Abstract
Background
Although there is a low incidence of shoulder instability in women, this population is still representative and is often associated with lower rates of return to sports. Few studies have evaluated the results of the Latarjet procedure in this population.
Methods
This was a prospective cohort study of female athletes who underwent the Latarjet procedure between 2013 and 2018. The participants were followed up for 3 years. The primary outcomes of the study included the visual analog scale for pain; range of motion: active elevation, passive elevation, active external rotation, and passive external rotation. The functional scores were as follows: American Shoulder and Elbow Surgeons score, the Western Ontario Shoulder Instability Index, and the Athletic Shoulder Outcome Rating Scale. Additional data were collected regarding return to sport, complication rates, and patient satisfaction.
Results
Thirteen female athletes who practice Soccer, Volleyball, Basketball, Handball, Judo, or Weight training were evaluated. There was a significant reduction in the mean range of motion for all movements at 4 weeks after surgery. Patients recovered a range of motion similar to the preoperative values after 6 months. The mean visual analog scale reached 6.39 at the first week after surgery and decreased to values below preop at 8 weeks. The mean preoperative Western Ontario Shoulder Instability Index was 126.77 (min 118; max 135), and at the end of follow-up, the WOSI index was 45.08 (min 37; max 65; P < .05). The mean preoperative American Shoulder and Elbow Surgeons score was 41.61 (min 35; max 46), and at the end of follow-up, the mean ASES score was 84.46 (min 80; max 90; P < .05). The mean Athletic Shoulder Outcome Rating Scale in the preoperative period was 39.38 (min 37; max 42), and at the end of follow-up, the mean ASORS score was 83.15 (min 77; max 85; P < .05). The rate of return to sports was 92.3%, and 84.6% of patients were satisfied with the surgery. The aesthetic satisfaction rate was 76.9%. The complication rate was 15.4% (1 screw failure and 1 dislocation recurrence).
Conclusion
Latarjet surgery in female athletes showed high rates of return to sports and improved functional scores without impairing range of motion after the procedure. Recurrence and complication rates were low. In addition, treatment was associated with improved functionality and patient satisfaction.
Keywords: Latarjet, Athletes, Female, Shoulder injury, Shoulder dislocation, Shoulder instability, Shoulder pain, Sports
The Latarjet technique is a well-established surgery for the treatment of shoulder instability in athletes, performed in the setting of glenoid bone loss with good to excellent functional results.12 It proved to be an effective technique to prevent recurrent dislocations while allowing fast recovery and return to sports.1,7 Nevertheless, there are epidemiological and prognostic differences between female and male orthopedic patients.16,23 These variations can be attributed to anatomical, hormonal, and genetic factors.29
It is known that women have a lower incidence of shoulder dislocation than men (approximately 20%) and a higher incidence of complications after the Latarjet procedure.14,21,27 The average age of primary dislocation and surgery is generally higher in women than in men.23,24 Although there is a low incidence of shoulder instability in women, this population is still representative and is often associated with lower rates of return to sports.19 Few studies have evaluated the results of Latarjet surgery in female athletes.
This prospective study aimed to assess and evaluate the results of Latarjet surgery in female athletes regarding their return to sports, shoulder function and range of motion, pain scores, surgical wound aesthetics, and overall satisfaction. The participants were followed up for 3 years at a large Brazilian center of sports traumatology.
Materials and methods
This prospective cohort study was carried out between 2013 and 2018 at a large sports traumatology center in Brazil and analyzed female athletes with anterior shoulder instability treated with the Latarjet procedure for shoulder stabilization. The study was approved by the Research Ethics Committee under registration 57674116.9.0000.5505.
Study population
Female patients with anterior shoulder instability were clinically and radiographically evaluated at our clinic. Radiography and computerized tomography were used to identify and measure bone defects. Ultrasound examination was used to diagnose tendinous injuries. Patients with the following criteria were included: female athletes, regardless of the intensity of sports practice or type of sport, over 15 years old, diagnosed with anterior shoulder instability and 10–20% glenoid bone loss or off-track lesion. Participants with ligamentous laxity (Beighton Score higher or equal 4), any other shoulder lesion, or who had undergone previous surgical treatment of the shoulder, and those who did not agree with the informed consent form were excluded. Participants were consecutively included in the study as new cases of shoulder instability appeared at our sports trauma center.
Surgical technique and rehabilitation
The Latarjet procedure was performed by the experienced shoulder and elbow surgeons in patients with a high risk of recurrence, such as in younger patients, professional or contact sport athletes, and in the presence of associated bone lesions.2,12 Patients were placed in a beach chair position under general anesthesia and brachial plexus block. Access to the coracoid process was made through the deltopectoral interval with a 5 cm anterior skin incision. Blunt dissection, exposure, and osteotomy of the coracoid were performed, preserving the conjoint tendon after the release of the pectoralis minor and the coracoacromial ligament. For accessing the glenohumeral joint, the subscapularis muscle was opened longitudinally between the upper two-thirds and the lower one-third of its fibers, and the articular capsule was opened vertically near the glenoid. After cleaning the glenoid defect, the bone graft was fixed vertically on the anterior rim of the glenoid, with its tip facing down, with 2 parallel screws (3.5 mm diameter) and a washer placed with the superior screw. The graft and screw positions were verified using fluoroscopy after fixation. We did not repair the capsule to the coracoacromial ligament using the Latarjet technique.
