Abstract
AIM
To compare the effectiveness of network-based perception learning (NBPL) and traditional training in the treatment of amblyopia children.
METHODS
This randomized controlled clinical trial recruited 56 participants aged 4-12y with anisometropic and/or strabismic amblyopia. Participants were randomly divided into two groups: the NBPL group (n=28) who received patching and NBPL for 3mo, and the control group (n=28) who got 3mo of patching and traditional training. Best-corrected visual acuity (BCVA) in the amblyopic eye and stereoacuity were measured and compared at baseline, 1, 2, and 3mo post-randomization.
RESULTS
There were no significant differences in age, gender ratio, and BCVA between the two groups at baseline. At 3mo, most patients gained lines (2 logMAR lines on average) of BCVA in both groups except one 11-year-old girl in the control group (P<0.05). But no significant difference in BCVA improvement of the amblyopic eye between the two groups was found (P=0.725), and amblyopia resolved (BCVA of 0.1 logMAR or better or within 1 logMAR line of the fellow eye) for 13 (46.4%) participants in both groups. The number of patients with improvement of stereoacuity was 25 and 13 in the NBPL group and control group (P=0.041), respectively, and a significant difference exists in the distribution of stereopsis at 3mo between the two groups (P=0.015). Besides, in patients with measurable stereopsis improvement degree and space for improvement in the two groups, the NBPL group also achieved better stereoscopic improvement than the control group (10/11 vs 4/11, P<0.05).
CONCLUSION
The NBPL system has a significant effect on the improvement of BCVA and stereoacuity of amblyopia children and is better than traditional training in terms of stereoacuity improvement. Perceptual learning visual training may play a more important role in the treatment of amblyopia in the future.
Keywords: amblyopia, perceptual learning, stereoacuity, best-corrected visual acuity
INTRODUCTION
Amblyopia reduces the best-corrected visual acuity (BCVA) of one or both eyes without any organic cause. It is a common eye disease and the most common cause of vision loss among children and adults, with the pooled prevalence rate of amblyopia was about 1.44%[1]. Amblyopia affects vision and visual function, such as spatial resolution, contrast sensitivity, color vision, stereoscopic vision, which have different effects on all aspects of life[2]–[4].
For centuries the main approach to the treatment of amblyopia consisted of optical correction of any refractive error and occlusion or penalization of the “strong” eye, thus “forcing” the brain to use the input from the “weaker” amblyopic eye[5]. However, it does not help much in building binocular function. Furthermore, due to the lack of binocular vision, there is always a high recurrence rate, and some patients have residual amblyopia[6]. Research in recent years suggested that binocular cortical communication persists in subjects with amblyopia[7]–[8]. These findings prompted that activation of these persistent binocular neural circuits might be exploited to ‘awaken’ an amblyopic eye. Therefore, binocular vision training is considered necessary to treat amblyopia, which is essential for establishing visual function[9]–[11].
In the past, we used traditional visual training eyesight exercises to improve children's stereoacuity, such as needle threading, wearing beads, and tracing. Nowadays, with the development of computer technology, many visual perception trainings have emerged[12]–[14]. Visual perceptual learning is the improvement in visual task performance with practice or training. It reflects learning and plasticity in the visual system and a network of other brain substrates of behavior[15]–[17]. Visual perceptual learning has been used to improve visual performance in different conditions, including amblyopia, presbyopia, low vision, cortical blindness, and rehabilitation after surgical interventions[16],[18]–[20].
The network-based perception learning (NBPL) system is a multimedia bio-stimulation perceptual learning software program. The program directly targets the binocular function using dichoptic presentation and presents 3D images using a complete split screen view. The program is based on visual biometric information stimulation and has various perceptual learning training games, making the training process attractive. It utilizes cloud medical technology; when the data center receives the patient's visual function test results or medical record data uploaded by the client, the intelligent expert system in the cloud can instantly develop targeted, individualized visual training plans for amblyopia patients. With this program, all patients' treatment information will be preserved, facilitating the doctor's tracking and management of the patient's treatment.
It is unclear whether visual perceptual training or traditional training is better in the treatment of amblyopia, especially in the improvement of visual acuity (VA) and stereopsis. Therefore, we evaluated the effectiveness of visual perceptual training in untreated amblyopic children between 4-12y using the NBPL system.
SUBJECTS AND METHODS
Ethical Approval
The study protocol was approved by the Ethics Committee of Tongji Hospital affiliated to Tongji University in Shanghai. Detailed signed informed consent was obtained from each subject and their guardians before the research. Trial registration: Chinese Clinical Trial Registry, ChiCTR. Trial ID: ChiCTR1800015444. Registered March 30, 2018.
