Abstract
Background:
Home visits after hospital discharge may reduce future healthcare utilization. We assessed the association of home visits by advanced practice registered nurses (APRN) and paramedics with healthcare utilization and mortality, and provider and patient experience.
Methods:
We conducted a retrospective cohort study using convergent mixed methods in one health system including adult medical patients discharged to home from November 2017–September 2019. We assessed outcomes for home visit vs. matched comparison patients at 30, 90, and 180 days, including hospital admission, emergency department (ED) use, and death: Phase 1 (APRN or paramedic visits assigned by geographic location) and Phase 2 (APRN and paramedic visit teams assigned to patients). Patients declining home visits and those accepting were also compared. Semi-structured interviews were conducted with home visit patients and providers, primary care providers, and nurse care coordinators.
Results:
In Phase 1, the 101 home visit matched to 303 comparison patients showed no differences in readmissions, ED visits, or death at 30, 90, and 180 days. In Phase 2, 157 home visit matched to 471 comparison patients had fewer 30-day readmissions (19.1% vs. 28.7%, p 0.024) and no differences in other outcomes. Compared with patients declining home visits, patients accepting had lower odds of 30-day readmission. In 44 interviews, themes of Medication Understanding, Knowledge Gap after Discharge, Patient Medical Complexity, Social Context, and Patient Engagement/Need for Reassurance emerged.
Conclusion:
Post-discharge home visits by APRNs and paramedics working together were associated with reduced 30-day readmissions. Identified themes could inform strategies to improve patient support.
Keywords: Primary health care, Home care services, Hospital readmission
1. Introduction
Given significant financial penalties faced by hospitals for excess readmissions,1 strategies to reduce 30-day readmissions after hospitalization have been a focus of multiple types of interventions.2,3 Home visits after discharge may be an important component of post-discharge interventions that may reduce readmissions,4,5 may improve functional ability in older patients,6 or reduce unplanned readmissions.7 We aimed to study the association of home visits delivered after discharge by a novel combination of provider types and, using a mixed-methods approach, to also study contextual factors that may influence observed outcomes of the home visit implementation.
A post-discharge home visit program utilizing the skills of advances practice nurses (APRNs) who are independent practitioners, and paramedics who have expertise in responding to acute care, was implemented in Cleveland Clinic Health System (CCHS) primary care practices in May 2018. This program identified patients in all health system hospitals who had a CCHS primary care provider (PCP) and were determined to be at high risk for readmission based upon an internally validated CCHS readmissions risk calculator The risk calculator utilizes variables in the following categories:
Admission and discharge type, prior utilization, comorbidities, medication use, patient demographics, laboratory values, health literacy, and cognitive assessment and is applied at the time of hospital discharge. Those patients with a high risk score (≥40) were offered post-discharge home visits. In addition, patients could be directly referred to the home visit program by a primary care practice registered nurse care coordinator (RNCC) based upon subjective assessment of need for home visits. The goals of this study were to assess the association with health care utilization and mortality for patients at high risk for readmission who participated in the post-discharge home visit program and to examine provider and patient experience regarding program participation.
2. Methods
In the initial rollout phase (Phase 1, May–September 2018), the group of patients at high risk for readmission was offered 3 home visits by either an APRN or a paramedic based upon the geographical region of their residence. The health system primary care practice regions were divided into East and West which determined the paramedic or APRN assignment. The program was then modified to include an independent practitioner (APRN) on each home visit team in both East and West regions (Phase 2, effective October 2018). During this phase, patients were offered 4 home visits delivered by both APRNs and paramedics on different dates. Having an APRN on each team in the new model facilitated efficiency of completing any necessary orders that required sign off by an independent practitioner. Each home visit provider used a standardized template in the electronic medical record to document the home visit. The RNCC remained active with following their assigned patients by phone as part of usual team-based and transitional primary care for patients and was also the point of contact on the primary care team for the paramedic or APRN home visit provider.
Using a convergent, mixed methods design,8 we studied adult patients with a CCHS PCP discharged to home from a medicine service in the CCHS from November 2017–September 2019. The quantitative and qualitative data were mixed after completion of data collection.
