Abstract
AIM
To compare the visual results of non-topography-guided and topography-guided photorefractive keratectomy (PRK) applying sequential and simultaneous corneal cross-linking (CXL) treatment for keratoconus.
METHODS
Interventional and comparative prospective study. Sixty-nine eyes (36 patients) suffering from keratoconus (stages 1 Amsler-Krumeich classification) were divided into four groups: sequential topography-guided photorefractive keratectomy with CXL, simultaneous topography-guided photorefractive keratectomy with CXL, simultaneous non-topography guided photorefractive keratectomy with CXL, and sequential non-topography guided photorefractive keratectomy with CXL. The main outcome measures were pre- and postoperative uncorrected distance visual acuity (UDVA), best corrected distance visual acuity (CDVA), manifest refraction, contrast sensitivity, and keratometry.
RESULTS
All analyzed visual, contrast sensitivity, and refractive parameters showed a significant improvement in the four groups (all P<0.05). A noticeable improvement was seen in keratometry in all the groups, and a remarkable difference was observed between topography-guided groups in comparison to non-topography-guided groups (P<0.05). Interestingly, the improvement in all parameters showed a degree of stability to the end of the follow-up.
CONCLUSION
The treatment priorities in all four groups are safety, efficacy, and predictability in the correction of the sphero-cylindrical errors in mild and moderate keratoconus. No significant differences among groups in the recorded objective outcomes were found.
Keywords: photorefractive keratectomy, corneal collagen cross-linking, keratoconus
INTRODUCTION
Effective therapy for corneal ectatic diseases, such as iatrogenic corneal ectasia, keratoconus, and pellucid marginal degeneration, involve confronting two specific parameters: the corneal optical deficiency and the biomechanical inconsistency of the irregular cornea[1]–[2]. Contact lenses have corrected patients with irregular astigmatism for years (scleral lenses and rigid gas permeable contact lenses) in mild cases of keratoconus, and penetrating keratoplasty has been the surgical option in severe cases. Other effective surgical methods are now being used, such as intracorneal ring segments and deep anterior lamellar keratoplasty while other approaches were proposed and attempted in the past, such as conductive keratoplasty and epikeratophakia[3]–[5].
Corneal collagen cross-linking (CXL) opened a new horizon in the effective treatment of progressive corneal ectasia[6]. The blend of ultra-violet A and riboflavin as a light sensitivity factor produced inter-fibrillary connection between cornea stromal collagen fibers, and as a result, decreased corneal deformability, corneal resistance, and stabilized keratoconus[7]. With CXL, the issue of biomechanical instability has been effectively confronted, as indicated by the confirmation that CXL has been successful in stopping the progression of ectatic disorders[8]–[10].
However, the visual outcomes and the topography of patients treated only by CXL demonstrate no change or insignificant change due to remaining irregular astigmatism. Excimer laser surgery in the form of non-topography-guided and topography-guided photorefractive keratectomy, besides decreasing irregular astigmatism, changes the shape of the cornea improving visual outcomes[11]–[12]. The combination of CXL with excimer laser photorefractive keratectomy has recently gained interest in treating mild to moderate keratoconus[12]. However, there is still no evidence confirming the potential benefits of topography-guided photorefractive keratectomy method over standard, non-topograph-guided photorefractive keratectomy.
This study aims to compare and appraise the visual outcomes of topography and non-topography-guided photorefractive keratectomy with sequential and simultaneous CXL in keratoconus patients.
SUBJECTS AND METHODS
Ethical Approval
The study received approval from the local ethics committee (IR. SBMU. RETECH.RECH.1400.1216). As a standard protocol, all surgeries were performed by one surgeon (Doroodgar F) after obtaining appropriate written consent from a trained, certified good clinical practice (GCP) examiner.
Subjects and Groups
This prospective study included four groups of keratoconus patients: Sequential topography-guided photorefractive keratectomy with CXL (sequential TG-PRK, 19 eyes/10 patients), simultaneous topography-guided photorefractive keratectomy with CXL (simultaneous TG-PRK, 15 eyes/8 patients), simultaneous non-topography guided photorefractive keratectomy with CXL (simultaneous non-TG-PRK, 17 eyes/9 patients), and sequential non-topography guided photorefractive keratectomy with CXL (sequential non-TG-PRK, 18 eyes/9 patients). The patients were treated between January 2014 and October 2015.
Inclusion criteria for the study focused on patients over 34y (range from 34 to 41y) with stable corneal topography and refraction for at least six months and an estimated residual bed thickness of >410 µm.
