PURPOSE:
The purpose of this study was to validate time frames for postoperative care following stoma surgery and to determine participants' current practice with convex pouching systems during the postoperative period.
DESIGN:
A Cross-sectional survey.
SUBJECTS AND SETTING:
The sample comprised 332 ostomy care specialists practicing in the United States. Most (n = 220; 66%) had more than 10 years' experience caring for patients with ostomies, 82% (n = 272) were certified WOC or ostomy care nurses (CWOCN and COCN), and 7% (n = 23) were board-certified colorectal surgeons.
METHODS:
A 23-item online questionnaire was created for purposes of the study. Items in the questionnaire queried professional background and experience caring for patients with an ostomy. A single item was used to identify postoperative care periods following ostomy surgery. Additional items queried current practice patterns related to use of convex pouching systems and the timing of their use. Data were collected from January 18 to February 8, 2021.
RESULTS:
Most respondents (n = 270; 90%) agreed with the following postoperative periods after ostomy surgery: immediate postoperative period (days 0-8); postoperative period (days 9-30); and transition phase (days 31-180). Most respondents (n = 274; 95%) indicated they would use a convex pouching system when clinically appropriate during the first 30 days following ostomy surgery and 79% (n = 228) indicated using a convex pouching system regardless of when the surgery was performed. Less than 1% (n = 2) indicated never using convexity within the first 30 days following stoma surgery, and only 3% (n = 8) indicated avoidance of convexity pouching systems in the immediate postoperative period.
CONCLUSIONS:
Findings indicate that use of convexity during the postoperative period is prevalent to provide a secure seal and predictable wear time.
Keywords: Colostomy, Convex pouching system, Convexity, Ileostomy, Mucocutaneous junction, Ostomy, Peristomal skin complications, Postoperative
INTRODUCTION
Evidence concerning the use of convex pouching systems for management of the patient with a stoma during the postoperative period is lacking.1,2 Further, controversy exists concerning the frequency and severity of potential complications associated with the use of a convex pouching system during the postoperative period, particularly mucocutaneous separation. Limited evidence suggests that variability in clinical care delivery negatively impacts patient outcomes1,2 and health care system costs.2,3 Best practice guidelines consistently recognize that a secure seal around the stoma is required to minimize leakage that is associated with peristomal skin complications and diminished health-related quality of life.4–6
As convex pouching systems are used to provide a secure seal for the appropriate clinical presentation, guidance on the use of convexity would benefit clinicians. Convexity assists in flattening the skin surrounding the stoma7 and directing the flow from the os into the pouch resulting in decreased leakage, which has been associated with a decrease in peristomal skin complications.8,9 During the postoperative period, changes in the stoma and peristomal body profile are expected. As such, the product that creates the most secure seal may need to be adjusted to adapt to these changes.
The survey was designed by an expert panel to address the paucity of evidence on the use of convexity in the postoperative period. This cross-sectional study aimed to validate the suggested definitions for the postoperative periods and to determine participants' current practice with convex pouching systems during the postoperative period. Findings from this cross-sectional survey were used to develop consensus statements to provide best practice guidance for the use of convexity during the postoperative period following stoma surgery.10
METHODS
A cross-sectional survey study design was used to assess US-based ostomy clinical practice following stoma surgery. The target audience was nurses with expertise in ostomy care and colorectal surgeons. An invitation to participate in the study was sent via email to members of the Wound Ostomy and Continence Nurses (WOCN) Society and the American Society of Colorectal Surgeons (ASCRS). Study procedures were reviewed and approved by the Biomedical Research Alliance of New York LLC Organizational Review Board (Study Protocol # A20-074-691). Completion of the questionnaire comprised consent to study participation.
