Abstract
Objective
To assess the Simplified Acute Physiology Score 3 (SAPS3) prognostic score performance across different body mass index categories.
Methods
A retrospective cohort study in a general ICU in Brazil. A secondary analysis of medical records was performed with clinical and epidemiological data. Patients were stratified according to their body mass index (BMI) category, and a binary logistic regression was then performed to identify factors independently associated with mortality. SAPS3 accuracy was determined using the area under the receiver operating characteristics curve and the Hosmer-Lemeshow test. A modified Kaplan-Meyer plot was employed to evaluate death probability according to BMI. ICU mortality was evaluated as the primary outcome.
Results
A total of 2,179 patients (mean age of 67.9 years and female predominance (53.1%)) were enrolled. SAPS3 was found accurate in all groups except in the underweight (AUC: 0.694 95% CI 0.616–0.773; HL = 0.042). The patients in the underweight group tended to be older, have longer hospital stay, have worse functional status, and have a higher value on prognostic scores. After the adjustments, no statistically significant difference between the BMI groups was noted in relation to mortality, except for the low weight that presented a likelihood of death of 3.50 (95% CI, 1.43–8.58, p = 0.006).
Conclusion
This research showed that SAPS3 had poor accuracy in predicting ICU mortality in underweight patients. This group was shown to be an independent risk factor for worse clinical outcomes.
Keywords: Intensive care unit, Simplified Acute Physiology Score 3, Body mass index, Mortality, Prognosis
Intensive care unit; Simplified Acute Physiology Score 3; Body Mass Index, Mortality, Prognosis.
1. Introduction
Healthcare, a dynamically evolving field, involves a broad range of complex variables, as patients characteristics and therapeutic and diagnostic tools change over time. Thus, prognostic scores need to be reassessed frequently to ensure their optimal functionality [1]. Body weight is commonly used in the composition of scores, but the body composition of the population has been changing over recent years; the prevalence of obesity almost tripled between 1975 and 2016 [2].
The World Health Organization (WHO) has reported that obesity is the abnormal or excessive accumulation of body fat that can affect health. The Body mass index (BMI) is one of the recommended tools for its diagnosis [2]. Following the global trend of increasing obesity rates, data collected in Brazil, from 2018 onwards, reveal that 55.7% of the country's adult population is overweight and 19.8% is obese, while the corresponding values in 2006 were 42.6% and 11.8%, respectively [3]. Excess body fat has a well-established association with increased morbidity and mortality in long-term follow-up of out-of-hospital populations. In addition, the increase in the prevalence of obesity in the general population and the burden of comorbidities associated with this disease resulted in an increase in the number of hospitalizations of obese people in intensive care units (ICU) [4].
Despite the obesity epidemic, developing countries present a double burden, in which the obese coexist with a significant population of underweight individuals [5, 6]. Several studies have demonstrated the association of low BMI with all-cause mortality and underlying pathologies in an advanced stage. However, this condition is not considered by most prognostic scores and is not widely studied in the context of ICU [7]. The Simplified Acute Physiology Score 3 (SAPS3) was developed from a multinational database of general ICU patients and is commonly used in Brazilian ICUs, as it has shown good calibration and discrimination in low- and middle-income countries [1, 8]. However, as the country's epidemiological scenario has changed over the years, this study seeks to assess the accuracy of the score in a large cohort of critically ill patients, emphasizing the differences between BMI strata.
2. Methods
2.1. Clinical study design
An observational, analytical cohort study was conducted from August 2015 through July 2018 in a general ICU at Hospital da Cidade in Salvador, Bahia, Brazil. A secondary analysis of admission data stored in the Epimed Monitor system was performed. All patients consecutively admitted to the ICU with the length of stay >24 h were included. Patients <18 years or those with missing data were excluded.
Covariates included were age, weight, height, sex, comorbidities, functional capacity, admission diagnosis, length of ICU and hospital stay, physiological and laboratorial data within the first six hours of admission, complications, use of supportive therapy in the ICU, Modified Frailty Index (MFI) [9], the SAPS3 [8], the Charlson Comorbidity Index (CCI) [10]. The patients were stratified based on their BMI values obtained at ICU admission into underweight (BMI <18.5 kg/m2), normal weight (BMI range, 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), obese grade I (BMI, 30–34.9 kg/m2) or obese grade II/III (BMI >35 kg/m2) [2]. Our primary outcome was ICU death.
2.2. Ethics statement
This article was ethically approved by the Research Ethics Committee of Hospital Ana Nery under number 2,571,265 and CAAE 52892315.1.0000.0045. This same ethics committee approved the waiver of consent to participate in accordance with the regulatory standards of the national health council (N° 466/12), which addresses observational, analytical, or descriptive studies that use the information available in medical records; in which data is analyzed anonymously. The present study was conducted in accordance with the Declaration of Helsinki.
2.3. Data analysis
Categorical variables were expressed as frequencies and percentages and analyzed by Fisher's exact test and Z-test. Continuous variables with normal distribution were expressed as means (standard deviation, SD) and means between groups were compared with the one-way analysis of variance (ANOVA) and Tukey's HSD test. Non-normal continuous variables were expressed as median (interquartile range, IQR) and compared with the Mann-Whitney U test and the Kruskal-Wallis test. Normality was assessed by the d'Agostino-Pearson test. All tests results were two-tailed and considered statistically significant for p < 0.05. A binary logistic regression, the backward stepwise method, was used to identify characteristics independently associated with ICU mortality. Finally, the area under the receiver operating characteristic curve (ROC) was determined to assess the discriminative capacity of SAPS3. AUC >0.8 was considered satisfactory. Calibration was assessed using Hosmer-Lemeshow goodness-of-fit test.
The data were analyzed with Microsoft Excel suite Office 365, GraphPad Prism version 6.01, and Statistical Package for the Social Sciences, SPSS version 25.0 (IBM, SPSS, USA).
3. Results
During the study period, 2401 patients were admitted to the ICU. Two hundred and twenty-two subjects were excluded due to missing height, weight, or outcome data or because they did not meet the study inclusion criteria. Finally, 2179 patients were divided into five groups according to their BMI categories (Figure 1). General patient characteristics are provided in Table 1.
Figure 1.
Study flowchart.
Table 1.
Characteristics of the study population.