2.1. Quantitative
Patients receiving home visits for 4 weeks after hospital discharge were matched to a comparison group of patients with a CCHS PCP discharged to home from a medicine service in the CCHS in the same period using coarsened exact matching (CEM). Patients who declined home visits were excluded from the comparison group. Patients were matched on age, gender, race, insurance, median income by zip code,9 both the internal CCHS readmission risk score and the HOSPITAL score for preventable readmissions,10,11 and number of admissions and primary care visits in 180 days prior to admission. Matching was performed using a 1:3 nearest neighbor matching without replacement within the CEM matched pairs. We chose one-to-many matching to increase precision in our cohort study and to allow smaller confidence intervals than one-to-one matching. Outcomes at 30, 90, and 180 days, including hospital admission, emergency department(ED) use, and death, were analyzed in two time periods - Phase 1, which represented the initial program structure, during which either an APRN or paramedic delivered home visits with assignment based upon the patient’s geographic location of residence, lasting 5 months, and Phase 2, the modified version and current model, where APRNs and paramedics both delivered visits to the same patient on different dates (Fig. 1), lasting 6 months of the study period. Results were compared using the Mann-Whitney U test and Chi-Square test. Mixed effects logistic regression models with receiving home visits as predictor were used to adjust outcomes for patients with multiple discharges. Patients declining home visits and those accepting were then also compared using mixed effects logistic regression adjusted for age, marital status, race, insurance, median income, the internal CCHS readmission risk score, the HOSPITAL score for preventable readmissions,10,11 and random effects to account for patients with multiple discharges. Analyses were performed using R software, (version 3.5.1).
Fig. 1.
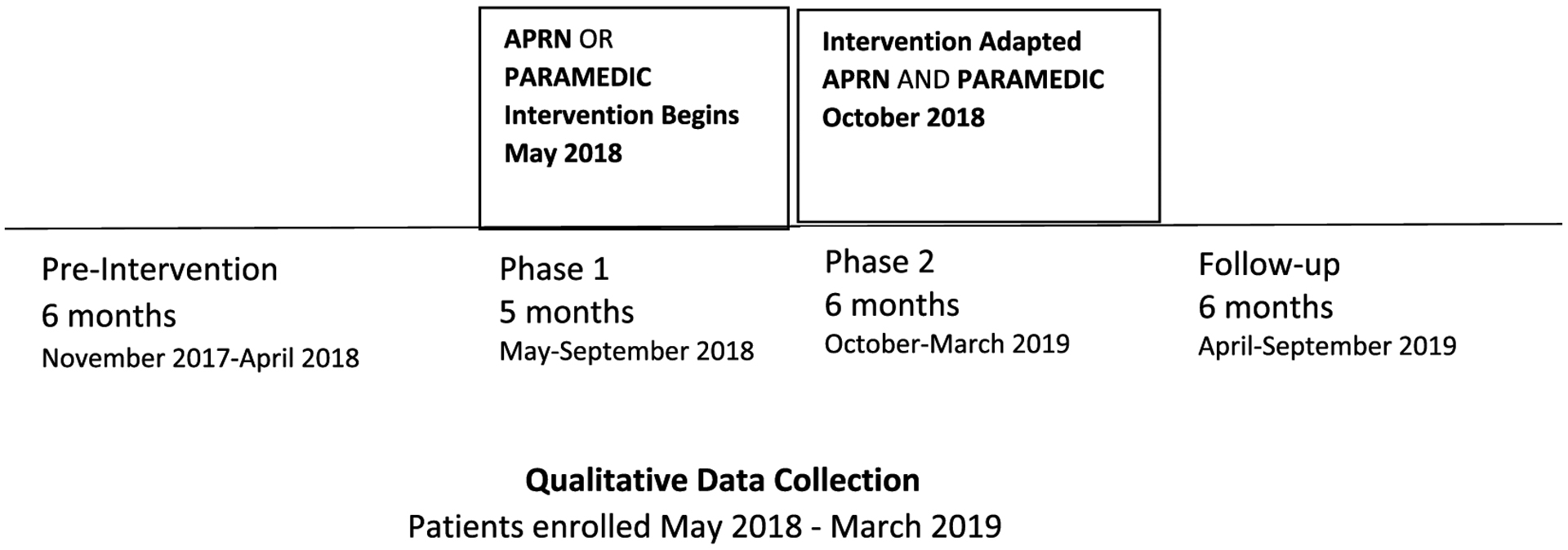
Study timeline.
2.2. Qualitative
Semi-structured audio recorded interviews were conducted with patients receiving home visits, APRNs, paramedics, PCPs, and primary care RNCC. After their participation in the home visit program, patients were approached for study participation by a research nurse (JF) and informed consent was obtained at a regularly scheduled PCP visit. Providers were recruited by email and included all paramedics and APRNs involved in delivering home visits, the PCPs of the patients who were recruited, and the RNCC at the sites where the patients received outpatient care. Interviews were conducted either over the phone or in person by a research nurse (JF) or medical student (AO) using interview guides; the patient interview guide was revised during the study based upon input from a previously assembled primary care patient stake-holder panel to improve clarity of the questions (Final versions, Appendix 1). Interviews were transcribed verbatim and transcripts coded by two research team members (AMH and AO) with regular meetings to discuss final coding. Then, using an editing and immersion/crystallization analysis of text,12,13 emergent themes were identified. Analyses were completed using NVivo software, Version 11.14 The full mixed methods study protocol was approved prior to data collection by the Institutional Review Board at Cleveland Clinic.