Methods
This study is a randomized controlled trial to assess the effectiveness of a network vision treatment for amblyopia. Between February 20, 2016, and May 20, 2018, a total of 56 amblyopic subjects (25 males, 31 females) with a mean age of 6.7y (range, 4-12y) were enrolled in this study.
Inclusion Criteria
Participants were recruited via ophthalmologists in Tongji Hospital affiliated to Tongji University, Shanghai. Eligible children 4 to 12 years old were diagnosed as having anisometropic and/or strabismic amblyopia. All patients underwent a baseline ophthalmological examination, including visual testing, manifest and cycloplegic refraction, cover test, Worth four dot test, anterior segment examination with the slit lamp, corneal topography, and funduscopy. The eligible children had amblyopic eye BCVA of 0.2 to 1.0 logMAR (20/32 to 20/200). Children who had prior treatment with either patching or atropine penalization were not eligible for recruitment providing.
Exclusion Criteria
None of the children had systemic disease, congenital infections, malformations, or coexisting ocular disease (previous ocular surgery, corneal irregularity, opacification of ocular media including cataracts, and active ocular disease).
Protocol
Participants that met the inclusion criteria were randomly assigned to either NBPL group (n=28) or control group (n=28) based on the random number table method. After being enrolled in the two groups, they were given corresponding treatment. All results were based on the comparison between NBPL and the control group. Because of the small sample size, we did not further stratify the analysis within the group.
NBPL group (n=28) and the control group (n=28) got patching and corresponding training (NBPL and traditional training) for 3mo. Follow-up was performed at 1, 2, and 3mo after treatment in both groups. BCVA and visual function tests were performed, including three-level visual function examination using synoptophore and a comprehensive refractometer. Unfortunately, the total number of samples is small, so it is not enough for further subgroup analysis.
VA was measured with a standard logarithmic VA chart. The stereoacuity was automatically determined according to the stereoscopic test in the NBPL system. Patients in the NBPL group were instructed to do NBPL with red/green anaglyphic glasses and optical correction if applicable.
Vision Training
Examine of stereoacuity
Stereoacuity was carried out by line-element stereograms in NBPL program and guided by the same doctor on the same computer. Each test was repeated 3 times to obtain stable results.
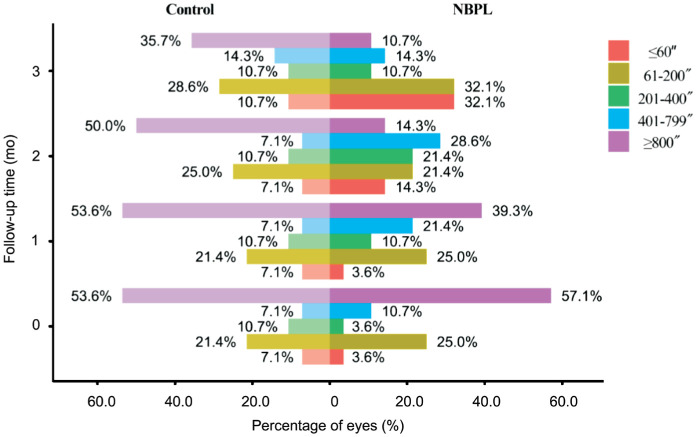
Network-based perception learning
Multimedia bio-stimulation perceptual learning visual training system (Guangzhou Vision Medical Software Co., Ltd., China) was used to train amblyopia in the NBPL group. After the patient's name, age, treatment history, VA, BCVA, diopter, eye movement, eye position, simultaneous vision function, fusion function, and stereoscopic function were input into the treatment system, the system automatically generated a treatment plan, which contained stimulation training, fine training, simultaneous visual training, fusion training and stereoscopic training (Figure 1). The training time and training program differed depending on the BCVA of the amblyopia eye. Amblyopia eye with BCVA worse than 0.4 logMAR was trained separately, with 15min each time, twice a day, and 5min between two times. If the BCVA of amblyopia eye was better than 0.4 logMAR, and the BCVA difference between two eyes was less than 3 lines, both eyes were trained simultaneously, 15min each time, twice a day. When BCVA of amblyopia eye increased to 0.2 logMAR, and BCVA difference between eyes did not exceed 2 lines, simultaneous vision, fusion training, and stereo training were added. Exotropia patients did the convergence training when they had the fusion function, and esotropia patients did the separate training. All trainings were done via computer (recommended display setting: monitor screen size: 19-inch or larger; refresh rate: 60 Hz; resolution 1920×1080; color depth: true color/24-bit). Patients could visit the hospital for training or use their computers to conduct online training at home. The ophthalmologist monitored the patient's daily training through network back-end management software.
