Abstract
Background
Cardiovascular disease (CVD) brings high mortality and economic burden to patients, especially in rural areas. Simple, low-cost abdominal adiposity measures may help identify individuals with increased CVD risk. It is unclear that which obesity indices is the best to predict CVD in hypertensive people.
Methods
Northeast China Rural Cardiovascular Health Study (NCRCHS) is a prospective cohort study in a general population in Northeast China. The study examined the cardiovascular health from 2013 to 2015, and follow-up captured the CVD incidence in 2018. Baseline waist-to-height ratio (WHtR), waist circumference (WC), waist-to-hip (WHR)and body mass index (BMI) were calculated and analyzed in relation to the CVD incidence.
Results
A total of 4244 hypertensive adults without pre-existing CVD at baseline were included in this analysis (age 35–92 years; 2108 men). Over a median follow-up of 4.66 years, a total of 290 CVD cases (6.83%) were documented during the follow-up. Baseline WHtR showed a significant positive association with CVD incidence, even after adjusting for age, sex, diabetes, drinking, smoking, SBP, DBP, Triglyceride, HDL-C, LDL-C, and TC (Hazard Ratios per SD of WHtR ranging from 1.03 to 1.31, p = 0.017). Reclassification and discrimination analyses indicated WHtR addition could improve the conventional model for predicting adverse outcomes within 4 years. Moreover, WHtR predicted the CVD incidence better than other obesity indices (BMI, WC, WHR).
Conclusion
These findings support a positive association between WHtR and CVD incidence in CVD-free hypertensive adults. WHtR can be used to predict CVD incidence in hypertensive adults.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12872-022-02646-1.
Keywords: Cardiovascular disease, Hypertensive adults, WHtR
Background
Cardiovascular disease (CVD), has becoming a public health challenge strongly linked with the aging global population [1–3]. In China, CVD is the leading cause of death. It accounts for 45.01% of total deaths in rural areas in 2015, while the proportion of urban areas is relatively lower than rural areas. The number of CVD patients is on the rise and predicted to increase substantially over the next 10 years [4].
Obesity, particularly abdominal, is a key risk factor of cardiovascular disease (CVD) [5–7]. Using anthropometric indices to categorize obesity such as waist circumference (WC), the waist-to-height ratio (WHtR), body mass index (BMI), and the waist-to hip ratio (WHR) [8] are the simplest and the most cost-effective methods recommended in clinical practice and epidemiological research, especially in developing countries. Some studies demonstrated that WHtR was better for predicting CVD risk, but it is unclear in the hypertensive adults [9, 10].
Hypertension (HTN) is regarded as a serious public health problem [11–13]. The prevalence of HTN has been increasing all over the world [14–16]. However, it is not known that which anthropometric indices are the best to predict CVD in people with hypertension. Thus, elucidation of the best predictive indicator of cardiovascular disease incidence in hypertension adults is of great significance.
In the present study, we aimed to determine the role of WHtR as a predictor of CVD incidence in the NCRCHS (the Northeast China Rural Cardiovascular Health Study) cohort of hypertensive adults without previous CVD, and compare its discriminating ability against other commonly anthropometric indices of central obesity (i.e., WC, WHR and BMI).
Methods
Study population
Northeast China Rural Cardiovascular Health Study (NCRCHS) is a cohort study in a general population. The methods of the study, including design, personnel recruitment, and laboratory techniques, have been described in previous publications [16, 17]. Between January 2013 and August 2013, 11,956 subjects aged ≥ 35 years were recruited from rural areas of Liaoning province. Subsequently, subjects were invited to attend follow-up visits in 2015 and 2018, and 6017 hypertensive participants were consented and eligible for the follow-up study. A total of 5249 participants of hypertension completed at least one follow-up visit. In the present study, we excluded baseline history of coronary heart disease (n = 355) and stroke (n = 590), and missing data (n = 60). Eventually, data from 4244 participants were available for analysis. The Ethics Committee of the First Hospital of China Medical University (Shenyang, China) approved the study. All participants wrote the informed consent.