3. Results
3.1. Quantitative
For all of the patient discharges from a medicine service in our dataset, the 30-day readmission rate remained relatively stable during the 6 months pre-implementation and during the Phase 1 and Phase 2 home visit implementation periods, ranging from 17.0–17.6 %.
The baseline characteristics of the unmatched patient hospital discharges by home visit status during Phase 1 and 2 of program implementation are shown in Table 1. In both Phase I and Phase 2, compared to patients not receiving home visits, those receiving home visits were older (71 vs. 63 years Phase 1, 74 vs. 64 years Phase 2, p < 0.001), less likely to be of white race (58.4 vs. 70.1% Phase 1, 55.9 vs. 69.6% Phase 2, p < 0.001), had lower median income, both higher median CCHS readmission risk score and HOSPITAL score, were more likely to have Medicare insurance (71% vs. 36.2 % Phase 1, 78.1% vs. 50.8 % Phase 2, p < 0.001) and had more hospital admissions in the previous 180 days. The distribution of readmission risk scores for those participating in home visits is shown in Appendix 2.
Table 1.
Baseline characteristics of patient hospital discharges by home visit status in phase 1 and phase 2 of post-discharge home visit implementation.
| Phase 1 | Phase 2 | |||||
|---|---|---|---|---|---|---|
| No Home visit N(%) or Median [25/75 percentile] | Home Visit N(%) or Median [25/75 percentile] | p | Home visit = No | Home Visit = Yes | p | |
| Number of discharges | 29405 | 221 | 34426 | 247 | ||
| Age | 63 [48, 75] | 71 [62, 80] | <0.001 | 64 [49, 75] | 74 [64, 82] | <0.001 |
| Gender = Male | 12258 (41.7) | 99 (44.8) | 0.387 | 14569 (42.3) | 98 (39.7) | 0.439 |
| Race | <0.001 | <0.001 | ||||
| White | 20604 (70.1) | 129 (58.4) | 23944 (69.6) | 138 (55.9) | ||
| Black | 7060 (24.0) | 65 (29.4) | 8363 (24.3) | 95 (38.5) | ||
| Other/Unknown | 1741 (5.9) | 27 (12.2) | 2119 (6.2) | 14 (5.7) | ||
| Median Income(thousands of dollars) | 52230 [37958, 68130] | 47163 [32090, 66612] | 0.021 | 52230 [37958, 68130] | 50715 [32357, 66612] | 0.034 |
| Readmission Score | 14 [8, 21] | 36 [25, 43] | <0.001 | 14 [9, 21] | 31 [23, 41] | <0.001 |
| HOSPITAL Score | 3 [2, 4] | 5 [4, 7] | <0.001 | 3 [2, 4] | 5 [3, 7] | <0.001 |
| Insurance | <0.001 | <0.001 | ||||
| Commercial | 6392 (21.7) | 16 (7.2) | 9862 (28.6) | 14 (5.7) | ||
| Medicaid | 3082 (10.5) | 17 (7.7) | 4853 (14.1) | 26 (10.5) | ||
| Medicare | 10642 (36.2) | 157 (71.0) | 17489 (50.8) | 193 (78.1) | ||
| Other | 9289 (31.6) | 31 (14.0) | 2222 (6.5) | 14 (5.7) | ||
| During 180 days prior to index Admission | ||||||
| Number of Admissions | 0 [0, 0] | 1 [0, 2] | <0.001 | 0 [0, 0] | 0 [0, 1] | <0.001 |
| Number of Admissions Mean (Standard Deviation) | 0.3 (0.8) | 1.0 (1.5) | <0.001 | 0.3 (0.8) | 0.9 (1.3) | <0.001 |
| Number of Primary Care Visits | 0 [0, 1] | 0 [0, 1] | 0.021 | 0 [0, 1] | 0 [0, 0] | <0.001 |
| Number of Primary Care Visits Mean (Standard Deviation) | 0.8 (1.4) | 0.8 (1.6) | 0.97 | 0.8 (1.3) | 0.7 (1.6) | 0.264 |
For the analysis during Phase 1 Implementation, 101 discharges participating in home visits were matched to 303 discharges not participating in home visits (excluding those who were offered and declined home visits). In Phase 2, 157 home visit discharges were matched to 471 no home visit discharges (Table 2). The home visit and comparison groups were well-matched on the chosen variables. Of note, the range of CCHS readmission risk scores were 0–77 for the matched home visit discharges and 0–80 for the matched comparison group, with 40 used as the cut-off for high risk for readmission. Outcomes from the initial 5 month home visit implementation model showed a lower percentage of 30 day readmissions in the home visit group compared to the no home visit group (22.8 % vs. 29.7%) but this was not statistically significant (p = 0.224). There were also no significant differences in the proportion of patients who were readmitted to hospital at 90 or 180 days, number of readmissions within 180 days, ED visits at 90 or 180 days or mortality at 90 or 180 days (Table 3).