Conditions for exclusion from the study included the presence of macular or retinal disease, dry eye, history of recurrent corneal erosions, anterior segment abnormalities, unstable refractive error, post-surgically residual stromal bed thickness of under 350 µm, autoimmune disease, collagen vascular disease, immunosuppressive therapy or current use of systemic corticosteroids, diabetes mellitus, pregnancy, and lactation.
Examinations
Preoperative examinations were uncorrected and best-corrected distance visual acuity (UCVA and BCVA) applying a standard Snellen eye chart, cycloplegic refraction with cyclopentolate 1.0%, contrast sensitivity exam under mesopic (3 cd/m2) and photopic (85 cd/m2) conditions using the CVS1000 contrast sensitivity exam (VectorVision, Greenville, SC, USA) manifest refraction, slit-lamp biomicroscopy of the anterior and posterior segment evaluation, Scheimpflug imaging with the Pentacam HR device (Oculus Surgical, Inc., USA), and intraocular pressure measurements for each group separately. Contact lens users were instructed to stop wearing contact lenses for about fourteen days before being screened in the case of soft contact lens users and a month before being screened in the case of rigid gas permeable or scleral contact lenses. The patients were examined for 1, 3, and 6y after the surgery. All postoperative follow-ups included a measurement of UCVA and BCVA, contrast sensitivity, and refraction.
Surgical Technique
Simultaneous topography-guided photorefractive keratectomy and corneal collagen cross-linking
The restrictive programming in the Wavelight Customized technology uses topographic information from Topolyzer. The software uses information from eight geographies from Topolyzer and averages the information. Therefore, it enables the specialist to modify the desired corneal asphericity (selected as zero in all cases). The technology additionally provides the choice of tilt amendment. “No Tilt” alternative was selected in all subjects. Zernike analysis was performed in all patients to coordinate defocus (C4) and spherical aberration (C12), maintaining the refractive correction at zero. Once the sphere, cylinder, and axis modification were done, the treatment zone was kept at 5.5 mm in all subjects. Using the lid speculum and topical anesthesia by oxybuprocaine 0.4% (Dorsacaine, Novesin) and tetracaine hydrochloride 1%, the epithelium was debrided utilizing ethanol 20%, and Weck-Cel wipe.
Topo-guided photorefractive keratectomy was performed using an excimer laser (Allegretto Wave Topolyzer, Alcon, Inc., USA) with a 6 mm optical area and a transition area of 2 mm in all eyes. At that point, the partial topography-guided photorefractive keratectomy laser treatment was finished. The arrangement was to treat 70% of the cylindrical and spherical part to not surpass 50 µm of stromal expulsion. The estimation of 50 µm as the most extreme removal depth recommended by Kanellopoulos[11] in Athens protocol was chosen.
Topo-guided photorefractive keratectomy methods were followed by accelerated CXL with the corneal cross-linking system (KXL System; Avedro, Inc., USA). As in previous studies[13]–[14], eyes with myopic spherical equivalent >4.0 D were applied with mitomycin C 0.4 mg/mL (0.02%) for 25s and washed with 45 mL of basal salt solution (BSS; Alcon Laboratories, Fort Worth, TX, USA). Quickened CXL was performed with washing the vicinity of the stroma with 0.20% isotonic riboflavin (VibeX; Avedro, Inc., Waltham, MA, USA) for 90s. After rinsing the corneal stroma with BSS, ultra-violet A sequential light treatment was initiated at 30 mW/cm2 for 90s with the full power of 2.7 J/cm2 on the cornea. During ultra-violet A treatment, the stroma was rinsed with the BSS as required. The same method was used in patients for both eyes. A soft bandage contact lens was applied at the end of the surgical procedure. This was removed after the epithelial deformity healed (3-6d post-surgery).
Sequential photorefractive keratectomy and corneal collagen cross-linking
Accelerated CXL was performed as described above with the same postoperative treatment. Topography-guided photorefractive keratectomy was completed six months later in a similar way to the simultaneous system. The same method was performed in patients with keratoconus in both eyes.
Simultaneous non-topography guided photorefractive keratectomy and corneal collagen cross-linking
After topical anesthesia with oxybuprocaine HCl, benoxinate HCl 0.4% eye drop (Benox®, Eipico) was used. The epithelium was debrided utilizing a mechanical beaver with a surgical blade of 8.00 mm in diameter. Then, photorefractive keratectomy was performed with the Schwind Amaris 750S (Schwind eye-tech-solutions, Kleinostheim, Germany). After that, mitomycin 0.2 mg/mL was applied for 10s, and photorefractive keratectomy was followed immediately by cross-linking. Hypotonic riboflavin was applied and ultrasonic pachymetry (Sonogage, Inc., Cleveland, OH, USA) was performed. If the cornea was less than 400 µm, extra hypotonic riboflavin was regulated for 30min to the point when the stroma had swollen to no less than 400 µm. Then ultra-violet A (UVX1000; IROC, Zurich, Switzerland) with 365 nm wavelengths were applied to the direct vicinity of the cornea for 15min at the radiation of 3.0 mW/cm2. During the ultra-violet A treatment, hypotonic riboflavin (0.1% one drops every 2min) was applied. The same method was used in patients with keratoconus in both eyes.
