Abstract
In Ethiopia, community-based health insurance was implemented to promote equitable access to sustainable quality health care and increase financial protection. The purpose of this study was to identify factors associated with community-based Health Insurance, Health Care Service Utilization of Households in the South Gondar Zone. A community-based cross-sectional study was employed. Data were collected among 619 randomly selected households in the south Gondar zone. Chi-square and binary logistic regression analyses with a P-Value of less than .05 were used to determine the association. Out of the total households, 511(82.6%) were using the CBHI scheme for health care service utilization. Residence, marital status, education level, occupation status, family size, presence of under-five children in the household, presence of elders in the households, nearest health institution, presence of chronic illness in the household’s, time taken to reach health institution, an attitude of a household were the determinant factors of community-based health insurance scheme health care service utilization of households. It is recommended that the local, regional and national governments, policymakers on optimal actions, NGOs, and other supporting organizations shall improve or scale-up the scheme by providing awareness to the community based on these significant factors and the attitude of households.
Keywords: Household, logistic regression, community based health insurance, out-of-pocket
Background
Community-based health insurance (CBHI) schemes have been implemented all over the world. The CBHI was created in response to a need for financial protection for the poor against catastrophic medical expenses. CBHI plans to reduce out-of-pocket payments and increase access to healthcare services, in addition to generating additional revenue for the health sector. 1 The World Health Organization (WHO) recommends CBHI as one of the approaches for reducing catastrophic out-of-pocket expenditure for registered families. 2
In most developing nations, healthcare costs were primarily paid through out-of-pocket (OOP) payments by patients at the time and place of treatment, which faced the challenge of raising sufficient funds to finance health services equitably. In many low-income and middle-income countries (LMICs) the entire economic cost of illness for households is typically estimated to be greater than 10% of household income, which is classified as catastrophic.3,4 CBHI has emerged as a valuable alternative to user fees in countries with limited capacity to develop and sustain national health insurance programmes by pooling risks and resources at the community level.5,6
Globally, millions of people suffer and die because they do not have the money to pay for health care. No country in the world can successfully give full health coverage to its citizens because of a shortage of spending money for health care services. According to the WHO, 150 million people worldwide experience financial hardship each year, and more than 100 million are pushed into poverty because of direct payments for healthcare-related services. According to reports, even the United States is unable to provide health care coverage to all of its inhabitants, with 46 million Americans lacking adequate coverage.7,8
In Africa, out-of-pocket payments (which account for 30%-85% of total health spending in the poorest nations) are still the most common method of payment, which is attributed to a higher risk of accruing very expensive health costs and impoverishment. The most common reason for families falling below the poverty line is health-related expenditures. 9 Some African countries have recently introduced health insurance as a strategy for achieving Universal Health Coverage, to improve citizens’ access to health care, provide financial protection for the sick and poor, mobilize resources for service improvement, and ultimately contribute to improved health quality. 10
In Sub-Saharan Africa, the majority of health care service is accessed through out-of-pocket user fees expenditure, which in many instances may lead to the use of low-standard health care services. However, the CBHI scheme has recently emerged as a promising alternative for a risk pooling healthcare system that will hopefully result in better utilization of healthcare services, reduced illness-related income shocks, and eventually a fully functional and sustainable universal healthcare system. 11 The problems with the affordability of premiums, the trust in the integrity and competence of the managers, the attractiveness of the benefits package, and the quality of care are offered by the providers. 12
In Ethiopia, public health care suffers from poor management, poor service quality, and weak finance.13,14 To promote equitable access to sustainable quality health care and increase financial protection community-based health insurance was implemented. Ethiopia’s Federal Ministry of Health (FMoH) launched the programme in partnership with USAID, Abt Associates Inc., an international consulting firm, and CARE Ethiopia, an international non-governmental organization. The programme is part of the government’s larger healthcare financing reform agenda, which aims to increase healthcare quality and coverage by discovering alternative healthcare resources. 15 CBHI benefits packages include all family health services and curative care including inpatient, outpatient services, and chronic, and acute illnesses. 16 Despite the Ethiopian government’s efforts, the community-based health insurance (CBHI) enrolment rate still failed to achieve the expected goal. 17 According to the Ethiopian Health Insurance Agency Pilot Schemes final report, 58% of Ethiopian households have enrolled in CBHI, whereas 38% of households in the south Gondar zone are involved in CBHI. 18
CBHI schemes are effective in reducing out-of-pocket payments of their members, and in improving access to health services. However, many schemes also reported low enrollment rates. 19 One of the reasons for the low utilization of modern health care services is the user fee charges. User fees can present a substantial psychological and financial burden to the families. It is one of the barriers to healthcare use, especially for poor households who are themselves likely to be particularly vulnerable to ill health. Thus, moving away from out-of-pocket charges for health care at the time of use is an important step towards averting the financial hardship associated with paying for health care services.20,21 CBHI aims to improve access to care for the poor but this scheme has been unsuccessful due to low enrollment rates. These variations in membership of voluntary schemes suggest that there are factors that limit individuals from Use of CBHI. 22 Hence, to fill this gap we aimed to identify factors associated with CBHI healthcare service utilization of households in South Gondar Zone, Ethiopia.
Methods and Materials
Study design and area
A community-based cross-sectional study was employed in South Gondar Zone. South Gondar zone is located 666 km to the north of Addis Ababa, the capital of Ethiopia. According to the 2007 census conducted by the Central Statistical Agency of Ethiopia (CSA), this Zone has a total population of 2 051 738 and an increase of 16% over the 1994 census, of whom 1 041 061 are men and 1 010 677 women. With an area of 14 095.19 square kilometers, South Gondar has a population density of 145.56; 195 619 or 9.53% are urban inhabitants. A total of 468,238 households were counted in this Zone . 23 Among 13 woreda’s in the South Gondar zone 3 districts/woreda’s that implementing CBHI were randomly selected (these randomly selected woredas are Laye Gayint, Libokekem, and Fogera).
Source of data and method of data collection
The main sources of data for this study were primary data, which were directly collected from households. A structured questionnaire was prepared in English, which was then translated into Amharic, the local language. The heads of households were the major responders. Face-to-face interviews were carried out with the help of structured, pre-tested questions. Diploma holders who spoke the native language fluently served as data collectors. Data collectors received 3 days of instruction on the study’s objectives, data collection methods, and tools. Senior public health professionals served as supervisors.