Table 2.
Matched patient hospital discharges (no home visit and home visit) in phase 1 and phase 2 of post-discharge home visit implementation.
| Phase 1 | Phase 2 | |||||
|---|---|---|---|---|---|---|
| No Home Visit N(%) or Median[25/75 percentile] | Home Visit N(%) or Median[25/75 percentile] | p-value | No Home Visit N(%) or Median[25/75 percentile] | Home Visit N(%) or Median[25/75 percentile] | p-value | |
| Number of discharges | 303 | 101 | 471 | 157 | ||
| Age | 73.6 [65.0, 80.8] | 74.0 [65.1, 81.4] | 0.878 | 75.2 [68.2, 83.4] | 75.9 [68.6, 82.7] | 0.729 |
| Gender = Male | 108 (35.6) | 36 (35.6) | 1 | 195 (41.4) | 65 (41.4) | 1 |
| Race | 1 | 1 | ||||
| White | 201 (66.3) | 67 (66.3) | 291 (61.8) | 97 (61.8) | ||
| Black | 96 (31.7) | 32 (31.7) | 174 (36.9) | 58 (36.9) | ||
| Other/Unknown | 6 (2.0) | 2 (2.0) | 6 (1.3) | 2 (1.3) | ||
| Median Income(thousands of dollars) | 47.2 [32.4, 67.1] | 50.9 [32.7, 68.1] | 0.459 | 51.8 [34.5, 68.8] | 53.6 [37.0, 72.2] | 0.396 |
| Readmission Score | 32.0 [21.0, 40.0] | 32.0 [21.0, 42.0] | 0.629 | 28.0 [20.0, 39.0] | 28.0 [20.0, 39.0] | 0.989 |
| HOSPITAL Score | 5.0 [4.0, 7.0] | 5.0 [4.0, 7.0] | 0.72 | 5.0 [3.0, 7.0] | 5.0 [3.0, 7.0] | 0.913 |
| Insurance | 1 | 1 | ||||
| Commercial | 9 (3.0) | 3 (3.0) | 6 (1.3) | 2 (1.3) | ||
| Medicaid | 6 (2.0) | 2 (2.0) | 15 (3.2) | 5 (3.2) | ||
| Medicare | 234 (77.2) | 78 (77.2) | 438 (93.0) | 146 (93.0) | ||
| Other | 54 (17.8) | 18 (17.8) | 12 (2.5) | 4 (2.5) | ||
| During 180 days prior to index Admission | ||||||
| Number of Admissions | 0.0 [0.0, 1.0] | 0.0 [0.0, 1.0] | 1 | 0.0 [0.0, 1.0] | 0.0 [0.0, 1.0] | 0.152 |
| Number of Admissions Mean (Standard Deviation) | 0.6 (0.7) | 0.6 (0.7) | 1.0 | 0.5 (0.8) | 0.6 (0.9) | |
| Number of Primary Care Visits | 0.0 [0.0, 0.0] | 0.0 [0.0, 1.0] | 0.244 | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.313 |
| Number of Primary Care Visits Mean (Standard Deviation) | 0.4 (1.0) | 0.5 (1.1) | 0.38 | 0.5 (1.1) | 0.4 (1.2) | 0.78 |
Table 3.
Six-month outcomes of matched discharges (no home visit and home visit) in phase 1 and phase 2 of post-discharge home visit implementation.
| Phase 1 | Phase 2 | |||||
|---|---|---|---|---|---|---|
| Non Home Visit N (%) or Median [25/75 percentile] | Home Visit N (%) or Median [25/75 percentile] | p-value | Non Home Visit N (%) or Median [25/75 percentile] | Home Visit N (%) or Median [25/75 percentile] | p-value | |
| Readmission in 30 Days | 90 (29.7) | 23 (22.8) | 0.224 | 135 (28.7) | 30 (19.1) | 0.024 |
| Readmission in 90 Days | 158 (52.1) | 57 (56.4) | 0.527 | 223 (47.3) | 63 (40.1) | 0.139 |
| Readmission in 180 days | 204 (67.3) | 66 (65.3) | 0.807 | 288 (61.1) | 95 (60.5) | 0.962 |
| Number of Readmission in 180 Days | 1.0 [0.0, 3.0] | 1.0 [0.0, 2.0] | 0.577 | 1.0 [0.0, 2.0] | 1.0 [0.0, 2.0] | 0.67 |
| Emergency Departments Visit in 90 days | 91 (30.0) | 29 (28.7) | 0.9 | 114 (24.2) | 44 (28.0) | 0.396 |
| Emergency Department Visits in 180 days | 129 (42.6) | 44 (43.6) | 0.954 | 168 (35.7) | 66 (42.0) | 0.182 |
| Number of Emergency Department Visits in 180 days | 0.0 [0.0, 1.0] | 0.0 [0.0, 1.0] | 0.819 | 0.0 [0.0, 1.0] | 0.0 [0.0, 1.0] | 0.164 |
| Death in 90 days | 91 (30.0) | 29 (28.7) | 0.9 | 29 (6.2) | 10 (6.4) | 1 |
| Death in 180 days | 129 (42.6) | 44 (43.6) | 0.954 | 49 (10.4) | 21 (13.4) | 0.38 |
During Phase 2 implementation, the proportion experiencing 30-day readmission was significantly lower in the home visit group vs. no home visit group (19.1 vs. 28.7%, p 0.024) with no significant differences in the proportion readmitted at 90 or 180 days, number of readmissions within 180 days, ED visits at 90 or 180 days or mortality at 90 or 180 days (Table 3).
