Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent of the ongoing coronavirus disease 2019 (COVID-19) pandemic. Viral replication in the respiratory tract induces the death of infected cells and the release of pathogen- associated molecular patterns (PAMPs). PAMPs give rise to local inflammation, increasing the secretion of pro- inflammatory cytokines and chemokines, which attract immune cells from the blood into the infected lung. In most individuals, lung-recruited cells clear the infection, and the immune response retreats. However, in some cases, a dysfunctional immune response occurs, which triggers a cytokine storm in the lung, leading to acute respiratory distress syndrome (ARDS). Severe COVID-19 is characterized by an impaired innate and adaptive immune response and by a massive expansion of myeloid-derived suppressor cells (MDSCs). MDSCs function as protective regulators of the immune response, protecting the host from over-immunoreactivity and hyper-inflammation. However, under certain conditions, such as chronic inflammation and cancer, MDSCs could exert a detrimental role. Accordingly, the early expansion of MDSCs in COVID-19 is able to predict the fatal outcome of the infection. Here, we review recent data on MDSCs during COVID-19, discussing how they can influence the course of the disease and whether they could be considered as biomarker and possible targets for new therapeutic approaches.
Keywords: PMN-MDSC, M-MDSC, SARS-CoV-2, COVID-19, immune response
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent of the ongoing coronavirus disease 2019 (COVID-19) pandemic. It is a positive-sense, single-stranded RNA virus of the Coronaviridae family. The pathogenesis of SARS-CoV-2 initiates when the viral particles infect airway epithelial cells, alveolar epithelial cells, vascular endothelial cells, and macrophages in the lung through angiotensin-converting enzyme 2 (ACE2) (1). Viral replication induces the cell destruction and the release of pathogen-associated molecular patterns (PAMPs), inducing local inflammation characterized by increased secretion of the pro-inflammatory cytokines and chemokines interleukin 6 (IL-6), interferon gamma (IFN-γ), monocyte chemoattractant protein 1 (MCP1), and IFN-γ-inducible protein 10 (IP-10) (2). These cytokines and chemokines attract immune cells, notably monocytes and T lymphocytes, from the blood into the infected lung (3).
In most individuals, lung-recruited immune cells clear the infection, and the immune response retreats. However, in some cases, a dysfunctional immune response occurs, which triggers a cytokine storm, mediating widespread lung inflammation. In particular, IL-6 was associated with a high risk of mortality during COVID-19 (4). IL-6 can stimulate various cell types expressing the membrane-bound IL-6 receptor and the glycoprotein (gp130) receptor, leading to constitutive activation of the Janus kinase (JAK) signal transducer and activator of transcription (STAT) (5, 6). Accordingly, JAK-STAT signaling has been shown to be increased in COVID-19 patients (7, 8). STAT3 activation promotes IL-6 gene expression, amplifying this inflammatory pathway (6). On the other hand, the suppressor of cytokine signaling 3 (SOCS3) pathway, which has negative feedback on IL-6 production, is downregulated during COVID-19, thus contributing to IL-6 hyper-production (9). In turn, the uncontrolled inflammation can cause multi-organ damage, leading to organ failure. A large body of literature reported the effects of immune-based therapies targeting inflammatory mediators such as JAK or cytokine inhibitors, demonstrating improved outcomes and survival (10, 11).
Beyond cytokine storm, lymphopenia, high leukocyte counts, and increased neutrophil–lymphocyte ratios have been described as features of severe COVID-19 (12). Neutrophils have been demonstrated to play a role in COVID-19 pathology through the release of neutrophil extracellular traps (NETs). Indeed, tracheal aspirates and pulmonary autopsies from COVID-19 patients showed NET-containing microthrombi` and neutrophil–platelet infiltration (13, 14). SARS-CoV-2 can directly induce the release of NETs by healthy neutrophils, and NETs released by SARS-CoV-2-activated neutrophils promote lung epithelial cell death in vitro (14).
In order to dissect the biology of the virus–immune system interaction during COVID-19, several studies employed high-dimensional phenotypic and molecular approaches. These studies highlighted the absence of an IFN signature in severe patients compared to mild and moderate cases and evidenced a sustained emergency myelopoiesis associated with an increase in immature neutrophils and monocytes with immunosuppressive features (15–18). Among immunosuppressive cells, myeloid-derived suppressor cells (MDSCs) emerged as one of the players in the pathogenesis of SARS-CoV-2 infection.
Herein, we review recent data on MDSCs during COVID-19 and their pleiotropic activities, discuss how they can influence the course of the disease, and whether they could be considered as possible targets for new therapeutic approaches.
MDSC Differentiation
A huge number of leukocytes are generated and replaced daily. Different pathological conditions can perturb the leukocyte turnover, resulting in the emergency of myelopoiesis (19) to provide cells for eliminating tumor cells, infectious agents, or tissue damage. If these conditions resolve quickly, the myelopoiesis declines without negative consequences for the host. However, a number of conditions associated with various types of chronic inflammation result in aberrant sustained myelopoiesis characterized by the accumulation of immature myeloid cells with regulatory functions, ultimately defined as MDSCs (20–22). The first observation of myeloid cells with suppressive functions was reported in cancer-bearing mice, where they were able to inhibit T-cell activities (23). The importance of this cell population has been pointed out by accumulating evidence on its contribution to the negative regulation of immune responses during cancer and other diseases in humans. MDSCs are able to inhibit T-cell proliferation and activation (24, 25), modulate cytokine production by macrophages (26), suppress the function of natural killer (NK) cells (27), impair dendritic cell (DC) differentiation and action (28, 29), and induce regulatory T cells (Tregs) (30). Furthermore, MDSCs are capable of inhibiting the proliferation and differentiation of B cells and inducing regulatory B cells in several pathological conditions (31–34).
Besides their immunological functions, MDSCs exert other actions such as the promotion of tumor angiogenesis (35, 36), invasion, and metastasis (37), indicating that they can exert pleiotropic activities.
A pro-inflammatory microenvironment is responsible for MDSC expansion, inducing their proliferation, recruitment, and activation. Several factors, usually associated with pro-inflammatory processes, are involved in MDSC differentiation: prostaglandin E2 (PGE-2) (38), cyclooxygenase-2 (COX-2) (39), stem cell factor (SCF) (40), macrophage colony-stimulating factor (M-CSF), granulocyte/macrophage colony-stimulating factor (GM-CSF) (41), IL-6 (42), tumor necrosis factor alpha (TNF-α) (43), IFN-γ (44), and vascular endothelial grow factor (VEGF) (45). These molecules trigger the STAT3 pathway, which is the master transcription factor regulating the expressions of genes involved in the expansion of MDSCs (46).
MDSC Identification and Function
MDSCs include two major subsets based on their phenotypic and morphological features: polymorphonuclear (PMN) and monocytic (M) MDSCs. In physiological conditions, bone marrow hematopoietic stem cells (HSCs) differentiate into common myeloid progenitor (CMP) cells and then into immature myeloid cells (IMCs). Normally, IMCs migrate to different peripheral organs, where they differentiate into dendritic cells, macrophages, and granulocytes. However, factors produced by tumor cells or during acute or chronic infections and after trauma promote MDSC generation by preventing IMC differentiation and acquiring immunosuppressive functions (38, 44, 47, 48). The classic definition of MDSCs as immature myeloid cells blocked in their differentiation has been updated by recent studies suggesting that, under certain conditions, M-MDSCs and PMN-MDSCs may originate from monocytes and granulocytes (49). Thus, the family of MDSCs includes not only immature cells but also highly differentiated elements belonging to the monocyte and granulocyte lineages.
Murine PMN-MDSC can be clearly identified as CD11b++Ly6G+Ly6Clow cells, while M-MDSCs as CD11b+Ly6G−Ly6Chigh. Due to the lack of specific markers for human MDSCs, recently, a standard characterization has been suggested for their identification: among human peripheral blood mononuclear cells (PBMCs), the equivalent to PMN-MDSCs is defined as HLA-DR−/lowCD11b+CD14−CD15+ (or CD66b+) and M-MDSCs as HLA-DR−/lowCD11b+ (or CD33+) CD14+CD15−. A third group of MDSCs, early-stage MDSCs (e-MDSCs), can be identified as HLA-DR−CD33+CD15−Lin− (CD3−CD56−CD19−CD14−) (50). The ability to suppress immune cells is an important characteristic of MDSCs, and the gold standard for the designation of cells as MDSCs is the inhibition of T-cell functions (50).