| Variable | General (n = 2179) |
Non-survivors (n = 343) |
Survivors (n = 1836) |
p-value |
|---|---|---|---|---|
| Age (years) | 68 ± 18 | 77 ± 15 | 66 ± 18 | <0.0001 |
| Gender, female | 1158 (53.1) | 172 (50.1) | 986 (53.7) | 0.239 |
| BMI | 25.6 ± 5.7 | 23.1 ± 5.5 | 26.0 ± 5.6 | <0.0001 |
| Eutrophic | 914 (41.9) | 172 (50.1) | 742 (40.4) | 0.001 |
| Underweight | 171 (7.8) | 64 (18.7) | 107 (5.8) | <0.0001 |
| Overweight | 700 (32.1) | 76 (22.2) | 624 (34.0) | <0.0001 |
| Obese Grade I | 272 (12.5) | 21 (6.1) | 251 (13.7) | <0.0001 |
| Obese Grade II/III | 122 (5.6) | 10 (2.9) | 112 (6.1) | 0.015 |
| Congestive heart failure | 132 (6.1) | 16 (4.7) | 116 (6.3) | 0.268 |
| Chronic renal failure | 251 (11.5) | 45 (13.1) | 206 (11.2) | 0.311 |
| Cirrhosis | 28 (1.3) | 6 (1.7) | 22 (1.2) | 0.430 |
| Cancer | 302 (13.9) | 71 (20.7) | 231 (12.6) | <0.0001 |
| Immune deficiency | 27 (1.2) | 7 (2.0) | 20 (1.1) | 0.177 |
| Diabetes | 817 (37.5) | 132 (38.5) | 685 (37.3) | 0.716 |
| Coronary Artery Disease | 241 (11.1) | 31 (9.0) | 210 (11.4) | 0.223 |
| Chronic Atrial Fibrillation | 137 (6.3) | 32 (9.3) | 105 (5.7) | 0.015 |
| Stroke | 340 (15.6) | 77 (22.4) | 263 (14.3) | <0.0001 |
| Dementia | 125 (5.7) | 48 (14.0) | 77 (4.2) | <0.0001 |
| Tobacco | 164 (7.5) | 19 (5.5) | 145 (7.9) | 0.147 |
| Alcoholism | 119 (5.5) | 22 (6.4) | 97 (5.3) | 0.436 |
| Psychiatric disease | 169 (7.8) | 23 (6.7) | 146 (8.0) | 0.509 |
| Dyslipidemias | 201 (9.2) | 24 (7.0) | 177 (9.6) | 0.128 |
| Systolic arterial pressure (mmHg) | 138 ± 29 | 130 ± 30 | 139 ± 28 | 0.846 |
| Diastolic Blood Pressure (mmHg) | 79 ± 20 | 75 ± 21 | 80 ± 20 | <0.0001 |
| Mean Arterial Pressure (mmHg) | 99 ± 21 | 93 ± 22 | 100 ± 20 | <0.0001 |
| HR (bpm) | 86 ± 20 | 94 ± 22 | 84 ± 20 | <0.0001 |
| RR (bpm) | 20 ± 4 | 21 ± 5 | 20 ± 4 | <0.0001 |
| Temperature (°C) | 36 ± 1 | 36 ± 1 | 36 ± 1 | 0.692 |
| Urea (mmol/L) | 57 ± 47 | 86 ± 64 | 51 ± 42 | <0.0001 |
| Creatinine (mg/dL) | 1.44 ± 2 | 1.86 ± 2 | 1.36 ± 2 | <0.0001 |
| Platelets (x103) | 235 ± 113 | 230 ± 130 | 236 ± 109 | 0.420 |
| Hematocrit (%) | 34 ± 7 | 32 ± 8 | 35 ± 7 | <0.0001 |
| Leukocytes total (x103; /uL) | 11 ± 11 | 13 ± 7 | 11 ± 11 | 0.011 |
| Bands (/uL) | 176.1 ± 511.6 | 304.6 ± 666.5 | 152.1 ± 473.5 | <0.0001 |
| Segmented (x103; /uL) | 9.26 ± 5.74 | 11.05 ± 6.40 | 8.92 ± 5.54 | <0.0001 |
| Eosinophils (/uL) | 123.5 ± 246.5 | 112.6 ± 286.0 | 125.5 ± 238.4 | 0.404 |
| Basophils (/uL) | 18.6 ± 48.7 | 8.58 ± 27.55 | 20.47 ± 51.55 | <0.0001 |
| Lymphocytes (x103; /uL) | 1.69 ± 8.84 | 1.27 ± 1.04 | 1.77 ± 9.61 | 0.360 |
| Atypical (/uL) | 9.78 ± 172.8 | 28.58 ± 390.26 | 6.26 ± 83.38 | 0.034 |
| Monocytes (/uL) | 562.6 ± 390.2 | 521.38 ± 410.73 | 570.34 ± 385.85 | 0.040 |
| Na (mEq/L) | 139.3 ± 7.11 | 138.86 ± 9.56 | 139.4 ± 6.53 | 0.211 |
| K (mEq/L) | 4.32 ± 0.85 | 4.56 ± 1.07 | 4.28 ± 0.79 | <0.0001 |
| Use of vasoactive drug | 201 (9.2) | 93 (27.1) | 108 (5.9) | <0.0001 |
| Use of mechanical ventilation | 347 (15.9) | 149 (43.4) | 198 (10.8) | <0.0001 |
| C-reactive Protein (mg/L) | 84.64 ± 69.73 | 136.75 ± 63.45 | 74.37 ± 66.25 | <0.0001 |
| Length of stay prior to ICU admission (days) | 2.37 ± 11.31 | 4.12 ± 11.20 | 2.05 ± 11.30 | 0.002 |
| ICU Duration (days) | 8.04 ± 13.30 | 16.08 ± 24.20 | 6.54 ± 9.31 | <0.0001 |
| ICU readmission | 200 (9.2) | 49 (2.2) | 151 (8.2) | <0.0001 |
Results expressed by number (%), mean ± standard deviation (SD). MAP = Mean arterial pressure; HR = heart rate; RR = Respiratory rate.
When comparing the BMI groups, the underweight participants had significantly different characteristics. They were older and had a longer length of stay prior to ICU admission and lower mean arterial pressure. A third of this group had an infection as the main diagnosis, in addition to a higher prevalence of comorbidities such as cancer, stroke, and dementia. In contrast, overweight and obese patients had a higher frequency of admissions for surgery and cardiovascular pathologies. No significant difference was observed regarding the need for organic support in ICU (Table 2). There were 343 (15.7%) deaths reported in the ICU during the study period. Especially among the underweight group, there was a higher mortality rate, accompanied by higher scores on the modified Frailty Index (MFI), CCI, and SAPS3 (Table 2). Multiple comparisons between each BMI group are represented in Tables 3 and 4.
Table 2.
Comparison between BMI groups.
