Abstract
BACKGROUND:
Nurses are in close contact with COVID-19 patients and due to the high risk of infection, they experience fear and anxiety that can result in burnout. This study aimed to review the studies on burnout among nurses during the COVID-19 epidemic.
MATERIALS AND METHODS:
The study followed the guideline for Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA). Using the keywords: “burnout,” “nurse,” and “COVID-19” and with the help of Boolean operators, “AND” and “OR” the online databases, namely PubMed, Scopus, Google Scholar, Web of Science, and Science Direct were searched. Articles published from the first of February 2020 to 30 October, 2020 were retrieved. After the quality appraisal, the required data were extracted and analyzed.
RESULTS:
Out of 85 articles identified in the initial search, and after removing duplicates and those that did not have the required data, seven articles entered the analysis. Among these articles, four (57.14%) reported moderate burnout and three articles (42.86) reported high level of burnout among nurses during the COVID-19 pandemic.
CONCLUSIONS:
A majority of the studies reported that nurses experienced a moderate level of burnout during the COVID-19 pandemic. Given the prevalence of burnout in nurses and because nurses are the largest portion of the healthcare providers who are in close contact with patients infected by COVID-19, it is necessary for health care policymakers to adopt strategies for preventing or reducing burnout among nurses.
Keywords: COVID-19, job burnout, nurse
Introduction
On January 30, 2019, the World Health Organization announced the outbreak of a public health emergency and international concern[1] called coronavirus-2019 (COVID-19) which is caused by severe acute respiratory syndrome coronavirus 2.[2] In December 2019,[3] the COVID-19 disease has emerged in Wuhan, China, and is spreading rapidly worldwide.[4] The COVID-19 epidemic is now considered a global public health emergency.[2,5,6] Health care workers, especially nurses who are in close contact with these patients, are at high risk of this infection and therefore, experience fear, anxiety, depression, and burnout.[7] Among health care workers, nurses make up the largest portion of the health care providers[8] and have always played an important role in infection prevention, infection control, isolation, containment, and public health.[4,9] When nurses are exposed to workplaces with high job demands and low resources, they experience symptoms of physical and emotional stress that consequently would affect their health.[9] In addition, maintaining the mental health of nursing staff is essential to control infectious diseases.[10]
Health professionals who care for COVID-19 patients experience severe stress that can lead to burnout and decreased capacity to continue working.[11] Burnout has been described as a dangerous condition resulting from overwork and chronic workplace stress that has not been successfully managed. It can lead to physical or mental illness.[2] Burnout can not only induce negative emotions but can also diminish positive emotions.[12] A study of health care professionals has shown a direct significant relationship between stress and burnout.[13] Another study revealed that during the COVID-19 epidemic, physicians and nurses suffer from mental health problems, including burnout[14] due to the physical, mental, and social pressures they experience in the workplace.[11]
Because of the special nature of the nursing profession, clinical nurses experience different degrees of burnout. On the other hand, the fight against COVID-19 is a big challenge; and the burnout of nurses caring for patients with COVID-19 may not be the same as burnout experienced in other work-related conditions.[2,15] Sporadic reports published on the prevalence of burnout among nurses who care for patients with COVID-19 reported different rates.[16,17] Therefore, this study aimed to provide a more accurate estimate of the prevalence of burnout among nurses who cared for patients with COVID-19.
Materials and Methods
A systematic review design was conducted in 2020 on studies that investigated the prevalence of burnout among nurses who cared for patients with COVID-19. The study is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Search strategy
Relevant studies were identified through electronic searches of PubMed, Scopus, Google Scholar, Web of Science, and Science Direct. The snowballing method of searching the bibliographies of retrieved references was applied to identify relevant articles. The articles were screened first of February 2020–October 30, 2020. No language restrictions were imposed.
Direct were searched using the following keywords: “burnout,” “nurse,” and “COVID-19.” Boolean operators, “AND” and “OR” were used to narrow or broaden search results. Articles were included if they were the reports of original researches, were in English, included data on the prevalence of burnout among nurses during the COVID-19 epidemic, and had been published from the first of February 2020–October 30, 2020.
Study selection
Twice reviewers screened titles and abstracts of all retrieved records for duplication. Full texts of all potentially relevant studies were then independently studied to determine the final study selection. Discrepancies were resolved by consensus. Duplicate information on the same patients was combined to obtain complete data.
Data extraction
Study characteristics were extracted from eligible articles: Authors/Country/Year, Design and Method, Sampling, Sample size/Age group or mean age, Instrument used, Analysis methods, Important findings, The prevalence/severity of burnout among nurses, and P value.
