Abstract
Hypertension is one of the most common causes of preventable death worldwide. The prevalence of pediatric hypertension has increased significantly in recent decades. The cause of this is likely multifactorial, related to increasing childhood obesity, high dietary sodium intake, sedentary lifestyles, perinatal factors, familial aggregation, socioeconomic factors, and ethnic blood pressure (BP) differences. Pediatric hypertension represents a major public health threat. Uncontrolled pediatric hypertension is associated with subclinical cardiovascular disease and adult-onset hypertension. In children with chronic kidney disease (CKD), hypertension is also a strong risk factor for progression to kidney failure. Despite these risks, current rates of pediatric BP screening, hypertension detection, treatment, and control remain suboptimal. Contributing to these shortcomings are the challenges of accurately measuring pediatric BP, limited access to validated pediatric equipment and hypertension specialists, complex interpretation of pediatric BP measurements, problematic normative BP data, and conflicting society guidelines for pediatric hypertension. To date, limited pediatric hypertension research has been conducted to help address these challenges. However, there are several promising signs in the field of pediatric hypertension. There is greater attention being drawn on the cardiovascular risks of pediatric hypertension, more emphasis on the need for childhood BP screening and management, new public health initiatives being implemented, and increasing research interest and funding. This article summarizes what is currently known about pediatric hypertension, the existing knowledge-practice gaps, and ongoing research aimed at improving future kidney and cardiovascular health.
Keywords: blood pressure, cardiovascular health, children, hypertension, kidney disease, pediatric
Hypertension is one of the most common causes of preventable global disease and death.1, 2, 3 Global hypertension prevalence has doubled from 1990 to 2019, but less than half of the patients with hypertension are diagnosed and less than one-quarter are adequately controlled.2 Significant global disparities exist, with lower rates of hypertension diagnosis, treatment, and control in low- and middle-income countries.2,4 There is strong evidence that pediatric hypertension tracks into adulthood and is associated with premature cardiovascular and kidney diseases.5, 6, 7, 8, 9, 10, 11, 12 Therefore, early detection and adequate management of pediatric hypertension should be prioritized.
Hypertension Prevalence
The prevalence of pediatric hypertension has increased in recent decades, contributed partly by rising childhood obesity.13,14 However, rates of pediatric hypertension depend on the definition used, which have changed over time and vary globally (Table 1).5,15,16,17 Without direct evidence linking specific BP thresholds to cardiovascular outcomes, pediatric hypertension is defined using normative distributions. Between 3% and 5% of children and adolescents have hypertension and 10% and 14% have elevated BP levels (“prehypertension”).13,14,18, 19, 20 In a global meta-analysis, the pooled prevalence of hypertension was 4.0% and prehypertension was 9.7%.14 Hypertension prevalence increased from 1.3% (1990–1999) to 6.0% (2010–2014).
Table 1.
Classification of office-based BP in children and adolescents by the American Academy of Pediatrics 2017, European Society of Hypertension 2016, and Hypertension Canada 2020 guidelines
| Guidelines | American Academy of Pediatrics (2017)5 | European Society of Hypertension (2016)15 | Hypertension Canada (2020)16 |
|---|---|---|---|
| BP screening and measurement | - Annual BP measurement in children ≥3 yr of age, or at every visit if risk factors for hypertension - Oscillometric methods can be used for screening, but must be confirmed by auscultatory method - Elevated BP should be confirmed on 3 separate clinic visits - ABPM recommended |
- BP measurement should be performed in children ≥3 yr of age, can repeat every 2 yr if BP normal - Auscultatory method preferred - Elevated BP should be confirmed on 3 separate clinic visits - ABPM recommended |
- BP should be regularly measured in children ≥3 yr of age, no recommendation on screening frequency - Oscillometric methods can be used for screening, but must be confirmed by auscultatory method - Elevated BP should be confirmed on 3 separate clinic visits - ABPM should be considered |
| Hypertension threshold | ≥95th percentile (<13 yr) Or ≥130/80 (≥13 yr) |
≥95th percentile (<16 y) Or ≥140/90 mm Hg (≥16 y) |
≥95th percentile Or >120/80 mm Hg (6–11 yr) Or >130/85 mm Hg (≥12 yr) |
| Target BP (general pediatric population) | <90th percentile (<13 yr) Or <130/80 (≥13 yr) |
<95th percentile recommended <90th percentile should be considered |
<95th percentile <90th percentile (for patients with risk factors or target organ damage) |
| Target BP (pediatric CKD) | 24-h MAP (by ABPM) of <50th percentile | <75th percentile (nonproteinuric CKD) <50th percentile (proteinuric CKD) |
<90th percentile |
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CKD, chronic kidney disease; MAP, mean arterial pressure.
State of Pediatric Hypertension Care
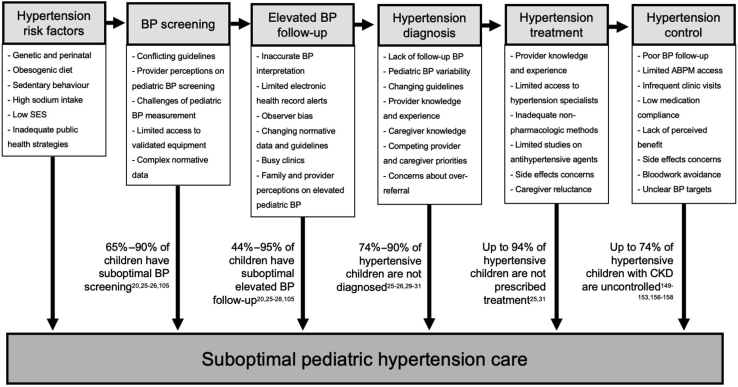
Despite the high prevalence, pediatric hypertension care remains suboptimal (Figure 1). There are conflicting recommendations on pediatric BP screening. Although the most recent guidelines of the American Academy of Pediatrics, European Society of Hypertension, and Hypertension Canada recommend yearly BP screening for healthy children ≥ 3 years old (Table 1),5,15,21 both the United States Preventative Services Taskforce and the United Kingdom National Screening Committee do not recommend screening.22,23 In theory, a good screening test should be safe, inexpensive, widely available, and able to detect preclinical disease with effective treatment.2 All of these characteristics apply to pediatric office-based BP measurement. Pediatric BP screening may also help detect hypertension comorbidities and causes of secondary hypertension. BP screening and follow-up are incomplete. In 2 Canadian studies of 9667 and 378,002 children, respectively, only 15% to 33% of children had annual BP measurement.19,24 Only 5% to 56% of children have appropriate follow-up after elevated BP level measurement.19,24, 25, 26, 27 Less than 25% of children with hypertension are accurately diagnosed, less than half receive lifestyle counseling, and only 6% are prescribed antihypertensive medication.19,25,26,28, 29, 30 Clear challenges and knowledge-practice gaps exist in pediatric hypertension care (Figure 1).
Figure 1.
Barriers and knowledge-practice gaps leading to suboptimal pediatric hypertension care. Estimates are provided for the proportion of children in each of the referenced studies that fit the stated description. These are included to provide approximations of the proportion of children who receive suboptimal care at each stage, including population BP screening, follow-up of elevated BP readings, diagnosis of hypertension, management of hypertension, and adequate BP control. Details of the specific populations included and study methods can be found in the references provided. Aside from the studies of hypertension control in children with CKD, all of the other referenced studies were conducted in the United States (and 1 Canadian study21). There may be significant global practice variation in pediatric hypertension care. Without data from other countries, it is not possible to extrapolate beyond the North American context. We used existing guidelines at the time of study publication to define what proportion of children received “suboptimal care.” These guidelines were the NHLBI fourth report (from 2004 to 2017), the AAP 2017 guidelines (from 2017 to present), and the KDIGO guidelines (for children with CKD).5,17,22 ABPM, ambulatory BP monitoring; AAP, American Academy of Pediatrics; BP, blood pressure; CKD, chronic kidney disease; KDIGO, Kidney Disease Improving Global Outcomes; NHLBI, National Heart Lung and Blood Institute.
Determinants of Pediatric Hypertension
The cause of increasing pediatric hypertension is multifactorial. Primary hypertension accounts for 50% to 90% of cases and is more common in older children and adolescents.31, 32, 33 However, secondary causes should be excluded after hypertension diagnosis, particularly in treatment-resistant and young children (Table 2).
Table 2.
Causes of pediatric hypertension
| Primary (“essential”) hypertension |
|---|
| Risk factors: |
| ▪ Obesity |
| ▪ Sedentary lifestyle |
| ▪ High sodium intake and sodium sensitivity |
| ▪ Low socioeconomic status and food insecurity |
| ▪ Tobacco use |
| ▪ Males |
| ▪ Minority ethnic groups (e.g., Black, Hispanic, and Asian children) |
| ▪ Family history of hypertension |
| ▪ Perinatal factors (e.g., low birthweight, prematurity, maternal BP, and age) |
| Renal disease |
| ▪ Acute kidney injury |
| ▪ Chronic kidney disease |
| ▪ Renal scarring (e.g., previous pyelonephritis, trauma) |
| ▪ Glomerulonephritis |
| ▪ Renal vasculitis |
| ▪ Nephrotic syndrome |
| ▪ Polycystic kidney disease |
| ▪ CAKUT |
| ▪ Hemolytic-uremic syndrome |
| Endocrine disease |
| ▪ Congenital adrenal hyperplasia |
| ▪ Cushing syndrome |
| ▪ Familial hyperaldosteronism |
| ▪ Apparent mineralocorticoid excess |
| ▪ Liddle, Geller, and Gordon syndromes |
| ▪ Hyperthyroidism and hypothyroidism |
| ▪ Hyperparathyroidism |
| ▪ Diabetes mellitus |
| Vascular disease |
| ▪ Aortic coarctation |
| ▪ Renal artery stenosis |
| ▪ Renal vein thrombosis |
| ▪ Midaortic syndrome |
| ▪ Other genetic/syndromic conditions (e.g., neurofibromatosis, tuberous sclerosis, Williams, Turner, Alagille) |
| Oncologic disease |
| ▪ Wilms tumor |
| ▪ Phaeochromocytoma, paraganglioma |
| ▪ Neuroblastoma |
| ▪ Reninoma |
| Neurologic disease |
| ▪ Raised intracranial pressure |
| ▪ Autonomic system dysfunction (e.g., Guillain-Barré syndrome) |
| Medications and toxins |
| ▪ Iatrogenic volume and sodium loading (e.g., excess 0.9% saline administration) |
| ▪ Corticosteroids |
| ▪ Stimulants |
| ▪ Sympathomimetics |
| ▪ Oral contraceptives |
| ▪ Nicotine |
| ▪ Cocaine |
| ▪ Caffeine |
| ▪ Licorice |
| ▪ Heavy metal toxicity (e.g., lead, cadmium, mercury) |
| Other causes |
| ▪ Obstructive sleep apnea |
| ▪ Pain, anxiety |
BP, blood pressure; CAKUT, congenital anomalies of the kidneys and urinary tract.