| Characteristics | Underweight (n = 171) |
Normal weight (n = 914) |
Overweight (n = 700) |
Obese Grade I (n = 272) |
Obese Grade II/III (n = 122) |
p-value |
|---|---|---|---|---|---|---|
| Age (years; mean, SD) | 76.06 ± 16.39 | 69.48 ± 18.51 | 66.10 ± 16.73 | 64.67 ± 16.19 | 62.40 ± 18.78 | <0.0001 |
| Gender, female (n, %) | 98 (57.3) | 438 (47.9) | 356 (50.9) | 176 (64.7) | 90 (73.8) | <0.0001 |
| SAPS3 (mean, SD) | 54.06 ± 11.49 | 48.52 ± 12.68 | 44.63 ± 11.49 | 43.01 ± 11.87 | 44.02 ± 12.39 | <0.0001 |
| CCI (mean, SD) | 2.06 ± 1.90 | 1.75 ± 1.84 | 1.55 ± 1.68 | 1.28 ± 1.63 | 1.24 ± 1.50 | <0.0001 |
| MFI (mean, SD) | 1.94 ± 1.30 | 1.62 ± 1.30 | 1.68 ± 1.21 | 1.67 ± 1.06 | 1.75 ± 1.08 | 0.040 |
| Admission Diagnosis (n, %) | <0.0001 | |||||
| Cardiovascular | 25 (14.6) | 152 (16.6) | 160 (22.9) | 81 (29.8) | 34 (27.9) | |
| Respiratory | 13 (7.6) | 55 (6.0) | 40 (5.7) | 13 (4.8) | 5 (4.1) | |
| Neurological | 22 (12.9) | 171 (18.7) | 115 (16.4) | 41 (15.1) | 11 (9.0) | |
| Infectious | 57 (33.3) | 184 (20.1) | 96 (13.7) | 30 (11.0) | 25 (20.5) | |
| Surgical | 10 (5.8) | 141 (15.4) | 143 (20.4) | 65 (23.9) | 21 (17.2) | |
| Other | 44 (25.7) | 211 (23.1) | 146 (20.9) | 42 (15.4) | 26 (21.3) | |
| Use of VAD (n, %) | 21 (12.3) | 86 (9.4) | 60 (8.6) | 27 (9.9) | 7 (5.7) | 0.375 |
| Use of MV (n, %) | 32 (18.7) | 157 (17.2) | 110 (15.7) | 38 (14.0) | 10 (8.2) | 0.081 |
| Length of stay prior to ICU (days) | 4.95 ± 16.70 | 2.95 ± 14.58 | 1.65 ± 6.28 | 1.22 ± 4.77 | 1.08 ± 3.47 | 0.001 |
| ICU length of stay (days) | 9.77 ± 12.86 | 9.34 ± 15.85 | 6.84 ± 10.74 | 6.79 ± 12.07 | 5.58 ± 5.51 | <0.0001 |
| Congestive Heart Failure (n, %) | 11 (6.4) | 59 (6.5) | 44 (6.3) | 13 (4.8) | 5 (4.1) | 0.257 |
| Chronic Kidney Disease (n, %) | 17 (9.9) | 119 (13.0) | 82 (11.7) | 26 (9.6) | 7 (5.7) | 0.021 |
| Cirrhosis (n, %) | 1 (0.6) | 9 (1.0) | 14 (2.0) | 3 (1.1) | 1 (0.8) | 0.453 |
| Cancer (n, %) | 29 (17.0) | 149 (16.3) | 90 (12.9) | 23 (8.5) | 11 (9.0) | 0.004 |
| Immunodeficiency (n, %) | 2 (1.2) | 17 (1.9) | 4 (0.6) | 3 (1.1) | 1 (0.8) | 0.056 |
| Diabetes Mellitus (n, %) | 61 (35.7) | 315 (34.5) | 277 (39.6) | 108 (39.7) | 56 (45.9) | 0.003 |
| Coronary Artery Disease (n, %) | 12 (7.0) | 86 (9.4) | 106 (15.1) | 23 (8.5) | 14 (11.5) | 0.098 |
| Stroke (n, %) | 41 (24.0) | 157 (17.2) | 96 (13.7) | 35 (12.9) | 11 (9.0) | 0.002 |
| Dementia (n, %) | 29 (17.0) | 60 (6.6) | 25 (3.6) | 7 (2.6) | 4 (3.3) | <0.0001 |
| Performance status (n, %) | <0.0001 | |||||
| Completely independent | 113 (66.1) | 778 (85.1) | 641 (91.6) | 245 (90.1) | 109 (89.3) | |
| Partially independent | 18 (10.5) | 65 (7.1) | 39 (5.6) | 18 (6.6) | 8 (6.6) | |
| Fully dependent | 40 (23.4) | 71 (7.8) | 20 (2.9) | 9 (3.3) | 5 (4.1) | |
| Clinical and Laboratory (mean, SD) | ||||||
| Mean arterial pressure (mmHg) | 91.88 ± 21.22 | 97.45 ± 20.80 | 99.73 ± 20.22 | 102.45 ± 20.71 | 101.32 ± 21.53 | <0.0001 |
| Heart rate (bpm) | 89.70 ± 21.04 | 86.31 ± 20.83 | 84.46 ± 19.55 | 82.57 ± 19.17 | 87.90 ± 21.52 | 0.001 |
| Respiratory rate (ipm) | 21.21 ± 4.98 | 20.10 ± 4.43 | 20.23 ± 4.34 | 19.83 ± 4.55 | 20.45 ± 4.21 | 0.021 |
| Creatinine (mg/dL) | 1.40 ± 2.27 | 1.49 ± 2.28 | 1.52 ± 2.63 | 1.26 ± 1.82 | 1.08 ± 1.10 | 0.249 |
| Platelets (x103) | 252.5 ± 136.0 | 239.7 ± 113.7 | 227.3 ± 110.3 | 221.1 ± 76.0 | 259.8 ± 149.3 | 0.001 |
| Hematocrit (%) | 32.34 ± 6.75 | 34.17 ± 7.58 | 35.20 ± 7.38 | 36.75 ± 6.65 | 36.10 ± 5.94 | <0.0001 |
| Na (mEq/L) | 140.2 ± 8.87 | 138.7 ± 7.68 | 139.7 ± 6.25 | 140.0 ± 6.48 | 139.1 ± 5.40 | 0.014 |
| C Reactive Protein (mg/dL) | 96.77 ± 64.73 | 91.38 ± 70.15 | 79.53 ± 70.15 | 72.48 ± 67.35 | 73.09 ± 68.99 | <0.0001 |
| ICU deaths (n, %) | 64 (37.4) | 172 (18.8) | 76 (10.9) | 21 (7.7) | 10 (8.2) | <0.0001 |
Results expressed by number (%), mean ± standard deviation (SD). CCI = Charlson Comorbidity Index, MFI = Modified Frailty Index, ICU = Intensive care unit; VAD = Vasoactive drug; MV = Mechanical ventilation; bpm = beats per minute; incursions per minute.
Table 3.
Multiple comparisons between BMI categories.
| Variable | BMI Reference category | BMI comparison group | Mean difference (95% CI) | Error2 | p-value |
|---|---|---|---|---|---|
| Age | Underweight | Normal weight | 6,58 (2,48; 10,69) | 1.46 | 0.001 |
| Overweight | 9,97 (5,77; 14,17) | 1.5 | 0.001 | ||
| Obese grade I | 11,39 (6,58; 16,2) | 1.71 | 0.001 | ||
| Obese grade II/III | 13,66 (7,82; 19,5) | 2.08 | 0.001 | ||
| Normal weight | Underweight | -6,58 (-10,69; -2,48) | 1.46 | 0.001 | |
| Overweight | 3,39 (0,91; 5,86) | 0.88 | 0.001 | ||
| Obese grade I | 4,81 (1,41; 8,21) | 1.21 | 0.001 | ||
| Obese grade II/III | 7,08 (2,33; 11,83) | 1.69 | 0.001 | ||
| Overweight | Underweight | -9,97 (-14,17; -5,77) | 1.5 | 0.001 | |
| Normal weight | -3,39 (-5,86; -0,91) | 0.88 | 0.001 | ||
| Obese grade I | 1,42 (-2,1; 4,94) | 1.25 | 0.787 | ||
| Obese grade II/III | 3,7 (-1,14; 8,53) | 1.72 | 0.2 | ||
