angiogram demonstrated no further flow in the pseudoaneurysm sac with reduction in the sac size (Figure 1E).
Conclusions
A pseudoaneurysm is described as a collection of blood that leaks outside of the vessel wall confined by the tissues surrounding it.3 A pulmonary pseudoaneurysm can be secondary to various causes, including infections and autoimmune diseases, but it can also rarely occur from an iatrogenic cause, as in the case of our patient, who experienced it after an open ascending thoracic aortic repair for a type A aortic dissection. It is presumed that the pseudoaneurysm was caused either by an intraoperative complication or by a Swan Ganz catheter used to monitor the patient’s intraoperative and postprocedural hemodynamics. These pseudoaneurysms are rare but are often fatal if left untreated, requiring prompt diagnosis and treatment. Presenting symptoms vary depending on pseudoaneurysm size and location, but may include chest pain, dyspnea, and fatal hemoptysis. Life-threatening bleeding usually occurs secondary to rupture.4 The treatment modality is determined on the basis of the cause, the patient’s risk factors, comorbidities, anatomical location, and technical feasibility.5
Some pseudoaneurysms may resolve spontaneously; however, owing to the high risk of rupture, most require either surgical or endovascular definitive treatment.6 We report a novel approach to treat large pseudoaneurysms in a challenging anatomical location.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this article.
Appendix
Pretreatment Angiogram of Proximal Right Pulmonary Artery, Right anterior 30 degree oblique pulmonary digital subtraction angiogram obtained through a 6 French pigtail catheter at 6 frames per second with 20 cc of contrast per second for a total of 30 cc of contrast demonstrates a defect arising from the proximal right pulmonary artery with feeding the large pseudoaneurysm.
Posttreatment Angiogram of Proximal Right Pulmonary Artery, Posttreatment angiogram obtained through a 6-F guide catheter in anterior-posterior projection after placement of the plug demonstrates diminished filling of the pseudoaneurysm sac.
References
- 1.Fukuda Y., Homma T., Uno T., et al. Fatal rupture of pulmonary artery pseudoaneurysm after thoracic radiation therapy against lung squamous cell carcinoma: a case report and literature review. Clin Case Rep. 2020;9:737–741. doi: 10.1002/ccr3.3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elangovan S., Too C.W. Embolisation of large pulmonary artery pseudoaneurysm with conservative treatment of delayed coil extrusion. Singapore Med J. 2020;61:162–164. doi: 10.11622/smedj.2020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumoto H., Izawa D., Nishiyama H., Toki N. A case of progressing pseudoaneurysm formation after intermittent minor leak from an aneurysm. Interdiscip Neurosurg. 2021;25:101192. [Google Scholar]
- 4.Zugazaga A., Stachno M.A., Garcia A., et al. Pulmonary artery pseudoaneurysms: endovascular management after adequate imaging diagnosis. Eur Radiol. 2021;31:6480–6488. doi: 10.1007/s00330-021-07819-8. [DOI] [PubMed] [Google Scholar]
- 5.Khurram R., Karia P., Naidu V., Quddus A., Woo W.L., Davies N. Pulmonary artery pseudoaneurysm secondary to COVID-19 treated with endovascular embolisation. Eur J Radiol Open. 2021;8:100346. doi: 10.1016/j.ejro.2021.100346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta M., Agrawal A., Iakovou A., Cohen S., Shah R., Talwar A. Pulmonary artery aneurysm: a review. Pulm Circ. 2020;10 doi: 10.1177/2045894020908780. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pretreatment Angiogram of Proximal Right Pulmonary Artery, Right anterior 30 degree oblique pulmonary digital subtraction angiogram obtained through a 6 French pigtail catheter at 6 frames per second with 20 cc of contrast per second for a total of 30 cc of contrast demonstrates a defect arising from the proximal right pulmonary artery with feeding the large pseudoaneurysm.
Posttreatment Angiogram of Proximal Right Pulmonary Artery, Posttreatment angiogram obtained through a 6-F guide catheter in anterior-posterior projection after placement of the plug demonstrates diminished filling of the pseudoaneurysm sac.