Sequential non-topography-guided photorefractive keratectomy and corneal collagen cross-linking
Accelerated CXL was performed as described above with the same postoperative regimen. Non-topography-guided photorefractive keratectomy was completed six months later in a similar way to the simultaneous method. The same procedure was performed in patients with keratoconus in both eyes. Postoperatively, levofloxacin 0.5% eye drop (Oftaquix, Santen, Tampere, Finland) was applied four times a day together with betamethasone eye drop (Betasonit 0.1%, betamethasone disodium phosphate; Sina Darou, Tehran, Iran) six times a day for two weeks, and artifcial tears (Artelac™, Hypromellose; Bausch and Lomb, Montpellier, France) were administered every 4h for 4wk. Topical corticosteroid (fluorometholone) and anti-infection (moxifloxacin) drops (6 hourly and steroid decreased more than 5wk) were controlled and preceded from 1 to 6wk after surgery, separately. Artificial tears were applied every four hours for three months. A therapeutic contact lens (AIR OPTIX, USA; therapeutic contact lens was used in all cases) was placed at the end of the procedure and was then removed after epithelial recovery. Patients were observed for three months after the procedure and were given yearly examinations for six years. Patients were analyzed for 1, 3, and 6y and data collected for each patient included uncorrected and corrected distance visual acuity using a standard Snellen eye diagram for 1, 3, and 6y.
In each protocol, efficacy, and safety indexes were measured as follows: efficacy index=(mean post-surgically UCVA)/(mean pre-surgically BCVA) and safety index=(mean post-surgically BCVA)/(mean pre-surgically BCVA) for all the groups (decimals for visual acuity). The initial outcomes of the study were an improvement in UCVA and BCVA. In addition, the secondary outcomes were the safety, efficacy, and predictability indices of the different techniques.
Statistical Analysis
The statistical package for the social sciences software (SPSS Statistics for Windows, V.23.0, 2013; IBM, USA) was used to statistically analyze the results. The nonparametric Friedman exam was used to determine the significant differences between the objective results before and after surgery, such as contrast sensitivity and the logMAR visual acuity. The nonparametric one-way analysis of variance was also applied to define any statistically significant differences between the means of the predictability, safety, stability, and efficacy of all the groups studied. We considered 5% to be a statistically significant threshold in our analysis.
RESULTS
A total of 69 eyes (36 patients) in four groups ranging from 34 to 41 years old (36±5.4y) were included in the study, and nearly half of the eyes (n=30, 43.5%) were from male patients. All subjects had keratoconus in both eyes. The outcomes were obtained by contrasting clinical parameters in the four groups at a post-operative checkup and later at the last follow-up (1, 3, and 6y; Tables 1 and 2).
Table 1. Preoperative spherical equivalent, astigmatism, visual acuities and keratometry.
| Parameters | Simultaneous TG-PRK (n=15) | Sequential TG-PRK (n=19) | Simultaneous non-TG-PRK (n=17) | Sequential non-TG-PRK (n=18) |
| Steep K, D | 47.22±0.91 | 47.33±0.92 | 47.44±0.95 | 47.62±0.89 |
| Flat K, D | 44.67±1.29 | 44.87±0.99 | 45.14±1.41 | 45.02±1.06 |
| Spherical equivalent, D | -2.83±1.23 | -2.93±1.49 | -3.00±1.36 | -3.17±1.71 |
| Astigmatism, D | -2.40±0.67 | -2.41±0.61 | -2.38±0.68 | -2.46±0.70 |
| UCVA (logMAR) | 0.97±0.15 | 0.94±0.15 | 0.94±0.14 | 0.99±0.15 |
| BCVA (logMAR) | 0.02±0.04 | 0.02±0.04 | 0.02±0.04 | 0.04±0.05 |
K: Keratometry; UCVA: Uncorrected visual acuity; BCVA: Best corrected visual acuity; TG-PRK: Topography-guided photorefractive keratectomy.
mean±SD
Table 2. Postoperative UCVA, BCVA, and keratometry.