Data collection
Data was collected during a single clinic visit by cardiologists and trained nurses using a standard questionnaire by face-to-face interview. During data collection, our inspectors had further instructions and support.
All participants were asked about the current status of smoking, drinking and the history of diseases. All participants were performed according to the BMI levels of China (BMI < 18.5 kg/m2, 18.5 kg/m2 ≤ BMI < 24 kg/m2, 24 kg/m2 ≤ BMI < 30 kg/m2, BMI ≥ 30 kg/m2). WC divided by height is the waist-to-height ratio. We categorized WHtR according to the Ashwell's reports. The reference group was the participants with WHtR between 0.40 and 0.50 [18–20].
According to American Heart Association protocol, blood pressure was measured three times at 2-min intervals after at least 5 min of rest using a standardized automatic electronic sphygmomanometer (HEM-907; Omron). The mean of three blood pressure measures was calculated and used in all analyses. Hypertension was defined as a mean DBP ≥ 90 mmHg, and/or a mean SBP ≥ 140 mmHg, and/or use of the antihypertensive medication in the previous 2 weeks [21, 22]. Diabetes mellitus was defined as FBG ≥ 7.0 mmol/l and/or self-reported physician-confirmed diagnosis [23]. Fasting blood samples were collected after at least 10 h of fasting. Blood samples were taken from an antecubital vein into BD Vacutainer tubes containing ethylenediaminetetraacetic acid. Serum was subsequently isolated from the whole blood, and all serum samples were frozen at − 80 °C for testing at a central, certified laboratory. We used the Olympus AU640 auto-analyzer (Olympus, Kobe, Japan) for analyzing blood biochemical indexes. All blinded duplicate samples were used for these analyses.
Judgment and definition of clinical outcomes
We collected all available clinical information about possible diagnoses or mortality, including data from medical records and death certificates. CVD was defined as stroke or Coronary heart disease (CHD). Stroke were diagnosed by neurologists following the examination of computed tomography and magnetic resonance imaging data in accordance with World Health Organization (WHO) criteria [24]. CHD was defined as a diagnosis of angina requiring hospitalization, myocardial infarction (MI), revascularization procedure and CHD-related mortality [25].
Statistical analysis
Continuous variables were presented as means and SDs and categorical variables were reported as frequencies and percentages in each group. Differences between categories were evaluated using the t test, or the Chi-Square test. Kaplan–Meier method was used to calculate the cumulative incidence for adverse events, and log-rank test was used to compare differences. We used Cox proportional hazards models to estimate the Hazard ratios (HR) and 95% confidence intervals (95% CI) for the association between anthropometric obesity indicators and CVD event. To evaluate the improvement in risk prediction for adverse outcomes by adding WHtR to the conventional model (including age, sex, current smoking, current drinking, SBP, DBP, TC, HDL-C, LDL-C, triglyceride, and diabetes), net reclassification improvement (NRI) and integrated discrimination improvement (IDI) was calculated for CVD prediction models respectively (conventional model vs. conventional model + WHtR). The calculation method is IDI = (Pnew, events-Pold, events)-(Pnew, non-events-Pold, non-events). With the larger value of IDI, the new model has the better prediction ability.
SPSS software version 22.0 was used for statistical analysis and statistical software packages R (http://www.R-project.org, The R Foundation). P < 0.05 was considered to be statistically significant.
Results
Baseline characteristics of the study sample according to CVD incidence
In this study, there are 6017 hypertensive participants consented and eligible for the follow-up study. A total of 5249 participants of hypertension completed at least one follow-up visit. In the current study, we excluded baseline history of coronary heart disease (n = 355) and stroke (n = 590), and missing physical indicators (n = 60). Table 1 presents the baseline characteristics of participants according to the CVD incidence. CVD was defined as stroke or Coronary heart disease (CHD). 4244 participants (2108 men and 2136 women, mean age 56.26 ± 10.15 years) were included in this cohort study (Additional file 1: Figure S1). During a median follow-up of 4.66 years, 290 participants (6.83%) incident stroke or CHD (crude incidence rate, 14.66 incident stroke or CHD per 1000 person-years).
