Abstract
Objective
To study the knowledge of Saudi women regarding contraceptive use.
Methodology
In Al-Qunfudah, Saudi Arabia, 1107 Saudi women aged 18 to 45 years old participated in a cross-sectional descriptive study utilizing a closed-question survey. Data were compiled using SPSS v 21 software.
Results
The participants in our study were 1107 females between the ages of 18 and 45. The majority of them were married, educated, and had used or were using oral contraceptives (OC) (50.2%), mostly for family planning (81.1%). Fear of OC side effects was stated by 39.9% of women who had never used it as a reason for not using it, and some women were unsure about consequences, such as mood changes (20.2%) and headaches (28%); 44.7% of women did not believe that they needed OC. Many women were ignorant of OC’s health and menstrual cycle benefits, with only 7.9% and 5.8% agreeing that it can help with premenstrual syndrome and acne problems, respectively. Majority of women said that they learned about contraception through doctors and friends/relatives, but 73.0% felt that the information available from health-care service was inadequate.
Conclusion
The findings revealed that women in this region were lack awareness regarding contraceptive techniques, including OC, as well as its side effects and potential health hazards. It is necessary to strengthen family knowledge and how they can planning and contraception initiatives.
Keywords: oral contraception, side effects, knowledge, Saudi Arabia, family planning
Introduction
Family planning or contraceptive methods refers to the utilization of methods that interfere with the normal processes of ovulation, fertilization, and/or implantation to prevent pregnancy as a result of sexual intercourse.1 A prominent feature of Saudi Arabian society is the tendency to have large families – the birth rate and total fertility rate in Saudi Arabia is high compared with developed countries,2 with a total fertility rate estimated in 2017 as 2.09 live births per woman.3
Women may disregard the complications of pregnancy and overrate the risks of contraception. Approximately 350,000 women, almost 99% of whom are in developing countries, die every year while pregnant or giving birth. An estimated 8 million more women suffer from severe disease and life-long impairment as a result of childbirth complications.2 Increasing contraceptive utilization in developing countries has decreased the number of maternal deaths by 40% over the past 20 years, mainly by reducing the number of unwanted pregnancies.4 Contraception is essential to women of childbearing age, to improve their reproductive health and avoid unintended pregnancy.5 Changes in women’s education and work has been and continues to be a significant factor in changing perceptions and fertility practices, with trends toward birth spacing and, consequently, the use of contraception.6
Methods of contraception include OC, implants, injectables, patches, vaginal rings, intrauterine devices (IUDs), condoms, male and female sterilization, lactational amenorrhea methods, withdrawal, and fertility awareness-based methods. These methods have different mechanisms of action and effectiveness in preventing unintended pregnancy.7 Contraception has other benefits, which may include regulation of the menstrual cycle, reduction in dysmenorrhea, reduction pelvic inflammatory disease and sexually transmitted disease risk, reduction in endometrial and ovarian cancer risk, and treatment of polycystic ovarian syndrome.8
Oral contraception (OC) is the most widely used method of contraception due to its accessibility, reliability, and reversibility.9 OC has important health benefits, as high- and low-dose combination OC decreases the risk of endometrial and ovarian cancer by about 50% for at least 20 years after it is discontinued. It also decreases the risk of benign ovarian tumors, abnormal uterine bleeding due to ovulatory dysfunction, dysmenorrhea, osteoporosis, premenstrual dysphoric disorder, iron deficiency anemia, benign breast disorders, and functional ovarian cysts. Ectopic pregnancy and salpingitis, which can impair fertility, also occur less frequently in OC users.10
Oral contraceptives contain estrogen and progesterone, and their efficacy is restricted by concerns such as adherence to prescribed regimens, which is linked to awareness of proper usage and the probability of unpleasant events. Women who use OCPs correctly have reported failure rates of less than 1%, whereas those who use the tablets inconsistently or inaccurately have reported rates as high as 9%.9
Most OC side effects are mild and disappear with continued use or switching to another pill formulation. The most common adverse effects of combined oral contraceptive pills is breakthrough bleeding. Users may also complain of nausea (which can be avoided by taking the medication at night before sleep), headaches, abdominal cramping, breast tenderness, an increase in vaginal discharge, or decreased libido. Serious side effects of OC are deep venous thrombosis and thromboembolism.10,11 With the long-term use of OCs the risk of cervical cancer is slightly increased, but after stopping OCs the risk decrease to baseline.10
Condoms are the only method of contraception that can prevent both pregnancy and the transfer of sexually transmitted illnesses like HIV.7
