Abstract
A 77-year-old man underwent radiofrequency catheter ablation of incessant ventricular arrhythmias (VAs) originating from the right ventricular (RV) moderator band (MB). Activation mapping during the VAs exhibited a centrifugal pattern with the earliest activation site (EAS) on the RV septum. A local impedance (LI)-guided radiofrequency application targeting the EAS with a maximum power output of 50W successfully eliminated the VAs and resulted in an LI drop of up to 35 Ω. Late gadolinium enhancement magnetic resonance imaging (LGE-MRI) on the day after the ablation procedure demonstrated a confluent non-enhanced dark core on the RV septal portion of the MB. On the LGE-MRI two months after the procedure, the dark core region became contracted and instead the peripheral region surrounding the dark core exhibited a bright enhancement. The size of the dark core and peripheral enhanced regions on the LGE-MRI remained almost unchanged two months to two years after the procedure. He had no VA recurrences during a two-year follow-up period. Previous LGE-MRI studies reported that an ablated area within healthy ventricular myocardium exhibits a bright homogenous enhancement during the post-ablation chronic phase, while that within ventricular scar tissue exhibits a confluent non-enhanced dark core. This case suggested the presence of a dark core with a peripheral enhancement corresponding to the ablated area within the healthy myocardium of the RV-MB. LGE-MRI may be useful for accurately detecting RF ablation lesions on the RV-MB and visualizing the serial changes in the LGE-MRI characteristics from the post-ablation acute to chronic phases.
Keywords: Confluent non-enhanced dark core, High-resolution mapping, Moderator band, Radiofrequency catheter ablation, Ventricular tachycardia
1. Introduction
The moderator band (MB) in the right ventricle (RV) has been recognized as a source of idiopathic ventricular arrhythmias (VAs) [1]. Late gadolinium enhancement (LGE) sequences of cardiac magnetic resonance imaging (MRI) can detect acute and chronic radiofrequency (RF) ablation lesions. Previous LGE-MRI studies reported that an ablated area within healthy ventricular myocardium exhibits a bright homogenous enhancement in the post-ablation chronic phase, while that within ventricular scar tissue exhibits a confluent non-enhanced dark core [[2], [3], [4], [5], [6], [7]]. We present a case with a successful RF catheter ablation of VAs originating from the RV-MB, guided by a high-resolution electroanatomic mapping system (Rhythmia; Boston Scientific, Marlborough, MA). In the present case, LGE-MRI from the acute to subacute and chronic phases after the ablation procedure identified the RF ablation lesion as a confluent non-enhanced dark core with a peripheral bright enhancement on the RV-MB and visualized the serial changes in the LGE-MRI characteristics.
2. Case report
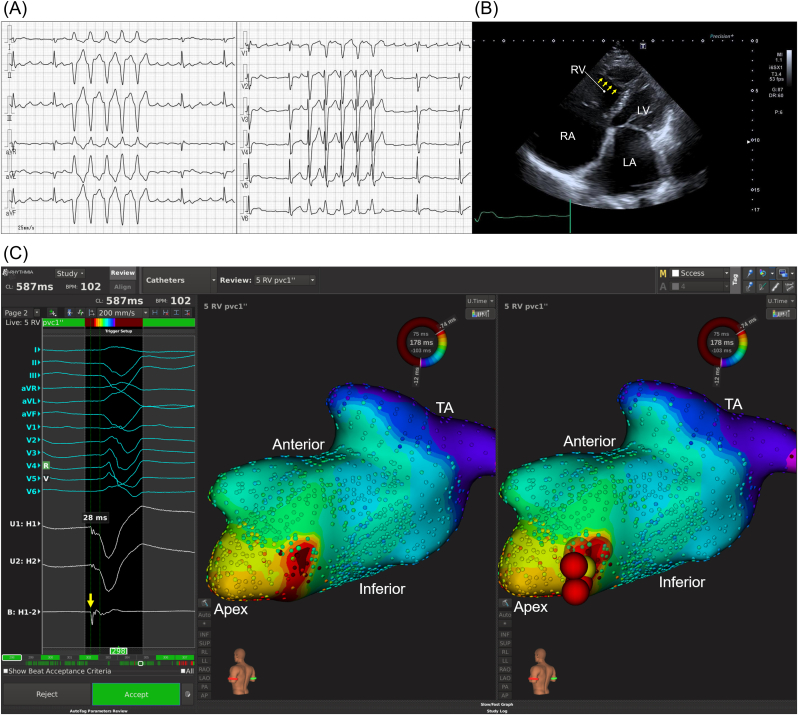
A 77-year-old man with persistent atrial fibrillation and flutter and a previous surgical closure of an atrial septal defect underwent RF catheter ablation of an incessant non-sustained ventricular tachycardia and ventricular premature contractions (VPCs) (Fig. 1A). Transthoracic echocardiography revealed the presence of the MB in the RV and absence of any structural ventricular abnormalities or intracardiac thrombi (Fig. 1B). Activation mapping during the clinical VPCs based on an automated electrogram annotation using the Rhythmia mapping system with a mini-basket catheter (IntellaMap Orion, Boston Scientific) exhibited a centrifugal pattern with the earliest activation site (EAS) on the RV septum, which was suspected to be located on the septal portion of the MB (Fig. 1C, Online Video). The local bipolar electrogram at the EAS during the VPCs preceded the QRS onset of the VPCs by 28 ms, and the unipolar electrogram exhibited a QS pattern. An RF application targeting the EAS, with a maximum power output of 50W and RF duration of 60 seconds using an irrigated ablation catheter capable of local impedance (LI) monitoring (IntellaNav MiFi OI, Boston Scientific), successfully eliminated the VAs and resulted in an LI drop of up to 35 Ω. Additional RF applications were performed around the EAS with an RF power output of 35–45W and LI drop of 22–37 Ω. Thereafter, none of the VAs could further be induced.