Table 1.
Baseline characteristics of the study sample
| Variable | Without CVD (N = 3954) | With CVD (N = 290) | P value |
|---|---|---|---|
| Age (years) | 55.85 (± 10.10) | 61.85 (± 9.26) | < 0.001 |
| Male [n (%)] | 1945 (50.8%) | 163 (56.2%) | 0.021 |
| Current smoking [n (%)] | 1406 (35.6%) | 118 (40.8%) | 0.090 |
| Current drinking [n (%)] | 1065 (26.9%) | 87 (30.0%) | 0.287 |
| Body Mass Index (kg/m2) | 25.55 (± 3.58) | 25.79 (± 3.54) | 0.268 |
| Waist circumference (cm) | 84.39 (± 9.52) | 85.80 (± 10.49) | 0.016 |
| Waist-to-hip ratio | 0.87 (± 0.07) | 0.89 (± 0.10) | < 0.001 |
| Waist-to-height ratio | 0.53 (± 0.06) | 0.54 (± 0.06) | 0.001 |
| SBP (mmHg) | 157.90 (± 18.18) | 168. 47 (± 23.21) | < 0.001 |
| DBP (mmHg) | 88.69 (± 10.78) | 91.47 (± 14.12) | 0.001 |
| TC (mmol/L) | 5.40 (± 1.09) | 5.55 (± 1.11) | 0.023 |
| LDL-C (mmol/L) | 3.08 (± 0.85) | 3.22 (± 0.91) | 0.017 |
| HDL-C (mmol/L) | 1.45 (± 0.41) | 1.45 (± 0.45) | 0.909 |
| Triglyceride (mmol/L) | 1.76 (± 1.65) | 1.77 (± 1.53) | 0.978 |
| Diabetes [n (%)] | 192 (4.9%) | 19 (6.6%) | 0.253 |
Date are presented as mean ± standard deviation, or n (%), as appropriate
SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; CVD, cardiovascular disease
The group of participants who developed CVD during the study follow-up consisted mainly of older men and exhibited higher anthropometric indices/ratios of total and central obesity (BMI, WC, WHR, WHtR), compared to those who remained CVD-free. Furthermore, this group had higher baseline DBP, SBP levels and lipids (TC and LDL-C) (all p < 0.05; Table 1). The mean WHtR value at baseline was 2% higher in the group of participants who developed a CVD event than in those who remained CVD-free (p < 0.05, Table 1).
Baseline WHtR in relationship to the CVD incidence
The four groups of the Kaplan–Meier survival curves were showed in Fig. 1. The figure showed that the cumulative CVD incidence in the group with WHtR > 0.60 was highest and was much higher than that in the group with 0.4 ≤ WHtR < 0.5. (p for Log-rank test = 0.003, p < 0.05) Sex didn’t have statistically significant interaction in the association between obesity indicators and CVD incidence.
Fig. 1.
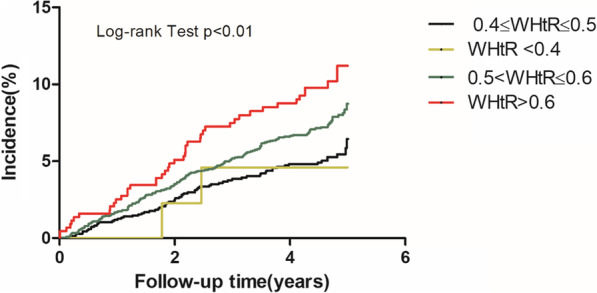
Unadjusted Kaplan–Meier curves for incident adverse events stratified by waist-to-height ratio. WHtR, waist-to-height ratio
Table 2 shows the HRs for CVD according to the value of four abdominal adiposity indices. Univariate HR of CVD for people with WHtR > 0.60 by 1.98-fold (P < 0.001), compared with the group with 0.4 ≤ WHtR < 0.5. After adjustment for sex, age, current drinking, current smoking, TC, HDL-C, LDL-C, triglyceride, diabetes, SBP and DBP, the HR (95% CI) for participants with WHtR 0.60 increased was 1.87 (95% CI 1.23–2.83) for CVD (P = 0.003). Moreover, the participants with 0.50 ≤ WHtR < 0.60 still had a significant difference comparing with the reference group. The multivariate-adjusted HR (95% CI) for 0.50 ≤ WHtR < 0.60 was 1.45 (95% CI: 1.09–1.94) for CVD. However, the other three abdominal adiposity indices didn’t show the such significant results.