Data synthesis
Search results (n = 85) were exported to the EndNote software (v. X7) and two researchers independently screened their titles and abstracts to identify duplicate records. The reference lists of eligible articles were also hand-searched for additional studies. Then, two reviewers independently appraised the quality of the retrieved studies using a checklist including the research method, validity, and reliability of data collection instruments, the sample size, and the absence of bias in data collection and statistic test and software.
A data collection form was used to extract data on the following items from the retrieved articles: Author, publication year, country, study design, sample size, sampling method, main results, burnout prevalence, level of significance, and conclusion. Figure 1 presents the process of the study. Table 1 shows levels of nurse's burnout during the COVID-19 pandemic and Table 2 refers to a summary of the characteristics and the quality indicators of the included studies.
Figure 1.
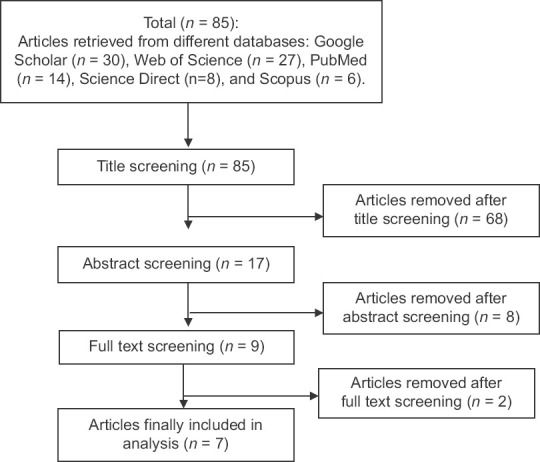
PRISMA flow diagram
Table 1.
Levels of nurse’s burnout during the coronavirus disease 2019 pandemic (n=7)
| Level of nurse’s burnout | Frequency (%) | Country |
|---|---|---|
| Low | - | - |
| Moderate | 4 (57.14) | China |
| High | 3 (42.86) | Iran, China, Istanbul |
Table 2.
A summary of the characteristics and the quality indicators of the included studies
| Authors/country/year | Design and method | Sampling | Sample size/age group or mean age | Instrument used | Analysis methods | Important findings | The prevalence/severity of burnout among nurses | P |
|---|---|---|---|---|---|---|---|---|
| Hu et al./China/2020[4] | Descriptive cross sectional | All frontline nurses in two hospitals in Wuhan/online WeChat | 2014 nurses | MBI-HSS Star |
Descriptive statistics, independent - samples t-test, Pearson correlation coefficient | Frontline nurses experienced a variety of mental health challenges, especially burnout and fear, which warrants more attention and support from policymakers | Moderate level | <0.05 |
| Wan et al./China/2020[16] | Descriptive cross sectional | Online | 1011 nurses | MBI-GS, STAI | Descriptive statistics, linear regression | The anxiety level among nurses during the COVID-19 is serious | Mild to medium | <0.05 |
| Guixia and Hui/2020[2] | Descriptive cross sectional | Convenient sampling, online survey (WeChat friends) | - | MBI, SAS, and SDS | Spearman/Pearson correlation analyses, Chi-square, multiple regression | The incidence of nurses’ burnout was high in the period of COVID-19 | Mainly mild (81.6%) | ≤0.05 |
| Hoseinabadi et al./Iran/2020[17] | Cross sectional | Frontline nurses in a hospital | 245 nurse/23-54 years | OLBI, JSQ, and questionnaires of hospital resources, family support, and measuring the fear of COVID-19 | Descriptive statistics, Chi-square test, Fisher’s exact test, independent samples t-test | The strong relationship between burnout and problems influenced | Burnout in the group exposed to COVID-19 patients was significantly higher than those who cared for non-COVID-19 patients | <0.05 |
| Murat/China/October 2020[18] | Cross-sectional | Purposive sampling/online | 705 nurses | MBI, PSS and BDI | Descriptive analysis, means and standard, deviations samples t-tests and regression | preventive and promotive interventions in mental health should be planned and implemented to improve the mental health and maintain the well-being of front-line nurses | High levels of stress and burnout | <0.05 |
| Chen et al./October 2021[19] | Cross-sectional | Online (WeChat app) | 350 nurses | TSQ, MBI-GS, PTGI-SF | Descriptive analysis, Chi-square, logistic and multiple linear regressions | Nurses who care for patients with infectious diseases exhibit higher levels of burnout | Higher levels | <0.05 |
| Hardiyono/2020[20] | Qualitative | Census | - | Group discussion (FGD) | Qualitative analysis | Nurses experienced burnout when they care for a large number of patients with positive COVID-19 | Moderate level | - |
COVID-19=Coronavirus disease 2019, SAS=Self-rating Anxiety Scale, SDS=Self-rating Depression Scale, JSQ=Job stress questionnaire, MBI-GS=Maslach Burnout inventory - general survey, STAI=State-trait anxiety inventory, OLBI=Oldenburg burnout inventory, PANAS=The positive and negative affective schedule, CD-RISC=The Connor-Davidson Resilience Scale, MBI-HSS=Maslach burnout inventory - human services survey, TSQ=Trauma screening questionnaire, PTGI-SF=Posttraumatic growth inventory-short form, FGD=Focus group discussion, SAI=State anxiety inventory, TAI=Trait anxiety inventory, PSS=Perceived Stress Scale, BDI=Beck Depression Inventory
Ethical consideration
To extract data from the mentioned articles, all ethical principles related to competing essays were observed. No attempt was made to obtain ethical approval due to the lack of sample collection and interview.