Figure 1. Examples of the training methods in network-based perception learning training system.
The system recorded the patient's training time and performance in each training module. Based on the patient's compliance and accuracy rate, a training score from level 1 to level 5 was given and result was sent to the ophthalmologist. If there was a sudden change larger than 2 levels, the ophthalmologist had to contact the patient for follow up and decide if any adjustment needed to be made.
Traditional comprehensive training
The control group was treated according to the traditional training method. A total of 28 children of developmental amblyopia underwent traditional exercise, such as needle threading, wearing beads, and tracing, etc. The training duration and policy were the same as that of the NBPL group, except for the training method.
Statistical Analysis
StataMP 13 (StataCorp LP, College Station, Texas, USA) was used for statistical analysis, and R 3.5.1 (R Development Core Team, New Zealand) was used for graphical display. The stereoacuity was represented by the median (25%, 75%). The primary outcome was a change in amblyopic eye BCVA and the distribution of stereoacuity. The change in amblyopic eye BCVA from baseline to 3mo post-randomization between the two groups was compared with independent-samples t-test. The distribution of stereoacuity at 3mo was compared with CMH Chi-square test.
RESULTS
A total of 56 patients were enrolled in the study, with 28 randomized to the network-based perception treatment and 28 to traditional treatment. All 56 children completed the 3mo visit. There was no dropout during the trial.
Patient Characteristics
Baseline characteristics are listed in Table 1. Seven children (12.5%) had strabismic amblyopia, 45 (80.36%) had anisometropic amblyopia, and 4 children (7.14%) had combined-mechanism amblyopia. Their mean age was 6.71y (age range, 4-12y), and 25 (44.64%) patients were male. The mean (SD) amblyopic eye BCVA at enrollment was 0.42 logMAR [approximately 20/52; range, 0.2-1.0 logMAR (20/32 to 20/200)]. Mild amblyopia [0.1-0.2 logMAR (20/25 to 20/32)] was present in 12 children (21.43%), moderate amblyopia [range, 0.3-0.6 logMAR (20/40 to 20/80)] was present in 36 children (64.29%), and severe amblyopia [range, 0.7-1.0 logMAR (20/100 to 20/200)] was present in 8 cases (14.29%). None children had received prior amblyopia treatment.
Table 1. Baseline characteristic of randomized participants in groups.
| Characteristic | NBPL group (n=28) | Control group (n=28) | P |
| Female | 15 | 16 | >0.05 |
| Age (y) | >0.05 | ||
| 4 to <5 | 4 | 3 | |
| 5 to <7 | 10 | 12 | |
| 7 to <9 | 9 | 9 | |
| 9 to <12 | 5 | 4 | |
| Mean±SD | 6.79±2.06 | 6.64±1.77 | |
| Distance amblyopic-eye BCVA (logMAR) | >0.05 | ||
| 1 | 1 | 0 | |
| 0.9 | 0 | 1 | |
| 0.8 | 1 | 2 | |
| 0.7 | 2 | 1 | |
| 0.6 | 2 | 3 | |
| 0.5 | 3 | 3 | |
| 0.4 | 7 | 6 | |
| 0.3 | 5 | 7 | |
| 0.2 | 7 | 5 | |
| Mean±SD (logMAR) | 0.41±0.21 | 0.43±0.20 | |
| Baseline stereoacuity (second of arc) | >0.05 | ||
| ≥800 | 16 | 15 | |
| 401-800 | 3 | 2 | |
| 201-400 | 1 | 3 | |
| 61-200 | 7 | 6 | |
| ≤60 | 1 | 2 | |
| Amblyopia cuase | >0.05 | ||
| Strbismus | 3 | 4 | |
| Anisometropia | 23 | 22 | |
| Combined | 2 | 2 | |
NBPL: Network-based perception learning; BCVA: Best-corrected visual acuity; SD: Standard deviation.
There were no significant differences in age, gender ratio, and BCVA between the two groups, as shown in Table 1.