| Obese grade I | Underweight | -11,39 (-16,2; -6,58) | 1.71 | 0.001 | |
| Normal weight | -4,81 (-8,21; -1,41) | 1.21 | 0.001 | ||
| Overweight | -1,42 (-4,94; 2,1) | 1.25 | 0.787 | ||
| Obese grade II/III | 2,27 (-3,1; 7,64) | 1.91 | 0.758 | ||
| Obese grade II/III | Underweight | -13,66 (-19,5; -7,82) | 2.08 | 0.001 | |
| Normal weight | -7,08 (-11,83; -2,33) | 1.69 | 0.001 | ||
| Overweight | -3,7 (-8,53; 1,14) | 1.72 | 0.2 | ||
| Obese grade I | -2,27 (-7,64; 3,1) | 1.91 | 0.758 | ||
| SAPS3 | Underweight | Normal weight | 5,55 (2,71; 8,38) | 1.01 | 0.001 |
| Overweight | 9,43 (6,53; 12,33) | 1.03 | 0.001 | ||
| Obese grade I | 10,96 (7,64; 14,28) | 1.18 | 0.001 | ||
| Obese grade II/III | 10,04 (6,01; 14,07) | 1.43 | 0.001 | ||
| Normal weight | Underweight | -5,55 (-8,38; -2,71) | 1.01 | 0.001 | |
| Overweight | 3,88 (2,18; 5,59) | 0.61 | 0.001 | ||
| Obese grade I | 5,42 (3,07; 7,77) | 0.84 | 0.001 | ||
| Obese grade II/III | 4,5 (1,22; 7,77) | 1.17 | 0.001 | ||
| Overweight | Underweight | -9,43 (-12,33; -6,53) | 1.03 | 0.001 | |
| Normal weight | -3,88 (-5,59; -2,18) | 0.61 | 0.001 | ||
| Obese grade I | 1,53 (-0,9; 3,96) | 0.87 | 0.39 | ||
| Obese grade II/III | 0,61 (-2,72; 3,95) | 1.19 | 0.986 | ||
| Obese grade I | Underweight | -10,96 (-14,28; -7,64) | 1.18 | 0.001 | |
| Normal weight | -5,42 (-7,77; -3,07) | 0.84 | 0.001 | ||
| Overweight | -1,53 (-3,96; 0,9) | 0.87 | 0.39 | ||
| Obese grade II/III | -0,92 (-4,63; 2,78) | 1.32 | 0.957 | ||
| Obese grade II/III | Underweight | -10,04 (-14,07; -6,01) | 1.43 | 0.001 | |
| Normal weight | -4,5 (-7,77; -1,22) | 1.17 | 0.001 | ||
| Overweight | -0,61 (-3,95; 2,72) | 1.19 | 0.986 | ||
| Obese grade I | 0,92 (-2,78; 4,63) | 1.32 | 0.957 | ||
| CCI | Underweight | Normal weight | 0,31 (-0,1; 0,72) | 0.15 | 0.205 |
| Overweight | 0,51 (0,09; 0,93) | 0.15 | 0.006 | ||
| Obese grade I | 0,78 (0,29; 1,26) | 0.17 | 0.001 | ||
| Obese grade II/III | 0,82 (0,24; 1,4) | 0.21 | 0.001 | ||
| Normal weight | Underweight | -0,31 (-0,72; 0,1) | 0.15 | 0.205 | |
| Overweight | 0,2 (-0,05; 0,45) | 0.09 | 0.153 | ||
| Obese grade I | 0,46 (0,12; 0,8) | 0.12 | 0.001 | ||
| Obese grade II/III | 0,51 (0,03; 0,98) | 0.17 | 0.022 | ||
| Overweight | Underweight | -0,51 (-0,93; -0,09) | 0.15 | 0.006 | |
| Normal weight | -0,2 (-0,45; 0,05) | 0.09 | 0.153 | ||
| Obese grade I | 0,26 (-0,09; 0,61) | 0.13 | 0.222 | ||
| Obese grade II/III | 0,31 (-0,18; 0,79) | 0.17 | 0.38 | ||
| Obese grade I | Underweight | -0,78 (-1,26; -0,29) | 0.17 | 0.001 | |
| Normal weight | -0,46 (-0,8; -0,12) | 0.12 | 0.001 | ||
| Overweight | -0,26 (-0,61; 0,09) | 0.13 | 0.222 | ||
| Obese grade II/III | 0,05 (-0,49; 0,58) | 0.19 | 0.999 | ||
| Obese grade II/III | Underweight | -0,82 (-1,4; -0,24) | 0.21 | 0.001 | |
| Normal weight | -0,51 (-0,98; -0,03) | 0.17 | 0.022 | ||
| Overweight | -0,31 (-0,79; 0,18) | 0.17 | 0.38 | ||
| Obese grade I | -0,05 (-0,58; 0,49) | 0.19 | 0.999 | ||
| MFI | Underweight | Normal weight | 0,32 (0,03; 0,61) | 0.01 | 0.016 |
| Overweight | 0,26 (-0,03; 0,56) | 0.01 | 0.091 | ||
| Obese grade I | 0,27 (-0,07; 0,61) | 0.01 | 0.168 | ||
| Obese grade II/III | 0,2 (-0,22; 0,61) | 0.01 | 0.665 | ||
| Normal weight | Underweight | -0,32 (-0,61; -0,03) | 0.01 | 0.016 | |
| Overweight | -0,06 (-0,23; 0,12) | 0.01 | 0.893 | ||
| Obese grade I | -0,05 (-0,29; 0,19) | 0.01 | 0.976 | ||
| Obese grade II/III | -0,12 (-0,46; 0,21) | 0.01 | 0.839 | ||
| Overweight | Underweight | -0,26 (-0,56; 0,03) | 0.01 | 0.091 | |
| Normal weight | 0,06 (-0,12; 0,23) | 0.01 | 0.893 | ||
| Obese grade I | 0,01 (-0,24; 0,25) | 0.01 | 1 | ||
| Obese grade II/III | -0,07 (-0,41; 0,27) | 0.01 | 0.982 | ||
| Obese grade I | Underweight | -0,27 (-0,61; 0,07) | 0.01 | 0.168 | |
| Normal weight | 0,05 (-0,19; 0,29) | 0.01 | 0.976 | ||
| Overweight | -0,01 (-0,25; 0,24) | 0.01 | 1 | ||
| Obese grade II/III | -0,07 (-0,45; 0,3) | 0.01 | 0.983 | ||
| Obese grade II/III | Underweight | -0,2 (-0,61; 0,22) | 0.01 | 0.665 | |
| Normal weight | 0,12 (-0,21; 0,46) | 0.01 | 0.839 | ||
| Overweight | 0,07 (-0,27; 0,41) | 0.01 | 0.982 | ||
| Obese grade I | 0,07 (-0,3; 0,45) | 0.01 | 0.983 | ||
| Length of stay prior to ICU | Underweight | Normal weight | 0,43 (-2,67; 3,54) | 0.94 | 0.211 |
| Overweight | 2,93 (-0,24; 6,11) | 0.96 | 0.006 | ||
| Obese grade I | 2,98 (-0,65; 6,61) | 1.1 | 0.007 | ||
| Obese grade II/III | 4,19 (-0,22; 8,6) | 1.34 | 0.031 | ||
| Normal weight | Underweight | -0,43 (-3,54; 2,67) | 0.94 | 0.211 | |
| Overweight | 2,5 (0,63; 4,37) | 0.57 | 0.15 | ||
| Obese grade I | 2,55 (-0,02; 5,12) | 0.79 | 0.179 | ||
| Obese grade II/III | 3,76 (0,17; 7,34) | 1.09 | 0.422 | ||
| Overweight | Underweight | -2,93 (-6,11; 0,24) | 0.96 | 0.006 | |
| Normal weight | -2,5 (-4,37; -0,63) | 0.57 | 0.15 | ||
| Obese grade I | 0,05 (-2,61; 2,71) | 0.81 | 0.985 | ||
| Obese grade II/III | 1,26 (-2,4; 4,91) | 1.11 | 0.986 | ||
