Abstract
Chemodynamic therapy (CDT) is considered as a promising modality for selective cancer therapy, which is realized via Fenton reaction-mediated decomposition of endogenous H2O2 to produce toxic hydroxyl radical (•OH) for tumor ablation. While extensive efforts have been made to develop CDT-based therapeutics, their in vivo efficacy is usually unsatisfactory due to poor catalytic activity limited by tumor microenvironment, such as anti-oxidative systems, insufficient H2O2, and mild acidity. To mitigate these issues, we have witnessed a surge in the development of CDT-based combinatorial nanomedicines with complementary or synergistic mechanisms for enhanced tumor therapy. By virtue of their bio-imaging capabilities, Fenton metal nanomedicines (FMNs) are equipped with intrinsic properties of imaging-guided tumor therapies. In this critical review, we summarize recent progress of this field, focusing on FMNs for imaging-guided combinatorial tumor therapy. First, various Fenton metals with inherent catalytic performances and imaging properties, including Fe, Cu and Mn, were introduced to illustrate their possible applications for tumor theranostics. Then, CDT-based combinatorial systems were reviewed by incorporating many other treatment means, including chemotherapy, photodynamic therapy (PDT), sonodynamic therapy (SDT), photothermal therapy (PTT), starvation therapy and immunotherapy. Next, various imaging approaches based on Fenton metals were presented in detail. Finally, challenges are discussed, and future prospects are speculated in the field to pave way for future developments.
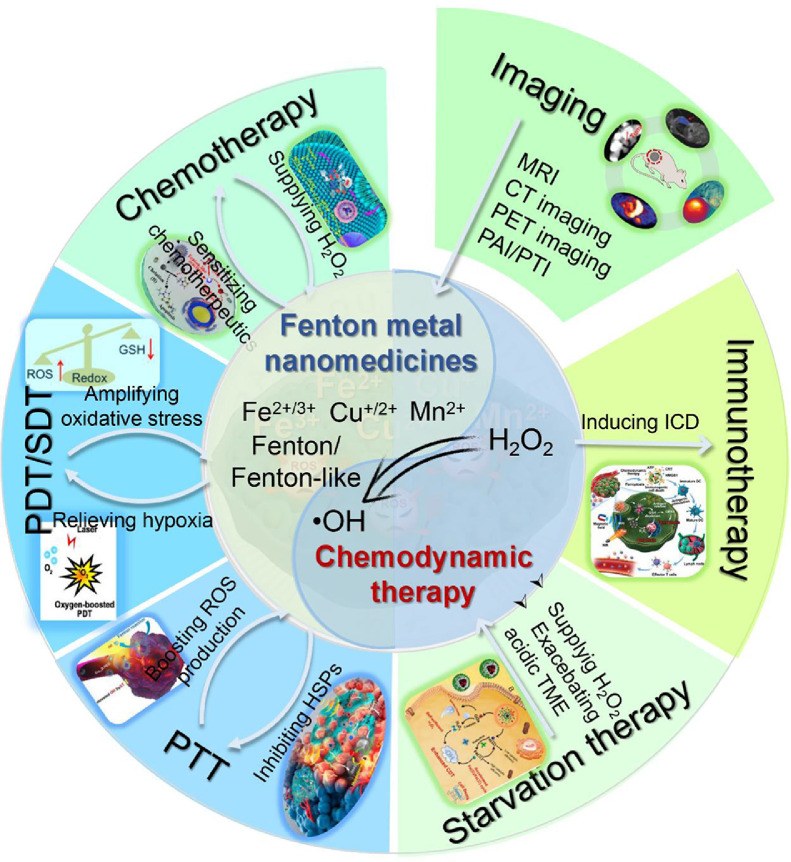
Graphical abstract

1. Introduction
Cancer, as one of the major causes of diseases-related death throughout the world, is severely threatening the human health [1]. Over the past few decades, extensive efforts have been made for the development of advanced treatment modalities to improve therapeutic outcomes, and chemotherapy, radiotherapy and surgery have become the standard-of-care for clinical cancer management [2], [3], [4]. However, these conventional treatment approaches often suffer from the risk of recurrence, treatment resistance, severe side effects and high-cost [5]. Alternatively, several novel therapeutic modalities based on energy conversion, such as photodynamic therapy (PDT), photothermal therapy (PTT) and sonodynamic therapy (SDT), have gained particular interest, showing great potential for tumor therapy [6,7]. For example, PDT employs photosensitizers to transfer oxygen molecules into singlet oxygen (1O2) upon light stimulation, thereby inducing cancer cell apoptosis and necrosis [8]. This light triggered therapy is advantageous for temporal- and spatial-controlled specificity with minimized side-effects, while its efficacy is often limited by tumor hypoxia, leading to low reactive oxygen species (ROS) generation efficiency. What's more, the oxygen consumption during photodynamic process would worsen the tumor microenvironment (TME) to further compromise treatment outcomes [9,10]. Similarly, the efficacy of PTT and SDT is usually limited by the poor tissue penetration of light[11] and tumor hypoxia [12], respectively.
In addition to hypoxia, TME is also pathologically characterized by high level of H2O2 [13,14], which can be used as an endogenous substance to generate toxic ROS in situ for selective tumor ablation with minimal harmfulness to normal tissues. With such purpose, chemodynamic therapy (CDT) has emerged as a promising therapeutic mean for its unique pattern of ROS generation. It is based on Fenton or Fenton-like reaction, which utilizes Fenton metals (such as Fe, Cu, Mn) to convert endogenous H2O2 into highly biocidal hydroxyl radical (•OH) with no need for external stimulation [15], [16], [17]. This process causes irreversible oxidative damage of biomolecules, such as lipid peroxidation, DNA and protein damage [18]. The acidic condition could facilitate Fenton reaction efficacy, which matches the TME. In comparison with other energy-driven cancer-therapeutic modalities, CDT exhibits several unique superiorities, including endogenous energy activation, high TME selectivity, and capacity for TME modulation [19]. In addition, the such metal-based nanomedicines possess multifunctional imaging capability [20], [21], [22], based on which imaging-guided tumor therapy can be achieved to dynamically monitor the in vivo fate of the nanoparticles and their therapeutic outcomes.
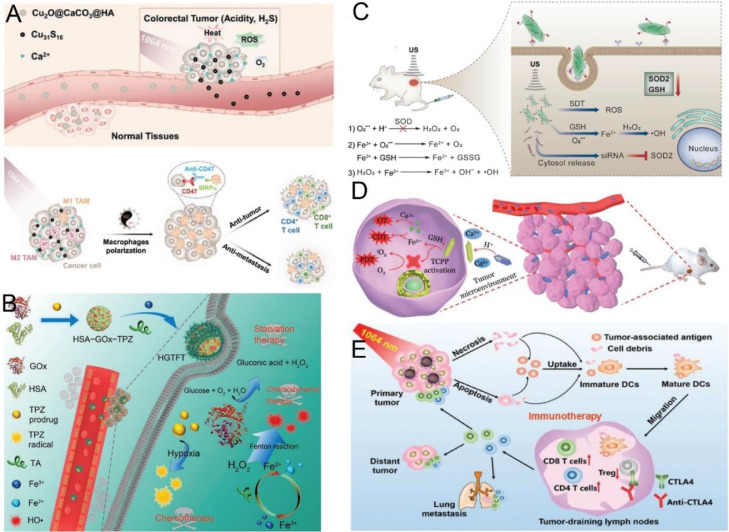
However, while varieties of Fenton metal nanomedicines (FMNs) have been demonstrated for effective CDT in vitro, their efficacy is far from satisfactory in vivo for complete tumor ablation. Possible limitations include unabundant intratumoral H2O2 for •OH production, the mild acidity of TME that is not optimal for Fenton reaction, as well as the anti-oxidative systems in tumor to scavenge ROS [19,23,24]. To mitigate these issues, multimodal systems that combine CDT with other therapeutics are suggested to complement each other for synergistic tumor therapy (Fig. 1). For example, therapeutic benefit can be improved by combining with PTT. On one hand, PTT-induced hyperthermia promotes •OH generation and accelerates ROS oxidation of biological molecules [25]. Meanwhile, the oxidative stress alleviates heat resistance of tumor cells to some extent by inhibiting heat shock proteins (HSPs), thereby improving the PTT efficacy [25,26]. Another typical example is glucose oxidase (GOx)-mediated starvation therapy to synergize CDT via H2O2 generation and acidification of TME [27].
Fig. 1.
Schematic illustration of the imaging-guided combinatorial CDT strategies for cancer therapy. Reproduced from [28]. Copyright 2018 American Chemical Society. Reproduced from [29]. Copyright 2019 American Chemical Society. Reproduced from [30]. Copyright 2018 American Chemical Society. Reproduced from [31]. Copyright 2020 American Chemical Society. Reproduced from [32]. Copyright 2018 2019 Elsevier. Reproduced from [26]. Copyright 2019 American Chemical Society. Reproduced from [33]. Copyright 2018 American Chemical Society. Reproduced from [34]. Copyright 2020 John Wiley & Sons.
In this review article, we first introduced diverse FMNs for CDT, and their mechanisms were elucidated in detail for theranostic applications. Then, the recent development of multi-modal strategies combining CDT with other treatments, such as chemotherapy, PTT, PDT, SDT, starvation therapy and immunotherapy, is discussed. Afterwards, various imaging-guided systems were described, including magnetic resonance imaging (MRI), computed tomography (CT) imaging, positron emission tomography (PET) imaging, photothermal imaging (PTI), photoacoustic imaging (PAI). Finally, challenges and future perspectives of FMNs in biomedical applications are summarized for further development.
2. FMNs for CDT
The basic requirement of CDT is the integration of Fenton metal to trigger Fenton or Fenton-like reactions in tumor [19,35]. Currently, the nanomaterials containing redox-active transition metal, such as Fe2+/Fe3+, Cu+/Cu2+, Mn2+, Co2+, Ce3+ and Ag+, are widely explored as Fenton catalysts for CDT [15,36]. The types and properties of various FMNs for CDT are summarized (Table 1), and each type of metal species were reviewed in the following section.
Table 1.