Genetic and Perinatal Factors
Familial aggregation of hypertension is well known. Genetic factors significantly contribute, as demonstrated by the stronger association between parent/child BP than between spouses34 and lack of BP correlation between parents and adopted children.35,36 Familial and twin studies demonstrate that BP heritability is ∼30% to 50%.37, 38, 39, 40 Genome-wide association studies have identified many BP loci, although each individually accounts for small BP differences (<1 mm Hg).41, 42, 43 Epigenetic and gene-environment interactions are likely significant. Multiple perinatal factors are associated with childhood BP, including low birthweight, prematurity, and maternal factors (i.e., pre-eclampsia, BP, age, and body mass index).44, 45, 46, 47 These factors can impair nephrogenesis, predisposing affected individuals to hypertension and salt sensitivity.48, 49, 50, 51, 52 A systematic review by Rabe et al.53 found some evidence that maternal age, BP, body mass index, and smoking were associated with neonatal BP, although there are insufficient published data. Postnatally, breastfeeding has been consistently associated with lower childhood BP level.53, 54, 55, 56, 57, 58 Lower sodium exposure in breastfed infants is a potential contributor.59
Obesity, Diet, and Physical Activity
Obesity is a major risk factor for pediatric hypertension.60, 61, 62, 63, 64 The risk of hypertension is 2.6× greater in overweight children (body mass index-for-age ≥85th percentile)65 and 9.2× greater in obese children (≥95th percentile).65 Obesity-hypertension begins early in children (<5 years).66, 67, 68 The mechanisms of obesity-hypertension are complex but include impaired sodium handling, sympathetic nervous system overactivation, oxidative stress, hemodynamic changes, and renal/endocrine dysfunction.69 Physical activity is inversely associated with childhood obesity and directly counteracts obesity-hypertension mechanisms.70
Dietary sodium intake is also closely associated with BP.13,71,72 In North American children, daily sodium intake is ∼3000 mg to 3400 mg (approximately 2–3 times the recommended daily intake), and three-quarters of Canadian children exceed upper tolerable limits.73, 74, 75 Approximately 80% of dietary sodium comes from packaged and processed foods.74 Salt sensitivity (i.e., BP rise following sodium intake) is an important mediator.76 Individuals with hypertension, obesity, low birthweight, and African Americans have greater salt sensitivity, which is associated with increased target organ damage, cardiovascular disease, and mortality.77, 78, 79, 80 However, assessing an individual’s salt sensitivity is still clinically impractical. Salt sensitivity testing requires either strict adherence to high and low sodium diets on a prolonged outpatient protocol, or i.v. sodium loading studies, neither of which are practical for most children with hypertension.
Ethnic Differences, Socioeconomic Status, and the Developing World
Significant racial and ethnic BP differences are well characterized in adults.81, 82, 83, 84 Minority ethnic groups are consistently shown to have more hypertension and worse BP control.81, 82, 83,85,86 BP level is also higher among Black, Hispanic, and Asian children.87, 88, 89 Associations are reported between low socioeconomic status, parental income, and education with childhood BP.90, 91, 92, 93, 94 Kelly et al.94 found that socioeconomic status improvement into adulthood significantly decreased BP level. In a meta-analysis by Beltrán et al.,95 food insecurity was significantly associated with hypertension (odds ratio 1.44, 95% CI 1.16–1.79). Ethnic and socioeconomic differences may relate to diet (i.e., access to high-quality foods and salt intake), obesity, prenatal factors, timing of sexual maturity, psychological stress, and health care access.
Although hypertension detection and management have improved significantly in high-income countries, the same is not true in the developing world.2,4 High rates of tobacco use, salt intake, and obesity contribute to high hypertension prevalence, whereas low health literacy and limited health care access are major barriers to adequate hypertension control. These issues may be further exacerbated by rapid urbanization in low- and middle-income countries.4,96, 97, 98
Pediatric Hypertension Outcomes
Although uncontrolled adult hypertension is clearly associated with cardiovascular disease and mortality, there is limited direct evidence for hard cardiovascular outcomes in pediatric hypertension. Demonstrating this association would require a large cohort of children with hypertension, many decades of follow-up, and high participant retention, which is neither financially nor practically feasible. However, there is substantial evidence that pediatric BP tracks into adulthood and that pediatric hypertension increases the risk of subclinical cardiovascular disease (“target organ damage”).5, 6, 7,99
BP Tracking
Children with hypertension and adolescents are more likely to become adults with hypertension, although the correlation is incomplete.9, 10, 11, 12,95,100, 101, 102, 103, 104 Reported correlation coefficients between childhood and adult BP are 0.2 to 0.5 (weak-to-moderate correlation).9,10,12,94,104 However, BP tracking between adolescence and adulthood and among obese individuals is stronger.10, 11, 12 Individuals with persistent hypertension (through childhood and adolescence) have a 7.6× greater odds of adult hypertension.12 Of note, many children with hypertension have BP normalization over time. In 1881 children with hypertension, nearly three-quarters had normal or only elevated BP level in the following 3 years.105 Factors associated with BP normalization include decreased body mass index, increased vegetable intake, decreased alcohol use, and improved socioeconomic status.95
Subclinical Cardiovascular Outcomes
Pediatric hypertension is associated with target organ damage, which in turn is associated with future cardiovascular disease. Children with hypertension have higher left ventricular mass index and left ventricular hypertrophy (LVH).106, 107, 108, 109, 110, 111, 112, 113, 114 Between 5% and 50% of children with hypertension have LVH, and a dose-dependent relationship is shown with increasing BP severity.115,116 Children with hypertension also have increased carotid intima-media thickness,117, 118, 119, 120 higher pulse-wave velocity,121,122 arterial calcification and atherosclerotic changes,123, 124, 125, 126, 127 retinal microvascular disease,128, 129, 130 and microalbuminuria.131,132 In a large cohort of Israeli military recruits (16–19 years old), adolescent hypertension was associated with an increased risk of long-term kidney failure, as defined by dialysis and transplant registries (adjusted hazard ratio 1.98, 95% CI 1.42–2.77), although the absolute risk was low (0.5%).8 In a meta-analysis of 19 studies, Yang et al.6 found that elevated office BP level in children was significantly associated with adult LVH, carotid intima-media thickness, and pulse-wave velocity, as well as cardiovascular events and mortality. In another meta-analysis by Chung et al.,99 children with ambulatory hypertension (defined by ambulatory BP monitoring [ABPM]) had significantly increased carotid intima-media thickness, pulse-wave velocity, left ventricular mass index, and LVH rates. Overall, there is strong evidence that pediatric hypertension is associated with adverse subclinical cardiovascular outcomes. In adults, these subclinical cardiovascular outcomes are consistently associated with an increased risk of cardiovascular events.127,133, 134, 135, 136 However, pediatric data demonstrating a direct association between these subclinical outcomes, mortality, and clinical cardiovascular events are lacking. To further explore these associations, the Study of High Blood Pressure in Pediatrics: Adult Hypertension Onset in Youth study is establishing a multiethnic cohort of adolescents to define optimal BP thresholds and evaluate markers of hypertensive target organ damage.137 Fortunately, antihypertensive treatment is shown to improve LVH in pediatric studies, including patients with CKD.138, 139, 140, 141, 142
Hypertension in Pediatric CKD
Hypertension is strongly associated with CKD progression in children and adults, and BP lowering prevents CKD progression.143, 144, 145, 146, 147, 148 In childhood CKD, hypertension is common (48%–70%),149, 150, 151, 152, 153, 154, 155 and <50% are adequately controlled.149, 150, 151, 152, 153,156, 157, 158 In the Chronic Kidney Disease in Children study, 83% of the participants had ambulatory hypertension (including abnormal BP load) and 35% had masked hypertension.157 The optimal BP target in pediatric CKD has not been established (Table 1). The Kidney Disease: Improving Global Outcomes 2021 guidelines recommend a systolic BP target <120 mm Hg for adults with hypertension and CKD.159 In children, the Kidney Disease: Improving Global Outcomes guidelines recommend targeting a 24-hour mean arterial pressure (MAP) <50th percentile (level 2C; weak recommendation, low-quality evidence). This is supported by the Effect of Strict Blood Pressure Control and ACE Inhibition on the Progression of CKD in Pediatric Patients (ESCAPE) trial (385 participants), which demonstrated lower CKD progression with intensive BP control, particularly in proteinuric kidney disease.144 Recent data from the Chronic Kidney Disease in Children study also found that high MAP (>90th percentile) was associated with CKD progression.149 However, using ABPM-based targets for pediatric hypertension management is impractical and limits global applicability. The 2016 guidelines of the European Society of Hypertension instead recommend an office-based BP target of ≤75th percentile (nonproteinuric CKD) and of ≤50th percentile (proteinuric CKD).15
Challenges in BP Measurement and Interpretation
Standardized, reliable BP measurement is critical to hypertension diagnosis. Unfortunately, pediatric BP measurement is challenging. In North America, pediatric BP screening, elevated BP level follow-up, and hypertension diagnosis are suboptimal (Figure 1). There are minimal data on the extent of pediatric hypertension screening in low- to middle-income countries, where underdiagnosis may be more prevalent.