| Obese grade I | Underweight | -2,98 (-6,61; 0,65) | 1.1 | 0.007 | |
| Normal weight | -2,55 (-5,12; 0,02) | 0.79 | 0.179 | ||
| Overweight | -0,05 (-2,71; 2,61) | 0.81 | 0.985 | ||
| Obese grade II/III | 1,21 (-2,85; 5,26) | 1.23 | 1 | ||
| Obese grade II/III | Underweight | -4,19 (-8,6; 0,22) | 1.34 | 0.031 | |
| Normal weight | -3,76 (-7,34; -0,17) | 1.09 | 0.422 | ||
| Overweight | -1,26 (-4,91; 2,4) | 1.11 | 0.986 | ||
| Obese grade I | -1,21 (-5,26; 2,85) | 1.23 | 1 | ||
| ICU length of stay | Underweight | Normal weight | 2 (-0,65; 4,64) | 1.1 | 0.995 |
| Overweight | 3,3 (0,59; 6) | 1.13 | 0.071 | ||
| Obese grade I | 3,72 (0,62; 6,82) | 1.29 | 0.143 | ||
| Obese grade II/III | 3,87 (0,11; 7,62) | 1.57 | 0.059 | ||
| Normal weight | Underweight | -2 (-4,64; 0,65) | 1.1 | 0.995 | |
| Overweight | 1,3 (-0,3; 2,9) | 0.67 | 0.002 | ||
| Obese grade I | 1,73 (-0,48; 3,93) | 0.92 | 0.043 | ||
| Obese grade II/III | 1,87 (-1,19; 4,93) | 1.28 | 0.027 | ||
| Overweight | Underweight | -3,3 (-6; -0,59) | 1.13 | 0.071 | |
| Normal weight | -1,3 (-2,9; 0,3) | 0.67 | 0.002 | ||
| Obese grade I | 0,43 (-1,85; 2,7) | 0.95 | 1 | ||
| Obese grade II/III | 0,57 (-2,54; 3,68) | 1.3 | 0.87 | ||
| Obese grade I | Underweight | -3,72 (-6,82; -0,62) | 1.29 | 0.143 | |
| Normal weight | -1,73 (-3,93; 0,48) | 0.92 | 0.043 | ||
| Overweight | -0,43 (-2,7; 1,85) | 0.95 | 1 | ||
| Obese grade II/III | 0,14 (-3,32; 3,6) | 1.44 | 0.919 | ||
| Obese grade II/III | Underweight | -3,87 (-7,62; -0,11) | 1.57 | 0.059 | |
| Normal weight | -1,87 (-4,93; 1,19) | 1.28 | 0.027 | ||
| Overweight | -0,57 (-3,68; 2,54) | 1.3 | 0.87 | ||
| Obese grade I | -0,14 (-3,6; 3,32) | 1.44 | 0.919 | ||
| Hospital length of stay | Underweight | Normal weight | 1,33 (-3,63; 6,29) | 1.77 | 0.944 |
| Overweight | 6,5 (1,42; 11,58) | 1.81 | 0.003 | ||
| Obese grade I | 7,95 (2,14; 13,76) | 2.07 | 0.001 | ||
| Obese grade II/III | 7,58 (0,53; 14,64) | 2.51 | 0.022 | ||
| Normal weight | Underweight | -1,33 (-6,29; 3,63) | 1.77 | 0.944 | |
| Overweight | 5,17 (2,18; 8,16) | 1.06 | 0.001 | ||
| Obese grade I | 6,62 (2,51; 10,74) | 1.46 | 0.001 | ||
| Obese grade II/III | 6,25 (0,51; 11,99) | 2.04 | 0.019 | ||
| Overweight | Underweight | -6,5 (-11,58; -1,42) | 1.81 | 0.003 | |
| Normal weight | -5,17 (-8,16; -2,18) | 1.06 | 0.001 | ||
| Obese grade I | 1,45 (-2,8; 5,71) | 1.51 | 0.873 | ||
| Obese grade II/III | 1,08 (-4,76; 6,92) | 2.08 | 0.985 | ||
| Obese grade I | Underweight | -7,95 (-13,76; -2,14) | 2.07 | 0.001 | |
| Normal weight | -6,62 (-10,74; -2,51) | 1.46 | 0.001 | ||
| Overweight | -1,45 (-5,71; 2,8) | 1.51 | 0.873 | ||
| Obese grade II/III | -0,37 (-6,86; 6,11) | 2.31 | 1 | ||
| Obese grade II/III | Underweight | -7,58 (-14,64; -0,53) | 2.51 | 0.022 | |
| Normal weight | -6,25 (-11,99; -0,51) | 2.04 | 0.019 | ||
| Overweight | -1,08 (-6,92; 4,76) | 2.08 | 0.985 | ||
| Obese grade I | 0,37 (-6,11; 6,86) | 2.31 | 1 | ||
| Mean arterial pressure | Underweight | Normal weight | -5,57 (-10,41; -0,72) | 1.72 | 0.011 |
| Overweight | -7,85 (-12,81; -2,89) | 1.77 | 0.001 | ||
| Obese grade I | -10,56 (-16,24; -4,89) | 2.02 | 0.001 | ||
| Obese grade II/III | -9,44 (-16,34; -2,53) | 2.46 | 0.001 | ||
| Normal weight | Underweight | 5,57 (0,72; 10,41) | 1.72 | 0.011 | |
| Overweight | -2,28 (-5,21; 0,65) | 1.04 | 0.185 | ||
| Obese grade I | -5 (-9,01; -0,98) | 1.43 | 0.004 | ||
| Obese grade II/III | -3,87 (-9,49; 1,76) | 2 | 0.3 | ||
| Overweight | Underweight | 7,85 (2,89; 12,81) | 1.77 | 0.001 | |
| Normal weight | 2,28 (-0,65; 5,21) | 1.04 | 0.185 | ||
| Obese grade I | -2,72 (-6,87; 1,44) | 1.48 | 0.353 | ||
| Obese grade II/III | -1,59 (-7,31; 4,14) | 2.04 | 0.936 | ||
| Obese grade I | Underweight | 10,56 (4,89; 16,24) | 2.02 | 0.001 | |
| Normal weight | 5 (0,98; 9,01) | 1.43 | 0.004 | ||
| Overweight | 2,72 (-1,44; 6,87) | 1.48 | 0.353 | ||
| Obese grade II/III | 1,13 (-5,23; 7,48) | 2.26 | 0.988 | ||
| Obese grade II/III | Underweight | 9,44 (2,53; 16,34) | 2.46 | 0.001 | |
| Normal weight | 3,87 (-1,76; 9,49) | 2 | 0.3 | ||
| Overweight | 1,59 (-4,14; 7,31) | 2.04 | 0.936 | ||
| Obese grade I | -1,13 (-7,48; 5,23) | 2.26 | 0.988 | ||
| Heart rate | Underweight | Normal weight | 3,39 (-1,36; 8,14) | 1.69 | 0.262 |
| Overweight | 5,24 (0,38; 10,11) | 1.73 | 0.021 | ||
| Obese grade I | 7,14 (1,57; 12,7) | 1.98 | 0.003 | ||
| Obese grade II/III | 1,8 (-4,97; 8,57) | 2.41 | 0.945 | ||
| Normal weight | Underweight | -3,39 (-8,14; 1,36) | 1.69 | 0.262 | |
| Overweight | 1,85 (-1,02; 4,71) | 1.02 | 0.368 | ||
| Obese grade I | 3,74 (-0,2; 7,68) | 1.4 | 0.059 | ||
| Obese grade II/III | -1,59 (-7,11; 3,92) | 1.96 | 0.927 | ||
| Overweight | Underweight | -5,24 (-10,11; -0,38) | 1.73 | 0.021 | |
| Normal weight | -1,85 (-4,71; 1,02) | 1.02 | 0.368 | ||
| Obese grade I | 1,9 (-2,18; 5,97) | 1.45 | 0.687 | ||
| Obese grade II/III | -3,44 (-9,05; 2,17) | 2 | 0.421 | ||
| Obese grade I | Underweight | -7,14 (-12,7; -1,57) | 1.98 | 0.003 | |