Fig. 1.
(A) Twelve-lead electrocardiograms of the non-sustained ventricular tachycardia. (B) Transthoracic echocardiography demonstrating the presence of an RV-MB (yellow arrows). (C) Activation maps during the VPCs demonstrating the earliest activation (dark red) on the RV septum in the left posterior view. The red and yellow tags on the maps represent the RF application sites and earliest activation site, respectively.
Abbreviations: LA, left atrium; LV, left ventricle; RA, right atrium; RV right ventricle; TA, tricuspid annulus.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ipej.2022.02.001
The following is the supplementary data related to this article:
Video 1Propagation maps during the VPCs in the left posterior (left panel) and left anterior (right panel) views.
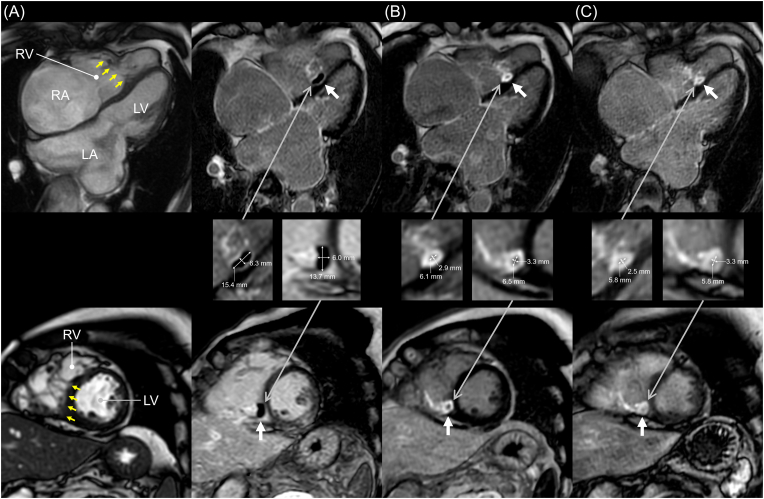
Cardiac MRI with a 1.5 T MR unit (Ingenia, Philips Medical Systems, Einthoven, The Netherland) was performed on the next day, two months, and two years after the ablation procedure. The scanning parameters of the LGE sequences were as follows: repetition time/echo time 4.7/2.3 ms, matrix 256 × 231, field of view 380 × 380 mm, slice thickness/gap 10/5 mm, and number of signals averaged 1. The LGE-MRI on the day after the procedure demonstrated a confluent non-enhanced dark core on the RV septal portion of the MB (Fig. 2A). On the LGE-MRI two months after the procedure, the dark core region became contracted and instead the peripheral region surrounding the dark core exhibited a bright enhancement (Fig. 2B). The size of the dark core and peripheral enhanced regions on the follow-up LGE-MRI remained almost unchanged two months to two years after the procedure (Fig. 2C). He had no VA recurrences during a two-year follow-up period.
Fig. 2.
(A) Cine MRI (left panels) and LGE-MRI (right panels) findings on the day after the ablation procedure, (B) LGE-MRI findings two months after, and (C) LGE-MRI findings two years after. The yellow and white arrows represent the RV-MB and a confluent non-enhanced dark core with a peripheral bright enhancement on the LGE-MRI, respectively. The major/minor diameters of the dark core regions were 15.4/6.3 mm in the four-chamber image (upper panel) and 13.7/6.0 mm in the short axial image (lower panel) in the acute phase after the ablation, 6.1/2.9 mm and 6.5/3.3 mm in the subacute phase, and 5.8/2.5 mm and 5.8/3.3 mm in the chronic phase, respectively.
3. Discussion
This was a case report describing the ablation lesion characteristics on the LGE-MRI in the acute, subacute, and chronic phases after an LI-guided RF catheter ablation of VAs originating from the RV-MB. A confluent non-enhanced dark core on the LGE-MRI was observed corresponding to the ablated area in the post-ablation acute phase, and a contracted dark core with a peripheral bright enhancement was observed in the post-ablation subacute and chronic phases.
