Abstract
Backgrounds
Salivary biomarkers hold huge potential for the non-invasive diagnosis of oral squamous cell carcinoma. Angiogenic factors and matrix-metalloproteinases (MMPs) are highly expressed in OSCC tissue, but their expression patterns in the saliva are unknown. This study aimed to analyze the levels of angiogenic factors and MMPs in tumor tissue and saliva of OSCC patients.
Methods
OSCC-tissue, adjacent normal tissue (ANT), saliva from OSCC patients, and healthy controls were obtained. The expression patterns of angiogenic factors and MMPs were analyzed by immunohistochemistry, protein chip array, and RT-qPCR.
Results
Results showed higher expression of ANG, ANG-2, HGF, PIGF, VEGF, MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1, and TIMP-2 in OSCC-tissues compared to the ANT. Among the overexpressed markers in OSCC-tissues, HGF, VEGF, PIGF, PDGF-BB, MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 were significantly upregulated in the saliva of OSCC patients compared to healthy controls.
Conclusions
The levels of HGF, VEGF, PIGF, MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 were upregulated both in OSCC tissue and saliva of OSCC patients. Bioinformatic analysis revealed the correlation of these factors with patient survival and cancer functional states in head and neck cancer, indicating these factors as possible saliva-based non-invasive diagnostic/prognostic markers and therapeutic targets of OSCC.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-022-09630-0.
Keywords: Angiogenic factors, Diagnostic markers, MMPs, Oral squamous cell carcinoma, Saliva
Introduction
Oral squamous cell carcinoma (OSCC) is the most common oral cancer, accounting for 90% of all oral cancer [1]. Although many advances have been made in cancer treatment, the mortality rate of OSCC has remained unchanged. The 5-year survival rate is around 50% in intermediate patients and less than 20% in advanced patients [2, 3]. Surgery, radiotherapy, and chemotherapy are currently available therapy for OSCCs [4]. Surgical resection is considered to be a promising treatment strategy for early cancer [5]. At present, the diagnosis of OSCC mainly relies on clinical examination, imaging, and histological analysis of suspicious sites, but the lesion location of OSCC often occurs in hidden places [6], making it difficult to diagnose at an early stage.
Induced angiogenesis in OSCC had been reported to promote cancer progression and metastasis [7–10]. Vascular endothelial growth factor (VEGF), angiogenin (ANG), and platelet-derived growth factor (PDGF) signaling are reported as possible therapeutic targets in OSCC [11]. Similarly, angiogenic factors including hepatocyte growth factor (HGF) and placental growth factor (PIGF) had been reported to regulate OSCC invasion [12–14]. Furthermore, matrix metalloproteinases (MMPs) are a family of zinc ion and calcium ion-dependent proteins, which promote tumor progression and metastasis [15]. Therefore, it is essential to investigate the role of angiogenic factors and MMPs in OSCC progression.
Similar to blood, saliva is a complex body fluid known to contain several cellular and molecular components [16]. Saliva contacts directly with the oral mucosa and cancerous lesions thus are practicable for OSCC screening [17]. The altered level of certain molecules in saliva could be linked with oral and systemic diseases [18]. Saliva-based diagnosis is practical, non-invasive, and more accurate than available alternatives [19]. These advantages of saliva-based diagnosis may contribute to the early screening of many oral/systemic diseases and improve clinical management. It has been demonstrated that saliva is a useful diagnostic tool for assessing distant malignancies, including breast cancer [20], lung cancer [21], and Sjögren syndrome [22]. Similarly, salivary immunoglobulins have long been described as biomarkers for HIV infection [19]. Interleukin (IL)-1, IL-6, IL-8, VEGF, s90K/Mac-2 binding protein (M2BP), profilin, myeloid-related protein-14 (MRP14), and catalase have been reported as salivary biomarkers of oral cancer [18, 20–23]. Various angiogenic factors and MMPs are upregulated in OSCC tissue and serum. However, the expression pattern of angiogenic factors and MMPs in the saliva of OSCC patients is not fully understood.
In this study, we aimed to evaluate the expression pattern of various angiogenic factors and MMPs in OSCC tissue and saliva of OSCC patients to unravel the possible non-invasive diagnostic/prognostic markers and therapeutic targets of OSCC.
Materials and Methods
Patients and specimen collection
OSCC and adjacent normal tissues (ANT) of 10 OSCC patients were obtained. The study was approved by the medical ethics committee of Affiliated Stomatology Hospital of Guangzhou Medical University (Approval no. KY2019026). Informed consent was obtained from all subjects (patients and healthy controls). All the experimental protocols involving human samples were in accordance with the guidelines of the Declaration of Helsinki. Patients neither received radiotherapy nor chemotherapy before surgery. ANT sample was obtained from a 2 cm distance from the tumor tissue. Tissue specimens were stained with H&E staining to distinguish cancerous tissue from ANT. Saliva samples were collected from OSCC patients without chemotherapy or radiotherapy. Healthy controls without oral mucosal lesions, pulpitis, gingivitis, or periodontitis were recruited. OSCC patients and healthy controls had no other systemic and autoimmune diseases. Medication was stopped 3 days before the saliva collection. Similarly, smoking and alcohol consumption was prohibited 24 h before saliva collection. Subjects were adjusted to regulatory sleep and required not to eat or drink within 1–2 h after brushing their teeth in the morning. OSCC patients or healthy controls were instructed to spit unstimulated pooled saliva (around 4 ml) in a container. The collected saliva was centrifuged for 2 min at 10,000 rpm to acquire the supernatant. Saliva was collected from 8 OSCC patients and 8 healthy control and stored at -80˚C. And the tumor tissues were collected from 10 OSCC patients including 8 patients for saliva collection. Tissue and saliva were obtained from the same OSCC patients. The clinical characteristics and demographics of patients and healthy controls are shown in Table S1.
Immunohistochemistry (IHC)
OSCC and normal tissues were fixed with 4% paraformaldehyde and embedded in paraffin, 5 µm thick tissue sections were deparaffinized and rehydrated in sequential xylene and gradient ethanol. The tissue sections were immersed in citrate buffer (pH 6.0) and heated for 30 min for antigen retrieval. After incubating with 3% H2O2, the tissue sections were blocked with bovine serum albumin (BSA, Serivicebio, China), followed by overnight incubation with the primary antibodies CD31 (Serivicebio, China, 1:300), CK18 (Abcam, USA, 1:200), MMP2 (Serivicebio, China, 1:1200), MMP3 (Serivicebio, China, 1:800), and MMP13 (Serivicebio, China, 1:200) at 4˚C. Tissue sections were then washed three times with PBS and incubated with goat anti-rabbit IgG (Serivicebio, China, 1:200) with HRP at room temperature. The bound antibody was then observed with diaminobezidin (DAB, Serivicebio, China), and hematoxylin. Substitution of the primary antibody with PBS was used as a negative control. CD31 staining was used to assess microvascular density (MVD) following the method described previously [24]. The micrograph of IHC was taken using PRECICE 500B ScanScope image analyzer (UNIC, China). The immunostained positive area was calculated in the epithelial basal cells, spinous cells, inflammatory cells, and fibroblasts as described previously [25]. IHC Profiler plugin in the ImageJ software was used for calculating the intensity of IHC. And the percentage of positive cells was calculated by ImageJ. The intensity scores were quantified as follows: 0 = negative, 1 = weak, 2 = moderate, 3 = strong. The proportion of immunopositive area was defined as follows: 0 = negative, 1 = < 10%, 2 = 11–50%, 3 = 51–80%, and 4 = ≥ 80% of positive cells. The final immunoreactive score was determined by multiplying the intensity and the proportion scores of the stained cells to obtain an immunoreactive score.
Real-time quantitative PCR (RT-qPCR) analysis
Total RNA was extracted from OSCC tissue and ANT using TRIzol reagent (Invitrogen, USA) according to the manufacturer’s instructions. The cDNA was generated in the T100 gradient PCR machine (Bio-rad, USA) using a PrimeScript RT reagent kit with gDNA Eraser (Takara, Japan). RT-qPCR was performed using TB Green Premix Ex Taq II Kit (Takara, Japan) on an AriaMx Real-time quantitative PCR machine (Agilent, USA). The PCR reaction conditions were 95℃ for 30 s, followed by 40 cycles at 95℃ for 5 s and 60℃ for 30 s. Each reaction was performed in triplicate. The expressions of the angiogenic genes including ANG, bFGF, EGF, HGF, HB-EGF, VEGF, PDGF-BB, Leptin, and MMPs including MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1, TIMP-2, and TIMP-4 were analyzed by RT-qPCR. GAPDH gene was used as the internal control. The fold change relative to the control group was measured by the 2−∆∆Ct method. Primer sequences used in this study are listed in Table S2.