Sample size determination and sampling procedure
Before the actual data collection, the emphasis was made on the determination of sample size that mainly depended on the purpose of the study, the available resources, and the precision required. The sample size for this study was calculated using a single population proportion formula, with the following assumptions: 95% confidence level, 5% margin of error, and 58% proportion of households enrolled in community-based health insurance, which is obtained from the previous study in Ethiopia, 3 as well as a design effect of 1.5 and a 10% non-response rate. The sample size (n) was determined as follow;
After adding a non-response rate of 10%, the total number of houses in the study was 619. To assess the study participants, a multi-stage sampling technique was used. proportional allocation will be utilized to determine the number of households from each district and kebele (the smallest administrative unit in Ethiopia). Finally, simple random sampling was employed to select study participants by their name using computer-generated random numbers in an Excel spreadsheet from the sampling frame.
Operational definitions
Out-Of-Pocket (OOP) health service utilization: expenditure of household for healthcare utilization at the time and place of treatment.
Household: is defined as a person or group of people related or adopted legally, who live together and share a common pot of food.
Head of household: is a person who provides actual support and maintenance to other members of the household.
Healthcare Institutions: health-oriented organizations that established formally including health posts, health centres, clinics, pharmacies, and hospitals working in the study area.
Health care Service Utilization (Visits): is the receiving of healthcare services from formal healthcare providers or use of drugs that are intended to respond to perceived illness and diseases or to improve an individual’s health status including inpatient and outpatient services.
Variables of the study
The study variables for this investigation were taken from the relevant literature. We measured all variables at the household level; because the use of CBHI is at the household level.
Response variables
The dependent variable is CBHI health care services utilization of households.
Independent variables
Based on the reviewed literature, some of the common predictors that had been expected to influence the dependent variable were sociodemographic factors, Economic Factors, healthcare access-related factors, and health perception and healthcare needs Factors.
The independent variables are; gender, Age, Education level, Religion, Occupation, Marital status, Family size, Average yearly income (in Birr), Presence of chronic illness in the household, Presence of elderly people (above 65 years) in the household, Nearest health institution, Distance from a health facility in Kilometers, the time taken to reach health, Presence of transportation road, Presence of pone in the households, Presence of radio in the households, Presence of TV in the household's, Perceived quality of care, and Attitude of the household's towards CBHI scheme.
Data management and analysis
We assessed the quality, accuracy, and completeness of the collected data using cross-validation checks. The data was entered into EPI-Data vs 3.02 for Windows and exported to SPSS vs 25 and R vs 4.1.0. The data were analysed using descriptive statistics (summary measures) and inferential analysis. To show the relationship between the response and the independent categorical variables, we used chi-square taste of association. The determinants of CBHI health care service utilization were also determined using logistic regression. For variables shown to have a significant association with the outcome variable, a P-Value of less than .05 and a 95% confidence level of significance were used.
Ethical considerations
Ethical approval was obtained from the Institutional Ethics Review Board [IRB] of Debre Tabor University. An official authorization letter was written to each of the 3 districts and kebeles (Ethiopia’s smallest administrative unit) where the study was conducted. The purpose of the study was explained to the participants, and oral agreement was obtained from each household head/ study participant prior to beginning the interview, with the respondents assured of confidentiality.
Results
Descriptive statistics
The descriptive statistics for the socio-demographic, economic, health-care access-related, health perception, and healthcare needs-related categorical variables were described in Table 1. In this study, we used 619 respondents, of which 511 (82.6%) used the CBHI scheme for health care service utilization and the remaining 108 (17.4%) were used out-of-pocket healthcare service utilization. Out of these total respondents, 370 (59.8%) were male respondents, of which 296 (80.0%) of them utilize the CBHI scheme and the remaining 74 (20%) were use OPP health care service. The majority (90.3%) of the respondents were from rural areas. When we see the marital status of the respondents 486 (78.5%) were married, 84 (13.6%) were single and the remaining 49 (7.9%) of the respondents were divorced and widowed. The majority (92.1%) of the respondents were had orthodox religion and the remaining 49 (7.9%) respondents were Muslim. When we see the education level of the respondents 234 (37.8%) of them were cannot read and write, 216 (34.9%) were can read and write, 82 (13.2%) were had primary (1-8) education level, 53 (8.6%) were had secondary education level (9-12), and the remaining 34 (5.5%) were had college and above education level. majority of the respondents, 426 (68.8%) were farmers, and the remaining 113 (18.3%), 80 (12.9%) were merchants and had other occupations respectively.
Table 1.
Sociodemographic and economic characteristics of respondents in south Gondar zone, Amhara Region, Ethiopia.
| Variables | Categories | Number of respondent’s (%) | Health care service utilization | Pearson
chi-square(X2) (P-value) |
|
|---|---|---|---|---|---|
| CBHI (%) | OPP (%) | ||||
| Gender of respondent’s | Male | 370 (59.8) | 296 (80.0) | 74 (20.0) | 4.161 (.041) |
| Female | 249 (40.2) | 215 (86.3) | 34 (13.7) | ||