Office-Based BP Measurement
Office-based BP was traditionally measured using mercury sphygmomanometers. These have been gradually replaced by aneroid sphygmomanometers, although there are limited pediatric validation data, and these require routine calibration. Oscillometric devices are popular, given their ease of use and consistency. They overcome observer bias and prevent terminal digit preference (i.e., rounding measurements to certain digits). However, oscillometric devices estimate systolic and diastolic BP levels using proprietary formulas by measuring MAP and pulse pressure. Significant differences may exist between oscillometric devices, and they tend to overestimate pediatric BP level by 3 to 10 mm Hg.160, 161, 162 Normative BP data are typically derived by auscultatory methods, so abnormal oscillometric BP should be confirmed by auscultation.5,15,16 Repeated or averaged BP measurements are also more reliable, because BP level can decrease during a single visit.163,164 Newer automated devices can repeat BP measurements in clinic without an observer present and have been shown to reduce white coat phenomenon in adults.165 Elevated BP level should be confirmed on 3 separate visits to diagnose hypertension.88,106 Interpretation of pediatric BP is also challenging; with large reference tables, changing normative data, and conflicting definitions of pediatric hypertension. The development of accessible tools, including simple BP screening tables and mobile applications (e.g., PedBP), has simplified diagnosis.5 Although convenient, office-based BP provides only a snapshot of a patient’s BP. In the Study of High Blood Pressure in Pediatrics: Adult Hypertension Onset in Youth, office-based BP level ≥85th percentile was most predictive of ambulatory hypertension and may be considered as a threshold for ABPM.166
Home and ABPM
Ambulatory BP is more reproducible and better associated with target organ damage than office-based BP.167, 168, 169 There are limited pediatric data on home BP monitoring (HBPM),170 although it is commonly used (>70% of surveyed German pediatric nephrologists171) and has gained popularity during the COVID-19 pandemic.172 HBPM provides a more longitudinal BP assessment than either office-based BP or ABPM, is cost-effective, and is well tolerated.173,174 Although not recommended for pediatric hypertension diagnosis, HBPM can help detect white coat or masked hypertension. HBPM is also useful for BP monitoring in patients with hypertension, especially when strict BP control is desired.5,15 However, there can be reporting bias, the optimal timing of measurements is unknown, and validated pediatric devices and cuff sizes are lacking.15 HBPM should be supported by adequate caregiver training and device calibration with office-based auscultatory BP. Telemedicine strategies for hypertension management, including BP telemonitoring, have been shown to be feasible and associated with improved BP control in adults with hypertension.175 However, there are minimal data on the use of BP telemonitoring in children. Incorporation of these strategies could improve access to pediatric hypertension care, may promote disease self-management, and enhance lifestyle modification. However, these potential benefits are balanced against limited access to validated pediatric home BP devices, a lack of standardized protocols for HBPM, few pediatric telemedicine services, regulatory and privacy issues, and provider reimbursement considerations.175 Further research on the clinical application of HBPM in children is needed to facilitate BP telemonitoring programs.170
ABPM is the gold standard for adults and is recommended by the European Society of Hypertension and the American Academy of Pediatrics for children (>5 years).5,15 ABPM is well correlated with target organ damage167, 168, 169 and is reliable in pediatric CKD.144 It can detect nocturnal and masked hypertension, which are both more common in CKD.158,159 An “ABPM-first” approach for pediatric hypertension referrals (i.e., performing ABPM in all new referrals to confirm hypertension before consultation and to avoid unnecessary expensive secondary hypertension workups) is a potential cost-saving strategy.176 However, there are limitations to widespread pediatric ABPM utilization. There are few validated pediatric devices, costs are prohibitive, and global access is limited. Existing ABPM normative data are also problematic. Current normative data were derived from a relatively small Caucasian German population.177,178 There are minimal data for children <120 cm in height, and concerns exist regarding low diastolic BP variation in this cohort. BP varies by ethnicity and geographic region. Xi et al.179 attempted to create international normative BP data from 52,636 children in 7 countries using office-based BP methods. Median systolic/diastolic BP levels varied up to 10 mm Hg between countries, with India and Poland having the highest BP level. Based on these differences in BP by ethnicity, existing ABPM normative data may not be applicable to non-Caucasian children. Yip et al.180 developed ABPM normative data for East Asian children in Hong Kong, and BP values were 5 to 6 mm Hg higher than those in Caucasian children. There are ongoing efforts to develop validated normative data sets in other ethnicities, including South Asian children in Canada in the Ambulatory blood pressure monitoring for SoutH Asian children study.181
Another limitation is the existing pediatric ABPM classification. In adults, ambulatory hypertension is defined by simple thresholds (i.e., mean wake BP > 130/80 mm Hg, sleep BP > 110/65, or 24-hour BP > 125/75), that predict cardiovascular events.182,183 In the pediatric American Heart Association guidelines, ambulatory hypertension is categorized by mean BP and BP load.169 However, up to 20% to 40% of children are unclassified using these criteria and hypertension thresholds may be higher than adult thresholds for children ≥12 years old.184, 185, 186 There is emerging evidence that isolated elevated BP load is not significantly associated with target organ damage.185,187,188 Removing BP load criteria and using adult thresholds for adolescents would simplify ABPM interpretation.186,188 Because oscillometric ABPM devices measure MAP, it may also be preferable to classify ABPM using MAP, instead of calculated systolic/diastolic BP.
Pediatric Hypertension Management
Optimal pediatric BP thresholds are unknown (Table 1), but the goal is to reduce BP to a level that minimizes cardiovascular and kidney disease risks. In adults with hypertension, the Systolic Blood Pressure Intervention Trial demonstrated that intensive BP control (systolic BP target <120 mm Hg) was associated with a significantly lower risk of cardiovascular outcomes,189 which has led to the incorporation of lower BP targets in recent adult hypertension guidelines.182,190 Strategies to improve pediatric hypertension typically address the individual level. However, pediatric hypertension is a growing pandemic, and effective population-based interventions are essential to address the global disease burden (Figure 2). Improving awareness of pediatric hypertension among primary care physicians, community organizations, and families may increase detection, provide earlier treatment opportunities, and mitigate adverse consequences.
Figure 2.
Strategies to improve global pediatric hypertension care. ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
Population-Based Strategies
Population-based sodium reduction strategies are highly cost-effective.191 In Finland and the United Kingdom, public health campaigns, food industry regulations, and product labeling have successfully decreased population sodium intake by 15% to 40%.192 Public health strategies should also address childhood obesity and sedentary lifestyles, including awareness campaigns, creating safe spaces for physical activity, integrating exercise into schools and communities, and improving access to high-quality nutrition (e.g., through food taxes, subsidies, and school-based programs).4 In 2013, the World Health Organization created a Global Action Plan for the control of noncommunicable diseases and described a series of “best buy” interventions, considered to be the most cost effective and feasible. These include reducing tobacco and alcohol use, reducing salt and transfat intake, and public health physical activity campaigns.193 In rural South Asia, the COBRA-BPS trial found that a multicomponent community hypertension intervention (including community health education, BP monitoring, provider training in hypertension management, designated hypertension clinics, and additional funding) significantly improved hypertension control and was cost effective.194,195 Strategies to improve pregnancy outcomes, early childhood education, and nutrition are also critical. The Carolina Abecedarian Project found that an early childhood education and nutrition program significantly decreased adult hypertension.196
Nonpharmacologic Management
Effective nonpharmacologic strategies for pediatric BP lowering include weight loss (for overweight children), regular physical activity, reduced sodium intake, the Dietary Approaches to Stop Hypertension diet, and smoking/alcohol avoidance (Figure 2). There is strong evidence in both adults and children that dietary sodium reduction is associated with improved BP control, in a dose-dependent relationship.197, 198, 199 In 2 pediatric meta-analyses (966 and 58,531 patients respectively), reduced dietary sodium intake was associated with small, but significant BP reductions (∼1 mm Hg).199,200 The association between BP and sodium intake was stronger in overweight children and children with low potassium intake.199 Achieving sustainable sodium reductions is challenging, given the sodium content in processed foods.75 Although optimal sodium reduction targets for children are uncertain, the National Academic of Sciences, Engineering and Medicine have recommended Chronic Disease Risk Reduction Intake limits, based on extrapolated adult data (1–3 years: <1200 mg/d; 4–8 years: <1500 mg/d; 9–13 years: <1800 mg/d; 14–18 years: <2300 mg/d).76 A practical approach for sodium reduction is to recommend a no added salt diet, a reduction of high-salt, processed foods, and to provide education to families regarding food label interpretation. Self-reported sodium intake is also inaccurate.201 Urine sodium excretion is more reliable, and novel formulas to estimate sodium excretion from spot urine samples are available.201, 202, 203 Higher sodium excretion is associated with major cardiovascular events.204
The Dietary Approaches to Stop Hypertension diet was designed in the 1990s as an optimal BP-lowering diet for adults.205 The Dietary Approaches to Stop Hypertension diet promotes consumption of vegetables, fruit, lean meat, and dairy, and reduces intake of sodium, saturated fat, added sugars, and highly processed foods. The Dietary Approaches to Stop Hypertension diet has also been shown to improve BP in children and adolescents, although there are limited published data.206,207 Regular physical activity has also been shown to reduce BP in children and adolescents with hypertension.208, 209, 210 However, the results of published studies are inconsistent and the effect size is generally small. Physical activity interventions appear to be more effective when combined with diet or weight loss programs.209
Pharmacologic Management
Nonpharmacologic interventions should be optimized before antihypertensive treatment. Antihypertensive medications should be selected based on underlying hypertension pathophysiology, anticipated efficacy, side effects, available formulations, and associated costs.5 Long-acting medications and simplified dosing schedules can improve compliance. Few pediatric trials compare antihypertensive medications. A systematic review by Simonetti et al.211 found that angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and calcium channel blockers had similar antihypertensive efficacy. A 2014 Cochrane review found that angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and beta-blockers each significantly reduced BP versus placebo, whereas calcium channel blockers did not.212 A subsequent network meta-analysis by Burrello et al.213 found similar BP reductions across antihypertensive classes, but only renin-angiotensin-aldosterone system inhibitors significantly reduced BP versus placebo. Generally, renin-angiotensin-aldosterone system inhibitors are considered first-line pediatric antihypertensives, particularly in CKD.144 Calcium channel blockers are considered for sexually active adolescent females or if laboratory surveillance (for renin-angiotensin-aldosterone system inhibitors) is poorly tolerated.5,15,16 Samuel et al.214 described a novel antihypertensive selection approach, by conducting serial n-of-1 trials in 42 children with ABPM, identifying each patient’s “preferred” medication (49% lisinopril, 24% amlodipine, and 12% hydrochlorothiazide).
