Abstract
Despite the prevalence of suicide risk in inflammatory bowel disease populations, research has yet to examine associations between childhood trauma, resilience, depression and suicide risk. In the present online study, 172 participants responded to measures of childhood trauma, resilience, depression and suicide risk. A moderated mediation revealed that resilience does not moderate the associations between childhood trauma, depressive symptoms and suicide risk. However, a serial mediation revealed that childhood trauma is associated with decreased resilience, which is related to higher depressive symptoms, and ultimately higher suicide risk, thus suggesting resilience and depression as significant intervention targets.
Keywords: depression, suicide, resilience, inflammatory bowel disease, childhood trauma
Inflammatory bowel disease (IBD) is a chronic disease with relapsing and remitting courses of inflammation of the gastrointestinal tract. Crohn’s disease and ulcerative colitis are subtypes of IBD, differentiated primarily by the location of inflammation (Targownik and Bernstein, 2017). IBD is inflammation of the gastrointestinal tract, where Crohn’s disease may affect anywhere from mouth to anus, and ulcerative colitis manifests primarily in the colon (Wehkamp et al., 2016). Primary IBD symptoms include abdominal pain, frequent/urgent bowel movements, blood in the stool, weight loss and fatigue (Sans and Figueroa, 2008). The chronicity of IBD, the early age of onset, and the increasing incidence in North America have significant impact on North American health (Crohn’s and Colitis Foundation of Canada, 2012).
IBD is associated with lower quality of life and higher rates of depression compared to the general population (Knowles et al., 2018; Mikocka-Walus et al., 2015). Depression, in turn, is associated with more severe IBD course, higher rates of pain, and lower quality of life (Malik, 2015). Excessive inflammation may play a role in the development of both depression and a more severe IBD course, with depressive symptoms further exacerbating gastrointestinal symptoms (Capuco et al., 2020; Moulton et al., 2019). Despite this, depression among IBD patients often remains undiagnosed or undertreated (Keefer and Kane, 2017). This is concerning as depression is a major risk factor for suicidal behaviours (Angst et al., 1999), including suicidal ideation (i.e., thoughts and plans for suicide), nonfatal suicide attempts and death by suicide. Suicidal behaviours are prevalent among adults with depression (Angst et al., 1999; Schwartz-Lifshitz et al., 2012), chronic disease (Ferro et al., 2017; Zhang et al., 2018) and chronic pain (Racine, 2018). Likewise, IBD lifetime rates of suicidal ideation have exceeded 30% (Fuller-Thomson and Sulman, 2006), patients have historically reported greater suicide risk than the general population (Gradus et al., 2010), and recent point prevalence estimates of suicide risk are over 40% (Mihajlovic et al., 2020).
Childhood trauma is also a risk factor for suicidal behaviour (de Mattos Souza et al., 2016; Tunnard et al., 2014). Childhood trauma—experiencing or witnessing an event that is frightening, dangerous, or violent—has long been associated with the development of depressive symptoms (Hammen et al., 2000) and IBD (Drossman et al., 1995). Specifically, certain types of trauma including sexual and physical abuse are associated with the development of ulcerative colitis (Fuller-Thomson et al., 2015). Although childhood trauma and depression have been associated with IBD incidence, higher patient resiliency can moderate and/or mediate the relationship between trauma and depressive symptoms (Ding et al., 2017; Meng et al., 2018). Indeed, patients with IBD and higher resiliency report fewer depressive symptoms (Sirois and Hirsch, 2017). Despite the various associations between childhood trauma, depression, resiliency and suicide risk, a single model of these associations remains unexamined in an IBD sample. Thus, the primary aim here was to document the associations between childhood trauma, depression, resilience and self-reported suicide risk. Understanding these associations in individuals with IBD can provide clinicians a new care-map aimed at identifying and perhaps intervening with those at-risk.