| Respondent’s residence | Rural | 559 (90.3) | 497 (88.9) | 62 (11.1) | 161.768 (<.001) |
| Urban | 60 (9.7) | 14 (23.3) | 46 (76.7) | ||
| Marital status | Married | 486 (78.5) | 421 (86.6) | 65 (13.4) | 28.289 (<.001) |
| Single | 84 (13.6) | 60 (71.4) | 24 (28.6) | ||
| Others (divorced and widowed) | 49 (7.9) | 30 (61.2) | 19 (38.8) | ||
| Religion | Orthodox | 570 (92.1) | 468 (82.1) | 102 (17.9) | 1.000 (.317) |
| Muslim | 49 (7.9) | 43 (87.8) | 6 (12.2) | ||
| Education level | Cannot read and write | 234 (37.8) | 179 (76.5) | 55 (23.5) | 29.393 (<.001) |
| Can read and write | 216 (34.9) | 170 (78.7) | 46 (21.3) | ||
| Primary (1-8) | 82 (13.2) | 77 (93.9) | 5 (6.1) | ||
| Secondary (9-12) | 53 (8.6) | 52 (98.1) | 1 (1.9) | ||
| College and above | 34 (5.5) | 33 (97.1) | 1 (2.9) | ||
| Occupation status | Farmer | 426 (68.8) | 376 (88.3) | 50 (11.7) | 73.561 (<.001) |
| Merchant | 113 (18.3) | 96 (85.0) | 17 (15.0) | ||
| Others(un employment, housewife, Labor, Student) | 80 (12.9) | 39 (48.8) | 41 (51.3) | ||
| Family size of household’s | Less than 3 | 123 (19.9) | 76 (61.8) | 47 (38.2) | 48.048 (<.001) |
| 3 up to 5 | 301 (48.6) | 258 (85.7) | 43 (14.3) | ||
| Above 5 | 195 (31.5) | 177 (90.8) | 18 (9.2) | ||
| Presence of under five children in the household’s’ | Yes | 390 (63.0) | 347 (89.0) | 43 (11.0) | 30.184 (<.001) |
| No | 229 (37.0) | 164 (71.6) | 65 (28.4) | ||
| Presence of elders above 60 years in the household’s | Yes | 145 (23.4) | 132 (91.0) | 13 (9.0) | 9.458 (.002) |
| No | 474 (76.6) | 379 (80.0) | 95 (20.0) | ||
| Nearest health institution | Health post | 177 (28.6) | 121 (68.4) | 56(31.6) | 35.099 (<.001) |
| Health centre | 411(66.4) | 364 (88.6) | 47(11.4) | ||
| hospital | 31(5.0) | 26 (83.9) | 5(16.1) | ||
| Presence of chronic illness in the household’s | Yes | 169 (27.3) | 158 (93.5) | 11(6.5) | 19.312 (<.001) |
| No | 450 (72.7) | 353 (78.4) | 97(21.6) | ||
| household enrolled in any other solidarity group | Yes | 601 (97.1) | 498 (82.9) | 103(17.1) | 1.374 (.241) |
| No | 18 (2.9) | 13 (72.2) | 5(27.8) | ||
| level of awareness about CBHI | Low | 81 (13.1) | 59 (72.8) | 22 (27.2) | 6.184 (.045) |
| Medium | 258 (41.7) | 218 (84.5) | 40 (15.5) | ||
| High | 280 (45.2) | 234 (83.6) | 46 (16.4) | ||
| Presence of Radio in the household’s | Yes | 211 (34.1) | 166 (78.7) | 45 (21.3) | 3.345 (.067) |
| No | 408 (65.9) | 345 (84.6) | 63 (15.4) | ||
| Presence of Television in the household’s | Yes | 49 (7.9) | 36 (73.5) | 13 (26.5) | 3.048 (.081) |
| No | 570 (92.1) | 475 (83.3) | 95 (16.7) | ||
| Presence of phone in the household’s | Yes | 264(42.6) | 221 (83.7) | 43 (16.3) | 0.430 (.512) |
| No | 355(57.4) | 290 (81.7) | 65 (18.3) | ||
| Time taken to reach health institution | 1 up to 60 min | 414 (66.9) | 340 (82.1) | 74 (17.9) | 0.159 (.024) |
| 61 up to 120 min | 103(16.6) | 86 (83.5) | 17 (16.5) | ||
| greater than 120 min | 102(16.5) | 85 (83.3) | 17 (16.7) | ||
| Transportation road | Available | 283 (45.7) | 204 (72.1) | 79 (27.9) | 39.662 (<.001) |
| not available | 336 (54.3) | 307 (91.4) | 29 (8.6) | ||
| Satisfaction on perceived quality of care | not-satisfied | 304 (49.1) | 241 (79.3) | 63 (20.7) | 4.452 (.035) |
| Satisfied | 315 (50.9) | 270 (85.7) | 45 (14.3) | ||
| Attitude of household towards CBHI scheme | Had negative attitude | 428 (69.1) | 334 (78.0) | 94 (22.0) | 19.633 (<.001) |
| Had positive attitude | 191 (30.9) | 177 (92.7) | 14 (7.3) | ||
When we see the family size of households, 123 (19.9%) of the households had less than 3 family members, 301(48.6%) had 3 up to 5 members and the remaining 195(31.5%) had above 5 members. 390 (63.0%) of the households had under-five children in households. One hundred and forty-five (23.4%) of the households’ had above 60 years old elder persons in the households. The nearest health institutions for 177 (28.6%), 411 (66.4%), 31 (5.0%) households were health posts, health centres and hospitals, respectively. One hundred and sixty-nine (27.3%) of the households had a chronic illness positive in households. almost all of the households (601 [97.1%]) enrolled in any other solidarity group. When we see the level of awareness of the respondents about CBHI 81(13.1%), 258 (41.7%), 280 (45.2%) of the respondents had Low, Medium and High awareness respectively. Two hundred and eleven (34.1%) of the households had Radioed in the households, and 49 (7.9%) of the respondents had a television in the households. This indicates that the majority of the respondents had no media access in the households. Two hundred and sixty-four (42.6%) of the households had a mobile phone.
To reach the nearest health institution average, 414 (66.9%) of the household’s taken 1 up to 60 minutes, 103 (16.6%) of the household’s taken 61 up to 120 minutes and the remaining 102(16.5%) respondent’s taken greater than 120 minutes. 336 (54.3%) of the respondent does not have a road for transportation. 304 (49.1%) of the respondents were not satisfied with the perceived quality of care and the remaining 315 (50.9%) were satisfied. 428 (69.1%) of households had a negative attitude towards the CBHI scheme and the remaining 191(30.9%) of the respondents had a positive attitude towards the CBHI scheme. This indicates that the majority of the respondents had a negative attitude towards the use of CBHI for health care service utilization. Even if households had a negative attitude on the CBHI scheme 334(78.0%) of them used CBHI health care service utilization.
Table 2 below displays characteristics of continuous variables distance from a health facility in KM, Annual income, and age of respondents. Distance from a health facility in KM, Annual.
Table 2.
Characteristics of continuous variables of respondent’s.
| Variables | N | Minimum | Maximum | Mean | Std.dev |
|---|---|---|---|---|---|
| Distance from health facility in KM | 619 | 1 | 20 | 5.01 | 4.527 |
| Annual income | 619 | 5000 | 151 000 | 20649.56 | 16 983.323 |
| age of respondent | 619 | 19 | 75 | 39.42 | 10.578 |
Income of respondents was 5.01 K.M (with a standard deviation of 4.527 K.M), 20649.56 birrs (with a standard deviation of 16 983.323 birrs), and 39.42 years (with a standard deviation of 10.578 years) respectively.