Long-lasting action Reversible contraceptives are methods that give effective contraception for a long time without requiring the user’s action and with minimal user burden after beginning. They include IUDs and subdermal implants, and they allow for a quick return to fertility after they have been removed. They are cost-effective, can save governments a lot of money, and directly help to achieving national and international health goals.5
Many studies have been performed to determine women’s knowledge and patterns of contraception use. A comprehensive search of PubMed of the years 1989 to 2019 found that around 51% of females between 15 and 49 years in Middle Eastern countries used contraception, well below the 64% global average. This highlights an unmet need for greater understanding and adoption of family planning programs in this region.1
One cross-sectional study of 708 women mostly aged between 15 and 35 years was conducted in Saudi Arabia to determine the relationship between various demographic variables and Knowledge and use of contraception. The study found that although knowledge about contraception increased with age, a knowledge deficiency existed across all age groups, particularly among 15–25-year-old women. Women demonstrated inadequate knowledge about OC and its potential side effects and health-related issues. Many women in the study were found to use OC for causes other than preventing pregnancy, including postponing their menstrual periods.9
Another cross-sectional study conducted among women in Riyadh estimated the prevalence, knowledge, behaviors, and practices in terms of OC use. The majority (89%) of OC users reported at least one side effect, with a small proportion (7.2%) experiencing many side effects. Married OC users reported significantly more weight gain and headaches than unmarried OC users.12 Women in a study conducted in Al-Ahsa, Saudi Arabia, most of whom primarily used OC to prevent pregnancy, also considered OC to have side effects (96%).13
Another study carried out in Abha, Aseer Region found a prevalence of unmet contraception need of 32.6%. Contraception inaccessibility was the main reason for not using contraception, with lack of knowledge, religious beliefs, fear of the side effects based on previous experience, and lack of consensus with their husband all featuring as barriers to contraceptive use. Unmet need was especially high amongst women in the lowest and oldest age groups.14 Another cross-sectional survey study, performed in Al-Qassim region, Saudi Arabia among married women aged 18–49 years, demonstrated how sociodemographic status and lifestyle are significantly associated with knowledge of contraceptive methods, as well as use of contraception for pregnancy spacing. This study showed that contraceptive use was significantly increased in working, educated women, particularly those aged 30 years or older;15 these studies emphasize how low educational levels are linked strongly with unmet contraceptive needs.14
The study of Alotaibi et al16 conducted in Riyadh assessed women’s knowledge of OC compliance, complications, and side effects. No significant differences in knowledge of compliance and side effects were found across educational levels; however, women who had more children and those between 30 and 39 years old had better understanding of the use of OC. An online survey conducted in Riyadh on combined OC use among women aged 18–40, most of whom were married university graduates and current or past users of OC, noted inadequate knowledge across all five surveyed domains of type, risks, side effects, contraindications, and OC use.17
The majority of Saudi Arabian women appear to have some knowledge of contraception, as evidenced by one survey conducted in Aseer. In this survey, OC was the best-known method, with 87% of respondents reporting knowledge of this method. These women reported mainly using contraception to prevent pregnancy, with child spacing, husband’s orders, and medical disorders cited as other reasons for using contraception.18
Globally, the World Health Organization indicated that in 2019, 1.1 billion of the 1.9 billion Women of Reproductive Age (15–49 years) in the world have a need for family planning; 842 million of these are utilizing contraceptive methods, while 270 million have an unmet need for contraception.
Indicator 3.7.1 of the Sustainable Development Goals (SDGs) has remained stable at roughly 77% globally between 2015 and 2020, but has increased from 55% to 58% in Africa.7
The literature overall indicates poor knowledge, knowledge gaps, and negative attitudes about contraception in Saudi women.16 Women of reproductive age in Al-Qunfudah district have not been previously surveyed on their contraception knowledge or practices, so this study’s objective was to fill this gap in information by measuring women’s contraception knowledge, specifically of OC use and its complications.
Materials and Methods
In this cross-sectional descriptive study, we used a survey questionnaire among Saudi women aged 18 to 45 years old living in Al-Qunfudah, Saudi Arabia to identify the knowledge of women of reproductive age on contraceptive methods. All Saudi women in the district who were using OCs or had used OCs for contraception or other reasons were included and the survey was conducted between March 2020 and March 2021. Pregnant and non-Saudi women were excluded from the survey, which was carried out using a questionnaire written in Arabic. Ethical approval was obtained from the Institutional Review Board of King Abdulaziz University.