The first objective examined resilience as a moderator on the associations between childhood trauma, depressive symptoms and suicide risk; hypothesising that the association between childhood trauma and suicide risk would be mediated by depressive symptoms, and that the associations between childhood trauma and depressive symptoms, and depressive symptoms and suicide risk, would be moderated by resilience. Here, greater resilience relates to lower levels of depressive symptoms and suicide risk. The second objective examined the mediating effects of resilience and depressive symptoms through a causal chain, hypothesising that resilience and depressive symptoms would serially mediate the relationship between childhood trauma and suicide risk, with resilience preceding depressive symptoms in the model, as in previous research (Ding et al., 2017). Greater childhood trauma was expected to be associated with lower resilience, which in turn was expected to be related to greater levels of depressive symptoms, which were ultimately expected to be associated with greater risk of suicide. The serial mediation model would indicate both a direct and indirect pathway on which childhood trauma may affect suicide risk.
Method
Participants
All participants were aged at least 18 years, able to read and write in English, and diagnosed with IBD. Participants were excluded if they had a diagnosis for a major psychiatric disorder (e.g., psychosis) or a medical condition (e.g., severe cardiac, pulmonary, renal or hepatic disease) that may have interfered with study participation. The final sample size was 172 (Mage = 40.50, range = 19–79) which reflects the median sample size in psychological research (Kline, 2015) and is likely sufficient for conditional process analyses, which do not have generalized guidelines for sample size requirements. Demographic information for the study sample can be found in Table 1.
Table 1.
Demographic information for study sample.
| n (%) | |
|---|---|
| Ethnicity | |
| Caucasian | 163 (94.8) |
| Hispanic/Latino | 1 (0.6) |
| Aboriginal | 1 (0.6) |
| Asian | 3 (1.7) |
| Black/African-Canadian | 1 (0.6) |
| Other | 3 (1.7) |
| Education | |
| Less than high school | 4 (2.3) |
| High school/GED | 34 (19.8) |
| Some college/university | 31 (18) |
| Graduate from college/university | 67 (39) |
| Some graduate/professional school | 8 (4.7) |
| Graduate from graduate/professional school | 28 (16.3) |
| Employment status | |
| Employed | 113 (65.7) |
| Unemployed | 16 (9.3) |
| Retired | 10 (5.8) |
| Disabled | 16 (9.3) |
| Student | 16 (9.3) |
| Missing data | 1 (0.6) |
| Sex | |
| Female | 132 (76.7) |
| Male | 40 (23.3) |
| Living with spouse | |
| Yes | 115 (66.9) |
| No | 57 (33.1) |
| Disease type | |
| Crohn’s disease | 96 (55.8) |
| Ulcerative colitis | 59 (34.3) |
| Both | 17 (9.9) |
| Place of residence | |
| North America | 94 (54.6) |
| Oceania | 28 (16.3) |
| Europe | 50 (29) |
| Types of childhood traumatic experiences | |
| Death of a close friend or family member | 101 (58.7) |
| Major upheaval between parents | 73 (42.4) |
| Traumatic sexual experience | 43 (25) |
| Victim of violence | 41 (23.8) |
| Extreme illness or injury | 52 (30.2) |
| Other | 71 (41.3) |
Study measures
Demographics
Demographic questions included participants’ date of birth, gender, ethnicity, country of residence, education, relationship status, employment status and IBD diagnosis.
Resilience
The Brief Resilience Scale (BRS; Smith et al., 2008) is a reliable, 6-item, self-report measure (current α = 0.84) assessing resilience in terms of ability to bounce back from stressful events. The BRS score ranging from 1 to 5 was calculated by dividing the total sum by the total number of items answered. Each of the six items can be scored from 1 (strongly disagree) to 5 (strongly agree) with higher scores indicating higher levels of resilience.
Depressive symptoms
The Patient Health Questionnaire Nine (PHQ-9; Kroenke et al., 2001) is a valid measure with good reliability (α = 0.89) and has similar reliability in other IBD samples (Bernstein et al., 2018). The PHQ-9 assesses the presence of nine depressive symptoms based on DSM-IV criteria for depression. The PHQ-9 score can range from 0 to 27, with the 9 items scored from 0 (not at all) to 3 (nearly every day) with higher scores indicating higher levels of depressive symptoms.