Amblyopic-Eye Best-Corrected Visual Acuity
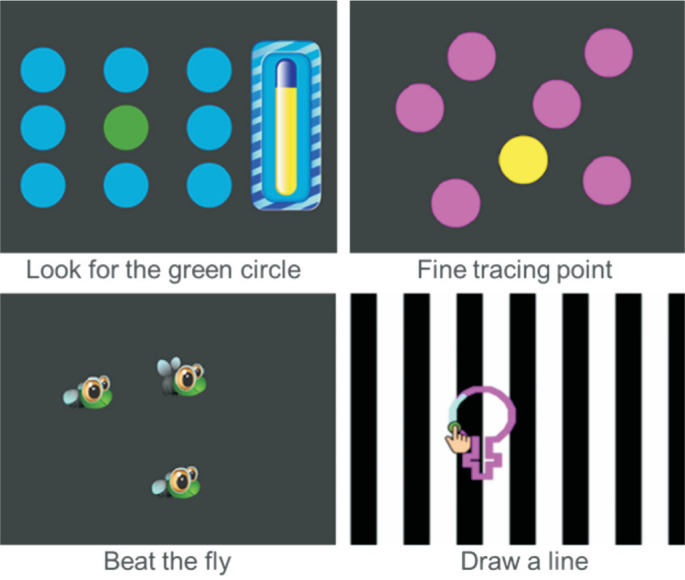
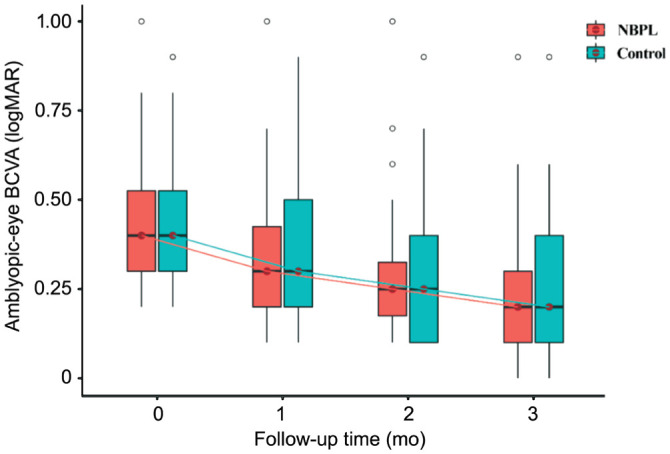
At 3mo, mean amblyopic-eye BCVA improved from baseline by 2.07 lines in the NBPL group and by 1.93 lines in the control group (Figure 2), respectively. There is no significant difference in the change of amblyopic eye BCVA between the two groups with P=0.481 (Figure 3).
Figure 2. BCVA of the amblyopic eye at baseline, 1, 2, and 3mo visit.
NBPL: Network-based perception learning; BCVA: Best-corrected visual acuity.
Figure 3. The change in amblyopic eye's BCVA from baseline to 3mo' post randomization.
BCVA: Best-corrected visual acuity.
At 3mo, amblyopic-eye BCVA improved by 2 lines or more from baseline for 21 (75%) and 20 (71.43%) participants in the NBPL group and the control group, respectively (P=0.725), and amblyopia resolved (BCVA of 20/25 or better and within 1 logMAR line of the fellow eye) for 13 (46.4%) participants in both groups. Most of the patients gained lines of BCVA improvement except for one 11-year-old girl with the lowest BCVA (0.9 logMAR) in the control group.
At 1, and 2mo, the mean change from baseline in the NBPL group was 0.75 and 1.36 lines; and in the control group was 0.43 and 1.21 lines, respectively.
Stereoacuity
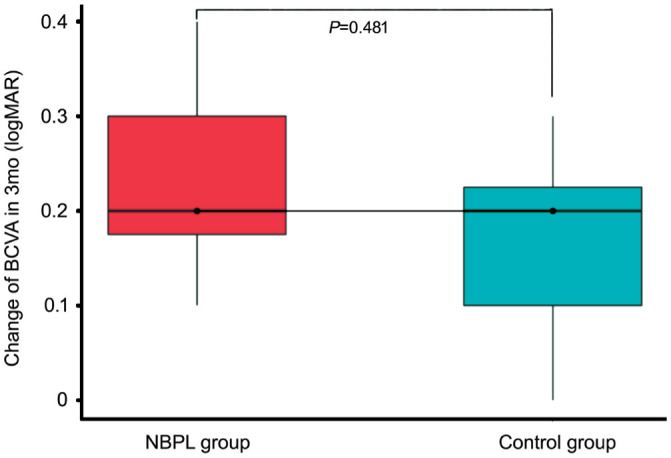
The distribution of stereoacuity at baseline, 1, 2, and 3mo post-randomization was shown in Figure 4 and Table 2.
Figure 4. Percentages of different levels of stereopsis at baseline, 1, 2, and 3mo visit.