Questionnaire
A panel of clinicians with clinical experience and expertise caring for patients with an ostomy designed a survey to assess current clinical practice in the use of postoperative convex pouching systems (see Supplemental Digital Content 1, Appendix A, Survey Questionnaire, available at: http://links.lww.com/JWOCN/A71). The questionnaire comprised 23 items and required approximately 12 minutes to complete. Items queried professional background of respondents including practice location, years of experience as both a health care professional and providing ostomy care, care setting, professional role (nurse, physician), and ostomy-related certifications. One item asked respondents to agree or disagree with proposed definitions for postoperative care periods following stoma surgery. Additional forced-choice items (NA was not an option) queried clinical indications and situations that would lead to their use of convex pouching systems during the postoperative period.
Study Procedures
Data were collected from January 18 to February 8, 2021, using an online survey software platform (SurveyMonkey, San Mateo, California). Invitations to participate in the study were emailed to members of the WOCN Society and the ASCRS through each society's management group. No identifiable information was collected as part of survey participation.
Data Analysis
Responses to the survey were collected from the software platform and exported for analysis in Microsoft Excel (Microsoft, Inc, Redmond, Washington). Responses were analyzed using descriptive statistics and Excel Pivot Tables (Excel 365 version 2019, Microsoft, Redmond, Washington). All data were analyzed and reported in aggregate form using basic demographic data. Data analyzed included descriptive statistics such as mean, median, mode, and standard deviation as well as comparative analyses between regions and between professional groups.
RESULTS
Questionnaires were completed by 342 respondents. Ten responses were discarded because respondents were not clinicians practicing in the United States and were excluded from the analysis. The remaining 332 respondents were evenly disturbed across the United States with 289 answering all questions. Respondents were experienced ostomy clinicians, 66% (n = 220) with more than 10 years' experience. Eighty-two percent (n = 272) of respondents were certified and 7% (n = 23) were colorectal surgeons. Seventy-two percent (n = 238) worked in acute care settings (Table).
TABLE. Characteristics of Respondents.
| Specialization | |||||
| Nurse with a specialty in ostomy care (ie, WOC nurse) | Advanced practice registered nurse with a specialty in ostomy care | Registered nurse, but not certified in ostomy care | Advanced practice registered nurse, but not certified in ostomy care | Surgeon | |
| 68% | 14% | 9% | 0% | 7% | |
| Years of Ostomy Practice | |||||
| >20 y | 10 to <20 y | 5 to <10 y | 2 to <5 y | <2 y | |
| 32% | 34% | 17% | 13% | 3% | |
| Location of Practice Setting | |||||
| Acute, hospital, inpatient | Outpatient clinic | Home health agency | Long-term care hospital | Skilled nursing facility | Other (please specify) |
| 72% | 36% | 14% | 3% | 4% | 7% |
Postoperative Care Periods
The survey proposed the following definitions for the postoperative care periods: immediate postoperative period (days 0-8); postoperative period (days 9-30); and transition phase (days 31-180). Ninety percent (n = 294) of respondents agreed with these definitions. No alternative definitions were suggested by respondents.
Pouch Selection and Ostomy Use in the Postoperative Period
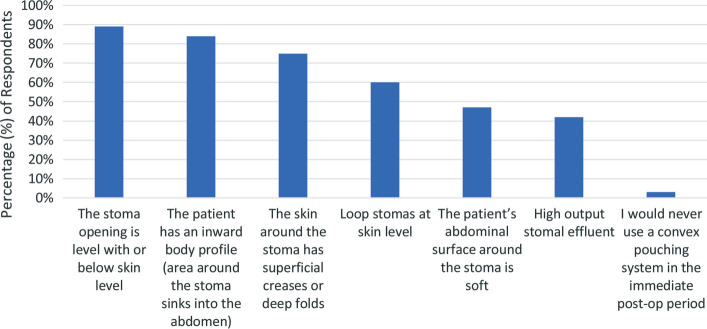
Respondents were asked about their use of convex pouching systems in the first 30 days following stoma creation; 95% (n = 274) answered that they use a convex pouching system depending on the circumstances, with 79% (n = 228) stating that they use a convex pouching system whenever the height of the stoma or the shape and condition of the peristomal skin does not allow for a secure fit if a flat or concave system is used, regardless of when the surgery was performed. Less than 1% (n = 2) of respondents indicated that they never use convexity in the first 30 days. When asked specifically about the immediate postoperative period, 94% (n = 273) of respondents agreed that the most appropriate pouching system should be chosen to prevent leakage of effluent onto the peristomal skin in the first 8 days following ostomy surgery. Only 3% (n = 8) indicated they do not consider convexity in the immediate postoperative period. When asked which clinical indications would lead respondents to use a convex pouching system in the immediate postoperative and postoperative periods, 89% (n = 258) indicated appropriate use if the stoma opening is level with or below the skin and 84% (n = 244) indicated pertinent use if the patient has an inward body profile (Figure). When respondents were asked what further information they would need to be comfortable using a convex pouching system, when indicated, in the immediate postoperative period, 71% (n = 203) indicated that they are already using a convex pouching system.