After surgery, the patients were immobilized with a simple sling and were discharged as soon as they were awakened from general anesthesia. Pain pills and antibiotics were prescribed for 1 week. Patients were kept with sling immobilization for 4 weeks, and then physiotherapy was initiated for a progressive gain of range of motion. Strength exercises were initiated 12 weeks after surgery, and gradual return to sport was allowed after 4 months if the patient had no complaints.
Data gathering and outcomes
Data were collected during preoperative and postoperative consultations (1st, 2nd, 4th, 8th, 12th weeks, 6 months, and 1st, 2nd, and 3rd years).
The following demographic characteristics were analyzed: age, body mass index (BMI), dominant limb, injured limb, sport experience, sport played, type of sport (contact or overhead), and athlete category (professional or amateur). Participants whose main income was from sports practice were considered professional players.
The outcomes evaluated were: range of motion—active elevation (AEL), passive elevation (PEL), active external rotation (AER), passive external rotation (PER), and the visual analog scale (VAS) for pain. The following functional scales were also used to evaluate outcomes: American Shoulder and Elbow Surgeons score (ASES), Western Ontario Shoulder Instability Index (WOSI), and Athletic Shoulder Outcome Rating Scale (ASORS). Finally, return to sport, the occurrence of complications, recurrence of dislocations, patient satisfaction with the surgery, and aesthetic results were also included as outcome evaluation measures. Return to the sport was defined as the return to the same physical activity regardless of the level of practice through the 3 years of follow-up. Patient satisfaction was assessed by asking, ‘Would you do this procedure again?’ and aesthetic satisfaction was assessed by asking, ‘Were you satisfied with the surgery aesthetics? Yes, or no?’.
Statistical analysis
For statistical analysis, we used nonparametric tests because of the non-normality of the variables. Descriptive statistical analysis was performed using Excel 2016 (Microsoft Corporation, Redmond, WA, USA), and STATA 17 (Timberlake Consultants Limited, London, England) was used for statistical inference. The Mann–Whitney U test was used for quantitative variables, and the chi-square test was used for qualitative variables. Differences with values of P < .05 were considered statistically significant.
Results
A total of 13 female patients were included in this study, with a mean age of 29.23 ± 9.47 years (min 15 years; max 46 years) and mean BMI of 24.56 ± 2.64 kg/m2 (min 21.90 kg/m2; max 28.05 kg/m2), all patients reported to have no comorbidities. Nine (69.23%) shoulders were operated on the right side, and the lesion was on the dominant side in 69.23% of cases (n = 9). Three participants (23.07%) were professional athletes, while the other participants were amateur athletes. The average time of sports practice was 176.07 months (min 48; max 400). One hundred percent of the injuries were traumatic. Regarding the type of sport, 4 patients practiced weight training exclusively (30.77%), 3 practiced handball (23.07%), 2 played soccer (15.38%), 1 played volleyball (7.69%), and 1 patient practiced basketball and beach volleyball (7.69%). Sports such as handball, basketball, and judo were considered overhead and contact, volleyball and weight training were considered as overhead and noncontact, and soccer was considered as nonoverhead and contact. The characteristics of the sample are summarized in Table I.
Table I.
General characteristics of participants.
| Characteristic | Mean ± STD | Max | Min | |||
|---|---|---|---|---|---|---|
| Age | 29.23 ± 9.47 | 46 | 15 | |||
| Body mass index (BMI) (kg/m2) | 24.56 ± 2.64 | 28.05 | 21.9 | |||
| Experience (months) | 176.07 ± 120.67 |
400 |
48 |
|||
| Right (%) |
Left (%) |
|||||
| Dominant member | 13 (100%) |
0 (0%) |
||||
| Injured member | 9 (69.23%) |
4 (30.77%) |
||||
| Professional |
Amateur |
|||||
| Category | 3 (23.07%) |
10 (76.92%) |
||||
| Sport type | Nonoverhead and contact |
Overhead and contact |
Overhead noncontact |
|||
| 2 (15.38%) |
5 (38.46%) |
6 (46.15%) |
||||
| Sport | Weight training |
Handball |
Volleyball |
Soccer |
Judo |
Basketball and volleyball∗ |
| 4 (30.77%) | 3 (23.07%) | 2 (15.38%) | 2 (15.38%) | 1 (7.69%) | 1 (7.69%) | |
SD, standard deviation.
The overhead and contact sport (basketball) were considered for sport type classification.