Data collection was carried out using an electronic, closed-ended questionnaire. The questionnaire was validated to determine the comprehensibility of the questions and the repeatability of the responses. The Google form electronic questionnaire and collected data were encoded into Statistical Package for Social Sciences (SPSS) version 21 (SPSS Inc., Armonk, NY, USA).
Data Analysis
The questionnaire included three sections. The first section requested demographic data, including age, social status, education level of both wife and husband, job status, family income, number of children, and number of previous births. The second section asked about OC use, purpose of use, and the reasons for not using it, as appropriate. The third section used questions to measure extent of knowledge about OC side effects and effect on the menstrual cycle.
Finally, there were two questions about family planning and the need for awareness about contraceptives and their complications. Descriptive analyses were conducted calculating frequencies and percentages.
Results
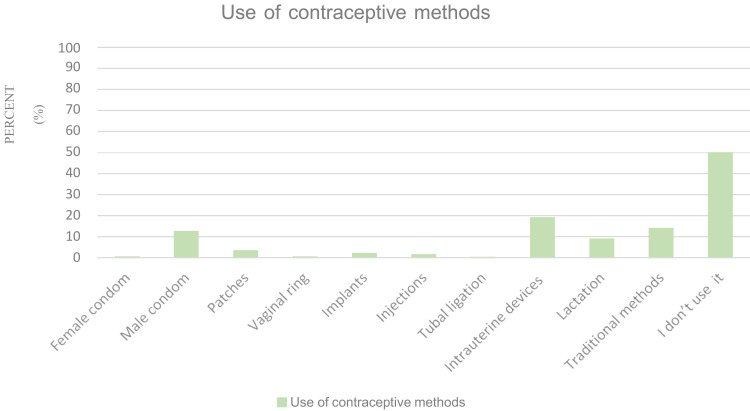
When asked about contraceptive methods used previously or currently, IUD was most commonly used (210/1107, 19%), followed by traditional methods (148/1107, 13.4%), male condom (138/1107, 12.5%), and lactation amenorrhea method (99/1107, 8.9%). Smaller proportions of women used or had used contraceptive patches (37/1107, 3.3%), contraceptive implants (22/1107, 2%), injections (16/1107, 1.4%), female condoms (4/1107, 0.4%), and vaginal ring (4/1107, 0.4%). Two women had had tubal ligation (0.2%). A total of 552 (49.9%) surveyed women had not used any contraceptive method (Figure 1).
Figure 1.
Contraceptive method used.
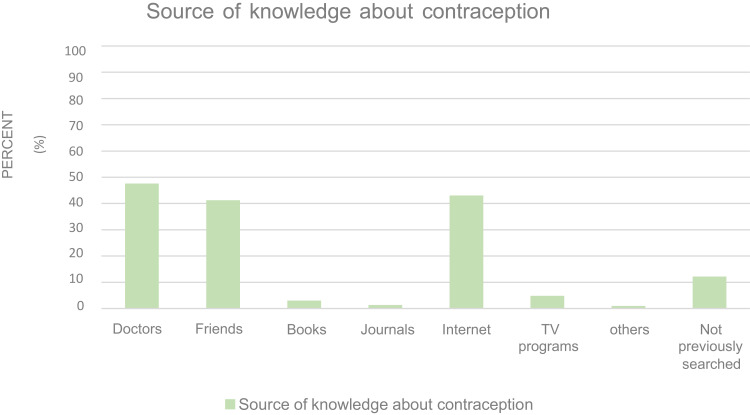
Figure 2 shows the source of contraception information. A total of 525 (47.4%) received contraception information from doctors, 474 (42.8%) from the internet, 454 (41%) from friends, 51 (4.6%) from TV programs, 31 (2.8%) from books, 12 (1.1%) from journals, and 8 (0.7%) from other sources. A total of 132 (11.9%) reported that they had never sought or received information about contraception (Figure 2).
Figure 2.
Source of women’s knowledge about contraception.
A total of 1107 female participants responded to the questionnaire. Their ages ranged from 18 to 45 years, with the largest age group (45.3%) between 18 and 29 years (Table 1). The majority of participants were married (82.9%), with a very small proportion of divorced or widowed participants. We divided education into five levels, and most of the wives (74.4%) were university graduates and better educated than their husbands, of whom 47.3% were university graduates. Of the respondents, 51% were housewives and 34.1% were employed, with a small percentage of students. Most had one or two children (41%), although 39% had three or more, and 20% did not have any children. In terms of monthly household income, most participants (39.1%) earned SAR5000–10 000 (Table 1).