Out of a total of 108 out-of-pocket users, the reason for non-enrolment in CBHI was described in the table below (see Table 3). The majority (58.3%) of the OPP user household are non-enrollment in CBHI because the quality of healthcare services is low. 46.3% of them said that the benefits package does not meet our needs. 42.6% of them do not utilize the CBHI scheme because of the limited availability of health services. The remaining 28.7%, 13.9%, 12.0%,3.7%,1.9% and 1.9% were CBHI non-users because of do not know enough about the CBHI scheme, Waiting time to access services is longer for CBHI members, the registration fee, and premiums are not affordable, by other reasons, illness and injury does not occur frequently in our household, and fee waiver beneficiary respectively.
Table 3.
Reason for non-enrolment in CBHI for OOP users.
| Reason of non-enrolment | n | % |
|---|---|---|
| Illness and injury does not occur frequently in our household | 2 | 1.9 |
| The registration fee and premiums are not affordable | 13 | 12.0 |
| We do not know enough about the CBHI scheme | 31 | 28.7 |
| There is limited availability of health services | 46 | 42.6 |
| The quality of health care services is low | 63 | 58.3 |
| The benefit package does not meet our needs | 50 | 46.3 |
| Waiting time to access services is longer for CBHI members | 15 | 13.9 |
| I am fee waiver beneficiary | 2 | 1.9 |
| Others | 4 | 3.7 |
The source of information for households obtained to be a member of the CBHI scheme were described in Table 4 below. 48.5% of the CBHI scheme user households obtained the information from another person previously used. 47.5% of the households have obtained the information from Kebele leaders. The rest 24.7% and 3.6% of the household have obtained information from Health professionals and Mass media respectively.
Table 4.
Source of information for households to be a member of CBHI scheme.
| Source of information for household’s | n | % |
|---|---|---|
| Health professionals | 153 | 24.7 |
| Kebele leaders | 294 | 47.5 |
| From other person previously use | 300 | 48.5 |
| Mass media | 22 | 3.6 |
Out of the CBHI scheme registered households, 494 households benefited from the scheme. Out of these household’s 147(29.85%) households benefited from the scheme by Increased access to health care,194(39.3%) households benefited from the scheme by reducing concerns about expected health care costs,360(72.9%) households benefited from the scheme by reduced costs of healthcare and 15(3%) households benefited from the scheme by other means (see Table 5 below).
Table 5.
Benefits of CBHI scheme for a member of the CBHI scheme household’s.
| Benefits of CBHI scheme | n | % |
|---|---|---|
| Increased access to health care | 147 | 29.8 |
| Reduced concerns about expected health care costs | 194 | 39.3 |
| Reduced costs of health care | 360 | 72.9 |
| Others | 15 | 3.0 |
Out of the CBHI scheme member households, 45 households were not-benefited from the CBHI scheme. The reasons respondents had not-benefited from the scheme were described in Table 6 below. Sixteen (2.6%) of them were because no one in the households has visited health facilities, 11(1.8%) of the respondents were still paid other additional costs for treatment, 18 (2.9%) of them were because of quality of health care service is poor for CBHI user.
Table 6.
Reasons of not-benefited from the CBHI scheme.
| Reasons of not-benefited | n | % |
|---|---|---|
| No one in my households has visited health facilities | 16 | 2.6 |
| We still pay other additional costs for treatment | 11 | 1.8 |
| The quality of service | 18 | 2.9 |
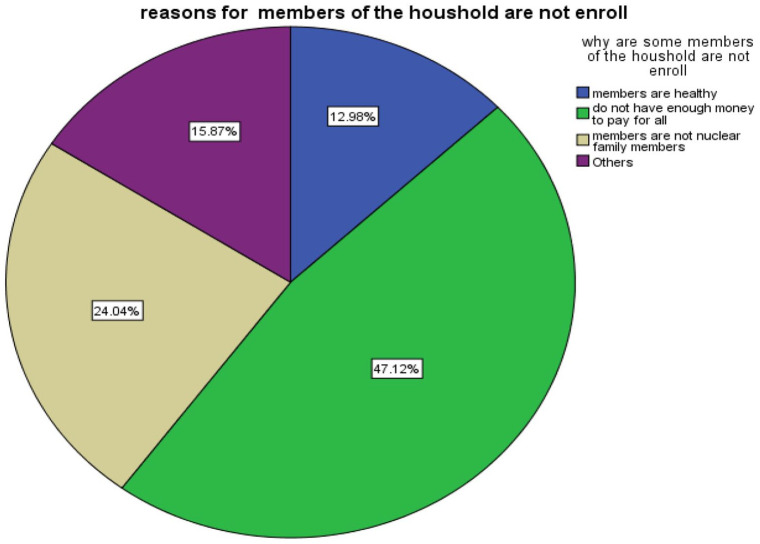
Out of a total CBHI scheme user households, 208 of the households said all household members are not enrolled in the CBHI scheme. The reason for the non-enrolment of all household members was described in Figure 1. 47.12% of the households were not-enrol all members of the household in the CBHI scheme because they do not have enough money to pay for all. 24.04% were because members are not nuclear family members. 12.69% were because family members are healthy, and the remaining 15.87% were not enrolled in all family members because of other reasons (Figure 1).
Figure 1.
Reasons of households for non-enrollment of all members in the CBHI scheme.
Factors associated with CBHI scheme health care service utilization
To identify the factors associated with the CBHI health care service utilization, the chi-squared test of association were applied. Based on a bi-variable (chi-squared) analysis, categorical variables such as gender (X2 = 4.161; P-value = .041), residence (X2 = 161.768; P-value ⩽ .001), marital status (X2 = 28.289; P-value ⩽ .001), education level (X2 = 29.393; P-value ⩽ .001), occupation status (X2 = 73.561; P-value ⩽ .001), family size (X2 = 48.048; P-value ⩽ .001), presence of under 5 children in the household (X2 = 30.184; P-value ⩽ .001), presence of elders in the households (X2 = 9.458; P-value = .002), nearest health institution(X2 = 35.099; P-value ⩽ .001), presence of chronic illness in the household’s (X2 = 19.312; P-value ⩽ .001), level of awareness about CBHI (X2 = 6.184; P-value = 0.045), presence of road for transportation (X2 = 39.662; P-value ⩽ .001), time taken to reach health institution (X2 = 0.159; P-value = .024), Satisfaction of household’s on perceived quality of care (X2 = 4.161; P-value = .041), Attitude of household towards CBHI scheme (X2 = 4.161; P-value = .041) were statistically significant at 5% levels of significance (see Table 1).