NBPL: Network-based perception learning.
Table 2. BCVA and stereoacuity at 3mo visit.
| Characteristic | NBPL group (n=28) | Control group (n=28) | P |
| Distance amblyopic-eye BCVA (logMAR) | >0.05 | ||
| 1 | 1 | 0 | |
| 0.9 | 0 | 1 | |
| 0.8 | 1 | 0 | |
| 0.7 | 0 | 0 | |
| 0.6 | 0 | 1 | |
| 0.5 | 2 | 2 | |
| 0.4 | 3 | 4 | |
| 0.3 | 0 | 2 | |
| 0.2 | 9 | 5 | |
| 0.1 | 10 | 9 | |
| 0 | 3 | 4 | |
| Mean±SD (logMAR) | 0.207±0.18 | 0.236±0.21 | |
| Stereoacuity (second of arc) | 0.015 | ||
| ≥800 | 3 | 10 | |
| 401-800 | 4 | 4 | |
| 201-400 | 3 | 3 | |
| 61-200 | 9 | 8 | |
| ≤60 | 9 | 3 | |
NBPL: Network-based perception learning; BCVA: Best-corrected visual acuity; SD: Standard deviation.
In the NBPL group, a total of 16 patients (57.14%) had unmeasurable stereoacuity (≥800″) before the treatment, while this only occurred in 3 patients (10.71%) after 3mo training. In the control group, 15 patients (53.6%) had unmeasurable stereoacuity before treatment, while this occurred in 10 patients (35.71%) after training. The number of patients with improvement of stereoacuity was 25 and 13 in the NBPL group and control group (P=0.041).
At 3mo, the median stereoacuity was 150″ (60″, 400″) and 450″ (120″, 800″) in the NBPL group and the control group, respectively. The median change in stereoacuity from baseline to 3mo was 650″ in the NBPL group and 350″ in the control group. The ratio of central fovea stereoacuity (≤60″) presented by bright orange bar seems better in the NBPL group (P=0.051) at the 3mo point.
The distribution of stereopsis at baseline and the end of treatment in the two groups is shown in Figure 5, and a significant difference exists at 3mo (P=0.015). Besides, considering that the degree of stereopsis of patients with stereoacuity ≥800″ between the two groups might be different, and the two groups' basic stereoacuity might not be well compared, we screened out patients with stereoacuity ≥800″. At the same time, patients with stereoacuity ≤60″ had limited room for improvement, and we further screened them out. Then we compared the number of patients with stereoacuity improvement in the two groups. There were 11 people in each group who were within the measuring range and had room for improvement. An increase in stereoacuity by one level was considered an effective improvement in stereoacuity. The number of participants with improvement of stereoacuity in NBPL and control group was 10 and 4 respectively. The results showed that the NBPL group also achieved better stereoscopic improvement, with P<0.05.
Figure 5. Percentages of different levels of stereoacuity in two groups at baseline and 3mo visit.
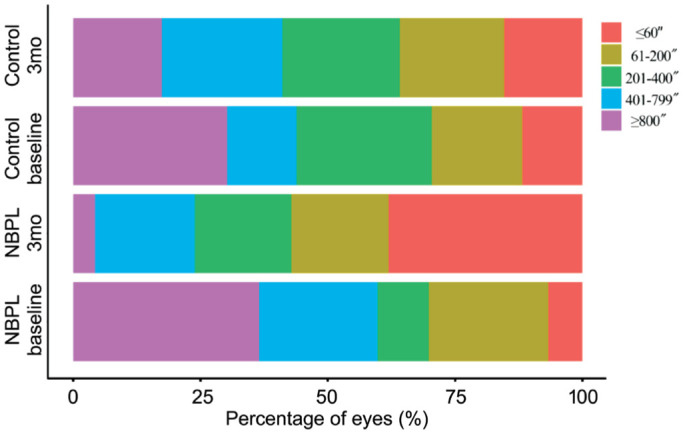
NBPL: Network-based perception learning.
DISCUSSION
Amblyopia is a condition in which one eye is more dominant than the other. It is commonly treated by patching the dominant eye to encourage activity in the lazy eye. However, the traditional treatment is relatively monotonous, and children are not easy to cooperate with.