Table 2.
Associations between risks of adverse outcomes and different values of waist-to-height ratio, Body Mass Index, waist circumference and waist-to-hip ratio
| All participants | Unadjusted HR (95%CI) | P value | Adjusted HR (95%CI) | P value |
|---|---|---|---|---|
| WHtR | ||||
| WHtR < 0.4 | 0.83 (0.20–3.37) | 0.790 | 0.98 (0.24–3.99) | 0.973 |
| 0.4 ≤ WHtR < 0.5 | 1 | – | 1 | – |
| 0.5 ≤ WHtR < 0.6 | 1.42 (1.08–1.87) | 0.013 | 1.45 (1.09–1.94) | 0.012 |
| WHtR > 0.6 | 1.98 (1.35–2.89) | < 0.001 | 1.87 (1.23–2.83) | 0.003 |
| BMI | ||||
| BMI < 18.5 | 1.42 (0.33–2.40) | 0.496 | 1.03 (0.38–2.82) | 0.954 |
| 18.5 ≤ BMI < 24 | 1 | – | 1 | – |
| 24 ≤ BMI < 30 | 1.07 (0.83–1.38) | 0.601 | 1.12 (0.86–1.47) | 0.399 |
| BMI > 30 | 1.42 (0.96–2.10) | 0.083 | 1.52 (0.99–2.33) | 0.055 |
| WC | ||||
| 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 1.38 (0.98–1.95) | 0.063 | 1.36 (0.96–1.92) | 0.081 |
| 3rd quartile | 1.34 (0.96–1.88) | 0.086 | 1.28 (0.90–1.81) | 0.170 |
| 4th quartile | 1.45 (1.03–2.05) | 0.033 | 1.33 (0.92–1.92) | 0.133 |
| WHR | ||||
| 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 1.58 (1.12–2.23) | 0.009 | 1.47 (1.04–2.08) | 0.031 |
| 3rd quartile | 1.62 (1.13–2.32) | 0.009 | 1.43 (0.99–2.07) | 0.059 |
| 4th quartile | 1.85 (1.31–2.62) | < 0.001 | 1.41 (0.98–2.03) | 0.064 |
Adjusted for age, sex, current smoking, current drinking, TC, HDL-C, LDL-C,triglyceride, diabetes, SBP and DBP
WHtR, waist-to-height ratio; BMI, Body Mass Index; WHR, waist-to-hip ratio; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; CVD, cardiovascular disease
Reclassification and discrimination statistics for adverse outcomes within 4 years by waist-to-height ratio, Body Mass Index, waist circumference and waist-to-hip ratio
Furthermore, we evaluated whether adding WHtR to the conventional model could improve prediction performance. Fortunately, the IDI value and NRI value suggested that the model after addition of WHtR led to a significant improvement in predicting incident stroke or CHD within 4 years (Table 3).
Table 3.