The models adjusting for multiple discharges for the same patient confirmed no significant association of home visits with the outcomes in Phase 1 and significant association of home visits with 30 day readmissions only in Phase 2(Odds ratio(OR) 0.910, 95% Confidence Interval(CI) 0.841 to 0.984, p = 0.019). Additionally, a subgroup analysis for the matched home visit compared to no home visit groups by race category showed no significant differences in outcomes by white vs. non-white subgroups (Appendix 3).
Patients who were offered home visits and declined were different from those patients who accepted the home visits (Appendix 4). In Phase 1, there were 223 patients who were offered and declined home visits while 221 patients accepted (50% uptake) while in Phase 2 there were 339 patients who declined and 247 patients who accepted (42% uptake). The documented reasons for declining selected from specific options included “does not need any additional help” (50.2 % Phase 1, 64.9% Phase 2), “too many caregivers in the home”(20.6% Phase 1, 13.6% Phase 2), “has caregiver who is knowledgeable” (11.2% Phase 1, 5.6% Phase 2), “back to work”(0.9% Phase 1, 2.1% Phase 2) and more than 1 reason(17% Phase 1, 13.3% Phase 2). In Phase 1, those accepting home visits were less likely to be married (33.9% vs. 47.5%, p 0.019), less likely to be of white race (58.4% vs. 75.3%, p < 0.001), had lower median income(47,163 vs. 59,553 dollars, p < 0.001) had a higher median CCHS readmission risk score (36 vs. 31, p 0.015), were more likely to have Medicare (71% vs. 56.1%) or Medicaid (7.7 vs 4.0%) insurance (p < 0.001). In Phase 2, those patients accepting home visits were older (73.7 vs. 69.6, p0.014), less likely to be married (34.8% vs. 46.6%, p 0.015), less likely to be of white race (55.9 vs 69.6%, p 0.002), and more likely to have Medicare (78.1 vs. 75.5%) or Medicaid (10.5 vs. 7.4%) insurance, p 0.008.
After adjusting for age, marital status, race, insurance, median income, the CCHS readmission risk score, the HOSPITAL score for preventable readmissions,10,11 and random effects to account for patients with multiple discharges, patients who were offered home visits and accepted vs. those who declined had lower odds of 30 day readmissions during both Phase 1 and Phase 2 of implementation (OR = 0.886, CI 0.808 to 0.971, p = 0.010 for Phase I and OR 0.884 95% CI 0.820 to 0.953, p = 0.001 for Phase 2), and also lower odds of 90 and 180 day readmission in Phase 2 (OR 0.913, CI 0.843–0.989, p 0.026 for 90 days, OR 0.911, CI 0.847–0.980, p 0.013 for 180 days). (Appendix 5).There were no significant differences in ED use or mortality.
3.2. Qualitative
Forty-four interviews were conducted including 22 patients, 7 RNCC, 9 PCPs, 3 paramedics and 3 APRNs. Five major themes emerged from the data: 1) Medication Understanding 2) Knowledge Gap After Discharge including issues with health literacy and need for education, 3) Patient Medical Complexity 4)Social Context including financial barriers and need for social support, and 5) Patient Engagement/Need for Reassurance after discharge.
3.2.1. Medication Understanding
A consistent theme across patient and provider interviews pointed to a lack of patient understanding about prescribed medications after hospital discharge. For example, an APRN who performed home visits stated,
“A lot of times you find that they didn’t pick up a prescription or they didn’t know it was decreased or increased,’
Or as a patient receiving home visits remarked,
“…she helped with my issues with my medicine. Because I didn’t know … what was for what.”
