Abstract
BACKGROUND:
Delay in seeking medical help in patients with acute myocardial infarction (AMI) challenges the patients in terms of diagnosis and treatment. This study aimed to evaluate the outcomes of delay referral (≥12 h) in patients with AMI.
MATERIALS AND METHODS:
In this retrospective cohort study, the medical records of 252 patients with AMI (2017–2019) admitted to Shahid Beheshti Hospital, Qom, Iran, was reviewed. Data collection tool was a researcher-made data sheet that included demographic characteristics, times, hospitalization costs, risk factors, history of heart disease, results of paraclinical tests, clinical information at the time of admission, and outcomes of delayed referral. Data were analyzed using t-test, Chi-square, Kaplan–Meier estimator, log-rank test, Cox regression by STATA, and SPSS (version 25).
RESULTS:
The levels of troponin, creatine phosphokinase, lactate dehydrogenase were significantly higher in the delayed referral group (P < 0.05). After treatment, the cardiac ejection fraction was significantly different in the nondelayed referral (41.56 ± 9.16) and the delayed referral group (38.39 ± 11.01) (P < 0.001). There was no significant difference in the percentage of hospital deaths in the groups (P = 0.078).
CONCLUSION:
Delayed referral of patients with AMI is associated with decreased physiological cardiac function, which complicates recovery for these patients.
Keywords: Delay, in-hospital mortality, myocardial infarction, outcome, ST-segment elevation myocardial infarction, survival
Introduction
Today, noncommunicable diseases included 43% burden of all diseases[1] and cardiovascular diseases are the leading causes of death globally; causing 17 million deaths per year. About half of all deaths from cardiovascular disease are due to ischemic heart disease,[2] Among ischemic heart diseases, acute myocardial infarction (AMI) is the leading cause of death.[3] AMI is the most common coronary artery disease, accounting for 2–4 million deaths annually in the United States and more than 4 million deaths in Europe and north Asia.[4]
In the management of AMI, delay in seeking treatment after the onset of symptoms can severely affect the patient's prognosis. Patient delay is a combination of delay in decision time to seek treatment and time delay in transportation to hospitalization. Decision time delay is described as the longest interval of delay.[5] Data show that immediate treatment after the onset of symptoms of AMI reduces the extent of ischemia and the risk of death.[6,7] Therefore, reducing the delay in starting standard treatments such as reperfusion therapy is a critical strategy to increase the success rate of treatment in AMI.[8]
Although in AMI the acceptable time interval between the onset of symptoms and treatment is <60 min, evidence suggests that prehospital delay are still 2–4 h, greatly reducing the effectiveness of treatment interventions. A study in Iran shows that 75% of patients had prodromal symptoms 2 weeks before the onset of myocardial infarction, and interestingly, the average delay in referring time was even higher in these group patients.[9] Xie et al. showed elderly, female gender and patients with a history of diabetes, hypertension, or angina pectoris have been associated with a longer prehospital delay. Furthermore, time when the symptoms occur, location where symptoms occur, and whether there is a bystander when the symptoms occur were recognized as contextual factors resulted in a longer delay to treatment in patients with AMI. This is while cognitive, affective, and behavioral factors are presented as influencing factors in delayed referral.[10]
Balk et al. suggest it is not a surprise for delay primary angioplasty in patients with myocardial infarction when there are delays in contacting medical and transport services, obtaining authorization from the emergency departments for ambulance and increased transport time due to travel distance.[11] Therefore, timely referral can improve the prognosis and may be the only way to save lives of patients with acute myocardial.[12] Some studies have suggested a delay of 6 h from the onset of symptoms of AMI.[13,14,15] In any case, there are studies that consider 12 h from the onset of symptoms as a time frame for deciding to reperfusion treatment.[16,17] Known Outcomes of delay in referral in AMI patients include heart failure, increased length of stay, decreased treatment benefits, expansion of cardiac ischemia, and death.[16,18] In Iranian patients with AMI, there is not enough information to clearly show the outcomes of delay in referral. The current knowledge has focused to identify factors contributing to the prehospital delay, causes of late referral to the emergency department.[19,20]
There are studies that show some of the outcomes of delay, such as delay in drug administration for AMI patients. Therefore, in an attempt to identify different dimensions of the effect of delay on patients’ outcomes, this study evaluates the outcomes of delay referral in patients with AMI.