Range of motion
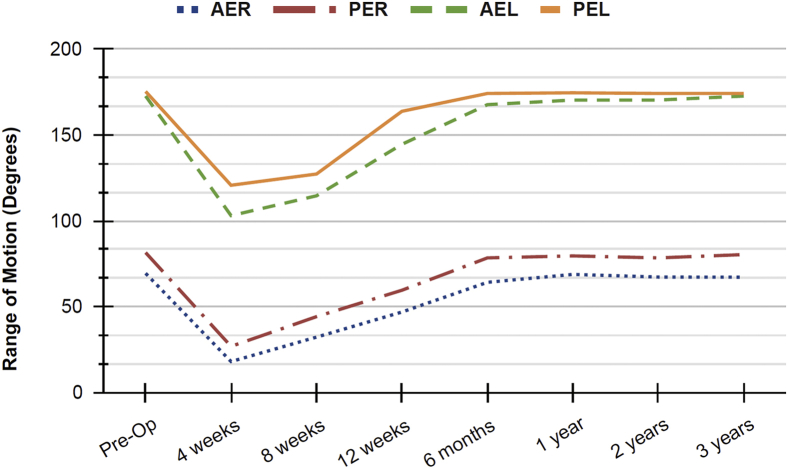
The preoperative mean range of motion according to each functional scale was: AER = 69.46 (min 60; max 80), PER = 81.53 (min 75; max 85), AEL = 172.69 (min 165; max 180), and PEL = 175.38 (min 165; max 180). There was no statistical difference between the preoperative range of motion or at the 6-month, 1-year, 2-year, and 3-year postoperative follow-up (P = 1.000).
In the fourth week of postoperative follow-up, when patients were allowed to remove the sling and begin physiotherapy, the average range of motion was: AER = 8.07 (min 10; max 25), PER = 26.92 (min 20; max 40), AEL = 103.07 (min 90; max 115), and PEL = 120.77 (min 110; max 130). The preoperative range of motion was significantly reduced for all movements compared to the fourth week after surgery (P < .05).
At 6 months of postoperative follow-up, the average range of motion was: AER = 64.23 (min 55; max 75), PER = 78.46 (min 75; max 85), AEL = 167.69 (min: 155; max 175), and PEL = 174.23 (min 165; max 180). The range of motion at 6 months postoperation compared with that at 4 weeks postoperation increased significantly for all movements (P < .05).
At the end of the 3-year follow-up period, the average range of motion was: AER = 64.23 (min 55; max 75), PER = 78.46 (min 75; max 85), AEL = 167.69 (min 155; max 175), PEL = 174.23 (min165; max 180). The evolution of range of motion throughout the follow-up period is shown in Table II and Figure 1.
Table II.
Range of motion.
| Follow-up | Active external rotation |
Passive external rotation |
Active elevation |
Passive elevation |
||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | P value | Mean ± SD | P value | Mean ± SD | P value | Mean ± SD | P value | |
| Pre Op | 69.46 ± 6.16 | - | 81.53 ± 3.15 | - | 172.69 ± 4.84 | - | 175.38 ± 5.19 | - |
| 4 weeks | 18.07 ± 5.96 | .000∗ | 26.92 ± 6.63 | .000∗ | 103.07 ± 7.23 | .000∗ | 120.76 ± 5.34 | .000∗ |
| 8 weeks | 32.30 ± 7.53 | .000∗ | 44.23 ± 3.44 | .000∗ | 114.61 ± 6.91 | .000∗ | 127.30 ± 6.96 | .000∗ |
| 12 weeks | 46.92 ± 4.80 | .025∗ | 59.61 ± 4.77 | .016∗ | 144.61 ± 7.76 | .016∗ | 163.84 ± 7.12 | .010∗ |
| 6 months | 64.23 ± 6.07 | 1.000 | 78.46 ± 3.76 | 1.000 | 167.69 ± 5.25 | 1.000 | 174.23 ± 4.49 | 1.000 |
| 1 year | 68.84 ± 6.18 | 1.000 | 79.61 ± 3.80 | 1.000 | 170.38 ± 5.94 | 1.000 | 174.61 ± 3.80 | 1.000 |
| 2 years | 67.30 ± 6.96 | 1.000 | 78.46 ± 5.16 | 1.000 | 170.38 ± 5.58 | 1.000 | 174.23 ± 4.00 | 1.000 |
| 3 years | 67.23 + 14.34 | 1.000 | 80.38 ± 5.19 | 1.000 | 172.69 ± 3.88 | 1.000 | 174.23 ± 4.00 | 1.000 |
SD, standard deviation.
Data is represented in degrees. (∗) Statistically significant values.
Figure 1.
Range of motion variation through time: Active External Rotation, Passive External Rotation, Active Elevation, Passive Elevation. Data are expressed in degrees.