Protein chip array
Tissue and saliva samples from patients were used to measure the expression of ANG, angiopoietin-2 (ANG-2), bFGF, heparin-binding EGF (HB-EGF), HGF, LEP, PDGF-BB, PIGF, and VEGF by the Quantibody® Human Angiogenesis Array 1 (RayBiotech, USA) and MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1, and TIMP-2 by the Quantibody® Human MMP Array 1 (RayBiotech, USA). The detection was performed according to the manufacturer's instructions. Briefly, supernatant from centrifuged tissue samples treated with cell lysate and centrifuged saliva samples were used. The glass slide was completely air dry and blocked by a blocking solution for 1 h. The tissue sample diluent 100 µL (500 µg/mL) and 80 µL of the diluted tissue lysate or saliva samples were separately added to the slides and incubated overnight at 4˚C. The samples diluted were decanted from the wells and washed with wash buffer at room temperature with gentle rocking. The detection antibody cocktail was added to each well and incubated at room temperature, followed by a washing step. Afterward, Cy3 equivalent dye-conjugated streptavidin was added and incubated in a dark room, followed by a washing step. Fluorescence signals were obtained by an InnoScan 300 Microarray Scanner (Innopsys, France) at 532 nm wavelength and 10 µm resolution. Data were analyzed using Mapix (Innopsys, France) analysis software.
Survival analysis
The expression data of head and neck squamous carcinoma for angiogenic-related and MMPS was downloaded from the cancer genome atlas database (TCGA). The patients’ information is shown in Table S3. The survival curve for 260 HNSCC patients with higher expression of angiogenic factors/MMPs and other 259 patients with lower angiogenic factors/MMPs expression was plotted to evaluate the 5-Year survival percentage and duration.
Correlation analysis of angiogenic factors and MMPs expression with the functional states in head and neck squamous cell carcinoma (HNSCC)
Average correlations data between genes of interest and functional states in HNSCC patients were downloaded from CancerSEA (http://biocc.hrbmu.edu.cn/CancerSEA). CancerSEA is a dedicated database that aims to comprehensively decode distinct functional states of cancer cells at the single-cell level. The expression pattern of ANGs and MMPs and their correlation with 14 crucial biological functions in HNSCC, including cancer cell stemness, invasion, metastasis, proliferation, EMT, angiogenesis, apoptosis, cell cycle, cell differentiation, DNA damage, DNA repair, hypoxia, inflammation, and quiescence were analyzed.
Statistical analysis
The results were represented as the mean ± standard deviation (SD). The statistical significance was determined by Student’s t-test at p < 0.05. Cox proportional hazards models were used for the survival analysis by considering ages, sex, tumor sites, alcohol/smoking status, and tumor stages. The graphs were plotted using GraphPad Prism 7.0.
Results
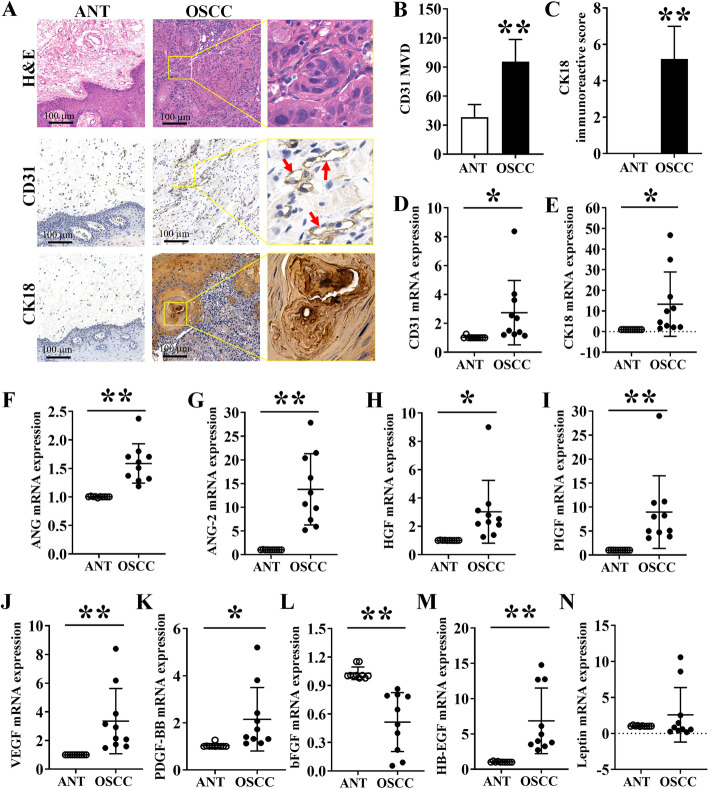
Histology and immunohistochemistry of angiogenic factors in ANT and OSCC tissues
H&E stained ANT histological tissue sections showed normal oral tissue histology. In contrast, H&E stained OSCC tissue sections showed a distinct pattern of well-differentiated OSCC (Fig. 1A). Tissue sections showed few CD31 stained areas in ANT sections, and distinct CD31-stained microvessels in OSCC tissue sections (Fig. 1A). CK18 is a soluble cytokeratin present in proliferating cells with a high expression in the G2-M phase of the cell cycle [26]. Since CK18 is highly expressed in OSCC tissues, we further performed CK18 immunohistochemistry. Brown granular staining in the nucleus of tumor cells was considered positive for CK18. ANT sections were hardly stained with CK18, but OSCC tissue sections showed intense CK18 staining (Fig. 1A). Quantitative analysis of CD31 stained microvessel structure revealed 2.5-fold higher MVD in OSCC tissue compared to ANT (Fig. 1B). Similarly, OSCC tissue showed a 5.06-fold higher expression of CK18 compared to ANT (Fig. 1C). mRNA expression analysis by RT-qPCR also showed upregulation of CD31 and CK18 in OSCC tissue compared to ANT (Fig. 1D and E).
Fig. 1.
Histology and IHC analysis of angiogenic markers in OSCC tissues and ANT. (A) H&E-stained histological as well as CD31 and CK18 IHC images of human OSCC tissue and ANT sections. (B) Quantitative analysis of MVD in the CD31-stained area. (C) CK18 positive area in ANT and OSCC tissue (n = 5). Relative mRNA expression of (D) CD31, (E) CK18, (F) angiogenin, (G) ANG-2, (H) HGF, (I) PIGF, (J), VEGF, (K) PDGF-BB, (L) bFGF, (M) HB-EGF, and (N) leptin in ANT and OSCC tissue. Data are presented as mean ± SD, n = 10. Significant differences compared to the ANT group, *p < 0.05 and **p < 0.01
mRNA expression of angiogenic factors in OSCC tissues and ANT
We further analyzed the mRNA level expression of angiogenic factors in OSCC and ANT tissue by RT-qPCR. The expressions of ANG, ANG-2, HGF, PIGF, VEGF, PDGF-BB, and HB-EGF in the OSCC-group were 1.58-, 13.56-, 3.00-, 8.86-, 3.34-, 2.08-, and 4.63-fold higher, respectively compared to ANT-group (Fig. 1F-Fig. 1K, Fig. 1M). LEP expression in OSCC-group was not significantly affected compared to the ANT group (Fig. 1N). The expression of bFGF was reduced in OSCC-group compared to the ANT group (Fig. 1L).