Materials and Methods
Study design and setting
The present retrospective cohort study was conducted in Shahid Beheshti educational hospital affiliated to Qom University of medical sciences, 2019–2020.
Study participants and sampling
In this study, medical records of patients with a diagnosis of AMI admitted to Shahid Beheshti educational hospital from March 2017 to March 2019 were assessed. Sampling was used as the Census method. According to the study of McNair et al., Type I error = 5%, and the 80% power, 118 people were calculated for each group (delayed referral and nondelayed referral). The diagnosis of AMI was based on cardiac biomarkers (creatine phosphokinase [CPK], CKMB, lactate dehydrogenase [LDH] troponin I) and specific ECG changes to confirm AMI. In the time interval in this study, 541 patients with CVD were admitted to Shahid Beheshti Educational and Medical Center, and a total of 252 patients had the inclusion criteria. Inclusion criteria were completeness of patients’ medical records, the possibility of following up patients in terms of 1-year survival through contact, and patients with Iranian nationality. Nonresponsive patients or lack of access to follow-up on patients’ survival information were considered as exclusion criteria
Delay in referral means ≥12 h from the onset of symptoms to hospital admission and initiating appropriate treatment. The duration of the patient's referral was determined based on the patient's history, interview with the patient, or his family. Patients who presented <12 h after the onset of symptoms were in the nondelayed referral group and patients who presented 12 h or more after the onset of symptoms were in the delayed referral group. Finally, 119 patients were assigned in the delayed referral group and 133 people were considered in the nondelayed referral group.
Data collection tool and technique
Researcher-made datasheet consists of questions about demographic-social characteristics (age, sex, marital status, educational status, income level, insurance status), referral time, death time, discharge time, referral time of hospitalization, hospitalization costs, risk factors (hyperlipidemia, hypertension, diabetes, smoking), opium use, dysrhythmia, history of heart disease (myocardial infarction in patients or family), paraclinical test results (troponin, CPK, LDH), clinical information on entry (ejection fraction [EF], systolic blood pressure [SBP], diastolic blood pressure [DBP]) and outcomes (EF, survival status, survival period). These data were extracted from the patients’ medical records. Survival information was also recorded by telephone contact with the patient or his/her family. The data collection form was designed based on the study of similar researches and finalized according to the opinions of the research team.
After obtaining the code of ethics (IR.MUQ.REC.1399.102) from the Ethics Committee in research and obtaining an introduction letter from research deputy of Qom University of Medical Sciences, the researcher presented in the research setting. With the permission of the hospital management, the researcher presented in the medical records unit to study patients’ medical records and browsing the necessary information in the hospital information system (HIS). The extracted information was recorded in the relevant form every day. The researcher made a phone call to the patient or family member to complete the information, and after explaining the objectives of the study and emphasizing the confidentiality of the information, asked them to retell the required information.
Data were analyzed using t-test, Chi-square, Kaplan–Meier estimator, log-rank test, Cox regression by STATA (Statacorp. 2021. Stata Statistical Software: Release 17. College Station, TX: Statacorp LLC) and SPSS (IBM SPSS Statistics for windows, version 25.0 Armonk, NY: IBM Corp). The significance level is considered less than 0.05.
Ethical consideration
Ethical considerations were observed regarding telephone contact with the patient and his families. Since the information was retrospectively extracted from patients’ records, verbal consent was obtained from the patient and his companions during the telephone call, and the necessary information was given to them in the field of research. In addition, cooperation and sincere interaction with the medical records unit and not interfering with their duties, and assuring participants to keep personal information confidential and anonymity were considered.
Results
In the present study, 252 patients admitted with a diagnosis of AMI were included in the study. 119 patients (47.2%) were in the delayed referral group and 133 patients (52.8%) were in the nondelayed referral group. Most of the patients were male (64.7%) with a mean age of 64.15 ± 13.03 years. Statistical comparison of patients’ demographic-social characteristics did not show a statistically significant difference between the two groups (P > 0.05) [Table 1].
Table 1.
