Abstract
Overcoming the COVID-19 pandemic in the United States will require most Americans to vaccinate against the disease. However, considerable research suggests that a significant proportion of Americans intend to forego vaccination, putting pandemic recovery at risk. Republicans are one of the largest groups of COVID-19 vaccine hesitant individuals. Therefore, identifying strategies to reduce vaccine hesitancy within this group is vital to ending the pandemic. In this study, we investigate the effectiveness of messages from co-partisan sources in reducing vaccine hesitancy. In a large (N = 3000) and demographically representative survey, we find that exposing “Middle-of-the-Road” partisans to pro-vaccine messages from co-partisan source cues reduces vaccine hesitancy. However, for those who identify as “Strong” or “Weak” partisans, we find no statistically significant differences in vaccination intentions when exposed to pro-vaccine messages from co-partisan sources. We conclude by discussing how our findings are helpful for vaccine communication efforts.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10865-022-00323-4.
Keywords: COVID-19, Health communication, Vaccine hesitancy, Public opinion, Public health, COVID-19 vaccine
Introduction
Despite messaging from the public health community about the benefits of vaccinating against COVID-19, a significant proportion of Americans have not yet been vaccinated against the virus. Without interventions to improve vaccination rates in the United States (US), COVID-19 will continue to spread across the US, with devastating consequences for hospitalization and mortality, as well as the potential for new vaccine-resistant variants to develop. One segment of the American public that has been particularly reluctant to vaccinate has been those who self-identify as members of the Republican Party (Callaghan, Moghtaderi, et al., 2021). The politicization of COVID-19 vaccination has led to high levels of uptake among Democrats and lower levels of uptake among Republicans (Russonello, 2021). We refer to this phenomenon as asymmetric vaccine hesitancy.
With COVID-19 variants still developing and spreading, overcoming this asymmetric vaccine hesitancy has taken on new importance. Public health officials, politicians, and pundits alike–on both sides of the partisan aisle–have noted the importance of devising communication strategies that encourage Americans on the ideological right to vaccinate against COVID-19 (Balk, 2021; Colvin & Slodysko, 2021).
To overcome vaccine hesitancy and increase vaccine uptake, previous research has pointed to the importance of tailoring communication strategies to appeal to the social and psychological correlates of vaccine aversion rather than only attempting to debunk factual misperceptions (Lunz Trujillo et al., 2020). Building on this previous research suggesting that vaccine messages should be tailored to specific subgroups in American society, our study seeks to test whether asymmetric vaccine hesitancy can be overcome by presenting self-identified Republicans and Democrats who have yet to vaccinate against COVID-19 with pro-vaccine messages from co-partisan political elites. In our research, we define co-partisan political elites as public officials who share one’s professed partisan loyalties and who have vaccinated against COVID-19. We assess whether pro-vaccination messages from these individuals–which we call co-partisan source cues–have the potential to mitigate ideologically-driven vaccine hesitancy and increase willingness to vaccinate.
While previous studies have shown that exposing unvaccinated Americans to elite source cues can increase intentions to vaccinate and change health behaviors (see Pink et al., 2021; Spälti et al., 2021), we feel our work extends this research in two ways. First, we find merit in examining how the strength of partisan identity influences the effect of the pro-vaccine message. We theorize that partisans should not be viewed uniformly, and that some partisans may be more receptive to these messages than others (i.e., moderate partisans vs. strong and weak partisans). Second, unlike prior studies comparing treatment effects of pro-vaccine messages from Democratic and Republican elites, our study instead compares the effect of co-partisan source cues within each partisan subgroup. In other words, we are comparing the effect of exposing unvaccinated individuals to pro-vaccine messages from only those partisans with whom they identify.
The politicization of COVID-19 and vaccine hesitancy
Politically salient topics and events in the US have a tendency to become polarized (Bafumi & Shapiro, 2009). COVID-19 quickly became one of the most significant political issues in recent memory due to its direct threat to people's health, as well as its need for a large-scale governmental response. Consequently, the virus almost immediately became polarized along partisan lines (Sharfstein et al., 2021). With former President Trump participating in public briefings on the virus and referring to COVID-19 as the "China Virus" while governors of different ideological stripes took different approaches to masking and social distancing, many in the American public quickly began to view the COVID-19 pandemic through a political lens (Barrow, 2021; Groves & Kolpack, 2020; Milligan, 2020; Roberts, 2020). This politicization was further amplified through misinformation about the severity of the virus from right-wing media outlets and President Trump himself, which has hampered public health officials' ability to contain the spread of COVID-19 (Motta et al., 2021; Sylvester, 2021).
The politicization of the pandemic has also undermined widespread vaccination against COVID-19. Despite messaging from the health community about the safety and effectiveness of the COVID-19 vaccines and the benefits of vaccinating for society, segments of the population remain hesitant about receiving the COVID-19 vaccine (Ahmed & Kirkpatrick, 2021). Vaccine hesitancy is defined as the delay in acceptance, reluctance, or refusal of vaccination despite the availability of a vaccination (Callaghan et al., 2019; MacDonald, 2015). While some degree of resistance to vaccinating has been present in the US for decades, dating back to smallpox mandates that were seen by some as a violation of individual freedom, hesitancy toward the COVID-19 vaccine has been particularly vexing due to individuals viewing the pandemic through a partisan lens (Healy et al., 2020; Kestenbaum & Feemster, 2015).
COVID-19 vaccine hesitancy has been identified as being more prevalent among certain individuals, including those with high levels of religiosity, Blacks, and—critically for our purposes—among conservatives and Trump supporters (Callaghan, Moghtaderi, et al., 2021; Sharfstein et al., 2021). Political partisanship and ideology is also a well-documented determinant of vaccine uptake beyond COVID-19. Despite a common belief that liberals tend toward anti-vaccination attitudes in the United States, there is strong evidence that hesitancy is more likely among conservatives (Motta, 2021). In the context of COVID-19, a Kaiser Family Foundation survey done in May of 2021 found that a plurality of unvaccinated respondents self-identified as Republicans, as were nearly all respondents who said they "definitely would not get" the vaccine (Hamel et al., 2021). COVID resistance is also higher among individuals in rural counties, which tend to be more conservative than in urban counties (Callaghan et al., 2021; Murthy et al., 2021).
While there are various reasons why hesitancy toward COVID vaccines exists, the most frequently cited reasons for reluctance to vaccinate against COVID-19 are the beliefs that the vaccines are not safe or effective (Callaghan, Moghtaderi, et al., 2021). Perceived health risk also influences vaccine acceptance; when individuals perceive a risk to themselves, such as the threat of getting sick from COVID-19, they become more favorable toward interventions, including vaccinations (Sheeran et al., 2014).