Previous studies have reported that LGE-MRI can visualize acute RF ablation lesions in the ventricle as a microvascular obstruction (MVO) and chronic RF ablation lesions as a homogenous enhanced area [[2], [3], [4], [5], [6]]. Vunnam et al. suggested that an MVO on LGE-MRI transitions to a bright homogenous enhancement several weeks after RF ablation in normal ventricular myocardium [2]. On the other hand, Dabbagh et al. demonstrated that LGE-MRI months after a post-infarction VT ablation exhibits a confluent non-enhanced subendocardial dark core, corresponding to the prior ablation lesions, within post-infarction scar [7]. In general, an MVO has a transient appearance and transitions to a bright homogenous enhancement over time, while a confluent non-enhanced dark core is likely to present persistently due to permanent microvascular damage. The LGE-MRI characteristics in the present case were regarded as a confluent non-enhanced dark core rather than an MVO, because the central hypointense area still persisted for two years after the ablation procedure. Dabbagh et al. reported that dark core regions correspond to electrically unexcitable areas [7]. Thus, we speculated that both the dark core and peripheral enhanced regions represented the total ablated area during the ablation procedure, and the dark core region became contracted over time and finally represented dense unexcitable scar. However, it remains unclear whether the dark core only or both the dark core and peripheral enhanced regions represent effective RF lesions.
To the best of our knowledge, there have been few studies reporting the presence of a confluent non-enhanced dark core corresponding to an ablated area within healthy ventricular myocardium, not within ventricular scar tissue. When RF ablation is performed within scar tissue, probably hardly any blood flow can be supplied to the ablated area from its surroundings, which may result in permanent microvascular damage, that is, the occurrence of a dark core. On the other hand, when endocardial RF ablation is performed within healthy tissue, the blood flow can be supplied from its surroundings, such as blood flow from the intra-myocardium, which may lead to the absence of permanent microvascular damage. In the present case, the RF applications were performed intensively so as to surround the RV septal portion of the MB. That may have been why the ablated area within the healthy myocardium of the RV-MB exhibited a confluent non-enhanced dark core on the LGE-MRI. Further investigation of the LGE-MRI characteristics of the ablated areas within healthy ventricular myocardium from the post-ablation acute to chronic phases is needed.
LGE-MRI may be useful for accurately detecting RF ablation lesions on the RV-MB and visualizing the serial changes in the LGE-MRI characteristics from the post-ablation acute to chronic phases.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
No author has a real or perceived conflict of interest.
Acknowledgment
We would like to thank Mr. John Martin for his help in the preparation of the manuscript.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Sadek M.M., Benhayon D., Sureddi R., et al. Idiopathic ventricular arrhythmias originating from the moderator band: electrocardiographic characteristics and treatment by catheter ablation. Heart Rhythm. 2015;12:67–75. doi: 10.1016/j.hrthm.2014.08.029. [DOI] [PubMed] [Google Scholar]
- 2.Vunnam R., Maheshwari V., Jeudy J., et al. Ventricular arrhythmia ablation lesions detectability and temporal changes on cardiac magnetic resonance. Pacing Clin Electrophysiol. 2020;43:314–321. doi: 10.1111/pace.13886. [DOI] [PubMed] [Google Scholar]
- 3.Yamashita K., Kholmovski E., Ghafoori E., et al. Characterization of edema after cryo and radiofrequency ablations based on serial magnetic resonance imaging. J Cardiovasc Electrophysiol. 2019;30:255–262. doi: 10.1111/jce.13785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghafoori E., Kholmovski E.G., Thomas S., et al. Characterization of gadolinium contrast enhancement of radiofrequency ablation lesions in predicting edema and chronic lesion size. Circ Arrhythm Electrophysiol. 2017;10 doi: 10.1161/CIRCEP.117.005599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ilg K., Baman T.S., Gupta S.K., et al. Assessment of radiofrequency ablation lesions by CMR imaging after ablation of idiopathic ventricular arrhythmias. JACC Cardiovasc Imaging. 2010;3:278–285. doi: 10.1016/j.jcmg.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 6.Estornell-Erill J., Ridocci-Soriano F., Quesada-Dorador A., et al. Images in cardiology. Microvascular obstruction after radiofrequency ablation of ventricular tachycardia: comprehensive evaluation by magnetic resonance imaging and computed tomography. J Am Coll Cardiol. 2010;56:e25. doi: 10.1016/j.jacc.2009.11.107. [DOI] [PubMed] [Google Scholar]
- 7.Dabbagh G.S., Ghannam M., Siontis K.C., et al. Magnetic resonance mapping of catheter ablation lesions after post-infarction ventricular tachycardia ablation. JACC Cardiovasc Imaging. 2021;14:588–598. doi: 10.1016/j.jcmg.2020.08.041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1Propagation maps during the VPCs in the left posterior (left panel) and left anterior (right panel) views.