| Normal weight | -3,74 (-7,68; 0,2) | 1.4 | 0.059 | ||
| Overweight | -1,9 (-5,97; 2,18) | 1.45 | 0.687 | ||
| Obese grade II/III | -5,34 (-11,56; 0,89) | 2.22 | 0.114 | ||
| Obese grade II/III | Underweight | -1,8 (-8,57; 4,97) | 2.41 | 0.945 | |
| Normal weight | 1,59 (-3,92; 7,11) | 1.96 | 0.927 | ||
| Overweight | 3,44 (-2,17; 9,05) | 2 | 0.421 | ||
| Obese grade I | 5,34 (-0,89; 11,56) | 2.22 | 0.114 | ||
| Respiratory rate | Underweight | Normal weight | 1,12 (0,07; 2,16) | 0.37 | 0.023 |
| Overweight | 0,98 (-0,08; 2,05) | 0.38 | 0.073 | ||
| Obese grade I | 1,38 (0,16; 2,61) | 0.44 | 0.013 | ||
| Obese grade II/III | 0,76 (-0,73; 2,25) | 0.53 | 0.606 | ||
| Normal weight | Underweight | -1,12 (-2,16; -0,07) | 0.37 | 0.023 | |
| Overweight | -0,13 (-0,76; 0,5) | 0.22 | 0.977 | ||
| Obese grade I | 0,27 (-0,6; 1,13) | 0.31 | 0.907 | ||
| Obese grade II/III | -0,36 (-1,57; 0,86) | 0.43 | 0.925 | ||
| Overweight | Underweight | -0,98 (-2,05; 0,08) | 0.38 | 0.073 | |
| Normal weight | 0,13 (-0,5; 0,76) | 0.22 | 0.977 | ||
| Obese grade I | 0,4 (-0,5; 1,29) | 0.32 | 0.72 | ||
| Obese grade II/III | -0,22 (-1,46; 1,01) | 0.44 | 0.987 | ||
| Obese grade I | Underweight | -1,38 (-2,61; -0,16) | 0.44 | 0.013 | |
| Normal weight | -0,27 (-1,13; 0,6) | 0.31 | 0.907 | ||
| Overweight | -0,4 (-1,29; 0,5) | 0.32 | 0.72 | ||
| Obese grade II/III | -0,62 (-2; 0,75) | 0.49 | 0.707 | ||
| Obese grade II/III | Underweight | -0,76 (-2,25; 0,73) | 0.53 | 0.606 | |
| Normal weight | 0,36 (-0,86; 1,57) | 0.43 | 0.925 | ||
| Overweight | 0,22 (-1,01; 1,46) | 0.44 | 0.987 | ||
| Obese grade I | 0,62 (-0,75; 2) | 0.49 | 0.707 | ||
| Temperature | Underweight | Normal weight | -0,13 (-0,38; 0,12) | 0.09 | 0.598 |
| Overweight | -0,11 (-0,37; 0,15) | 0.09 | 0.755 | ||
| Obese grade I | -0,14 (-0,44; 0,15) | 0.1 | 0.64 | ||
| Obese grade II/III | -0,11 (-0,46; 0,25) | 0.13 | 0.917 | ||
| Normal weight | Underweight | 0,13 (-0,12; 0,38) | 0.09 | 0.598 | |
| Overweight | 0,02 (-0,13; 0,17) | 0.05 | 0.996 | ||
| Obese grade I | -0,02 (-0,22; 0,19) | 0.07 | 1 | ||
| Obese grade II/III | 0,02 (-0,27; 0,31) | 0.1 | 1 | ||
| Overweight | Underweight | 0,11 (-0,15; 0,37) | 0.09 | 0.755 | |
| Normal weight | -0,02 (-0,17; 0,13) | 0.05 | 0.996 | ||
| Obese grade I | -0,03 (-0,25; 0,18) | 0.08 | 0.991 | ||
| Obese grade II/III | 0 (-0,29; 0,3) | 0.1 | 1 | ||
| Obese grade I | Underweight | 0,14 (-0,15; 0,44) | 0.1 | 0.64 | |
| Normal weight | 0,02 (-0,19; 0,22) | 0.07 | 1 | ||
| Overweight | 0,03 (-0,18; 0,25) | 0.08 | 0.991 | ||
| Obese grade II/III | 0,04 (-0,29; 0,36) | 0.12 | 0.998 | ||
| Obese grade II/III | Underweight | 0,11 (-0,25; 0,46) | 0.13 | 0.917 | |
| Normal weight | -0,02 (-0,31; 0,27) | 0.1 | 1 | ||
| Overweight | 0 (-0,3; 0,29) | 0.1 | 1 | ||
| Obese grade I | -0,04 (-0,36; 0,29) | 0.12 | 0.998 | ||
| Creatinine | Underweight | Normal weight | -0,08 (-0,65; 0,49) | 0.2 | 0.994 |
| Overweight | -0,11 (-0,7; 0,47) | 0.21 | 0.983 | ||
| Obese grade I | 0,14 (-0,52; 0,81) | 0.24 | 0.974 | ||
| Obese grade II/III | 0,32 (-0,48; 1,12) | 0.28 | 0.793 | ||
| Normal weight | Underweight | 0,08 (-0,49; 0,65) | 0.2 | 0.994 | |
| Overweight | -0,03 (-0,37; 0,31) | 0.12 | 0.999 | ||
| Obese grade I | 0,23 (-0,24; 0,69) | 0.17 | 0.646 | ||
| Obese grade II/III | 0,4 (-0,24; 1,04) | 0.23 | 0.393 | ||
| Overweight | Underweight | 0,11 (-0,47; 0,7) | 0.21 | 0.983 | |
| Normal weight | 0,03 (-0,31; 0,37) | 0.12 | 0.999 | ||
| Obese grade I | 0,26 (-0,23; 0,74) | 0.17 | 0.565 | ||
| Obese grade II/III | 0,43 (-0,22; 1,09) | 0.23 | 0.339 | ||
| Obese grade I | Underweight | -0,14 (-0,81; 0,52) | 0.24 | 0.974 | |
| Normal weight | -0,23 (-0,69; 0,24) | 0.17 | 0.646 | ||
| Overweight | -0,26 (-0,74; 0,23) | 0.17 | 0.565 | ||
| Obese grade II/III | 0,18 (-0,55; 0,9) | 0.26 | 0.96 | ||
| Obese grade II/III | Underweight | -0,32 (-1,12; 0,48) | 0.28 | 0.793 | |
| Normal weight | -0,4 (-1,04; 0,24) | 0.23 | 0.393 | ||
| Overweight | -0,43 (-1,09; 0,22) | 0.23 | 0.339 | ||
| Obese grade I | -0,18 (-0,9; 0,55) | 0.26 | 0.96 | ||
| Platelets | Underweight | Normal weight | 12,75 (-14,8; 40,29) | 9.8 | 0.691 |
| Overweight | 25,15 (-3,07; 53,38) | 10.04 | 0.09 | ||
| Obese grade I | 31,41 (-0,81; 63,62) | 11.46 | 0.049 | ||
| Obese grade II/III | -7,35 (-46,3; 31,59) | 13.86 | 0.984 | ||
| Normal weight | Underweight | -12,75 (-40,29; 14,8) | 9.8 | 0.691 | |
| Overweight | 12,41 (-4,11; 28,92) | 5.88 | 0.216 | ||
| Obese grade I | 18,66 (-4,01; 41,33) | 8.07 | 0.141 | ||
| Obese grade II/III | -20,1 (-51,61; 11,41) | 11.21 | 0.378 | ||
| Overweight | Underweight | -25,15 (-53,38; 3,07) | 10.04 | 0.09 | |
| Normal weight | -12,41 (-28,92; 4,11) | 5.88 | 0.216 | ||
| Obese grade I | 6,26 (-17,23; 29,75) | 8.36 | 0.945 | ||
| Obese grade II/III | -32,51 (-64,61; -0,4) | 11.43 | 0.036 | ||
| Obese grade I | Underweight | -31,41 (-63,62; 0,81) | 11.46 | 0.049 | |