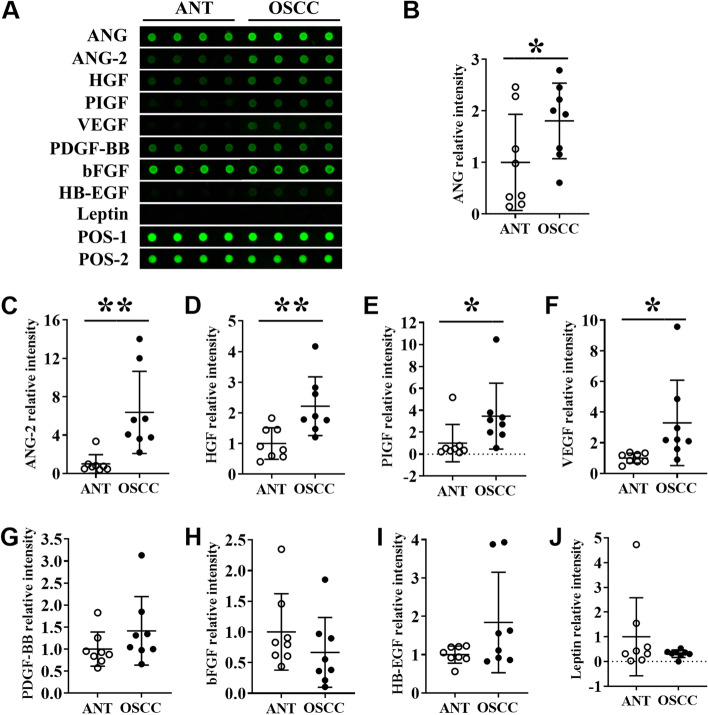
Protein level expression of angiogenic factors in OSCC tissues and ANT
We analyzed the protein level expression of angiogenic factors in OSCC and ANT tissue lysates by protein chip array. Among the angiogenic factors tested, the fluorescence intensities of angiogenin, ANG, ANG-2, HGF, PIGF, and VEGF were prominent in OSCC-group compared to the ANT group (Fig. 2A). Quantitative analysis revealed 1.80-, 6.37-, 2.21-, 3.47-, and 3.30-fold higher expression of ANG, ANG-2, HGF, PIGF, and VEGF in the OSCC-group, respectively compared to ANT-group (Fig. 2B-Fig. 2F). Expressions of PDGF-BB, bFGF, HB-EGF, and leptin were not significantly changed in OSCC tissue compared to ANT (Fig. 2G-Fig. 2J).
Fig. 2.
Angiogenic markers’ protein level expression analysis in OSCC tissues and ANT by protein array. (A) Representative protein array images showing the expression pattern of angiogenesis factors in ANT and OSCC tissue lysates. Quantitative analysis of (B) angiogenin, (C) ANG-2, (D) HGF, (E) PIGF, (F) VEGF, (G) PDGF-BB, (H) bFGF, (I) HB-EGF, and (J) leptin expression from protein array images. Data are presented as mean ± SD, n = 8. Significant differences compared with the ANT group, *p < 0.05 and **p < 0.01
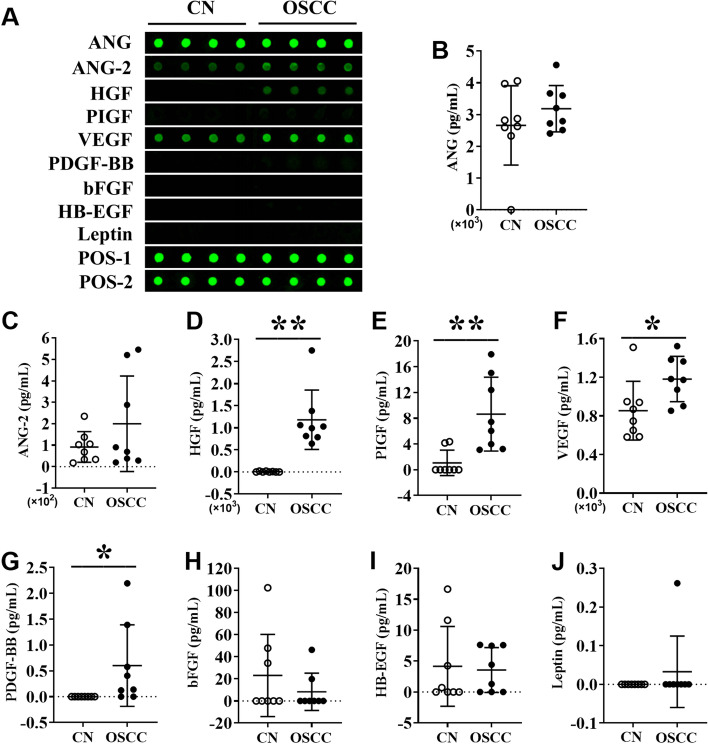
Protein level expression of angiogenic factors in the saliva of OSCC patients and healthy controls
We further analyzed the protein level expression of angiogenic factors in the saliva of OSCC patients and healthy controls. The main aim of this experiment was to further determine the potential application of angiogenic factors as non-invasive diagnostic and prognostic markers in OSCC. Among the angiogenic markers tested, the expressions of HGF, PIGF, and VEGF were 2.00-, 8.10-, and 1.38-fold higher in the saliva of OSCC patients compared to healthy controls (Fig. 3D-Fig. 3F). Interestingly, PDGF-BB was not detected in healthy controls, while 62.5% of OSCC patients showed higher expression of PDGF-BB in saliva (Fig. 3G). Expressions of ANG, ANG-2, bFGF, HB-EGF, and leptin in saliva were not significantly different in OSCC compared to control (Fig. 3A-Fig. 3C, Fig. 3H-Fig. 3J). Expressions of PIGF, PDGF-BB, bFGF, HB-EGF, and leptin in saliva were relatively low to visualize the fluorescence intensity by the naked eye. However, fluorescence signals of these proteins were obtained by an InnoScan 300 Microarray Scanner and quantified.
Fig. 3.
Angiogenic markers’ protein level expression analysis in the saliva of OSCC patients and healthy controls. (A) Representative protein array images showing the expression pattern of angiogenesis factors in the saliva of healthy controls and OSCC patients. Quantitative analysis of (B) angiogenin, (C) ANG-2, (D) HGF, (E) PIGF, (F) VEGF, (G) PDGF-BB, (H) bFGF, (I) HB-EGF, and (J) leptin expression from protein array images. Data are presented as mean ± SD, n = 8. Significant differences compared with the healthy control group, *p < 0.05 and **p < 0.01
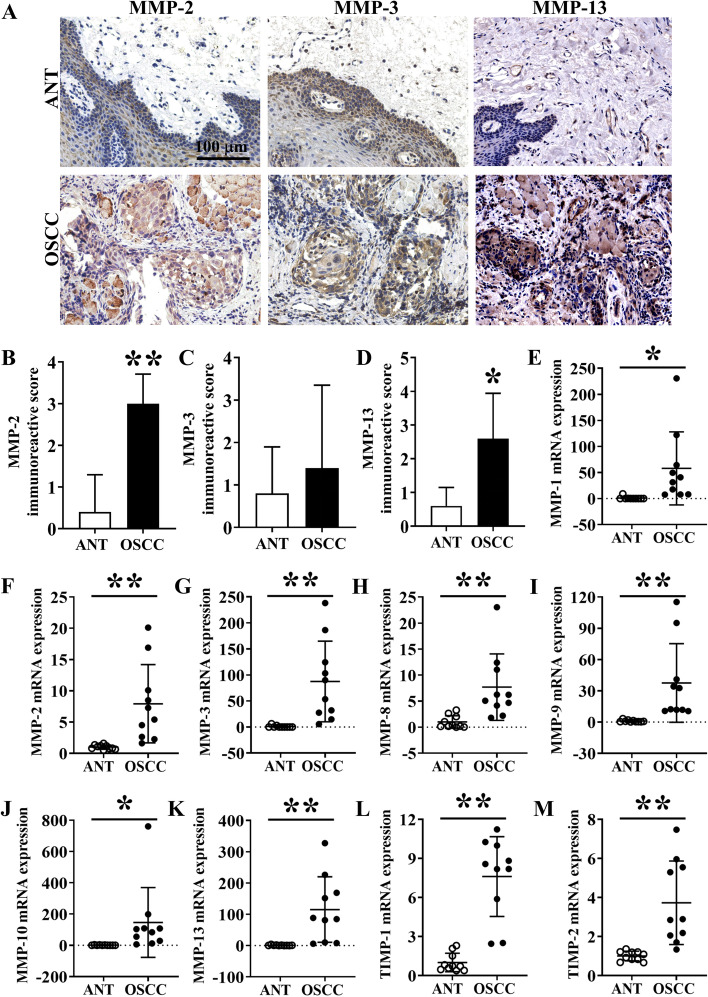
Immunohistochemistry of MMPs in ANT and OSCC tissues
In addition, the expression pattern of MMPs in ANT and OSCC tissues was evaluated. IHC images showed more clear and distinct staining of MMP-2 and MMP-13 in OSCC tissue sections compared to ANT sections (Fig. 4A). There was not much difference in MMP-3 staining in ANT and OSCC groups. The negative control of IHC staining of MMP13 for ANT and OSCC was shown in Fig. S1. According to quantitative analysis data, MMP-2 and -13 showed significant differences between ANT and OSCC, in contrast to MMP-3 which did not reach statistical significance (P = 0.86) (Fig. 4B-Fig. 4D).