Functional and pain scores
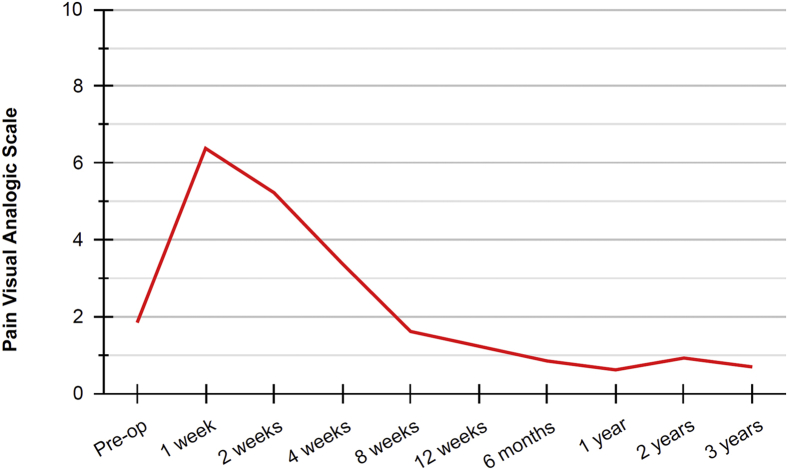
The mean preoperative VAS for pain was 1.84 (min 0; max 4); in the 1st postoperative week there was an increase in the mean VAS to 6.38 (min 3; max 8) with P = .003. In the 8th week, there was a reduction to the average VAS to 1.62 (min 1; max 4) with P = 1.000; at the end of follow-up at 3 years, the mean VAS for pain was 0.69 (max 2; min 0) with P = 1.00. At 8 weeks of follow-up, participants reached a mean pain score lower than the preoperative VAS; however, the difference was not statistically significant (P = 1.000). Figure 2 illustrates the pain over time.
Figure 2.
Evolution of pain, according to the Visual Analogue Scale for pain throughout the postoperative follow-up.
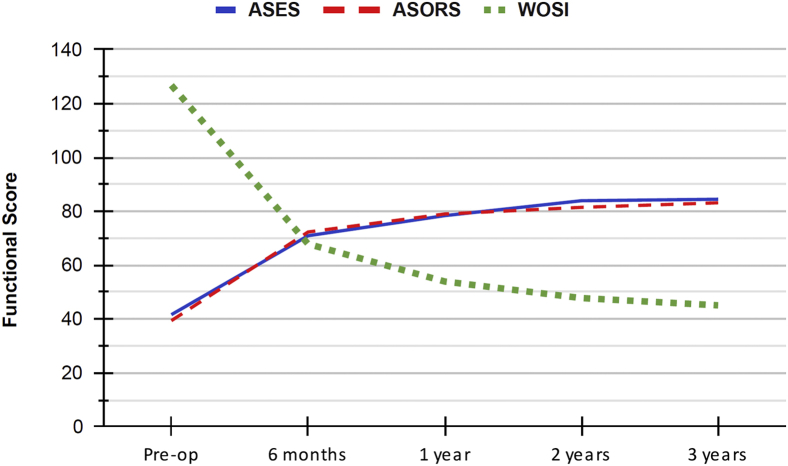
The mean preoperative ASES value was 41.61 (min 35; max 46) and at the end of follow-up was 84.46 (min 80; max 90). The mean value of the ASORS preoperatively was 39.38 (min 37; max 42) and at the end of follow-up was 83.15 (min 77; max 85). The WOSI score ranges from 0 to 210, with 0 representing the best possible response in terms of function and stability.15 The mean preoperative WOSI value was 126.77 (min 118; max 135) and at the end of follow-up was 45.08 (min 37; max 65). The evolution of functional scores over time is shown in Figure 3 and Table III.
Figure 3.
Evolution of scores in the American Shoulder and Elbow Surgeons score (ASES), Athletic Shoulder Outcome Rating Scale (ASORS), and Western Ontario Shoulder Instability (WOSI) Index functional scores throughout the postoperative follow-up.
Table III.
Evolution of functional and pain scores during follow-up, P values considered preop measures for comparison (∗) of statistically significant values.