| Parameters | Simultaneous TG-PRK (n=15) | Sequential TG-PRK (n=19) | Simultaneous non-TG-PRK (n=17) | Sequential non-TG-PRK (n=18) | P |
| UCVA, logMAR | |||||
| 1y | 0.01±0.07 | 0.01±0.07 | 0.02±0.08 | 0.03±0.15 | 0.81 |
| 3y | 0.01±0.07 | 0.01±0.07 | 0.03±0.08 | 0.02±0.08 | 0.66 |
| 6y | 0.02±0.06 | 0.01±0.07 | 0.03±0.08 | 0.02±0.08 | 0.74 |
| BCVA, logMAR | |||||
| 1y | 0.01±0.18 | 0.01±0.05 | 0.02±0.17 | 0.02±0.05 | 0.57 |
| 3y | 0.01±0.05 | 0.01±0.05 | 0.02±0.05 | 0.02±0.06 | 0.26 |
| 6y | 0.02±0.05 | 0.01±0.05 | 0.02±0.05 | 0.02±0.06 | 0.80 |
| Steep K, D | |||||
| 1y | 44.45±0.83 | 44.76±0.92 | 45.18±0.87 | 45.18±0.83 | 0.01 |
| 3y | 44.52±0.93 | 45.02±0.71 | 45.35±0.77 | 45.33±0.77 | 0.01 |
| 6y | 44.50±0.94 | 45.16±0.73 | 45.47±0.79 | 45.48±0.73 | 0.01 |
| Flat K, D | |||||
| 1y | 42.01±0.63 | 42.73±1.25 | 43.28±0.93 | 43.21±0.85 | 0.01 |
| 3y | 42.08±0.68 | 42.84±1.22 | 43.52±0.82 | 43.36±0.82 | 0.01 |
| 6y | 42.02±0.82 | 42.84±1.18 | 43.58±0.89 | 43.36±0.82 | 0.01 |
K: Keratometry; UCVA: Uncorrected visual acuity; BCVA: Best corrected visual acuity; TG-PRK: Topography-guided photorefractive keratectomy.
mean±SD
Visual and Refractive Outcomes
A significant improvement was observed in visual acuity and mean spherical equivalent refraction in all patients after surgery at the 3-year follow-up visit (P<0.05). Accordingly, no noticeable difference was observed in the four groups regarding the post-surgery visual and refractive outcomes. Patients in all groups had a significant improvement in UCVA and BCVA (P<0.05; Table 2, Figure 1).
Figure 1. Six years post-operative refraction.
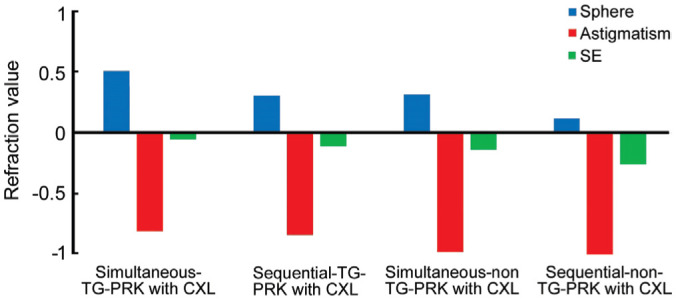
SE: Spherical equivalent; TG-PRK: Topography-guided photorefractive keratectomy.
Safety
BCVA (logMAR) in the sequential TG-PRK and simultaneous TG-PRK were 0.01±0.05, 0.02±0.05. In sequential non-TG-PRK and simultaneous non-TG-PRK were 0.02±0.06 and 0.02±0.05, six years after the operation, respectively. There was a remarkable difference between preoperative BCVA and all follow-ups (P<0.05, Wilcoxon signed-rank test). We calculated that the safety index of sequential TG-PRK and simultaneous TG-PRK were 1.08 and 1.05. The sequential non-TG-PRK and simultaneous non-TG-PRK were 1.00 and 1.01 in six years, respectively.
Treatment Effectiveness
UCVA at 6y postoperative for all groups was ≥20/20 (0.0 logMAR) in 62.31% of eyes and ≥20/40 (0.3 logMAR) in 100% of eyes. At 6y, post-surgery UCVA was the same or more than pre-operative BCVA in the TG-PRK group, which showed that simultaneous TG-PRK and sequential TG-PRK were 73.33% (11/15) and 73.68% (14/19) of eyes. In the simultaneous non-TG-PRK and sequential non-TG-PRK groups were 64.7% (11/17), 55.56% (10/18) eyes.
Predictability
The following outcomes are relied on to give a more precise appraisal of refraction than the post-surgery mean refractive spherical equivalent results. During six years, the post-surgery refraction of eyes in the TG-PRK groups were 84.21% within ±0.50 D, and 100% within ±1.0 D, and in the non-TG-PRK groups, the refraction of eyes was 86% within ±0.50 D while 100% within ±1.0 D of the desired correction (Figure 1). The spherical equivalent, cylinder, and sphere differences were statistically significant between pre-operative and six years after surgery.