Fig. 4.
MMPs expression analysis by IHC in OSCC tissues and ANT. (A) MMP-2, MMP-3, and MMP-13 IHC images of ANT and OSCC tissue sections. Quantification of (B) MMP-2, (C) MMP-3, and (D) MMP-13 positive area in ANT and OSCC tissue sections, n = 5. Relative mRNA expression of (E) MMP-1, (F) MMP-2, (G) MMP-3, (H) MMP-8, (I) MMP-9, (J) MMP-10, (K) MMP-13, (L) TIMP-1, and (M) TIMP-2 in ANT and OSCC tissue, n = 10. Data are presented as mean ± SD. Significant differences compared with the ANT group, *p < 0.05 and **p < 0.01
mRNA expression of MMPs in OSCC tissues and ANT
We further analyzed the mRNA level expression of MMPs in OSCC and ANT tissue by RT-qPCR. The expressions of MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1, and TIMP-2 in OSCC-group were 58.01-, 7.92-, 87.54-, 7.69-, 37.51-, 146.29-, 115.20-, 7.60-, and 3.73-fold higher, respectively compared to ANT-group (Fig. 4E-Fig. 4M).
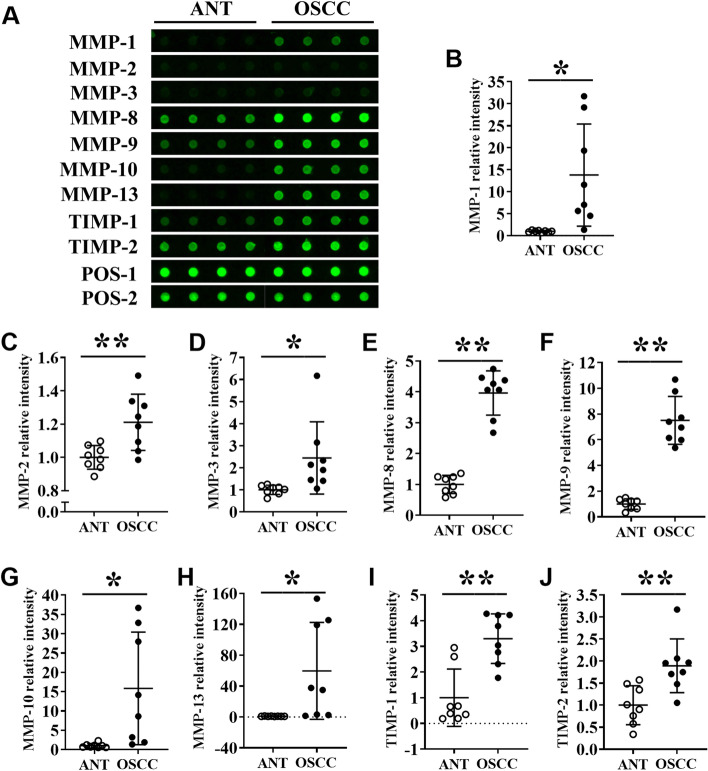
Protein level expression of MMPs in OSCC tissues and ANT
To determine the protein levels of MMPs in tissues, we performed a semi-quantitative protein chip array. The results showed that the fluorescence intensities of MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1, and TIMP-2 in the OSCC group were significantly increased compared with the ANT-group (Fig. 5A). The mean fluorescence intensities of MMP-1, MMP-2, MMP3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1 and TIMP-2 in OSCC tissue were 13.80-, 1.21-, 2.44-, 3.96-, 7.50-, 15.83-, 59.75-, 3.29-, and 1.89-fold higher than ANT-group, respectively (Fig. 5B-Fig. 5J). The result of protein level expression of MMPs was in accordance with the results of RT-qPCR (Fig. 4).
Fig. 5.
MMPs protein level expression analysis in OSCC tissues and ANT by protein array. (A) Representative protein array images showing the expression pattern of MMPs in ANT and OSCC tissue lysates. Quantitative analysis of (B) MMP-1, (C) MMP-2, (D) MMP-3, (E) MMP-8, (F) MMP-9, (G) MMP-10, (H) MMP-13, (I) TIMP-1, and (J) TIMP-2 expression from protein array images. Data are presented as mean ± SD, n = 8. Significant differences compared with the ANT group, *p < 0.05 and **p < 0.01
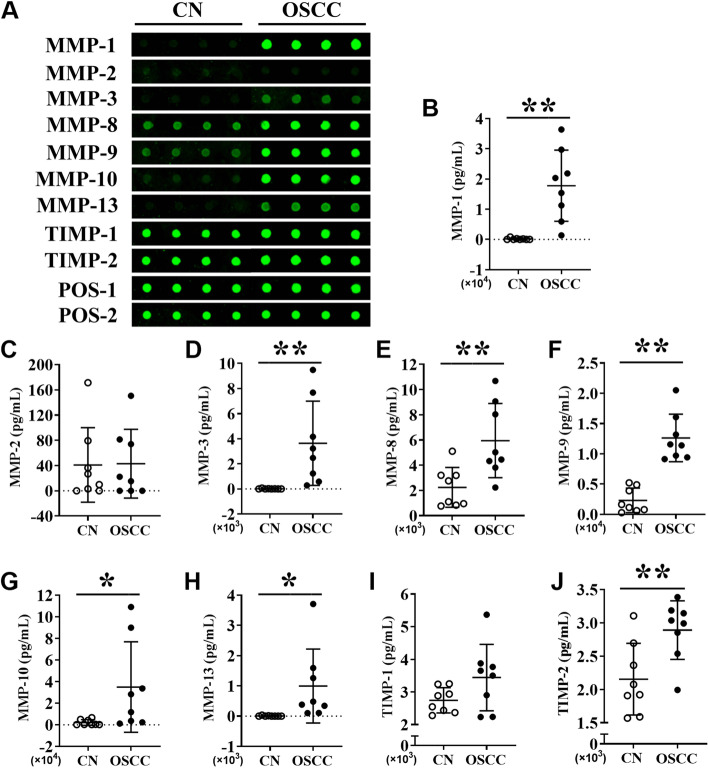
Protein level expression of MMPs in the saliva of OSCC patients and healthy controls
The protein level expression of MMPs in the saliva of OSCC patients and healthy controls was further analyzed. It demonstrated that the expression levels of MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, and MMP-13 in saliva were relatively high to visualize the green fluorescence (Fig. 6A). Quantification analysis revealed that the levels of MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 were upregulated by 111.71-, 256.32-, 2.66-, 5.48-, 16.31-, 174.20-, and 1.34-fold in the saliva of OSCC patients, respectively, compared to healthy controls (Fig. 6B, Fig. 6D-Fig. 6H and Fig. 6J). Expressions of MMP2 and TIMP-1 in saliva were not significantly different in OSCC compared to control (Fig. 6C, Fig. 6I). Intriguingly, MMP-1, MMP-3, and MMP-13 were highly expressed in the saliva of the OSCC group, but their expressions were too low to be detected in healthy individuals.
Fig. 6.