Future Directions and Knowledge Gaps
Despite significant advances in pediatric hypertension research, knowledge gaps persist. It is unclear what BP thresholds are associated with cardiovascular outcomes and should be targeted. We must determine the optimal intermediate markers (e.g., LVH) for predicting cardiovascular events. Because BP tracking and target organ damage are incomplete, we must identify relevant predictive factors. We should also evaluate the effect of hypertension duration on cardiovascular outcomes. It remains unclear if transient hypertension (i.e., during childhood chemotherapy) has long-term risks and warrants treatment. The optimal role and timing of HBPM and ABPM are unclear, and progress is needed to validate and improve access to pediatric devices. Additional ABPM normative data sets are needed, in diverse ethnic populations. Finally, further trials are needed to evaluate various antihypertensive medications, particularly among specific populations (e.g., obesity, nonproteinuric CKD, and congenital heart disease). Fortunately, ongoing research will help answer some of these questions, including the Study of High Blood Pressure in Pediatrics: Adult Hypertension Onset in Youth study,138 further Chronic Kidney Disease in Children analyses (https://statepi.jhsph.edu/ckid), the Ambulatory blood pressure monitoring for SoutH Asian children study, the Pediatric Hypertension Registry, prospective longitudinal cohorts including the Young Finns study (https://youngfinnsstudy.utu.fi), and novel intervention trials (e.g., pharmacist- or youth-led programs, n-of-1 medication trials, and clinical decision support tools).
Disclosure
All the authors declared no competing interests.
Acknowledments
The authors thank Dr. Sujane Kandasamy for her assistance in preparing the manuscript figures and infographics.
References
- 1.Danaei G., Ding E.L., Mozaffarian D., et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou B., Perel P., Mensah G.A., Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802. doi: 10.1038/s41569-021-00559-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forouzanfar M.H., Liu P., Roth G.A., et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990-2015. JAMA. 2017;317:165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 4.Schutte A.E., Srinivasapura Venkateshmurthy N., Mohan S., Prabhakaran D. Hypertension in low- and middle-income countries. Circ Res. 2021;128:808–826. doi: 10.1161/CIRCRESAHA.120.318729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flynn J.T., Kaelber D.C., Baker-Smith C.M., et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140 doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 6.Yang L., Magnussen C.G., Yang L., Bovet P., Xi B. Elevated blood pressure in childhood or adolescence and cardiovascular outcomes in adulthood: a systematic review. Hypertension. 2020;75 doi: 10.1161/HYPERTENSIONAHA.119.14168. 2020:948-955. [DOI] [PubMed] [Google Scholar]
- 7.Thompson M., Dana T., Bougatsos C., Blazina I., Norris S.L. Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics. 2013;131:490–525. doi: 10.1542/peds.2012-3523. [DOI] [PubMed] [Google Scholar]
- 8.Leiba A., Fishman B., Twig G., et al. Association of adolescent hypertension with future end-stage renal disease. JAMA Intern Med. 2019;179:517–523. doi: 10.1001/jamainternmed.2018.7632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Juhola J., Magnussen C.G., Viikari J.S.A., et al. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: the Cardiovascular Risk in Young Finns Study. J Pediatr. 2011;159:584–590. doi: 10.1016/j.jpeds.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Chen X., Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Theodore R.F., Broadbent J., Nagin D., et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66:1108–1115. doi: 10.1161/HYPERTENSIONAHA.115.05831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Urbina E.M., Khoury P.R., Bazzano L., et al. Relation of blood pressure in childhood to self-reported hypertension in adulthood: the international childhood cardiovascular cohort consortium. Hypertension. 2019;73:1224–1230. doi: 10.1161/HYPERTENSIONAHA.118.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosner B., Cook N.R., Daniels S., Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension. 2013;62:247–254. doi: 10.1161/HYPERTENSIONAHA.111.00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song P., Zhang Y., Yu J., et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. 2019;173:1154–1163. doi: 10.1001/jamapediatrics.2019.3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lurbe E., Agabiti-Rosei E., Cruickshank J.K., et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–1920. doi: 10.1097/HJH.0000000000001039. [DOI] [PubMed] [Google Scholar]
- 16.National High Blood Pressure Education Program working group on high blood pressure in children and adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(suppl):555–576. [PubMed] [Google Scholar]
- 17.Dionne J.M., Harris K.C., Benoit G., et al. Hypertension Canada’s 2017 guidelines for the diagnosis, assessment, prevention, and treatment of pediatric hypertension. Can J Cardiol. 2017;33:577–585. doi: 10.1016/j.cjca.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 18.Koebnick C., Black M.H., Wu J., et al. The prevalence of primary pediatric prehypertension and hypertension in a real-world managed care system. J Clin Hypertens (Greenwich) 2013;15:784–792. doi: 10.1111/jch.12173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Moraes A.C.F., Lacerda M.B., Moreno L.A., Horta B.L., Carvalho H.B. Prevalence of high blood pressure in 122,053 adolescents: a systematic review and meta-regression. Medicine (Baltimore) 2014;93:e232. doi: 10.1097/MD.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aliarzadeh B., Meaney C., Moineddin R., et al. Hypertension screening and follow-up in children and adolescents in a Canadian primary care population sample: a retrospective cohort study. CMAJ Open. 2016;4:E230–E235. doi: 10.9778/cmajo.20150016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rabi D.M., McBrien K.A., Sapir-Pichhadze R., et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol. 2020;36:596–624. doi: 10.1016/j.cjca.2020.02.086. [DOI] [PubMed] [Google Scholar]
- 22.US Preventive Services Task Force. Krist A.H., Davidson K.W., et al. Screening for high blood pressure in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2020;324:1878–1883. doi: 10.1001/jama.2020.20122. [DOI] [PubMed] [Google Scholar]
- 23.UK National Screening Committee Screening to prevent adverse outcom4es from primary hypertension in children and young people. UK National Screening Committee. https://view-health-screening-recommendations.service.gov.uk/document/384/download Published 2018.
- 24.Herman C. What Makes a Screening Exam “good”? AMA J Ethics. 2006;8:34–37. doi: 10.1001/virtualmentor.2006.8.1.cprl1-0601. [DOI] [PubMed] [Google Scholar]
- 25.Ding L, Singer A, Kosowan L, Dart A. Pediatric hypertension screening and recognition in primary care clinics in Canada. Paediatr Child Health. Published online October 11, 2021. https://doi.org/10.1093/pch/pxab081 [DOI] [PMC free article] [PubMed]
- 26.Shapiro D.J., Hersh A.L., Cabana M.D., et al. Hypertension screening during ambulatory pediatric visits in the United States, 2000-2009. Pediatrics. 2012;130:604–610. doi: 10.1542/peds.2011-3888. [DOI] [PubMed] [Google Scholar]
- 27.Rea C.J., Brady T.M., Bundy D.G., et al. Pediatrician adherence to guidelines for diagnosis and management of high blood pressure. J Pediatr. 2022;242:12–17e1. doi: 10.1016/j.jpeds.2021.11.008. [DOI] [PubMed] [Google Scholar]
- 28.Daley M.F., Sinaiko A.R., Reifler L.M., et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics. 2013;132:e349–e355. doi: 10.1542/peds.2012-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansen M.L., Gunn P.W., Kaelber D.C. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–879. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 30.Brady T.M., Neu A.M., Miller E.R., Appel L.J., Siberry G.K., Solomon B.S. Real-time electronic medical record alerts increase high blood pressure recognition in children. Clin Pediatr (Phila) 2015;54:667–675. doi: 10.1177/0009922814559379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaelber D.C., Liu W., Ross M., et al. Diagnosis and medication treatment of pediatric hypertension: a retrospective cohort study. Pediatrics. 2016;138 doi: 10.1542/peds.2016-2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dionne J.M. Evidence gaps in the identification and treatment of hypertension in children. Can J Cardiol. 2020;36:1384–1393. doi: 10.1016/j.cjca.2020.02.076. [DOI] [PubMed] [Google Scholar]
- 33.Robinson R.F., Batisky D.L., Hayes J.R., Nahata M.C., Mahan J.D. Body mass index in primary and secondary pediatric hypertension. Pediatr Nephrol. 2004;19:1379–1384. doi: 10.1007/s00467-004-1588-8. [DOI] [PubMed] [Google Scholar]
- 34.Silverstein D.M., Champoux E., Aviles D.H., Vehaskari V.M. Treatment of primary and secondary hypertension in children. Pediatr Nephrol. 2006;21:820–827. doi: 10.1007/s00467-006-0087-5. [DOI] [PubMed] [Google Scholar]
- 35.Havlik R.J., Feinleib M. Epidemiology and genetics of hypertension. Hypertension. 1982;4:III121–III127. doi: 10.1161/01.hyp.4.5_pt_2.iii121. [DOI] [PubMed] [Google Scholar]
- 36.Biron P., Mongeau J.G., Bertrand D. Familial aggregation of blood pressure in 558 adopted children. Can Med Assoc J. 1976;115:773–774. [PMC free article] [PubMed] [Google Scholar]
- 37.Annest J.L., Sing C.F., Biron P., Mongeau J.G. Familial aggregation of blood pressure and weight in adoptive families. II. Estimation of the relative contributions of genetic and common environmental factors to blood pressure correlations between family members. Am J Epidemiol. 1983;117:492–506. doi: 10.1093/oxfordjournals.aje.a113567. [DOI] [PubMed] [Google Scholar]
- 38.Snieder H., Hayward C.S., Perks U., Kelly R.P., Kelly P.J., Spector T.D. Heritability of central systolic pressure augmentation: a twin study. Hypertension. 2000;35:574–579. doi: 10.1161/01.hyp.35.2.574. [DOI] [PubMed] [Google Scholar]
- 39.Levy D., Larson M.G., Benjamin E.J., et al. Framingham Heart Study 100K Project: genome-wide associations for blood pressure and arterial stiffness. BMC Med Genet. 2007;8(suppl 1):S3. doi: 10.1186/1471-2350-8-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miall W.E., Oldham P.D. The hereditary factor in arterial blood-pressure. Br Med J. 1963;1:75–80. doi: 10.1136/bmj.1.5323.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu X., Ding X., Zhang X., et al. Genetic and environmental influences on blood pressure variability: a study in twins. J Hypertens. 2013;31:690–697. doi: 10.1097/HJH.0b013e32835e2a4a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giri A., Hellwege J.N., Keaton J.M., et al. Trans-ethnic association study of blood pressure determinants in over 750,000 individuals. Nat Genet. 2019;51:51–62. doi: 10.1038/s41588-018-0303-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Evangelou E., Warren H.R., Mosen-Ansorena D., et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50:1412–1425. doi: 10.1038/s41588-018-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhu X., Feng T., Tayo B.O., et al. Meta-analysis of correlated traits via summary statistics from GWASs with an application in hypertension. Am J Hum Genet. 2015;96:21–36. doi: 10.1016/j.ajhg.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davis E.F., Lazdam M., Lewandowski A.J., et al. Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: a systematic review. Pediatrics. 2012;129:e1552–e1561. doi: 10.1542/peds.2011-3093. [DOI] [PubMed] [Google Scholar]
- 46.Law C.M., Shiell A.W. Is blood pressure inversely related to birth weight? The strength of evidence from a systematic review of the literature. J Hypertens. 1996;14:935–941. [PubMed] [Google Scholar]
- 47.Huxley R.R., Shiell A.W., Law C.M. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens. 2000;18:815–831. doi: 10.1097/00004872-200018070-00002. [DOI] [PubMed] [Google Scholar]