Reclassification and discrimination statistics for adverse outcomes within 4 years by waist-to-height ratio, Body Mass Index, waist circumference and waist-to-hip ratio
| NRI(95% CI) | IDI | P | |
|---|---|---|---|
| WHtR | 0.05 (− 0.01 to 0.12) | 0.0026 | 0.01 |
| BMI | − 0.01 (− 0.05 to 0.03) | 0.0009 | 0.09 |
| WC | − 0.01 (− 0.05 to 0.02) | 0.0007 | 0.14 |
| WHR | − 0.01 (− 0.05 to 0.04) | 0.0013 | 0.04 |
Conventional model: age, sex, current smoking, current drinking, TC, HDL-C, LDL-C, triglyceride, diabetes, SBP and DBP
WHtR, waist-to-height ratio; BMI, Body Mass Index; WHR, waist-to-hip ratio; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol
The result showed that the NRI value of WHtR was 0.05(more than 0 indicating improvement). The IDI value of WHtR was 0.0026 (p = 0.01). Based on these models, WHtR exhibited better predictive value for the CVD incidence as revealed through the IDI value and NRI value (the higher the better), than other common anthropometric indices. Similarly, baseline WHtR was also a better predictor of the CVD than BMI, WHR and WC.
Discussion
WHtR was associated with risk of the CVD in people with hypertension in the prospective cohort study. Notably, this positive association remained significant even after adjusting for various CVD risk factors. Moreover, in the performed comparisons of the predictive value of WHtR on the CVD incidence, WHtR was better than other common anthropometric indices of obesity (BMI, WHR and WC). WHtR exhibited better predictive value for the CVD incidence than the others.
CVD is a public health challenge. The number and mortality of CVD patients is on the rise. The incidence rate of CVD in rural areas was higher than the Chinese average level. Therefore, the results of our study will have important clinical predictive significance. Especially the rural population, their income is generally low, WHtR without cost is the simplest and effective method in clinical practice.
WHtR is a rapid application tool that can help predict CVD risk, and then reduce the CVD incidence. Our results also indicated that addition of WHtR could improve the conventional model for predicting adverse outcomes within 4 years. In addition, our results appear to be stable because the value of WHtR for predicting adverse events remained constant. It is the best indicator of obesity that predicts CVD risk in the population with hypertension.
Recently, there are some studies that reveal the relationship between WHtR and CVD [8, 26, 27]. The study of Gelber pointed that WHtR had the highest association with CVD in male [28]. In addition, the superiority of WHtR in detecting the risk of CVD in children and adolescents has been reported [29]. Other studies demonstrated that WHtR was better for predicting CVD risk [30, 31]. However, the result is from mostly cross-sectional studies, and the study population is not hypertensive.
Our Population in young adults where > P90 over three measures. The strength of current study is that it is a large prospective cohort study. It is the first study to show the association between CVD and WHtR in hypertensive people. Moreover, confounding factors were adequately adjusted and the results were still stable. Nevertheless, our study also has limitations. Cohort sampling loss should be considered a limitation of the study. Our study is a Chinese cohort, which limits the generalizability of our findings to other ethnic groups.
Conclusion
The present study emerges evidence suggesting that WHtR may constitute a simple and accurate prognostic marker of CVD risk as compared to other obesity-related indices in hypertensive people. Indeed, the present findings offer new prospective data suggesting that WHtR exhibits a positive association with the CVD incidence in Asiatic adults from the hypertensive population without pre-existing CVD. WHtR appears to be a much better predictor of CVD risk than the other anthropometric indices of total and central obesity. Future studies are still required to further evaluate the association between WHtR and CVD in different ethnic and patient populations.
Supplementary Information
Additional file 1. Supplemental figure S1. Study flow chart.
Acknowledgements
We would like to thank Professor Liqiang Zheng for his help with data collection and data management.
Abbreviations
- WHtR
Waist-to-height ratio
- BMI
Body Mass Index
- WHR
Waist-to-hip
- WC
Waist circumference
- CVD
Cardiovascular disease
- NCRCHS
Northeast China Rural Cardiovascular Health Study
- TC
Total cholesterol
- CHD
Coronary heart disease
- NRI
Net reclassification improvement
- IDI
Integrated discrimination improvement
Author contributions
ZS participated in wrote the manuscript. DZ conducted statistical analyses. GXF, SYX and SGZ assisted with critical revision of manuscript for intellectual content. LZ, ZY, YHM, YSS coordinated data collection and subjects’ follow-up. FX, ZS and ZXG were responsible for the study concept and design. All authors have read and approved the final manuscript.