Unfortunately, views of vaccine safety, efficacy and health risks have become heavily politicized. This may be partly due to how popular media have framed their coverage of these topics, influencing the way individuals perceive the pandemic and life-saving vaccines. Although no media outlet is devoid of misinformation or political bias entirely, previous research suggests that right-leaning outlets like Fox News are comparatively more likely to lend airtime to misinformation about the pandemic’s origins and severity (see: Motta et al., 2020). For example, a Pew poll found that 56% of respondents whose primary news source was Fox News believed the news media greatly exaggerated the risks of the COVD-19 pandemic. In comparison, among individuals whose primary news source was CNN, only 25% thought the news media exaggerated the risks of the COVID-19 pandemic (Jurkowitz & Mitchell, 2020). These findings are consistent with previous research documenting that consumption of conservative news is related to the acceptance of conspiracy beliefs about COVID-19 (Jamieson & Albarracin, 2020; Motta et al., 2020). Another common reason for COVID-19 vaccine hesitancy is that many individuals—and especially Republicans (see: Motta et al., 2021)—were already hesitant about vaccinating in general before the pandemic. For example, a Kaiser Family Foundation report in June 2021 found that of those individuals who are unvaccinated, 26% do not trust vaccines in general (Hamel et al., 2021).
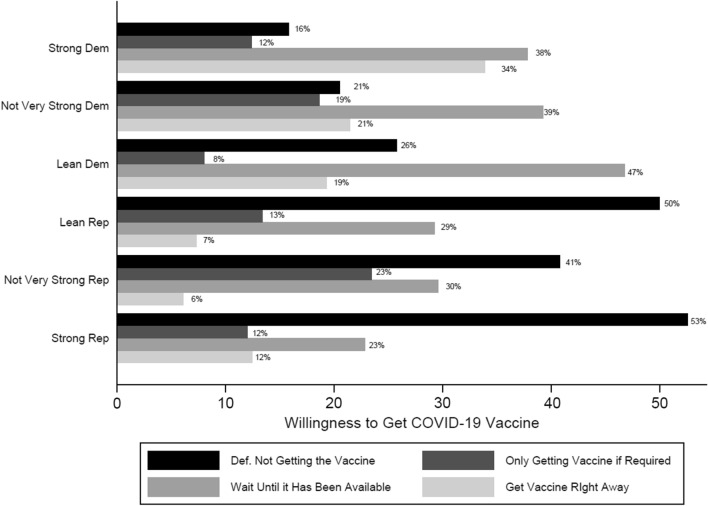
Low levels of trust and high vaccine hesitancy among Republicans lead to what we call asymmetric vaccine hesitancy. In our sample, we see clear evidence of this phenomenon. Figure 1 below lays out the percentage of respondents willing to get a COVID-19 vaccine, broken down by partisanship. As is shown in the Figure, as of mid-May 2021,1 those who identify as Democrats are much more likely to answer "Getting the Vaccine Right Away" than Republican respondents. For those respondents who identify as Strong Republicans, 53% say they will "Definitely Not Get the Vaccine, while only 16% of Strong Democrats will "Definitely Not Get the Vaccine." While most Republicans appear to be unwilling to vaccinate against COVID-19, this resistance is not uniform among Republicans. For example, while 41% of those respondents who identify as Not Very Strong Republicans are "Definitely Not Getting the Vaccine," 59% are at least open to getting the vaccine versus 47% of Strong Republicans who are open to getting a COVID vaccine. This partisan split has remained over time (Kates et al., 2022). Regardless of the reasons for individuals to be hesitant toward a COVID-19 vaccine, public health officials must create strategies to mitigate this hesitancy.
Fig. 1.
Percentage of respondents willing to get a COVID-19 vaccine–by partisanship
Overcoming asymmetric COVID-19 vaccine hesitancy
Since the COVID-19 vaccine became widely available to the US population, public health officials have worked to overcome vaccine hesitancy (Stolberg & Karni, 2021). Previous research on overcoming vaccine hesitancy to the MMR and flu vaccines provides a helpful foundation to inform current efforts to increase vaccination uptake for COVID-19. For example, Nyhan and Reifler, (2015) found that providing individuals with vaccine safety information from the CDC could reduce vaccination misinformation (see also: Vraga & Bode, 2017). Other research suggests that highlighting the scientific consensus surrounding vaccinations effectively reduces concern about the MMR vaccine, its connection to autism, and increases overall support for vaccination (van der Linden et al., 2015).
While fact-based communication programs can help to reduce hesitancy, more recent research suggests that tailored communication strategies can be particularly effective in moving individuals towards vaccination. For example, Lunz Trujillo et al., (2020) found that presenting the public with pro-vaccine messages tailored to appeal to the specific psychological predispositions underlying vaccine hesitancy reduced the endorsement of vaccine misinformation. Other research has shown that providing additional information addressing misinformation can also increase vaccination intentions. For instance, despite extreme polarization in COVID-19 vaccination intentions among the public, Motta et al., (2021) found that emphasizing the personal health risks and collective health consequences of not vaccinating significantly increased vaccination intentions among Americans.
Some studies (such as Pink et al., 2021) have found that exposing respondents to elite party cues increases vaccination intention among Republicans. Further, other studies have argued that general messaging to increase COVID-19 vaccine uptake works for both conservatives and liberals (Green et al., 2022). However, these studies fail to consider how to resolve asymmetric vaccine hesitancy among not just conservatives and supporters of former President Trump (Callaghan, Moghtaderi, et al., 2021), but also among subgroups within Republicans and conservatives.
The persuasive power of co-partisan vaccine source cues
Given the politicization of COVID-19, there is good reason to suspect that partisans will be more likely to intend to vaccinate against COVID-19 if exposed to pro-vaccine communications that provide evidence of political elites from one's preferred party ("co-partisan source cues") choosing to vaccinate against COVID-19. This may be especially true for self-identified Republicans, who are substantially less likely to intend to vaccinate against COVID-19 than Democrats (Vakil, 2021) and therefore have more ground to "make up" concerning vaccine uptake.
Psychologically, people tend to attach themselves to the groups they are members of to receive positive psychological benefits, such as increased self-esteem and a sense of belonging (Huddy, 2003; Tajfel, 1981). This is reinforced by group identifiers promoting the group's positive image and status, often through developing norms and values perceived as placing the group in a positive light while also viewing fellow in-group members—and especially leaders within the in-group—more positively than non-group members (Huddy, 2003). Therefore, group members often engage in motivated reasoning when presented with information relating to the in-group or its worldview. Information that portrays the group positively communicates and reinforces the group member's attachment to the group and is therefore accepted. Conversely, information that goes against the group is rejected (Huddy, 2003). These tendencies are especially strong if the individual strongly identifies with the group and are weaker if the individual weakly identifies with the group (Huddy et al., 2015).
When considering partisanship as a group identity, if pro-vaccine communications include co-partisan vaccination source cues, they provide a "functional match" (Clary et al., 1994; Lavine & Snyder, 1996; Petty & Wegener, 1998) between the message content and the audience's partisanship. Whereas pro-vaccine communications might ordinarily challenge Republicans' political identities given messages from many Republican politicians downplaying the virus, and its severity, messages including co-partisan source cues should affirm individuals' partisan identities by drawing attention to the vaccination choices of trusted communicators (i.e., one's fellow partisans; e.g., seeDunn, 2020; Jurkowitz & Mitchell, 2020).