Table 1.
Demographic Characteristics of the Participants (N=1107)
| n (%) | ||
|---|---|---|
| Total | 1107 (100.0) | |
| Age (years) | 18–29 | 502 (45.3) |
| 30–39 | 346 (31.3) | |
| 40–45 | 259 (23.4) | |
| Social status | Single | 137 (12.4) |
| Married | 918 (82.9) | |
| Divorced | 42 (3.8) | |
| Widow | 10 (0.9) | |
| Educational level of wife | Illiterate | 8 (0.7) |
| Primary school | 14 (1.3) | |
| Secondary school | 36 (3.3) | |
| High school | 225 (20.3) | |
| University | 824 (74.4) | |
| Educational level of husband | None | 173 (15.6) |
| Illiterate | 10 (0.9) | |
| Primary school | 35 (3.2) | |
| Secondary school | 65 (5.9) | |
| High school | 300 (27.1) | |
| University | 524 (47.3) | |
| Job status | Employee | 377 (34.1) |
| Housewife | 565 (51.0) | |
| Student | 165 (14.9) | |
| Monthly family income (SAR) | 0–1500 | 113 (10.2) |
| 1500–5000 | 241 (21.8) | |
| 5000–10,000 | 433 (39.1) | |
| >10,000 | 320 (28.9) | |
| Number of children | None | 221 (20.0) |
| <3 | 454 (41.0) | |
| ≥3 | 432 (39.0) | |
| Number of births | None | 221 (20.0) |
| <3 | 454 (41.0) | |
| ≥3 | 432 (39.0) | |
Of the 555 participants who had used OC, 21% were currently using it and 29.2% had previously used it, mostly for family planning purposes (81.1%). Other uses were treatment of menstrual pain (2%), treatment of endometriosis (0.5%), for relief of premenstrual syndrome symptoms (1.3%), and for other reasons (5.6%). Among the 552 participants (49.9%) who had never used OC, the most common reason for non-use was a lack of need for it (44.7%), followed by fear of side effects (39.9%). Other reasons were refusal by husband (2.7%), religious reasons (1.4%), and family planning completed (0.9%) (Table 2).
Table 2.
Use of Oral Contraception and Reasons for Use/Non-Use
| n (%) | ||
|---|---|---|
| Do you use combined contraceptive pills? | No, not used currently or previously | 552 (49.9) |
| Yes, previously used | 323 (29.2) | |
| Yes, currently used | 232 (21.0) | |
| Total | 1107 (100.0) | |
| If your answer is yes: (previously or currently used, n=555) | n (%) | |
| What is the purpose of using it? | For family planning | 450 (81.1) |
| For treatment of menstrual pain | 11 (2.0) | |
| For treatment of endometriosis | 3 (0.5) | |
| To relieve the symptoms of PMS | 7 (1.3) | |
| Other reasons | 31 (5.6) | |
| If your answer is no: (n=552) | n (%) | |
| What is the reason for not using it? | Fear of side effects | 220 (39.9) |
| Religious reasons | 8 (1.4) | |
| Refusal by husband | 15 (2.7) | |
| Family planning finished | 5 (0.9) | |
| No need for it | 247 (44.7) | |
| Others | 42 (7.6) | |
Women were asked whether OC caused side effects or affected other medical conditions. Their responses are shown in Table 3. They were most likely to believe that OC caused mood changes, with 805/1107 (72.7%) believing that mood changes increased on OC. Large proportions of women reported not knowing about the effects of OC on various conditions, with more than 50% reporting not knowing about the effects of OC on breast cancer, endometrial cancer, blood clots, greasy hair, HIV/sexually transmitted infections (STIs), anemia, and polycystic ovarian syndrome (PCOS). Many women thought that OC increased nausea (46.7%) and blood clots (30.7%).
Table 3.