Childhood trauma
The Childhood Trauma Questionnaire (CTES; Pennebaker and Susman, 1988) is a brief self-report measure of six childhood traumatic experiences (death, divorce, violence, sexual abuse, illness, or other), as well as one’s understanding of the trauma (i.e., their perception of the traumatic event and its personal significance; Pennebaker & Susman, 1988). Participants rated trauma for each event experienced on a scale from 1 (not at all traumatized) to 7 (extremely traumatic). The CTES total score sums responses, ranging from 1 to 42 where higher scores indicate greater trauma.
Suicide risk
The Suicidal Behaviors Questionnaire Revised (SBQ-R; Osman et al., 2001) is a reliable self-report measure (current α = 0.80) assessing four elements of suicidal behaviour (i.e., item 1 assessed lifetime suicidal ideation and attempts [scored 0–4], item 2 assessed frequency of suicidal ideation in the past year [scored 1–5], item 3 examined threat of suicidal behaviour [scored 0–3], and item 4 assessed likelihood of suicidal behaviour in the future [scored 0–6]). A total score is calculated by summing the four items, with higher scores indicating greater suicide risk; total scores range from 3 to 18.
Procedure
Data for the present study were drawn from a larger study documenting a high prevalence rate of suicide risk and its biopsychosocial predictors in individuals with IBD (Mihajlovic et al., 2020). Participants were recruited online through patient support groups and social media (e.g., Facebook) using recruitment scripts and advertisements. The survey was administered through the online platform Qualtrics, which is Queen’s University’s selected enterprise survey software. Participants accessed the survey through an anonymous link that was included on online postings. They were then directed to a page where they read a Letter of Information and Consent Form and were prompted to check a box as indication of consent. Following consent, the survey was provided to the participant. Participants were able to refrain from answering any question of their choosing. Upon completion of the survey, a debriefing form was provided along with resources for coping with any potential distress. Ethics clearance was provided by Queen’s University Health Sciences Research Board.
Statistical analysis
Preliminary analyses
One-way ANOVAs examined whether suicide risk differed significantly by country, type of IBD diagnosis (i.e., Crohn’s disease, ulcerative colitis, both), age, or gender to determine whether the data could be analysed as a homogenous sample.
Objective 1: Depression as a mediator, resilience as a moderator
A moderated mediation examined the moderating effects of resilience on the associations between childhood trauma, depressive symptoms and suicide risk. Specifically, childhood trauma was the independent variable, depressive symptoms the mediator, resilience the moderator and suicide risk the dependent variable. The moderated mediation was tested with Models 7, 14 and 58 of Hayes’ (2013) PROCESS macro in SPSS Statistics Version 24.
Objective 2: Resilience and depression as mediators
A serial mediation examined the mediating effects of resilience and depressive symptoms on the relationship between childhood traumatic experiences and suicide risk. Childhood trauma was the independent variable, resilience the first mediator, depressive symptoms the second mediator and suicide risk the dependent variable. The serial mediation was tested with Model 6 of Hayes’ (2013) PROCESS macro in SPSS Statistics Version 24.
Data sharing statement
The de-identified data set containing all variables used in the analyses, syntax file and log files will be available on the Figshare respository.
Results
Preliminary analyses
One-way ANOVAs indicated that there were no significant differences across countries, F(8, 163) = 1.49, p = 0.165; type of IBD diagnosis, F(2, 169) = 0.453, p = 0.636; age, F(50, 119) = 0.864, p = 0.717; or gender, F(1, 170) = 0.545, p = 0.461, for suicide risk. Thus, the data were analysed as a homogenous sample.