Co-partisan source cues may provide partisans, particularly Republicans (who are less likely to vaccinate and have more “ground to gain” concerning vaccine uptake), with the cognitive motivation to process pro-vaccine communications favorably and potentially influence vaccine uptake. In other words, the messages flip the logic of motivated partisan reasoning away from the tendency to evaluate pro-vaccine communications in line with one's prior partisan commitments (Kraft et al., 2015; Kunda, 1990; Lodge & Taber, 2013; Taber & Lodge, 2006). Messages sourced by co-partisans have the potential to replace (in this case) Republicans' partisan commitments to reject pro-vaccine communications that challenge elite rhetoric about vaccine safety, with the motivation to take actions recommended by trusted sources.
Critically, a rich line of political and social science research suggests that messages sourced by co-partisans can increase partisans' willingness to accept counter-attitudinal information. Past work finds, for example, that partisans are more likely to accept counter-attitudinal information about public health (Berinsky, 2017), climate change (Benegal & Scruggs, 2018), and a variety of other issues (Druckman et al., 2013) when those messages are attributed to trusted partisan elites, or other sources with well-known partisan reputations (see also: Bolsen et al., 2019; Motta et al., 2021).
However, research on the influence of elite source cues on public opinion toward COVID is considerably more mixed. For example, Myers, (2021) found no significant effects (across various dependent variables) for partisan frames when he exposed respondents to frames that included a non-partisan frame, partisan conflict frame, or a framing where one party was winning and the other losing. Similarly, Gadarian et al., (2021) found no significant effect for partisan frames, including a message framing including former President Trump, across various dependent variables, including trust in various government actors and policies dealing with the effects of coronavirus and immigration policies. On the other hand, Green et al., (2022), Pink et al., (2021), and Bhanot and Hopkins (2020) found that elite source cues can change attitudes toward health behaviors, specifically social distancing, and vaccination intention.
Concerning pro-vaccine messaging, we suspect the effects of co-partisan source cues to be most effective for "middle-of-the-road" Republicans who neither strongly nor weakly identify with the GOP. While we might expect strong partisans to be highly receptive to co-partisan source cues, these individuals might also be highly motivated to maintain salient anti-vaccine attitudes signaled by strong and repeated elite messages to reject the vaccine (see: Kraft et al., (2015) for a theoretical demonstration of this principle). Simultaneously, weak partisans may be less likely to hold the party's most visible political figures in high esteem, thereby reducing the effect of a message from a leading political figure.
"Middle-of-the-road" Republicans, however, may represent something of a “sweet spot.” These individuals may be both receptive to messages from GOP elites while nevertheless being less motivated to uphold the “party line” on vaccination. Consequently, we expect them to be the most likely to vaccinate upon being exposed to pro-vaccine messages from Republican politicians and other leading Republican voices.
H1
"Middle-of-the-road" Republicans exposed to messages from co-partisan sources will be more likely than strong or weak Republicans to vaccinate against COVID-19.
For Democrats, however, the effect of co-partisan source cues is less clear. Although the psychologyical principles underlying the effectiveness of co-partisan source messages are no different for Democrats than for Republicans, the context in which Democrats are presented with these messages is quite different. For many Democrats, and especially “Strong Democrats,” the effect of pro-vaccine messages from partisan cues may have reached a ceiling effect. For example, a recent CBS News-YouGov poll found that 77% of Democrats said they were either fully or partially vaccinated, while 12% plan to be vaccinated, and 6% are undecided (Vakil, 2021). For most Democrats, then, the idea that vaccinating against COVID-19 is something they ought to pursue is not a position contrary to group expectations like it is among many Republicans. Thus, for those individuals who identify as “Strong Democrats,” the use of pro-vaccine messages by co-partisan source cues may not be very effective because there are not many individuals to move, and those that exist will have already been exposed to many similar messages. Notably, we are more hopeful for the impact of these pro-vaccine messages among “Middle-of-the-Road” Democrats who have not yet chosen to vaccinate. These individuals may be less likely to have already been exposed to many pro-vaccination messages from co-partisan elites but could still be very receptive to them, especially compared to weak partisans who might not have strong attachments to party elites. Finally, much like those who weakly identify with the Republican party, we expect those who weakly identify with the Democratic party to be less susceptible to in-group leadership cues.
H2
"Middle-of-the-road" Democrats exposed to messages from co-partisan sources will be more likely than strong or weak Democrats to vaccinate against COVID-19.
Methods
Data and procedure
To test these expectations, we fielded a large and demographically diverse survey of US adults (N = 3000) from May 6–15, 2021. Lucid's Fulcrum Academic service invited 3388 members of its large online opt-in panel to participate in the study, 93% of whom ultimately completed the survey. Lucid provides a national sample that approximates representativeness by targeting several known demographic benchmarks—including race, age, sex, household income and Census region. Despite concerns with online opt-in panels, Lucid has been found to be an appropriate survey tool for social science research (Coppock & McClellan, 2019). Research in political science and public health have successfully used Lucid data to study vaccine hesitancy and health politics more generally (Callaghan et al., 2019; Cassese et al., 2020; Lunz Trujillo et al., 2020; Callaghan, Moghtaderi, et al., 2021; Haeder et al., 2021).
In the survey that serves as the basis for this study, respondents first answered several questions about their current vaccination status. We first asked respondents a simple Yes/No question inquiring whether they had received the COVID-19 vaccine. To control for social desirability effects, we asked subsequent questions regarding which vaccine they received (including a “Don’t Know” response). If they answered that they received the Pfizer, Moderna, or Don’t Know options, they were then asked if they received just the first dose or both doses. Full question wording can be found in the Supplemental Materials. Respondents who reported not receiving the COVID-19 vaccine (42% of respondents) were then randomly assigned to read one of five short pro-vaccine messages as part of a survey experiment, varying the source of the pro-vaccine message, which included images of political and non-political elites who had already received a vaccine. Table 1 summarizes the key elements of our experimental design, including the number of respondents assigned to each of the five conditions. The full text for each experimental treatment condition (including images) can be found in the Supplemental Materials (see Supplemental Figure S1).
Table 1.