Summary of types and properties of various FMNs for CDT.
| Fenton metal | Types | Properties for CDT |
|---|---|---|
| Fe | Iron oxide, iron sulfide, MOFs, Prussian blue |
|
| Cu | Copper oxide, copper sulfide, CuSe, MOFs, CuETs |
|
| Mn | Manganese oxides |
|
2.1. Fe-based nanomaterials
Since the initial attempt of using amorphous Fe as Fenton agent in breast cancer cells in 2016 [37], various Fe-containing nanomaterials, such as iron oxide, iron sulfide, Fe-based metal-organic frameworks (MOFs), Prussian blue, have been developed for CDT against malignant tumor [30,[38], [39], [40], [41], [42]. Under acidic condition, Fe2+/Fe3+ reacts with H2O2 to generate ROS, and the reactions were shown below (Eqs. 1 and 2) [43].
| (1) |
| (2) |
Besides CDT, other biological functions of Fe-based nanomaterials were also explored. For example, ferroptosis, a type of nonapoptotic programmed cell death caused by accumulation of lipid hydroperoxides, is closely related to the iron-dependent intracellular oxidative stress, and Fe-based FMNs could induce ferroptosis via the Fenton-like reaction of Fe2+ and lipid peroxidation [44,45]. Ferroptosis has attracted great research interest for tumor therapy owing to its non-apoptotic pathway to bypass the treatment resistances. In addition, it is also reported recently that Fe2+/Fe3+could polarize tumor-related macrophages (TAMs) and reprogram TME to synergize CDT [46,47]. Moreover, Fe-based nanomaterials can act as imaging agents for tumor diagnosis and imaging. For instance, iron oxide nanoparticles (IONPs) have been applied in T1/T2-weighted MR imaging [48,49]. Despite these functionalities, there are still two critical issues of the Fe-based nanomaterials, i.e., insufficient acidity in TME and low H2O2 concentration that limits the CDT efficacy [50,51].
2.2. Cu-based nanomaterials
Cu-based nanomaterials are compared favorably over Fe-based nanomaterials for CDT owing to their broader reactive pH range and higher Fenton reactivity (Eq. 3, the catalytic rate of Cu+ is ∼160-fold higher than that of Fe2+) [36].
| (3) |
As such, Cu-based nanomaterials have been extensively attempted as Fenton reagent, including copper oxide, copper sulfide, CuSe and Cu-based MOF [32,[52], [53], [54]. For example, Cu-tannic acid networks (Cu-TA) could effectively covert H2O2 into toxic •OH, exhibiting robust CDT efficacy with high biosafety [55]. Meanwhile, the inherent biological activity of Cu2+ and photothermal conversion capability of several Cu-based oxides and sulfides endow the nanomaterials with versatile applications for combinatorial therapy [21,56], and they also possess the capability for imaging-guided therapies, such as PAI, PTI, PET and CT performance [21].
2.3. Mn-based nanomaterials
Mn-based nanomaterials have also been employed as the Fenton-like metal for chemodynamic conversion [57]. Manganese oxides (MnOx) were the most commonly used Mn-based Fenton nanomaterials for cancer theranostics, and combinatorial therapy can be easily realized since this type of nanomaterials has been extensively used as carriers to deliver small molecular drugs and gene therapeutics. [22,40] Compared with many other FMNs, these nanomaterials possess additional function to relieve tumor hypoxia via their catalase-mimicking activity to produce oxygen, and the generated Mn2+ from MnOx decomposition triggers the Fenton-like chemical reaction for CDT [58]. Moreover, MnOx were able to deplete intracellular GSH to promote the efficacy of CDT. For bioimaging, Mn-based nanomaterials have been demonstrated as excellent contrast agent for tumor T1-weighted MR imaging, and their capabilities for PTI, PAI and ultrasonic imaging (USI) were also demonstrated [59,60].
2.4. Other metal-based nanomaterials
Other transition metals, such as Co2+, Ce3+ and Ag+, also showed the potential as Fenton agents for CDT [61], [62], [63], while their biological applications are limited by biosafety issues caused by metal poisoning [64]. For example, Co or Ag-contained nanomaterials could cause DNA mutations or damage, induce genotoxicity and carcinogenicity [65]. Moreover, the cerium oxides (CeO2) have intrinsic pulmonary toxicity [66].
3. CDT-based combinatorial therapy
Although CDT is considered as a new type of “green” cancer therapy, its efficacy is not good in vivo due to the poor catalytic activity and intrinsic resistance of tumor [67]. Therefore, combination strategies have been developed to optimize the therapeutic outcomes, and we have witnessed the incorporation of various treatments into CDT systems, including chemotherapy, PDT, SDT, PTT, starvation therapy and immunotherapy, for multi-modal tumor therapy (Table 2) [43].
Table 2.
Summary of representative FMNs for imaging-guided combinatorial tumor therapy.
| Name of the nanomaterials | Fenton metals | Theranostic modalities | Performance | Refs. |
|---|---|---|---|---|
| DEN-DOX@TA-FeIII | Fe3+/Fe2+ | Chemotherapy /CDT | CDT sensitization by DOX-mediated apoptosis | [68] |
| DSF@PEG/Cu-HMSNs | Cu2+/Cu+ | Chemotherapy /CDT | Cu2+ released from HMSNs in acidic TME to form toxic CuETs, or converse into Cu+ by endogenous H2O2 to produce ROS. | [29] |
| DDMON-IONP-CUR | Fe3+/Fe2+ | Chemotherapy /CDT | Cancer-cell-specific Ca2+ and GSH depletion, •OH generation, thioredoxin reductase inhibition, and tumor ICD. | [69] |
| UCNPs@MnO2-Pt-PEG | Mn2+ | MRI/UCL imaging-guided chemotherapy /CDT | GSH depletion- and cisplatin-activation-enhanced •OH generation, along with TME-triggered MRI/UCL imaging. | [70] |
| SRF@Hb-Ce6 | Fe2+ | CDT/PDT | Sorafenib/Fe-induced ferroptosis combining with PDT | [31] |
| mCMSNs | Cu2+/Cu+, Mn2+ | MRI-guided PDT/CDT | Programing TME via hypoxia relief and GSH depletion to enhance PDT/CDT. | [71] |
| Cu2-xSe-CD-Ce6 | Cu2+/Cu+ | PAI-guided CDT/PDT | Fenton-like Haber-Weiss catalyst for ICD and M1-macrophages polarization. | [72] |
| Au-MnO@ PEG/PPADT |
Mn2+ | FI/MRI-guided CDT/ST | ROS and GSH-triggered Au NPs release as numerous cavitation nucleation for sonodynamic conversion, and Mn2+ production for Fenton-like reaction. | [73] |
| EA-Fe@BSA | Fe3+/Fe2+ | MRI-guided CDT/PTT | Endogenous H2S triggered Fe3+/Fe2+ conversion and PTT-enhanced •OH generation. | [74] |
| Au@MSN@ IONP | Fe3+/Fe2+ | MRI-guided PTT-enhanced CDT | Heat-triggered intracellular H2O2 production to fuel Fenton reaction, and PI3K/Akt/FoxO axis inhibition. | [75] |
| Cu(I) phosphide nanocrystals | Cu+ | PAI/MRI/PTI guided CDT/PTT | GSH depletion and NIR II photothermal conversion to increase •OH generation, along with in situ T1−MR imaging. | [76] |
| FP NRs | Fe3+/Fe2+ | PAI/MRI-guided CDT/PTT | Ultrasound and photothermal-enhanced Fenton reaction, along with PA/MR imaging. | [77] |
| MnOx@silicene-BSA | Mn2+ | PAI/MRI-guided CDT/PTT | Hyperthermia-augmented Fenton-like catalytic activity, along with TME-responsive T1−MRI and PAI. | [78] |
| Co-Fc@GOx | Fe2+ | Starvation therapy/CDT | Promoting intracellular acidity and H2O2 production by GOx to boost the Fenton reaction. | [79] |
| GOx@ZIF@TA-FeIII | Fe3+/Fe2+ | MRI-guided starvation therapy enhanced CDT | GOx-mediated H2O2 generation and TA-induced Fe3+/Fe2+ conversion for enhanced CDT. | [33] |
| Fe5C2-GOx@ MnO2 | Fe2+ | T1/T2 MRI-guided starvation therapy /CDT | MnO2 decomposition and GOx release under acidic TME for starvation therapy to enhance CDT, along with MR imaging. | [80] |
| MnOx-TF | Mn2+ | MRI/PAI-guided immunotherapy /CDT |
TME-responsive capability and tumor ICD. | [34] |
| Cu2O@CaCO3@HA | Cu2+/Cu+ | PTT/PDT/CDT/ immunotherapy | Hyperthermia and oxidative stress induced by acidic and H2S-overexpressed TME to reprogram macrophages and facilitate immunotherapy. | [81] |
| HSA-GOx-TPZ@ TA-FeIII | Fe3+/Fe2+ | starvation therapy enhanced CDT/ chemotherapy | GOx-mediated H2O2 generation and hypoxia exacerbation, as well as TA-accelerated Fe3+/Fe2+conversion for cascade cancer therapy. | [82] |
| GOx-MnCaP-DOX | Mn2+ | MRI-guided starvation therapy CDT/chemotherapy | Acidic-responsive NPs degradation, GOx-mediated glucose elimination and Mn2+-mediated Fenton-like reaction for cascade-enhanced anti-tumor therapy. | [83] |
| FeIII-TPPS@Bis (DPA-Zn)-RGD /SOD2 siRNA | Fe3+ | FI/MRI-guided SDT/gene therapy/CDT | Enhanced ROS production via SOD2 downregulation, GSH depletion and Fenton reaction. | [84] |
| TCPP-FeIII@ DHA@CaCO3 | Fe3+/Fe2+ | Oncosis therapy /CDT/PDT | Acidic TME- and GSH-triggered DHA release, Ca2+ and Fe2+ supply, and TCPP activation for combinatorial therapy. | [85] |
| GOx@Cu2MoS4 | Cu2+/Cu+Mo4+/ Mo6+ | CDT/starvation therapy/PDT/PTT/ immunotherapy | GSH peroxidase mimicking activity to deplete GSH, and O2/H2O2 supply. | [86] |
| PtCu3-PEG | Cu2+/Cu+ | FI/PAI/CT imaging-guided SDT/CDT | GSH peroxidase mimicking activity to deplete GSH, along with FI/PAI/CT imaging. | [87] |
| HMON-Au-Col@ Cu-TA-PVP | Cu2+/Cu+ | FI/PET imaging-guided PDT/CDT | Au NPs catalysis-based H2O2 supply, along with PET imaging by 64Cu2+ labeling. | [55] |
3.1. CDT combined with chemotherapy
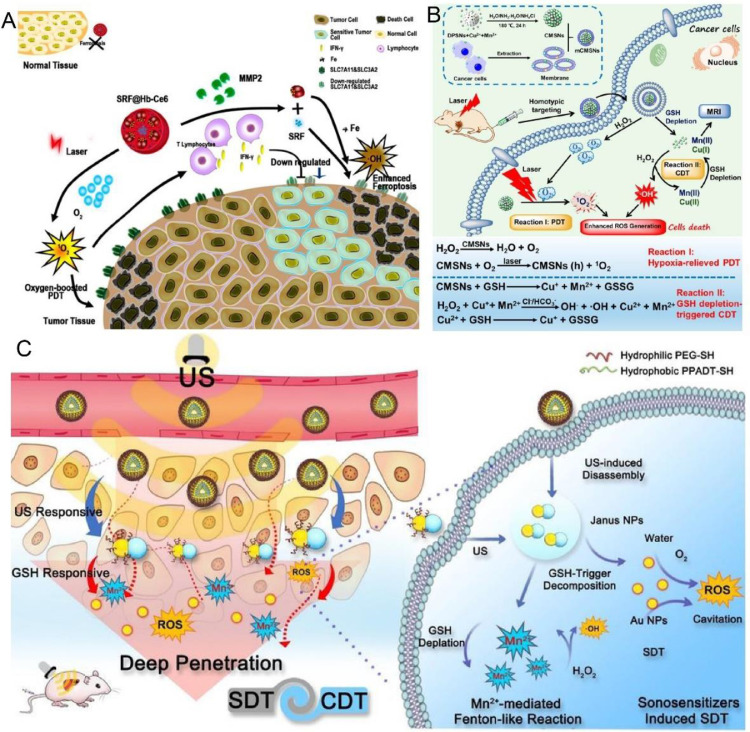
Chemotherapy is one of the most prevailing treatment of various cancer, and hundreds of chemotherapeutic drugs have been discovered. However, the nonspecific distribution, rapid clearance and multidrug chemoresistance cause the undesirable therapeutic efficiency and severe side effects of chemotherapy [88], [89], [90]. ROS, as an important part of redox balance and cell signaling pathway in biological processes, exhibits outstanding synergistic effect with chemotherapy. Integrating chemotherapy drugs with FMNs into one nanoplatform is highly desirable for combinational therapy [91]. For instance, Shi et al. fabricated Cu2+-doped PEGylated hollow mesoporous silica nanoparticles (HMSNs) to encapsulate disulfiram (DSF) [29]. DSF, as a Cu2+-dependent chemotherapy drug, could chelate Cu2+ released from HMSNs in acidic TME to generate toxic CuETs for chemotherapy. Meanwhile, Cu+conversed from Cu2+triggered Fenton-like reaction to produce ROS in presence of endogenous H2O2 condition, improving the therapeutic outcomes of CuETs (Fig. 2A and 2B). With these synergistic effects, tumor tissue was remarkably inhibited.