MMPs protein level expression analysis in the saliva of OSCC patients and healthy controls. (A) Representative protein array images showing the expression pattern of MMPs in the saliva of healthy controls and OSCC patients. Quantitative analysis of (B) MMP-1, (C) MMP-2, (D) MMP-3, (E) MMP-8, (F) MMP-9, (G) MMP-10, (H) MMP-13, (I) TIMP-1, and (J) TIMP-2 expression from protein array images. Data are presented as mean ± SD, n = 8. Significant differences compared with the healthy control group, *p < 0.05 and **p < 0.01
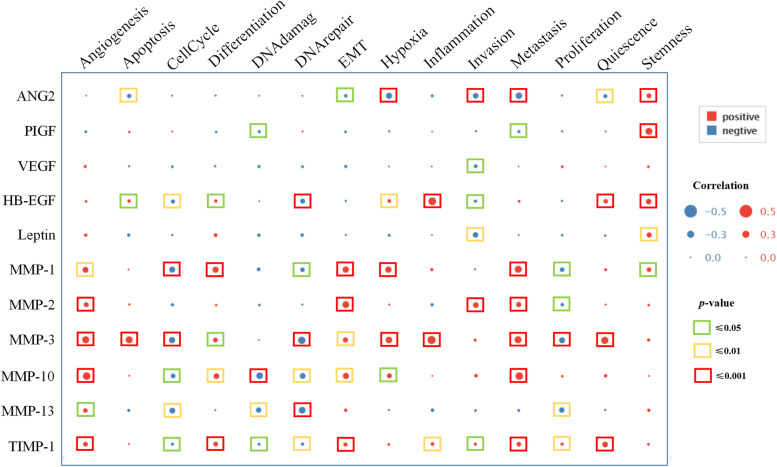
The correlation between angiogenic factors and MMPs expression with the functional states in HNSCC
Figure 7 depicts the correlation between the expression patterns of ANGs and MMPs expression with the functional states in HNSCC at the single-cell level. ANG2 and PIGF expression positively correlated with cancer cell stemness. HB-EGF expression positively correlated with inflammation, cancer cell quiescence, and stemness. The expression of leptin positively correlated with cancer cell stemness. MMPs expression was positively correlated with angiogenesis, EMT, and metastasis. Intriguingly, HB-EGF, MMP-1, MMP-3, MMP-10, MMP-13, and TIMP-1 showed a negative correlation with cell cycle and DNA repair. While, the expressions of MMP-10, MMP-13, and TIMP-1 were negatively correlated with DNA damage. And the higher expression of ANG-2 was negatively correlated with invasion, metastasis, and hypoxia.
Fig. 7.
Correlation analysis of ANGs and MMPs expressions with HNSCC tumor cell functions by CancerSEA. Functional states mainly include angiogenesis, apoptosis, cell cycle, differentiation, DNA damage, DNA repair, EMT, hypoxia, inflammation, invasion, metastasis, proliferation, quiescence, and stemness. EMT: endothelial mesenchymal transition
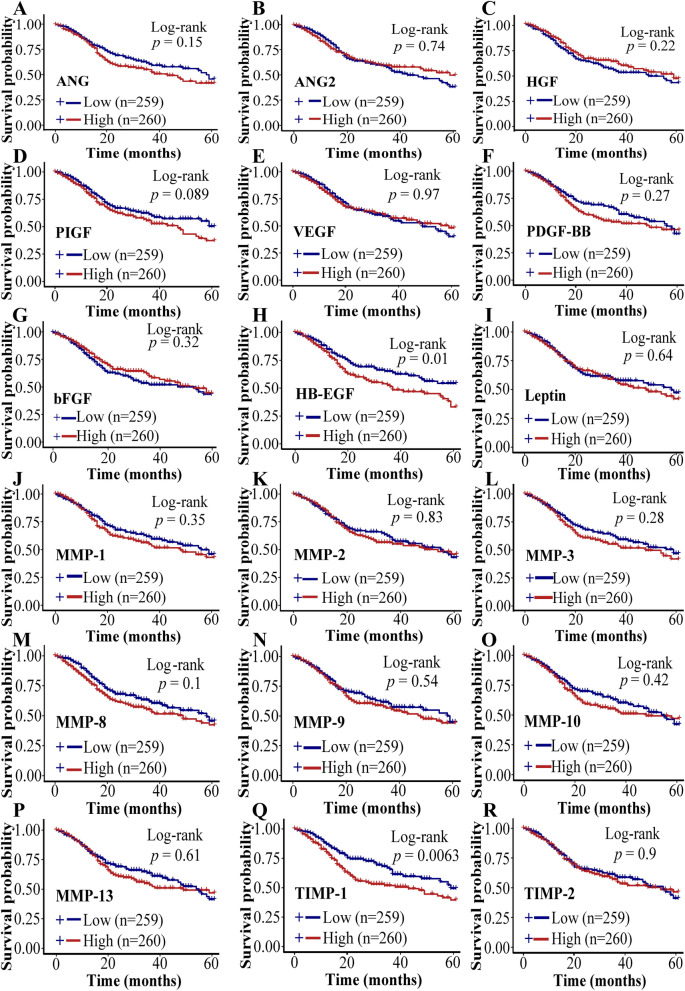
Survival analysis
We further analyzed the survival curve from 260 HNSCC patients (50%) with higher expressions of ANGs and MMPs and 249 patients (50%) with lower expressions of ANGs and MMPs. HNSCC patients with lower expressions of HB-EGF (p = 0.01), TIMP-1 (p = 0.0063) showed a significantly higher 5 years survival rate compared to those HNSCC patients with higher expressions of these factors (Fig. 8 D, Fig. 8Q). Similarly, HNSCC patients with lower expressions of ANG (p = 0.15), Leptin (p = 0.64), PIGF (p = 0.089), MMP- MMP-1 (p = 0.35), MMP-3 (p = 0.28), MMP-8 (p = 0.1), and MMP-9 (p = 0.54) showed higher 5 years survival rate compared to those HNSCC patients with higher expressions of these factors but there was no significant difference between lower and higher expression groups (Fig. 8A, Fig. 8F, Fig. 8H, Fig. 8J, Fig. 8L-Fig. 8N). HNSCC patients with higher expression of ANG-2 (p = 0.74), bFGF (p = 0.32), HGF (p = 0.22), VEGF (p = 0.97), PDGF-BB (p = 0.27), MMP-2 (p = 0.83), MMP-10 (p = 0.42), MMP-13 (p = 0.61), and TIMP-2 (p = 0.9) showed higher 5 years survival rate compared to those HNSCC patients with higher expressions of these factors but there was no significant difference between lower and higher expression groups (Fig. 8B, Fig. 8C, Fig. 8E, Fig. 8G, Fig. 8I, Fig. 8K, Fig. 8O, Fig. 8P, Fig. 8R).
Fig. 8.
Correlation analysis of ANGs and MMPs expressions with HNSCC patient survival. Correlation of (A) ANG, (B) ANG-2, (C) HGF, (D) PIGF, (E) VEGF, (F) PDGF-BB, (G) bFGF, (H) HB-EGF, (I) Leptin, (J) MMP-1, (K) MMP-2, (L) MMP-3, (M) MMP-8, (N) MMP-9, (O) MMP-10, (P) MMP-13, (Q) TIMP-1, or (R) TIMP-2 expression pattern with HNSC patient survival rate and duration (248 OSCC patients). *p < 0.05 and **p < 0.01
Discussion
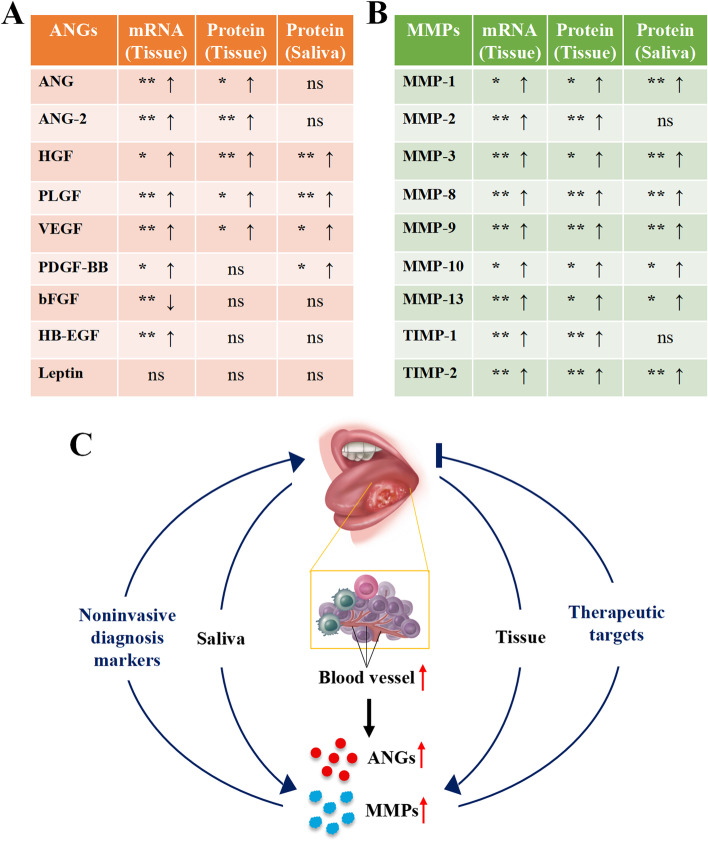
Identification of novel biomarkers for OSCC diagnosis/prognosis helps early diagnosis and treatment and decreases patient morbidity and mortality. Considering the importance of angiogenesis and MMPs in OSCC development and metastasis, it is wise to explore the expression patterns of angiogenic factors and MMPs. Results of this study found a direct correlation between angiogenesis with OSCC development. This study found higher expression of HGF, VEGF, PIGF, PDGF-BB, MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 both in OSCC tissue and saliva of OSCC patients based on the protein chip-array. IHC and protein chip array of some of the factors did not give the same results. Our findings indicate these factors have the potential as saliva-based non-invasive possible diagnostic/prognostic markers and therapeutic targets of OSCC (Fig. 9).