Objective 1: Depression as a mediator, resilience as a moderator
Model 7 of the PROCESS macro was used to examine whether resilience moderated the relationship between childhood trauma and depressive symptoms. Model 7 of the PROCESS macro revealed that resilience did not moderate the path between childhood trauma and depressive symptoms as the 95% confidence interval of the index of moderated mediation straddled zero, 95% CI [−0.042, 0.030], in the simple mediation model of childhood trauma (predictor), depressive symptoms (mediator) and suicide risk (outcome). Similar to results of Model 7, Model 14 of the PROCESS macro revealed that resilience did not moderate the path between depressive symptoms and suicide risk, 95% CI [−0.019, 0.027].
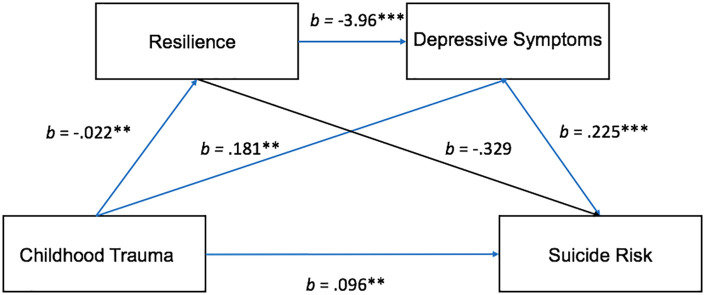
Then, Model 58 examined whether resilience moderated both pathways of the indirect effect of childhood trauma on suicide risk (Figure 1). The direct effect of childhood traumatic experiences on suicide was significant, b = 0.096, SE = 0.030, p = 0.002. As no inferential test is available through the PROCESS macro to test moderated mediation for Model 58, the indirect effect was examined at three resilience scores (one standard deviation below the mean, the mean and one standard deviation above the mean) to determine if the indirect effect changed substantially across the three scores. The indirect effect through depression was significant both at the resilience score one standard deviation below the mean (2.13) and at the mean resilience score (2.93), with both 95% confidence intervals entirely above zero, CI [0.006, 0.085] and CI [0.014, 0.068], respectively. The indirect effect was not significant when the resilience score was one standard deviation above the mean (3.73) as the 95% confidence interval straddled zero, CI [−0.002, 0.079]. The confidence intervals observed for Model 58 were also similar to those observed in Models 7 and 14 for the same resilience scores (i.e., one standard deviation below the mean, the mean and one standard deviation above the mean). The similarity of the confidence intervals in Model 58 combined with the pattern of results for Models 7 and 14 suggests that resilience did not moderate the indirect effect of childhood trauma on suicide risk through depressive symptoms.
Figure 1.
Moderated mediation model tested by Model 58 of the PROCESS macro with blue lines representing significant pathways.
**p < 0.01.
Objective 2: Resilience and depression as mediators
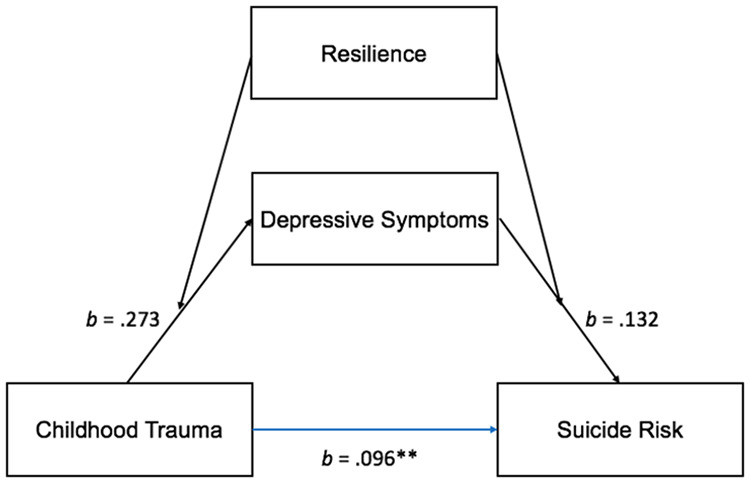
Model 6 of the PROCESS macro examined whether resilience and depressive symptoms causally mediate the relationship between childhood traumatic experiences and suicide risk (Figure 2). The total effect of childhood traumatic experiences on suicide was significant, b = 0.164, SE = 0.033, p < 0.001, as was the direct effect, b = 0.096, SE = 0.030, p = 0.002, of childhood traumatic experiences on suicide risk. The overall indirect effect childhood trauma on suicide risk through resilience and depression was significant, b = 0.020, SE = 0.008, 95% CI [0.006, 0.037]; childhood trauma was associated with lower resilience, which was related to higher depressive symptoms, which ultimately were associated with higher suicide risk. The indirect effect of childhood trauma on suicide risk through resilience was not significant, b = 0.007, SE = 0.008, CI [−0.006, 0.025]. Resilience did not mediate the association between childhood trauma and suicide risk on its own; resilience was only a significant mediator when preceding depressive symptoms. Conversely, the indirect effect of childhood trauma on suicide risk through depression was significant, b = 0.041, SE = 0.014, 95% CI [0.014, 0.070]; childhood trauma was associated with higher depressive symptoms and higher depressive symptoms were associated with increased suicide risk.
Figure 2.
Serial mediation model tested by Model 6 of the PROCESS macro with blue lines representing significant pathways.