MDSCs have a potent immunosuppressive function that is mediated by different mechanisms: they are able to deplete l-arginine from the microenvironment by secreting arginase 1 Arg-1 and inducible nitric oxide synthase (iNOS). The deprivation of l-arginine inhibits the activity of T cells by decreasing CD3ζ, a key molecule in T-cell receptor (TCR) signaling. Other important factors that contribute to the suppressive activity of MDSCs are reactive oxygen species (ROS) and reactive nitrogen species (RNS). ROS production reduces the expression of CD3ζ on T cells (51), and its inhibition abrogates the suppressive effects of MDSCs in vitro (52). The RNS peroxynitrite produced by MDSCs is able to silence T-cell activation by nitrating TCR and CD8 molecules, thus preventing antigen-specific stimulation (25). Furthermore, the production of nitric oxide (NO) by iNOS interferes with the JAK/STAT signaling pathway in T cells (24, 53).
MDSCs can secrete transforming growth factor beta (TGF-β) and IL-10, which exert direct immunosuppressive effects on T cells, induce the generation of Tregs (30), and inhibit IL-12 production by macrophages (26). Moreover, MDSCs can suppress the activity of NK cells by expressing membrane-bound TGF-β (27). Finally, MDSCs express programmed death-ligand 1 (PD-L1), a potent mediator of immunosuppression (54, 55). The engagement of PD-L1 with programmed cell death protein 1 (PD-1) in T cells induces dysfunction, exhaustion, and IL-10 production (56).
MDSCs and COVID-19
MDSC Expansion During SARS-CoV-2 Infection
Several reports have highlighted the potential role of MDSCs during infections. In particular, in humans, some bacterial (57), viral (58), and parasitic (59) infections are characterized by the expansion of the MDSC population. The first paper showing the expansion of MDSCs during COVID-19 was published in October 2020 by our group, showing a high frequency of phenotypically resembling MDSCs in PBMCs from patients with COVID-19 (60). MDSCs frequency correlated with the level of inflammatory mediators in patients with COVID-19. We then showed a massive expansion of PMN-MDSCs in severe COVID-19 patients with the capacity to inhibit T-cell proliferation and IFN-γ production upon superantigen stimulation (61). In the same paper, we followed COVID-19 patients after hospital admission and found a persistently higher frequency of PMN-MDSCs in patients with severe compared to those with mild disease.
One of the features of severe COVID-19 is the altered neutrophil abundance, phenotype, and functionality. A high number of neutrophils have been observed in the nasopharyngeal epithelium (62), the lung (63), and in the blood of patients infected with SARS-CoV-2 (64). Interestingly, single-cell RNA sequencing (scRNA-seq) revealed the emergence of CD10lowCD101−CXCR1+ immature neutrophils that are reminiscent of PMN-MDSCs (65, 66). Thus, immunosuppressive neutrophil precursors, such as the pre-neutrophil (preNeu) population, which is CXCR4-positive (67), may be released prematurely into the blood from the bone marrow and infiltrate the lung tissue in patients with severe disease. We could then speculate that the expansion of PMN-MDSCs may account, at least in part, for the neutrophilia observed during severe COVID-19.
ScRNA-seq revealed high levels of HLA-DR−/low monocytes in patients with severe COVID-19, whose phenotype resembled M-MDSCs (65, 66, 68). The scRNA-seq data were confirmed by Falck-Jones et al. using flow cytometry, showing an increased frequency of M-MDSCs in the blood of patients with severe COVID-19 (69), even if to a lesser extent than PMN-MDSCs. The highest levels of MDSCs were reported in fatal cases of COVID-19 (69, 70), suggesting a detrimental role of MDSCs in COVID-19. A significant increase of low-density neutrophils (LDNs) expressing lectin-type oxidized low-density lipoprotein receptor 1 (LOX-1) in the blood of patients with acute COVID-19 was also observed (71). Functional assays demonstrated the immunosuppressive capacities of these cells, thus confirming them as PMN-MDSCs. LOX-1 has been recently identified as a specific marker distinguishing PMN-MDSCs from polymorphonuclear cells (PMNs). In fact, among PMNs, the LOX-1+ subset exerted a potent suppressive activity (72).
Immunometabolic phenotypical characterization of PBMCs from COVID-19 patients also highlighted the presence of voltage-dependent anion channel (VIDACI)+ hexokinase II (HKII)+ PMN-MDSCs (73). The concurrent upregulation of VIDACI and HKII has been described to be associated with the production of ROS (74) and with the prevention of ROS-induced cell death (75), aimed, with other mechanisms, at increasing MDSC survival in the presence of high ROS levels (76). Moreover, carnitine palmitoyltransferase 1a (CPT1a)+VIDCAI+DR− M-MDSC expansion was observed in patients with severe COVID-19 (73). CPT1a is involved in fatty acid oxidation and has been correlated with the recruitment and differentiation of MDSCs (77).
Hyper-inflammation is a hallmark of severe COVID-19 (2). Pro-inflammatory mediators are pivotal in the regulation of MDSC differentiation and accumulation (78). Indeed, during COVID-19, the frequency of MDSC correlated with the plasma levels of IL-1β, IL-6, IL-8, and TNF-α (69–71), confirming that the immune system attempted to curb the excessive and potentially harmful immune response to SARS-CoV-2 infection. However, in severe COVID-19 patients, in addition to monocytes, MDSCs were able to produce IL-6 under stimulation (79), suggesting that they could contribute to hyper-inflammation in certain conditions.
Suppressive Functions of MDSC During COVID-19
Studies evaluating MDSC function showed that MDSCs from COVID-19 patients were correlated with Arg-1 activity. Several papers have reported high levels of Arg-1 in the plasma of patients with moderate to severe/fatal COVID-19 (69, 80). Accordingly, Reizine et al. found that the expansion of MDSCs was paralleled by a high Arg-1 activity, evaluated as the ornithine/arginine ratio in plasma of patients with ARDS at hospital admission. However, the difference in Arg-1 activity was lost at the subsequent time points (81). The high activity of Arg-1 paralleled with plasma l-arginine shortage (80–82). Importantly, the addition of l-arginine to MDSC/T-cell co-cultures partially restored the production of IFN-γ and the proliferation of T cells (69, 81). Bost et al. obtained similar results, showing a correlation between the percentage of suppression of M-MDSCs and the plasma levels of Arg-1 (83). PMN-MDSCs from COVID-19 patients were able to inhibit the SARS-CoV-2-specific IFN-γ production by T cells (70) and expressed high levels of Arg-1, iNOS, and TGF-β messenger RNAs (mRNAs). However, treatment with a specific inhibitor of Arg-1 was not able to restore IFN-γ production. Differently, an increase of IFN-γ release was observed by inhibiting iNOS or by neutralizing TGF-β (70). Furthermore, a persistently higher indolamine-2,3-dioxygenase (IDO) activity was found in patients with ARDS compared to those with moderate pneumonia (79, 81). IDO catabolizes tryptophan, which is another essential amino acid for T-cell function; indeed, the decrease of tryptophan and the accumulation of its catabolites inhibited the activation of T cells (84).
Altogether, these data indicate that MDSCs from COVID-19 patients exert their suppressive activity using different mechanisms, which possibly depend on the MDSC subsets involved. MDSCs establish different metabolic pathways in different microenvironments, determining different mechanisms of suppression (85). Whether the diverse degrees of severity of COVID-19 could influence the suppressive functions of MDSCs needs further investigation.
MDSCs seem to be able to infiltrate the lung during infection. Immunohistochemistry and immunofluorescence on the lung autopsy of patients who died due to COVID-19 showed the presence of large numbers of Arg-1-positive cells and a high expression of intracytoplasmic Arg-1 in CD66b+, confirming them to be Arg-1-positive PMN-MDSC-like cells (80).
It has been demonstrated that MDSCs regulate the immune response of B cells directly by the expression of effector molecules and indirectly by controlling other immune regulatory cells (86). While the suppressive ability of MDSCs on T-cell proliferation and cytokine production has been assessed during COVID-19, their potential action on B-cell function has not been explored. To our knowledge, only one paper evaluated the correlation between the frequency of PMN-MDSCs and the level of anti-SARS-CoV-2 S1 immunoglobulin G (IgG) in 10 convalescence patients who recovered from a mild or asymptomatic SARS-CoV-2 infection. The authors showed an almost significant negative correlation between PMN-MDSCs and anti-S IgG (87), suggesting a possible involvement of MDSCs on B-cell functional modulation. However, a larger group is needed to confirm this preliminary result.