Responses to Questions on the Extent Knowledge About the Side Effects of OC
| Side Effect/Health Issue, n (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Response | Anemia | Greasy Hair | Acne | HIV/STD | Polycystic Ovary | Breast Cancer | Endometrial Cancer | Mood Change | Nausea | Blood Clot |
| No change | 205(18.5) | 163(14.7) | 254(22.9) | 230(20.8) | 143(12.9) | 156(14.1) | 127(11.5) | 76(6.9) | 236(21.3) | 160(46.7) |
| I do not know | 596(53.8) | 586(52.9) | 460(41.6) | 702(63.4) | 561(50.7) | 687(62.1) | 755(68.2) | 208(18.8) | 326(29.4) | 596(53.8) |
| Decrease | 121(10.9) | 160(14.5) | 64(5.8) | 65(5.9) | 121(10.9) | 40(3.6) | 37(3.3) | 18(1.6) | 28(2.5) | 11(1.0) |
| Increase | 185(16.7) | 198(17.9) | 329(29.7) | 110(9.9) | 282(25.5) | 224(20.2) | 188(17.0) | 805(72.7) | 517(46.7) | 340(30.7) |
| Total all: 1107 (100) | ||||||||||
For the effect of OC on anemia, 53.8% reported that they did not know, followed by 18.5% for no changes, and 16.7% and 10.9% for increase and decrease in the condition, respectively. For greasy hair, 52.9% reported that they did not know, 17.9% believed it increased on OC, 14.7% reported no change, and 14.5% maintained that OC decreased greasy hair. Most of the participants (52.9%) did not know if acne changed with OC, and 29.7% thought that it increased.
A total of 702 (63.4%) respondents did not know if OC influenced HIV/STIs, with only 20.8% answering that there was no change in HIV or STIs on OC. Many women were also unaware of the impact of OC on PCOS, with 50.7% not knowing if there was any effect, and 25.5% believing OC increased PCOS symptoms; 62.1% of the respondents did not know the effect of OC on breast cancer and 20.2% thought it increased breast cancer (Table 3).
The respondents were asked what they knew about the effects of OC on the menstrual cycle. Most indicated that headaches increased (55%), although 29.2% did not know about headaches being an effect of OC. In terms of mood changes, 766/1107 (69.2%) shared that they thought mood changes increased with OC, whereas 20.2% reported being unaware of this effect. Many women thought menstrual pain increased on OC (37.3%), with 16.3% believing it decreased and 17.7% claiming it did not change. In terms of premenstrual syndrome (PMS), 47.5% of women did not know the effect of OC and 28.7% thought PMS increased, with only 7.9% believing that OC made PMS symptoms less.
Blood flow was believed to increase on OC during the menstrual cycle by 38.1% of the respondents and thought to decrease by 19.9%. Some participants did not know about change to blood flow (28.1%) and 13.9% claimed that it did not change. Many did not know about leg edema on OC (43.9%) and 28.8% believed that OC had no impact this. Half of the respondents (49.8%) claimed that body weight increased on OC; conversely, 18.5% believed body weight did not change (Table 4).
Table 4.
Beliefs About the Effect of Oral Contraception on the Menstrual Cycle
| How Does Oral Contraception Affect the Menstrual Cycle? | n | % | |
|---|---|---|---|
| Total | 1107 | 100.0 | |
| Headache | No changes | 147 | 13.3 |
| I do not know | 323 | 29.2 | |
| Decrease | 28 | 2.5 | |
| Increase | 609 | 55.0 | |
| Mood changes | No changes | 91 | 8.2 |
| I do not know | 224 | 20.2 | |
| Decrease | 26 | 2.3 | |
| Increase | 766 | 69.2 | |
| Menstrual pain | No changes | 196 | 17.7 |
| I do not know | 318 | 28.7 | |
| Decrease | 180 | 16.3 | |
| Increase | 413 | 37.3 | |
| PMS | No changes | 180 | 16.3 |
| I do not know | 526 | 47.5 | |
| Decrease | 87 | 7.9 | |
| Increase | 314 | 28.4 | |
| Blood flow during menstrual cycle | No changes | 154 | 13.9 |
| I do not know | 311 | 28.1 | |
| Decrease | 220 | 19.9 | |
| Increase | 422 | 38.1 | |
| Leg swelling | No changes | 319 | 28.8 |
| I do not know | 486 | 43.9 | |
| Decrease | 27 | 2.4 | |
| Increase | 275 | 24.8 | |
| Weight change | No changes | 205 | 18.5 |
| I do not know | 271 | 24.5 | |
| Decrease | 80 | 7.2 | |
| Increase | 551 | 49.8 | |
When asked about the need for education about contraceptives and their complications, 530 (47.9%) participants reported that they needed more education, and 73% reported not receiving adequate education about contraception and its complications at health-care centers and hospitals in the region (Table 5).
Table 5.