Experimental design summary
| Frame | Treatment wording |
|---|---|
| Control | |
| N = 412 (Dem) | When an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine? |
| N = 224 (Rep) | |
| Celebrities | |
| N = 420 (Dem) | As you may have heard, celebrities like Willie Nelson, Dolly Parton, and Samuel L. Jackson recently chose to receive a COVID-19 vaccine and are encouraging others to do the same. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine? |
| N = 245 (Rep) | |
| Political | |
| N = 393 (Dem) | As you may have heard, Democratic politicians like Joe Biden, Nancy Pelosi, and Jim Clyburn recently chose to receive a COVID-19 vaccine and are encouraging others to do the same. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine? |
| N = 251 (Rep) | As you may have heard, Republican politicians like Joni Ernst, Mike Pence, and Tim Scott recently chose to receive a COVID-19 vaccine and are encouraging others to do the same. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine? |
| N = 240 (Trump) | As you may have heard, former President Donald Trump received the vaccine before leaving office and encouraged others to do the same on Fox News. Given this, when an FDAapproved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine? |
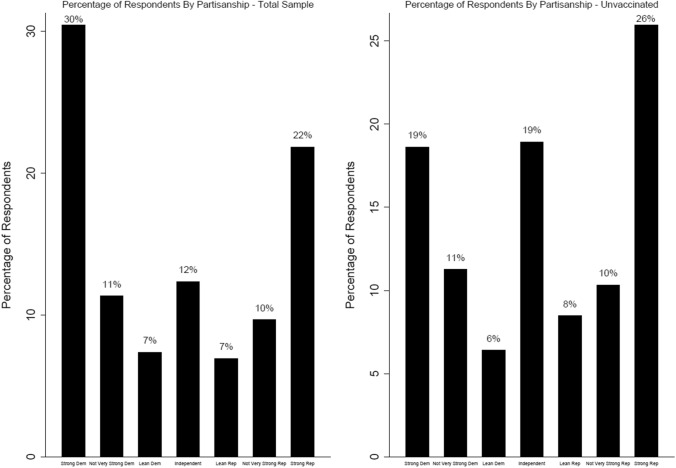
Respondents first answered a partisan measure that determined which treatment they would receive. We asked respondents to place themselves on a seven-point scale (ranging from 1 = Strong Democrat to 7 = Strong Republican) to measure respondents' partisanship. Figure 2 below shows the percentage of our sample that identified with each point on the scale to underscore that our treatment effects were not limited to small groups. In addition, we believe it is necessary to show the distribution of unvaccinated individuals within each partisan category as it further illustrates the need to break examine the influence of messages based on an individual’s partisan strength.
Fig. 2.
Percentage of respondents by partisanship
Figure 2 shows 48% of our sample identified with the Democratic Party and 39% of the sample identified as Republican. However, of those who were unvaccinated, 44% of those identified with the Republican Party. More importantly, those who we would classify as “Middle-of-the-Road” partisans, make up 22% of the unvaccinated population in our sample. Having this varied partisan breakdown within our unvaccinated group allows us to test if our treatments influence a significant portion of the unvaccinated population.
Respondents who identified as Republican were randomly exposed to one of two political treatments. The first treatment included the following statement: "As you may have heard, politicians like Joni Ernst, Mike Pence, and Tim Scott recently chose to receive a COVID-19 vaccine and are encouraging others to do the same. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine?” This was followed by a combined picture of all three co-partisan source cues receiving the COVID-19 vaccine.
These politicians were chosen for several reasons. Mike Pence was the sitting Vice-President and the face of the COVID-19 response for the Trump administration. He was also vocal in his support for the vaccine and received the vaccine in a televised appearance (Shabad, 2020). Senators Tim Scott and Joni Ernst are also two prominent Republican Senators. Both made public statements about having been vaccinated through social media and further provide the ability to descriptively represent various respondents across different racial and gender backgrounds.
The second Republican political treatment focused on the effect former President Trump has as a co-partisan exemplar. This treatment included the following statement: "As you may have heard, former President Donald Trump received the vaccine before leaving office and encouraged others to do the same on Fox News. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine?" A stock photo of President Trump followed this as he elected not to receive his COVID-19 vaccine in public.
Like we did for Republican respondents, we also designed treatments to reach individuals who identified as Democrats and had not been vaccinated. Those respondents who identified as Democrats that were exposed to the Democratic political treatment received the following statement: "As you may have heard, Democratic politicians like Joe Biden, Nancy Pelosi, and Jim Clyburn recently chose to receive a COVID-19 vaccine and are encouraging others to do the same. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine?" Like the first Republican condition, this was followed by a picture of all three Democratic co-partisan source cues receiving the COVID-19 vaccine. At the time he received his vaccine, Joe Biden was the president-elect and received both doses of the vaccine in televised appearances (Sullivan, 2020). Similar to Senators Scott and Ernst, both Nancy Pelosi and Jim Clyburn are prominent members of the Democratic Party. They were vocal about their vaccination status on social media and provided the ability to target across different demographic backgrounds.
Notably, President Joe Biden was not included in his own treatment like former President Trump for two reasons. First, we were most interested in increasing vaccine uptake among those political groups most likely to refuse the vaccine (in this case, Republicans). Second, omitting an additional condition for President Biden alone allows us to preserve sufficient statistical power to detect sub-group effects across conditions.
Next, we designed a treatment that exposed both Republicans and Democrats to the same non-political elites (celebrities). Those respondents that were exposed to the celebrity treatment read the following statement: "As you may have heard, celebrities like Willie Nelson, Dolly Parton, and Samuel L. Jackson recently chose to receive a COVID-19 vaccine and are encouraging others to do the same. Given this, when an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine?" This was followed by a picture of all three celebrities receiving their COVID-19 vaccine.
These celebrities were chosen mainly because they were vocal about receiving their vaccine on social media. For example, Dolly Parton adapted her Grammy Award-winning song from "Jolene" to “Vaccine” in order to promote vaccination while receiving a vaccine at Vanderbilt University (Treisman, 2021). In addition, like the co-partisan source cues, using these celebrities allows us to target respondents with pro-vaccine messages across different racial, gender and ideological backgrounds. Finally, our study included a control group that was not exposed to a pro-vaccine message but was only asked the outcome measure on COVID-19 vaccine intentions, which is described below.
Measures
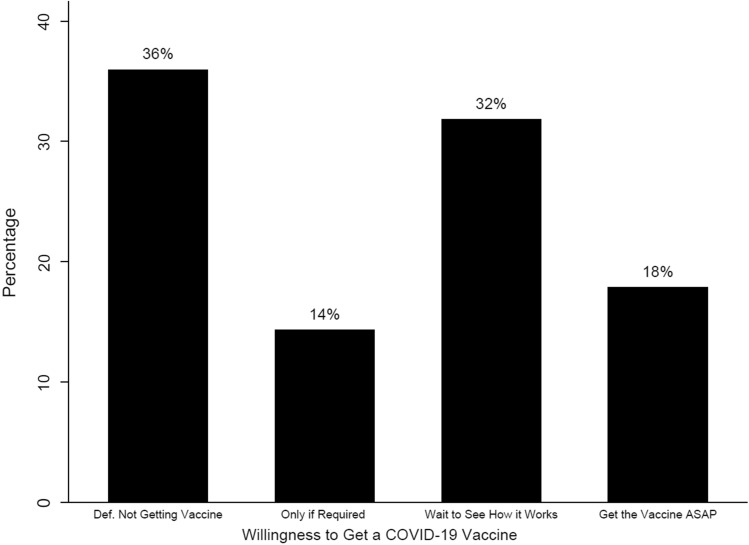
The key outcome variable in our analysis was an indicator of whether respondents intended to vaccinate against COVID-19. While it is an open question if expressing an intention to get a COVID-19 vaccine leads to individuals getting vaccinated, prior research has shown that individuals’ vaccination intentions tend to be a strong predictor of whether or not they actually choose to get vaccinated (see: Godin et al., 2010; Gerend & Shepherd, 2012). To measure respondent vaccination intentions, we asked the following question: When an FDA-approved vaccine for COVID-19 is available to you for free, which of these statements best describes your willingness to get a COVID-19 vaccine? (1) Get the vaccine as soon as you can; (2) Wait until it has been available for a while to see how it is working for other people; (3) Only get the vaccine if you are required to do so for work, school, or other activities; or (4) Definitely not getting the vaccine. These responses were coded so that higher values indicated a willingness to get the vaccine as soon as possible.2
Figure 3 below shows the distribution of responses for our vaccine intentions outcome measure. As Fig. 3 indicates, 36% of our respondents stated they are “Definitely not getting the vaccine,” 14% will “Only get the vaccine if they are required to do so for work, school, or other activities,” 32% will “wait until it has been available for a while to see how it is working for other people,” and 18% of respondents will “get the vaccine as soon as they can”.