Perceptual learning is a process by which the ability of sensory systems is improved through experience. Visual perceptual learning, an essential branch of perception learning, has been used to treat visual impairment, and it has proven useful in different situations[16],[21]–[22]. The training system we used in this study is a multimedia bio-stimulation perceptual learning software. With the software, all patients' treatment information will be preserved, facilitating the doctor's management of the patient's treatment. The training system is based on visual biometric information stimulation and has various perceptual learning training games, making the training process attractive. It utilizes cloud medical technology; the data could be synchronized automatically by the training system and specific therapy plan will be generated for each patient by the built-in intelligent expert system. Ophthalmologists can also adjust the training parameters remotely. Overall, our research has found that it has certain advantages over traditional training methods, such as diversified training modes and shorter treatment time, which improve children's treatment compliance.
Many researchers discovered that using multimedia games in amblyopia therapy could effectively improve VA, although the treatment time and specific methods of different experiments differ[23]–[24]. The binocularity-stimulating therapy is even beneficial in children with residual amblyopia[25]. There are also some different options regarding the therapy. Holmes et al[26] found there was no extra benefit to VA from 4 or 8wk of treatment with the dichoptic binocular Dig Rush iPad game in children aged 7 to 12y. From our study, after three months of training, we found that there was no significant difference in the improvement of BCVA comparing with traditional training. The result is consistent with Holmes et als' [26].
On the contrary, Manh et al[27] evaluated binocular iPad game therapy's effectiveness on amblyopic teenagers aged 13 to 17y with amblyopia compared to part-time patching and found that the outcome could be worse with the binocular iPad game therapy. Manh et al's[27] result is different from other experiments. We believe that the major variation is patching. Patching has essential value in the early stage of the treatment, especially in severe amblyopia[28]. A single binocular game without the patching of the relative healthy eye may have a weaker effect on promoting the use of amblyopia eye.
In the study with 2 children age 9 to 12 years old, the amblyopia children had moderate improvement in the visual acuities after about 15h' perceptual learning, and the improvement reached a plateau after about 50h' training[29]. Similarly, our study found the NBPL group had a better result at the 1-mo point (0.75 lines in NBPL group vs 0.43 lines in control group), which confirmed that the perceptual learning could speed the recovery time. But we did not notice any obvious plateau period in our study as our total training time was around 50h.
Our study found that in patients with measurable stereopsis improvement degree, the NBPL group achieved better stereoscopic improvement. The difference in stereoacuity improvement between the two training methods could be due to the higher compliance, more personalized therapeutic plan for binocular function in the NBPL group. Besides, an essential characteristic of amblyopia is crowding, limiting object recognition in individuals with amblyopia[30]. Perceptual learning can reduce crowding in amblyopia and the normal periphery[31], which may also contribute to the more remarkable improvement of stereoacuity in the NBPL group. Our result is in accordance with prior studies that dichoptic game played by amblyopic adults and children resulted in significant improvements in stereoacuity[11],[32]. In the present study, 4 children's stereoacuity did not improve significantly in those amblyopic children whose VA improved while taking binocular vision training. It may be related to their relatively older age (9 and 11y) and higher amblyopia severity. Although some studies have found that adult amblyopia patients are also malleable[33], it may require longer perceptual training time.
Overall, this research has shown that the NBPL program has a significant vision and stereoacuity improvement, especially in stereoacuity. Besides, compared with traditional training, NBPL has certain advantages over traditional training methods, such as diversified training modes, which significantly improve children's treatment compliance and makes the training process attractive. Recent years, the study of virtual reality has become more and more mature. We will combine virtual reality glasses with perception learning software later, and it is believed that the combination will have more significant effects on the treatment of amblyopia.
However, this study has some defects. Its sample size was small, and a larger sample size research needs to be further organized. Other visual functions, such as contrast sensitivity, were not observed in this study. For the children with insufficient vision or stereoacuity improvement in this study, whether the therapeutic efficacy could be further enhanced by extending training time, intensity, or increasing training frequency deserves further research. The two training treatments' recurrence rates were not reported, and we will continue to follow up with these patients.
In conclusion, this study showed that the multimedia bio-stimulation perceptual learning visual training system was better than traditional training in the treatment of amblyopia, mainly in terms of the improvement of stereoacuity. Multimedia bio-stimulation perceptual learning visual training is practical for children of amblyopia, improving patient compliance, and reducing treatment time.
Acknowledgments
Authors' contributions: Design of the study (Xu W); Conduct of the study, data collection, analysis and interpretation (Zheng CY, Wu SQ, Han DX); Manuscript preparation and review (Zheng CY, Xu W). All authors read and approved the final manuscript.
Foundations: Supported by Shanghai Health Situation Project (No.201540252); Shanghai Tongji Hospital Clinical Research Incubation Project [No.ITJ(QN)1812]; Shanghai Science and Technology Committee (STCSM) Science and Technology Innovation Program (No.20S31906000).