Family Planning and Need for Awareness About Contraception and Its Complications
| Total | n | % | |
|---|---|---|---|
| 1107 | 100.0 | ||
| Have you ever planned a pregnancy with your husband?* | No | 229 | 23.5 |
| Yes | 745 | 76.5 | |
| Missing | 133 | ||
| Have you been adequately educated about contraceptives and their complications in healthcare centers and hospitals in the region? | No | 808 | 73.0 |
| Yes | 299 | 27.0 | |
| Do you need education about contraceptives and their complications? | No | 577 | 52.1 |
| Yes | 530 | 47.9 | |
Note: *Percentages shown for this question are of women that answered the question.
When asked whether pregnancy was something that was planned with her husband, 76.5% of women stated that they planned pregnancy together.
Discussion
In this study, we aimed to measure the knowledge of women of childbearing age about OC use and its complications. As well as collecting demographic data, we surveyed women on their knowledge and use of contraception, and reasons for not using it. We also surveyed women about the extent of their knowledge about side effects of OC and the effects of OC on the menstrual cycle, and we asked them about their use of family planning and need for greater awareness about contraception and its complications.
Most of the respondents were married and well educated, and had used or were currently using contraception, with most using it for family planning. Half of respondents had never used OC, believing that they either did not need it or that it had side effects. Most of the women in our study who used contraception were using OC, with IUDs and male condoms being next most frequently use contraceptive methods. This is comparable with the reported usage in another study conducted in Al-Qassim region.2 The vast majority (76.5%) of women reported that family planning was done in consultation with their husband.
We looked at women’s awareness of some of the benefits of OC. Acne vulgaris and hirsutism in women of reproductive and late reproductive age is known to improve on OC by up to 40%,19 yet the majority of women in our study were unaware of this. OC is considered one of the treatments for PCOS,20 and our results indicated low knowledge among women of the use of OC in PCOS. Another benefit of OC is the relief of menstrual pain.10 Only 16.3% of the respondents identified this as an effect of OC, and over half of respondents were either unaware of the effect of OC on menstrual pain or thought that OC increased it. This confirms similar findings in another Saudi study.9 There were similar findings in our study for PMS, the recurrent luteal-phase condition characterized by physical, psychological, and behavioral changes of sufficient severity to result in deterioration of interpersonal relationships and normal activity. Symptoms of PMS have been reported to affect as many as 90% of women of reproductive age sometime during their lives.21 Although OC is considered a treatment for PMS,22 only 7.9% of our survey respondents were aware that OC can reduce its symptoms. Many of the results indicated low knowledge about OC. For example, very few women knew that OC can decrease anemia, a known positive effect of OC.10 In terms of long-term benefits of OC, it is known that OCs decrease the risk of endometrial cancer.10 Once again, most of the respondents in our survey did not know this.
We found that women had little knowledge about using contraception to protect against STIs. This finding was similar to that in a study conducted in Al-Kharj, Saudi Arabia, about the knowledge and use of contraceptives in relation to STIs, which also found that most women believed that OCs do not protect against STIs.9
In terms of the negative effects of OC and side effects, we asked women about mood changes. The majority of women expressed that mood changes increased on OC; this was the most common side effect reported in another study conducted among Saudi women about prevalence of side effects from OC.13 Nausea was reported as a known effect of OC, in keeping with information from another study on experience, knowledge, and practice of OC.12 Most of our respondents knew that headache was a side effect of OC; however, a sizable proportion were not aware of this. OCP may make migraines worse, and in migraine with aura, the use of combined oral contraceptives is always contraindicated.23 A considerable proportion (38.1%) of our participants believed that blood flow increased during menstrual periods as an effect of OC. This compares with a study conducted in Riyadh, Saudi Arabia in which 41.77% of women reported severe bleeding.12 About half of the respondents were unaware of leg edema as a side effect of OC.24 About half of our participants identified weight gain as a side effect of OC. This compares with another study conducted in primary care clinics in Saudi Arabia where 36.1% of respondents reported knowledge of weight gain in OC use.24
The use of OC is well-known a risk factor for venous thromboembolism; however, most of the respondents in our study did not know this, with only about one-third reporting they were aware of increased risk of blood clots. A study conducted in Al-Kharj found that even highly educated women were not aware or had low awareness of the risk of serious complications such as thromboembolism from OC.9,25 In terms of other serious side effects, women in our study had low knowledge about the relationship between OC and breast cancer, despite the risk of breast cancer being increased with longer duration of use of oral contraceptives.26
When asked whether there was adequate education about contraception and its side effects in healthcare centers and hospitals in the region, the majority of our respondents answered no, although interestingly about half of women reported that they do need more education, suggesting that more research into this is required. The main source of information about contraception was doctors; this is similar to another study performed in Hail region.27 We found that social media and friends/relatives also play a significant role in awareness of contraception.