| Follow-up | VAS |
ASES |
ASORS |
WOSI |
||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | P value | Mean ± SD | P value | Mean ± SD | P value | Mean ± SD | P value | |
| Preop | 1.84 ± 1.14 | - | 41.61 ± 2.99 | - | 39.38 ± 1.76 | - | 126.76 ± 5.37 | - |
| 1 week | 6.38 ± 1.66 | .003∗ | NA | NA | NA | NA | NA | NA |
| 2 weeks | 5.23 ± 1.48 | .084 | NA | NA | NA | NA | NA | NA |
| 4 weeks | 3.38 ± 1.33 | 1.000 | NA | NA | NA | NA | NA | NA |
| 8 weeks | 1.61 ± 0.87 | 1.000 | NA | NA | NA | NA | NA | NA |
| 12 weeks | 1.23 ± 1.17 | 1.000 | NA | NA | NA | NA | NA | NA |
| 6 months | 0.84 ± 0.80 | 1.000 | 70.92 ± 1.80 | 1.000 | 72.30 ± 2.50 | 1.000 | 67.84 ± 4.79 | .699 |
| 1 year | 0.61 ± 0.65 | 1.000 | 78.38 ± 2.33 | .013∗ | 79.00 ± 3.08 | .005∗ | 53.92 ± 5.33 | .290 |
| 2 years | 0.92 ± 0.64 | 1.000 | 83.92 ± 2.90 | .000∗ | 81.46 ± 2.82 | .000∗ | 47.76 ± 6.70 | .000∗ |
| 3 years | 0.69 ± 0.63 | 1.000 | 84.46 ± 2.60 | .000∗ | 83.15 ± 2.19 | .000∗ | 45.07 ± 7.30 | .000∗ |
VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons; ASORS, Athletic Shoulder Outcome Rating Scale; WOSI, Western Ontario Shoulder Instability Index; SD, standard deviation.
Return to sport, satisfaction, and complications
Lower WOSI scores, after 3 years of follow-up, were related to return to sport (P = .026) and surgical satisfaction (P = .026). Only 1 patient (7.69%) did not return to sport because of pain in the operated shoulder. The patient was a 16-year-old amateur handball athlete with the shortest experience. The patient’s preoperative pain assessment scores at 1 week and 3 years were 3.8 (worst) and 2 (worst), respectively; ASES preop and at 3 years were 43 and 80 (worst); ASORS preop and at 3 years were 39 and 77 (worst); WOSI preop and at 3 years were 135 and 65 (worst).
Three athletes (23.07%) returned to their sport at a lower level of performance than preinjury, and 2 of them (15.38%) had postoperative complications: 1 screw failure, which did not require revision, and 1 recurrence of dislocation, the only 1 in the sample, which required revision with the Eden-Hybinette procedure. The other nine athletes (69.23%) returned to the sport at the same preinjury level. Regarding the modalities and return to sports activities, 75% (3:4) of the patients who practice weight training and 100% (1:1) of those who practice basketball returned to their preinjury level of performance. As for the participants who returned to the sport at a lower level, the modalities were Judo (1:1), Soccer (1:2), and Weight training (1:4). Only 1 patient who practiced handball did not return to the sport (1:3).
Two patients (15.38%) reported not being satisfied with the surgery; 1 of them needed a new surgical procedure due to dislocation, and the other did not return to the sport due to shoulder pain. Three patients (23.07%) were not satisfied with the postoperative aesthetics.
Discussion
The Latarjet procedure can be performed either arthroscopically or with open surgery and still efficiently treat shoulder instability in athletes who practice overhead and contact sports.4,5 Previous studies that evaluated postoperative results focused on male athletes or had a small population of female athletes.22,23 Although there is a lower incidence of shoulder instability in women, this population is still representative and is often associated with lower rates of return to sports.16,19,21,22 Studies with athletes of both sexes often have female participants who experience longer periods of complaints of pain after the procedure or those who never return to the practice of sports.9,25 However, this population is under-represented in the literature on orthopedic studies.22
In addition, the female population compared to that of males has a smaller coracoid that may compromise the ability of the Latarjet procedure to compensate for bone loss in female patients.24 This may compromise the Latarjet technique and favor the Bristow technique instead since it uses only 1 screw to fix the bone graft.24 To avoid complications related to the female anatomical characteristics, it is recommended to measure the coracoid size and graft prior to surgery.
Return to sports
A literature review by Hurley et al. reported that the mean time for the return to sports following the Latarjet procedure was 5.8 months with a minimum of 3.2 and a maximum of 8 months.14 They found that 74% of athletes returned to sports at the same level before shoulder injury. However, the review included studies of both sexes and did not make specific considerations for each sex. A previous study focused on female athletes had only a 37.5% rate of return to sport at the same level of performance.23 Our results showed that approximately 93% of the female athletes returned to sports after surgery and 69% at the same level of play. Most of our participants played overhead sports, and previous studies showed that this type of sport has a lower rate of return to the sport at the preinjury level.4,6,25 As for time to return to sports, we did not collect data, representing a limitation for this analysis.
Although our rate of return to sports at the same level is high, the disparity between mixed studies and those focused on our population is alarming. Hence, it is risky to generalize the results of Latarjet for men and women. Therefore, there is a need for future research to better understand the implications and results of Latarjet in female athletes.