- 48.Leon D.A., Koupilova I., Lithell H.O., et al. Failure to realise growth potential in utero and adult obesity in relation to blood pressure in 50 year old Swedish men. BMJ. 1996;312:401–406. doi: 10.1136/bmj.312.7028.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Keller G., Zimmer G., Mall G., Ritz E., Amann K. Nephron number in patients with primary hypertension. N Engl J Med. 2003;348:101–108. doi: 10.1056/NEJMoa020549. [DOI] [PubMed] [Google Scholar]
- 50.Bertram J.F., Douglas-Denton R.N., Diouf B., Hughson M.D., Hoy W.E. Human nephron number: implications for health and disease. Pediatr Nephrol. 2011;26:1529–1533. doi: 10.1007/s00467-011-1843-8. [DOI] [PubMed] [Google Scholar]
- 51.Simonetti G.D., Raio L., Surbek D., Nelle M., Frey F.J., Mohaupt M.G. Salt sensitivity of children with low birth weight. Hypertension. 2008;52:625–630. doi: 10.1161/HYPERTENSIONAHA.108.114983. [DOI] [PubMed] [Google Scholar]
- 52.Ruys C.A., Rotteveel J., van de Lagemaat M., Lafeber H.N., Finken M.J.J. Salt sensitivity of blood pressure at age 8 years in children born preterm. J Hum Hypertens. 2018;32:367–376. doi: 10.1038/s41371-018-0045-2. [DOI] [PubMed] [Google Scholar]
- 53.Rabe H., Bhatt-Mehta V., Bremner S.A., et al. Antenatal and perinatal factors influencing neonatal blood pressure: a systematic review. J Perinatol. 2021;41:2317–2329. doi: 10.1038/s41372-021-01169-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martin R.M., Ness A.R., Gunnell D., Emmett P., Davey Smith G. Does breast-feeding in infancy lower blood pressure in childhood? The Avon longitudinal study of parents and children (ALSPAC) Circulation. 2004;109:1259–1266. doi: 10.1161/01.cir.0000118468.76447.ce. [DOI] [PubMed] [Google Scholar]
- 55.Lawlor D.A., Najman J.M., Sterne J., Williams G.M., Ebrahim S., Davey Smith G. Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes. Circulation. 2004;110:2417–2423. doi: 10.1161/01.CIR.0000145165.80130.B5. [DOI] [PubMed] [Google Scholar]
- 56.Miliku K., Moraes T.J., Becker A.B., et al. Breastfeeding in the first days of life is associated with lower blood pressure at 3 years of age. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.019067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Amorim R de, Coelho A.F., de Lira P.I., Lima Mde C. Is breastfeeding protective for blood pressure in schoolchildren? A cohort study in northeast Brazil. Breastfeed Med. 2014;9:149–156. doi: 10.1089/bfm.2013.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hosaka M., Asayama K., Staessen J.A., et al. Breastfeeding leads to lower blood pressure in 7-year-old Japanese children: Tohoku Study of Child Development. Hypertens Res. 2013;36:117–122. doi: 10.1038/hr.2012.128. [DOI] [PubMed] [Google Scholar]
- 59.Horta B.L., Loret de Mola C., Victora C.G. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:30–37. doi: 10.1111/apa.13133. [DOI] [PubMed] [Google Scholar]
- 60.Geleijnse J.M., Hofman A., Witteman J.C., Hazebroek A.A., Valkenburg H.A., Grobbe D.E. Long-term effects of neonatal sodium restriction on blood pressure. Hypertension. 1997;29:913–917. doi: 10.1161/01.hyp.29.4.913. [DOI] [PubMed] [Google Scholar]
- 61.McNiece K.L., Poffenbarger T.S., Turner J.L., Franco K.D., Sorof J.M., Portman R.J. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640–644.e1. doi: 10.1016/j.jpeds.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 62.Tu W., Eckert G.J., DiMeglio L.A., Yu Z., Jung J., Pratt J.H. Intensified effect of adiposity on blood pressure in overweight and obese children. Hypertension. 2011;58:818–824. doi: 10.1161/HYPERTENSIONAHA.111.175695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jago R., Harrell J.S., McMurray R.G., Edelstein S., El Ghormli, Bassin S. Prevalence of abnormal lipid and blood pressure values among an ethnically diverse population of eighth-grade adolescents and screening implications. Pediatrics. 2006;117:2065–2073. doi: 10.1542/peds.2005-1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wirix A.J., Nauta J., Groothoff J.W., et al. Is the prevalence of hypertension in overweight children overestimated? Arch Dis Child. 2016;101:998–1003. doi: 10.1136/archdischild-2015-309969. [DOI] [PubMed] [Google Scholar]
- 65.Dasgupta K., O’Loughlin J., Chen S., et al. Emergence of sex differences in prevalence of high systolic blood pressure: analysis of a longitudinal adolescent cohort. Circulation. 2006;114:2663–2670. doi: 10.1161/CIRCULATIONAHA.106.624536. [DOI] [PubMed] [Google Scholar]
- 66.Redwine K.M., Acosta A.A., Poffenbarger T., Portman R.J., Samuels J. Development of hypertension in adolescents with pre-hypertension. J Pediatr. 2012;160:98–103. doi: 10.1016/j.jpeds.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 67.Falkner B., Gidding S.S., Ramirez-Garnica G., Wiltrout S.A., West D., Rappaport E.B. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr. 2006;148:195–200. doi: 10.1016/j.jpeds.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 68.Belfort M.B., Rifas-Shiman S.L., Rich-Edwards J., Kleinman K.P., Gillman M.W. Size at birth, infant growth, and blood pressure at three years of age. J Pediatr. 2007;151:670–674. doi: 10.1016/j.jpeds.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vale S., Trost S.G., Rêgo C., Abreu S., Mota J. Physical activity, obesity status, and blood pressure in preschool children. J Pediatr. 2015;167:98–102. doi: 10.1016/j.jpeds.2015.04.031. [DOI] [PubMed] [Google Scholar]
- 70.Susic D., Varagic J. Obesity: a perspective from hypertension. Med Clin North Am. 2017;101:139–157. doi: 10.1016/j.mcna.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 71.Strambi M., Giussani M., Ambruzzi M.A., et al. Novelty in hypertension in children and adolescents: focus on hypertension during the first year of life, use and interpretation of ambulatory blood pressure monitoring, role of physical activity in prevention and treatment, simple carbohydrates and uric acid as risk factors. Ital J Pediatr. 2016;42:69. doi: 10.1186/s13052-016-0277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.He F.J., Marrero N.M., Macgregor G.A. Salt and blood pressure in children and adolescents. J Hum Hypertens. 2008;22:4–11. doi: 10.1038/sj.jhh.1002268. [DOI] [PubMed] [Google Scholar]
- 73.Yang Q., Zhang Z., Kuklina E.V., et al. Sodium intake and blood pressure among US children and adolescents. Pediatrics. 2012;130:611–619. doi: 10.1542/peds.2011-3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gowrishankar M., Blair B., Rieder M.J. Dietary intake of sodium by children: why it matters. Paediatr Child Health. 2020;25:47–61. doi: 10.1093/pch/pxz153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Food and Nutrition Board . In: Dietary Reference Intakes for Sodium and Potassium. Oria M., Harrison M., Stallings V.A., editors. National Academies Press (US); 2019. Committee to review the dietary reference intakes for sodium and potassium. [PubMed] [Google Scholar]
- 76.Balafa O., Kalaitzidis R.G. Salt sensitivity and hypertension. J Hum Hypertens. 2021;35:184–192. doi: 10.1038/s41371-020-00407-1. [DOI] [PubMed] [Google Scholar]
- 77.Weinberger M.H., Fineberg N.S., Fineberg S.E., Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001;37:429–432. doi: 10.1161/01.hyp.37.2.429. [DOI] [PubMed] [Google Scholar]
- 78.Mu J., Zheng S., Lian Q., Liu F., Liu Z. Evolution of blood pressure from adolescents to youth in salt sensitivies: a 18-year follow-up study in Hanzhong children cohort. Nutr J. 2012;11:70. doi: 10.1186/1475-2891-11-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bihorac A., Tezcan H., Ozener C., Oktay A., Akoglu E. Association between salt sensitivity and target organ damage in essential hypertension. Am J Hypertens. 2000;13:864–872. doi: 10.1016/s0895-7061(00)00253-3. [DOI] [PubMed] [Google Scholar]
- 80.Sanders P.W. Dietary salt intake, salt sensitivity, and cardiovascular health. Hypertension. 2009;53:442–445. doi: 10.1161/HYPERTENSIONAHA.108.120303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ong K.L., Cheung B.M., Man Y.B., Lau C.P., Lam K.S. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 82.Wright J.D., Hughes J.P., Ostchega Y., Yoon S.S., Nwankwo T. Mean systolic and diastolic blood pressure in adults aged 18 and over in the United States, 2001–2008. Natl Health Stat Report. 2011;(35):1–24. [PubMed] [Google Scholar]
- 83.Lackland D.T. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014;348:135–138. doi: 10.1097/MAJ.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gasevic D., Ross E.S., Lear S.A. Ethnic differences in cardiovascular disease risk factors: a systematic review of North American evidence. Can J Cardiol. 2015;31:1169–1179. doi: 10.1016/j.cjca.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 85.Fei K., Rodriguez-Lopez J.S., Ramos M., et al. Racial and ethnic subgroup disparities in hypertension prevalence, New York City health and nutrition examination survey, 2013–2014. Prev Chronic Dis. 2017;14:E33. doi: 10.5888/pcd14.160478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gillespie C.D., Hurvitz K.A., Centers for Disease Control and Prevention (CDC) Prevalence of hypertension and controlled hypertension - United States, 2007-2010. MMWR Suppl. 2013;62:144–148. [PubMed] [Google Scholar]
- 87.Cheung E.L., Bell C.S., Samuel J.P., Poffenbarger T., Redwine K.M., Samuels K.M., Samuels J.A. Race and obesity in adolescent hypertension. Pediatrics. 2017;139 doi: 10.1542/peds.2016-1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rosner B., Cook N., Portman R., Daniels S., Falkner B. Blood pressure differences by ethnic group among United States children and adolescents. Hypertension. 2009;54:502–508. doi: 10.1161/HYPERTENSIONAHA.109.134049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lo J.C., Sinaiko A., Chandra M., et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131:e415–e424. doi: 10.1542/peds.2012-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kaczmarek M., Stawińska-Witoszyńska B., Krzyżaniak A., et al. Who is at higher risk of hypertension? Socioeconomic status differences in blood pressure among Polish adolescents: a population-based ADOPOLNOR study. Eur J Pediatr. 2015;174:1461–1473. doi: 10.1007/s00431-015-2554-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fallah Z., Kelishadi R., Heshmat R., et al. A nationwide report on blood pressure of children and adolescents according to socioeconomic status: the CASPIAN-IV study. J Res Med Sci. 2015;20:646–655. doi: 10.4103/1735-1995.166210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.van den Berg G., van Eijsden M., Galindo-Garre F., et al. Explaining socioeconomic inequalities in childhood blood pressure and prehypertension: the ABCD study. Hypertension. 2013;61:35–41. doi: 10.1161/HYPERTENSIONAHA.111.00106. [DOI] [PubMed] [Google Scholar]
- 93.Leng B., Jin Y., Li G., Chen L., Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33:221–229. doi: 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 94.Kelly R.K., Thomson R., Smith K.J., Dwyer T., Venn A., Magnuessen C.G. Factors affecting tracking of blood pressure from childhood to adulthood: the childhood determinants of adult health study. J Pediatr. 2015;167:1422–1428.e2. doi: 10.1016/j.jpeds.2015.07.055. [DOI] [PubMed] [Google Scholar]
- 95.Beltrán S, Pharel M, Montgomery CT, López-Hinojosa IJ, Arenas DJ, DeLisser HM. Food insecurity and hypertension: a systematic review and meta-analysis. Chokesuwattanaskul R, ed. PloS One. 2020;15:e0241628. https://doi.org/10.1371/journal.pone.0241628 [DOI] [PMC free article] [PubMed]
- 96.Vos T., Lim S.S., Abbafati C., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cohen B. Urbanization in developing countries: current trends, future projections, and key challenges for sustainability. Technol Soc. 2006;28:63–80. doi: 10.1016/j.techsoc.2005.10.005. [DOI] [Google Scholar]
- 98.Yach D., Hawkes C., Gould C.L., Hofman K.J. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291:2616–2622. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 99.Chung J, Yu A, Bamhraz A, et al. Risk of subclinical-cardiovascular outcomes in children with ambulatory hypertension: a systematic review and meta-analysis. In: Vol 32; 2021:13.