Fig. 2.
(A) Schematic showing the construction of DSF@PEG/Cu-HMSNs for synergistic CDT/chemotherapy. (B) Mechanisms of DSF/Cu2+ interaction for chemo/CDT combination. Reproduced from [29]. Copyright 2019 American Chemical Society. (C) Schematic illustration of the construction of DDTF nanocomplexes and their application for chemotherapy/CDT cancer therapy. Reproduced from [68]. Copyright 2019 American Chemical Society.
Interestingly, several typical chemotherapeutic drugs, such as doxorubicin (DOX) [68], cisplatin, [70] and β-lapachone [92], can activate some enzymes to generate H2O2, which in turn supply the substrate of Fenton reaction to enhance CDT, thereby achieving synergistic chemotherapy/CDT to overcome chemoresistance of cancer. Capitalized on this fact, Wu et al. designed a DEN-DOX@TA-FeIII nanocomplex (namely DDTF) by mixing metal-phenolic network (MPN) with DOX-loaded dendrimer (DEN) [68]. After intracellular internalization, the released DOX induced cell apoptosis and elevated the H2O2 level to sensitize Fe2+/3+-mediated CDT (Fig. 2C). The nanoplatform provides a novel solution to surmount multidrug-resistance of cancer.
3.2. CDT combined with PDT or SDT
PDT is a ROS-mediated treatment modality. It employs photosensitizers to convert molecular oxygen into singlet oxygen (1O2) under light irradiation, which causes cancer cells death via apoptosis and necrosis [93,94]. As a non-invasive therapeutics, PDT has the advantages of low systemic toxicity, spatiotemporal selectivity and the lack of resistance mechanisms [95,96]. However, the treatment outcome of PDT was often limited by poor tissue penetration and hypoxic TME [97]. Combining PDT with CDT is a powerful strategy to employ multiple antitumor mechanisms for amplified tumor oxidative stress. Li et al. constructed a sorafenib-loaded hemoglobin (Hb)-Ce6 nanoplatform (namely SRF@Hb-Ce6) for oxygen-boosted PDT/CDT (Fig. 3A) [31]. Fe-containing hemoglobin (Hb) simultaneously furnished oxygen for enhanced PDT and triggered Fenton reaction to synergize with sorafenib for enhanced ferroptosis. Moreover, PDT/CDT-induced tumor immunogenic cell death (ICD) activated robust immune response, which further improved the efficacy of ferroptosis via interferon-γ (IFN-γ) secretion. Notably, several nanosystems release Fenton metal ions in a GSH-dependent manner, and the concurrent depletion of GSH could amplify ROS-mediated PDT/CDT therapy. For example, Zhang et al. utilized cancer cell membrane to coat mesoporous copper/manganese silicate nanospheres (namely mCMSNs) for homotype-targeted CDT/PDT therapy (Fig. 3B) [71]. The catalase-mimic activity of mCMSNs converted H2O2 into O2 to relieve the hypoxia TME, and thus enhanced O2-dependent PDT. Meanwhile, GSH-mediated mCMSNs decomposition produced Cu+ and Mn2+ to trigger Fenton reaction, and oxidation stress was further enhanced via GSH depletion. This study demonstrated a multifunctional nanosystem with oxygen supply, tumor response and TME regulation capabilities for enhanced CDT/PDT.
Fig. 3.
(A) The schematic showing the mechanisms of SRF@Hb-Ce6 for synergistic tumor therapy. Reproduced from [31]. Copyright 2020 American Chemical Society. (B) Schematic illustration showing the therapeutic mechanism of mCMSNs for synergistic CDT/PDT. Reproduced from [71]. Copyright 2019 American Chemical Society. (C) Illustration of the Janus Au-MnO nanosystem for CDT/SDT against deep tumor. Reproduced from [73]. Copyright 2020 John Wiley & Sons. Abbreviations; MMP-2: matrix metalloproteinase-2; Hb: hemoglobin; SRF: sorafenib; IFN-γ: interferon-γ; US: ultrasound.
SDT, which utilizes sonosensitizers to produce ROS under ultrasound irradiation to ablate tumor, could also synergize with CDT, and a notable advantage is the deep penetration of ultrasound [98]. In one example, Yang et al. prepared Janus Au-MnO nanoparticles coated with PEG and ROS-responsive polymer for deep-seated tumor CDT/SDT (Fig. 3C) [73]. After ultrasound to generate ROS, this nanosystem was disassembled into small Au-MnO NPs, and then degraded into Au NPs and Mn2+. Au NPs served as sonosensitizer for SDT, which amplified oxidative stress and facilitated Mn2+-mediated CDT.
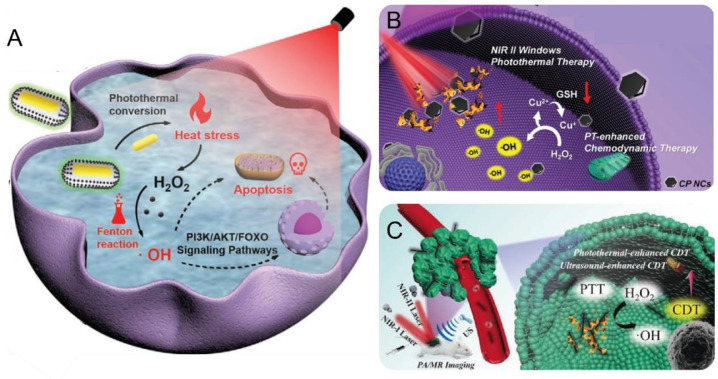
3.3. CDT combined with PTT
Among various CDT combinatorial therapy, integrating PTT with CDT into one system is most attractive owing to their multiple synergistic mechanism. First, some nanomaterials, such as copper oxide [81], copper sulfide [32], ferric oxide [99], MPN [74], and Prussian blue [40], can simultaneously induce photothermal conversion for PTT and release Cu2+ or Fe2+/Fe3+ for CDT, offering simple platforms to combine these two modalities. Second, hyperthermia is capable of facilitating drug release, thus realizing triggered release of Fenton-based agents [100]. Third, the photothermal effect not only causes tumor cells death but also increases the yield of ROS and accelerates the ROS oxidation of biological molecules, thereby improving efficiency of CDT [25,101]. Finally, heat shock proteins (HSPs), which cause thermoresistance via resisting heat damage, were inhibited by ROS in cancer cell, thus enhancing hyperthermia-induced tumor ablation [26].
Ling et al. fabricated core-shell-satellite nanomaces (namely Au@MSN@IONP) composed of Au nanorod, mesoporous silica nanoshell and ultrasmall iron oxide nanoparticles (IONP) for triple-negative breast cancer (TNBC) therapy. The Au nanorod core could transform near infrared (NIR) light into heat to increase ROS generation, thus fueling IONP-mediated Fenton reaction for robust CDT (Fig. 4A) [75]. Meanwhile, the Au@MSN@IONP was found to inhibit PI3K/Akt/FoxO signaling pathways, which is related to redox regulation and survival of TNBC. Therefore, this system could realize self-enhanced and PTT-fueled CDT against TNBC. To improve tissue penetration and energy conversion efficiency, Yang et al. synthesized copper phosphide nanocrystals, which combined NIR II laser-mediated PTT and CDT for deep tumor elimination (Fig. 4B) [76]. These nanocrystals depleted endogenous GSH to enhance •OH accumulation, and induced NIR II photothermal conversion under 1064 nm laser irradiation to promote the penetration of nanoparticle into deep-seated tumor. In another work, ferrous phosphide nanorods (namely FP NRs) were developed by Yang et al. for ultrasound and photothermal-enhanced CDT (Fig. 4C) [77]. The prepared FP NRs, as an “all-in-one” Fenton agent, facilitated the production of ROS under ultrasound and NIR II laser irradiation, showing high therapeutic effect with high maximum permissible exposure and deep tissue penetration.
Fig. 4.
(A) Schematic illustration showing the Au@MSN@IONP as photothermal-triggered self-fueling Fenton agents for TNBC ablation. Reproduced from [75]. Copyright 2020 John Wiley & Sons. (B) Schematic illustration of the copper phosphide nanocrystals for PTT-enhanced CDT to treat deep-seated tumor. Reproduced from [76]. Copyright 2019 John Wiley & Sons. (C) Schematic showing the FP NRs for enhanced CDT/PTT treatment. Reproduced from [77]. Copyright 2019 John Wiley & Sons. Abbreviations; US: ultrasonic.