Figure.
Clinical indications: use of a convex pouching system in the immediate postoperative (0-8 days) and postoperative periods (9-30 days).
DISCUSSION
The use of convex products during the postoperative period has been controversial due to lack of evidence and clear clinical guidance. This cross-sectional survey identified perspectives of clinicians with experiences and expertise in ostomy care concerning their use of convex pouching systems during this postoperative period. The majority of respondents (90%; n = 270) agreed with postoperative period definitions designed by a smaller group of 10 clinicians with extensive expertise and experience caring for patients with an ostomy. Identification of key time frames for the person with a new ostomy is clinically relevant because of the evolution of the ostomy during the days, weeks, and months following stoma surgery.9,11
Respondents were also questioned whether their current practice included use of convex pouching systems, when indicated, in the immediate postoperative (days 0-8) and postoperative period (days 9-30). A majority of respondents indicated using convexity during both periods whereas 3% (n = 8) indicated avoidance of convex products during the immediate postoperative period, and less than 1% (n = 2) indicated avoidance of convexity during both periods. Results from this study are consistent with published guidance on the use of convexity.11,12 Colwell and colleagues12 recommend using a convex pouching system based on a patient's stomal and peristomal body profile. The most recent WOCN Society Guidelines recommend considering the use of a convex pouching system when the stoma is retracted and/or flush, or if the os is at/or below the skin level.11 These findings differ from best practice recommendations from Roveron and colleagues,6 who advise against use of convexity during the “first days” following stoma surgery. This difference may reflect geographic differences between best practices in Italy versus the United States. Additional research is needed to further define the impact of geography and other factors influencing the use of convex pouching systems following ostomy surgery. Findings from this study also highlight the need for additional research and best practice guidance for using convexity to provide a secure seal thereby protecting the peristomal skin from undermining, leakage, and skin damage regardless of when the surgery was performed.
Limitations
The respondents of the survey were wholly US-based to reflect clinical practice in the United States; therefore, it is not necessarily reflective of the international community. Further, the survey was distributed to selected ostomy specialists and may not be representative of the broader medical community. We recommend additional research focusing on practice patterns among nurses, general surgeons, uro-oncology specialist surgeons, and general urologists as well.
CONCLUSIONS
A survey of ostomy care clinicians' use of convex pouching systems during the postoperative periods found that a majority of clinicians practicing in the United States use convexity during the immediate postoperative and postoperative periods following ostomy surgery. Study findings support current best practice guidelines.11,12 In addition, these results were used to develop consensus statements and a decision pathway10 that will help health care professionals to determine when to use convexity to prevent leakage, provide predictable wear time, and contribute to the optimal quality of life for the patient.
Supplementary Material
ACKNOWLEDGMENTS
Development of the postoperative convexity consensus was facilitated by BainGroup Consulting, including administration and statistical analysis of the survey.
Footnotes
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (JWOCNOnline.com).
The panelists and authors received payment from Coloplast Inc in relation to the activities of the Post-operative Convexity Panel. Mathew Kelly and Holly Norman are employees of Coloplast Inc.