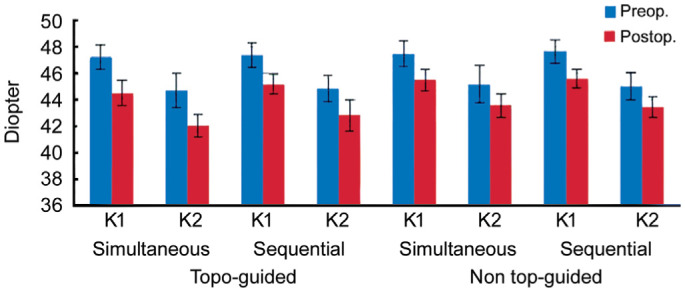
Topographic Outcomes
The average steep and flat keratometry (steep K and flat K) was significantly decreased at the 3-year follow-up visit in all groups (P<0.05; Figure 2). Postoperative mean keratometric astigmatism also decreased compared to pre-surgery in all groups (P<0.05). However, after six years, significant differences were observed of flat K and steep K between groups. Simultaneous TG-PRK had a better and more significantly different outcome than other groups (P<0.05).
Figure 2. Keratometry change preoperative and six years postoperative.
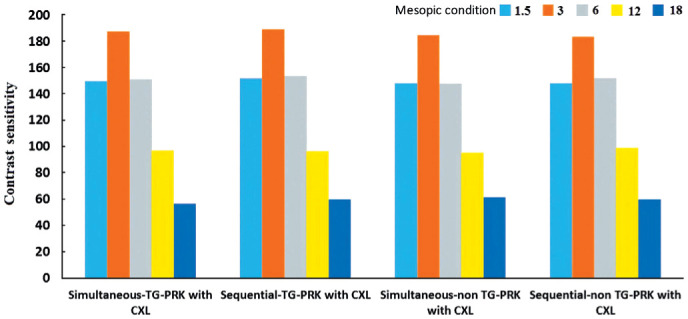
Contrast Sensitivity
Figures 3 and 4 showed the mean postoperative contrast sensitivity in logarithmic scale under binocular photopic and mesopic situation six years after surgery. There was no significant difference in the value obtained among the groups at spatial frequencies of 1, 3, 6, 12, and 18 cpd.
Figure 3. The postoperative contrast sensitivity in logarithmic scale under binocular photopic situation six years after surgery.
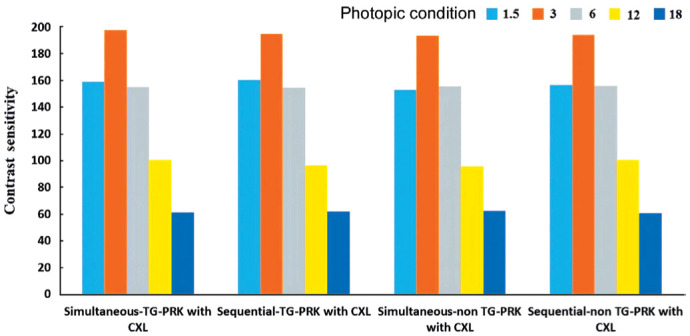
Figure 4. The postoperative contrast sensitivity in logarithmic scale under binocular mesopic situation six years after surgery.
DISCUSSION
CXL increases the level of entombed fibrillar linkages enhancing the biomechanical quality of the cornea. Many investigations have confirmed the effective stabilization of keratoconus progression after CXL[3],[5],[15]. Almost all previous studies have proven that TG-PRK and non-TG-PRK with sequential, and simultaneous CXL are effective and safe and result in good visual performance in keratoconus eyes[16]–[18]. Most studies have reported that simultaneous treatment (TG-PRK and non-TG-PRK followed immediately by CXL) produces excellent results compared to sequential treatment[19], and other studies have not indicated a difference between these two methods[20]. Efficacy and safety of simultaneous and sequential methods would enhance the refractive condition of the eye[21].
To our knowledge, this is the first study to compare four surgical methods in keratoconus patients. The comparison aims to determine the best method to treat patients with keratoconus and evaluate functional and consistent outcomes. Achieving useful vision comprises enhancing UCVA and BCVA and standardization of corneal topography, demonstrating that these patients are less subject to contact lens use. Therefore, a higher postoperative visual quality would be achieved.