3.4. CDT combined with starvation therapy
Starvation therapy kill cancer cells via exhausting nutrients or blocking the energy supply. GOx, a type of oxido-reductase, can effectively catalyze glucose oxidation into gluconic acid and H2O2, and oxygen is consumed during this process. GOx-mediated glucose depletion provides a noninvasive strategy for cancer starvation therapy [27,102]. More interestingly, the generated H2O2 and gluconic acid can provide sufficient H2O2 and acidifies TME to boost Fenton reaction. Therefore, combining GOx-mediated starvation with CDT has outstanding synergistic therapeutic effects. Han et al. synthesized a cascade enzymatic/Fenton catalytic nanoplatform (namely Co-Fc@GOx) by incorporating GOx into Co-ferrocene metal-organic framework to achieve enhanced Fenton reaction with intracellular anabatic acidity and self-supplied H2O2 production (Fig. 5A) [79]. Once internalization into cancer cells, GOx exhausted endogenous glucose to kill the cells, and provided enough intracellular acidity and H2O2 for the subsequent Fenton reaction (Fig. 5B). Consequently, enhanced CDT was achieved both in vitro and in vivo, resulting in significant tumor growth inhibition in 4T1-tumor-bearing mice. While this pioneering work demonstrated the benefits of CDT/GOx combination, the catalytic activity of GOx is limited by the hypoxic TME. To mitigate this issue, a TME-responsive and oxygen self-supplied nanocatalyst composed of iron carbide (Fe5C2), GOx and MnO2 was constructed by Feng et al. (Fig. 5C) [80]. After cellular internalization, MnO2 was decomposed into Mn2+ accompanied by O2 generation in acidic TME, and GOx was concomitantly released. The in situ generated O2 elevated the catalytic effect of GOx to synergize Fe5C2-mediated CDT. Such oxygen supply-enhanced CDT/starvation combinatorial therapy provides a promising strategy for selective tumor ablation with amplified treatment outcomes and minimized side effects.
Fig. 5.
(A) The scheme of Co-Fc@GOx as a GOx-enhanced Fenton reaction platform for CDT/starvation therapy. (B) Schematic showing the mechanism of synergistic effect between GOx-based starvation therapy and CDT. Reproduced from [79]. Copyright 2020 John Wiley & Sons. (C) Schematic diagram of catalytic therapeutic mechanism of Fe5C2-GOx@MnO2 for cancer therapy. Reproduced from [80]. Copyright 2018 American Chemical Society.
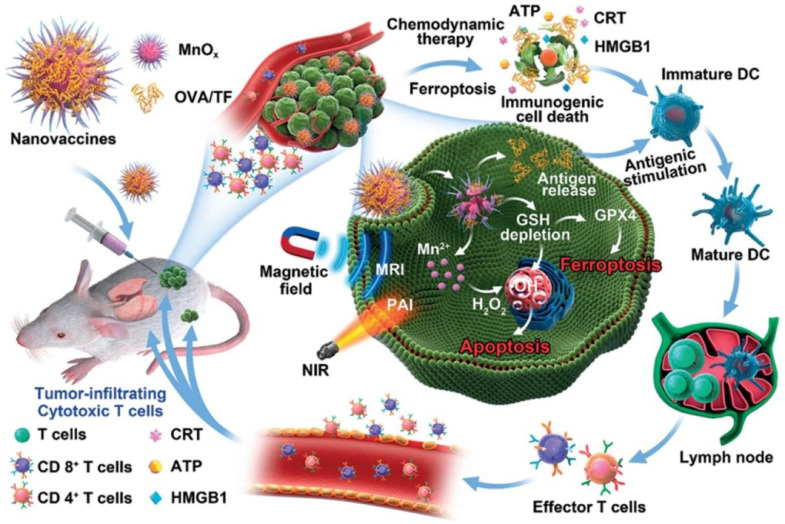
3.5. CDT combined with immunotherapy
Immunotherapy, which activates patient's own immune system to fight cancer, hold great promise to inhibit both primary and metastatic tumor, as well as tumor recurrence [103]. Among them, cancer vaccines, cytokine therapy and immune checkpoint blockade therapy have recently received more and more attention owing to high efficiencies and minimal side effects [104,105]. Nevertheless, various immune-suppressive mechanisms of tumor lead to poor lymphocytes infiltration, thus inhibiting immune response [106]. Toward this issue, CDT can strengthen the antitumor immune response via inducing ICD, indicating the potential advantages of CDT/immunotherapy combination [69,107]. ICD is characterized by secretion of danger associated molecular patterns (DAMPs) and tumor-associated antigens (TAAs), which promotes antigens presentation and elicits robust immune response [108]. For instance, Lin et al. constructed manganese oxide nanomaterials-based nanovaccines (namely MnOx-TF) for cancer immunotherapy (Fig. 6) [34]. After intratumoral injection, the Fenton-like reaction can be triggered for CDT and ferroptosis, which induced ICD with the release of tumor-associated antigens. Subsequently, the cascade immune responses were activated to produce an immunogenic TME. Consequently, MnOx-TF not only inhibited the primary tumor, but also suppressed distal tumor growth and tumor metastasis.
Fig. 6.
Schematic presentation of the MnOx-TF nanovaccines for cancer CDT/immunotherapy. Reproduced from [34]. Copyright 2020 John Wiley & Sons.
3.6. Multimodal therapy
In addition to binary combination, multimodal systems that integrate more than two therapeutics were also developed to further improve the treatment outcomes [109]. For example, with the fact that Fenton reaction-induced oxidative stress is insufficient to elicit robust ICD for immunotherapy, Lin et al. have fabricated a core-shell nanostructure (namely Cu2O@CaCO3@HA) for multimodal therapy against colorectal cancer (Fig. 7A) [81]. The acidic colorectal TME facilitated CaCO3 shell decomposition to generate Ca2+ for intracellular calcium overload. Subsequently, the Cu2O core was sulfuretted by overexpressed H2S in tumor for in-situ generation of copper sulfide nanocrystals (Cu31S16). The produced Cu31S16 increased oxidative stress via Fenton reaction, and also possessed photodynamic and photothermal capabilities, displaying outstanding CDT/PTT/PDT effect under NIR laser irradiation. More importantly, this Cu2O@CaCO3@HA-mediated calcification and multimodal therapies repolarized tumor-associated macrophages and strengthened immunotherapy. By further combining with CD47 blockade, this nanostructure not only ablated primary/distant tumor, but also suppressed cancer recurrence and metastasis, showing unprecedented potency for cancer therapy.
Fig. 7.
(A) Schematic diagram showing the Cu2O@CaCO3@HA combined with CD47 blockade for combinatorial tumor therapy. Reproduced from [81]. Copyright 2020 John Wiley & Sons. (B) Scheme of the synthetic route of the MPN-based nanoreactors and their applications for combinatorial therapy. Reproduced from [82]. Copyright 2020 John Wiley & Sons. (C) Schematic diagram showing the multifunctional sonotheranostics for synergistic tumor therapy. Reproduced from [84]. Copyright 2019 John Wiley & Sons. (D) Schematic illustration showing the TCPP-FeIII@DHA@CaCO3 for synergistic tumor therapy. Reproduced from [85]. Copyright 2019 John Wiley & Sons. (E) Schematic illustration showing the anti-tumor mechanisms of GOx@Cu2MoS4 when combining with checkpoint blockade therapy. Reproduced from [86]. Copyright 2019 John Wiley & Sons.
Given the various TME modulation effects of GOx, including H2O2 generation, acidification and hypoxia exacerbation, GOx has been incorporated into multimodal tumor therapy. For instance, Wu et al. fabricated a self-amplified MPN-based nanoreactor composed of tirapazamine (TPZ), human serum albumin (HSA) and GOx for sustainable and cascade therapy (Fig. 7B) [82]. The starvation therapy induced by GOx obviously increased the intracellular H2O2 for Fe2+/3+-mediated Fenton reaction and aggravated hypoxia to activate TPZ (a hypoxic prodrug) for chemotherapy. The nanosystem achieved high tumor accumulation and synergistic anticancer effect for effective tumor ablation.
Multi-modal systems have also been explored to enhance ROS production to improve CDT. In one design, Liu and coworkers developed a FeIII-porphyrin nano-sonosensitizer anchored with Bis(DPA-Zn)-RGD and superoxide dismutase 2 (SOD2) siRNA for SDT/gene therapy/CDT therapy (Fig. 7C) [84]. This nano-sonosensitizer effectively delivered siRNA into tumor cells for SOD2 silencing, and ROS generation can be enhanced via porphyrin-mediated SDT, Fe3+-induced GSH depletion and Fe2+-triggered Fenton reaction, which collectively leads to amplified intracellular oxidative stress. In another case, Tang et al. fabricated a dihydroartemisinin (DHA)-loaded Fe-TCPP MOF with CaCO3 mineralized coating for synergistic oncosis therapy/CDT/PDT (Fig. 7D) [85]. This nanoplatform released DHA in response to acidic and GSH-overexpressed TME, accompanied with Ca2+/Fe2+ generation and photosensitizer activation. The anticancer mechanism of DHA is to act on cell membrane and Ca2+ pump ATPase, leading to oncosis-like cell death, which can be enhanced by introducing exogenous Ca2+. Meanwhile, the produced Fe2+ reacted with DHA to generate free radicals, causing cell apoptosis. Therefore, Ca2+-DHA-mediated oncosis therapy and TCPP-mediated PDT synergized with Fe2+/DHA-mediated CDT, resulting in high cancer therapeutic efficiency and negligible side effects.
We noticed that the most complicated system has combined five different modalities for tumor therapy, which integrated CDT, starvation therapy, PDT, PTT and immunotherapy [86]. They fabricated the GOx-loaded hollow mesoporous Cu2MoS4 as multifunctional cascade bioreactor (Fig. 7E), which realized efficient cancer therapy through a variety of synergistic mechanisms. (I) the multivalent elements (Cu+/2+, Mo4+/6+) triggered Fenton-like reaction and depleted GSH for CDT. (II) Converting H2O2 into O2 via catalase-like catalysis to enhance GOx-induced starvation therapy. (III) Effective photothermal conversion and superoxide anion production under 1064 nm laser irradiation. (IV) Robust immune responses elicited by multiple treatments that can combine with checkpoint blockade therapy to eliminate both primary and metastatic tumor. However, while such system is robust enough for tumor therapy, the contribution of each treatment modality is rather elusive.
4. Imaging-guided CDT-based therapy
Precise diagnosis is vital for the management of various diseases, particularly when the cancer is involved. The imaging-guided therapy is a theranostic approach to visualize the location of the tumors and dynamically monitor the drug delivery [110,111]. Fenton metals could serve as versatile nanoplatforms for tumor bioimaging, such as MRI, PET imaging, CT imaging, PAI and PTI. These Fenton metal-based imaging modalities, as well as multimodal imaging-guided therapy have been summarized in Table 2, and will be introduced in the following section.