Comparison of demographicsocial characteristics of patients in the delayed referral group and the nondelayed referral group
| Variable | Referral time | P | |
|---|---|---|---|
|
| |||
| <12 h (n=133), n (%) | ≥12 h (n=119), n (%) | ||
| Age (years)* | 63.85±12.26 | 64.46±13.80 | 0.713 |
| Gender | |||
| Man | 86 (64.7) | 77 (64.7) | 0.994 |
| Female | 47 (35.3) | 42 (35.3) | |
| Marital status | |||
| Married | 106 (79.7) | 93 (78.2) | 0.113 |
| Single | 1 (0.8) | 4 (3.4) | |
| Divorced | 0 | 3 (2.5) | |
| Widowed | 26 (19.5) | 19 (16) | |
| Educational status | |||
| Illiterate | 61 (45.9) | 68 (57.1) | 0.062 |
| High school | 45 (33.8) | 40 (33.6) | |
| Diploma and postdiploma | 23 (17.3) | 8 (6.7) | |
| Bachelor’s degree and higher | 4 (3) | 3 (2.5) | |
| Family income | |||
| Good | 9 (6.8) | 7 (5.9) | 0.074 |
| Medium | 53 (39.8) | 32 (26.9) 2 | |
| Weak | 71 (53.4) | 80 (67.2) | |
| How to refer | |||
| By personal vehicle | 77 (57.9) | 71 (59.7) | 0.823 |
| By ambulance | 43 (32.3) | 39 (32.8) | |
| Referrals from other centers | 13 (9.8) | 9 (7.5) | |
| Referral day | |||
| Normal day | 107 (80.5) | 95 (79.8) | 0.902 |
| Holiday | 26 (19.5) | 24 (20.2) | |
| Referral time | |||
| Day | 87 (65.4) | 67 (56.3) | 0.139 |
| Night | 46 (34.6) | 52 (43.7) | |
*Mean and SD. SD=Standard deviation
The main underlying diseases among patients with AMI were hypertension (50.8%), diabetes (34.5%), and dyslipidemia (32.9%). History of smoking and opium use, history of dysrhythmia, and heart disease in the individual, and his family were examined as other related factors. The difference between these characteristics between the two groups was not statistically significant [Table 2].
Table 2.
Information about the underlying disease and risk factors in the delayed referral group, and the nondelayed referral group
| Variable | Referral time | P | |
|---|---|---|---|
|
| |||
| <12 h (n=133), n (%) | ≥12 h (n=119), n (%) | ||
| Hyperlipidemia | |||
| Yes | 45 (33.8) | 38 (31.9) | 0.748 |
| No | 88 (66.2) | 81 (68.1) | |
| Hypertension | |||
| Yes | 69 (51.9) | 59 (49.6) | 0.715 |
| No | 64 (48.1) | 60 (50.4) | |
| DM | |||
| Yes | 42 (31.6) | 45 (37.8) | 0.299 |
| No | 91 (68.4) | 74 (62.2) | |
| Smoking | |||
| Yes | 38 (28.6) | 34 (28.6) | 1 |
| No | 95 (71.4) | 85 (71.4) | |
| Opium consumption | |||
| Yes | 27 (20.3) | 26 (21.8) | 0.763 |
| No | 106 (79.7) | 93 (78.2) | |
| History of dysrhythmia | |||
| Yes | 1 (0.8) | 1 (0.8) | 0.463 |
| No | 132 (99.2) | 118 (99.2) | |
| History of myocardial infarction | |||
| Yes | 36 (27.1) | 33 (27.7) | 0.906 |
| No | 97 (72.9) | 86 (72.3) | |
| Family history of heart disease | |||
| Yes | 25 (18.8) | 29 (24.4) | 0.282 |
| No | 108 (81.2) | 90 (75.6) | |
DM=Diabetes mellitus
There was a statistically significant difference in the level of troponin at the time of admission in the delayed referral group and the nondelayed referral group (P < 0.001). CPK (P = 0.020) and LDH (P = 0.044) were also significantly different in both groups. In post-treatment echocardiography, the mean EF in the nondelayed referral group (41.56 ± 9.16) was statistically significantly different from the delayed referral group (38.39 ± 11.01) and was higher (P < 0.001).