Complications and reoperation
Despite the Latarjet procedure having good to excellent functional results, the surgery may result in complications such as screw breakage, recurrence of dislocation, nonunion, pseudarthrosis, osteolysis, and screw and graft malpositioning, which can lead to arthrosis and loss of external rotation.8,12 Nonunion or screw breakage is a complication that occurs in less than 5% of patients.12 In our study, 2 patients presented with recurrent subluxation or dislocation and screw breakage (approximately 15% of our sample). Complications related to the Latarjet procedure range from 25–31% in the literature.21,24
A retrospective study with modified Latarjet surgery in twenty-nine female patients reported a reoperation rate of 13.8%.21 Our findings had an approximately 7.7% reoperation rate due to recurrent dislocation, which is slightly higher than the rates found in the literature (studies of both sexes, between 1% and 7.5%).4,11,23 However, due to the shortage of studies focusing on female athletes or examining complication rates by sex, it is challenging to directly compare results.23,24
Range of motion
The preoperative range of motion was significantly reduced for all movements in the fourth week after surgery (P < .05). Since for this study, participants used a sling for 4 weeks, it reduced the range of movement at this period. In addition, the participants started physiotherapy after the removal of the sling and did not test the range of motion before. From the removal of the sling at 4 weeks until 6 months of follow-up, there was an increase in the range of motion, reaching values similar to the preoperative results (P < .05) for all measures.
Although the study protocol for sling removal and beginning of physiotherapy may vary, our results are compatible with those presented in the literature. Regardless of the particularities of female athletes, after the Latarjet procedure, participants may recover their range of motion to similar results before surgery.3,26,27
For active or passive elevation, participants experienced a variation of 5 degrees of gain or loss of range of motion. This result is compatible with previous studies that considered a loss of 5 degrees as a slight change in mobility.26 As for active or passive rotation, participants experienced a minimum of 5 degrees and a maximum of 15 degrees of movement gain or loss after Latarjet. In our study, five participants lost range of motion for active and passive rotation (min 5; max 15 degrees), and 7 participants increased their active rotation range (min 2; max 15 degrees). Likewise, Rosa et al. evaluated 26 patients with a follow-up of 38 months and observed that there was a limitation of mobility in the operated shoulder in all planes, especially in relation to movements of lateral rotation.26,27
Functional and pain scores
In our study, patients with the worst clinical results developed some complications. This has also been shown in other studies.13,23,24 For our sample, the participant with the worst VAS for pain, WOSI, ASORS, and ASES prior to surgery maintained the worst parameters until the last follow-up, 3 years later, in comparison with the rest of the sample.
Belangero and colleagues assessed the WOSI scores in a prospective randomized trial with athletes and found a mean of 122 (range 46–185) in the preoperative period and a mean of 52.6 (range 18–77) in their final follow-up period 2. Our results showed a mean of 126.76 (range 118–135) in the preoperative period and a mean of 45.07 (range 37–65) at the 3-year follow-up. The study conducted by Belangero et al. did not address the WOSI results for the female population in their trial. In comparison, in our study, participants started with a higher WOSI and ended the follow-up period with lower scores. The minimal clinically important differences for WOSI were achieved by 100% of our sample at 6-month follow-up and continued to decrease until the end of the follow-up for 23% of the athletes. We considered the results of a systematic review to establish the cut-off point of minimal clinically important difference of WOSI.18
Belangero et al. assessed the ASORS scores in a prospective randomized trial with athletes and found a mean of 39 in the preoperative period and a mean of 88 at a 3-year follow-up period.3 Their results are similar to those presented in our study, where the majority of patients had good to excellent scores, showing satisfactory results in this group of patients.
Chen and colleagues assessed the ASES scores at a five-year follow-up study to evaluate sex differences in clinical outcomes after arthroscopic Bankart procedure and found a mean of 89.8 in the follow-up period.9 Their study also found that most clinical outcomes of women were no worse than those of men. They did not collect data on the ASES before surgery. Magnuson and colleagues compared male and female athlete outcomes in patients undergoing shoulder instability, and female patients had a preoperative mean ASES of 56.9 19. They did not include athletes. Our results showed a mean of 41.61 in the preoperative period and a mean of 84.46 at the 3-year follow-up, and an increased ASES higher than the minimal clinically important difference of 6.4 points at the 6-month follow-up for all participants.20 For this, we considered the results of a systematic review to establish the cut-off point for minimal clinically important differences in ASES for shoulder instability.10,20
Aesthetics and surgery satisfaction
Aesthetic satisfaction after the Latarjet procedure has been discussed and analyzed over the past few years.19 The deltopectoral approach to the shoulder, located on an interneural plane between the musculocutaneous and axillary nerves, is the standard approach for the open Latarjet procedure.17,28 The incision leaves a scar at an exposed area of the body that may be related to lower aesthetic satisfaction, especially for young patients, or cicatrization complications such as keloids.28 This may explain the lower aesthetic satisfaction rate (76.9%) compared to the overall surgical satisfaction rate (84.6%).