Fig. 3.
Percentage of respondents willing to get a COVID-19 vaccine
Finally, balance tests included in the Supplemental Material (Supplementary Figure S2) reveal that our randomization protocol produced treatment groups that were similar across demographic indicators (age, race, gender, educational attainment and income) and their prior attitudes toward COVID vaccine safety. Therefore, adding additional control variables is unnecessary.
Results
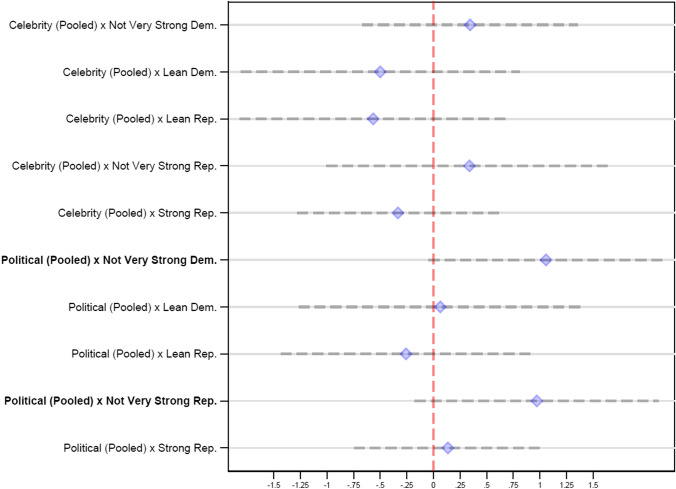
Figure 4 displays the results of an ordered logistic regression model interacting the four-point vaccine intention variable with our partisan identification variable (excluding Pure Independents who are 19% of the unvaccinated population within the sample) and serves as a test for H1 and H2. Symbols correspond to the unique effects of each treatment, with 95% confidence intervals extending from each one. Those estimates that fall to the right of the dashed line and whose confidence intervals do not intersect with it suggest a statistically significant increase in vaccine intention.3
Fig. 4.
Pooled treatment effects. Note: Ordered logistic regression coefficients presented, with 95% confidence intervals. Outcome variable is an ordinal indicator of COVID-19 vaccine intention (with higher scores reflecting increased intention to vaccinate). Coefficients which do not intersect with the dashed red line are statistically significant from control group effects at the p < 0.05, level (one-tailed). Results are derived from a model regressing vaccine intention on indicators denoting assignment to each treatment, by partisanship.
It is important to note that we opted to pool both the political and celebrity treatments rather than providing disaggregated findings. The Political (Pooled) treatments consisted of all the political treatments (i.e. Trump, GOP and Dem), while the Celebrity (Pooled) variable consisted of the same celebrity treatment that was shown to both Democrats and Republicans. By pooling the treatments, it provides us the necessary power to see the substantive influence of the treatments. It also allows us to see the substantive effects of the treatments within the different partisan subgroups.
Figure 4 demonstrates that "Middle-of-the-Road" partisans (which we classify as “Not Very Strong Republicans” and “Not Very Strong Democrats”) exposed to a pro-vaccine message from co-partisan source cues are positively and significantly associated with an increased willingness to receive the COVID-19 vaccine. For example, "Not Very Strong Republicans" who are exposed to a pro-vaccine message are significantly more likely to be willing to get a COVID-19 vaccine (B = 0.97, p = 0.05 (one-tailed test)). We also see similar findings for "Not Very Strong Democrats). Those Democratic respondents who are exposed to a pro-vaccine message are significantly more likely to be willing to get a COVID-19 vaccine (B = 1.06, p = 0.03 (one-tailed test)). This provides strong evidence in favor of H1 and H2.
Of course, coefficients from ordered logistic regressions do not provide a good sense of the magnitude of these effects. Thus, we present (in text) predicted probabilities that reflect the increase in indicating that respondents are willing to get the vaccine in each of these treatments (relative to the control group). We focus on the "Get the vaccine as soon you can" category, as we expect these individuals to be the most likely to vaccinate, but we were unable to at the time of the survey.
Substantively, among "Not Very Strong Republicans," assignment to the political co-partisan source cues (pooled across conditions) is associated with a 5% increase in the likelihood that respondents will be willing to vaccinate from 7% in the control group to 12% to those assigned to the co-partisan source cues treatment. For "Not so Strong Democrats," we see similar increases. For example, "Not Very Strong Democrats" who were assigned to the political co-partisan source cues were 12% more likely to vaccinate than "Not Very Strong Democrats" who were not exposed to a political treatment.
Finding substantive effects among “Middle-of-the-Road” partisans is important for several reasons. First, “Middle-of-the-Road” partisans make up close to 20% of the unvaccinated population within our sample. Any movement toward vaccination among any subgroup is notable progress. Second, it shows the benefits of using messages that appeal to those individuals who do not have a strong partisan attachment.
We should also note the null effects of the Political (Pooled) treatments on vaccine intentions among respondents who identify as “Strong/Lean” Republican/Democrat. We see that for those respondents who identify as either “Lean Democrat” or “Strong Republican,” the co-partisan source cues do move individuals toward vaccination but are not statistically significant when compared to the control group (B = 0.07, p = 0.46; B = 0.14, p = 0.38). We also see some movement away from vaccination intentions for those respondents who “Lean Republican.” Once again though, those results are statistically insignificant (B = − 0.26, p = 0.34). It appears that at both ends of the political spectrum (along with those who weakly align with either party), the usefulness of pro-vaccine messages elite partisan source cues is unsubstantiated with at least the current cues.
Conclusion
This piece offers novel evidence that partisan political elites can be effective communicators of pro-vaccine messages for vaccine skeptical groups via a randomized controlled survey experiment. However, consistent with our theoretical expectations, partisan elites' effectiveness in doing this is conditional on the strength of their audiences' partisan identities. Specifically, our messages are effective at moving vaccination intentions among the over 1 in 5 Americans who self-identify as “middle-of-the-road” partisans (see: Fig. 1).