- 100.Beckett L.A., Rosner B., Roche A.F., Guo S. Serial changes in blood pressure from adolescence into adulthood. Am J Epidemiol. 1992;135:1166–1177. doi: 10.1093/oxfordjournals.aje.a116217. [DOI] [PubMed] [Google Scholar]
- 101.Sun S.S., Grave G.D., Siervogel R.M., Pickoff A.A., Arslanian S.S., Daniels S.R. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 102.Lauer R.M., Anderson A.R., Beaglehole R., Burns T.L. Factors related to tracking of blood pressure in children. U.S. National Center for Health Statistics Health Examination Surveys Cycles II and III. Hypertension. 1984;6:307–314. doi: 10.1161/01.hyp.6.3.307. [DOI] [PubMed] [Google Scholar]
- 103.Bao W., Threefoot S.A., Srinivasan S.R., Berenson G.S. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa heart study. Am J Hypertens. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 104.Li Z., Snieder H., Harshfield G.A., Treiber F.A., Wang X. A 15-year longitudinal study on ambulatory blood pressure tracking from childhood to early adulthood. Hypertens Res. 2009;32:404–410. doi: 10.1038/hr.2009.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kaelber D.C., Localio A.R., Ross M., et al. Persistent hypertension in children and adolescents: a 6-year cohort study. Pediatrics. 2020;146 doi: 10.1542/peds.2019-3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Daniels S.R., Loggie J.M., Khoury P., Kimball T.R. Left ventricular geometry and severe left ventricular hypertrophy in children and adolescents with essential hypertension. Circulation. 1998;97:1907–1911. doi: 10.1161/01.cir.97.19.1907. [DOI] [PubMed] [Google Scholar]
- 107.Daniels S.R., Witt S.A., Glascock B., Khoury P.R., Kimball T.R. Left atrial size in children with hypertension: the influence of obesity, blood pressure, and left ventricular mass. J Pediatr. 2002;141:186–190. doi: 10.1067/mpd.2002.125851. [DOI] [PubMed] [Google Scholar]
- 108.Toprak A., Wang H., Chen W., Paul T., Srinivasn S., Berenson G. Relation of childhood risk factors to left ventricular hypertrophy (eccentric or concentric) in relatively young adulthood (from the Bogalusa Heart Study) Am J Cardiol. 2008;101:1621–1625. doi: 10.1016/j.amjcard.2008.01.045. [DOI] [PubMed] [Google Scholar]
- 109.Zhang H., Zhang T., Li S., et al. Long-term excessive body weight and adult left ventricular hypertrophy are linked through later-life body size and blood pressure: the Bogalusa heart study. Circ Res. 2017;120:1614–1621. doi: 10.1161/CIRCRESAHA.116.310421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang T., Li S., Bazzano L., He J., Whelton P., Chen W. Trajectories of childhood blood pressure and adult left ventricular hypertrophy: the Bogalusa heart study. Hypertension. 2018;72:93–101. doi: 10.1161/HYPERTENSIONAHA.118.10975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pieruzzi F., Antolini L., Salerno F.R., et al. The role of blood pressure, body weight and fat distribution on left ventricular mass, diastolic function and cardiac geometry in children. J Hypertens. 2015;33:1182–1192. doi: 10.1097/HJH.0000000000000552. [DOI] [PubMed] [Google Scholar]
- 112.Urbina E.M., Khoury P.R., McCoy C., Daniels S.R., Kimball T.R., Dolan L.M. Cardiac and vascular consequences of pre-hypertension in youth: cardiovascular consequences of pre-hypertension in youth. J Clin Hypertens. 2011;13:332–342. doi: 10.1111/j.1751-7176.2011.00471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hao G., Wang X., Treiber F.A., Harshfield G., Kapuku G., Su S. Blood pressure trajectories from childhood to young adulthood associated with cardiovascular risk: results from the 23-year Longitudinal Georgia stress and heart study. Hypertension. 2017;69 doi: 10.1161/HYPERTENSIONAHA.116.08312. 2017:435-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lai C.C., Sun D., Cen R., et al. Impact of long-term burden of excessive adiposity and elevated blood pressure from childhood on adulthood left ventricular remodeling patterns: the Bogalusa Heart Study. J Am Coll Cardiol. 2014;64:1580–1587. doi: 10.1016/j.jacc.2014.05.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kavey R.E. Left ventricular hypertrophy in hypertensive children and adolescents: predictors and prevalence. Curr Hypertens Rep. 2013;15:453–457. doi: 10.1007/s11906-013-0370-3. [DOI] [PubMed] [Google Scholar]
- 116.Woroniecki R.P., Kahnauth A., Panesar L.E., Supe-Markovina K. Left ventricular hypertrophy in pediatric hypertension: a mini review. Front Pediatr. 2017;5:101. doi: 10.3389/fped.2017.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Juhola J., Magnussen C.G., Berenson G.S., et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation. 2013;128:217–224. doi: 10.1161/CIRCULATIONAHA.113.001614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Baroncini L.A.V., Sylvestre Lde C., Baroncini C.V., Pecoits R. Assessment of carotid intima-media thickness as an early marker of vascular damage in hypertensive children. Arq Bras Cardiol. 2017;108:452–457. doi: 10.5935/abc.20170043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lande M.B., Carson N.L., Roy J., Meagher C.C. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40–44. doi: 10.1161/01.HYP.0000227029.10536.e8. [DOI] [PubMed] [Google Scholar]
- 120.Sorof J.M., Alexandrov A.V., Cardwell G., Portman R.J. Carotid artery intimal-medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111:61–66. doi: 10.1542/peds.111.1.61. [DOI] [PubMed] [Google Scholar]
- 121.Li S., Chen W., Srinivasan S.R., Berenson G.S. Childhood blood pressure as a predictor of arterial stiffness in young adults: the Bogalusa heart study. Hypertension. 2004;43:541–546. doi: 10.1161/01.HYP.0000115922.98155.23. [DOI] [PubMed] [Google Scholar]
- 122.Aatola H., Magnussen C.G., Koivistoinen T., et al. Simplified definitions of elevated pediatric blood pressure and high adult arterial stiffness. Pediatrics. 2013;132:e70–e76. doi: 10.1542/peds.2012-3426. [DOI] [PubMed] [Google Scholar]
- 123.Tracy R., Newman W.P., Wattigney W.A., Srinivasan S.R., Strong J.P., Berenson G.S. Histologic features of atherosclerosis and hypertension from autopsies of young individuals in a defined geographic population: the Bogalusa Heart Study. Atherosclerosis. 1995;116:163–179. doi: 10.1016/0021-9150(95)05525-2. [DOI] [PubMed] [Google Scholar]
- 124.Homma S., Ishii T., Malcom G.T., et al. Histopathological modifications of early atherosclerotic lesions by risk factors—findings in PDAY subjects. Atherosclerosis. 2001;156:389–399. doi: 10.1016/s0021-9150(00)00669-9. [DOI] [PubMed] [Google Scholar]
- 125.McGill H.C., Jr., McMahan C.A., Herderick E.E., Malcom G.T., Tracy R.E., Strong J.P. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr. 2000;72 doi: 10.1093/ajcn/72.5.1307s. (5)(suppl):1307s-1315s. [DOI] [PubMed] [Google Scholar]
- 126.Mahoney L.T., Burns T.L., Stanford W., et al. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study. J Am Coll Cardiol. 1996;27:277–284. doi: 10.1016/0735-1097(95)00461-0. [DOI] [PubMed] [Google Scholar]
- 127.Davis P.H., Dawson J.D., Mahoney L.T., Lauer R.M. Increased carotid intimal-medial thickness and coronary calcification are related in young and middle-aged adults. The Muscatine study. Circulation. 1999;100:838–842. doi: 10.1161/01.cir.100.8.838. [DOI] [PubMed] [Google Scholar]
- 128.Li L.J., Cheung C.Y.L., Liu Y., et al. Influence of blood pressure on retinal vascular caliber in young children. Ophthalmology. 2011;118:1459–1465. doi: 10.1016/j.ophtha.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 129.Gopinath B., Wang J.J., Kifley A., Tan A.G., Wong T.Y., Mitchell P. Influence of blood pressure and body mass index on retinal vascular caliber in preschool-aged children. J Hum Hypertens. 2013;27:523–528. doi: 10.1038/jhh.2013.15. [DOI] [PubMed] [Google Scholar]
- 130.Murgan I., Beyer S., Kotliar K.E., et al. Arterial and retinal vascular changes in hypertensive and prehypertensive adolescents. Am J Hypertens. 2013;26:400–408. doi: 10.1093/ajh/hps091. [DOI] [PubMed] [Google Scholar]
- 131.Seeman T., Pohl M., Palyzova D., John U. Microalbuminuria in children with primary and white-coat hypertension. Pediatr Nephrol. 2012;27:461–467. doi: 10.1007/s00467-011-2019-2. [DOI] [PubMed] [Google Scholar]
- 132.Flynn J.T. Microalbuminuria in children with primary hypertension. J Clin Hypertens. 2016;18:962–965. doi: 10.1111/jch.12858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Brown D.W., Giles W.H., Croft J.B. Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am Heart J. 2000;140:848–856. doi: 10.1067/mhj.2000.111112. [DOI] [PubMed] [Google Scholar]
- 134.Desai C.S., Ning H., Lloyd-Jones D.M. Competing cardiovascular outcomes associated with electrocardiographic left ventricular hypertrophy: the Atherosclerosis Risk in Communities Study. Heart. 2012;98:330–334. doi: 10.1136/heartjnl-2011-300819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Vlachopoulos C., Aznaouridis K., Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 136.Iribarren C., Sidney S., Sternfeld B., Browner W.S. Calcification of the aortic arch: risk factors and association with coronary heart disease, stroke, and peripheral vascular disease. JAMA. 2000;283:2810–2815. doi: 10.1001/jama.283.21.2810. [DOI] [PubMed] [Google Scholar]