Conflicts of Interest: Zheng CY, None; Xu W, None; Wu SQ, None; Han DX, None.
REFERENCES
- 1.Fu ZJ, Hong H, Su ZC, Lou B, Pan CW, Liu H. Global prevalence of amblyopia and disease burden projections through 2040: a systematic review and meta-analysis. Br J Ophthalmol. 2020;104(8):1164–1170. doi: 10.1136/bjophthalmol-2019-314759. [DOI] [PubMed] [Google Scholar]
- 2.Kumaran SE, Rakshit A, Hussaindeen JR, Khadka J, Pesudovs K. Does non-strabismic amblyopia affect the quality of life of adults? Findings from a qualitative study. Ophthalmic Physiol Opt. 2021;41(5):996–1006. doi: 10.1111/opo.12864. [DOI] [PubMed] [Google Scholar]
- 3.Hatt SR, Leske DA, Castañeda YS, Wernimont SM, Liebermann L, Cheng-Patel CS, Birch EE, Holmes JM. Understanding the impact of residual amblyopia on functional vision and eye-related quality of life using the PedEyeQ. Am J Ophthalmol. 2020;218:173–181. doi: 10.1016/j.ajo.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webber AL. The functional impact of amblyopia. Clin Exp Optom. 2018;101(4):443–450. doi: 10.1111/cxo.12663. [DOI] [PubMed] [Google Scholar]
- 5.McConaghy JR, McGuirk R. Amblyopia: detection and treatment. Am Fam Physician. 2019;100(12):745–750. [PubMed] [Google Scholar]
- 6.Birch EE. Amblyopia and binocular vision. Prog Retin Eye Res. 2013;33:67–84. doi: 10.1016/j.preteyeres.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hess RF, Thompson B, Baker DH. Binocular vision in amblyopia: structure, suppression and plasticity. Ophthalmic Physiol Opt. 2014;34(2):146–162. doi: 10.1111/opo.12123. [DOI] [PubMed] [Google Scholar]
- 8.Kiorpes L, Daw N. Cortical correlates of amblyopia. Vis Neurosci. 2018;35:E016. doi: 10.1017/S0952523817000232. [DOI] [PubMed] [Google Scholar]
- 9.Kraus CL, Culican SM. New advances in amblyopia therapy I: binocular therapies and pharmacologic augmentation. Br J Ophthalmol. 2018;102(11):1492–1496. doi: 10.1136/bjophthalmol-2018-312172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernández-Rodríguez CJ, Piñero DP, Molina-Martín A, Morales-Quezada L, de Fez D, Leal-Vega L, Arenillas JF, Coco-Martín MB. Stimuli characteristics and psychophysical requirements for visual training in amblyopia: a narrative review. J Clin Med. 2020;9(12):E3985. doi: 10.3390/jcm9123985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu XY, Zhang YW, Gao F, Chen F, Zhang JY. Dichoptic perceptual training in children with amblyopia with or without patching history. Invest Ophthalmol Vis Sci. 2021;62(6):4. doi: 10.1167/iovs.62.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papageorgiou E, Asproudis I, Maconachie G, Tsironi EE, Gottlob I. The treatment of amblyopia: current practice and emerging trends. Graefes Arch Clin Exp Ophthalmol. 2019;257(6):1061–1078. doi: 10.1007/s00417-019-04254-w. [DOI] [PubMed] [Google Scholar]
- 13.Levi DM. Rethinking amblyopia 2020. Vision Res. 2020;176:118–129. doi: 10.1016/j.visres.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.To L, Thompson B, Blum JR, Maehara G, Hess RF, Cooperstock JR. A game platform for treatment of amblyopia. IEEE Trans Neural Syst Rehabil Eng. 2011;19(3):280–289. doi: 10.1109/TNSRE.2011.2115255. [DOI] [PubMed] [Google Scholar]
- 15.Tan QL, Wang ZY, Sasaki Y, Watanabe T. Category-induced transfer of visual perceptual learning. Curr Biol. 2019;29(8):1374–1378.e3. doi: 10.1016/j.cub.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dosher B, Lu ZL. Visual perceptual learning and models. Annu Rev Vis Sci. 2017;3:343–363. doi: 10.1146/annurev-vision-102016-061249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Capotosto P, Committeri G, Baldassarre A. Causal topography of visual cortex in perceptual learning. Neuroimage. 2020;204:116257. doi: 10.1016/j.neuroimage.2019.116257. [DOI] [PubMed] [Google Scholar]