To investigate factors associated with community based health insurance healthcare service utilization of households a multi-variable analysis were performed using the binary logistic regression model (Table 7). The results of multi-variable analysis shows that urban residence (AOR = 0.018; 95%CI: 0.01, 0,05), marital status (divorced and widowed (AOR = 0.35; 95%CI: 0.02, 0.99)), education level (primary (1-8) (AOR = 9.44; 95%CI: 2.19, 5.82); secondary (9-12) (AOR = 50.43; 95%CI: 3.73, 2142.25); college and above (AOR = 13.31; 95%CI: 1.72, 300.28)), occupation status (others [un employment, housewife, Labor, Student] (AOR = 0.21; 95%CI: 0.08,0. 52), family size (3 up to 5(AOR = 2.81; 95%CI: 1.19, 6.67); greater than 5(AOR = 2.95; 95%CI: 1.13, 7.93)), presence of under 5 children in the households (no (AOR = 0.32; 95%CI: 0.16, 0.61)), presence of elders in the households (No (AOR= 0.33; 95%CI: 0.13, 0.76)), nearest health institution (health centre (AOR = 2.52; 95%CI: 1.21, 5.29)), presence of chronic illness in the household’s (No (AOR = 0.37; 95%CI: 0.15,0. 85)), Time taken to reach health institution (61 up to 120 minutes(AOR = 0.36; 95%CI: 0.16,0.99)); greater than 120 minutes (AOR = 0.29; 95%CI: 0.08, 9.91)), attitude of household towards CBHI scheme (positive attitude (AOR = 2.46; 95%CI: 1.056, 6.22)) significantly determined the CBHI scheme health care service utilization of household’s.
Table 7.
Factors associated with CBHI health service utilization among households in south Gondar zone, Amhara region, Ethiopia.
| Variables | Estimates | COR(95% CI) | AOR(95% CI) | P-value |
|---|---|---|---|---|
| Intercept | 2.29621 | 4.73(3.86, 5.85) | 9.94 (1.91, 57.13) | .008* |
| Gender (ref = Male) | ||||
| Female | 0.44274 | 1.58(1.02, 2.48) | 1.56 (0.80,3.10) | .197 |
| Residence (ref = Rural) | ||||
| Urban | −4.03028 | 0.04(0.02, 0.07) | 0.018 (0.01, 0,05) | <.001* |
| Marital status (ref = Married) | ||||
| Single | −0.10286 | 0.39(0.23, 0.67) | 0.90 (0.34,2.50) | .839 |
| Others (divorced and widowed) | −1.05894 | 0.24(0.13,0.46) | 0.35 (0.02, 0.99) | .048* |
| Education level | ||||
| (ref = Cannot read and write) | ||||
| Can read and write | −0.47273 | 4.7 (1.99, 1.77) | 0.62 (0.31,1.25) | .185 |
| Primary (1-8) | 2.24482 | 4.73 (1.99, 13.97) | 9.44 (2.19, 5.82) | .007* |
| Secondary (9-12) | 3.92052 | 15.98 (3.38,285.89) | 50.43 (3.73, 2142.25) | .018* |
| College and above | 2.58830 | 10.14 (2.11,182.36) | 13.31 (1.72, 300.28) | .035* |
| Occupation status (ref = farmer) | ||||
| Merchant | 0.41709 | 0.75 (0.42, 1.39) | 1.52 (0.59, 4.08) | .395 |
| Others(un employment, housewife, Labor, Student) | −1.55751 | 0.13 (0.07, 0.21) | 0.21 (0.08,0. 52) | .001* |
| Family size (ref ⩽ 3) | ||||
| 3 up to 5 | 1.03434 | 3.71, 2.28, 6.06) | 2.81 (1.19, 6.67) | .018* |
| Greater than 5 | 1.08288 | 6.08 (3.37, 11.39) | 2.95 (1.13, 7.93) | .029* |
| Had under-five children (ref = Yes) | ||||
| No | −1.14947 | 0.31 (0.20, 0.48) | 0.32 (0.16, 0.61) | <.001* |
| Presence of elders (ref = Yes) | ||||
| No | −1.11315 | 0.39 (0.20, 0.70) | 0.33 (0.13, 0.76) | .013* |
| Nearest health institution (ref = health post) | ||||
| Health centre | 0.92460 | 3.58 (2.31,5.58) | 2.52 (1.21, 5.29) | .014* |
| Hospital | −0.01198 | 2.41 (0.95, 7.40) | 0.99 (0.19, 6.31) | .989 |
| Presence of chronic illness (ref = Yes) | ||||
| No | −0.99255 | 0.25 (0.12, 0.47) | 0.37 (0.15, 0. 85) | .025* |
| Distance from health facility in KM | 0.05623 | 1.05 (0.99,1.11) | 1.06 (0.95, 1.19) | .319 |
| Level of awareness about CBHI (ref = Low) | ||||
| Medium | 0.42629 | 2.03 (1.11, 3.66) | 1.53 (0.56, 4.05) | .395 |
| High | 0.26382 | 1.89 (1.05, 3.37) | 1.30 (0.48, 3.37) | .592 |
| Time taken to reach health institution (ref = 1 up to 60 min) | ||||
| 61 up to 120 minutes | −1.03268 | 1.10 (0.63, 2.01) | 0.36 (0.16,0.99) | .049* |
| >120 minutes | −1.23342 | 1.09 (0.62, 1.99) | 0.29 (0.08,9.91) | .049 * |
| Transportation road (ref = available) | ||||
| Not available | 0.50467 | 4.09 (2.61,6.59) | 1.66 (0.88, 3.16) | .121 |
| Satisfaction on perceived quality of care (ref = not-satisfied) | ||||
| Satisfied | 0.27224 | 1.57 (1.03, 2.39) | 1.31 (0.64, 2.68) | .454 |
| Attitude towards CBHI scheme (ref = had negative attitude) | ||||
| Had positive attitude | 0.90027 | 3.56 (2.03,6.68) | 2.46 (1.056, 6.22) | .045* |
Abbreviations: AOR, adjusted odds ratio; COR, crude odds ratio; CI, confidence interval, ref, reference categories of the variable.
Statistically significant variables at 5% level of significance.
Discussions
In this study, we used a sample of 619 respondents, of which 511(82.6%) were use CBHI scheme health care service utilization and the remaining 108 (17.4%) were used OOP health care service utilization. We investigated the significant factors associated with community-based health insurance healthcare service utilization of households in south Gondar zone, Amhara, Ethiopia by considering different variables from the previous literature and dataset, which were collected primarily from the households. Residence, marital status, education level, occupation status, family size, presence of under-five children in the household, presence of elders in the households, nearest health institution, presence of chronic illness in the household’s, time taken to reach health institution, the attitude of household towards CBHI were the determinant factors that affected CBHI scheme health care service utilization of households.