**p < 0.01. ***p < 0.001.
Discussion
The current study was designed to better understand the associations between childhood trauma, resilience, depression and suicide risk in a sample of individuals with IBD using moderated mediation and serial mediation models. Taken together, the results suggest that childhood trauma, resilience and depression play significant roles in promoting and/or mitigating suicide risk.
Objective 1 tested resilience as a moderator of the indirect effect of depressive symptoms on the association between childhood trauma and suicide risk. Contrary to hypothesis, resilience was not a significant moderator in the associations between childhood trauma, depressive symptoms and suicide risk; similar to Wang et al. (2018) suggesting that resilience does not moderate perceived stress and depression. One explanation for why resilience may not moderate is that childhood trauma negatively affects resilience levels (Crosta et al., 2018). The results of the present study suggest that resilience may not be innate, rather it is fostered in childhood and influenced by many contextual factors including personal traits (e.g., problem solving skills), familial relationships (e.g., positive attachment) and community relations (Lopez et al., 2019). Therefore, resilience may be better conceptualized as a mediator in a causal pathway between childhood trauma and suicidal behaviours, rather than a moderator of this association.
In objective 2, resilience and depression significantly mediated the relationship between childhood trauma and suicide risk. Increased childhood trauma was associated with lower resilience levels, which were associated with increased depressive symptoms, and ultimately increased suicide risk. These results suggest that traumatic experiences in childhood may blunt resilience in adulthood, thereby increasing vulnerability to depression. The present findings are consistent with research suggesting that resilience can act as a protective factor against depression and that childhood trauma may be associated with decreased resilience (Crosta et al., 2018; Ding et al., 2017; Wingo et al., 2010).
Childhood trauma was also associated with increased depressive symptoms directly, which then were associated with higher suicide risk. Consistent with prior research in other populations, this suggests that childhood trauma is a risk factor for depression and that depression increases suicide risk among IBD patients (Angst et al., 1999; Hammen et al., 2000).
Resilience alone does not appear to be associated with increased suicide risk, as there were no significant indirect effects of resilience on suicide risk in objective 2 and resilience was not a significant moderator in objective 1. Regardless, the current study suggests that resilience may affect suicide risk by increasing one’s vulnerability to depression.
These results provide important clinical implications. First, clinicians should consider a multidisciplinary approach that involves both medical and psychological factors. Psychological factors should be considered with assessments of depressive symptomology and/or suicide risk, particularly if patients with IBD present with medical factors that are associated with elevated suicide risk (e.g., active disease, high levels of pain; Mihajlovic et al., 2020). Identification and treatment of depression in IBD populations may be key in reducing the high rate of patients at risk for suicide (Schwartz-Lifshitz et al., 2012). Clinicians may also wish to examine childhood traumas as these may increase suicide risk. Acknowledging factors such as resilience may allow for clinicians to be proactive in addressing and reducing suicide risk among IBD patients through reductions in depressive symptomology. For example, Pereira et al. (2016) observed significant improvements in depressed patients when treated with resilience and mindfulness approaches.