MDSC and Platelet Activation
We and others found a decrease of plasma l-arginine during severe COVID-19 that correlated with the activities of Arg-1 and iNOS (80–82). We also demonstrated that the frequency of PMN-MDSCs directly correlated with platelet activation, and purified PMN-MDSCs from patients with COVID-19 were able to induce platelet activation, possibly by reducing l-arginine. The concentration of l-arginine can modulate platelet activation and aggregation (88). Indeed, its deprivation reduced substrate availability for iNOS, thus reducing NO production. NO plays a pivotal role in inhibiting platelet activation. It enters the platelets and promotes the upregulation of cyclic guanosine monophosphate (cGMP). cGMP activates protein kinase G, which directly diminishes platelet reactivity by phosphorylating crucial proteins involved in platelet activation (88).
Altogether, these data highlight a novel role of MDSCs in driving the immunopathogenesis of COVID-19 and increasing the complexity of the immune response to SARS-CoV-2.
MDSCs as a Biomarker of COVID-19 Severity
Studies evaluating the frequency of MDSC-like cells in patients with different COVID-19 disease severities showed the highest MDSC percentages in the severe form of the disease (61, 68–71, 79, 80, 89). In detail, patients with more severe COVID-19 disease had significantly higher percentage of M-MDSCs and PMN-MDSCs compared with those with mild disease and healthy donors (HDs) (61, 69, 70, 80). The frequency of M-MDSCs in blood from patients with COVID-19 seemed to decrease over time and returned to frequency similar to those seen in HDs in follow-up samples taken during convalescence (69). ScRNA-seq revealed the expansion of monocytes with a MDSC-like phenotype only in severe COVID-19 patients (68). The expansion of LDNs with suppressive function was observed in severe COVID-19 patients. In particular, LOX-1+ LDNs were higher in severe COVID-19 compared to mild cases (71). Tomic et al. showed increased frequency and number of both M-MDSCs and PMN-MDSCs in the group of patients with severe disease compared to those with mild COVID-19 and in HDs. Moreover, principal component analysis (PCA) showed a clear clustering of severe, mild, and non-COVID-19 disease, suggesting that MDSCs are associated with the severity of COVID-19. Moreover, the frequency of MDSCs producing IL-10 was higher in severe compared to mild COVID-19 patients and in HDs (79). Some studies also observed a higher frequency of MDSCs in non-survival compared to survival patients (69–71), suggesting that the frequency of MDSCs could be used as a predictive marker of the disease outcome. Specifically, a receiver operating characteristic (ROC) curve analysis indicated that the frequency of MDSCs at the time of hospitalization might predict fatal outcomes of the disease, with a cutoff value of 54.91% (70). Moreover, by estimating the hazard ratio (HR) of death adjusted for age and gender, it has been observed that the percentage of PMN-MDSCs at the time of hospitalization was independently associated with fatal outcomes of COVID-19 (70).
Overall, several publications have shown that the MDSC frequency could be used as a biomarker of COVID-19 severity. However, larger prospective multicenter studies are needed to evaluate the predictive biomarker potential of MDSCs and its possible use in monitoring disease progression.
Due to the suppressive role of MDSCs, it would be very interesting to examine whether they could play a role in the response to anti-SARS-CoV-2 vaccinations in fragile patients. Vaccines are the main tools in counteracting SARS-CoV-2-induced disease. Several studies have reported a low humoral response after vaccination in patients with malignancies or diseases that required immunosuppressive therapies (90–94). Different mechanisms can be postulated, such as the underlying disease and, mostly, the treatment of the specific disease. Whether MDSCs can impact on the effectiveness of vaccination is completely unexplored and should be investigated in order to evaluate new markers for patient monitoring and vaccine treatment optimization.
MDSCs as Therapeutic Targets in COVID-19
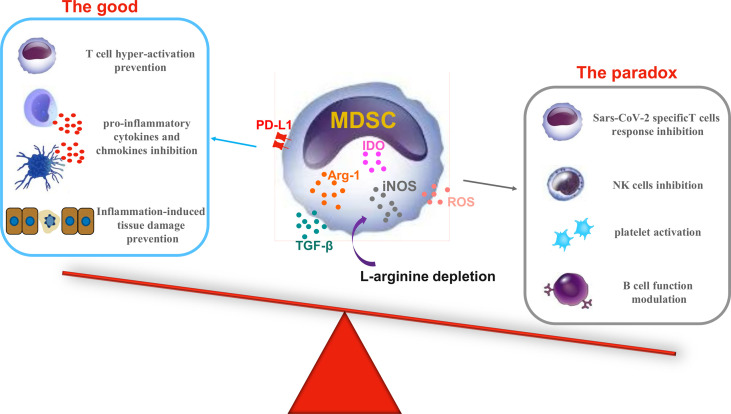
Data on MDSCs during COVID-19 suggest the detrimental role of this suppressive cell population and highlight the rationale for possible use of therapeutic approaches focused on reducing MDSC number/function. Surprisingly, Bost et al. reported a decline in the percentage of T-cell suppression by monocytes/M-MDSC-like and LDNs/PMN-MDSC cells in severe compared to mild patients. An even lower percentage of T-cell suppression was observed in non-survival patients (83). Altogether, these data raise the question of the balance between the beneficial/detrimental roles of MDSCs during the different stages of COVID-19 ( Figure 1 ).
Figure 1.
The good and the paradox of myeloid-derived suppressor cell (MDSC) activities during coronavirus disease 2019 (COVID-19). During severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, MDSC subsets increase and are activated by the virus-induced inflammatory response. The left panel shows the plausible beneficial role of suppressive molecules produced by MDSCs during COVID-19 (the good); the right panel shows the downside of good, pointing out the detrimental effects of the same molecules (the paradox). Arg-1, arginase 1; IDO, indoleamine-2,3-dioxygenase; iNOS, inducible nitric oxide synthase; ROS, reactive oxygen species; PD-L1, programmed death-ligand 1; TGF-β, transforming growth factor beta.
Preclinical studies on new cancer therapy approaches proposed numerous strategies to target MDSCs: i) depletion of MDSCs (95, 96); ii) inhibition of the suppressive functions of MDSCs (97–99); iii) prevention of MDSC recruitment (100, 101); and iv) induction of MDSC differentiation toward monocytes/granulocytes (102, 103).
Among the therapeutic approaches that are being tested to treat COVID-19, some could affect MDSC differentiation and function. The first example is the anti-IL-6 receptor tocilizumab. As mentioned above, due to the association between the plasma levels of IL-6 and the fatal outcomes of COVID-19, the anti-IL-6 receptor monoclonal antibody tocilizumab was introduced for treatment of the disease, showing reduced mortality, an increased chance of successful hospital discharge, and a reduced risk of invasive mechanical ventilation (104). IL-6 inhibitors have been successfully tested for their ability to block MDSC expansion (105). However, the impact of tocilizumab, or other immunomodulatory agents, on MDSC frequency has been poorly explored. Tomić et al. did not find any difference in the frequency of M-MDSCs and PMN-MDSCs in a very small group of COVID-19 patients previously treated with tocilizumab compared to non-treated patients matched for age, sex, and disease severity (79). New studies are necessary to clarify the effect of this inhibitor on the modulation of the number and function of MDSCs during treatment and its association with therapy efficacy.
Some clinical trials are ongoing evaluating the effect of l-arginine supplementation on clinical improvements of COVID-19 (clinicaltrials.gov). l-Arginine is involved in several biological processes, including the regulation of endothelial function, serving as a substrate for NO production by endothelial cells, thus regulating cardiovascular homeostasis (106). MDSCs exert their suppressive functions through Arg-1 and iNOS, which are involved in reducing the availability of l-arginine during COVID-19 (107). In vitro l-arginine addition increased the proliferation rates of CD4 and CD8 T cells from COVID-19 patients (81). It would be interesting to evaluate whether in vivo l-arginine supplementation may overcome the MDSC-mediated l-arginine deprivation.