4.1. Fenton metals for bioimaging
Fenton metals, including Fe, Cu, Mn, not only show Fenton-like catalytic activity to produce •OH, but also serve as contrast agents (CAs) for bioimaging. As clinically approved diagnostic T1-weighted MR imaging CAs, Mn-based nanomaterials act as T1-positive agents of paramagnetic species to produce hyperintense regions on the MR image. By virtue of the five unpaired electrons, Mn2+ shows longer electronic relaxation time and higher spin number than Mn4+ [59]. Therefore, the TME-responsive disassembly behavior (from MnO2 to Mn2+) for contrast-enhanced MRI promotes their applications in theranostics [22]. Fe2+/Fe3+ can also be applied in T1-weighted MR imaging. Superparamagnetic iron oxide nanoparticles (SPIONs), which can induce magnetization on the perpendicular plane disappearing by the dephasing of the spins, are excellent T2-weighted MRI CAs for imaging-guided CDT [112]. The SPIONs have been demonstrated as MRI CAs for liver tumor imaging and metastasis monitoring [113]. Moreover, Positron-emitting isotope 64Cu-labeled Fenton-based nanomaterials exhibit powerful PET imaging capability with sufficient tissue penetration [55]. As a high Z value element, Cu displays large X-ray attenuation coefficient, making it ideal X-ray computed tomography contrast agent for CT imaging [21]. The FMNs with photothermal conversion performance (CuO, CuS, MPN, Prussian blue et al.) induce tissue thermoelastic expansion and hyperthermia under NIR light irradiation, which can be utilized for noninvasive PAI and PTI [114,115].
4.2. Multimodal imaging-guided combinatorial CDT
Integrating multiple imaging means into one nanoplatform was prevailing in imaging-guided combinatorial CDT, which overcomes drawbacks of each singular imaging signal to provide complementary information of cancer. As an example, Yang et al. fabricated a highly efficient CDT agent (namely CP NCs) for PAI/MRI/PTI-guided CDT/PTT [76]. Unlike other hybrid nanomaterials, The CP NCs represent simple and multifunctional Cu-based FMNs, which can realize multiple imaging-guided therapy with a singular nanosystem. In response to H2O2, the CP NCs generated MRI contrast agent of paramagnetic Cu2+ via in-situ oxidation (Fig. 8A), which produced strong T1-weighted MRI signal (Fig. 8B). After in vivo injection, the MRI signal increased at tumor site overtime (Fig. 8C), owing to gradual generation of Cu2+. Benefiting from the photothermal capability, the applications of CP NCs for PAI and PTI were also explored, and PA signals were significantly boosted at the tumor site at 12 h post-injection in contrast to that of before injection (Fig. 8D). Meanwhile, the photothermal imaging showed a rapid temperature elevation of tumor within 10 min under laser illumination (Fig. 8E). Combining all these signals, this CDT-based nanoplatform provided abundant information for precise cancer theranostics. As a complementary example, Yang et al. reported PtCu3 nanocages serving as sonosensitizer for FI/PAI/CT imaging-guided SDT/CDT [87]. The in vivo behavior was monitored by labeling the nanocages with Cyanine 5.5 for FI, and obvious fluorescence was observed in the tumor regions more than 72 h post-injection (Fig. 8F). The similar results were also obtained from PA imaging with amplified and sustained signal at tumor site within 72 h (Fig. 8G). More importantly, these nanocages might serve as CT imaging contrast agent, exhibiting stronger X-ray attenuation than commercially used Iohexol (Fig. 8H). In addition, a 64Cu-labeled biocatalysis nanoreactor was fabricated by Chen et al. for FI/PET imaging-guided PDT/CDT [55]. An obviously stronger PET imaging signal was observed at the tumor site over a long time after intravenous injection (Fig. 8I), meanwhile the fluorescence imaging agreed well with the PET imaging result (Fig. 8J). This imaging performance was demonstrated to be robust enough to guide the ROS-mediated therapy.
Fig. 8.
(A) Schematic illustration showing in situ self-generation of Cu2+ for MR imaging. (B) T1−MR imaging of CP NCs solution with different concentrations in absence or presence of 100 µM H2O2. In vivo T1−MRI (C), PAI (D) and PTI (E) of tumor-bearing mice. Reproduced from [76]. Copyright 2019 John Wiley & Sons. (F) Fluorescence images of 4T1 tumor-bearing mice by intravenous injection of Cy5.5-labeled nanocages. PAI (G) and CT imaging (H) of 4T1 tumor-bearing mice. Reproduced from [87]. Copyright 2020 John Wiley & Sons. (I) PET imaging of tumor-bearing mice after intravenous injection with the 64Cu-labeled nanoreactor. (J) Fluorescence images of tumor-bearing mice after intravenous injection with the nanoreactor. Reproduced from [55]. Copyright 2020 John Wiley & Sons.
5. Conclusion and future perspective
As a catalysis-driven cancer-therapeutic modality, CDT has obtained increased interest owing to its tumor selectivity. Especially, CDT-based combinatorial systems with imaging-guided therapy are highly encouraging for cancer theranostics attributing to precise tumor treatment with robust therapeutic outcomes. In this review, we have introduced the typical Fenton metals and their catalytic mechanisms, and summarized the recent development of FMNs for imaging-guided combinatorial CDT. Overall, the research in the field is still in its infancy, and there needs a lot of work to be done for potential clinical translation. To make real clinic impact, several crucial issues and challenges are remained to be addressed as listed below.
-
(I)
Mechanism: The Fenton/Fenton-like catalytic reaction-mediated ROS production has been widely explored, whereas the catalytic mechanism and ROS-induced molecular damage have not yet been fully revealed, making it difficult to rationally improve and optimize catalytic efficiency. Deep exploration of in vivo CDT process and its relevant mechanisms is important to guide cancer treatment. For example, techniques that can monitor Fenton reaction in vivo are necessary to better elucidate the real contribution of CDT for tumor therapy.
-
(II)
Efficacy: CDT performance is limited by unamiable TME, and both of the exogenous H2O2 and the acidity in the cancer cell are not enough to initiate traditional Fenton reaction. Meanwhile, the intratumoral overexpressed GSH also passivates Fenton-induced ROS via antioxidation [116]. Although numerous FMNs have been designed to overcome the above obstacles, the more smart and versatile combinatorial nanoplatforms, which can overcome multiple limitations of TME, are desired in the future.
-
(III)
Delivery: Nanoscale delivery systems can be utilized to load Fenton metal for targeted delivery via EPR effect. However, this passive targeting is usually not sufficient [117]. Active targeting can be realized by further modification of specific ligands on particle surface to selectively recognize tumor. Moreover, the CDT-based combinatorial systems are powerful solution to improve the tumor treatment outcomes, while effective integration CDT with various therapeutics into one set usually requires complicated preparation procedures with sophisticated materials design. The development of simple, cost-effective and robust multimodal nanoplatforms are still deemed necessary to realize combinatorial therapy with synergistic effects.
-
(IV)
Biosafety: The biosafety of Fenton metals is another important issue that need to be taken into consideration for their potential clinical applications. Although their biocompatibility has been widely investigated in animal model during the treatment period, the long-term toxicity is rather unclear and needs further research. For FMNs, their biodegradation is important, which is the pre-requisite for body elimination of the Fenton metals. Hence, intensive studies on ADME (absorption, distribution, metabolism, and excretion) performances of FMNs should be conducted for further applications.
Taken together, CDT represents a highly promising strategy for tumor theranostic applications, which have garnered significant research interest to contribute the rapid progress of the field. Since the first attempt of CDT five years before, nearly 500 papers have been published by searching the ISI Web of Knowledge database, and various FMNs have been constructed with excellent anti-tumor efficacy at animal models. However, as mentioned above, to reach a clinical impact, substantial work has to be done both fundamentally and at animal/clinical levels, which may fuel the growth of the field in the future.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
This work was supported by Innovation-Driven Project of Central South University (No. 20170030010004), and National Natural Science Foundation of China (Nos. 21804144, U1903125, 82073799).