Discussion
Four out of seven articles reviewed in the present study reported that nurses experienced a moderate level of burnout during the COVID-19 pandemic and three articles reported high levels of burnout among nurses in the same period. Due to their responsibility for human health, continual confrontation with patients[18] , performing clinical procedures, exposure to dying patients, dealing with emergency, and unpredictable situations, and exposure to too much noise at the workplace, nurses are exposed to high levels of work pressure.[19,20,21] Epidemiological studies have shown that about 17%–41% of nurses in different countries have symptoms of depression and approximately 20%–40% of them have symptoms of anxiety.[2,22] Anxiety and depression overlap with burnout. Burnout may also exacerbate negative emotions. Work pressure along with depression and anxiety would exacerbate job burnout.[12] Although nurses experience degrees of anxiety and depression during the COVID-19 pandemic, anxiety has a greater effect on job burnout. A study also showed that each additional patient added to a nurse's workload was associated with a 23% increase in the probability of burnout.[4] Because burnout has a serious impact on nurses’ mental health and work capacity,[2] and by reporting that 15.6% of nurses experience burnout, the Joint Commission for Quick safety advisory on Combating Nurse Burnout emphasized that organizations should remove barriers to nurses’ workflow and workplace environment concerns to decrease the rate of burnout among them.[23] Nonetheless, self-control and regulation of emotions are important in the handling of burnout and resolving difficult and anxiogenic workplace issues.[24] Consistently, studies reported that flexibility and feeling of self-efficacy as well as the effective use of organizational resources improve mental health, reduce anxiety, depression, and burnout among frontline nurses, and help them be prepared for stressful and difficult situations.[4,25] Some studies also showed that using stress management techniques, adequacy of hospital resources for the treatment of patients with COVID-19, and support received from family, friends, colleagues, and superiors can help reduce stress and burnout in nurses during the COVID-19 epidemic.[17,24,26] Furthermore, the availability of mental health professionals for psychological counseling, social support, and protective measures for nosocomial infections can prevent burnout in nurses or help reduce it.[3,24] Studies also confirmed the role of a balance between rest and activity, good nutrition and exercise, personal hobbies, entertainment, and timely vacations in the reduction of chronic stress, anxiety, and burnout in employees, especially when they feel overwhelmed.[24] Therefore, nursing managers and hospital authorities should pay more attention to health care workers, – especially nurses – and design long-term preventive plans, reduce working shifts, and find the sources of stress and resolve them to manage not only the ongoing outbreak but also to control future pandemics.[17]
Limitations and recommendation
Limited studies have been published on the prevalence of burnout among nurses in the COVID-19 pandemic. The results of these studies might not be generalized. Therefore, further studies should be conducted in this area.
Conclusion
A majority of the studies reviewed reported that nurses experienced a moderate level of burnout during the COVID-19 pandemic. Given the prevalence of burnout in nurses and its consequences, and because nurses are the largest group of the health care providers in service of patients with COVID-19, it is necessary for health care policymakers to adopt appropriate strategies and methods to prevent or reduce burnout among nurses. Increasing personal protection equipment, providing alternative workforce, and periodic rotation of front-line nurses, providing adequate organizational, and social support, and ensuring their willingness to work as frontline can help prevent or reduce burnout among nurses.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to appreciate the efforts of all health care providers, – especially nurses – in dealing with COVID-19.