Fig. 9.
Scheme showing ANGs and MMPs expression based on protein chip array and their possible application in OSCC diagnosis and treatment. (A) ANGs and MMPs in the OSCC may serve as non-invasive diagnostic markers and therapeutic targets. (B) The expression of ANGs in tissues and saliva. (C) The expression of MMPs in tissues and saliva. *p < 0.05 and **p < 0.01
Histological analysis is the gold standard for OSCC diagnosis. No tumor progression in ANT-tissue was verified by histological analysis. CD31, an endothelial marker, is highly expressed in various cancer tissues, including OSCC [27, 28]. In this study, CD31 is highly expressed in the connective tissue of OSCC samples compared to ANT. The higher degree of angiogenesis promotes not only OSCC progression but also cancer invasion [29]. CK18, a cytokeratin protein, is highly expressed in proliferating cancer cells, including OSCC [30]. We found higher MVD in OSCC tissue compared to ANT. Similarly, the expression pattern of CK18 was in accordance with the higher CD31 expression and angiogenesis in OSCC. These findings indicate the key role of angiogenesis in OSCC progression.
ANG, ANG-2, HGF, PIGF, PDGF-BB, HB-EGF, VEGF, bFGF, and leptin are key growth factors that regulate angiogenesis in pathophysiological conditions [31]. In this study, we evaluated the expression of all these angiogenic growth factors in OSCC tissue and saliva of OSCC patients. The mRNA levels of ANG, ANG-2, HGF, PIGF, PDGF-BB, HB-EGF, and VEGF were upregulated in OSCC tissues compared to paired-ANT. Furthermore, the protein levels of ANG, ANG-2, HGF, PIGF, and VEGF were significantly increased in OSCC tissues. Saliva possesses tremendous potential in disease diagnosis due to its critical advantages, including minimum cost, non-invasiveness, and easy collection [32]. HGF, PIGF, and VEGF had been reported as therapeutic targets in OSCC [12–14, 33]. HGF regulates gastric cancer progression and metastasis [34]. In various cancers, PIGF is involved in tumor immune escape and metastasis [35]. Polz-Dacewicz and colleagues had reported the higher expression of VEGF in serum and saliva of oropharyngeal squamous cell carcinoma patients [36]. PDGF-BB is overexpressed in OSCC tissues and correlates with tumorigenesis and poor prognosis of OSCC [37]. In this study, HGF, PIGF, VEGF, and PDGF-BB were found to be significantly upregulated in OSCC tissue as well as in the saliva of the patients. Future research on the role of HGF, PIGF, VEGF, and PDGF-BB in OSCC progression, and metastasis could be useful to unravel these factors as novel diagnostic and therapeutic markers. This is the first study to show the higher expression of HGF, PIGF, and PDGF-BB in the saliva of OSCC patients. Our findings indicate that the angiogenic markers HGF, PIGF, VEGF, and PDGF-BB could be saliva-based novel diagnostic markers of OSCC.
MMPs participate in tumor progression, and metastasis, thereby hold diagnostic and therapeutic applications potential [38, 39]. MMP-1/protease-activated receptor-1 (PAR1) signaling axis plays an essential role in tumor angiogenesis by inducing vascular permeability [40]. Serum and salivary MMP1, MMP2, MMP-9, MMP-10, MMP-12, and MMP13 had been reported to upregulate in OSCC [41–44]. Moreover, MMP-9 triggers the angiogenic switch by releasing VEGF during tumorigenesis [45]. We found that the mRNA and protein levels of MMP-1, MMP-2, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, TIMP-1, and TIMP-2 were significantly increased in OSCC tissue compared to paired-ANT. Furthermore, the levels of MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 were significantly upregulated in the saliva of OSCC patients compared to the healthy ones. Accordingly, the expressions of MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 were upregulated both in OSCC tissue and in the saliva of OSCC patients. MMP-1, MMP-2, MMP-3, MMP-9, MMP-13, TIMP-1, and TIMP-2 had been reported to overexpress in HNSCC tissue compared with normal tissue. Thus, our data is consistent with previous reports [25, 46]. This is the first study to report the overexpression of salivary MMP-3, MMP-8, and TIMP-2 in OSCC suggesting these markers as saliva-based potential novel diagnostic/prognostic markers as well as therapeutic targets of OSCC. The HGF and MMP-9 content in saliva are quite different between healthy control and OSCC patients. In the present study, the highest HGF concentration in the control group saliva was 20.079 pg/mL, while the lowest in the OSCC group was 641.457 pg/mL. Similarly, the highest concentration for MMP9 in the control group was 5224.613 pg/mL, while the lowest in the OSCC group was 9135.693 pg/mL. More normal and tumor saliva samples should be collected and set the positive or negative cut-off value of HGF and MMP9.
In this study, we re-confirmed higher angiogenesis in human OSCC tissue. We analyzed the expression pattern of a panel of angiogenic factors and MMPs in OSCC tissue and saliva of OSCC patients. RT-qPCR, immunohistochemistry, and protein chip array analysis were used to extensively analyze the expression of the aforementioned markers in mRNA and protein levels in OSCC tissue and saliva. This study revealed the overexpression of HGF, PIGF, PDGF-BB, MMP-3, MMP-8, and TIMP-2 both in serum and saliva of OSCC patients for the first time. Moreover, the survival analysis of HNSCC showed a direct correlation between the higher expression of the HB-EGF and TIMP-1 expression with the lower survival rate of the patients. Moreover, the expression patterns of TIMP-1 in HNSCC positively correlated with angiogenesis, EMT, and metastasis. While HB-EGF was positively related to cancer inflammation and stemness. Although these are the results from HNSCC patients, the similarity between HNSCC and OSCC provides a hint about the functions of ANGs and MMPs in OSCC. The survival analysis and cancer cell functional states correlation with ANGs/MMPs expression are needed to confirm the exact roles of ANGs and MMPs in OSCC development and progression.
The overexpression of VEGF, MMP-1, MMP-2, MMP-3, MMP-9, MMP-10, and MMP-13 in OSCC tissue and saliva corroborates the findings of the previous studies [25, 41–46]. Sample inclusion from a small number of OSCC patients is a limitation of this study. A multicenter study with higher patient numbers is recommended to further validate the findings of this study. Since the higher levels of salivary HGF, PIGF, PDGF-BB, MMP-3, MMP-8, and TIMP-2 are first time reported, their role as diagnostic and prognostic markers, and therapeutic targets for OSCC should be thoroughly investigated.
Conclusions
In conclusion, this study showed overexpression of angiogenic factors HGF, PIGF, and VEGF in OSCC tissues and saliva of OSCC patients. Similarly, among the MMPs tested, the MMP-1, MMP-3, MMP-8, MMP-9, MMP-10, MMP-13, and TIMP-2 were significantly overexpressed in OSCC tissues and saliva of OSCC patients. Our results suggest these overexpressed angiogenic markers and MMPs, especially for HGF and MMP9 as possible saliva-based non-invasive diagnostic, prognostic, and therapeutic biomarkers of OSCC.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- OSCC
Oral squamous cell carcinoma
- VEGF
Vascular endothelial growth factor
- ANG
Angiogenin
- PDGF
Platelet-derived growth factor
- HGF
Hepatocyte growth factor
- PIGF
Placental growth factor
- MMPs
Matrix metalloproteinases
- M2BP
Mac-2 binding protein
- MRP14
Myeloid-related protein-14
- ANT
Adjacent normal tissues
- MVD
Microvascular density
- HNSCC
Head and neck squamous cell carcinoma
Authors’ contributions
LW, JLP, and GJ designed the project, interpreted the data, drafted the work, and substantively revised the work. MC, ZZ, ZB, KOY, QW, SX, LH, YJ, and LJW acquired and analyzed the data. All authors read and approved the final manuscript.