- 137.Mendizábal B., Urbina E.M., Becker R., et al. SHIP-AHOY (study of high blood pressure in pediatrics: adult hypertension onset in youth): rationale, design, and methods. Hypertension. 2018;72:625–631. doi: 10.1161/HYPERTENSIONAHA.118.11434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Litwin M., Niemirska A., Sladowska-Kozlowska J., et al. Regression of target organ damage in children and adolescents with primary hypertension. Pediatr Nephrol. 2010;25:2489–2499. doi: 10.1007/s00467-010-1626-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Seeman T., Dostálek L., Gilík J. Control of hypertension in treated children and its association with target organ damage. Am J Hypertens. 2012;25:389–395. doi: 10.1038/ajh.2011.218. [DOI] [PubMed] [Google Scholar]
- 140.Seeman T., Gilík J., Vondrák K., et al. Regression of left-ventricular hypertrophy in children and adolescents with hypertension during ramipril monotherapy. Am J Hypertens. 2007;20:990–996. doi: 10.1038/ajh.2011.218. [DOI] [PubMed] [Google Scholar]
- 141.Matteucci M.C., Chinali M., Rinelli G., et al. Change in cardiac geometry and function in CKD children during strict BP control: a randomized study. Clin J Am Soc Nephrol. 2013;8:203–210. doi: 10.2215/CJN.08420811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kupferman J.C., Aronson Friedman L., Cox C., et al. BP control and left ventricular hypertrophy regression in children with CKD. J Am Soc Nephrol. 2014;25:167–174. doi: 10.1681/ASN.2012121197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.ESCAPE Trial Group. Wühl E., Trivelli A., et al. Strict blood-pressure control and progression of renal failure in children. N Engl J Med. 2009;361:1639–1650. doi: 10.1056/NEJMoa0902066. [DOI] [PubMed] [Google Scholar]
- 144.Wingen A.M., Fabian-Bach C., Schaefer F., Mehls O. Randomised multicentre study of a low-protein diet on the progression of chronic renal failure in children. European Study Group of Nutritional Treatment of Chronic Renal Failure in Childhood. Lancet. 1997;349:1117–1123. doi: 10.1016/s0140-6736(96)09260-4. [DOI] [PubMed] [Google Scholar]
- 145.Tsai W.C., Wu H.Y., Peng Y.S., et al. Association of intensive blood pressure control and kidney disease progression in nondiabetic patients with chronic kidney disease: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:792–799. doi: 10.1001/jamainternmed.2017.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Peterson J.C., Adler S., Burkart J.M., et al. Blood pressure control, proteinuria, and the progression of renal disease. The Modification of Diet in Renal Disease Study. Ann Intern Med. 1995;123:754–762. doi: 10.7326/0003-4819-123-10-199511150-00003. [DOI] [PubMed] [Google Scholar]
- 147.Jafar T.H., Stark P.C., Schmid C.H., et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med. 2003;139:244–252. doi: 10.7326/0003-4819-139-4-200308190-00006. [DOI] [PubMed] [Google Scholar]
- 148.Dionne J.M., Jiang S., Ng D.K., et al. Mean arterial pressure and chronic kidney disease progression in the CKiD cohort. Hypertension. 2021;78:65–73. doi: 10.1161/HYPERTENSIONAHA.120.16692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Flynn J.T., Mitsnefes M., Pierce C., et al. Blood pressure in children with chronic kidney disease: a report from the chronic kidney disease in children study. Hypertension. 2008;52:631–637. doi: 10.1161/HYPERTENSIONAHA.108.110635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Chavers B.M., Solid C.A., Daniels F.X., et al. Hypertension in pediatric long-term hemodialysis patients in the United States. Clin J Am Soc Nephrol. 2009;4:1363–1369. doi: 10.2215/CJN.01440209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Halbach S.M., Martz K., Mattoo T., Flynn J. Predictors of blood pressure and its control in pediatric patients receiving dialysis. J Pediatr. 2012;160:621–625.e1. doi: 10.1016/j.jpeds.2011.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kramer A.M., van Stralen K.J., Jager K.J., et al. Demographics of blood pressure and hypertension in children on renal replacement therapy in Europe. Kidney Int. 2011;80:1092–1098. doi: 10.1038/ki.2011.232. [DOI] [PubMed] [Google Scholar]
- 153.Schaefer F., Doyon A., Azukaitis K., et al. Cardiovascular phenotypes in children with CKD: the 4C study. Clin J Am Soc Nephrol. 2017;12:19–28. doi: 10.2215/CJN.01090216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wong H., Mylrea K., Feber J., et al. Prevalence of complications in children with chronic kidney disease according to KDOQI. Kidney Int. 2006;70:585–590. doi: 10.1038/sj.ki.5001608. [DOI] [PubMed] [Google Scholar]
- 155.Mitsnefes M., Stablein D. Hypertension in pediatric patients on long-term dialysis: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) Am J Kidney Dis. 2005;45:309–315. doi: 10.1053/j.ajkd.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 156.Mitsnefes M., Ho P.L., McEnery P.T. Hypertension and progression of chronic renal insufficiency in children: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) J Am Soc Nephrol. 2003;14:2618–2622. doi: 10.1097/01.asn.0000089565.04535.4b. [DOI] [PubMed] [Google Scholar]
- 157.Samuels J., Ng D., Flynn J.T., et al. Ambulatory blood pressure patterns in children with chronic kidney disease. Hypertension. 2012;60:43–50. doi: 10.1161/HYPERTENSIONAHA.111.189266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Mitsnefes M., Flynn J., Cohn S., et al. Masked hypertension associates with left ventricular hypertrophy in children with CKD. J Am Soc Nephrol. 2010;21:137–144. doi: 10.1681/ASN.2009060609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cheung A.K., Chang T.I., Cushman W.C., et al. Executive summary of the KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int.Int. 2021;99(3):559–569. doi: 10.1016/j.kint.2020.10.026. [DOI] [PubMed] [Google Scholar]
- 160.Park M.K., Menard S.W., Yuan C. Comparison of auscultatory and oscillometric blood pressures. Arch Pediatr Adolesc Med. 2001;155:50–53. doi: 10.1001/archpedi.155.1.50. [DOI] [PubMed] [Google Scholar]
- 161.Duncombe S.L., Voss C., Harris K.C. Oscillometric and auscultatory blood pressure measurement methods in children: a systematic review and meta-analysis. J Hypertens. 2017;35:213–224. doi: 10.1097/HJH.0000000000001178. [DOI] [PubMed] [Google Scholar]
- 162.Flynn J.T., Pierce C.B., Miller E.R., et al. Reliability of resting blood pressure measurement and classification using an oscillometric device in children with chronic kidney disease. J Pediatr. 2012;160:434–440.e1. doi: 10.1016/j.jpeds.2011.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Outdili Z., Marti-Soler H., Bovet P., Chiolero A. Performance of blood pressure measurements at an initial screening visit for the diagnosis of hypertension in children. J Clin Hypertens (Greenwich) 2019;21:1352–1357. doi: 10.1111/jch.13645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Negroni-Balasquide X., Bell C.S., Samuel J., Samuels J.A. Is one measurement enough to evaluate blood pressure among adolescents? A blood pressure screening experience in more than 9000 children with a subset comparison of auscultatory to mercury measurements. J Am Soc Hypertens. 2016;10:95–100. doi: 10.1016/j.jash.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 165.Roerecke M., Kaczorowski J., Myers M.G. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Intern Med. 2019;179:351. doi: 10.1001/jamainternmed.2018.6551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hamdani G., Flynn J.T., Becker R.C., et al. Prediction of ambulatory hypertension based on clinic blood pressure percentile in adolescents. Hypertension. 2018;72 doi: 10.1161/HYPERTENSIONAHA.118.11530. 2018:955-961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Stabouli S., Kotsis V., Zakopoulos N. Ambulatory blood pressure monitoring and target organ damage in pediatrics. J Hypertens. 2007;25:1979–1986. doi: 10.1097/HJH.0b013e3282775992. [DOI] [PubMed] [Google Scholar]
- 168.Kollias A., Dafni M., Poulidakis E., et al. Out-of-office blood pressure and target organ damage in children and adolescents: a systematic review and meta-analysis. J Hypertens. 2014;32:2315–2331. doi: 10.1097/HJH.0000000000000384. [DOI] [PubMed] [Google Scholar]
- 169.Flynn J.T., Daniels S.R., Hayman L.L., et al. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63:1116–1135. doi: 10.1161/HYP.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Stergiou G., Stambolliu E., Bountzona I., et al. Home blood pressure monitoring in children and adolescents: systematic review of evidence on clinical utility. Curr Hypertens Rep. 2019;21:64. doi: 10.1007/s11906-019-0967-2. [DOI] [PubMed] [Google Scholar]
- 171.Bald M., Hoyer P.F. Measurement of blood pressure at home: survey among pediatric nephrologists. Pediatr Nephrol Berl Ger. 2001;16:1058–1062. doi: 10.1007/s004670100027. [DOI] [PubMed] [Google Scholar]
- 172.Raina R., Nair N., Yap H.K., et al. Survey of telemedicine by pediatric nephrologists during the COVID-19 pandemic. Kidney Int Rep. 2021;6:2316–2322. doi: 10.1016/j.ekir.2021.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Boubouchairopoulou N., Karpettas N., Athanasakis K., et al. Cost estimation of hypertension management based on home blood pressure monitoring alone or combined office and ambulatory blood pressure measurements. J Am Soc Hypertens JASH. 2014;8:732–738. doi: 10.1016/j.jash.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 174.Nasothimiou E.G., Karpettas N., Dafni M.G., Stergiou G.S. Patients’ preference for ambulatory versus home blood pressure monitoring. J Hum Hypertens. 2014;28:224–229. doi: 10.1038/jhh.2013.104. [DOI] [PubMed] [Google Scholar]