A few studies also suggested an association between vitamin D deficiency and hospitalization risk or COVID-19 severity (108, 109), and several trials are evaluating the impact of vitamin D treatment on the outcomes of COVID-19. Vitamin D has been demonstrated to inhibit the expansion and suppressive functions of MDSC (110, 111), but studies evaluating the correlation between vitamin D levels and MDSC functions during COVID-19 are still lacking.
Another example is leronlimab, an inhibitor of CCR5 signaling. Preliminary studies have shown that leronlimab treatment of COVID-19 patients induced a reduction of plasma IL-6, restoration of the CD4/CD8 ratio, and resolution of SARS-CoV-2 plasma viremia (112). CCR5 has a critical role not only in the recruitment but also in the activation of MDSCs in tumor lesions (113), and targeting the CCR5/CCL5 axis may reduce the suppressive activity of MDSCs (114).
Many other molecules have been successfully tested in cancer settings to reduce the accumulation and suppressive functions of MDSCs. Some of these had STAT3 signaling as a target: sunitinib reversed tumor MDSC accumulation through STAT3 or c-Kit signaling, and metformin downregulated the function of MDSCs through the AMPK/STAT3 pathway. Entinostat, a class I histone deacetylase inhibitor, neutralized MDSCs through reducing the expressions of both Arg-1 and iNOS [reviewed in (115)]. Another molecule tested is all-trans retinoic acid (ATRA). ATRA is a standard component of therapy for patients with acute promyelocytic leukemia (116), and several reports indicated its efficacy in reducing the number of MDSCs in murine cancer models (96, 117, 118). ATRA acts by inducing the differentiation of MDSCs toward monocytes, DCs, or granulocytes, thus abolishing their suppressive functions (119, 120). Interestingly, ATRA has shown an anti-SARS-CoV-2 activity in vitro (121, 122), possibly by increasing the expression of retinoic acid-inducible gene I (RIG-I) on target cells (123).
Altogether, these data suggest the possibility of combining immunomodulatory treatments and new approaches targeting MDSCs to avoid the detrimental role of MDSCs on SARS-CoV-2-specific immunity and platelet activation and, at the same time, to reduce the harmful impacts of the inflammatory storm and viral replication.
Conclusion
SARS-CoV-2 infection induces massive activation of the immune system, ultimately leading to the suppression of innate and adaptive immune responses. MDSCs are key cellular players in this complicated process. Both M-MDSCs and PMN-MDSCs accumulate in patients with COVID-19 and represent an attempt to maintaining a homeostatic balance between protective immune response and a maladaptive damaging uncontrolled inflammation. However, MDSC accumulation associates with fatal disease outcomes, indicating the detrimental role of MDSCs possibly mediated by the suppression of the adaptive immune response. More investigations are essential to define when (in terms of time or percentage) the suppressive functions of MDSCs could be harmful rather than beneficial during COVID-19. Clarifying this issue is pivotal to evaluating the timing and type of possible therapeutic approaches targeting MDSCs.
Author Contributions
AS, GG, and CA wrote sections of the paper. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was funded by Ministry of Health (Ricerca Corrente LR 1).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the INMI COVID-19 Study Group.
References
- 1. Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell (2020) 183:1735. doi: 10.1016/j.cell.2020.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, China. Lancet (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological Findings of COVID-19 Associated With Acute Respiratory Distress Syndrome. Lancet Respir Med (2020) 8:420–2. doi: 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients With COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen X, Zhao B, Qu Y, Chen Y, Xiong J, Feng Y, et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated With Drastically Elevated Interleukin 6 Level in Critically Ill Patients With Coronavirus Disease 2019. Clin Infect Dis (2020) 71:1937–42. doi: 10.1093/cid/ciaa449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hedrick TL, Murray BP, Mock JR. COVID-19: Clean Up on IL-6. Am J Respir Cell Mol Biol (2020) 63:541–3. doi: 10.1165/rcmb.2020-0277LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Herold T, Jurinovic V, Arnreich C, Lipworth BJ, Hellmuth JC, von Bergwelt-Baildon M, et al. Elevated Levels of IL-6 and CRP Predict the Need for Mechanical Ventilation in COVID-19. J Allergy Clin Immunol (2020) 146:128–136.e4. doi: 10.1016/j.jaci.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Musiu C, Caligola S, Fiore A, Lamolinara A, Frusteri C, Del Pizzo FD, et al. Fatal Cytokine Release Syndrome by an Aberrant FLIP/STAT3 Axis. Cell Death Differ (2022) 29:420–38. doi: 10.1038/s41418-021-00866-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ascierto PA, Fu B, Wei H. IL-6 Modulation for COVID-19: The Right Patients at the Right Time? J Immunother Cancer (2021) 9:e002285. doi: 10.1136/jitc-2020-002285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. REMAP-CAP Investigators. Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, Nichol AD, et al. Interleukin-6 Receptor Antagonists in Critically Ill Patients With Covid-19. N Engl J Med (2021) 384:1491–502. doi: 10.1056/NEJMoa2100433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aman J, Duijvelaar E, Botros L, Kianzad A, Schippers JR, Smeele PJ, et al. Imatinib in Patients With Severe COVID-19: A Randomised, Double-Blind, Placebo-Controlled, Clinical Trial. Lancet Respir Med (2021) 9:957–68. doi: 10.1016/S2213-2600(21)00237-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis (2020) 71:762–8. doi: 10.1093/cid/ciaa248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Middleton EA, He XY, Denorme F, Campbell RA, Ng D, Salvatore SP, et al. Neutrophil Extracellular Traps Contribute to Immunothrombosis in COVID-19 Acute Respiratory Distress Syndrome. Blood (2020) 136:1169–79. doi: 10.1182/blood.2020007008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Veras FP, Pontelli MC, Silva CM, Toller-Kawahisa JE, de Lima M, Nascimento DC, et al. SARS-CoV-2-Triggered Neutrophil Extracellular Traps Mediate COVID-19 Pathology. J Exp Med (2020) 217:e20201129. doi: 10.1084/jem.20201129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Laing AG, Lorenc A, Del Molino Del Barrio I, Das A, Fish M, Monin L, et al. A Dynamic COVID-19 Immune Signature Includes Associations With Poor Prognosis. Nat Med (2020) 26:1623–35. doi: 10.1038/s41591-020-1038-6 [DOI] [PubMed] [Google Scholar]
- 16. Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, et al. Impaired Type I Interferon Activity and Inflammatory Responses in Severe COVID-19 Patients. Science (2020) 369:718–24. doi: 10.1126/science.abc6027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bost P, Giladi A, Liu Y, Bendjelal Y, Xu G, David E, et al. Host-Viral Infection Maps Reveal Signatures of Severe COVID-19 Patients. Cell (2020) 181:1475–1488.e12. doi: 10.1016/j.cell.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wilk AJ, Rustagi A, Zhao NQ, Roque J, Martinez-Colon GJ, McKechnie JL, et al. A Single-Cell Atlas of the Peripheral Immune Response in Patients With Severe COVID-19. Nat Med (2020) 26:1070–6. doi: 10.1038/s41591-020-0944-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Boettcher S, Manz MG. Sensing and Translation of Pathogen Signals Into Demand-Adapted Myelopoiesis. Curr Opin Hematol (2016) 23:5–10. doi: 10.1097/MOH.0000000000000201 [DOI] [PubMed] [Google Scholar]