The findings of this study show that households from urban areas were 0.018 times less likely to utilize CBHI health care services than rural resident households holding other covariates in the model constant. This result was supported by other studies,24,25 which showed that urban respondents were willing to pay less as compared with rural respondents. This study was not in line with other previous studies, 26 which shows that rural respondents were willing to pay less as compared with urban respondents. This difference could be due to differences in the socio-economic characteristics of study populations.
Respondents who were divorced and widowed were 0.35 times less likely to utilize CBHI health care services than married respondents. This result was supported by most other studies,21,22,27 which revealed that married household heads were more likely to be CBHI users as compared to households heads with unmarried household heads. This could be explained by the fact that in Ethiopia, the payment policy for household membership contributions does not take married status into account.
The likelihood of CBHI scheme health care service utilization for households who had primary (1-8) education level, households who had secondary (9-12) education level, and households who had college and above education level was 9.44, 50.43, 13.31 times when compared with the household’s who Cannot read and write respectively, when other variables kept constant. This indicates households who had primary (1-8) education level was 9.44 times more likely, households who had secondary (9-12) education level was 50.43 times more likely, and households who had college and above education level was 13.31 times more likely utilized CBHI scheme health care service compared with household’s who cannot read and write respectively. This result was supported by most other studies,7,16,21,22,28 -32 which show education was positively related to the scheme's utilization. As one might think, education has an impact on people's knowledge, attitude, and practice on the importance of CBHI healthcare service utilization.
Respondents who were others (unemployment, housewife, labor or student) were 0.21 times less likely to be CBHI health care service utilizers compared with farmer respondents, by controlling other factors constant. However, in this study, there was no significant CBHI health care service utilization between farmers and merchants. This study was in line with other studies,21,33,34 which shows that farmers were more likely CBHI health care service utilizers when compared to households with other occupations. This might be due to CBHI being designed to protect farmers and informal sectors from unexpected healthcare costs during the harvesting season, which may be suitable for the farmer to pay the premium. Additionally, such findings could be because respondents who have jobs feel economically comfortable and able to pay. But, unemployment, housewife, labor, or student were unable to pay the premium.33,35 This study, in contrast to the previous study, 36 shows that farmers were less likely to enrol in the scheme. This difference may be by the scheme implementation policy and study setting difference.
Households who had 3 up to 5 family members were 2.81 times more likely to be CBHI health care service utilizers as compared with households who had less than 3 family members, by controlling other factors constant. This result was in line with other studies . 29 Households who had greater than 5 family members were 2.95 times more likely to be CBHI health care service utilizer as compared with households that had less than 3 family members while holding other covariates constant. This result was in line with other studies,4,21,32,37,38 which show that family size was positively related to the scheme’s utilization. This study, in contrast to the previous studies,36,39,40 shows that household size had no significant effect on household enrollment in CBHI in the scheme. It may be due to households with a big family size have a higher chance of being ill and are more likely to face financial difficulties. As a result, individuals may have chosen to utilize CBHI health care services to avoid OOP payments when members of the family were sick.
Households without under 5family members were 0.32 times less likely to be CBHI health care service utilizers as compared with households who had under 5 family members while holding other covariates constant. This study was in line with,30,41 the households with under 5 family members were more likely to enrol in the scheme. This study contradicts the previous study, 42 showing the number of children did not affect insurance uptake. This may be due to endemic and transition disease mostly happened on children’s and families with under-five children members were hade high expenditure for medication.
Households that had no elder members were 0.33 times less likely to be CBHI health care service utilizer as compared with households that had elder family members. It was in line with another study, 41 which shows household’s with elder family members were more likely to enrol in the scheme This result contradicted with the study, 22 which shows that the presence of elder household member’s had a negative impact on the CBHI scheme utilization of households.
Households whose nearest health institution is a health centre were 2.52 times more likely to be CBHI health care service utilizer compared to households with health post nearest health institution while holding other covariates constant. This might be due to the low accessibility of the treatment and the quality of public health posts in rural areas when compared to the health facilities in urban areas. In addition, this might be due to the respondents’ expectations about availability and quality service at health centres and hospitals. This study was not in line with, 21 Which shows that nearest health institutions had no significant effect on household enrolment in CBHI.
Households without chronic illness family members were 0.37 times less likely to be CBHI health care service utilizers as compared with households without chronic illness family members while holding other covariates constant. This result was supported by most other studies,19,30,41,43 which show chronic illness membered households were more likely CBHI healthcare service users. This may be due to households with chronic illnesses members being more likely to be admitted to the hospital. Because more hospitalization has financial consequences, they are more likely to seek CBHI healthcare services. This study contradicts the previous study, 44 shows households that have recorded sick members are less willing to pay to enrol in CBHI, and, 21 shows that the presence of chronic illness family members had no significant effect on household’s enrolment in CBHI. The difference might be due to sociodemographic, the time and study setting, the scheme implementation rule, and quality of health care difference.
Households with an estimated 61 up to 120 minutes taken to reach nearest health care institution were 0.36 times less likely CBHI health care service utilizer when compared with less than 61 estimated minutes while holding other covariates constant. Households with an estimated greater than 120 minutes taken to reach nearest health care institution were 0.29 times less likely CBHI health care service utilizer when compared with the reference category, less than 61 estimated minutes while holding other covariates constant. This indicates that households who were nearest to the health care institution were more likely CBHI health care service utilizers compared with households who were far from the health care institution. This study was in line with,4,21 which shows that time to the richest nearest health institution had a significant effect on household’s enrolment in CBHI. This result might be due to the fact that since The long distance between the community and the health centre was a barrier to CBHI enrollment, and the high cost of transportation was a factor to use CBHI healthcare service. 45 This study was contradicted with the previous studies,46,47 which shows households who travel long distances were found to be more willing to pay for CBHI than those that travel less distance. The difference might be due to sociodemographic factors, the time, and study setting, the scheme implementation rule difference in studies
Respondents who had a positive attitude towards the CBHI scheme were 2.46 times more likely CBHI health care service utilizer compared to respondents who had a negative attitude towards the CBHI scheme. This study was in line with other studies, 7 CBHI members who had a positive attitude towards CBHI were twice as likely to comply with CBHI requirements as those members who had a negative attitude. The respondents’ attitude reflects the current difference between the CBHI programme’s implementation and the client's expectations, meaning that clients with a negative attitude were less likely to use the CBHI scheme health care service.