Overall, our results indicated that uptake of contraception and knowledge of it among Saudi women remains low when compared with developed countries. Further education and awareness about contraceptive methods and their complications are required.
There is an established association between contraception use and maternal mortality. As contraception usage increases, the number of high-risk births decreases, and high parity is practically eliminated at high contraceptive usage levels.28 Increasing knowledge about contraception improves the health of both mothers and children, and thus efforts to facilitate this type of education are essential. Doctors remain a key source of contraception information, and we recommend increasing counseling about contraceptive methods throughout Saudi healthcare centers and hospitals.
This research had some limitations. It was conducted during the Covid-19 pandemic and therefore the questionnaire was published, and the responses collected electronically; thus, we were unable to ensure that the questions were all properly understood. The respondents were from one region of Saudi Arabia, limiting the generalization of results to all Saudi women. In addition, we did not explore for correlations between OC knowledge and use and the participant demographic data and further research on this is recommended.
Conclusion
This study measures the prevalence of knowledge about contraceptive methods among women of reproductive age in a district of Saudi Arabia, with an emphasis on knowledge of OC, which was the most widely used contraceptive method among the respondents. We found that women lacked awareness of contraceptive methods and that their understanding of the benefits and side effects of OC was inadequate. Our analysis indicated that appropriate approaches, specifically through health institutions such as clinics and hospitals, should be implemented, to increase women’s knowledge about contraception and improve their awareness of the benefits of family planning and its relationship to contraceptive use.
Acknowledgments
We would like to extend our sincere thanks and gratitude to REC at FOM & KAUH to approve research proposal.
Data Sharing Statement
Research data and material are with the principal investigator.
Ethical Approval and Consent to Participate
Ref No. 466-20. Response to the questionnaire was considered as agreement for participation No human right violation, and our study complies with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.AlYamani AA. Awareness and Use of Contraceptives in the Middle East. EC Microbiol. 2019;16:1–7. [Google Scholar]
- 2.Al Sheeha M. Awareness and use of contraceptives among Saudi women attending primary care centers in Al-Qassim, Saudi Arabia. Int J Health Sci. 2010;4:11–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Najimudeen M, Myint MH, Shyam Rao, et al. “scholars international journal of obstetrics and gynecology”; 2018.
- 4.Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui J. Contraception and health. Lancet. 2012;380:149–156. doi: 10.1016/S0140-6736(12)60609-6 [DOI] [PubMed] [Google Scholar]
- 5.Yalew SA, Zeleke BM, Teferra AS. Demand for long-acting contraceptive methods and associated factors among family planning service users, Northwest Ethiopia: a health facility based cross sectional study. BMC Res Notes. 2015;8:29. doi: 10.1186/s13104-015-0974-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Nahedh NN. The effect of sociodemographic variables on child-spacing in rural Saudi Arabia. East Mediterr Health J. 1999;5:136–140. doi: 10.26719/1999.5.1.136 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Family planning/contraception methods; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception. Accessed January 22, 2021.