Funding
This work was supported by the National Key Research and Development Program of China (Grant #2017YFC1307600), the Science and Technology Program of Liaoning Province, China (Grant #2020JH1/10300002, 2019-ZD-0335) and the Program of Health Commission of Shenyang (201904).
Availability of data and materials
Data are available upon reasonable request. Our data will not be shared because some articles are still being submitted. Corresponding author will be contact for the data.
Declarations
Ethics approval and consent to participate
Our study was approved by the Ethics Committee of China Medical University (Shenyang, China) (2018194). Our study got the written informed consent from all participants. Our protocol was performed in accordance with the relevant guidelines and Helsinki’s declaration.
Consent for publication
Not applicable.
Competing interests
None declared.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shu Zhang and Xin Fu contributed equally to this article and are co-first authors
References
- 1.Clauss SB, de Ferranti SD. Update on preventive cardiology. Pediatr Clin N Am. 2020;67(5):923–944. doi: 10.1016/j.pcl.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Moran AE, Tzong KY, Forouzanfar MH, et al. Variations in ischemic heart disease burden by age, country, and income: the Global Burden of Diseases, Injuries, and Risk Factors 2010 study. Glob Heart. 2014;9(1):91–99. doi: 10.1016/j.gheart.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pekka P, Tiina L, Vesa K, et al. Contribution of the North Karelia Project to international work in CVD and NCD prevention and health promotion. Glob Heart. 2016;11(2):243–246. doi: 10.1016/j.gheart.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Xueli Y, Jianxin L, Dongsheng H, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project. Circulation. 2016;134(19):1430–1440. doi: 10.1161/CIRCULATIONAHA.116.022367. [DOI] [PubMed] [Google Scholar]
- 5.Shilpa NB, Frank BH. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016;118(11):1723–1735. doi: 10.1161/CIRCRESAHA.115.306825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Francisco BO, Carl JL, Steven NB. Obesity and cardiovascular disease. Circ Res. 2016;118(11):1752–1770. doi: 10.1161/CIRCRESAHA.115.306883. [DOI] [PubMed] [Google Scholar]
- 7.Kathryn JM, Ravi S. Introduction to the obesity, metabolic syndrome, and CVD compendium. Circ Res. 2020;126(11):1475–1476. doi: 10.1161/CIRCRESAHA.120.317240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karl Z, Jakob L, Margit H, et al. Body fat distribution and risk of incident ischemic stroke in men and women aged 50 to 74 years from the general population: The KORA Augsburg cohort study. PLoS ONE. 2018;13(2):e0191630. doi: 10.1371/journal.pone.0191630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yukako T, Makoto W, Yoshihiro K, et al. Effect of age on the association between waist-to-height ratio and incidence of cardiovascular disease: the Suita study. J Epidemiol. 2013;23(5):351–359. doi: 10.2188/jea.JE20130004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ran X, Qianwen L, Yaping G, et al. Abdominal obesity and risk of CVD: a dose-response meta-analysis of thirty-one prospective studies. Br J Nutr. 2021;12:1–11. doi: 10.1017/S0007114521000064. [DOI] [PubMed] [Google Scholar]
- 11.Paul AJ, Suzanne O, Barry LC, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults. JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 12.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 13.Calhoun DA, Booth JN, Oparil S, et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63:451–458. doi: 10.1161/HYPERTENSIONAHA.113.02026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alejandro TG, Iván JNG, Hynek R, et al. Harish Ramakrishna Management of arterial hypertension: 2018 ACC/AHA versus ESC guidelines and perioperative implications. J Cardiothorac Vasc Anesth. 2019;33(12):3496–3503. doi: 10.1053/j.jvca.2019.03.068. [DOI] [PubMed] [Google Scholar]