Reference
- 1.Moscow J.A., Fojo T., Schilsky R.L. The evidence framework for precision cancer medicine. Nat Rev Clin Oncol. 2018;15(3):183–192. doi: 10.1038/nrclinonc.2017.186. [DOI] [PubMed] [Google Scholar]
- 2.Cleary A.S., Leonard T.L., Gestl S.A., Gunther E.J. Tumour cell heterogeneity maintained by cooperating subclones in Wnt-driven mammary cancers. Nature. 2014;508(7494):113–117. doi: 10.1038/nature13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho K., Wang X., Nie S., Chen Z., Shin D.M. Therapeutic nanoparticles for drug delivery in cancer. Clin Cancer Res. 2008;14(5):1310–1316. doi: 10.1158/1078-0432.CCR-07-1441. [DOI] [PubMed] [Google Scholar]
- 4.Yang Y., Yu Y., Chen H., Meng X., Ma W., Yu M., et al. Illuminating platinum transportation while maximizing therapeutic efficacy by gold nanoclusters via simultaneous near-infrared-I/II imaging and glutathione scavenging. ACS Nano. 2020;14(10):13536–13547. doi: 10.1021/acsnano.0c05541. [DOI] [PubMed] [Google Scholar]
- 5.Qi S., Sun J., Yu H., Yu S. Co-delivery nanoparticles of anti-cancer drugs for improving chemotherapy efficacy. Drug Deliv. 2017;24(1):1909–1926. doi: 10.1080/10717544.2017.1410256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong L., Li W., Sun L., Yu L., Chen Y., Hong G. Energy-converting biomaterials for cancer therapy: category, efficiency, and biosafety. WIREs Nanomed Nanobiotechnol. 2021;13(1):e1663. doi: 10.1002/wnan.1663. [DOI] [PubMed] [Google Scholar]
- 7.Yang B., Chen Y., Shi J. Reactive oxygen species (ROS)-based nanomedicine. Chem Rev. 2019;119(8):4881–4985. doi: 10.1021/acs.chemrev.8b00626. [DOI] [PubMed] [Google Scholar]
- 8.Castano A.P., Mroz P., Hamblin M.R. Photodynamic therapy and anti-tumour immunity. Nat Rev Cancer. 2006;6(7):535–545. doi: 10.1038/nrc1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Y.Y., Liu X., Ma W., Xu Q., Chen G., Wang Y.F., et al. Light-activatable liposomes for repetitive on-demand drug release and immunopotentiation in hypoxic tumor therapy. Biomaterials. 2021;265 doi: 10.1016/j.biomaterials.2020.120456. [DOI] [PubMed] [Google Scholar]
- 10.Kim Y., Nam H.J., Lee J., Kim C., Yu Y.S., Kim D., et al. Methylation-dependent regulation of HIF-1α stability restricts retinal and tumour angiogenesis. Nat Commun. 2016;7:10347. doi: 10.1038/ncomms10347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li X., Lovell J.F., Yoon J., Chen X. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat Rev Clin Oncol. 2020;17(11):657–674. doi: 10.1038/s41571-020-0410-2. [DOI] [PubMed] [Google Scholar]
- 12.Guan W., Tan L., Liu X., Cui Z., Zheng Y., Yeung K.W.K., et al. Ultrasonic interfacial engineering of red phosphorous-metal for eradicating MRSA infection effectively. Adv Mater. 2021;33(5) doi: 10.1002/adma.202006047. [DOI] [PubMed] [Google Scholar]
- 13.Hanahan D., Weinberg R.A. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 14.Qian X., Zhang J., Gu Z., Chen Y. Nanocatalysts-augmented Fenton chemical reaction for nanocatalytic tumor therapy. Biomaterials. 2019;211:1–13. doi: 10.1016/j.biomaterials.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 15.Liu X., Jin Y., Liu T., Yang S., Zhou M., Wang W., et al. Iron-based theranostic nanoplatform for improving chemodynamic therapy of cancer. ACS Biomater Sci Eng. 2020;6(9):4834–4845. doi: 10.1021/acsbiomaterials.0c01009. [DOI] [PubMed] [Google Scholar]
- 16.Li S.L., Jiang P., Jiang F.L., Liu Y. Recent advances in nanomaterial-based nanoplatforms for chemodynamic cancer therapy. Adv Funct Mater. 2021;31(22) [Google Scholar]
- 17.Cao R., Sun W., Zhang Z., Li X., Du J., Fan J., et al. Protein nanoparticles containing Cu(II) and DOX for efficient chemodynamic therapy via self-generation of H2O2. Chin Chem Lett. 2020;31(12):3127–3130. [Google Scholar]
- 18.Chen J.J., Zhu Y.F., Wu C.T., Shi J.L. Nanoplatform-based cascade engineering for cancer therapy. Chem Soc Rev. 2020;49(24):9057–9094. doi: 10.1039/d0cs00607f. [DOI] [PubMed] [Google Scholar]
- 19.Wang W., Jin Y., Xu Z., Liu X., Bajwa S.Z., Khan W.S., et al. Stimuli-activatable nanomedicines for chemodynamic therapy of cancer. WIREs Nanomed Nanobiotechnol. 2020;12(4):e1614. doi: 10.1002/wnan.1614. [DOI] [PubMed] [Google Scholar]
- 20.Israel L.L., Galstyan A., Holler E., Ljubimova J.Y. Magnetic iron oxide nanoparticles for imaging, targeting and treatment of primary and metastatic tumors of the brain. J Control Release. 2020;320:45–62. doi: 10.1016/j.jconrel.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dong C., Feng W., Xu W., Yu L., Xiang H., Chen Y., et al. The coppery age: copper (Cu)-involved nanotheranostics. Adv Sci. 2020;7(21) doi: 10.1002/advs.202001549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qian X., Han X., Yu L., Xu T., Chen Y. Manganese-based functional nanoplatforms: nanosynthetic construction, physiochemical property, and theranostic applicability. Adv Funct Mater. 2020;30(3) [Google Scholar]
- 23.Wang X.W., Zhong X.Y., Lei H.L., Geng Y.H., Zhao Q., Gong F., et al. Hollow Cu2Se nanozymes for tumor photothermal-catalytic therapy. Chem Mater. 2019;31(16):6174–6186. [Google Scholar]
- 24.Hu H., Feng W., Qian X.Q., Yu L.D., Chen Y., Li Y.H. Emerging nanomedicine-enabled/enhanced nanodynamic therapies beyond traditional photodynamics. Adv Mater. 2021;33(12) doi: 10.1002/adma.202005062. [DOI] [PubMed] [Google Scholar]
- 25.Tang Z., Zhang H., Liu Y., Ni D., Zhang H., Zhang J., et al. Antiferromagnetic pyrite as the tumor microenvironment-mediated nanoplatform for self-enhanced tumor imaging and therapy. Adv Mater. 2017;29(47) doi: 10.1002/adma.201701683. [DOI] [PubMed] [Google Scholar]
- 26.Wu H., Liu L., Song L., Ma M., Gu N., Zhang Y. Enhanced tumor synergistic therapy by injectable magnetic hydrogel mediated generation of hyperthermia and highly toxic reactive oxygen species. ACS Nano. 2019;13(12):14013–14023. doi: 10.1021/acsnano.9b06134. [DOI] [PubMed] [Google Scholar]
- 27.Wang M., Wang D., Chen Q., Li C., Li Z., Lin J. Recent advances in glucose-oxidase-based nanocomposites for tumor therapy. Small. 2019;15(51) doi: 10.1002/smll.201903895. [DOI] [PubMed] [Google Scholar]
- 28.Dai Y., Cheng S., Wang Z., Zhang R., Yang Z., Wang J., et al. Hypochlorous acid promoted platinum drug chemotherapy by myeloperoxidase-encapsulated therapeutic metal phenolic nanoparticles. ACS Nano. 2018;12(1):455–463. doi: 10.1021/acsnano.7b06852. [DOI] [PubMed] [Google Scholar]
- 29.Wu W., Yu L., Jiang Q., Huo M., Lin H., Wang L., et al. Enhanced tumor-specific disulfiram chemotherapy by in situ Cu2+ chelation-initiated nontoxicity-to-toxicity transition. J Am Chem Soc. 2019;141(29):11531–11539. doi: 10.1021/jacs.9b03503. [DOI] [PubMed] [Google Scholar]
- 30.Dong Z., Feng L., Chao Y., Hao Y., Chen M., Gong F., et al. Amplification of tumor oxidative stresses with liposomal Fenton catalyst and glutathione inhibitor for enhanced cancer chemotherapy and radiotherapy. Nano Lett. 2019;19(2):805–815. doi: 10.1021/acs.nanolett.8b03905. [DOI] [PubMed] [Google Scholar]
- 31.Xu T., Ma Y., Yuan Q., Hu H., Hu X., Qian Z., et al. Enhanced ferroptosis by oxygen-boosted phototherapy based on a 2-in-1 nanoplatform of ferrous hemoglobin for tumor synergistic therapy. ACS Nano. 2020;14(3):3414–3425. doi: 10.1021/acsnano.9b09426. [DOI] [PubMed] [Google Scholar]
- 32.Hu R., Fang Y., Huo M., Yao H., Wang C., Chen Y., et al. Ultrasmall Cu2-XS nanodots as photothermal-enhanced Fenton nanocatalysts for synergistic tumor therapy at NIR-II biowindow. Biomaterials. 2019;206:101–114. doi: 10.1016/j.biomaterials.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 33.Zhang L., Wan S.S., Li C.X., Xu L., Cheng H., Zhang X.Z. An adenosine triphosphate-responsive autocatalytic Fenton nanoparticle for tumor ablation with self-supplied H2O2 and acceleration of Fe(III)/Fe(II) conversion. Nano Lett. 2018;18(12):7609–7618. doi: 10.1021/acs.nanolett.8b03178. [DOI] [PubMed] [Google Scholar]
- 34.Ding B., Zheng P., Jiang F., Zhao Y., Wang M., Chang M., et al. MnO(x) nanospikes as nanoadjuvants and immunogenic cell death drugs with enhanced antitumor immunity and antimetastatic effect. Angew Chem Int Edit. 2020;59(38):16381–16384. doi: 10.1002/anie.202005111. [DOI] [PubMed] [Google Scholar]
- 35.Han Y., Gao S., Zhang Y., Ni Q., Li Z., Liang X.J., et al. Metal-based nanocatalyst for combined cancer therapeutics. Bioconjug Chem. 2020;31(5):1247–1258. doi: 10.1021/acs.bioconjchem.0c00194. [DOI] [PubMed] [Google Scholar]
- 36.Chen Q., Yang D., Yu L., Jing X., Chen Y. Catalytic chemistry of iron-free Fenton nanocatalysts for versatile radical nanotherapeutics. Mater Horiz. 2020;7(2):317–337. [Google Scholar]
- 37.Zhang C., Bu W., Ni D., Zhang S., Li Q., Yao Z., et al. Synthesis of iron nanometallic glasses and their application in cancer therapy by a localized Fenton reaction. Angew Chem Int Edit. 2016;55(6):2101–2106. doi: 10.1002/anie.201510031. [DOI] [PubMed] [Google Scholar]
- 38.Huo M., Wang L., Chen Y., Shi J. Tumor-selective catalytic nanomedicine by nanocatalyst delivery. Nat Commun. 2017;8:357. doi: 10.1038/s41467-017-00424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan C., Ou M., Cheng Q., Zhou Y., Yu Y., Li Z., et al. Z-scheme heterojunction functionalized pyrite nanosheets for modulating tumor microenvironment and strengthening photo/chemodynamic therapeutic effects. Adv Funct Mater. 2020;30(3) [Google Scholar]
- 40.Chen Y., Li Z.H., Pan P., Hu J.J., Cheng S.X., Zhang X.Z. Tumor-microenvironment-triggered ion exchange of a metal-organic framework hybrid for multimodal imaging and synergistic therapy of tumors. Adv Mater. 2020;32(24) doi: 10.1002/adma.202001452. [DOI] [PubMed] [Google Scholar]