References
- 1.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus disease 2019 (COVID-19): A perspective from China. Journal of Radiology. 2020;296:E15–25. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guixia L, Hui Z. A study on burnout of nurses in the period of COVID-19. Journal of Psychol Behav Sci. 2020;9:31. [Google Scholar]
- 3.Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. Journal of MedRxiv. 2020;1:1. [Google Scholar]
- 4.Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. Journal of EClinicalMedicine. 2020;24:100424. doi: 10.1016/j.eclinm.2020.100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coronini-Cronberg S, John Maile E, Majeed A. Health inequalities: The hidden cost of COVID-19 in NHS hospital trusts? Journal of the Royal Society of Medicin. 2020;113:179–84. doi: 10.1177/0141076820925230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oberfeld B, Achanta A, Carpenter K, Chen P, Gilette NM, Langat P, et al. SnapShot: COVID-19. Cell. 2020;181:954. e1. doi: 10.1016/j.cell.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: Address mental health care to empower society. Journal of Lancet. 2020;395:e37–8. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Said NB, Chiang VC. The knowledge, skill competencies, and psychological preparedness of nurses for disasters: A systematic review. Journal of Int Emerg Nurs. 2020;48:100806. doi: 10.1016/j.ienj.2019.100806. [DOI] [PubMed] [Google Scholar]
- 9.Smith GD, Ng F, Li WH. COVID-19: Emerging compassion, courage and resilience in the face of misinformation and adversity. Journal of Clin Nurs. 2020;29:1425. doi: 10.1111/jocn.15231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–9. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kisa S. Burnout among physicians and nurses during COVID-19 pandemic. European Journal of Environment and Public Health. 2020;4:2. [Google Scholar]
- 12.Bianchi R, Schonfeld IS. Burnout-depression overlap: Nomological network examination and factor-analytic approach. Scand J Psychol. 2018;59:532–9. doi: 10.1111/sjop.12460. [DOI] [PubMed] [Google Scholar]
- 13.Morgantini LA, Naha U, Wang H, Francavilla S, Acar Ö, Flores JM, et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. Journal of PLoS One. 2020;15:e0238217. doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sung CW, Chen CH, Fan CY, Su FY, Chang JH, Hung CC, et al. Burnout in medical staffs during a coronavirus disease (COVID-19) pandemic. Journal of the LANCET. 2020;5:1. [Google Scholar]
- 15.Bradley M, Chahar P. Burnout of healthcare providers during COVID-19. Cleve Clin J Med. 2020;1:9. doi: 10.3949/ccjm.87a.ccc051. [DOI] [PubMed] [Google Scholar]
- 16.Wan Z, Lian M, Ma H, Cai Z, Xianyu Y. Factors associated with burnout among Chinese nurses during COVID-19 epidemic: A cross-sectional study. Journal of research square. 2020;1:18. doi: 10.1186/s12912-022-00831-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarboozi Hoseinabadi T, Kakhki S, Teimori G, Nayyeri S. Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of coronavirus disease -COVID-19- in Iran. Invest Educ Enferm. 2020;38:e3. doi: 10.17533/udea.iee.v38n2e03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murat M, Köse S, Savaser S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. International Journal of Mental Health Nursing. 2021;30:533–543. doi: 10.1111/inm.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen R, Sun C, Chen JJ, Jen HJ, Kang XL, Kao CC, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. 2021;30:102–16. doi: 10.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hardiyono H. COVID-19: Burnout on nurse. Journal of Espacios. 2020;41:11–18. [Google Scholar]
- 21.Mousavi SV, Ramezani M, Salehi I, Hossein Khanzadeh AA, Sheikholeslami F. The relationship between burnout dimensions and psychological symptoms (depression, anxiety and stress) among nurses. Journal of Holistic Nursing and Midwifery. 2017;27:37–43. [Google Scholar]
- 22.Chen J, Li J, Cao B, Wang F, Luo L, Xu J. Mediating effects of self-efficacy, coping, burnout, and social support between job stress and mental health among young Chinese nurses. Journal of Advanced Nursing. 2020;76:163–73. doi: 10.1111/jan.14208. [DOI] [PubMed] [Google Scholar]
- 23.Ross J. The exacerbation of burnout during COVID-19: A major concern for nurse safety. J Perianesth Nurs. 2020;35:439–40. doi: 10.1016/j.jopan.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papathanasiou IV, Tsaras K, Kleisiaris CF, Fradelos EC, Tsaloglidou A, Damigos D. Anxiety and depression in staff of mental units: The role of burnout. In: GeNeDis 2016. Cham: Springer; 2017. pp. 185–97. [DOI] [PubMed] [Google Scholar]
- 25.Badu E, O’Brien AP, Mitchell R, Rubin M, James C, McNeil K, et al. Workplace stress and resilience in the Australian nursing workforce: A comprehensive integrative review. Int J Ment Health Nurs. 2020;29:5–34. doi: 10.1111/inm.12662. [DOI] [PubMed] [Google Scholar]
- 26.Sasangohar F, Jones SL, Masud FN, Vahidy FS, Kash BA. Provider burnout and fatigue during the COVID-19 pandemic: Lessons learned from a high-volume intensive care unit. Anesth Analg. 2020;131:106–11. doi: 10.1213/ANE.0000000000004866. [DOI] [PMC free article] [PubMed] [Google Scholar]