In this study, age, gender, religion and household income were not significantly associated with CBHI healthcare service utilization. However have had a significant association with enrollment in CBHI in previous studies,21,47,48 the reason for this contradiction may be due to socio-demographic and economic background differences of the study populations.
Limitation of the study
This study was conducted in a community setting, which may allow its findings to be generalized to the source population. However, as this is a cross-sectional analysis of data, individuals may have faced recall/social desirability bias since they were asked about past events.
Conclusions
In conclusion, CBHI health care service utilization of households was influenced by socio-demographic, economic, healthcare access related, health perception and healthcare need related factors. The prevalence of CBHI scheme health care service utilization of households was 82.6%. The reasons for non- enrolment for the majority (58.3%) of the OPP user household were the quality of health care services. Residence, marital status, education level, occupation status, family size, presence of under-five children in the household, presence of elders in the households, nearest health institution, presence of chronic illness in the household’s, time taken to reach health institution, the attitude of household towards CBHI were the determinant factors that affect CBHI scheme health care service utilization of households. The research provides solid evidence for CBHI policymakers to improve CBHI policies, and the healthcare quality at the district’s To achieve universal health care coverage through CBHI, special attention should be given to these significant predictors of CBHI. It is recommended that the local, regional, and national governments, policymakers on optimal actions, NGOs, and other supporting organizations shall improve or scale up the scheme by providing awareness to the community based on these significant factors and the attitude of households.
Acknowledgments
We would like to thank all the data collectors, supervisors, study participants, Zonal and wereda, and kebele administrative office for permitting us to collect all the relevant information. We would also like to say thank you to Debre Tabor University for financial support for data collection to this study.
Footnotes
Authors’ Contributions: YA; conceptualized, designed, prepared the original draft, data curation, performed the statistical analysis, interpretation of data, and participated in the supervision. SS SB EY SM and FT; methodology, coordinated the study, acquisition, analysis, interpretation of data and review, and editing edited the manuscript. MW, BM, and HB; supervised the project and reviewed and edited the final manuscript. All authors supervised the findings of this work. All authors read and approved the final manuscript.
Availability of Data and Material: The dataset we used for this study is available at the corresponding author.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Debre Tabor University.
ORCID iDs: Yikeber Abebaw Moyehodie  https://orcid.org/0000-0001-9275-8705
https://orcid.org/0000-0001-9275-8705
Solomon Sisay Mulugeta  https://orcid.org/0000-0002-7263-9634
https://orcid.org/0000-0002-7263-9634
Mitiku Wale Muluneh  https://orcid.org/0000-0002-2413-8026
https://orcid.org/0000-0002-2413-8026
Reference
- 1. Kakama AA, Namyalo PK, Basaza RK. Feasibility and desirability of scaling up community–based health insurance (CBHI) in rural communities in Uganda: lessons from Kisiizi hospital CBHI scheme. BMC health serv res. 2020;20:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Haven N, Dobson AE, Yusuf K, et al. Community-based health insurance increased health care utilization and reduced mortality in children under-5, around Bwindi community hospital, Uganda between 2015 and 2017. Front Public Health. 2018;6:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mirach TH, Demissie GD, Biks GA. Determinants of community-based health insurance implementation in west Gojjam zone, Northwest Ethiopia: a community based cross sectional study design. BMC health Serv Res. 2019;19:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dror DM, Hossain SS, Majumdar A, Pérez Koehlmoos TL, John D, Panda PK. What factors affect voluntary uptake of community-based health insurance schemes in low-and middle-income countries? A systematic review and meta-analysis. PLoS One. 2016;11:e0160479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Allegri M, Kouyaté B, Becher H, et al. Understanding enrolment in community health insurance in sub-Saharan Africa: a population-based case-control study in rural Burkina Faso. Bull World Health Organ. 2006;84:852-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Adebayo EF, Ataguba JE, Uthman OA, Okwundu CI, Lamont KT, Wiysonge CS. Factors that affect the uptake of community-based health insurance in low-income and middle-income countries: a systematic protocol. BMJ open. 2014;4:e004167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Workneh SG, Biks GA, Woreta SA. Community-based health insurance and communities’ scheme requirement compliance in Thehuldere district, northeast Ethiopia: cross-sectional community-based study. Clinico Econs Outcomes res: CEOR. 2017;9:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Uzochukwu B, Ughasoro M, Etiaba E, Okwuosa C, Envuladu E, Onwujekwe O. Health care financing in Nigeria: Implications for achieving universal health coverage. Nigerian journal of clinical practice. 2015;18:437-444. [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization. Global leprosy situation, 2012. Weekly Epidemiological Record = Relevidologique hebdomadaire. 2012;87:317-28. [Google Scholar]
- 10. Ulrika Enemark KaM. Policy Brief Health Insurance in Ghana and Tanzania: increasing access and equity. Aarhus University, Denmark. 2014. [Google Scholar]
- 11. Shimeles A. Community based health insurance schemes in Africa: the case of Rwanda. 2010. [Google Scholar]
- 12. Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Trop med int health. 2005;10:799-811. [DOI] [PubMed] [Google Scholar]
- 13. Ali EE. Health care financing in Ethiopia: implications on access to essential medicines. Value health reg issues. 2014;4:37-40. [DOI] [PubMed] [Google Scholar]
- 14. Molla A, Fentahun N. Predictors of willingness to participate in health insurance services among the community of Jimma town, Southwest Ethiopia. Health Serv Insights. 2014;7:HSI-S18046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. USAID. ‘Ethiopia Health Sector Financing Reform’, the United States Agency for International Development, the Global Health Technical Assistance Project, Addis Ababa. 2011. [Google Scholar]