Another patient stated the following about a home visit provider:
“Well, once he was here and I had a real bad cough. And he told me what to do. He was the one that told me using my inhaler… I didn’t know that’d help or stop that. And it did…”
Primary care providers and RNCC echoed similar sentiments:
PCP: “… I think that that is excellent that they get a look at their home environment, make sure they have their meds…I think that is closing a huge loop that we really have never been able to do before”
RNCC: “I think the biggest thing I think that has been helpful with them is that a lot of time medications might have maybe some misunderstandings or there might be even some errors going home from the hospital or some confusion.”
3.2.2. Knowledge gap after discharge
In addition to a gap in understanding related to medications, the data revealed an overall knowledge gap about recommendations after discharge. As a patient stated,
“I’m still having to be educated on what to do and how to do it because it’s not easy.”
As noted below, a PCP identified a knowledge gap as a barrier for patients,
“It’s just that the patients really need a better transitional plan that they can reference and … And so I feel like the – they’re discharged with too many things to understand. It overwhelms them and then they get a lot of things going on at home”
And an RNCC remarked,
“So sometimes it’s just lack of understanding. Education. So there’s that health literacy issue of understanding why you should do the things that you’re supposed to do, to keep you from going back to the hospital. Or understanding the services we have, the options we have, for express care.”
A paramedic performing home visits observed,
“Either they were so overwhelmed with the amount of information that was being given to them at the time of discharge, they didn’t fully understand it … when they got home or they just didn’t absorb all the information that was being given to them because it was too much.”
3.2.3. Patient Medical Complexity
The group of patients offered home visits are medically complex and the medical issues were a significant barrier to remaining at home. As a PCP remarked about the program,
“I think that the success of those has been somewhat variable, based partly on unpredictable patient characteristics.”
Another PCP stated,
“The support needed for those really sick-sick patients to get them their meds, to assist them with their daily needs and then just to feed them. I mean you’re talking food, water even. Just to be able to hydrate them and get their medicines in in a timely fashion. They’re exhausted.”
A paramedic commented on a specific patient, “…a patient with some ETOH (alcohol) abuse. And so I don’t know how much help she was getting with that piece of the puzzle.”
An RNCC reflected on patients’ acceptance of home visits:
“So, people try to set up services for patients and oftentimes, patients will refuse because they don’t think they need them or they’re in a hurry to get out of the hospital. And they don’t understand the discharge instructions. So, having – having the advanced practice nurse and the paramedic in the home provides that safety net, so to speak, for the patient, when they realize they did need – they did need that extra touch, they did need that professional assessment.”
3.2.4. Social Context
Patients in the home visit program had significant social needs. An APRN commented,
“I would say social and, you know – social – lack of social support and medical illiteracy are probably the two things that I would worry the most about.”
Or as another APRN comment notes,
“… if a patient, the family, you know, they don’t have the funds to maybe have the assistance that they need in the home. You know, like home health aides or something like that. And they don’t have the money to be able to pay for it. Which is, you know, happens a lot…”
An RNCC noted,
“Some of the barriers are financial. Where maybe they don’t have the proper nutrition. They don’t have support from family or friends. They can’t drive. They don’t drive. They have transportation issues. We deal with medication issues and getting to the pharmacy to get medications.”
A PCP provided the following insight:
“I think that the overarching presence or absence of family support is probably the key issue. Because those who have one or more people who are able to give them additional family support, I think do better regardless. And the addition of high-risk transition services probably helps those people more, who have those family resources, than those who don’t.”
3.2.5. Patient Engagement/Need for Reassurance
Patients valued post-discharge home visits as the visiting staff gave them reassurance and improved their engagement with their health.
A patient commented,
“I had, you know, new things going on with the dialysis…And it was all new to me. It was a little scary. And they kind of helped me through all that.”
Or as another patient stated,
“Because knowing that she’s coming out, one, makes me feel better because it lets me – when she gets through checking me, I’ll know whether or not I need to go back to the hospital or I’m doing just fine. And because she’s coming, I get up and I’ll straighten up the house. Because I live with my granddaughter. So I’ll straighten up the house a little and that – that’s helping me, you know.”
A patient referring to a home visit remarked,
“I mean, he would – just sitting there talking to him, it wasn’t like talking to a paramedic. It was talking to another person, you know. “
Please see additional supporting quotations by theme in Appendix 6.
4. Discussion
In this retrospective mixed methods evaluation of a post-discharge home visit program for patients at increased risk for readmissions, we found that patients receiving weekly home visits from an APRN and paramedic teams for the month after hospital discharge (Phase 2 model) had fewer hospital readmissions at 30 days compared to a matched group of patients not receiving home visits. There was no significant difference in readmissions at 90 or 180 days, ED visits, or mortality. Patients who were offered and accepted home visits were different from those who declined but, in analyses adjusting for baseline differences, those who were offered and accepted the home visits had lower odds of 30 day readmissions, suggesting patient factors leading to program acceptance may be protective for readmission as these effects were seen in Phase 2 for 30, as well as 90 and 180 days. The qualitative analyses including patients who accepted and received home visits added further clarification regarding potential issues for this group that may be contributing to their risk for hospital readmission, including medication understanding, knowledge gap after discharge, medical complexity, social context, engagement and need for reassurance.