Blood pressure in both groups at the admission time was not statistically different (P = 0.722) and (P = 0.355). On average, 15.9% of the study population had died in the hospital, of which 20.20% were related to those in the delayed referral group and 12.00% were related to the nondelayed referral group, but this difference was not statistically significant. The length of hospital stay (P = 0.583), hospitalization (P = 0.133), and treatment costs (P = 0.256) in the delayed client group was longer than the nondelayed client group, but this difference was not statistically significant [Table 3].
Table 3.
Clinical information on arrival, paraclinical test results, and outcomes of patients in the delayed referral group and the nondelayed referral group
| Variable | Referral time | P | |||
|---|---|---|---|---|---|
|
| |||||
| ≥12 h | <12 h | ||||
|
|
|
||||
| n | Mean±SD | n | Mean±SD | ||
| Ejection fraction (%) | 129 | 41.56±9.16 | 109 | 38.39±11.01 | 0.001 |
| Systolic blood pressure at hospitalization time (mmhg) | 129 | 138.89±26.60 | 115 | 137.63±28.77 | 0.722 |
| Systolic blood pressure at discharge (mmhg) | 129 | 119.10±14.91 | 115 | 121±16.95 | 0.355 |
| Diastolic blood pressure at hospitalization time (mmhg) | 129 | 83.86±12.73 | 115 | 85.94±16.79 | 0.282 |
| Diastolic blood pressure at discharge (mmhg) | 129 | 75.17±9.55 | 115 | 74.50±12.34 | 0.641 |
| Troponin at hospitalization (ng/mL) | 86 | 940.26±4360.26 | 77 | 8937.16±13,696.92 | <0.001 |
| Lactate dehydrogenase at hospitalization (U/L) | 23 | 472.73±130.97 | 20 | 674.25±403.27 | 0.044 |
| Creatine phosphokinase at hospitalization (U/L) | 57 | 160.38±154.14 | 34 | 283.41±339.27 | 0.020 |
| Duration of hospital stay (day) | 133 | 4.77±3.61 | 119 | 5.02±3.60 | 0.583 |
| Hospitalization and treatment costs with insurance (rial) | 133 | 6,444,832.46±8,137,108.52 | 119 | 15,370,137.90±8,825,100.64 | 0.133 |
| Hospitalization and treatment costs without insurance (rial) | 133 | 68,641,614.68±51,141,231.39 | 119 | 76,236,063.02±54,661,982.93 | 0.256 |
| Hospital death* | 16 | 12% | 24 | 20.20% | 0.078 |
| Death until the end of the study* | 26 | 19.5% | 40 | 33.06% | 0.011 |
*Data presented as, n (%). SD=Standard deviation
Log-rank test to compare 3-year survival of patients showed a significant difference between patient survival based on the time of referral so that the survival rate of patients in the nondelayed group was higher than the delayed group (P = 0.009) [Figure 1].
Figure 1.
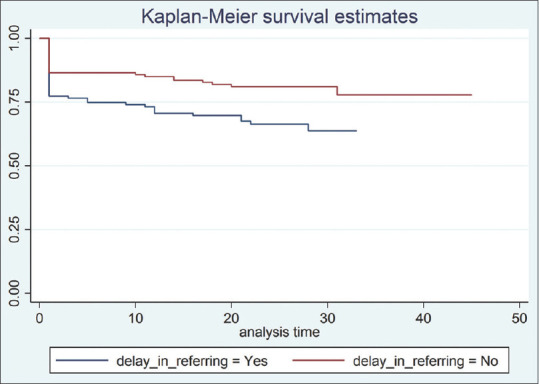
Kaplan–Meier time to event model for long-term mortality
COX regression survival analysis showed that among the studied variables, delayed referral, patient age, and SBP at baseline were related to the 3-year survival rate of patients. The survival rate of patients who presented without delay was higher than patients in the delayed referral group (hazard ratio [HR] = 1.8, P = 0.024), also with increasing age (HR = 1.04, P < 0.001) and lowering SBP (HR = 0.98, P = 0.003), patient survival was reduced [Table 4].
Table 4.