Whereas moderate "middle-of-the-road" Republicans are 5% more likely to intend to vaccinate after learning that politicians from their side of the partisan aisle have opted to do the same, the COVID-19 vaccination intentions of weaker Republicans and the strongest Republicans are not significantly impacted by co-partisan elite messages. We also find an analogous pattern of effects for middle-of-the-road Democrats exposed to similar messages from trusted partisan sources. This further underscores the power of our messaging approach, as Democrats are comparatively more likely to intend to vaccinate against COVID-19.
Our findings have important implications for health communication efforts to encourage vaccination. As is so often the case in strategic communication research (Lupia, 2016), there is no "one size fits all" solution to overcoming vaccine hesitancy (see also: Lunz Trujillo et al., 2020). While our research provides optimism that it is, in fact, possible to "move the needle" (so to speak) on the partisan dynamics of vaccine hesitancy, we caution that the partisan source cues studied in this piece are effective only for specific partisan audiences. Efforts to reach more and/or less-extreme partisans via other messaging strategies and efforts to address vaccine hesitancy in other areas (e.g., resulting from religious commitments, psychological aversions to needles and blood, etc.) will almost certainly require alternate messaging framing approaches and/or exemplar cues to be effective. For example, members of religious traditions with high levels of COVID-19 vaccine hesitancy, such as members of the church of Latter-Day Saints (PRRI, 2021), may be persuaded to vaccinate when presented with evidence that some religious leaders within the church have opted to do the same (Walch, 2021).
Our work also underscores the theoretical importance of taking both message and messenger into account when evaluating the effectiveness of efforts to encourage vaccine uptake. Making an effort to make theory-informed predictions about whom different audiences might find credible communicators about vaccine-related issues can help science communicators better understand the boundary conditions under which their interventions might be effective.
Turning again to the example of vaccine uptake among members of the church of Latter-Day Saints, one could imagine a situation—similar to the one outlined in this paper—wherein the most orthodox (i.e., those most highly committed to church teachings about the importance of bodily sanctity) and least orthodox (i.e., those least aware of and/or likely to hold in esteem important players in the church) members of the faith are unpersuaded by examples of religious leaders opting to vaccinate. In contrast, those with moderate views are comparatively more likely to opt to vaccinate. Alternatively, one could also imagine a situation more and less dogmatic. People alike are highly deferential to religious authorities, and therefore more likely to vaccinate. We encourage future studies that make an effort to understand how audiences and messengers interact to shape health communication effectiveness in future research.
Our research, of course, is not without important limitations. Chief among them are the challenges of implementing some of our work's central findings. Armed with the results presented here, it is easy to construct messages (similar to our own) designed to appeal to middle-of-the-road GOP partisans. However, what is more complicated is identifying the interpersonal, televised, and other mediated channels in which these audiences exist. In other words, while it is easy to identify, for instance, partisan networks on social media platforms (e.g., those who "like" or are "fans" of specific partisan political figures), presenting middle-of-the-road partisan sub-groups with messages like ours (via advertising, for example) assume that moderate partisans participate in these social networks, and are readily identifiable therein.
The extent to which this is true could have important implications for the effectiveness of messaging campaigns like ours. If no moderates reside in the network, the messages may fall on unreceptive ears. Moreover, mistargeting strong and/or weak partisans with messages designed to appeal to other audiences (i.e., the middle) also risks potential backlash to the message (Hersh & Schaffner, 2013). Still, we note that—at least in our study—we find no evidence that strong/weak Republicans and Democrats are resistant to our messages or that they experience a backfire effect. Correspondingly, we think it is at least plausible that efforts to micro-target partisans in general (a) have the potential to reach middle-of-the-road partisans, without (b) turning away those who reside at each party’s weaker/stronger poles. Consequently, we encourage future efforts to (1) profile the partisan composition of social and other media networks where we might circulate messages like those described in this paper and (2) assess the effectiveness of these trials in field experiments conducted outside of the controlled, virtual laboratory environment.
Moreover, we caution that our research takes up the issue of COVID-19 vaccine hesitancy in just a single group (i.e., among Republicans and Democrats) and takes just a single messaging approach (i.e., varying the inclusion of co-partisan exemplars), using a limited set of partisan sources. Much like how strategic health communication is often, as discussed above, a "patchwork" effort, future research should attempt to craft messages that reach different audiences (e.g., devout religious groups, people with psychological proclivities to avoid vaccination, etc.), using different messaging tactics (e.g., presenting various arguments for/against vaccination), and/or featuring the use of different messengers or mediums (Druckman, 2021). We look forward to these efforts.
Further, we note that we measure intentions to vaccinate rather than actual vaccination rates. That said, previous studies indicate that individuals’ vaccination intentions tend to be a strong predictor of whether they actually choose to receive a vaccine (see: Godin et al., 2010; Gerend & Shepherd, 2012). Further, other similar studies have measured vaccine intentions, rather than actual vaccination rates, when evaluating messaging strategies to increase vaccine uptake (e.g., Green et al., 2022; Pink et al., 2021). Even so, we cannot provide a reliable estimate of how much vaccine behavior would be directly changed from exposure to this messaging, and we encourage future work in this area.
Finally, we note that we obtained these results from a single, cross-sectional survey experiment. They are therefore necessarily time-bound, reflecting a reality wherein nearly all Americans had the opportunity to vaccinate against COVID-19, but prior to the emergency of the deadly and highly-transmissible "delta” and “omicron” variants that (1) renewed calls for stringent public health guidelines pertaining to social distancing and mask-wearing behavior (Abutaleb et al., 2021), and (2) may have encouraged previously-skeptical individuals to choose to vaccinate (Brooks, 2021).
With the possibility of recommended second (for non-mRNA vaccines) or third (for mRNA vaccines) "booster" shots, and/or other elements of our constantly-changing public health reality constantly changing, it is an open question whether or not our messages would hold as COVID-19 variants inevitably appear. In the present study, we also could not test the degree to which messages like ours are effective at moving opinion in competitive framing environments (Chong & Druckman, 2007, 2013); where people are exposed to both positive/negative messages about vaccinating from partisan elites (and noting that some elite GOP partisans continue to voice mixed and/or negative views toward vaccination, see also: Knight, 2021; Lerer, 2021). Such competitive framing environments may better reflect the reality in which most partisans encounter messages about vaccines and are, therefore, a worthwhile avenue for future research.
Supplementary Information
Below is the link to the electronic supplementary material.
Author’s contribution
All team members helped in the conceptualization of the project and the design of questions. SS led paper writing and data analysis with primary support from MM and secondary support from KLT and TC.
Funding
This project was funded by the History and Political Science Department at Utah Valley University.
Data availability
Data will be publicly posted to the OSF data repository after publication.
Code availability
Code to replicate our analysis will be publicly posted to the OSF data repository after publication.
Declarations
Conflict of interest
The authors have no known conflicts of interest related to this research.
Consent to participate
This research was approved by the Institutional Review Board at Utah Valley University. All participants had to note they were older than 18 and consent to participate before beginning the research.
Consent for publication
Not Applicable.