While choosing interventions to prevent 30 day readmissions based upon risk for readmission seem promising,15 the longer term effect (after 30 days) on hospital readmissions may not be observed.16 The concepts of need for improved information for patients after hospital discharge17,18 and confidence after discharge18 have been previously identified through qualitative work. Our work highlighted the need for information, but specifically about prescribed medications, after discharge. This need was identified and observed at the home, after the medication reconciliation was performed in the hospital at the time of discharge, demonstrating the value of home visits to address this significant lack of understanding.
Providing education and reinforcement for following recommendations after discharge in the environment at home, when the patient may be less overwhelmed with information, may be an effective approach, as the standard of care may be to wait until the next face to face post-discharge primary care office visit to reinforce these instructions. While primary care based RNCC are able to offer telephone follow-up post –discharge and on an ongoing basis, patients appreciated that the home visits provided more help for the patient or “that extra touch.” A significant difference was only observed in Phase 2 of the program, which was modified from the initial phase to include an additional visit after discharge (4 vs. 3 visits) but also to include an APRN on each team who could serve as an independent practitioner. While we were not able to assess fidelity of the delivery of each intended visit, our findings suggest that frequency of visits may be a driver of success of the program. This is further supported by the fact that readmissions were not reduced once the home visits ended suggesting that even greater frequency and longer term home visit support may be necessary to keep patients out of the hospital.
The overall medical complexity of this group of patients and the social context makes any health system-based intervention to improve readmission risk in this group challenging. However, the patients appreciated the program as having someone visit the home gave them a sense of reassurance. Indeed multicomponent transitional care programs are needed19 but home visits may be a critical component of these interventions.5 While the Phase 2 team composition of APRNs who can serve as independent practitioners in making treatment decision and paramedics who are trained to address acute care seems ideal, one of the components of the Ideal Transition in Care model20 includes social and community supports. For example, a previous novel transitional care initiative utilizing paramedics and a social worker/social care coordinator team that provided in home assessments and support was associated with lower inpatient utilization.21 Future work should also explore how community-based resources, such as lay health workers22 may be utilized at least to provide the sense of reassurance for patients, and could potentially also be trained to provide diagnosis-specific ongoing support after the initial post-hospital discharge phase.
Exploring reasons for non-acceptance of the home visit program will be imperative for future implementation to determine if modifiable factors exist. As at least 50% of patients offered home visits chose “does not need additional help” as a reason for declining the program, perhaps patient insight into needs after discharge are not as clear immediately following discharge when the program is offered, so timing of the offering may need to be considered. Alternatively, patients may require further explanation of program benefits based upon patient experiences captured through our work.
While our health system is composed of diverse practices and hospitals, our study involves a single health system, thus it is possible that our findings may not be generalizable to other health systems or regions. Our retrospective design has additional limitations which we have worked to mitigate in our analyses. First, similar to an intention to treat design, we assigned patients to the home visit group and to Phase 1 and Phase 2 of the program implementation based upon the date of the first home visit to capture outcomes from the planned evolution of the program as we were unable to capture fidelity to visit count or content of visits. We chose to analyze the program in the 2 phases to more accurately assess the effects of the paramedic/APRN team when the program was modified. Second, given the baseline differences in the home visit vs. no home visit group, to assess the effect of the home visit program, we matched the home visit patients to a comparison group on variables that may have an effect on our outcomes, and utilized both our internally validated readmission risk score but also the published HOSPITALscore10,11 as matching variables. However, we believe the interpretation of our quantitative results is strengthened by our mixed methods approach which allowed important contextual factors around the transition of care from hospital to home to emerge and to suggest the need for targeted solutions to improve the post-discharge experience-such as a focus on medication understanding at home.
In conclusion, a post discharge home visit program by APRNs and paramedics working together offered to patients at higher risk for hospital readmission was associated with lower 30-day readmissions. Home-based interventions with a focus on medication education and improving understanding of recommendations after discharge, as well as providing social support may hold promise for medically complex patients. Strategies to improve uptake and acceptance of home visit programs may further improve outcomes at the population level.
Supplementary Material
Funding source
Dr. Misra-Hebert receives funding from the Agency for Healthcare Research and Quality grant # K08HS024128. The Agency for Healthcare Research and Quality had no role in the study design, conduct, or reporting.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Dr. Misra-Hebert reports grants from NHLBI, grants from Novo Nordisk, Inc, grants from Merck Inc., grants from Boehringer Ingelheim Pharmaceuticals, Inc, outside the submitted work. Mr. Milinovich reports grants from NovoNordisk, Inc, grants from Merck, Inc., grants from Novartis, and grants from Boehringer Ingelheim Pharmaceuticals, Inc, outside the submitted work.