- 20. Talmadge JE, Gabrilovich DI. History of Myeloid-Derived Suppressor Cells. Nat Rev Cancer (2013) 13:739–52. doi: 10.1038/nrc3581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Boros P, Ochando J, Zeher M. Myeloid Derived Suppressor Cells and Autoimmunity. Hum Immunol (2016) 77:631–6. doi: 10.1016/j.humimm.2016.05.024 [DOI] [PubMed] [Google Scholar]
- 22. Dai J, El Gazzar M, Li GY, Moorman JP, Yao ZQ. Myeloid-Derived Suppressor Cells: Paradoxical Roles in Infection and Immunity. J Innate Immun (2015) 7:116–26. doi: 10.1159/000368233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Young MR, Newby M, Wepsic HT. Hematopoiesis and Suppressor Bone Marrow Cells in Mice Bearing Large Metastatic Lewis Lung Carcinoma Tumors. Cancer Res (1987) 47:100–5. [PubMed] [Google Scholar]
- 24. Rodriguez PC, Quiceno DG, Ochoa AC. L-Arginine Availability Regulates T-Lymphocyte Cell-Cycle Progression. Blood (2007) 109:1568–73. doi: 10.1182/blood-2006-06-031856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nagaraj S, Gupta K, Pisarev V, Kinarsky L, Sherman S, Kang L, et al. Altered Recognition of Antigen is a Mechanism of CD8+ T Cell Tolerance in Cancer. Nat Med (2007) 13:828–35. doi: 10.1038/nm1609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sinha P, Clements VK, Bunt SK, Albelda SM, Ostrand-Rosenberg S. Cross-Talk Between Myeloid-Derived Suppressor Cells and Macrophages Subverts Tumor Immunity Toward a Type 2 Response. J Immunol (2007) 179:977–83. doi: 10.4049/jimmunol.179.2.977 [DOI] [PubMed] [Google Scholar]
- 27. Li H, Han Y, Guo Q, Zhang M, Cao X. Cancer-Expanded Myeloid-Derived Suppressor Cells Induce Anergy of NK Cells Through Membrane-Bound TGF-Beta 1. J Immunol (2009) 182:240–9. doi: 10.4049/jimmunol.182.1.240 [DOI] [PubMed] [Google Scholar]
- 28. Greifenberg V, Ribechini E, Rossner S, Lutz MB. Myeloid-Derived Suppressor Cell Activation by Combined LPS and IFN-Gamma Treatment Impairs DC Development. Eur J Immunol (2009) 39:2865–76. doi: 10.1002/eji.200939486 [DOI] [PubMed] [Google Scholar]
- 29. Poschke I, Mao Y, Adamson L, Salazar-Onfray F, Masucci G, Kiessling R. Myeloid-Derived Suppressor Cells Impair the Quality of Dendritic Cell Vaccines. Cancer Immunol Immunother (2012) 61:827–38. doi: 10.1007/s00262-011-1143-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Huang B, Pan PY, Li Q, Sato AI, Levy DE, Bromberg J, et al. Gr-1+CD115+ Immature Myeloid Suppressor Cells Mediate the Development of Tumor-Induced T Regulatory Cells and T-Cell Anergy in Tumor-Bearing Host. Cancer Res (2006) 66:1123–31. doi: 10.1158/0008-5472.CAN-05-1299 [DOI] [PubMed] [Google Scholar]
- 31. Lelis FJN, Jaufmann J, Singh A, Fromm K, Teschner AC, Poschel S, et al. Myeloid-Derived Suppressor Cells Modulate B-Cell Responses. Immunol Lett (2017) 188:108–15. doi: 10.1016/j.imlet.2017.07.003 [DOI] [PubMed] [Google Scholar]
- 32. Li Y, Tu Z, Qian S, Fung JJ, Markowitz SD, Kusner LL, et al. Myeloid-Derived Suppressor Cells as a Potential Therapy for Experimental Autoimmune Myasthenia Gravis. J Immunol (2014) 193:2127–34. doi: 10.4049/jimmunol.1400857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Park MJ, Lee SH, Kim EK, Lee EJ, Park SH, Kwok SK, et al. Myeloid-Derived Suppressor Cells Induce the Expansion of Regulatory B Cells and Ameliorate Autoimmunity in the Sanroque Mouse Model of Systemic Lupus Erythematosus. Arthritis Rheumatol (2016) 68:2717–27. doi: 10.1002/art.39767 [DOI] [PubMed] [Google Scholar]
- 34. Knier B, Hiltensperger M, Sie C, Aly L, Lepennetier G, Engleitner T, et al. Myeloid-Derived Suppressor Cells Control B Cell Accumulation in the Central Nervous System During Autoimmunity. Nat Immunol (2018) 19:1341–51. doi: 10.1038/s41590-018-0237-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kujawski M, Kortylewski M, Lee H, Herrmann A, Kay H, Yu H. Stat3 Mediates Myeloid Cell-Dependent Tumor Angiogenesis in Mice. J Clin Invest (2008) 118:3367–77. doi: 10.1172/JCI35213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yang L, DeBusk LM, Fukuda K, Fingleton B, Green-Jarvis B, Shyr Y, et al. Expansion of Myeloid Immune Suppressor Gr+CD11b+ Cells in Tumor-Bearing Host Directly Promotes Tumor Angiogenesis. Cancer Cell (2004) 6:409–21. doi: 10.1016/j.ccr.2004.08.031 [DOI] [PubMed] [Google Scholar]
- 37. Yang L, Huang J, Ren X, Gorska AE, Chytil A, Aakre M, et al. Abrogation of TGF Beta Signaling in Mammary Carcinomas Recruits Gr-1+CD11b+ Myeloid Cells That Promote Metastasis. Cancer Cell (2008) 13:23–35. doi: 10.1016/j.ccr.2007.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sinha P, Clements VK, Fulton AM, Ostrand-Rosenberg S. Prostaglandin E2 Promotes Tumor Progression by Inducing Myeloid-Derived Suppressor Cells. Cancer Res (2007) 67:4507–13. doi: 10.1158/0008-5472.CAN-06-4174 [DOI] [PubMed] [Google Scholar]
- 39. Chang CL, Ma B, Pang X, Wu TC, Hung CF. Treatment With Cyclooxygenase-2 Inhibitors Enables Repeated Administration of Vaccinia Virus for Control of Ovarian Cancer. Mol Ther (2009) 17:1365–72. doi: 10.1038/mt.2009.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pan PY, Wang GX, Yin B, Ozao J, Ku T, Divino CM, et al. Reversion of Immune Tolerance in Advanced Malignancy: Modulation of Myeloid-Derived Suppressor Cell Development by Blockade of Stem-Cell Factor Function. Blood (2008) 111:219–28. doi: 10.1182/blood-2007-04-086835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Serafini P, Carbley R, Noonan KA, Tan G, Bronte V, Borrello I. High-Dose Granulocyte-Macrophage Colony-Stimulating Factor-Producing Vaccines Impair the Immune Response Through the Recruitment of Myeloid Suppressor Cells. Cancer Res (2004) 64:6337–43. doi: 10.1158/0008-5472.CAN-04-0757 [DOI] [PubMed] [Google Scholar]
- 42. Wu CT, Hsieh CC, Lin CC, Chen WC, Hong JH, Chen MF. Significance of IL-6 in the Transition of Hormone-Resistant Prostate Cancer and the Induction of Myeloid-Derived Suppressor Cells. J Mol Med (Berl) (2012) 90:1343–55. doi: 10.1007/s00109-012-0916-x [DOI] [PubMed] [Google Scholar]
- 43. Sade-Feldman M, Kanterman J, Ish-Shalom E, Elnekave M, Horwitz E, Baniyash M. Tumor Necrosis Factor-Alpha Blocks Differentiation and Enhances Suppressive Activity of Immature Myeloid Cells During Chronic Inflammation. Immunity (2013) 38:541–54. doi: 10.1016/j.immuni.2013.02.007 [DOI] [PubMed] [Google Scholar]
- 44. Gallina G, Dolcetti L, Serafini P, De Santo C, Marigo I, Colombo MP, et al. Tumors Induce a Subset of Inflammatory Monocytes With Immunosuppressive Activity on CD8+ T Cells. J Clin Invest (2006) 116:2777–90. doi: 10.1172/JCI28828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gabrilovich D, Ishida T, Oyama T, Ran S, Kravtsov V, Nadaf S, et al. Vascular Endothelial Growth Factor Inhibits the Development of Dendritic Cells and Dramatically Affects the Differentiation of Multiple Hematopoietic Lineages In Vivo. Blood (1998) 92:4150–66. doi: 10.1182/blood.V92.11.4150 [DOI] [PubMed] [Google Scholar]