Human and animal rights and informed consent
Following all procedures on human experimentation, informed consent was obtained from all participants included in the study.
Footnotes
Data for this survey was collected May 6–15, 2021.
We also conducted supplemental analysis (see Supplementary Figure S3) that combined the “only if required” and “wait to see how it works” into a single group. Combining these two categories into one group did not change the results, so we opted to include the models with all the categories in the paper.
We also ran models that pooled the 7-point Party ID scale into two categories—Republican and Democrat (excluding pure Independents) similar to Pink et al., 2021 (see Supplementary Figure S4). We find when we pool the Party ID scale the statistical significance of the treatments is erased. This provides further justification for focusing our persuasive messaging attempts on the theoretical “sweet spot” we identified for “Middle-of-the-Road” partisans.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abutaleb, Y., Johnson, C. Y., & Achenbach, J. (2021). The war has changed’: Internal CDC document urges new messaging, warns delta infections likely more severe. Washington Post.
- Ahmed, N., & Kirkpatrick, N. (2021). "When will 70% of adults in your state have received at least one dose of coronavirus vaccine?" The Washington Post, 2021.
- Bafumi J, Shapiro RY. A new partisan voter. Journal of Politics. 2009;71:1–24. doi: 10.1017/S0022381608090014. [DOI] [Google Scholar]
- Balk, T. (2021). "McConnell, other GOP leaders pivot toward openly supporting COVID vaccinations." New York Daily News, 2021.
- Barrow B. GOP Governors ties economy to relaxed approach to coronavirus. The Associated Press; 2021. [Google Scholar]
- Benegal SD, Scruggs LA. Correcting misinformation about climate change: The impact of partisanship in an experimental setting. Climatic Change. 2018;148:61–80. doi: 10.1007/s10584-018-2192-4. [DOI] [Google Scholar]
- Berinsky AJ. Rumors and health care reform: experiments in political misinformation. British Journal of Political Science. 2017;47:241–262. doi: 10.1017/S0007123415000186. [DOI] [Google Scholar]
- Bhanot, S., & Hopkins, D. J. (2020). Partisan polarization and resistance to elite messages: Results from a survey experiment on social distancing. Available at SSRN 3593450.
- Bolsen T, Palm R, Kingsland JT. The impact of message source on the effectiveness of communications about climate change. Science Communication. 2019;41:464–487. doi: 10.1177/1075547019863154. [DOI] [Google Scholar]
- Brooks, B. (2021). Delta variant, Louisiana doctors, slowly cracking vaccine resistance.
- Callaghan T, Lueck JA, Trujillo KL, Ferdinand AO. Rural and urban differences in COVID-19 prevention behaviors. The Journal of Rural Health. 2021;37:287–295. doi: 10.1111/jrh.12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, Motta M. Correlates and disparities of intention to vaccinate against COVID-19. Social Science & Medicine. 2021;272:113638. doi: 10.1016/j.socscimed.2020.113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan T, Motta M, Sylvester S, Trujillo KL, Blackburn CC. Parent psychology and the decision to delay childhood vaccination. Social Science & Medicine. 2019;238:112407. doi: 10.1016/j.socscimed.2019.112407. [DOI] [PubMed] [Google Scholar]
- Cassese EC, Farhart CE, Miller JM. Gender differences in COVID-19 conspiracy theory beliefs. Politics & Gender. 2020;16:1009–1018. doi: 10.1017/S1743923X20000409. [DOI] [Google Scholar]
- Chong D, Druckman JN. Counterframing effects. The Journal of Politics. 2013;75:1–16. doi: 10.1017/S0022381612000837. [DOI] [Google Scholar]
- Chong D, Druckman JN. Framing theory. Annual Review of Political Science. 2007;10:103–126. doi: 10.1146/annurev.polisci.10.072805.103054. [DOI] [Google Scholar]
- Clary EG, Snyder M, Ridge RD, Miene PK, Haugen JA. Matching messages to motives in persuasion: A functional approach to promoting volunteerism 1. Journal of Applied Social Psychology. 1994;24:1129–1146. doi: 10.1111/j.1559-1816.1994.tb01548.x. [DOI] [Google Scholar]
- Colvin J, Slodysko B. GOP’s vaccine push comes with strong words, few actions. Associated Press; 2021. [Google Scholar]
- Coppock A, McClellan OA. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Research & Politics. 2019;6:1–14. doi: 10.1177/2053168018822174. [DOI] [Google Scholar]
- Druckman, J. N. (2021). "A framework for the study of persuasion." Available at SSRN 3849077.
- Druckman JN, Peterson E, Slothuus R. How elite partisan polarization affects public opinion formation. American Political Science Review. 2013;107:57–79. doi: 10.1017/S0003055412000500. [DOI] [Google Scholar]
- Dunn A. As the US copes with multiple crises, partisans disagree sharply on severity of problems facing the nation. Pew Research Center; 2020. [Google Scholar]
- Gadarian SK, Goodman SW, Pepinsky T. Partisan endorsement experiments do not affect mass opinion on COVID-19. Journal of Elections, Public Opinion and Parties. 2021;31:122–131. doi: 10.1080/17457289.2021.1924727. [DOI] [Google Scholar]
- Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine. 2012;44:171–180. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G, Vézina-Im L-A, Naccache H. Determinants of influenza vaccination among healthcare workers. Infection Control & Hospital Epidemiology. 2010;31:689–693. doi: 10.1086/653614. [DOI] [PubMed] [Google Scholar]
- Green, J., Druckman, J. N., Baum, M. A., Lazer, D., Ognyanova, K., Simonson, M., Lin, J., Santillana, M., & Perlis, R. H. (2022). Using general messages to persuade on a politicized scientific issue. British Journal of Political Science.
- Groves, S., & Kolpack, D. (2020). Dakotas lead us in virus growth as both reject mask rules.
- Haeder SF, Sylvester SM, Callaghan T. Lingering legacies: Public attitudes about medicaid beneficiaries and work requirements. Journal of Health Politics, Policy and Law. 2021;46:305–355. doi: 10.1215/03616878-8802198. [DOI] [PubMed] [Google Scholar]
- Hamel, L., Lopes, L., Kearney, A., Sparks, G., Stokes, M., & Brodie, M. (2021). KFF COVID-19 vaccine monitor: June 2021.
- Healy J, Robertson C, Tavernise S. How Coronavirus Is Already Being Viewed Through a Partisan Lens. The New York Times; 2020. [Google Scholar]
- Hersh ED, Schaffner BF. Targeted campaign appeals and the value of ambiguity. The Journal of Politics. 2013;75:520–534. doi: 10.1017/S0022381613000182. [DOI] [Google Scholar]
- Huddy, L. (2003). "Group identity and political cohesion".
- Huddy L, Mason L, Aarøe L. Expressive partisanship: Campaign involvement, political emotion, and partisan identity. American Political Science Review. 2015;109:1–17. doi: 10.1017/S0003055414000604. [DOI] [Google Scholar]
- Jamieson, K. H., & Albarracin, D. (2020). "The relation between media consumption and misinformation at the outset of the SARS-CoV-2 pandemic in the US". The Harvard Kennedy School Misinformation Review.