Regarding visual and refractive outcomes, in an investigation comparing a sequential group to simultaneous TG-PRK and non-TG-PRK with CXL in 69 keratoconus eyes, with an average follow-up of 3y, Kanellopoulos[19] demonstrated a greater improvement in UCVA and BCVA and a more prominent decrease in mean refractive spherical equivalent in the simultaneous group compared to the sequential one. Additionally, Kymionis et al[22] demonstrated satisfactory outcomes in 31 eyes undergoing simultaneous TG-PRK and CXL for keratoconus. The improvement remained stable for an average follow-up period of two years. All assessed visual and refractive parameters showed an exceptionally significant improvement after the operation in the two groups and subgroups (all P<0.001) 6y after the surgery, signaling no remarkable changes to the end of the follow-up period, thus demonstrating stabilization in results (Table 2).
In one study performed on early cases of keratoconus utilizing non-TG-PRK with CXL, the authors reported an extraordinary improvement in the UCVA, cylinder, and spherical equivalent, and the BCVA remained stable[23].
At the last follow-up visit, the mean refractive spherical equivalent reduced but no significant difference was found among all the groups (Figure 1). The same results were also recorded by Shaheen et al[21]. In terms of astigmatism, our study achieved a considerable decrease in the manifest cylinder and it is interesting to note that no significant difference between the groups was discovered. Shaheen et al[21] demonstrated a change in manifest astigmatism from a mean preoperative value of -2.79±1.82 D to a one-year postoperative value of -1.06±0.92 D.
Although the predictability of outcomes is assumed to be much better in the sequential approach due to restricted accuracy of manifest refraction in keratoconus before CXL and owing to some expected topographical and refractive changes occurring after the CXL procedure[21], our findings demonstrated no significant differences in the results of all techniques applied. Regarding keratometry, due to changes in corneal topography that occur after surgery, our outcomes showed a significant reduction in 1, 3, and 6y after surgery in the four groups, with no significant decrease of these parameters during the follow-up. In addition, in the present study, we observed that TG-PRK groups show better and more significant results than non-TG-PRK. The corneal surface can gauge more spots when incorporating those on the corneal outskirts. In addition, the topography-guided profile enables the excimer laser spots to be focused on steepening the flatter zones and flatten the top zone when ablating the cornea. This joint strategy for simultaneous myopic and hyperopic treatment expels significantly less tissue and maintains the stroma's prolate condition. Moreover, the topography-guided profile is fixed on the corneal summit instead of the pupil center and investigates the angle κ issue[24].
The previous investigations and basic science have demonstrated that surface ablation is better at maintaining the cornea's mechanical properties and hysteresis compared to other refractive surgeries[25]–[27]. This can be justified by developing another fibro-cellular film in ablated corneal layers which increases the corneal strength and acts as a shield preventing further progression of the keratoconus[28]. These fundamental changes could decrease the probability of haze, but there is still a chance[25]. However, in our investigation, there was an insignificant corneal haze in the entire sample, which could be attributed to the use of mitomycin C in most cases during the surgery.
Contrast sensitivity, optical aberrations, and defocus are visual quality indexes that assess light scattering in natural vision[28]. Our findings demonstrated no significant differences in the results of the four techniques, but the simultaneous/sequential TG-PRK group in low spatial frequency showed better results compared to the other groups, which may be due to the topography-guided correction in the corneal aberrations.
Choosing the best method is still controversial, and studies report different outcomes regarding one or two-step combined therapies (CXL followed by TG-PRK and non-TG-PRK), but most studies suggest that the one-step method is better because, according to this approach, there are three limitations. First, the conceivable advantages of CXL and plausibility of progression of keratoconus. Second, the viability of the methodology is restricted since the corneal ablation could be more diverse in cross-connected corneas than in the normal cornea (this could prompt unexpected refractive outcomes). Third, there is a greater plausibility of post photorefractive keratectomy haze. After CXL, the anterior stroma is reconstructed after six months using new keratocytes as indicated by in vivo confocal microscopy[29]–[30].
The study did not find a statistically significant difference in parameter measurements which might be due to the CXL effect. Therewith, CXL alone also changes the corneal shape by leveling it >2.00 D in the keratometry index[31]–[32], meaning that a planned laser treatment might elevate or even over flatten the shape with extra CXL treatments required later on. This is another motivation to prescribe the spherical segment of the refractive error and plan for 80% of the astigmatism correction. Accordingly, the performance of future large scale comparative randomized studies with a longer follow-up is necessary to establish the long-term stability of this methodology in keratoconus. Such discoveries could be useful to have generalized clinical rules and procedures for the administration of keratoconus[33].
In conclusion, the treatment priorities for all the groups are safety, efficacy, and predictability in order to correct the sphero-cylindrical errors in the mild and moderate keratoconus.
Acknowledgments
Conflicts of Interest: Niazi S, None; Alio del Barrio J, None; Sanginabadi A, None; Doroodgar F, None; Alinia C, None; Baradaran-Rafii A, None; Niazi F, None; Mohammad-Rabei H, None; Sadoughi MM, None; Alio JL, None.