| Normal weight | -18,66 (-41,33; 4,01) | 8.07 | 0.141 | ||
| Overweight | -6,26 (-29,75; 17,23) | 8.36 | 0.945 | ||
| Obese grade II/III | -38,76 (-74,42; -3,1) | 12.69 | 0.019 | ||
| Obese grade II/III | Underweight | 7,35 (-31,59; 46,3) | 13.86 | 0.984 | |
| Normal weight | 20,1 (-11,41; 51,61) | 11.21 | 0.378 | ||
| Overweight | 32,51 (0,4; 64,61) | 11.43 | 0.036 | ||
| Obese grade I | 38,76 (3,1; 74,42) | 12.69 | 0.019 | ||
| Hematocrit | Underweight | Normal weight | -1,83 (-3,6; -0,06) | 0.63 | 0.031 |
| Overweight | -2,86 (-4,68; -1,04) | 0.65 | 0.001 | ||
| Obese grade I | -4,41 (-6,48; -2,34) | 0.74 | 0.001 | ||
| Obese grade II/III | -3,75 (-6,26; -1,25) | 0.89 | 0.001 | ||
| Normal weight | Underweight | 1,83 (0,06; 3,6) | 0.63 | 0.031 | |
| Overweight | -1,03 (-2,09; 0,03) | 0.38 | 0.051 | ||
| Obese grade I | -2,58 (-4,04; -1,12) | 0.52 | 0.001 | ||
| Obese grade II/III | -1,92 (-3,95; 0,1) | 0.72 | 0.059 | ||
| Overweight | Underweight | 2,86 (1,04; 4,68) | 0.65 | 0.001 | |
| Normal weight | 1,03 (-0,03; 2,09) | 0.38 | 0.051 | ||
| Obese grade I | -1,55 (-3,06; -0,04) | 0.54 | 0.032 | ||
| Obese grade II/III | -0,89 (-2,96; 1,17) | 0.74 | 0.742 | ||
| Obese grade I | Underweight | 4,41 (2,34; 6,48) | 0.74 | 0.001 | |
| Normal weight | 2,58 (1,12; 4,04) | 0.52 | 0.001 | ||
| Overweight | 1,55 (0,04; 3,06) | 0.54 | 0.032 | ||
| Obese grade II/III | 0,66 (-1,64; 2,95) | 0.82 | 0.929 | ||
| Obese grade II/III | Underweight | 3,75 (1,25; 6,26) | 0.89 | 0.001 | |
| Normal weight | 1,92 (-0,1; 3,95) | 0.72 | 0.059 | ||
| Overweight | 0,89 (-1,17; 2,96) | 0.74 | 0.742 | ||
| Obese grade I | -0,66 (-2,95; 1,64) | 0.82 | 0.929 | ||
| Leukocytes | Underweight | Normal weight | 0,55 (-2,18; 3,28) | 0.97 | 0.98 |
| Overweight | 0,53 (-2,27; 3,32) | 0.99 | 0.984 | ||
| Obese grade I | 0,84 (-2,35; 4,03) | 1.14 | 0.946 | ||
| Obese grade II/III | -0,48 (-4,34; 3,37) | 1.37 | 0.997 | ||
| Normal weight | Underweight | -0,55 (-3,28; 2,18) | 0.97 | 0.98 | |
| Overweight | -0,02 (-1,66; 1,62) | 0.58 | 1 | ||
| Obese grade I | 0,3 (-1,95; 2,54) | 0.8 | 0.996 | ||
| Obese grade II/III | -1,03 (-4,15; 2,09) | 1.11 | 0.886 | ||
| Overweight | Underweight | -0,53 (-3,32; 2,27) | 0.99 | 0.984 | |
| Normal weight | 0,02 (-1,62; 1,66) | 0.58 | 1 | ||
| Obese grade I | 0,32 (-2,01; 2,64) | 0.83 | 0.996 | ||
| Obese grade II/III | -1,01 (-4,19; 2,17) | 1.13 | 0.899 | ||
| Obese grade I | Underweight | -0,84 (-4,03; 2,35) | 1.14 | 0.946 | |
| Normal weight | -0,3 (-2,54; 1,95) | 0.8 | 0.996 | ||
| Overweight | -0,32 (-2,64; 2,01) | 0.83 | 0.996 | ||
| Obese grade II/III | -1,33 (-4,86; 2,21) | 1.26 | 0.829 | ||
| Obese grade II/III | Underweight | 0,48 (-3,37; 4,34) | 1.37 | 0.997 | |
| Normal weight | 1,03 (-2,09; 4,15) | 1.11 | 0.886 | ||
| Overweight | 1,01 (-2,17; 4,19) | 1.13 | 0.899 | ||
| Obese grade I | 1,33 (-2,21; 4,86) | 1.26 | 0.829 | ||
| Segmented neutrophils | Underweight | Normal weight | 498,96 (-898,42; 1896,34) | 497.27 | 0.854 |
| Overweight | 1178,21 (-253,81; 2610,23) | 509.59 | 0.141 | ||
| Obese grade I | 1036,11 (-597,74; 2669,96) | 581.42 | 0.384 | ||
| Obese grade II/III | -244,51 (-2219,86; 1730,84) | 702.94 | 0.997 | ||
| Normal weight | Underweight | -498,96 (-1896,34; 898,42) | 497.27 | 0.854 | |
| Overweight | 679,25 (-159,73; 1518,23) | 298.56 | 0.153 | ||
| Obese grade I | 537,15 (-612,92; 1687,22) | 409.26 | 0.683 | ||
| Obese grade II/III | -743,47 (-2341,97; 855,02) | 568.84 | 0.687 | ||
| Overweight | Underweight | -1178,21 (-2610,23; 253,81) | 509.59 | 0.141 | |
| Normal weight | -679,25 (-1518,23; 159,73) | 298.56 | 0.153 | ||
| Obese grade I | -142,1 (-1334,02; 1049,82) | 424.15 | 0.997 | ||
| Obese grade II/III | -1422,72 (-3051,59; 206,14) | 579.64 | 0.102 | ||
| Obese grade I | Underweight | -1036,11 (-2669,96; 597,74) | 581.42 | 0.384 | |
| Normal weight | -537,15 (-1687,22; 612,92) | 409.26 | 0.683 | ||
| Overweight | 142,1 (-1049,82; 1334,02) | 424.15 | 0.997 | ||
| Obese grade II/III | -1280,62 (-3089,49; 528,24) | 643.7 | 0.271 | ||
| Obese grade II/III | Underweight | 244,51 (-1730,84; 2219,86) | 702.94 | 0.997 | |
| Normal weight | 743,47 (-855,02; 2341,97) | 568.84 | 0.687 | ||
| Overweight | 1422,72 (-206,14; 3051,59) | 579.64 | 0.102 | ||
| Obese grade I | 1280,62 (-528,24; 3089,49) | 643.7 | 0.271 | ||
| Band neutrophils | Underweight | Normal weight | 75,96 (-48,73; 200,65) | 44.37 | 0.427 |
| Overweight | 105,63 (-22,15; 233,41) | 45.47 | 0.138 | ||
| Obese grade I | 140,73 (-5,06; 286,52) | 51.88 | 0.052 | ||
| Obese grade II/III | 66,52 (-109,75; 242,78) | 62.72 | 0.827 | ||
| Normal weight | Underweight | -75,96 (-200,65; 48,73) | 44.37 | 0.427 | |
| Overweight | 29,67 (-45,19; 104,54) | 26.64 | 0.799 | ||
| Obese grade I | 64,77 (-37,85; 167,39) | 36.52 | 0.389 | ||
| Obese grade II/III | -9,44 (-152,08; 133,19) | 50.76 | 1 | ||
| Overweight | Underweight | -105,63 (-233,41; 22,15) | 45.47 | 0.138 | |