Limitations and future directions
There were several limitations to this study. First, given the online nature of this study, participants were not screened by gastroenterologists, rather they identified as IBD patients through self-report. The validity of responses to the questionnaires may be critiqued due to the self-report nature of the study. However, self-report measures are often unavoidable, particularly in suicide research, and the results of the study should not be discounted due to the possible subjectivity of the measures used. Further, the voluntary nature of the study also poses the possibility of self-selection effects or biases given that individuals experiencing greater negative impacts on their daily lives may be more inclined to participate.
Second, only individuals with computer/mobile and internet access were able to access the survey, thereby limiting the results to those with access to the technology requirements which may lead to a bias in recruitment. The sample was also relatively homogenous in being predominantly comprised of middle-aged, Caucasian females from North America, Europe, Australia and New Zealand. As such, the homogeneity of the sample limits the generalisability of findings to various ethnicities or cultures.
Regarding study measurement, the SBQ-R does not clearly discriminate between suicidal ideation, plans, or previous attempts which individually influence suicide risk. As such, one cannot quantify the presence or absence of these individual factors within the sample. However, it is a reliable measure for determining overall suicide risk in respondents as it is not limited to current suicidal behaviours but also considers past suicidal behaviours, which are important risk factors in predicting future suicidal behaviour (Osman et al., 2001). Additionally, the current study does not discriminate between different types of childhood traumatic events or the quantity of traumatic events experienced in the analyses. As such, future research may benefit from exploring how specific traumatic experiences and/or the quantity of traumatic events experienced influence the development of depressive symptoms and suicide risk.
Finally, as the current study was cross-sectional, causality cannot be established. Despite the inability to infer causality, the study suggests that there is an association between psychological factors and suicide risk among IBD patients. The current study examined how psychological factors are associated with suicide risk but the examination of other risk factors for suicide is suggested. In particular, the role of the inflammatory process and its effects may further elucidate the relationship between IBD, childhood trauma, depression and suicide risk (Capuco et al., 2020; Moulton et al., 2019).
In conclusion, this study stresses the importance of childhood traumatic events and depression in suicidal behaviour in individuals with IBD and highlights resilience as a potential avenue for reducing suicide risk. It is also suggested that clinicians be cognizant of risk factors for depression so as to quickly identify and treat depression to mitigate suicide risk in IBD patients. Overall, these results suggest treatment of individuals with IBD should involve a multidisciplinary approach where medical and psychological factors are considered to optimize care.
Supplemental Material
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-doc-1-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-docx-2-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-docx-3-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-4-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-5-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by the Inflammation, Microbiome and Alimentation: Gastro-Intestinal and Neuropsychiatric Effects (IMAGINE) Chronic Disease Network’s Incubator Grant [395157]. IMAGINE is part of the Strategy for Patient Oriented Research initiative of the Canadian Institute of Health Research.