- 46. Nefedova Y, Nagaraj S, Rosenbauer A, Muro-Cacho C, Sebti SM, Gabrilovich DI. Regulation of Dendritic Cell Differentiation and Antitumor Immune Response in Cancer by Pharmacologic-Selective Inhibition of the Janus-Activated Kinase 2/Signal Transducers and Activators of Transcription 3 Pathway. Cancer Res (2005) 65:9525–35. doi: 10.1158/0008-5472.CAN-05-0529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Young MR, Wright MA, Young ME. Antibodies to Colony-Stimulating Factors Block Lewis Lung Carcinoma Cell Stimulation of Immune-Suppressive Bone Marrow Cells. Cancer Immunol Immunother (1991) 33:146–52. doi: 10.1007/BF01756134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bronte V, Chappell DB, Apolloni E, Cabrelle A, Wang M, Hwu P, et al. Unopposed Production of Granulocyte-Macrophage Colony-Stimulating Factor by Tumors Inhibits CD8+ T Cell Responses by Dysregulating Antigen-Presenting Cell Maturation. J Immunol (1999) 162:5728–37. [PMC free article] [PubMed] [Google Scholar]
- 49. Millrud CR, Bergenfelz C, Leandersson K. On the Origin of Myeloid-Derived Suppressor Cells. Oncotarget (2017) 8:3649–65. doi: 10.18632/oncotarget.12278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bronte V, Brandau S, Chen SH, Colombo MP, Frey AB, Greten TF, et al. Recommendations for Myeloid-Derived Suppressor Cell Nomenclature and Characterization Standards. Nat Commun (2016) 7:12150. doi: 10.1038/ncomms12150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kusmartsev S, Nefedova Y, Yoder D, Gabrilovich DI. Antigen-Specific Inhibition of CD8+ T Cell Response by Immature Myeloid Cells in Cancer is Mediated by Reactive Oxygen Species. J Immunol (2004) 172:989–99. doi: 10.4049/jimmunol.172.2.989 [DOI] [PubMed] [Google Scholar]
- 52. Liu Y, Wei J, Guo G, Zhou J. Norepinephrine-Induced Myeloid-Derived Suppressor Cells Block T-Cell Responses via Generation of Reactive Oxygen Species. Immunopharmacol Immunotoxicol (2015) 37:359–65. doi: 10.3109/08923973.2015.1059442 [DOI] [PubMed] [Google Scholar]
- 53. Bingisser RM, Tilbrook PA, Holt PG, Kees UR. Macrophage-Derived Nitric Oxide Regulates T Cell Activation via Reversible Disruption of the Jak3/STAT5 Signaling Pathway. J Immunol (1998) 160:5729–34. [PubMed] [Google Scholar]
- 54. Yamauchi Y, Safi S, Blattner C, Rathinasamy A, Umansky L, Juenger S, et al. Circulating and Tumor Myeloid-Derived Suppressor Cells in Resectable Non-Small Cell Lung Cancer. Am J Respir Crit Care Med (2018) 198:777–87. doi: 10.1164/rccm.201708-1707OC [DOI] [PubMed] [Google Scholar]
- 55. Lu C, Redd PS, Lee JR, Savage N, Liu K. The Expression Profiles and Regulation of PD-L1 in Tumor-Induced Myeloid-Derived Suppressor Cells. Oncoimmunology (2016) 5:e1247135. doi: 10.1080/2162402X.2016.1247135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sun Z, Fourcade J, Pagliano O, Chauvin JM, Sander C, Kirkwood JM, et al. IL10 and PD-1 Cooperate to Limit the Activity of Tumor-Specific CD8+ T Cells. Cancer Res (2015) 75:1635–44. doi: 10.1158/0008-5472.CAN-14-3016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ost M, Singh A, Peschel A, Mehling R, Rieber N, Hartl D. Myeloid-Derived Suppressor Cells in Bacterial Infections. Front Cell Infect Microbiol (2016) 6:37. doi: 10.3389/fcimb.2016.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Goh C, Narayanan S, Hahn YS. Myeloid-Derived Suppressor Cells: The Dark Knight or the Joker in Viral Infections? Immunol Rev (2013) 255:210–21. doi: 10.1111/imr.12084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Van Ginderachter JA, Beschin A, De Baetselier P, Raes G. Myeloid-Derived Suppressor Cells in Parasitic Infections. Eur J Immunol (2010) 40:2976–85. doi: 10.1002/eji.201040911 [DOI] [PubMed] [Google Scholar]
- 60. Bordoni V, Sacchi A, Cimini E, Notari S, Grassi G, Tartaglia E, et al. An Inflammatory Profile Correlates With Decreased Frequency of Cytotoxic Cells in Coronavirus Disease 2019. Clin Infect Dis (2020) 71:2272–5. doi: 10.1093/cid/ciaa577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Agrati C, Sacchi A, Bordoni V, Cimini E, Notari S, Grassi G, et al. Expansion of Myeloid-Derived Suppressor Cells in Patients With Severe Coronavirus Disease (COVID-19). Cell Death Differ (2020) 27:3196–207. doi: 10.1038/s41418-020-0572-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chua RL, Lukassen S, Trump S, Hennig BP, Wendisch D, Pott F, et al. COVID-19 Severity Correlates With Airway Epithelium-Immune Cell Interactions Identified by Single-Cell Analysis. Nat Biotechnol (2020) 38:970–9. doi: 10.1038/s41587-020-0602-4 [DOI] [PubMed] [Google Scholar]
- 63. Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao J, et al. Single-Cell Landscape of Bronchoalveolar Immune Cells in Patients With COVID-19. Nat Med (2020) 26:842–4. doi: 10.1038/s41591-020-0901-9 [DOI] [PubMed] [Google Scholar]
- 64. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Silvin A, Chapuis N, Dunsmore G, Goubet AG, Dubuisson A, Derosa L, et al. Elevated Calprotectin and Abnormal Myeloid Cell Subsets Discriminate Severe From Mild COVID-19. Cell (2020) 182:1401–1418.e18. doi: 10.1016/j.cell.2020.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Schulte-Schrepping J, Reusch N, Paclik D, Bassler K, Schlickeiser S, Zhang B, et al. Severe COVID-19 Is Marked by a Dysregulated Myeloid Cell Compartment. Cell (2020) 182:1419–1440.e23. doi: 10.1016/j.cell.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Evrard M, Kwok IWH, Chong SZ, Teng KWW, Becht E, Chen J, et al. Developmental Analysis of Bone Marrow Neutrophils Reveals Populations Specialized in Expansion, Trafficking, and Effector Functions. Immunity (2018) 48:364–379.e8. doi: 10.1016/j.immuni.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 68. Kvedaraite E, Hertwig L, Sinha I, Ponzetta A, Hed Myrberg I, Lourda M, et al. Major Alterations in the Mononuclear Phagocyte Landscape Associated With COVID-19 Severity. Proc Natl Acad Sci USA (2021) 118:e2018587118. doi: 10.1073/pnas.2018587118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Falck-Jones S, Vangeti S, Yu M, Falck-Jones R, Cagigi A, Badolati I, et al. Functional Monocytic Myeloid-Derived Suppressor Cells Increase in Blood But Not Airways and Predict COVID-19 Severity. J Clin Invest (2021) 131:e144734. doi: 10.1172/JCI144734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Sacchi A, Grassi G, Bordoni V, Lorenzini P, Cimini E, Casetti R, et al. Early Expansion of Myeloid-Derived Suppressor Cells Inhibits SARS-CoV-2 Specific T-Cell Response and may Predict Fatal COVID-19 Outcome. Cell Death Dis (2020) 11:921–020-03125-1. doi: 10.1038/s41419-020-03125-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Cabrera LE, Pekkarinen PT, Alander M, Nowlan KHA, Nguyen NA, Jokiranta S, et al. Characterization of Low-Density Granulocytes in COVID-19. PloS Pathog (2021) 17:e1009721. doi: 10.1371/journal.ppat.1009721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Condamine T, Dominguez GA, Youn JI, Kossenkov AV, Mony S, Alicea-Torres K, et al. Lectin-Type Oxidized LDL Receptor-1 Distinguishes Population of Human Polymorphonuclear Myeloid-Derived Suppressor Cells in Cancer Patients. Sci Immunol (2016) 1:aaf8943. doi: 10.1126/sciimmunol.aaf8943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Thompson EA, Cascino K, Ordonez AA, Zhou W, Vaghasia A, Hamacher-Brady A, et al. Metabolic Programs Define Dysfunctional Immune Responses in Severe COVID-19 Patients. Cell Rep (2021) 34:108863. doi: 10.1016/j.celrep.2021.108863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Hall CJ, Boyle RH, Astin JW, Flores MV, Oehlers SH, Sanderson LE, et al. Immunoresponsive Gene 1 Augments Bactericidal Activity of Macrophage-Lineage Cells by Regulating Beta-Oxidation-Dependent Mitochondrial ROS Production. Cell Metab (2013) 18:265–78. doi: 10.1016/j.cmet.2013.06.018 [DOI] [PubMed] [Google Scholar]