REFERENCES
- 1.Choksi T, Sahdev S, Pawar R. Keratoconus: available treatment options. Delhi Journal of Ophthalmology. 2021;31:13–17. [Google Scholar]
- 2.Dupps WJ., Jr Corneal refractive surgery in keratoconus. J Cataract Refract Surg. 2020;46(4):495–496. doi: 10.1097/j.jcrs.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 3.Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011;95(8):1044–1050. doi: 10.1136/bjo.2010.185868. [DOI] [PubMed] [Google Scholar]
- 4.Coskunseven E, Kymionis GD, Tsiklis NS, Atun S, Arslan E, Jankov MR, Pallikaris IG. One-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconus. Am J Ophthalmol. 2008;145(5):775–779. doi: 10.1016/j.ajo.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Mohammadpour M, Heidari Z, Hashemi H. Updates on managements for keratoconus. J Curr Ophthalmol. 2017;30(2):110–124. doi: 10.1016/j.joco.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hafezi F, Richoz O, Torres-Netto EA, Hillen M, Hafezi NL. Corneal cross-linking at the slit lamp. J Refract Surg. 2021;37(2):78–82. doi: 10.3928/1081597X-20201123-02. [DOI] [PubMed] [Google Scholar]
- 7.Nattis AS, Rosenberg ED, Donnenfeld ED. One-year visual and astigmatic outcomes of keratoconus patients following sequential crosslinking and topography-guided surface ablation: the TOPOLINK study. J Cataract Refract Surg. 2020;46(4):507–516. doi: 10.1097/j.jcrs.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 8.Pircher N, Lammer J, Holzer S, Gschließer A, Donner R, Pieh S, Schmidinger G. Correlation between central stromal demarcation line depth and changes in K values after corneal cross-linking (CXL) Graefes Arch Clin Exp Ophthalmol. 2018;256(4):759–764. doi: 10.1007/s00417-018-3922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mazzotta C, Traversi C, Baiocchi S, Bagaglia S, Caporossi O, Villano A, Caporossi A. Corneal collagen cross-linking with riboflavin and ultraviolet A light for pediatric keratoconus: ten-year results. Cornea. 2018;37(5):560–566. doi: 10.1097/ICO.0000000000001505. [DOI] [PubMed] [Google Scholar]
- 10.Knyazer B, Krakauer Y, Baumfeld Y, Lifshitz T, Kling S, Hafezi F. Accelerated corneal cross-linking with photoactivated chromophore for moderate therapy-resistant infectious keratitis. Cornea. 2018;37(4):528–531. doi: 10.1097/ICO.0000000000001498. [DOI] [PubMed] [Google Scholar]
- 11.Kanellopoulos AJ. Femtosecond Laser Surgery in Ophthalmology. New York: Thieme; 2018. Laser's Place in CXL: Excimer Laser and Refractive Surgery Combined with Corneal CrossLinking, Femto-LASIK Combined with CXL. [Google Scholar]
- 12.Shah S, Mohan S, Rajan M, John B, Badlani V. Our experience with Athens protocol - simultaneous topo-guided photorefractive keratectomy followed by corneal collagen cross linking for keratoconus. Int J Res Med Sci. 2016:2639–2644. [Google Scholar]
- 13.See B, Tan M, Chia SE, Gan WH, Low R, Nah G. Photorefractive keratectomy in young Asian aviators with low-moderate myopia. Aviat Space Environ Med. 2014;85(1):25–29. doi: 10.3357/asem.3658.2014. [DOI] [PubMed] [Google Scholar]
- 14.Somani SN, Moshirfar M, Patel BC. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2022. Photorefractive Keratectomy. [PubMed] [Google Scholar]
- 15.Rabina G, Mimouni M, Kaiserman I. Epithelial photorefractive keratectomy vs mechanical epithelial removal followed by corneal crosslinking for keratoconus: the Tel-Aviv Protocol. J Cataract Refract Surg. 2020;46(5):749–755. doi: 10.1097/j.jcrs.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 16.Althomali TA. Visual and refractive outcomes of combined excimer laser ablation with accelerated corneal collagen cross-linking in subclinical keratoconus. Saudi Journal for Health Sciences. 2018;7:7–13. [Google Scholar]