Contributor Information
Janet Stoia-Davis, Email: janetsbc@sbcglobal.net.
Janice C. Colwell, Email: jcolwell22@sbcglobal.net.
Krisztina Emodi, Email: krisztina.emodi@ucsf.edu.
Jane Fellows, Email: janeafellows@msn.com.
Mary Mahoney, Email: mahonemf@gmail.com.
Bethany McDade, Email: bethany.mcdade@beaumont.org.
Sima P. Porten, Email: Sima.Porten@ucsf.edu.
Elizabeth R. Raskin, Email: raskinrettke@gmail.com.
Holly S. Norman, Email: ushsn@coloplast.com.
Matthew T. Kelly, Email: usmtk@coloplast.com.
Terran Sims, Email: mg5k@hscmail.mcc.virginia.edu.
REFERENCES
- 1.Maydick-Youngberg D. A descriptive study to explore the effect of peristomal skin complications on quality of life of adults with a permanent ostomy. Ostomy Wound Manage. 2017;63(5):10–23. [PubMed] [Google Scholar]
- 2.Taneja C, Netsch D, Rolstad BS, Inglese G, Lamerato L, Oster G. Clinical and economic burden of peristomal skin complications in patients with recent ostomies. J Wound Ostomy Continence Nurs. 2017;44(4):350–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taneja C, Netsch D, Rolstad BS, Inglese G, Eaves D, Oster G. Risk and economic burden of peristomal skin complications following ostomy surgery. J Wound Ostomy Continence Nurs. 2019;46(2):143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cronin E. A guide to the appropriate use of convex stoma care products. Gastrointestinal Nurs. 2008;6(2):12–16. [Google Scholar]
- 5.Hoeflok J, Salvadalena G, Pridham S, Droste W, McNichol L, Gray M. Use of convexity in ostomy care: results of an international consensus meeting. J Wound Ostomy Continence Nurs. 2017;44(1):55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roveron G, Barbierato M, Rizzo G, et al. Italian guidelines for the nursing management of enteral and urinary stomas in adults: an executive summary. J Wound Ostomy Continence Nurs. 2021;48(2):137–147. [DOI] [PubMed] [Google Scholar]
- 7.Colwell J, Hudson K. Selection of Pouching System. In: Carmel JE, Colwell JC, Goldberg M. eds. Wound, Ostomy, and Continence Nurses Society Core Curriculum: Ostomy Management. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2022:172–188. [Google Scholar]
- 8.González ER, Zurita CdP, Caballero GA, Rodríguez AH, Rodríguez EZ, Blázquez EG. Impact of convex ostomy appliances on leakage frequency, peristomal skin health and stomal protrusion. Gastrointestinal Nurs. 2021;19(suppl 9):S30–S37. [Google Scholar]
- 9.Erwin-Toth P, Thompson SJ, Davis JS. Factors impacting the quality of life of people with an ostomy in North America: results from the Dialogue Study. J Wound Ostomy Continence Nurs. 2012;39(4):417–422; quiz 423-424. [DOI] [PubMed] [Google Scholar]
- 10.Colwell J, Stoia-Davis J, Emodi K, et al. Use of a convex pouching system in the post-operative period—a national consensus. J Wound Ostomy Continence Nurs. 2022;49(3):240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wound, Ostomy and Continence Nurses Society; Guideline Development Task Force. WOCN Society Clinical Guideline: management of the adult patient with a fecal or urinary ostomy—an executive summary. J Wound Ostomy Continence Nurs. 2018;45(1):50–58. [DOI] [PubMed] [Google Scholar]
- 12.Colwell JC, Bain KA, Hansen AS, Droste W, Vendelbo G, James-Reid S. International consensus results: Development of practice guidelines for assessment of peristomal body and stoma profiles, patient engagement, and patient follow-up. J Wound Ostomy Continence Nurs. 2019;46(6):497–504. [DOI] [PubMed] [Google Scholar]