- 8.Costa FJ. Beneficios nao contraceptivos da contracepcao [non-contraceptive benefits of contraception]. Sex Planeam Fam. 1995;8:16–18. [PubMed] [Google Scholar]
- 9.Alshardan A, Bari M, AlSinan I, AlMuqhim M, AlRazeyg N. Knowledge and use of contraceptives among women in Al-Kharj City, Saudi Arabia. Int J Med Dev Ctries. 2020;4:902–909. doi: 10.24911/IJMDC.51-1585167321 [DOI] [Google Scholar]
- 10.Casey F. Oral contraceptives - gynecology and obstetrics. MSD Manual Professional Edition; 2021. Available from: https://www.msdmanuals.com/professional/gynecology-and-obstetrics/family-planning/oral-contraceptives. Accessed January 26, 2021. [Google Scholar]
- 11.Cooper D, Mahdy H. Oral contraceptive pills. StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430882/. Accessed January 22, 2021. [Google Scholar]
- 12.Al-Mass AA, Al-Shahranu BS, Al-Mweisheer AN, et al. User experience, knowledge and practice of oral contraceptive: a study from Riyadh, Saudi Arabia. Ann Med Health Sci Res. 2018;8:411–419. [Google Scholar]
- 13.Elmaghraby D. WJPR Archive VieW [Internet]. Wjpr.net; 2021. Available from: https://wjpr.net/dashboard/archive_show/2019/VOLUME%208,%20JANUARY%20ISSUE%201. Accessed March 21, 2021. [Google Scholar]
- 14.Khalil S, Alzahrani M, Siddiqui A. Unmet need and demand for family planning among married women of Abha, Aseer Region in Saudi Arabia. Middle East Fertil Soc J. 2018;23(1):31–36. doi: 10.1016/j.mefs.2017.07.004 [DOI] [Google Scholar]
- 15.Elgharabway R, Ahmed A, Alsuhaibani R. Awareness, prevalence and determinants of birth control methods use among women in Saudi Arabia. Int Arch Med. 2015;8. doi: 10.3823/1844 [DOI] [Google Scholar]
- 16.Alotaibi M, Shiddo O, Ghoraba M. Knowledge, attitude, and use of oral contraceptive pills among Saudi women seen at the primary care clinics of Security Forces Hospital, Riyadh, Saudi Arabia. J Med Sci Clin Res. 2018;6. doi: 10.18535/jmscr/v6i4.160 [DOI] [Google Scholar]
- 17.Alsulaiman T, Alamer M, Alrajah G, Khpjah Q, Alrumaihi S, Almutairi O. Knowledge of combined oral contraceptives among young females in Riyadh. Int J Med Sci Pub Health. 2017;6:752–757. [Google Scholar]
- 18.Mabashar H, Almushait M, Sukit B, Shaamash A. Knowledge, attitude and practice of contraceptives among Saudi Women in Aseer Region, Saudi Arabia. Bangladesh J Med Sci. 2016;15:430–434. doi: 10.3329/bjms [DOI] [Google Scholar]
- 19.Słopień R, Milewska E, Rynio P, Męczekalski B. Use of oral contraceptives for management of acne vulgaris and hirsutism in women of reproductive and late reproductive age. Prz Menopauzalny. 2018;17:1–4. doi: 10.5114/pm.2018.74895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.[Internet]. Bestpractice-bmj-com.sdl.idm.oclc.org; 2021. [cited 21 March 2021]. Available from: https://bestpractice-bmj-com.sdl.idm.oclc.org/topics/en-gb/141/treatment-algorithm#. Accessed April 29, 2022.
- 21.Moreno M. Premenstrual syndrome: practice essentials, pathophysiology and etiology, epidemiology. Medscape; 2021. Available from: https://emedicine.medscape.com/article/953696-overview. Accessed March 20, 2021. [Google Scholar]
- 22.[Internet]. Bestpractice-bmj-com.sdl.idm.oclc.org; 2021. [cited 23 March 2021]. Available from: https://bestpractice-bmj-com.sdl.idm.oclc.org/topics/en-gb/419/management-approach. Accessed April 29, 2022.
- 23.Allais G, Gabellari IC, De Lorenzo C, Mana O, Benedetto C Oral contraceptives in migraine. Medscape; 2021. Available from: https://www.medscape.com/viewarticle/589439. Accessed March 23, 2021. [Google Scholar]
- 24.Evans N, Ratchford E. The swollen leg. Vasc Med. 2016;21(6):562–564. doi: 10.1177/1358863X16672576 [DOI] [PubMed] [Google Scholar]
- 25.Almegren M, Eid AB, Alsuhaibani E, et al. Awareness about venous thromboembolism among Saudi female who use oral contraceptive pills: a descriptive cross-sectional study. Int J Med Sci Diag Res. 2021;5. doi: 10.32553/ijmsdrV5i1.750 [DOI] [Google Scholar]
- 26.Mørch L, Skovlund C, Hannaford P, Iversen L, Fielding S, Lidegaard Ø. Contemporary hormonal contraception and the risk of breast cancer. N Engl J Med. 2017;377(23):2228–2239. doi: 10.1056/NEJMoa1700732 [DOI] [PubMed] [Google Scholar]
- 27.Parveen N, AlShammari BH, AlRashedy LA, AlRashed ALBF, Alarjawe TAS, AlDuhaim MS. Contraceptive awareness in reproductive aged Saudi women of Hail region. Saudi Med J. 2017. doi: 10.21276/sjm.2017.2.2.6 [DOI] [Google Scholar]
- 28.Stover J, Ross J. How increased contraceptive use has reduced maternal mortality. Matern Child Health J. 2009;14:687–695. doi: 10.1007/s10995-009-0505-y [DOI] [PubMed] [Google Scholar]