Funding
This research was funded by National Natural Science Foundation of China (31801152), University Student Laboratory Open Project of Guangzhou Medical University (2020–27), and Innovation and Entrepreneurship Training program for College Students of Guangzhou Medical University (2019A049).
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in figshare repository (https://figshare.com/articles/dataset/Raw_data_for_Overexpression_of_angiogenic_factors_and_matrix_metalloproteinases_in_the_saliva_of_oral_squamous_cell_carcinoma_patients_potential_non-invasive_diagnostic_and_therapeutic_biomarkers/19602397).
Declarations
Ethics and approval and consent to participate
The study was approved by the medical ethics committee of Affiliated Stomatology Hospital of Guangzhou Medical University (Approval no. KY2019026). Informed consent was obtained from all subjects (patients and healthy controls). And all the experimental protocols involving human samples were in accordance with the guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meijuan Cai, Zhichao Zheng and Zhibao Bai contributed equally to this work and share first authorship.
Contributor Information
Jie Gao, Email: 48014713@qq.com.
Janak L. Pathak, Email: j.pathak@gzhmu.edu.cn
Lihong Wu, Email: wcanhong@163.com.
References
- 1.Chen TW, Lee C-C, Liu H, Wu C-S, Pickering CR, Huang P-J, Wang J. Chang IY-F, Yeh Y-M, Chen C-D: APOBEC3A is an oral cancer prognostic biomarker in Taiwanese carriers of an APOBEC deletion polymorphism. Nat Commun. 2017;8(1):465. doi: 10.1038/s41467-017-00493-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bloebaum M, Poort L, Böckmann R, Kessler P. Survival after curative surgical treatment for primary oral squamous cell carcinoma. Journal of Cranio-Maxillo-Facical Surgery. 2014;42(8):1572–1576. doi: 10.1016/j.jcms.2014.01.046. [DOI] [PubMed] [Google Scholar]
- 3.Hasegawa H, Kusumi Y, Asakawa T, Maeda M, Oinuma T, Furusaka T, Oshima T, Esumi M. Expression of von Hippel-Lindau tumor suppressor protein (pVHL) characteristic of tongue cancer and proliferative lesions in tongue epithelium. BMC Cancer. 2017;17(1):381. doi: 10.1186/s12885-017-3364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reis PP, Waldron L, Perez-Ordonez B, Pintilie M, Galloni NN, Xuan Y, Cervigne N, Warner GC, Makitie AA, Simpson C. A gene signature in histologically normal surgical margins is predictive of oral carcinoma recurrence. BMC Cancer. 2011;11(1):437. doi: 10.1186/1471-2407-11-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150(1):9–16. doi: 10.1001/jamasurg.2014.2895. [DOI] [PubMed] [Google Scholar]
- 6.Mehrotra R, Yadav S. Oral squamous cell carcinoma: etiology, pathogenesis and prognostic value of genomic alterations. Indian J Cancer. 2006;43(2):60–66. doi: 10.4103/0019-509x.25886. [DOI] [PubMed] [Google Scholar]
- 7.Kalra M, Rao N, Nanda K, Rehman F, Girish KL, Tippu S, Arora A. The role of mast cells on angiogenesis in oral squamous cell carcinoma. Medicina Oral Patologia Oral Y Cirugia Bucal. 2012;17(2):E190–E196. doi: 10.4317/medoral.17395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kabiraj A, Jaiswal R, Singh A, Gupta J, Singh A, Samadi FM. Immunohistochemical evaluation of tumor angiogenesis and the role of mast cells in oral squamous cell carcinoma. J Cancer Res Ther. 2018;14(3):495–502. doi: 10.4103/0973-1482.163693. [DOI] [PubMed] [Google Scholar]
- 9.Yoshida S, Kawai H, Eguchi T, Sukegawa S, Oo MW, Anqi C, Takabatake K, Nakano K, Okamoto K, Nagatsuka H. Tumor Angiogenic Inhibition Triggered Necrosis (TAITN) in Oral Cancer. Cells. 2019;8(7):E761. doi: 10.3390/cells8070761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cui Z, Liu QL, Sun SQ, Jiao K, Liu DR, Zhou XC, Huang L. MiR-378a-5p inhibits angiogenesis of oral squamous cell carcinoma by targeting KLK4. Neoplasma. 2020;67(1):85–92. doi: 10.4149/neo_2019_190306N191. [DOI] [PubMed] [Google Scholar]
- 11.Chen L, Hu GF. Angiogenin-mediated ribosomal RNA transcription as a molecular target for treatment of head and neck squamous cell carcinoma. Oral Oncol. 2010;46(9):648–653. doi: 10.1016/j.oraloncology.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hanzawa M, Shindoh M, Higashino F, Yasuda M, Inoue N, Hida K, Ono M, Kohgo T, Nakamura M, Notani K, et al. Hepatocyte growth factor upregulates E1AF that induces oral squamous cell carcinoma cell invasion by activating matrix metalloproteinase genes. Carcinogenesis. 2000;21(6):1079–1085. [PubMed] [Google Scholar]
- 13.Bu J, Bu X, Liu B, Chen F, Chen P. Inhibition of metastasis of oral squamous cell carcinoma by anti-PLGF treatment. Tumour Biol. 2015;36(4):2695–2701. doi: 10.1007/s13277-014-2892-y. [DOI] [PubMed] [Google Scholar]
- 14.Xuan K, Li B, Guo H, Sun W, Kou XX, He XN, Zhang YJ, Sun J, Liu AQ, et al. Deciduous autologous tooth stem cells regenerate dental pulp after implantation into injured teeth. Sci Transl Med. 2018;10(455):eaaf3227. doi: 10.1126/scitranslmed.aaf3227. [DOI] [PubMed] [Google Scholar]
- 15.Coussens LM, Fingleton B, Matrisian LM. Matrix metalloproteinase inhibitors and cancer: trials and tribulations. Science. 2002;295(5564):2387–2392. doi: 10.1126/science.1067100. [DOI] [PubMed] [Google Scholar]
- 16.Rehak NN, Cecco SA, Csako G. Biochemical composition and electrolyte balance of "unstimulated" whole human saliva. Clinical Chemistry Laboratory Medicine. 2000;38(4):335–343. doi: 10.1515/CCLM.2000.049. [DOI] [PubMed] [Google Scholar]
- 17.Yakob M, Fuentes L, Wang MB, Abemayor E, Wong DTW. Salivary biomarkers for detection of oral squamous cell carcinoma - current state and recent advances Current Oral. Health Rep. 2014;1(2):133–141. doi: 10.1007/s40496-014-0014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korostoff A, Reder L, Masood R, Sinha UK. The role of salivary cytokine biomarkers in tongue cancer invasion and mortality. Oral Oncol. 2011;47(4):282–287. doi: 10.1016/j.oraloncology.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Bonne NJ, Wong DTW. Salivary biomarker development using genomic, proteomic and metabolomic approaches. Genome Medicine. 2012;4(10):82. doi: 10.1186/gm383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bigler LR, Streckfus CF, Copeland L, Burns R, Dai X, Kuhn M, Martin P, Bigler SA. The potential use of saliva to detect recurrence of disease in women with breast carcinoma. J Oral Pathol Med. 2002;31(7):421–431. doi: 10.1034/j.1600-0714.2002.00123.x. [DOI] [PubMed] [Google Scholar]