Factors affecting the survival of patients with acute myocardial infarction based on cox survival analysis
| _t | HR | SE | z | P>z | 95% CI |
|---|---|---|---|---|---|
| Delay in referring | 1.805064 | 0.4711426 | 2.26 | 0.024 | 1.082229-3.01069 |
| Age | 1.042394 | 0.0111462 | 3.88 | <0.001 | 1.020775-1.064471 |
| SBP1 | 0.9854588 | 0.0049298 | −2.93 | 0.003 | 0.9758437-0.9951686 |
HR=Hazard ratio, SE=Standard error, CI=Confidence interval, SBP1=Systolic blood pressure 1
Discussion
In the present study, the records of 252 patients admitted with a diagnosis of AMI were reviewed. The mean cardiac EF after treatment was significantly different in both the delayed referral group and the nondelayed referral group. In addition, in laboratory tests there was a significant difference between the two groups and the level of enzymes was higher in the delayed referral group. The percentage of hospital deaths in the delayed referral group was higher than the nondelayed referral group, although this difference was not statistically significant. According, 47.2% of patients referred to Shahid Beheshti Medical Center in … were delayed. Similarly, Taghadosi et al., who reported a long delay of 45.1%, but in the study of McNair et al., the rate of delay in referring patients was reported to be 12%.[16] Although all three studies showed a delay in the referral of patients with AMI, the rate of delay in the referral group was higher in internal studies. This difference may be due to the culture and knowledge of the population under study. In internal studies, only individuals of Iranian nationality were included in the study, while in the study of McNair et al., different races and nationalities were included. The study by McNair et al., similar to the present study, considered the delay to be 12 h.[16] In the study of Cerrato et al., 59% of patients referred after 24 h and 68% after 12 hours’ delay.[21] It can be said that lack of education for the patient and his family, lack of awareness of the outcomes of delay, lack of knowledge about the causes and complications of heart attack, the expectation of spontaneous recovery, attributing the disease to noncardiac causes, not paying attention to pain, including causes of delay in patients.[22]
In the present study, the prevalence of AMI was higher in men, which is similar to the results of the Cerato study.[21] In this study, there was no significant difference in referrals between men and women, single and married people, level of education, different income, different ages, having or not having insurance, time of hospitalization, and the way of going to the hospital in the two groups. However, the majority of patients in the two groups were male, married, illiterate, and with low income. In the Cerato study, in line with the present study, there was no difference in gender between men and women at the hospitalization time.[21] Women were later than men in McNair study.[16] Moreover, it can be said that the level of tolerance of Iranians and their reaction to pain in their decision to seek and follow-up treatment was not ineffective and there was no difference in demographic variables.
In this study, no difference was observed in the underlying risk factors of the two groups (diabetes, hypertension, hypertension, smoking), drug addiction, previous myocardial infarction, and family history of heart disease, but in the study of McNair et al., people with diabetes had more delayed referrals.[16] In the study, the rate of diabetes, hypertension, history of previous angina, chronic heart failure, and consultation with a physician were higher in patients with a delayed referral.[16]
It should be noted that 34.5% of the subjects were diabetics, 50.8% had high blood pressure, 21% had a history of opium use, 32.9% had a history of hyperlipidemia, and 28.6% had a history of smoking, there is a possibility of neuropathic complications and hidden symptoms in these people. It can be argued that neuropathy due to underlying risk factors and old age has led to a misreporting of the first time symptoms appear. It is also possible that there is a time lag between the onset of symptoms and reports by patients that can lead to human error in recalling some information. In this study, the outcome of dysrhythmia and cardiac arrest in the hospital was higher in the delayed referral group. In the delayed referral group, the cardiac EF was significantly reduced. Furthermore, the length of hospitalization and its cost in the delayed referral group were more than the nondelayed referral group. According to the studies that have been done in this field inside and outside the country and the results that have been obtained similar to the present results, it can be said that the extent of the lesion and its outcomes increase the hospital stay and its costs.[16] The delayed referral is associated with decreased EF and cardiac dysfunction, and outcomes such as dyspnea, recurrent pulmonary edema, which leads to frequent hospitalization, increased hospital stay, and occupancy of hospital beds, increased costs imposed on the patient and hospital management, less patient presence in society, more dependence on others, and psychological problems.[23,24]
In the study of hospital mortality and survival of patients, in 3 years after discharge, people in the delayed referral group had more mortality than the nondelayed referral group. Furthermore, their survival time after discharge was shorter than the nondelayed referral group. The results were similar in the study of McNair et al.; patients were followed for 2.8 years in terms of survival, in which the survival rate in patients in the delayed referral group was significantly reduced compared to other patients.[16] However, the present study is somewhat of the first research in this field in Iran. Therefore, research in different medical centers and on a larger scale can improve the results of the study. Given the advances in the treatment of cardiovascular disease, we still see high mortality in many countries due to heart disease, especially AMI. Studies on the delayed referral of patients with AMI have pointed to the causes of delay and related factors, and no study has been conducted on the consequences of delayed referral of patients with myocardial infarction in Iran. Assessing the consequences of delayed referral of patients with AMI can provide information to develop the knowledge and education of patients and health care providers with the aim of reducing the delay in referral of patients with AMI symptoms.