- Jurkowitz, M., & Mitchell, A. (2020). Cable TV and COVID-19: How Americans perceive the outbreak and view media coverage differ by main news source.
- Kates, J., Tolbert, J. & Rouw, A. (2022). The red/blue divide in COVID-19 vaccination rates continues: An update.
- Kestenbaum LA, Feemster KA. Identifying and addressing vaccine hesitancy. Pediatric Annals. 2015;44:71–75. doi: 10.3928/00904481-20150410-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight, V. (2021). Is rand paul mixing up the vaccine message for Covid survivors?
- Kraft PW, Lodge M, Taber CS. Why people "Don't trust the evidence": Motivated reasoning and scientific beliefs. The ANNals of the American Academy of Political and Social Science. 2015;658:121–133. doi: 10.1177/0002716214554758. [DOI] [Google Scholar]
- Kunda Z. The case for motivated reasoning. Psychological Bulletin. 1990;108:480–498. doi: 10.1037/0033-2909.108.3.480. [DOI] [PubMed] [Google Scholar]
- Lavine H, Snyder M. Cognitive processing and the functional matching effect in persuasion: The mediating role of subjective perceptions of message quality. Journal of Experimental Social Psychology. 1996;32:580–604. doi: 10.1006/jesp.1996.0026. [DOI] [PubMed] [Google Scholar]
- Lerer L. How republican vaccine opposition got to this point. The New York Times; 2021. [Google Scholar]
- Lodge M, Taber CS. The Rationalizing Voter. Cambridge University Press; 2013. [Google Scholar]
- Lunz Trujillo, K., Motta, M., Callaghan, T., & Sylvester, S. (2020). "Correcting misperceptions about the MMR vaccine: Using psychological risk factors to inform targeted communication strategies." Political Research Quarterly: 1065912920907695.
- Lupia A. Uninformed: Why people know so little about politics and what we can do about it. Oxford University Press; 2016. [Google Scholar]
- MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Milligan, S. 2020. The political divide over the Coronavirus: From the origins to the response, republicans and democrats have very different ideas about the Coronavirus.
- Motta, M. (2021). "Republicans, not democrats, are more likely to endorse anti-vaccine misinformation." American Politics Research: 1532673X211022639.
- Motta M, Stecula D, Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the US. Canadian Journal of Political Science/revue Canadienne De Science Politique. 2020;53:335–342. doi: 10.1017/S0008423920000396. [DOI] [Google Scholar]
- Motta M, Sylvester S, Callaghan T, Lunz-Trujillo K. Encouraging COVID-19 vaccine uptake through effective health communication. Frontiers in Political Science. 2021;3:1. doi: 10.3389/fpos.2021.630133. [DOI] [Google Scholar]
- Murthy BP, Sterrett N, Weller D, Zell E, Reynolds L, Toblin RL, Murthy N, Kriss J, Rose C, Cadwell B. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020–April 10, 2021. Morbidity and Mortality Weekly Report. 2021;70:759. doi: 10.15585/mmwr.mm7020e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers CD. No effect of partisan framing on opinions about the COVID-19 pandemic. Journal of Elections, Public Opinion and Parties. 2021;31:132–144. doi: 10.1080/17457289.2021.1924747. [DOI] [Google Scholar]
- Nyhan B, Reifler J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine. 2015;33:459–464. doi: 10.1016/j.vaccine.2014.11.017. [DOI] [PubMed] [Google Scholar]
- Petty RE, Wegener DT. Matching versus mismatching attitude functions: Implications for scrutiny of persuasive messages. Personality and Social Psychology Bulletin. 1998;24:227–240. doi: 10.1177/0146167298243001. [DOI] [Google Scholar]
- Pink, S. L., Chu, J., Druckman, J. N., Rand, D. G., & Willer, R. (2021). Elite party cues increase vaccination intentions among Republicans. Proceedings of the National Academy of Sciences. [DOI] [PMC free article] [PubMed]
- PRRI. (2021). Religious identities and the race against the virus: Engaging faith communities on COVID-19 vaccination: (Wave 1: March 2021).
- Roberts, D. (2020). Partisanship is the strongest predictor of coronavirus response.
- Russonello G. Nearly half of Republicans say they don’t want a Covid vaccine, a big public health challenge. New York Times; 2021. [Google Scholar]
- Shabad, R. (2020). Pence receives Covid vaccine in televised appearance, hails 'medical miracle'.
- Sharfstein JM, Callaghan T, Carpiano RM, Sgaier SK, Brewer NT, Galvani AP, Lakshmanan R, McFadden SM, Reiss DR, Salmon DA, Hotez PJ. Uncoupling vaccination from politics: A call to action. The Lancet. 2021;398:1211–1212. doi: 10.1016/S0140-6736(21)02099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychological Bulletin. 2014;140:511. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Spälti AK, Lyons B, Mérola V, Reifler J, Stedtnitz C, Stoeckel F, Szewach P. Partisanship and public opinion of COVID-19: Does emphasizing Trump and his administration’s response to the pandemic affect public opinion about the coronavirus? Journal of Elections, Public Opinion and Parties. 2021;31:145–154. doi: 10.1080/17457289.2021.1924749. [DOI] [Google Scholar]
- Stolberg SG, Karni A. Nation faces ‘Hand-to-Hand Combat’ to get reluctant Americans vaccinated. New York Times; 2021. [Google Scholar]
- Sullivan, K. (2020). Biden receives first dose of Covid-19 vaccine on live television.
- Sylvester S. COVID-19 and motivated reasoning: The influence of knowledge on COVID-related policy and health behavior. Social Science Quarterly. 2021;102:2341–2359. doi: 10.1111/ssqu.12989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taber CS, Lodge M. Motivated skepticism in the evaluation of political beliefs. American Journal of Political Science. 2006;50:755–769. doi: 10.1111/j.1540-5907.2006.00214.x. [DOI] [Google Scholar]
- Tajfel, H. (1981). Human groups and social categories: Studies in social psychology. Cup Archive.
- Treisman, R. (2021). From 'Jolene' to vaccine: dolly parton gets COVID-19 shot she helped fund.
- Vakil C. Nearly 30 percent of Republicans say they won't get vaccinated: Poll. The Hill; 2021. [Google Scholar]
- van der Linden SL, Clarke CE, Maibach EW. Highlighting consensus among medical scientists increases public support for vaccines: Evidence from a randomized experiment. BMC Public Health. 2015;15:1–5. doi: 10.1186/s12889-015-2541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vraga EK, Bode L. Using expert sources to correct health misinformation in social media. Science Communication. 2017;39:621–645. doi: 10.1177/1075547017731776. [DOI] [Google Scholar]
- Walch T. Church’s First Presidency urges vaccination, says vaccines are ‘safe and effective’ in battle with COVID-19. Deseret News; 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be publicly posted to the OSF data repository after publication.
Code to replicate our analysis will be publicly posted to the OSF data repository after publication.