- 18.Maniglia M, Soler V, Trotter Y. Combining fixation and lateral masking training enhances perceptual learning effects in patients with macular degeneration. J Vis. 2020;20(10):19. doi: 10.1167/jov.20.10.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sterkin A, Levy Y, Pokroy R, Lev M, Levian L, Doron R, Yehezkel O, Fried M, Frenkel-Nir Y, Gordon B, Polat U. Vision improvement in pilots with presbyopia following perceptual learning. Vision Res. 2018;152:61–73. doi: 10.1016/j.visres.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Melnick MD, Tadin D, Huxlin KR. Relearning to see in cortical blindness. Neuroscientist. 2016;22(2):199–212. doi: 10.1177/1073858415621035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haris EM, McGraw PV, Webb BS, Chung STL, Astle AT. The effect of perceptual learning on face recognition in individuals with central vision loss. Invest Ophthalmol Vis Sci. 2020;61(8):2. doi: 10.1167/iovs.61.8.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gambacorta C, Nahum M, Vedamurthy I, Bayliss J, Jordan J, Bavelier D, Levi DM. An action video game for the treatment of amblyopia in children: a feasibility study. Vision Res. 2018;148:1–14. doi: 10.1016/j.visres.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo CX, Babu RJ, Black JM, Bobier WR, Lam CS, Dai S, Gao TY, Hess RF, Jenkins M, Jiang YN, Kowal L, Parag V, South J, Staffieri SE, Walker N, Wadham A, Thompson B, BRAVO study team Binocular treatment of amblyopia using videogames (BRAVO): study protocol for a randomised controlled trial. Trials. 2016;17(1):504. doi: 10.1186/s13063-016-1635-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Birch EE, Li SL, Jost RM, Morale SE, de la Cruz A, Stager D, Jr, Dao L, Stager DR., Sr Binocular iPad treatment for amblyopia in preschool children. J AAPOS. 2015;19(1):6–11. doi: 10.1016/j.jaapos.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee HJ, Kim SJ. Effectiveness of binocularity-stimulating treatment in children with residual amblyopia following occlusion. BMC Ophthalmol. 2018;18(1):253. doi: 10.1186/s12886-018-0922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Group PEDI. Holmes JM, Manny RE, Lazar EL, Birch EE, Kelly KR, Summers AI, Martinson SR, Raghuram A, Colburn JD, Law C, Marsh JD, Bitner DP, Kraker RT, Wallace DK. A randomized trial of binocular dig rush game treatment for amblyopia in children aged 7 to 12y. Ophthalmology. 2019;126(3):456–466. doi: 10.1016/j.ophtha.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manh VM, Holmes JM, Lazar EL, Kraker RT, Wallace DK, Kulp MT, Galvin JA, Shah BK, Davis PL, Group PEDI A randomized trial of a binocular iPad game versus part-time patching in children aged 13 to 16y with amblyopia. Am J Ophthalmol. 2018;186:104–115. doi: 10.1016/j.ajo.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Group PEDI The course of moderate amblyopia treated with atropine in children: experience of the amblyopia treatment study. Am J Ophthalmol. 2003;136(4):630–639. doi: 10.1016/s0002-9394(03)00458-6. [DOI] [PubMed] [Google Scholar]
- 29.Li RW, Provost A, Levi DM. Extended perceptual learning results in substantial recovery of positional acuity and visual acuity in juvenile amblyopia. Invest Ophthalmol Vis Sci. 2007;48(11):5046–5051. doi: 10.1167/iovs.07-0324. [DOI] [PubMed] [Google Scholar]
- 30.Levi DM, Knill DC, Bavelier D. Stereopsis and amblyopia: a mini-review. Vision Res. 2015;114:17–30. doi: 10.1016/j.visres.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hussain Z, Webb BS, Astle AT, McGraw PV. Perceptual learning reduces crowding in amblyopia and in the normal periphery. J Neurosci. 2012;32(2):474–480. doi: 10.1523/JNEUROSCI.3845-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xi J, Jia WL, Feng LX, Lu ZL, Huang CB. Perceptual learning improves stereoacuity in amblyopia. Invest Ophthalmol Vis Sci. 2014;55(4):2384–2391. doi: 10.1167/iovs.13-12627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Žiak P, Holm A, Halička J, Mojžiš P, Piñero DP. Amblyopia treatment of adults with dichoptic training using the virtual reality oculus rift head mounted display: preliminary results. BMC Ophthalmol. 2017;17(1):105. doi: 10.1186/s12886-017-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]