- 15.Liu XH, Bai GN, Li H, Li SP. Applying SF-6D to measure health state utilities among the middle and old aged patients with hypertension in China. Health Qual Life Outcomes. 2020;18(1):385. doi: 10.1186/s12955-020-01598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Z, Guo XF, Zheng LQ, Yang HM, Sun YX. Grim status of hypertension in rural China: results from Northeast China Rural Cardiovascular Health Study 2013. J Am Soc Hypertens. 2015;9:358–364. doi: 10.1016/j.jash.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Sun GZ, Ye N, Chen YT, et al. Early repolarization pattern in the general population: prevalence and associated factors. Int J Cardiol. 2017;230:614–618. doi: 10.1016/j.ijcard.2016.12.045. [DOI] [PubMed] [Google Scholar]
- 18.Ashwell M, Gibson S. Waist-to-height ratio as an indicator of 'early health risk': simpler and more predictive than using a 'matrix' based on BMI and waist circumference. BMJ Open. 2016;6(3):e010159. doi: 10.1136/bmjopen-2015-010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashwell M. Shape: the waist-to-height ratio is a good, simple screening tool for cardiometabolic risk. Nutr Today. 2011;46:85–89. [Google Scholar]
- 20.Xu J, Xu T, Bu XQ, et al. The predictive value of waist-to-height ratio for ischemic stroke in a population-based prospective cohort study among Mongolian men in China. PLoS ONE. 2014;9(10):e110245. doi: 10.1371/journal.pone.0110245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pres-sure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 22.Shea PM, Griffin TP, Fitzgibbon M. Hypertension: the role of biochemistry in the diagnosis and management. Clin Chim Acta. 2017;465:131–143. doi: 10.1016/j.cca.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 23.Jürgen H, Michael R. Diabetes mellitus-definition, classification, diagnosis, screening and prevention (Update 2019) Wien Klin Wochenschr. 2019;131(Suppl 1):6–15. doi: 10.1007/s00508-019-1450-4. [DOI] [PubMed] [Google Scholar]
- 24.Zhao D, Liu J, Wang W, et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONICA-Beijing Project. Stroke. 2008;39:1668–1674. doi: 10.1161/STROKEAHA.107.502807. [DOI] [PubMed] [Google Scholar]
- 25.Gaye B, Canonico M, Perier MC, et al. Ideal cardiovascular health, mortality, and vascular events in elderly subjects: the three-city study. J Am Coll Cardiol. 2017;69:3015–3026. doi: 10.1016/j.jacc.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Radholm K, Chalmers J, Ohkuma T, et al. Use of the waist-to-height ratio to predict cardiovascular risk in patients with diabetes: results from the ADVANCE-ON study. Diabetes Obes Metab. 2018;20:1903–1910. doi: 10.1111/dom.13311. [DOI] [PubMed] [Google Scholar]
- 27.Ioannis K, Demosthenes BP, Georgia MK, et al. Lipid accumulation product in relation to 10-year cardiovascular disease incidence in Caucasian adults: The ATTICA study. Atherosclerosis. 2018;279:10–16. doi: 10.1016/j.atherosclerosis.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 28.Gelber RP, Gaziano JM, Orav EJ, et al. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol. 2008;52:605–615. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mai TMT, Gallegos D, Jones L. The utility of anthopometric indicators to identify cardiovascular risk factors in Vietnamese children. Br J Nutr. 2020;123(9):1043–1055. doi: 10.1017/S0007114520000203. [DOI] [PubMed] [Google Scholar]
- 30.Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–286. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- 31.Yue Z, Yi'an G, Na W. Association between anthropometric indicators of obesity and cardiovascular risk factors among adults in Shanghai, China. BMC Public Health. 2019;19(1):1035. doi: 10.1186/s12889-019-7366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplemental figure S1. Study flow chart.
Data Availability Statement
Data are available upon reasonable request. Our data will not be shared because some articles are still being submitted. Corresponding author will be contact for the data.