An alternative for this was retrospectively evaluated by Vlajkovic et al. to increase patient satisfaction.28 The researchers drew the skin incision to a more vertical and medialized position so the scar can be covered by the bra strap in women; they called this the ‘bra strap incision’.28 In their study, they achieved an aesthetic satisfaction rate of 88.8%. The participants who were unsatisfied developed keloids or had a larger scar.28 This technique was not performed in our study but could be an alternative to increase aesthetic satisfaction in female patients. In addition, a more medial incision, such as the bra strap incision, could facilitate graft positioning and fixation. Surgery satisfaction is directly influenced by the occurrence of complications, reduced pain scores, or return to sports.28 In our study, most athletes reported that they would undergo surgery again.
Strengths and limitations
This is a single-center study to approach a population that is already less affected by shoulder instability; hence, the limitation of achieving a larger sample size. In addition, return to sports was not assessed over time, thus limiting the analysis. Although this study has limitations, it is one of the few investigations focusing exclusively on female athletes. The presented results bring awareness and pave the way for future studies on the theme of this representative population.
Conclusion
This prospective study successfully evaluated the results of Latarjet surgery in female athletes after 3 years of follow-up. The Latarjet surgery in female athletes showed high rates of return to sports, with no significant impairment of range of motion after the procedure. In addition, treatment was associated with improved functionality scores, pain reduction, high rates of return to a sport at the same level of performance, and lower complication rates. We observed a lower aesthetic satisfaction rate compared to overall surgical satisfaction, probably due to the scar location.
Disclaimers:
Funding: The study did not receive any funding or grants from private or public institutions. The institutions with which the authors are affiliated provided support in the form of salaries for all authors but did not have any additional role in the study design, data collection or analysis, decision to publish, or the preparation of the manuscript.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
The study was approved by the Research Ethics Committee from the São Paulo Hospital and the Federal University of São Paulo under the number 57674116.9.0000.5505. CEP-UNIFESP, NUMBER 2.749.030.
References
- 1.An V.V.G., Sivakumar B.S., Phan K., Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016;25:853–863. doi: 10.1016/j.jse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Balg F., Boileau P. The instability severity index score a simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. 2007;89:1470–1477. doi: 10.1302/0301-620X.89B11. [DOI] [PubMed] [Google Scholar]
- 3.Belangero P.S., Lara P.H.S., Figueiredo E.A., Andreoli C.V., de Castro Pochini A., Ejnisman B., et al. Bristow versus Latarjet in high-demand athletes with anterior shoulder instability: a prospective randomized comparison. JSES Int. 2021;5:165–170. doi: 10.1016/j.jseint.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beranger J.S., Klouche S., Bauer T., Demoures T., Hardy P. Anterior shoulder stabilization by Bristow–Latarjet procedure in athletes: return-to-sport and functional outcomes at minimum 2-year follow-up. Eur J Orthopaedic Surg Traumatol. 2016;26:277–282. doi: 10.1007/s00590-016-1751-5. [DOI] [PubMed] [Google Scholar]
- 5.Bradley H., Lacheta L., Goldenberg B.T., Rosenberg S.I., Provencher M.T., Millett P.J. Latarjet procedure for the treatment of anterior glenohumeral instability in the athlete - Key considerations for Rehabilitation. Int J Sports Phys Ther. 2021;16:259–269. doi: 10.26603/001c.18707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buckup J., Sternberg C., Smolen D., Leuzinger J. Functional outcome and return to sports after the arthroscopic Latarjet procedure in young and physically active patients. Arch Orthopaedic Trauma Surg. 2020;140 doi: 10.1007/s00402-020-03513-4. [DOI] [PubMed] [Google Scholar]
- 7.Cerciello S., Corona K., Morris B.J., Santagada D.A., Maccauro G. Early outcomes and Perioperative complications of the arthroscopic Latarjet procedure: systematic review and meta-analysis. Am J Sports Med. 2018;47:2232–2241. doi: 10.1177/0363546518783743. [DOI] [PubMed] [Google Scholar]