- 175.Omboni S., McManus R.J., Bosworth H.B., et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension. 2020;76:1368–1383. doi: 10.1161/HYPERTENSIONAHA.120.15873. [DOI] [PubMed] [Google Scholar]
- 176.Davis M.L., Ferguson M.A., Zachariah J.P. Clinical predictors and impact of ambulatory blood pressure monitoring in pediatric hypertension referrals. J Am Soc Hypertens. 2014;8:660–667. doi: 10.1016/j.jash.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wühl E., Witte K., Soergel M., Mehls O., Schaefer F. Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens. 2002;20:1995–2007. doi: 10.1097/00004872-200210000-00019. [DOI] [PubMed] [Google Scholar]
- 178.Soergel M., Kirschstein M., Busch C., et al. Oscillometric twenty-four-hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J Pediatr. 1997;130:178–184. doi: 10.1016/s0022-3476(97)70340-8. [DOI] [PubMed] [Google Scholar]
- 179.Xi B., Zong X., Kelishadi R., et al. Establishing international blood pressure references among nonoverweight children and adolescents aged 6 to 17 years. Circulation. 2016;133:398–408. doi: 10.1161/CIRCULATIONAHA.115.017936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yip G.W.K., Li A.M., So H.K., et al. Oscillometric 24-h ambulatory blood pressure reference values in Hong Kong Chinese children and adolescents. J Hypertens. 2014;32:606–619. doi: 10.1097/HJH.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 181.Nazarali S., Robinson C., Khan F., et al. Deriving normative data on 24-hour ambulatory blood pressure monitoring for South Asian children (ASHA): a clinical research protocol. Can J Kidney Health Dis. 2022;9 doi: 10.1177/20543581211072329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Hypertension. 2018;71:1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 183.Cheng Y.B., Thijs L., Zhang Z.Y., et al. Outcome-driven thresholds for ambulatory blood pressure based on the new American College of Cardiology/American Heart Association classification of hypertension. Hypertension. 2019;74:776–783. doi: 10.1161/HYPERTENSIONAHA.119.13512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Lubrano R., Paoli S., Spiga S., et al. Impact of ambulatory blood pressure monitoring on the diagnosis of hypertension in children. J Am Soc Hypertens. 2015;9:780–784. doi: 10.1016/j.jash.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 185.Lee J., McCulloch C.E., Flynn J.T., et al. Prognostic value of ambulatory blood pressure load in pediatric CKD. Clin J Am Soc Nephrol. 2020;15:493–500. doi: 10.2215/CJN.10130819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Mitsnefes M., Flynn J.T., Brady T., et al. Pediatric ambulatory blood pressure classification: the case for a change. Hypertension. 2021;78:1206–1210. doi: 10.1161/HYPERTENSIONAHA.121.18138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hamdani G., Mitsnefes M.M., Flynn J.T., et al. Pediatric and adult ambulatory blood pressure thresholds and blood pressure load as predictors of left ventricular hypertrophy in adolescents. Hypertension. 2021;78:30–37. doi: 10.1161/HYPERTENSIONAHA.120.16896. [DOI] [PubMed] [Google Scholar]
- 188.Campbell F, Shah S, Srivaths P, Sigler K, Acosta A. Elevated load with normal mean in pediatric hypertension (HTN): what does it mean? In: J Am Soc Nephrol. 2021;32:51.
- 189.The SPRINT Research Group. Wright J.T., Williamson J.D., et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Williams B., Mancia G., Spiering W., et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 191.Smith-Spangler C.M., Juusola J.L., Enns E.A., Owens D.K., Garber A.M. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost-effectiveness analysis. Ann Intern Med. 2010;152:481–487. doi: 10.7326/0003-4819-152-8-201004200-00212. [DOI] [PubMed] [Google Scholar]
- 192.World Health Organization Impact of salt reduction in Finland and the United Kingdom. World Health Organization. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/news/news/2014/12/reducing-salt-consumption/impact-of-salt-reduction-in-finland-and-the-united-kingdom Published 2014.
- 193.Bloom D., Chisholm D., Jane Llopis E., Prettner K., Stein A., Feigl A. From burden to “best buys”: reducing the economic impact of non-communicable disease in low and middle-income countries. Published Online January 1, 2011. World Health Organization. https://www.who.int/nmh/publications/best_buys_summary.pdf
- 194.Jafar T.H., Gandhi M., de Silva H.A., et al. A community-based intervention for managing hypertension in rural South Asia. N Engl J Med. 2020;382:717–726. doi: 10.1056/NEJMoa1911965. [DOI] [PubMed] [Google Scholar]
- 195.Finkelstein E.A., Krishnan A., Naheed A., et al. Budget impact and cost-effectiveness analyses of the COBRA-BPS multicomponent hypertension management programme in rural communities in Bangladesh, Pakistan, and Sri Lanka. Lancet Glob Health. 2021;9:e660–e667. doi: 10.1016/S2214-109X(21)00033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Campbell F., Conti G., Heckman J.J., et al. Early childhood investments substantially boost adult health. Science. 2014;343:1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Filippini T., Malavolti M., Whelton P.K., et al. Blood pressure effects of sodium reduction: dose-response meta-analysis of experimental studies. Circulation. 2021;143:1542–1567. doi: 10.1161/CIRCULATIONAHA.120.050371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Huang L., Trieu K., Yoshimura S., et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315. doi: 10.1136/bmj.m315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Leyvraz M., Chatelan A., da Costa B.R., et al. Sodium intake and blood pressure in children and adolescents: a systematic review and meta-analysis of experimental and observational studies. Int J Epidemiol. 2018;47:1796–1810. doi: 10.1093/ije/dyy121. [DOI] [PubMed] [Google Scholar]
- 200.He F.J., MacGregor G.A. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48:861–869. doi: 10.1161/01.HYP.0000245672.27270.4a. [DOI] [PubMed] [Google Scholar]
- 201.Rios-Leyvraz M., Bovet P., Tabin R., et al. Urine spot samples can be used to estimate 24-hour urinary sodium excretion in children. J Nutr. 2018;148:1946–1953. doi: 10.1093/jn/nxy211. [DOI] [PubMed] [Google Scholar]
- 202.Mente A., O’Donnell M., Rangarajan S., et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392:496–506. doi: 10.1016/S0140-6736(18)31376-X. [DOI] [PubMed] [Google Scholar]
- 203.O’Donnell M., Mente A., Rangarajan S., et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–623. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 204.Ma Y., He F.J., Sun Q., et al. 24-hour urinary sodium and potassium excretion and cardiovascular risk. N Engl J Med. 2022;386:252–263. doi: 10.1056/NEJMoa2109794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Sacks F.M., Svetkey L.P., Vollmer W.M., et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 206.Couch S.C., Saelens B.E., Khoury P.R., et al. Dietary approaches to stop hypertension dietary intervention improves blood pressure and vascular health in youth with elevated blood pressure. Hypertension. 2021;77:241–251. doi: 10.1161/HYPERTENSIONAHA.120.16156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zafarmand M.H., Spanjer M., Nicolaou M., et al. Influence of dietary approaches to stop hypertension-type diet, known genetic variants and their interplay on blood pressure in early childhood: ABCD study. Hypertension. 2020;75:59–70. doi: 10.1161/HYPERTENSIONAHA.118.12292. [DOI] [PubMed] [Google Scholar]
- 208.Kelley G.A., Kelley K.S., Tran Z.V. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6:8–16. doi: 10.1111/j.1520-037x.2003.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Cai L., Wu Y., Wilson R.F., Segal J.B., Kim M.T., Wang Y. Effect of childhood obesity prevention programs on blood pressure: a systematic review and meta-analysis. Circulation. 2014;129:1832–1839. doi: 10.1161/CIRCULATIONAHA.113.005666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Kim N., Seo D.C., King M.H., Lederer A.M., Sovinski D. Long-term predictors of blood pressure among adolescents during an 18-month school-based obesity prevention intervention. J Adolesc Health. 2014;55:521–527. doi: 10.1016/j.jadohealth.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 211.Simonetti G.D., Rizzi M., Donadini R., Bianchetti M.G. Effects of antihypertensive drugs on blood pressure and proteinuria in childhood. J Hypertens. 2007;25:2370–2376. doi: 10.1097/HJH.0b013e3282efeb7e. [DOI] [PubMed] [Google Scholar]
- 212.Chaturvedi S, Lipszyc DH, Licht C, et al. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9:498–580. [DOI] [PubMed]
- 213.Burrello J., Erhardt E.M., Saint-Hilary G., et al. Pharmacological treatment of arterial hypertension in children and adolescents: a network meta-analysis. Hypertension. 2018;72:306–313. doi: 10.1161/HYPERTENSIONAHA.118.10862. [DOI] [PubMed] [Google Scholar]
- 214.Samuel J.P., Tyson J.E., Green C., et al. Treating hypertension in children with n-of-1 trials. Pediatrics. 2019;143 doi: 10.1542/peds.2018-1818. [DOI] [PMC free article] [PubMed] [Google Scholar]