ORCID iDs: Krista Jones  https://orcid.org/0000-0002-7983-2381
https://orcid.org/0000-0002-7983-2381
Valentina Mihajlovic  https://orcid.org/0000-0002-8831-4316
https://orcid.org/0000-0002-8831-4316
References
- Angst J, Angst F, Stassen H. (1999) Suicide risk in patients with major depressive disorder. The Journal of Clinical Psychiatry 60(Suppl 2): 57–62. [PubMed] [Google Scholar]
- Bernstein CN, Zhang L, Lix LM, et al. (2018) The validity and reliability of screening measures for depression and anxiety disorders in inflammatory bowel disease. Inflammatory Bowel Diseases 24(9): 1867–1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capuco A, Urits I, Hasoon J, et al. (2020) Current perspectives on gut microbiome dysbiosis and depression. Advances in Therapy 37(4): 1328–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crohn’s and Colitis Foundation of Canada (2012) The Impact of Inflammatory Bowel Disease in Canada. Toronto: Crohn’s and Colitis Foundation Canada. Available at: http://crohnsandcolitis.ca/Crohns_and_Colitis/documents/reports/ccfc-ibd-impact-report-2012.pdf?ext=.pdf (accessed 20 June 2020). [Google Scholar]
- Crosta ML, De Simone C, Di Pietro S, et al. (2018) Childhood trauma and resilience in psoriatic patients: A preliminary report. Journal of Psychosomatic Research 106: 25–28. [DOI] [PubMed] [Google Scholar]
- de Mattos Souza LD, Molina ML, da Silva RA, et al. (2016) History of childhood trauma as risk factors to suicide risk in major depression. Psychiatry Research 246: 612–616. [DOI] [PubMed] [Google Scholar]
- Ding H, Han J, Zhang M, et al. (2017) Moderating and mediating effects of resilience between childhood trauma and depressive symptoms in Chinese children. Journal of Affective Disorders 211: 130–135. [DOI] [PubMed] [Google Scholar]
- Drossman DA, Talley NJ, Leserman J, et al. (1995) Sexual and physical abuse and gastrointestinal illness: Review and recommendations. Annals of Internal Medicine 123(10): 782. [DOI] [PubMed] [Google Scholar]
- Ferro M, Rhodes A, Kimber M, et al. (2017) Suicidal behaviour among adolescents and young adults with self-reported chronic illness. The Canadian Journal of Psychiatry 62(12): 845–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Thomson E, Sulman J. (2006) Depression and inflammatory bowel disease: Findings from two nationally representative Canadian surveys. Inflammatory Bowel Diseases 12(8): 697–707. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, West K, Sulman J, et al. (2015) Childhood maltreatment is associated with ulcerative colitis but not Crohn’s disease: Findings from a population-based study. Inflammatory Bowel Diseases 21(11): 2640–2648. [DOI] [PubMed] [Google Scholar]
- Gradus J, Qin P, Lincoln A, et al. (2010) Inflammatory bowel disease and completed suicide in Danish adults. Inflammatory Bowel Diseases 16(12): 2158–2161. [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley SE. (2000) Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology 68(5): 782–787. [PubMed] [Google Scholar]
- Hayes A. (2013) Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press. [Google Scholar]
- Keefer L, Kane SV. (2017) Considering the bidirectional pathways between depression and IBD: Recommendations for comprehensive IBD care. Gastroenterology & Hepatology 13(3): 164–169. [PMC free article] [PubMed] [Google Scholar]
- Kline RB. (2015) Principles and Practice of Structural Equation Modeling. New York: Guilford Press. [Google Scholar]
- Knowles SR., Graff LA, Wilding H, et al. (2018) Quality of life in inflammatory bowel disease: A systematic review and meta-analyses—Part I. Inflammatory Bowel Diseases 24(4): 742–751. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. (2001) The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine 16(9): 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik T. (2015) Inflammatory bowel disease: Historical perspective, epidemiology, and risk factors. Surgical Clinics of North America 95(6): 1105–1112. [DOI] [PubMed] [Google Scholar]
- Meng X, Fleury M, Xiang Y, et al. (2018) Resilience and protective factors among people with a history of child maltreatment: A systematic review. Social Psychiatry and Psychiatric Epidemiology 53(5): 453–475. [DOI] [PubMed] [Google Scholar]