- 75. Shoshan-Barmatz V, De Pinto V, Zweckstetter M, Raviv Z, Keinan N, Arbel N. VDAC, a Multi-Functional Mitochondrial Protein Regulating Cell Life and Death. Mol Aspects Med (2010) 31:227–85. doi: 10.1016/j.mam.2010.03.002 [DOI] [PubMed] [Google Scholar]
- 76. Jian SL, Chen WW, Su YC, Su YW, Chuang TH, Hsu SC, et al. Glycolysis Regulates the Expansion of Myeloid-Derived Suppressor Cells in Tumor-Bearing Hosts Through Prevention of ROS-Mediated Apoptosis. Cell Death Dis (2017) 8:e2779. doi: 10.1038/cddis.2017.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Mohammadpour H, MacDonald CR, McCarthy PL, Abrams SI, Repasky EA. Beta2-Adrenergic Receptor Signaling Regulates Metabolic Pathways Critical to Myeloid-Derived Suppressor Cell Function Within the TME. Cell Rep (2021) 37:109883. doi: 10.1016/j.celrep.2021.109883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Gabrilovich DI, Nagaraj S. Myeloid-Derived Suppressor Cells as Regulators of the Immune System. Nat Rev Immunol (2009) 9:162–74. doi: 10.1038/nri2506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Tomic S, Dokic J, Stevanovic D, Ilic N, Gruden-Movsesijan A, Dinic M, et al. Reduced Expression of Autophagy Markers and Expansion of Myeloid-Derived Suppressor Cells Correlate With Poor T Cell Response in Severe COVID-19 Patients. Front Immunol (2021) 12:614599. doi: 10.3389/fimmu.2021.614599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Dean MJ, Ochoa JB, Sanchez-Pino MD, Zabaleta J, Garai J, Del Valle L, et al. Severe COVID-19 Is Characterized by an Impaired Type I Interferon Response and Elevated Levels of Arginase Producing Granulocytic Myeloid Derived Suppressor Cells. Front Immunol (2021) 12:695972. doi: 10.3389/fimmu.2021.695972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Reizine F, Lesouhaitier M, Gregoire M, Pinceaux K, Gacouin A, Maamar A, et al. SARS-CoV-2-Induced ARDS Associates With MDSC Expansion, Lymphocyte Dysfunction, and Arginine Shortage. J Clin Immunol (2021) 41:515–25. doi: 10.1007/s10875-020-00920-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Sacchi A, Grassi G, Notari S, Gili S, Bordoni V, Tartaglia E, et al. Expansion of Myeloid Derived Suppressor Cells Contributes to Platelet Activation by L-Arginine Deprivation During SARS-CoV-2 Infection. Cells (2021) 10:2111. doi: 10.3390/cells10082111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Bost P, De Sanctis F, Cane S, Ugel S, Donadello K, Castellucci M, et al. Deciphering the State of Immune Silence in Fatal COVID-19 Patients. Nat Commun (2021) 12:1428–021-21702-6. doi: 10.1038/s41467-021-21702-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Smith C, Chang MY, Parker KH, Beury DW, DuHadaway JB, Flick HE, et al. IDO is a Nodal Pathogenic Driver of Lung Cancer and Metastasis Development. Cancer Discovery (2012) 2:722–35. doi: 10.1158/2159-8290.CD-12-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Li X, Li Y, Yu Q, Qian P, Huang H, Lin Y. Metabolic Reprogramming of Myeloid-Derived Suppressor Cells: An Innovative Approach Confronting Challenges. J Leukoc Biol (2021) 110:257–70. doi: 10.1002/JLB.1MR0421-597RR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Ozkan B, Lim H, Park SG. Immunomodulatory Function of Myeloid-Derived Suppressor Cells During B Cell-Mediated Immune Responses. Int J Mol Sci (2018) 19:E1468. doi: 10.3390/ijms19051468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Sieminska I, Weglarczyk K, Surmiak M, Kurowska-Baran D, Sanak M, Siedlar M, et al. Mild and Asymptomatic COVID-19 Convalescents Present Long-Term Endotype of Immunosuppression Associated With Neutrophil Subsets Possessing Regulatory Functions. Front Immunol (2021) 12:748097. doi: 10.3389/fimmu.2021.748097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Naseem KM, Roberts W. Nitric Oxide at a Glance. Platelets (2011) 22:148–52. doi: 10.3109/09537104.2010.522629 [DOI] [PubMed] [Google Scholar]
- 89. Parackova Z, Bloomfield M, Klocperk A, Sediva A. Neutrophils Mediate Th17 Promotion in COVID-19 Patients. J Leukoc Biol (2021) 109:73–6. doi: 10.1002/JLB.4COVCRA0820-481RRR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Perry C, Luttwak E, Balaban R, Shefer G, Morales MM, Aharon A, et al. Efficacy of the BNT162b2 mRNA COVID-19 Vaccine in Patients With B-Cell non-Hodgkin Lymphoma. Blood Adv (2021) 5:3053–61. doi: 10.1182/bloodadvances.2021005094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Mrak D, Tobudic S, Koblischke M, Graninger M, Radner H, Sieghart D, et al. SARS-CoV-2 Vaccination in Rituximab-Treated Patients: B Cells Promote Humoral Immune Responses in the Presence of T-Cell-Mediated Immunity. Ann Rheum Dis (2021) 80:1345–50. doi: 10.1136/annrheumdis-2021-220781 [DOI] [PubMed] [Google Scholar]
- 92. Picchianti-Diamanti A, Aiello A, Lagana B, Agrati C, Castilletti C, Meschi S, et al. ImmunosuppressiveTherapies Differently Modulate Humoral- and T-Cell-Specific Responses to COVID-19 mRNA Vaccine in Rheumatoid Arthritis Patients. Front Immunol (2021) 12:740249. doi: 10.3389/fimmu.2021.740249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Apostolidis SA, Kakara M, Painter MM, Goel RR, Mathew D, Lenzi K, et al. Cellular and Humoral Immune Responses Following SARS-CoV-2 mRNA Vaccination in Patients With Multiple Sclerosis on Anti-CD20 Therapy. Nat Med (2021) 27:1990–2001. doi: 10.1038/s41591-021-01507-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Monin L, Laing AG, Munoz-Ruiz M, McKenzie DR, Del Molino Del Barrio I, Alaguthurai T, et al. Safety and Immunogenicity of One Versus Two Doses of the COVID-19 Vaccine BNT162b2 for Patients With Cancer: Interim Analysis of a Prospective Observational Study. Lancet Oncol (2021) 22:765–78. doi: 10.1016/S1470-2045(21)00213-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Suzuki E, Kapoor V, Jassar AS, Kaiser LR, Albelda SM. Gemcitabine Selectively Eliminates Splenic Gr-1+/CD11b+ Myeloid Suppressor Cells in Tumor-Bearing Animals and Enhances Antitumor Immune Activity. Clin Cancer Res (2005) 11:6713–21. doi: 10.1158/1078-0432.CCR-05-0883 [DOI] [PubMed] [Google Scholar]
- 96. Bauer R, Udonta F, Wroblewski M, Ben-Batalla I, Santos IM, Taverna F, et al. Blockade of Myeloid-Derived Suppressor Cell Expansion With All-Trans Retinoic Acid Increases the Efficacy of Antiangiogenic Therapy. Cancer Res (2018) 78:3220–32. doi: 10.1158/0008-5472.CAN-17-3415 [DOI] [PubMed] [Google Scholar]