Limitations and recommendation
Conducting this study in a governmental center, lack of access to information of patients in other centers, lack of access to accurate medical records of critically ill patients while attending a medical center, or patients discharged with personal consent after initial procedures, as well as defects in the registration of medical records are the limitations of the present study.
Increase the knowledge of patients and caregivers about the consequences of delayed referral of patients with AMI, is necessary to prevent of deaths due to severe complications associated with delayed referral and reduce the health care costs due to unnecessary invasive treatments.
Conclusion
Despite advances in the diagnosis and treatment of heart disease, many patients with AMI present in the hospital with delay. Delay in patients’ admit leads to delays in starting treatment and various poor outcomes such as decreased cardiac EF, reduced survival time, increased hospital mortality, increased hospitalization and treatment costs, and increased hospital stay. Therefore, necessary training on the symptoms of heart disease and complications due to delay in treatment, especially in people who have risk factors for this disease, is necessary.
Financial support and sponsorship
This study was supported by Qom University of medical sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the Vice Chancellor for Research, respected professors of the School of Nursing and Midwifery, the director and staff of the Shahid Beheshti Educational and Medical Center in Qom, the medical records unit, the participants in the research, and all those who contributed in some way.
References
- 1.Mohebbi B, Tafaghodi B, Sadeghi R, Tol A, Yekanenejad MS. Factors predicting nutritional knowledge, illness perceptions, and dietary adherence among hypertensive middleaged women: Application of transtheoretical model. J Educ Health Promot. 2021;10:212. doi: 10.4103/jehp.jehp_1434_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shakibazadeh E, Sabouri M, Mohebbi B, Tol A, Yaseri M. Validity and reliability properties of the Persian version of perceived health competence scale among patients with cardiovascular diseases. J Educ Health Promot. 2021;10:19. doi: 10.4103/jehp.jehp_899_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ioacara S, Popescu AC, Tenenbaum J, Dimulescu DR, Popescu MR, Sirbu A, Fica S. Acute myocardial infarction mortality rates and trends in Romania between 1994 and 2017. Int. J. Environ. Res. Public Health. 2020;17(1):285. doi: 10.3390/ijerph17010285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. The Lancet 2017 14;389 (10065):197-210 Acute myocardial infarction. The Lancet. 2017 Jan 14;389(10065):197–210. doi: 10.1016/S0140-6736(16)30677-8. [DOI] [PubMed] [Google Scholar]
- 5.Chai LS, Putit Z, Siop S. Barriers to timely treatment-seeking in patients with acute myocardial infarction in Malaysia: A qualitative study. BMC nursing. 2016;15(1):1–0. doi: 10.1186/s12912-016-0155-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim SC, Rahman A, Yaacob NM. Pre-hospital factors influencing time of arrival at emergency departments for patients with acute ST-elevation myocardial infarction. Malays J Med Sci. 2019;26(1):87. doi: 10.21315/mjms2019.26.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ibañez EL, López RR, Palavecino JA, Amicone NC. Evaluation of Strategies to Reduce Reperfusion Times in ST-Segment elevation acute Myocardial infarction. Mobile health experience (mhealth) Rev Argent Cardiol. 2019;87:314–8. [Google Scholar]