Footnotes
Appendix A. Supplementary data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.hjdsi.2020.100518.
References
- 1.Medicare C for, baltimore MS 7500 SB, Usa M. Readmissions-Reduction-Program. Published January 16, 2019. Accessed January 23, 2019 https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html.
- 2.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic Review. Ann Intern Med. 2011;155(8):520. 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 3.McWilliams A, Roberge J, Anderson WE, et al. Aiming to improve readmissions through InteGrated hospital transitions (AIRTIGHT): a pragmatic randomized controlled trial. J Gen Intern Med. 2019;34(1):58–64. 10.1007/s11606-018-4617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281 (7):613–620. 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 5.Jackson C, Kasper EW, Williams C, DuBard CA. Incremental benefit of a home visit following discharge for patients with multiple chronic conditions receiving transitional care. Popul Health Manag. 2016;19(3):163–170. 10.1089/pop.2015.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avlund K, Jepsen E, Vass M, Lundemark H. Effects of comprehensive follow-up home visits after hospitalization on functional ability and readmissions among old patients. A randomized controlled study. Scand J Occup Ther. 2002;9(1):17–22. 10.1080/110381202753505827. [DOI] [Google Scholar]
- 7.Stewart S, Horowitz JD. Home-based intervention in congestive heart failure: long-term implications on readmission and survival. Circulation. 2002;105(24): 2861–2866. 10.1161/01.CIR.0000019067.99013.67. [DOI] [PubMed] [Google Scholar]
- 8.Creswell J Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Fourth. Sage Publications, Inc.; 2014. Accessed May 2, 2016 https://us.sagepub.com/en-us/nam/research-design/book237357. [Google Scholar]
- 9.Bureau UC. American community survey (ACS). Accessed October 31, 2019 https://www.census.gov/programs-surveys/acs.
- 10.Donźe JD, Williams MV, Robinson EJ, et al. International validity of the “HOSPITAL” score to predict 30-day potentially avoidable readmissions in medical patients. JAMA Int Med. 2016;176(4):496–502. 10.1001/jamainternmed.2015.8462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donźe J, Aujesky D, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Int Med. 2013;173(8):632–638. 10.1001/jamainternmed.2013.3023. [DOI] [PubMed] [Google Scholar]
- 12.Addison RB. Chapter 8: a grounded hermeneutic editing approach. In: Crabtree BF, Miller WL, eds. Doing Qualitative Research. Sage Publications, Inc.; 1999:145–161. [Google Scholar]
- 13.Borkan J Chapter 10: immersion/crystallization. In: Crabtree BF, Miller WL, eds. Doing Qualitative Research. Sage Publications, Inc.; 1999:179–194. [Google Scholar]
- 14.NVivo Qualitative Data Analysis Software; Version 11. QSR International Pty Ltd.; 2015. [Google Scholar]
- 15.Hoyer EH, Brotman DJ, Apfel A, et al. Improving outcomes after hospitalization: a prospective observational multicenter evaluation of care coordination strategies for reducing 30-day readmissions to Maryland hospitals. J Gen Intern Med. 2018;33(5): 621–627. 10.1007/s11606-017-4218-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finkelstein A, Zhou A, Taubman S, Doyle J. Health care hotspotting — a randomized, controlled trial. N Engl J Med. 2020;382(2):152–162. 10.1056/NEJMsa1906848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berendsen AJ, de Jong GM, Meyboom-de Jong B, Dekker JH, Schuling J. Transition of care: experiences and preferences of patients across the primary/secondary interface – a qualitative study. BMC Health Serv Res. 2009;9:62. 10.1186/1472-6963-9-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solan LG, Beck AF, Brunswick SA, et al. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136(6):e1539–e1549. 10.1542/peds.2015-2098. [DOI] [PubMed] [Google Scholar]
- 19.Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission: current strategies and future directions. Annu Rev Med. 2014;65:471–485. 10.1146/annurev-med-022613-090415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burke RE, Kripalani S, Vasilevskis EE, Schnipper JL. Moving beyond readmission penalties: creating an ideal process to improve transitional care. J Hosp Med Off Publ Soc Hosp Med. 2013;8(2):102–109. 10.1002/jhm.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siddle J, Pang PS, Weaver C, et al. Mobile integrated health to reduce post-discharge acute care visits: a pilot study. Am J Emerg Med. 2018;36(5):843–845. 10.1016/j.ajem.2017.12.064. [DOI] [PubMed] [Google Scholar]
- 22.Cardarelli R, Horsley M, Ray L, et al. Reducing 30-day readmission rates in a high-risk population using a lay-health worker model in Appalachia Kentucky. Health Educ Res. 2018;33(1):73–80. 10.1093/her/cyx064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