- 41.Zheng D.W., Lei Q., Zhu J.Y., Fan J.X., Li C.X., Li C., et al. Switching apoptosis to ferroptosis: metal–organic network for high-efficiency anticancer therapy. Nano Lett. 2016;17(1):284–291. doi: 10.1021/acs.nanolett.6b04060. [DOI] [PubMed] [Google Scholar]
- 42.Chen G., Yang Y., Xu Q., Ling M., Lin H., Ma W., et al. Self-amplification of tumor oxidative stress with degradable metallic complexes for synergistic cascade tumor therapy. Nano Lett. 2020;20(11):8141–8150. doi: 10.1021/acs.nanolett.0c03127. [DOI] [PubMed] [Google Scholar]
- 43.Ranji-Burachaloo H., Gurr P.A., Dunstan D.E., Qiao G.G. Cancer treatment through nanoparticle-facilitated Fenton reaction. ACS Nano. 2018;12(12):11819–11837. doi: 10.1021/acsnano.8b07635. [DOI] [PubMed] [Google Scholar]
- 44.Shen Z., Song J., Yung B.C., Zhou Z., Wu A., Chen X. Emerging strategies of cancer therapy based on ferroptosis. Adv Mater. 2018;30(12) doi: 10.1002/adma.201704007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu M., Liu B., Liu Q., Du K., Wang Z., He N. Nanomaterial-induced ferroptosis for cancer specific therapy. Coordin Chem Rev. 2019;382:160–180. [Google Scholar]
- 46.Chen Y., Huang Y., Zhou S., Sun M., Chen L., Wang J., et al. Tailored chemodynamic nanomedicine improves pancreatic cancer treatment via controllable damaging neoplastic cells and reprogramming tumor microenvironment. Nano Lett. 2020;20(9):6780–6790. doi: 10.1021/acs.nanolett.0c02622. [DOI] [PubMed] [Google Scholar]
- 47.Zanganeh S., Hutter G., Spitler R., Lenkov O., Mahmoudi M., Shaw A., et al. Iron oxide nanoparticles inhibit tumour growth by inducing pro-inflammatory macrophage polarization in tumour tissues. Nat Nanotechnol. 2016;11(11):986–994. doi: 10.1038/nnano.2016.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ren Z.G., Sun S.C., Sun R.R., Cui G.Y., Hong L.J., Rao B.C., et al. A metal-polyphenol-coordinated nanomedicine for synergistic cascade cancer chemotherapy and chemodynamic therapy. Adv Mater. 2020;32(6) doi: 10.1002/adma.201906024. [DOI] [PubMed] [Google Scholar]
- 49.Zhao Z., Zhou Z., Bao J., Wang Z., Hu J., Chi X., et al. Octapod iron oxide nanoparticles as high-performance T-2 contrast agents for magnetic resonance imaging. Nat Commun. 2013;4:2266. doi: 10.1038/ncomms3266. [DOI] [PubMed] [Google Scholar]
- 50.Zhao P., Tang Z., Chen X., He Z., He X., Zhang M., et al. Ferrous-cysteine–phosphotungstate nanoagent with neutral pH Fenton reaction activity for enhanced cancer chemodynamic therapy. Mater Horiz. 2019;6(2):369–374. [Google Scholar]
- 51.Masomboon N., Ratanatamskul C., Lu M.C. Chemical oxidation of 2,6-dimethylaniline in the Fenton process. Environ Sci Technol. 2009;43(22):8629–8634. doi: 10.1021/es802274h. [DOI] [PubMed] [Google Scholar]
- 52.Lin L.S., Huang T., Song J., Ou X.Y., Wang Z., Deng H., et al. Synthesis of copper peroxide nanodots for H2O2 self-supplying chemodynamic therapy. J Am Chem Soc. 2019;141(25):9937–9945. doi: 10.1021/jacs.9b03457. [DOI] [PubMed] [Google Scholar]
- 53.Wang Y.L., Li Z.L., Hu Y., Liu J., Guo M.Y., Wei H.X., et al. Photothermal conversion-coordinated Fenton-like and photocatalytic reactions of Cu2-xSe-Au Janus nanoparticles for tri-combination antitumor therapy. Biomaterials. 2020;255 doi: 10.1016/j.biomaterials.2020.120167. [DOI] [PubMed] [Google Scholar]
- 54.Ni K., Aung T., Li S., Fatuzzo N., Liang X., Lin W. Nanoscale metal-organic framework mediates radical therapy to enhance cancer immunotherapy. Chem. 2019;5(7):1892–1913. doi: 10.1016/j.chempr.2019.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 55.Li L., Yang Z., Fan W., He L., Cui C., Zou J., et al. In situ polymerized hollow mesoporous organosilica biocatalysis nanoreactor for enhancing ROS-mediated anticancer therapy. Adv Funct Mater. 2020;30(4) doi: 10.1002/adfm.201907716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang T.T., Zhang H., Liu H.H., Yuan Q., Ren F., Han Y.B., et al. Boosting H2O2-guided chemodynamic therapy of cancer by enhancing reaction kinetics through versatile biomimetic Fenton nanocatalysts and the second near-infrared light irradiation. Adv Funct Mater. 2020;30(3) [Google Scholar]
- 57.Ember E., Rothbart S., Puchta R., van Eldik R. Metal ion-catalyzed oxidative degradation of orange II by H2O2. High catalytic activity of simple manganese salts. New J Chem. 2009;33(1):34–49. [Google Scholar]
- 58.Lin L.S., Song J., Song L., Ke K., Liu Y., Zhou Z., et al. Simultaneous Fenton-like ion delivery and glutathione depletion by MnO2-based nanoagent to enhance chemodynamic therapy. Angew Chem Int Edit. 2018;57(18):4902–4906. doi: 10.1002/anie.201712027. [DOI] [PubMed] [Google Scholar]
- 59.Ding B., Zheng P., Ma P.a., Lin J. Manganese oxide nanomaterials: synthesis, properties, and theranostic applications. Adv Mater. 2020;32(10) doi: 10.1002/adma.201905823. [DOI] [PubMed] [Google Scholar]
- 60.Bi H., Dai Y., Yang P., Xu J., Yang D., Gai S., et al. Glutathione and H2O2 consumption promoted photodynamic and chemotherapy based on biodegradable MnO2-Pt@Au-25 nanosheets. Chem Eng J. 2019;356:543–553. [Google Scholar]
- 61.Gao S., Jin Y., Ge K., Li Z., Liu H., Dai X., et al. Self-supply of O2 and H2O2 by a nanocatalytic medicine to enhance combined chemo/chemodynamic therapy. Adv Sci. 2019;6(24) doi: 10.1002/advs.201902137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang Y., Liu Y., Xu J. Separation of hydrogen sulfide from gas phase using Ce3+/Mn2+-enhanced Fenton-like oxidation system. Chem Eng J. 2019;359:1486–1492. [Google Scholar]
- 63.Duan L.Y., Wang Y.J., Liu J.W., Wang Y.M., Li N., Jiang J.H. Tumor-selective catalytic nanosystem for activatable theranostics. Chem Commun. 2018;54(59):8214–8217. doi: 10.1039/c8cc03922d. [DOI] [PubMed] [Google Scholar]
- 64.Lewinski N., Colvin V., Drezek R. Cytotoxicity of nanoparticles. Small. 2008;4(1):26–49. doi: 10.1002/smll.200700595. [DOI] [PubMed] [Google Scholar]
- 65.Liu L., Kong L. Research progress on the carcinogenicity of metal nanomaterials. J Appl Toxicol. 2021;41(9):1334–1344. doi: 10.1002/jat.4145. [DOI] [PubMed] [Google Scholar]
- 66.Demokritou P., Gass S., Pyrgiotakis G., Cohen J.M., Goldsmith W., McKinney W., et al. An in vivo and in vitro toxicological characterisation of realistic nanoscale CeO2 inhalation exposures. Nanotoxicology. 2013;7(8):1338–1350. doi: 10.3109/17435390.2012.739665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tang Z., Liu Y., He M., Bu W. Chemodynamic therapy: tumour microenvironment-mediated Fenton and fenton-like reactions. Angew Chem Int Edit. 2019;58(4):946–956. doi: 10.1002/anie.201805664. [DOI] [PubMed] [Google Scholar]
- 68.Guo Y., Zhang X., Sun W., Jia H.R., Zhu Y.X., Zhang X., et al. Metal-phenolic network-based nanocomplexes that evoke ferroptosis by apoptosis: promoted nuclear drug influx and reversed drug resistance of cancer. Chem Mater. 2019;31(24):10071–10084. [Google Scholar]
- 69.Dai Z., Tang J., Gu Z., Wang Y., Yang Y., Yang Y., et al. Eliciting immunogenic cell death via a unitized nanoinducer. Nano Lett. 2020;20(9):6246–6254. doi: 10.1021/acs.nanolett.0c00713. [DOI] [PubMed] [Google Scholar]
- 70.Ding B., Shao S., Jiang F., Dang P., Sun C., Huang S., et al. MnO2-disguised upconversion hybrid nanocomposite: an ideal architecture for tumor microenvironment-triggered UCL/MR bioimaging and enhanced chemodynamic therapy. Chem Mater. 2019;31(7):2651–2660. [Google Scholar]
- 71.Liu C., Wang D., Zhang S., Cheng Y., Yang F., Xing Y., et al. Biodegradable biomimic copper/manganese silicate nanospheres for chemodynamic/photodynamic synergistic therapy with simultaneous glutathione depletion and hypoxia relief. ACS Nano. 2019;13(4):4267–4277. doi: 10.1021/acsnano.8b09387. [DOI] [PubMed] [Google Scholar]
- 72.Wang T.T., Zhang H., Han Y.B., Liu H.H., Ren F., Zeng J.F., et al. Light-enhanced O2-evolving nanoparticles boost photodynamic therapy to elicit antitumor immunity. ACS Appl Mater Inter. 2019;11(18):16367–16379. doi: 10.1021/acsami.9b03541. [DOI] [PubMed] [Google Scholar]
- 73.Lin X., Liu S., Zhang X., Zhu R., Chen S., Chen X., et al. An ultrasound activated vesicle of Janus Au-MnO nanoparticles for promoted tumor penetration and sono-chemodynamic therapy of orthotopic liver cancer. Angew Chem Int Edit. 2020;59(4):1682–1688. doi: 10.1002/anie.201912768. [DOI] [PubMed] [Google Scholar]
- 74.Tian Q.Q., An L., Tian Q.W., Lin J.M., Yang S.P. Ellagic acid-Fe@BSA nanoparticles for endogenous H2S accelerated Fe(III)/Fe(II) conversion and photothermal synergistically enhanced chemodynamic therapy. Theranostics. 2020;10(9):4101–4115. doi: 10.7150/thno.41882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Du Y., Yang C., Li F., Liao H., Chen Z., Lin P., et al. Core-shell-satellite nanomaces as remotely controlled self-fueling fenton reagents for imaging-guided triple-negative breast cancer-specific therapy. Small. 2020;16(31) doi: 10.1002/smll.202002537. [DOI] [PubMed] [Google Scholar]
- 76.Liu Y., Wu J., Jin Y., Zhen W., Wang Y., Liu J., et al. Copper(I) phosphide nanocrystals for in situ self-generation magnetic resonance imaging-guided photothermal-enhanced chemodynamic synergetic therapy resisting deep-seated tumor. Adv Funct Mater. 2019;29(50) [Google Scholar]
- 77.Liu Y., Zhen W., Wang Y., Liu J., Jin L., Zhang T., et al. One-dimensional Fe2P acts as a fenton agent in response to NIR II light and ultrasound for deep tumor synergetic theranostics. Angew Chem Inter Edit. 2019;58(8):2407–2412. doi: 10.1002/anie.201813702. [DOI] [PubMed] [Google Scholar]