- 97. Melani C, Sangaletti S, Barazzetta FM, Werb Z, Colombo MP. Amino-Biphosphonate-Mediated MMP-9 Inhibition Breaks the Tumor-Bone Marrow Axis Responsible for Myeloid-Derived Suppressor Cell Expansion and Macrophage Infiltration in Tumor Stroma. Cancer Res (2007) 67:11438–46. doi: 10.1158/0008-5472.CAN-07-1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Vasquez-Dunddel D, Pan F, Zeng Q, Gorbounov M, Albesiano E, Fu J, et al. STAT3 Regulates Arginase-I in Myeloid-Derived Suppressor Cells From Cancer Patients. J Clin Invest (2013) 123:1580–9. doi: 10.1172/JCI60083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Kuroda H, Mabuchi S, Yokoi E, Komura N, Kozasa K, Matsumoto Y, et al. Prostaglandin E2 Produced by Myeloid-Derived Suppressive Cells Induces Cancer Stem Cells in Uterine Cervical Cancer. Oncotarget (2018) 9:36317–30. doi: 10.18632/oncotarget.26347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Flores-Toro JA, Luo D, Gopinath A, Sarkisian MR, Campbell JJ, Charo IF, et al. CCR2 Inhibition Reduces Tumor Myeloid Cells and Unmasks a Checkpoint Inhibitor Effect to Slow Progression of Resistant Murine Gliomas. Proc Natl Acad Sci USA (2020) 117:1129–38. doi: 10.1073/pnas.1910856117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Bockorny B, Semenisty V, Macarulla T, Borazanci E, Wolpin BM, Stemmer SM, et al. BL-8040, a CXCR4 Antagonist, in Combination With Pembrolizumab and Chemotherapy for Pancreatic Cancer: The COMBAT Trial. Nat Med (2020) 26:878–85. doi: 10.1038/s41591-020-0880-x [DOI] [PubMed] [Google Scholar]
- 102. Lathers DM, Clark JI, Achille NJ, Young MR. Phase 1B Study to Improve Immune Responses in Head and Neck Cancer Patients Using Escalating Doses of 25-Hydroxyvitamin D3. Cancer Immunol Immunother (2004) 53:422–30. doi: 10.1007/s00262-003-0459-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Stiff A, Trikha P, Wesolowski R, Kendra K, Hsu V, Uppati S, et al. Myeloid-Derived Suppressor Cells Express Bruton's Tyrosine Kinase and Can Be Depleted in Tumor-Bearing Hosts by Ibrutinib Treatment. Cancer Res (2016) 76:2125–36. doi: 10.1158/0008-5472.CAN-15-1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. RECOVERY Collaborative Group . Tocilizumab in Patients Admitted to Hospital With COVID-19 (RECOVERY): A Randomised, Controlled, Open-Label, Platform Trial. Lancet (2021) 397:1637–45. doi: 10.1016/S0140-6736(21)00676-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Sumida K, Wakita D, Narita Y, Masuko K, Terada S, Watanabe K, et al. Anti-IL-6 Receptor mAb Eliminates Myeloid-Derived Suppressor Cells and Inhibits Tumor Growth by Enhancing T-Cell Responses. Eur J Immunol (2012) 42:2060–72. doi: 10.1002/eji.201142335 [DOI] [PubMed] [Google Scholar]
- 106. Gambardella J, Khondkar W, Morelli MB, Wang X, Santulli G, Trimarco V. Arginine and Endothelial Function. Biomedicines (2020) 8:E277. doi: 10.3390/biomedicines8080277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Rees CA, Rostad CA, Mantus G, Anderson EJ, Chahroudi A, Jaggi P, et al. Altered Amino Acid Profile in Patients With SARS-CoV-2 Infection. Proc Natl Acad Sci USA (2021) 118:e2101708118. doi: 10.1073/pnas.2101708118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Jude EB, Ling SF, Allcock R, Yeap BXY, Pappachan JM. Vitamin D Deficiency Is Associated With Higher Hospitalization Risk From COVID-19: A Retrospective Case-Control Study. J Clin Endocrinol Metab (2021) 106:e4708–15. doi: 10.1210/clinem/dgab439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Kazemi A, Mohammadi V, Aghababaee SK, Golzarand M, Clark CCT, Babajafari S. Association of Vitamin D Status With SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-Analysis. Adv Nutr (2021) 12:1636–58. doi: 10.1093/advances/nmab012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Bruns H, Bottcher M, Qorraj M, Fabri M, Jitschin S, Dindorf J, et al. CLL-Cell-Mediated MDSC Induction by Exosomal miR-155 Transfer is Disrupted by Vitamin D. Leukemia (2017) 31:985–8. doi: 10.1038/leu.2016.378 [DOI] [PubMed] [Google Scholar]
- 111. Fleet JC, Burcham GN, Calvert RD, Elzey BD, Ratliff TL. 1alpha, 25 Dihydroxyvitamin D (1,25(OH)2D) Inhibits the T Cell Suppressive Function of Myeloid Derived Suppressor Cells (MDSC). J Steroid Biochem Mol Biol (2020) 198:105557. doi: 10.1016/j.jsbmb.2019.105557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Patterson BK, Seethamraju H, Dhody K, Corley MJ, Kazempour K, Lalezari J, et al. CCR5 Inhibition in Critical COVID-19 Patients Decreases Inflammatory Cytokines, Increases CD8 T-Cells, and Decreases SARS-CoV2 RNA in Plasma by Day 14. Int J Infect Dis (2021) 103:25–32. doi: 10.1016/j.ijid.2020.10.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Umansky V, Blattner C, Gebhardt C, Utikal J. CCR5 in Recruitment and Activation of Myeloid-Derived Suppressor Cells in Melanoma. Cancer Immunol Immunother (2017) 66:1015–23. doi: 10.1007/s00262-017-1988-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Ban Y, Mai J, Li X, Mitchell-Flack M, Zhang T, Zhang L, et al. Targeting Autocrine CCL5-CCR5 Axis Reprograms Immunosuppressive Myeloid Cells and Reinvigorates Antitumor Immunity. Cancer Res (2017) 77:2857–68. doi: 10.1158/0008-5472.CAN-16-2913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Gao X, Sui H, Zhao S, Gao X, Su Y, Qu P. Immunotherapy Targeting Myeloid-Derived Suppressor Cells (MDSCs) in Tumor Microenvironment. Front Immunol (2021) 11:585214. doi: 10.3389/fimmu.2020.585214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Sanz MA, Fenaux P, Tallman MS, Estey EH, Lowenberg B, Naoe T, et al. Management of Acute Promyelocytic Leukemia: Updated Recommendations From an Expert Panel of the European LeukemiaNet. Blood (2019) 133:1630–43. doi: 10.1182/blood-2019-01-894980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Long AH, Highfill SL, Cui Y, Smith JP, Walker AJ, Ramakrishna S, et al. Reduction of MDSCs With All-Trans Retinoic Acid Improves CAR Therapy Efficacy for Sarcomas. Cancer Immunol Res (2016) 4:869–80. doi: 10.1158/2326-6066.CIR-15-0230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Ene-Obong A, Clear AJ, Watt J, Wang J, Fatah R, Riches JC, et al. Activated Pancreatic Stellate Cells Sequester CD8+ T Cells to Reduce Their Infiltration of the Juxtatumoral Compartment of Pancreatic Ductal Adenocarcinoma. Gastroenterology (2013) 145:1121–32. doi: 10.1053/j.gastro.2013.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Nefedova Y, Fishman M, Sherman S, Wang X, Beg AA, Gabrilovich DI. Mechanism of All-Trans Retinoic Acid Effect on Tumor-Associated Myeloid-Derived Suppressor Cells. Cancer Res (2007) 67:11021–8. doi: 10.1158/0008-5472.CAN-07-2593 [DOI] [PubMed] [Google Scholar]
- 120. Mirza N, Fishman M, Fricke I, Dunn M, Neuger AM, Frost TJ, et al. All-Trans-Retinoic Acid Improves Differentiation of Myeloid Cells and Immune Response in Cancer Patients. Cancer Res (2006) 66:9299–307. doi: 10.1158/0008-5472.CAN-06-1690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Morita T, Miyakawa K, Jeremiah SS, Yamaoka Y, Sada M, Kuniyoshi T, et al. All-Trans Retinoic Acid Exhibits Antiviral Effect Against SARS-CoV-2 by Inhibiting 3clpro Activity. Viruses (2021) 13:1669. doi: 10.3390/v13081669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Yamamotoya T, Nakatsu Y, Kanna M, Hasei S, Ohata Y, Encinas J, et al. Prolyl Isomerase Pin1 Plays an Essential Role in SARS-CoV-2 Proliferation, Indicating its Possibility as a Novel Therapeutic Target. Sci Rep (2021) 11:18581–021-97972-3. doi: 10.1038/s41598-021-97972-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Yamada T, Sato S, Sotoyama Y, Orba Y, Sawa H, Yamauchi H, et al. RIG-I Triggers a Signaling-Abortive Anti-SARS-CoV-2 Defense in Human Lung Cells. Nat Immunol (2021) 22:820–8. doi: 10.1038/s41590-021-00942-0 [DOI] [PubMed] [Google Scholar]