- 16. Kibret GD, Leshargie CT, Wagnew F, Alebel A. Willingness to join community based health insurance and its determinants in East Gojjam zone, Northwest Ethiopia. BMC res notes. 2019;12(1):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Abdilwohab MG, Abebo ZH, Godana W, Ajema D, Yihune M, Hassen H. Factors affecting enrollment status of households for community based health insurance in a resource-limited peripheral area in Southern Ethiopia. Mixed method. PLoS One. 2021;16:e0245952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. EHIA. Evaluation of Community-Based Health Insurance Pilot Schemes in Ethiopia: Final Report. Addis Ababa, Ethiopia. 2015. [Google Scholar]
- 19. Panda P, Dror I, Koehlmoos T, et al. Factors Affecting Uptake of Voluntary and Community-based Health Insurance Schemes in Low-and Middle-income Countries: A Systematic Review (No. Systematic Review 27). London: International Initiative for Impact Evaluation. 2016. [Google Scholar]
- 20. Feleke S, Mitiku W, Zelelew H, Ashagari T. Ethiopia’s community-based health insurance: a step on the road to universal health coverage. Washington: World Bank Group. 2015. [Google Scholar]
- 21. Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ open. 2018;8:e019613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Panda P, Dror IH, Koehlmoos TP, et al. Factors affecting uptake of voluntary and community-basedhealth insurance schemes in low-and middle-income countries. A systematic review June 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. CSA. 2007 Population and Housing Census of Ethiopia Administrative Report Central Statistical Authority April 2012 Addis Ababa. 2007. [Google Scholar]
- 24. Dong H, Kouyate B, Cairns J, Sauerborn R. Differential willingness of household heads to pay community-based health insurance premia for themselves and other household members. Health Policy Plann. 2004;19:120-126. [DOI] [PubMed] [Google Scholar]
- 25. Dror DM, Radermacher R, Koren R. Willingness to pay for health insurance among rural and poor persons: field evidence from seven micro health insurance units in India. Health policy. 2007;82:12-27. [DOI] [PubMed] [Google Scholar]
- 26. Dong H, De Allegri M, Gnawali D, Souares A, Sauerborn R. Drop-out analysis of community-based health insurance membership at Nouna, Burkina Faso. Health Policy. 2009;92:174-179. [DOI] [PubMed] [Google Scholar]
- 27. Mussa EC, Otchere F, Vinci V, Reshad A, Palermo T, Team IE. Linking poverty-targeted social protection and Community Based Health Insurance in Ethiopia: enrolment, linkages, and gaps. Social Sci Med. 2021;286:114312. [DOI] [PubMed] [Google Scholar]
- 28. Ethiopian Health Insurance Agency. Evaluation of community-based health insurance pilot schemes in Ethiopia. Ethiopian Health Insurance Agency; 2015. [Google Scholar]
- 29. Jembere M. Attitude of rural households towards community based health insurance in Northeast Ethiopia, the Case of Tehuledere District. Prim Health Care. 2018;8:2167-1079. [Google Scholar]
- 30. Nageso D, Tefera K, Gutema K. Enrollment in community based health insurance program and the associated factors among households in Boricha district, Sidama Zone, Southern Ethiopia; a cross-sectional study. PLoS One. 2020;15:e0234028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fite MB, Roba KT, Merga BT, Tefera BN, Beha GA, Gurmessa TT. Factors associated with enrollment for community-based health insurance scheme in Western Ethiopia: case-control study. PLoS One. 2021;16:e0252303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bayked EM, Kahissay MH, Workneh BD. Factors affecting community based health insurance utilization in Ethiopia: a systematic review. 2019. [Google Scholar]
- 33. Negash B, Dessie Y, Gobena T. Community based health insurance utilization and associated factors among informal workers in Gida Ayana District, Oromia Region, West Ethiopia. East Afr J Health Biomed Sci. 2019;3:13-22. [Google Scholar]
- 34. Kebede A, Gebreslassie M, Yitayal M. Willingness to pay for community based health insurance among households in the rural community of Fogera District, North West Ethiopia. Int J Econ Finance Manage Sci. 2014;2:263-269. [Google Scholar]
- 35. Solomon F, Hailu Z, Tesfaye D. Ethiopia’s community-based health insurance: a step on the road to universal health coverage. Health Financ Gov. 2011. [Google Scholar]
- 36. Bodhisane S, Pongpanich S. Factors affecting the willingness to join community-based health insurance (CBHI) scheme: a case study survey from Savannakhet Province, Lao PDR. Int J Health Plann Manage. 2019;34:604-618. [DOI] [PubMed] [Google Scholar]
- 37. Lammers J, Warmerdam S. Adverse selection in voluntary micro health insurance in Nigeria. AIDS Res Ser. 2010;6. [Google Scholar]
- 38. Alkenbrack S, Jacobs B, Lindelow M. Achieving universal health coverage through voluntary insurance: what can we learn from the experience of Lao PDR? BMC Health Serv Res. 2013;13:1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mladovsky P, Soors W, Ndiaye P, Ndiaye A, Criel B. Can social capital help explain enrolment (or lack thereof) in community-based health insurance? results of an exploratory mixed methods study from Senegal. Social Sci Med. 2014;101:18-27. [DOI] [PubMed] [Google Scholar]
- 40. Gnawali DP, Pokhrel S, Sié A, et al. The effect of community-based health insurance on the utilization of modern health care services: evidence from Burkina Faso. Health Policy. 2009;90:214-222. [DOI] [PubMed] [Google Scholar]
- 41. Macha J, Kuwawenaruwa A, Makawia S, Mtei G, Borghi J. Determinants of community health fund membership in Tanzania: a mixed methods analysis. BMC Health Serv Res. 2014;14:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Maina JM, Kithuka P, Tororei S. Perceptions and uptake of health insurance for maternal care in rural Kenya: a cross sectional study. Pan Afr Med J. 2016;23(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mekonen AM, Gebregziabher MG, Teferra AS. The effect of community based health insurance on catastrophic health expenditure in Northeast Ethiopia: a cross sectional study. PLoS One. 2018;13:e0205972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Asgary A, Willis K, Taghvaei AA, Rafeian M. Estimating rural households’ willingness to pay for health insurance. Eur J Health Econ formerly: HEPAC. 2004;5:209-215. [DOI] [PubMed] [Google Scholar]
- 45. Fadlallah R, El-Jardali F, Hemadi N, et al. Barriers and facilitators to implementation, uptake and sustainability of community-based health insurance schemes in low-and middle-income countries: a systematic review. Int J Equity Health. 2018;17:1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ataguba J, Ichoku EH, Fonta W. Estimating the willingness to pay for community healthcare insurance in rural Nigeria. Available at SSRN 1266163. 2008. [Google Scholar]
- 47. Ataguba JE. Community Health Insurance Scheme as a viable option for rural population in Nigeria. Paper submitted to the Centre for the study of African Economies (CSAE), Department of Economics, University of Oxford. 2008. [Google Scholar]
- 48. Adebayo EF, Uthman OA, Wiysonge CS, Stern EA, Lamont KT, Ataguba JE. A systematic review of factors that affect uptake of community-based health insurance in low-income and middle-income countries. BMC Health Serv Res. 2015;15:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]