- 78.Duan H., Guo H., Zhang R., Wang F., Liu Z., Ge M., et al. Two-dimensional silicene composite nanosheets enable exogenous/endogenous-responsive and synergistic hyperthermia-augmented catalytic tumor theranostics. Biomaterials. 2020;256 doi: 10.1016/j.biomaterials.2020.120206. 120206. [DOI] [PubMed] [Google Scholar]
- 79.Fang C., Deng Z., Cao G., Chu Q., Wu Y., Li X., et al. Co–ferrocene MOF/glucose oxidase as cascade nanozyme for effective tumor therapy. Adv Funct Mater. 2020;30(16) [Google Scholar]
- 80.Feng L., Xie R., Wang C., Gai S., He F., Yang D., et al. Magnetic targeting, tumor microenvironment-responsive intelligent nanocatalysts for enhanced tumor ablation. ACS Nano. 2018;12(11):11000–11012. doi: 10.1021/acsnano.8b05042. [DOI] [PubMed] [Google Scholar]
- 81.Chang M., Hou Z., Jin D., Zhou J., Wang M., Wang M., et al. Colorectal tumor microenvironment-activated bio-decomposable and metabolizable Cu2O@CaCO(3)nanocomposites for synergistic oncotherapy. Adv Mater. 2020;32(43) doi: 10.1002/adma.202004647. [DOI] [PubMed] [Google Scholar]
- 82.Guo Y., Jia H.R., Zhang X., Zhang X., Sun Q., Wang S.Z., et al. A glucose/oxygen-exhausting nanoreactor for starvation- and hypoxia-activated sustainable and cascade chemo-chemodynamic therapy. Small. 2020;16(31) doi: 10.1002/smll.202000897. [DOI] [PubMed] [Google Scholar]
- 83.Fu L.H., Hu Y.R., Qi C., He T., Jiang S., Jiang C., et al. Biodegradable manganese-doped calcium phosphate nanotheranostics for traceable cascade reaction-enhanced anti-tumor therapy. ACS Nano. 2019;13(12):13985–13994. doi: 10.1021/acsnano.9b05836. [DOI] [PubMed] [Google Scholar]
- 84.Zhu J., Chu C., Li D., Pang X., Zheng H., Wang J., et al. Fe(III)-porphyrin sonotheranostics: a green triple-regulated ROS generation nanoplatform for enhanced cancer imaging and therapy. Adv Funct Mater. 2019;29(36) [Google Scholar]
- 85.Wan X., Zhong H., Pan W., Li Y., Chen Y., Li N., et al. Programmed release of dihydroartemisinin for synergistic cancer therapy using CaCO3 mineralized metal-organic framework. Angew Chem Inter Edit. 2019;58(40):14134–14139. doi: 10.1002/anie.201907388. [DOI] [PubMed] [Google Scholar]
- 86.Chang M., Wang M., Wang M., Shu M., Ding B., Li C., et al. Hou Z., Lin J. A multifunctional cascade bioreactor based on hollow-structured Cu2MoS4 for synergetic cancer chemo-dynamic therapy/starvation therapy/phototherapy/immunotherapy with remarkably enhanced efficacy. Adv Mater. 2019;31(51) doi: 10.1002/adma.201905271. [DOI] [PubMed] [Google Scholar]
- 87.Zhong X.Y., Wang X.W., Cheng L., Tang Y.A., Zhan G.T., Gong F., et al. GSH-depleted PtCu3 nanocages for chemodynamic- enhanced sonodynamic cancer therapy. Adv Funct Mater. 2020;30(4) [Google Scholar]
- 88.Qin S.Y., Zhang A.Q., Cheng S.X., Rong L., Zhang X.Z. Drug self-delivery systems for cancer therapy. Biomaterials. 2017;112:234–247. doi: 10.1016/j.biomaterials.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 89.Qin Y., Guo Q., Wu S.J., Huang C.L., Zhang Z.M., Zhang L., et al. LHRH/TAT dual peptides-conjugated polymeric vesicles for PTT enhanced chemotherapy to overcome hepatocellular carcinoma. Chinese Chem Lett. 2020;31(12):3121–3126. [Google Scholar]
- 90.Ma W., Chen Q., Xu W., Yu M., Yang Y., Zou B., et al. Self-targeting visualizable hyaluronate nanogel for synchronized intracellular release of doxorubicin and cisplatin in combating multidrug-resistant breast cancer. Nano Res. 2021;14(3):846–857. [Google Scholar]
- 91.Meng X., Zhang X., Liu M., Cai B., He N., Wang Z. Fenton reaction-based nanomedicine in cancer chemodynamic and synergistic therapy. Appl Mater Today. 2020;21 [Google Scholar]
- 92.Wang S., Wang Z., Yu G., Zhou Z., Jacobson O., Liu Y., et al. Tumor-specific drug release and reactive oxygen species generation for cancer chemo/chemodynamic combination therapy. Adv Sci. 2019;6(5) doi: 10.1002/advs.201801986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lan G., Ni K., Veroneau S.S., Feng X., Nash G.T., Luo T., et al. Titanium-based nanoscale metal-organic framework for type i photodynamic therapy. J Am Chem Soc. 2019;141(10):4204–4208. doi: 10.1021/jacs.8b13804. [DOI] [PubMed] [Google Scholar]
- 94.Yu L., Wang Z., Mo Z., Zou B., Yang Y., Sun R., et al. Synergetic delivery of triptolide and Ce6 with light-activatable liposomes for efficient hepatocellular carcinoma therapy. Acta Pharm Sin B. 2021;11(7):2004–2015. doi: 10.1016/j.apsb.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dolmans D., Fukumura D., Jain R.K. Photodynamic therapy for cancer. Nat Rev Cancer. 2003;3(5):380–387. doi: 10.1038/nrc1071. [DOI] [PubMed] [Google Scholar]
- 96.Li L., Chen Y., Chen W., Tan Y., Chen H., Yin J. Photodynamic therapy based on organic small molecular fluorescent dyes. Chin Chem Lett. 2019;30(10):1689–1703. [Google Scholar]
- 97.Barker H.E., Paget J.T.E., Khan A.A., Harrington K.J. The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nat Rev Cancer. 2015;15(7):409–425. doi: 10.1038/nrc3958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liang S., Deng X., Ma P.a., Cheng Z., Lin J. Recent advances in nanomaterial-assisted combinational sonodynamic cancer therapy. Adv Mater. 2020;32(47) doi: 10.1002/adma.202003214. [DOI] [PubMed] [Google Scholar]
- 99.Wang K., Yang P., Guo R.R., Yao X.X., Yang W.L. Photothermal performance of MFe2O4 nanoparticles. Chin Chem Lett. 2019;30(12):2013–2016. [Google Scholar]
- 100.Yang Z., Tian R., Wu J., Fan Q., Yung B.C., Niu G., et al. Impact of semiconducting perylene diimide nanoparticle size on lymph node mapping and cancer imaging. ACS Nano. 2017;11(4):4247–4255. doi: 10.1021/acsnano.7b01261. [DOI] [PubMed] [Google Scholar]
- 101.Li W., Wang S., Ren C., Liu P., Lu Q., Yang L., et al. Exo/endogenous dual-augmented chemodynamic therapy based on bioreducible and bio-breakable copper (coproduct)-based truncated octahedron. Chem Eng J. 2020;396 [Google Scholar]
- 102.Fu L.H., Qi C., Lin J., Huang P. Catalytic chemistry of glucose oxidase in cancer diagnosis and treatment. Chem Soc Rev. 2018;47(17):6454–6472. doi: 10.1039/c7cs00891k. [DOI] [PubMed] [Google Scholar]
- 103.Couzin-Frankel J. Cancer immunotherapy. Science. 2013;342(6165):1432–1433. doi: 10.1126/science.342.6165.1432. [DOI] [PubMed] [Google Scholar]
- 104.Cho N.H., Cheong T.C., Min J.H., Wu J.H., Lee S.J., Kim D., et al. A multifunctional core-shell nanoparticle for dendritic cell-based cancer immunotherapy. Nat Nanotechnol. 2011;6(10):675–682. doi: 10.1038/nnano.2011.149. [DOI] [PubMed] [Google Scholar]
- 105.Hu Y.Y., Lin L., Guo Z.P., Chen J., Maruyama A., Tian H.Y., et al. In situ vaccination and gene-medeiated PD-L1 blockade for enhanced tumor immunotherapy. Chin Chem Lett. 2021;32(5):1770–1774. [Google Scholar]
- 106.Ma Y., Zhang Y., Li X., Zhao Y., Li M., Jiang W., et al. Near-infrared II phototherapy induces deep tissue immunogenic cell death and potentiates cancer immunotherapy. ACS Nano. 2019;13(10):11967–11980. doi: 10.1021/acsnano.9b06040. [DOI] [PubMed] [Google Scholar]
- 107.Sun Y.J., Feng X.R., Wan C., Lovell J.F., Jin H.L., Ding J.X. Role of nanoparticle-mediated immunogenic cell death in cancer immunotherapy. Asian J Pharm Sci. 2021;16(2):129–132. doi: 10.1016/j.ajps.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Duan X., Chan C., Lin W. Nanoparticle-mediated immunogenic cell death enables and potentiates cancer immunotherapy. Angew Chem Int Edit. 2019;58(3):670–680. doi: 10.1002/anie.201804882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fan W., Yung B., Huang P., Chen X. Nanotechnology for multimodal synergistic cancer therapy. Chem Rev. 2017;117(22):13566–13638. doi: 10.1021/acs.chemrev.7b00258. [DOI] [PubMed] [Google Scholar]
- 110.Sava Gallis D.F., Rohwer L.E.S., Rodriguez M.A., Barnhart -Dailey M.C., Butler K.S., Luk T.S., et al. Multifunctional, tunable metal-organic framework materials platform for bioimaging applications. ACS Appl Mater Inter. 2017;9(27):22268–22277. doi: 10.1021/acsami.7b05859. [DOI] [PubMed] [Google Scholar]
- 111.Siafaka P.I., Okur N.U., Karantas I.D., Okur M.E., Gundogdu E.A. Current update on nanoplatforms as therapeutic and diagnostic tools: a review for the materials used as nanotheranostics and imaging modalities. Asian J Pharm Sci. 2021;16(1):24–46. doi: 10.1016/j.ajps.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Na H.B., Song I.C., Hyeon T. Inorganic nanoparticles for MRI contrast agents. Adv Mater. 2009;21(21):2133–2148. [Google Scholar]
- 113.Yang L., Cao Z., Sajja H.K., Mao H., Wang L., Geng H., et al. Development of receptor targeted magnetic iron oxide nanoparticles for efficient drug delivery and tumor imaging. J Biomed Nanotechnol. 2008;4(4):439–449. doi: 10.1166/jbn.2008.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Liu P., Shi X., Zhong S., Peng Y., Qi Y., Ding J., et al. Metal-phenolic networks for cancer theranostics. Biomater Sci. 2021;9(8):2825–2849. doi: 10.1039/d0bm02064h. [DOI] [PubMed] [Google Scholar]
- 115.Manohar S., Gambhir S.S. Clinical photoacoustic imaging. Photoacoustics. 2020;19 doi: 10.1016/j.pacs.2020.100196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Balendiran G.K., Dabur R., Fraser D. The role of glutathione in cancer. Cell Biochem Funct. 2004;22(6):343–352. doi: 10.1002/cbf.1149. [DOI] [PubMed] [Google Scholar]
- 117.Wilhelm S., Tavares A.J., Dai Q., Ohta S., Audet J., Dvorak H.F., et al. Analysis of nanoparticle delivery to tumours. Adv Drug Deliv Rev. 2016;1(5):16014. [Google Scholar]