- 8.Cerciello S., Edwards T.B., Walch G. Chronic anterior glenohumeral instability in soccer players: results for a series of 28 shoulders treated with the Latarjet procedure. J Orthopaedics Traumatol. 2012;13:197–202. doi: 10.1007/s10195-012-0201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen M., Feng S., Chen Y., Ding Z., Xie Y., Chen J., et al. Sex-Based differences in clinical outcomes after arthroscopic anterior shoulder stabilization: results at 5-year follow-up. Orthopaedic J Sports Med. 2021;9 doi: 10.1177/23259671211008841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dabija D.I., Jain N.B. Minimal clinically important difference of shoulder outcome measures and diagnoses: a systematic review. Am J Phys Med Rehabil. 2019;98:671–676. doi: 10.1097/PHM.0000000000001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griesser M.J., Harris J.D., McCoy B.W., Hussain W.M., Jones M.H., Bishop J.Y., et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22:286–292. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Gupta A., Delaney R., Petkin K., Lafosse L. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med. 2015;8:59–66. doi: 10.1007/s12178-015-9258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hovelius L., Sandström B., Olofsson A., Svensson O., Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): Long-term follow-up in 319 shoulders. J Shoulder Elbow Surg. 2012;21:647–660. doi: 10.1016/j.jse.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 14.Hurley E.T., Montgomery C., Jamal M.S., Shimozono Y., Ali Z., Pauzenberger L., et al. Return to Play after the Latarjet procedure for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47:3002–3008. doi: 10.1177/0363546519831005. [DOI] [PubMed] [Google Scholar]
- 15.Kirkley A., Griffin S., Dainty K. Scoring Systems for the functional assessment of the shoulder. Arthroscopy. 2003;19:1109–1120. doi: 10.1016/j.arthro.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 16.Kraeutler M.J., McCarty E.C., Belk J.W., Wolf B.R., Hettrich C.M., Ortiz S.F., et al. Descriptive Epidemiology of the MOON shoulder instability cohort. Am J Sports Med. 2018;46:1064–1069. doi: 10.1177/0363546518755752. [DOI] [PubMed] [Google Scholar]
- 17.Kumar S. Surgical exposures in orthopedics: the anatomic approach. Indian J Orthop. 2010;44:233. [Google Scholar]
- 18.van der Linde J.A., van Kampen D.A., WAH van Beers L., van Deurzen D.F., Daniël Saris prof B., Terwee C.B. TITLE PAGE 1 the Responsiveness and minimal important change (MIC) of the Western Ontario shoulder instability index (WOSI) and Oxford shoulder instability score. J Orthop Sports Phys Ther. 2017;47:402–410. doi: 10.2519/jospt.2017.6548. [DOI] [PubMed] [Google Scholar]
- 19.Magnuson J.A., Wolf B.R., Cronin K.J., Jacobs C.A., Ortiz S.F., Bishop J.Y., et al. Sex-related differences in patients undergoing surgery for shoulder instability: a Multicenter Orthopaedic Outcomes Network (MOON)Shoulder Instability cohort study. J Shoulder Elbow Surg. 2019;28:1013–1021. doi: 10.1016/j.jse.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 20.Michener L.A., McClure P.W., Sennett B.J. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment form, patient self-report section: Reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–594. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 21.Owens B.D., Agel J., Mountcastle S.B., Cameron K.L., Nelson B.J. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37:1750–1754. doi: 10.1177/0363546509334591. [DOI] [PubMed] [Google Scholar]
- 22.Patzkowski J.C., Dickens J.F., Cameron K.L., Bokshan S.L., Garcia E.S.J., Owens B.D. Pathoanatomy of shoulder instability in collegiate female athletes. Am J Sports Med. 2019;47:1909–1914. doi: 10.1177/0363546519850810. [DOI] [PubMed] [Google Scholar]
- 23.du Plessis J.P., Dachs R.P., Vrettos B.C., Maasdorp D., Oliver J.M.A., Curtis S.C., et al. The modified Latarjet procedure in female patients: clinical outcomes and complications. J Shoulder Elbow Surg. 2018;27:e9–e15. doi: 10.1016/j.jse.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 24.du Plessis J.P., Dey R., Dachs R., de Wet T.J., Trevor T., Carrara H., et al. A gender-based comparison of coracoid and glenoid anatomy: CT analysis and discussion of potential impact on the Latarjet procedure. J Shoulder Elbow Surg. 2021;30:1503–1510. doi: 10.1016/j.jse.2020.09.039. [DOI] [PubMed] [Google Scholar]
- 25.Privitera D.M., Sinz N.J., Miller L.R., Siegel E.J., Solberg M.J., Daniels S.D., et al. Clinical outcomes following the Latarjet procedure in contact and collision athletes. J Bone Joint Surg Am Vol. 2018;100:459–465. doi: 10.2106/JBJS.17.00566. [DOI] [PubMed] [Google Scholar]
- 26.Rosa J.R.P., Checchia C.S., Miyazaki A.N. Instabilidade anterior traumática do ombro. Revista Brasileira de Ortopedia. 2017;52:513–520. doi: 10.1016/j.rbo.2017.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.da Silva L.A., da Costa Lima Á.G., Kautsky R.M., Santos P.D., do Val Sella G., Checchia S.L. Evaluation of the results and complications of the Latarjet procedure for recurrent anterior dislocation of the shoulder. Revista Brasileira de Ortopedia (English Edition) 2015;50:652–659. doi: 10.1016/j.rboe.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vlajkovic A., Meyer D.C., von Knoch M., Schmid S.L., Götschi T., Grubhofer F. The bra strap incision in the open Latarjet procedure. J Orthopaedic Surg Res. 2018;13 doi: 10.1186/s13018-018-1006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolf J.M., Cannada L., van Heest A.E., O’Connor M.I., Ladd A.L. Male and female differences in musculoskeletal disease. J Am Acad Orthopaedic Surgeons. 2015;23:339–347. doi: 10.5435/JAAOS-D-14-00020. [DOI] [PubMed] [Google Scholar]