- Mihajlovic V, Tripp DA, Jacobson JA. (2020) Modelling symptoms to suicide risk in individuals with inflammatory bowel disease. Journal of Health Psychology. 26(12): 2143–2152. DOI: 10.1177/1359105320904750. [DOI] [PubMed] [Google Scholar]
- Mikocka-Walus A, Knowles SR, Keefer L, et al. (2015) Controversies revisited: A systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflammatory Bowel Diseases 22(3): 752–762. [DOI] [PubMed] [Google Scholar]
- Moulton C, Pavlidis P, Norton C, et al. (2019) Depressive symptoms in inflammatory bowel disease: An extraintestinal manifestation of inflammation? Clinical and Experimental Immunology 197(3): 308–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Bagge C, Gutierrez P, et al. (2001) The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment 8(4): 443–454. [DOI] [PubMed] [Google Scholar]
- Pennebaker J, Susman J. (1988) Disclosure of traumas and psychosomatic processes. Social Science & Medicine 26(3): 327–332. [DOI] [PubMed] [Google Scholar]
- Pereira J, Barkham M, Kellett S, et al. (2016) The role of practitioner resilience and mindfulness in effective practice: A practice-based feasibility study. Administration and Policy in Mental Health and Mental Health Services Research 56(5): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine M. (2018) Chronic pain and suicide risk: A comprehensive review. Progress in Neuro-Psychopharmacology & Biological Psychiatry 87(Pt B): 269–280. [DOI] [PubMed] [Google Scholar]
- Sans M, Figueroa C. (2008) Inflammatory bowel disease. In: Shoenfeld Y, Cervera R, Gershwin EM. (eds) Diagnostic Criteria in Autoimmune Diseases, 1st edn. Totowa, NJ: Humana Press, pp.329–334. [Google Scholar]
- Schwartz-Lifshitz M, Zalsman G, Giner L, et al. (2012) Can we really prevent suicide? Current Psychiatry Reports 14(6): 624–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirois F, Hirsch J. (2017) A longitudinal study of the profiles of psychological thriving, resilience, and loss in people with inflammatory bowel disease. British Journal of Health Psychology 22(4): 920–939. [DOI] [PubMed] [Google Scholar]
- Smith B, Dalen J, Wiggins K, et al. (2008) The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine 15(3): 194–200. [DOI] [PubMed] [Google Scholar]
- Lopez S, Pedrotti J, Snyder C. (2019) Positive Psychology, 4th edn. Thousand Oaks, CA: SAGE. [Google Scholar]
- Targownik L, Bernstein C. (2017) The economics of inflammatory bowel disease. In: Cohen R. (ed.) Inflammatory Bowel Disease Diagnosis and Therapeutics, 3rd edn. Springer International Publishing. Available at: https://ebookcentral.proquest.com/lib/queen-ebooks/reader.action?docID=4890720&query (accessed 20 June 2020). [Google Scholar]
- Tunnard C, Rane L, Wooderson S, et al. (2014) The impact of childhood adversity on suicidality and clinical course in treatment-resistant depression. Journal of Affective Disorders 152–154: 122–130. [DOI] [PubMed] [Google Scholar]
- Wang L, Xu B, Gu Y, et al. (2018) The mediating and moderating effects of resilience on the relationship between perceived stress and depression in heroin addicts. Journal of Community Psychology 47(3): 495–503. [DOI] [PubMed] [Google Scholar]
- Wehkamp J, Götz M, Herrlinger K, et al. (2016) Inflammatory bowel disease: Crohn’s disease and ulcerative colitis. Deutsches Aerzteblatt International 113(5): 72–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo A, Wrenn G, Pelletier T, et al. (2010) Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. Journal of Affective Disorders 126(3): 411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Byrne G, Lee T, et al. (2018) Incidence of suicide in inflammatory bowel disease: A systematic review and meta-analysis. Journal of the Canadian Association of Gastroenterology 1(3): 107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-doc-1-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-docx-2-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-docx-3-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-4-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-sav-5-hpq-10.1177_1359105321999085 for Childhood trauma, depression, resilience and suicide risk in individuals with inflammatory bowel disease by Dean A Tripp, Krista Jones, Valentina Mihajlovic, Sandra Westcott and Glenda MacQueen in Journal of Health Psychology