- 21.Zhang L, Xiao H, Zhou H, Santiago S, Lee JM, Garon EB, Yang J, Brinkmann O, Yan X, Akin D. Development of transcriptomic biomarker signature in human saliva to detect lung cancer. Cell Mol Life Sci. 2012;69(19):3341–3350. doi: 10.1007/s00018-012-1027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu S, Gao K, Pollard R, Arellano-Garcia M, Zhou H, Zhang L, Elashoff D, Kallenberg CG, Vissink A, Wong DT. Preclinical validation of salivary biomarkers for primary Sjögren's syndrome. Arthritis Care Res. 2010;62(11):1633–1638. doi: 10.1002/acr.20289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu S, Arellano M, Boontheung P, Wang J, Zhou H, Jiang J, Elashoff D, Wei R, Loo JA, Wong DT. Salivary proteomics for oral cancer biomarker discovery. Clin Cancer Res. 2008;14(19):6246–6252. doi: 10.1158/1078-0432.CCR-07-5037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weidner N, Semple JP, Welch WR, Folkman J. Tumor angiogenesis and metastasis–correlation in invasive breast carcinoma. N Engl J Med. 1991;324(1):1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 25.Vincent-Chong VK, Salahshourifar I, Karen-Ng LP, Siow MY, Kallarakkal TG, Ramanathan A, Yang YH, Khor GH, Rahman ZA, Ismail SM, et al. Overexpression of MMP13 is associated with clinical outcomes and poor prognosis in oral squamous cell carcinoma. ScientificWorldJournal. 2014;2014:897523. doi: 10.1155/2014/897523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chou CF, Riopel CL, Rott LS, Omary MB. A significant soluble keratin fraction in ‘simple’ epithelial cells. Lack of an apparent phosphorylation and glycosylation role in keratin solubility. J Cell Sci. 1993;105(2):433–444. doi: 10.1242/jcs.105.2.433. [DOI] [PubMed] [Google Scholar]
- 27.Muller AM, Hermanns MI, Skrzynski C, Nesslinger M, Muller KM, Kirkpatrick CJ. Expression of the endothelial markers PECAM-1, vWf, and CD34 in vivo and in vitro. Exp Mol Pathol. 2002;72(3):221–229. doi: 10.1006/exmp.2002.2424. [DOI] [PubMed] [Google Scholar]
- 28.Iamaroon A, Pongsiriwet S, Jittidecharaks S, Pattanaporn K, Prapayasatok S, Wanachantararak S. Increase of mast cells and tumor angiogenesis in oral squamous cell carcinoma. J Oral Pathol Med. 2003;32(4):195–199. doi: 10.1034/j.1600-0714.2003.00128.x. [DOI] [PubMed] [Google Scholar]
- 29.Sappayatosok K, Maneerat Y, Swasdison S, Viriyavejakul P, Dhanuthai K, Zwang J, Chaisri U. Expression of pro-inflammatory protein, iNOS, VEGF and COX-2 in oral squamous cell carcinoma (OSCC), relationship with angiogenesis and their clinico-pathological correlation. Medicina Oral Patologia Oral Y Cirugia Bucal. 2009;14(7):E319–E324. [PubMed] [Google Scholar]
- 30.Nanda KD, Ranganathan K, Devi U, Joshua E. Increased expression of CK8 and CK18 in leukoplakia, oral submucous fibrosis, and oral squamous cell carcinoma: an immunohistochemistry study. Oral Surgery Oral Medicine Oral Pathology Oral Radiology. 2012;113(2):245–253. doi: 10.1016/j.tripleo.2011.05.034. [DOI] [PubMed] [Google Scholar]
- 31.Esposito E, Aldrees S, Mastromonaco C, Zoroquiain P, Vila N, Logan PT, Hari S, Burnier MN. Evaluation of nicotinamide as an anti-inflammatory and anti-angiogenic agent in uveal melanoma cell lines. Arq Bras Oftalmol. 2017;80(2):74–77. doi: 10.5935/0004-2749.20170019. [DOI] [PubMed] [Google Scholar]
- 32.Rapado-Gonzalez O, Martinez-Reglero C, Salgado-Barreira A, Takkouche B, Lopez-Lopez R, Suarez-Cunqueiro MM, Muinelo-Romay L. Salivary biomarkers for cancer diagnosis: a meta-analysis. Ann Med. 2020;14:1–20. doi: 10.1080/07853890.2020.1730431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ferrara N. VEGF as a therapeutic target in cancer. Oncology. 2005;69(3):11–16. doi: 10.1159/000088479. [DOI] [PubMed] [Google Scholar]
- 34.Ding XS, Ji J, Jiang JL, Cai Q, Wang C, Shi M, Yu YY, Zhu ZG, Zhang J. HGF-mediated crosstalk between cancer-associated fibroblasts and MET-unamplified gastric cancer cells activates coordinated tumorigenesis and metastasis. Cell Death Dis. 2018;9(9):867. [DOI] [PMC free article] [PubMed]
- 35.Albonici L, Giganti MG, Modesti A, Manzari V, Bei R. Multifaceted Role of the Placental Growth Factor (PlGF) in the Antitumor Immune Response and Cancer Progression. Int J Mol Sci. 2019;20(12):2970. [DOI] [PMC free article] [PubMed]
- 36.Polz-Dacewicz M, Strycharz-Dudziak M, Dworzanski J, Stec A, Kocot J. Salivary and serum IL-10, TNF-alpha, TGF-beta, VEGF levels in oropharyngeal squamous cell carcinoma and correlation with HPV and EBV infections. Infect Agent Cancer. 2016;11:45. doi: 10.1186/s13027-016-0093-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin LH, Lin JS, Yang CC, Cheng HW, Chang KW, Liu CJ. Overexpression of Platelet-Derived Growth Factor and Its Receptor Are Correlated with Oral Tumorigenesis and Poor Prognosis in Oral Squamous Cell Carcinoma. Int J Mol Sci. 2020;21(7):2360. [DOI] [PMC free article] [PubMed]
- 38.Malemud CJ. Matrix metalloproteinases (MMPs) in health and disease: an overview. Front Biosci. 2006;11:1696–1701. doi: 10.2741/1915. [DOI] [PubMed] [Google Scholar]
- 39.Gonzalez-Avila G, Sommer B, Mendoza-Posada DA, Ramos C, Garcia-Hernandez AA, Falfan-Valencia R. Matrix metalloproteinases participation in the metastatic process and their diagnostic and therapeutic applications in cancer. Crit Rev Oncol Hematol. 2019;137:57–83. doi: 10.1016/j.critrevonc.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 40.Juncker-Jensen A, Deryugina EI, Rimann I, Zajac E, Kupriyanova TA, Engelholm LH, Quigley JP. Tumor MMP-1 activates endothelial PAR1 to facilitate vascular intravasation and metastatic dissemination. Cancer Res. 2013;73(14):4196–4211. doi: 10.1158/0008-5472.CAN-12-4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Feng Y, Li Q, Chen J, Yi P, Xu X, Fan Y, Cui B, Yu Y, Li X, Du Y, et al. Salivary protease spectrum biomarkers of oral cancer. Int J Oral Sci. 2019;11(1):7. doi: 10.1038/s41368-018-0032-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peisker A, Raschke GF, Fahmy MD, Guentsch A, Roshanghias K, Hennings J, Schultze-Mosgau S. Salivary MMP-9 in the detection of oral squamous cell carcinoma. Med Oral Patol Oral Cir Bucal. 2017;22(3):e270–275. doi: 10.4317/medoral.21626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hema Shree K, Ramani P, Sherlin H, Sukumaran G, Jeyaraj G, Don KR, Santhanam A, Ramasubramanian A, Sundar R. Saliva as a Diagnostic Tool in Oral Squamous Cell Carcinoma - a Systematic Review with Meta Analysis. Pathol Oncol Res. 2019;25(2):447–453. doi: 10.1007/s12253-019-00588-2. [DOI] [PubMed] [Google Scholar]
- 44.Nosratzehi T, Alijani E, Moodi M. Salivary MMP-1, MMP-2, MMP-3 and MMP-13 Levels in Patients with Oral Lichen Planus and Squamous Cell Carcinoma. Asian Pac J Cancer Prev. 2017;18(7):1947–1951. doi: 10.22034/APJCP.2017.18.7.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bergers G, Brekken R, McMahon G, Vu TH, Itoh T, Tamaki K, Tanzawa K, Thorpe P, Itohara S, Werb Z, et al. Matrix metalloproteinase-9 triggers the angiogenic switch during carcinogenesis. Nat Cell Biol. 2000;2(10):737–744. doi: 10.1038/35036374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oc P. Rhys-Evans PH, Eccles SA: Expression of matrix metalloproteinases and their inhibitors correlates with invasion and metastasis in squamous cell carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg. 2001;127(7):813–820. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in figshare repository (https://figshare.com/articles/dataset/Raw_data_for_Overexpression_of_angiogenic_factors_and_matrix_metalloproteinases_in_the_saliva_of_oral_squamous_cell_carcinoma_patients_potential_non-invasive_diagnostic_and_therapeutic_biomarkers/19602397).