- 8.Rafi A, Sayeed Z, Sultana P, Aik S, Hossain G. Pre-hospital delay in patients with myocardial infarction: An observational study in a tertiary care hospital of northern Bangladesh. BMC Health Serv Res. 2020;20(1):1. doi: 10.1186/s12913-020-05505-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soltani L, Ravari A, Sabzevari S. Relationship between prodromal (warning) symptoms and referring time in patients with myocardial infarction. Iran J Cardiovasc Nurs. 2016;4:22–31. [Google Scholar]
- 10.Xie L, Huang SF, Hu YZ. Factors influencing pre-hospital patient delay in patients with acute myocardial infarction. Chin Nurs Res. 2015;2:75–9. [Google Scholar]
- 11.Balk M, Gomes HB, Quadros AS, Saffi MA, Leiria TL. Comparative analysis between transferred and self-referred STEMI patients undergoing primary angioplasty. Arq Bras Cardiol. 2019;5:112–402. doi: 10.5935/abc.20190014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lassen JF, Bøtker HE, Terkelsen CJ. Timely and optimal treatment of patients with STEMI. Nat Rev Cardiol. 2013;10(1):41–8. doi: 10.1038/nrcardio.2012.156. [DOI] [PubMed] [Google Scholar]
- 13.Hochberg CP, Jacobs AK. Prehospital delay in patients with ST-segment elevation myocardial infarction: Time for change. Coron Artery Dis. 2018;29(5):368–70. doi: 10.1097/MCA.0000000000000629. [DOI] [PubMed] [Google Scholar]
- 14.Maruhashi T, Ishihara M, Inoue I, Kawagoe T, Shimatani Y, Kurisu S, Nakama Y, Kagawa E, Dai K, Matsushita J, Ikenaga H. Effect of prodromal angina pectoris on the infarct progression in patients with first ST-elevation acute myocardial infarction. Circ J. 2010:1006150773. doi: 10.1253/circj.cj-10-0187. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: A systematic review. Circ Cardiovasc Qual Outcomes. 2010;3(1):82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McNair PW, Bilchick KC, Keeley EC. Very late presentation in ST elevation myocardial infarction: Predictors and long-term mortality. IJC Heart & Vasculature. 2019;22:156–9. doi: 10.1016/j.ijcha.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, De Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Ängerud KH, Sederholm Lawesson S, Isaksson RM, Thylén I, Swahn E. Differences in symptoms, first medical contact and pre-hospital delay times between patients with ST- and non-ST-elevation myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2019;8(3):201–7. doi: 10.1177/2048872617741734. [DOI] [PubMed] [Google Scholar]
- 19.Dianati M, Mosavi GA, Hajibagheri A, Alavi NM. The pre-hospital delay in seeking treatment in patients with acute myocardial infarction referring to a central hospital in Kashan, Iran. Indian J Med Sci. 2010;64(10):448–54. [PubMed] [Google Scholar]
- 20.Rad M, Bidi A, Khaligh RG, Rad M. Causes of late referral to the Emergency Department in patients with myocardial infarction in Iran. Acta Facult Med Naissensis. 2018;35:105–13. [Google Scholar]
- 21.Cerrato E, Forno D, Ferro S, Chinaglia A. Characteristics, in-hospital management and outcome of late acute ST-elevation myocardial infarction presenters. J Cardiovasc Med. 2017;18(8):567–71. doi: 10.2459/JCM.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 22.Nymark C, Henriksson P, Mattiasson AC, Saboonchi F, Kiessling A. Inability to act was associated with an extended delay prior to care-seeking, in patients with an acute myocardial infarction. Eur J Cardiovasc Nurs. 2019;18(6):512–20. doi: 10.1177/1474515119844654. [DOI] [PubMed] [Google Scholar]
- 23.Jäger B, Farhan S, Rohla M, Christ G, Podczeck-Schweighofer A, Schreiber W, Laggner AN, Weidinger F, Stefenelli T, Delle-Karth G, Kaff A. Clinical predictors of patient related delay in the VIENNA ST-elevation myocardial infarction network and impact on long-term mortality. E Eur Heart J Acute Cardiovasc Care. 2017;6(3):254–61. doi: 10.1177/2048872616633882. [DOI] [PubMed] [Google Scholar]
- 24.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) European Heart Journal. 2017;39(2):119–77. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]