- 17.Hashmani S, Hashmani N, Haroon H, Hashmi Y. Visual and refractive outcomes of topography-guided laser-assisted in situ keratomileusis in virgin eyes. Cureus. 2018;10(1):e2131. doi: 10.7759/cureus.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Amri AM. 5-year follow-up of combined non-topography guided photorefractive keratectomy and corneal collagen cross linking for keratoconus. Int J Ophthalmol. 2018;11(1):48–52. doi: 10.18240/ijo.2018.01.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9):S812–S818. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 20.Abou Samra WA, El Emam DS, Farag RK, Abouelkheir HY. Simultaneous versus sequential accelerated corneal collagen cross-linking and wave front guided PRK for treatment of keratoconus: objective and subjective evaluation. J Ophthalmol. 2016;2016:2927546. doi: 10.1155/2016/2927546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaheen MS, Shalaby Bardan A, Piñero DP, Ezzeldin H, El-Kateb M, Helaly H, Khalifa MA. Wave front–guided photorefractive keratectomy using a high-resolution aberrometer after corneal collagen cross-linking in keratoconus. Cornea. 2016;35(7):946–953. doi: 10.1097/ICO.0000000000000888. [DOI] [PubMed] [Google Scholar]
- 22.Kymionis GD, Portaliou DM, Kounis GA, Limnopoulou AN, Kontadakis GA, Grentzelos MA. Simultaneous topography-guided photorefractive keratectomy followed by corneal collagen cross-linking for keratoconus. Am J Ophthalmol. 2011;152(5):748–755. doi: 10.1016/j.ajo.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 23.Fadlallah A, Dirani A, Chelala E, Antonios R, Cherfan G, Jarade E. Non-topography-guided PRK combined with CXL for the correction of refractive errors in patients with early stage keratoconus. J Refract Surg. 2014;30(10):688–693. doi: 10.3928/1081597X-20140903-02. [DOI] [PubMed] [Google Scholar]
- 24.Ramamurthy S, Soundarya B, Sachdev GS. Topography-guided treatment in regular and irregular corneas. Indian J Ophthalmol. 2020;68(12):2699–2704. doi: 10.4103/ijo.IJO_2119_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dupps WJ, Jr, Wilson SE. Biomechanics and wound healing in the cornea. Exp Eye Res. 2006;83(4):709–720. doi: 10.1016/j.exer.2006.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang BJ, Zhang ZY, Naidu RK, Chu RY, Dai JH, Qu XM, Yu ZQ, Zhou H. Comparison of the change in posterior corneal elevation and corneal biomechanical parameters after small incision lenticule extraction and femtosecond laser-assisted LASIK for high myopia correction. Cont Lens Anterior Eye. 2016;39(3):191–196. doi: 10.1016/j.clae.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Guo H, Hosseini-Moghaddam SM, Hodge W. Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol. 2019;19(1):167. doi: 10.1186/s12886-019-1165-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dawson DG, Edelhauser HF, Grossniklaus HE. Long-term histopathologic findings in human corneal wounds after refractive surgical procedures. Am J Ophthalmol. 2005;139(1):168–178. doi: 10.1016/j.ajo.2004.08.078. [DOI] [PubMed] [Google Scholar]
- 29.Kankariya V, Kymionis G, Kontadakis G, Yoo S. Update on simultaneous topo-guided photorefractive keratectomy immediately followed by corneal collagen crosslinking for treatment of progressive keratoconus. Int J Kerat Ect Cor Dis. 2012;1(3):185–189. [Google Scholar]
- 30.Kymionis GD, Diakonis VF, Kalyvianaki M, Portaliou D, Siganos C, Kozobolis VP, Pallikaris AI. One-year follow-up of corneal confocal microscopy after corneal cross-linking in patients with post laser in situ keratosmileusis ectasia and keratoconus. Am J Ophthalmol. 2009;147(5):774–778. 778.e1. doi: 10.1016/j.ajo.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 31.Padmanabhan P, Radhakrishnan A, Venkataraman AP, Gupta N, Srinivasan B. Corneal changes following collagen cross linking and simultaneous topography guided photoablation with collagen cross linking for keratoconus. Indian J Ophthalmol. 2014;62(2):229–235. doi: 10.4103/0301-4738.111209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vinciguerra P, Albè E, Trazza S, Rosetta P, Vinciguerra R, Seiler T, Epstein D. Refractive, topographic, tomographic, and aberrometric analysis of keratoconic eyes undergoing corneal cross-linking. Ophthalmology. 2009;116(3):369–378. doi: 10.1016/j.ophtha.2008.09.048. [DOI] [PubMed] [Google Scholar]
- 33.Mohammadpour M, Farhadi B, Mirshahi R, Masoumi A, Mirghorbani M. Simultaneous photorefractive keratectomy and accelerated collagen cross-linking in high-risk refractive surgery (Tehran protocol): 3-year outcomes. Int Ophthalmol. 2020;40(10):2659–2666. doi: 10.1007/s10792-020-01447-9. [DOI] [PubMed] [Google Scholar]