| Normal weight | -29,67 (-104,54; 45,19) | 26.64 | 0.799 | ||
| Obese grade I | 35,1 (-71,26; 141,45) | 37.85 | 0.886 | ||
| Obese grade II/III | -39,12 (-184,46; 106,23) | 51.72 | 0.943 | ||
| Obese grade I | Underweight | -140,73 (-286,52; 5,06) | 51.88 | 0.052 | |
| Normal weight | -64,77 (-167,39; 37,85) | 36.52 | 0.389 | ||
| Overweight | -35,1 (-141,45; 71,26) | 37.85 | 0.886 | ||
| Obese grade II/III | -74,21 (-235,62; 87,19) | 57.44 | 0.696 | ||
| Obese grade II/III | Underweight | -66,52 (-242,78; 109,75) | 62.72 | 0.827 | |
| Normal weight | 9,44 (-133,19; 152,08) | 50.76 | 1 | ||
| Overweight | 39,12 (-106,23; 184,46) | 51.72 | 0.943 | ||
| Obese grade I | 74,21 (-87,19; 235,62) | 57.44 | 0.696 | ||
| Lymphocytes | Underweight | Normal weight | -28,93 (-2185,57; 2127,71) | 767.45 | 1 |
| Overweight | -796,2 (-3006,3; 1413,9) | 786.48 | 0.85 | ||
| Obese grade I | -360,33 (-2881,92; 2161,25) | 897.32 | 0.995 | ||
| Obese grade II/III | -274,81 (-3323,44; 2773,83) | 1084.88 | 0.999 | ||
| Normal weight | Underweight | 28,93 (-2127,71; 2185,57) | 767.45 | 1 | |
| Overweight | -767,27 (-2062,09; 527,56) | 460.77 | 0.456 | ||
| Obese grade I | -331,4 (-2106,35; 1443,55) | 631.63 | 0.985 | ||
| Obese grade II/III | -245,88 (-2712,9; 2221,15) | 877.91 | 0.999 | ||
| Overweight | Underweight | 796,2 (-1413,9; 3006,3) | 786.48 | 0.85 | |
| Normal weight | 767,27 (-527,56; 2062,09) | 460.77 | 0.456 | ||
| Obese grade I | 435,87 (-1403,67; 2275,4) | 654.61 | 0.964 | ||
| Obese grade II/III | 521,39 (-1992,5; 3035,29) | 894.59 | 0.978 | ||
| Obese grade I | Underweight | 360,33 (-2161,25; 2881,92) | 897.32 | 0.995 | |
| Normal weight | 331,4 (-1443,55; 2106,35) | 631.63 | 0.985 | ||
| Overweight | -435,87 (-2275,4; 1403,67) | 654.61 | 0.964 | ||
| Obese grade II/III | 85,53 (-2706,16; 2877,22) | 993.44 | 1 | ||
| Obese grade II/III | Underweight | 274,81 (-2773,83; 3323,44) | 1084.88 | 0.999 | |
| Normal weight | 245,88 (-2221,15; 2712,9) | 877.91 | 0.999 | ||
| Overweight | -521,39 (-3035,29; 1992,5) | 894.59 | 0.978 | ||
| Obese grade I | -85,53 (-2877,22; 2706,16) | 993.44 | 1 | ||
| Atypical lymphocytes | Underweight | Normal weight | -4,12 (-46,25; 38,01) | 14.99 | 0.999 |
| Overweight | -3,93 (-47,11; 39,25) | 15.37 | 0.999 | ||
| Obese grade I | -33,62 (-82,87; 15,64) | 17.53 | 0.308 | ||
| Obese grade II/III | 0,12 (-59,43; 59,67) | 21.19 | 1 | ||
| Normal weight | Underweight | 4,12 (-38,01; 46,25) | 14.99 | 0.999 | |
| Overweight | 0,19 (-25,12; 25,51) | 9.01 | 1 | ||
| Obese grade I | -29,5 (-64,17; 5,18) | 12.34 | 0.118 | ||
| Obese grade II/III | 4,24 (-43,95; 52,43) | 17.15 | 0.999 | ||
| Overweight | Underweight | 3,93 (-39,25; 47,11) | 15.37 | 0.999 | |
| Normal weight | -0,19 (-25,51; 25,12) | 9.01 | 1 | ||
| Obese grade I | -29,69 (-65,63; 6,25) | 12.79 | 0.138 | ||
| Obese grade II/III | 4,05 (-45,07; 53,16) | 17.48 | 0.999 | ||
| Obese grade I | Underweight | 33,62 (-15,64; 82,87) | 17.53 | 0.308 | |
| Normal weight | 29,5 (-5,18; 64,17) | 12.34 | 0.118 | ||
| Overweight | 29,69 (-6,25; 65,63) | 12.79 | 0.138 | ||
| Obese grade II/III | 33,74 (-20,8; 88,27) | 19.41 | 0.41 | ||
| Obese grade II/III | Underweight | -0,12 (-59,67; 59,43) | 21.19 | 1 | |
| Normal weight | -4,24 (-52,43; 43,95) | 17.15 | 0.999 | ||
| Overweight | -4,05 (-53,16; 45,07) | 17.48 | 0.999 | ||
| Obese grade I | -33,74 (-88,27; 20,8) | 19.41 | 0.41 | ||
| Monocytes | Underweight | Normal weight | -47,81 (-142,96; 47,33) | 33.86 | 0.62 |
| Overweight | -16,02 (-113,52; 81,48) | 34.7 | 0.991 | ||
| Obese grade I | -40,29 (-151,53; 70,96) | 39.59 | 0.847 | ||
| Obese grade II/III | -96,22 (-230,71; 38,28) | 47.86 | 0.261 | ||
| Normal weight | Underweight | 47,81 (-47,33; 142,96) | 33.86 | 0.62 | |
| Overweight | 31,8 (-25,33; 88,92) | 20.33 | 0.521 | ||
| Obese grade I | 7,53 (-70,77; 85,83) | 27.86 | 0.999 | ||
| Obese grade II/III | -48,4 (-157,24; 60,43) | 38.73 | 0.722 | ||
| Overweight | Underweight | 16,02 (-81,48; 113,52) | 34.7 | 0.991 | |
| Normal weight | -31,8 (-88,92; 25,33) | 20.33 | 0.521 | ||
| Obese grade I | -24,27 (-105,42; 56,89) | 28.88 | 0.918 | ||
| Obese grade II/III | -80,2 (-191,1; 30,7) | 39.47 | 0.251 | ||
| Obese grade I | Underweight | 40,29 (-70,96; 151,53) | 39.59 | 0.847 | |
| Normal weight | -7,53 (-85,83; 70,77) | 27.86 | 0.999 | ||
| Overweight | 24,27 (-56,89; 105,42) | 28.88 | 0.918 | ||
| Obese grade II/III | -55,93 (-179,09; 67,23) | 43.83 | 0.706 | ||
| Obese grade II/III | Underweight | 96,22 (-38,28; 230,71) | 47.86 | 0.261 | |
| Normal weight | 48,4 (-60,43; 157,24) | 38.73 | 0.722 | ||
| Overweight | 80,2 (-30,7; 191,1) | 39.47 | 0.251 | ||
| Obese grade I | 55,93 (-67,23; 179,09) | 43.83 | 0.706 | ||
| Basophils | Underweight | Normal weight | -1,16 (-13,03; 10,71) | 4.22 | 0.999 |
| Overweight | -9 (-21,16; 3,17) | 4.33 | 0.23 | ||
| Obese grade I | -6,38 (-20,26; 7,5) | 4.94 | 0.697 | ||
| Obese grade II/III | -9,9 (-26,68; 6,88) | 5.97 | 0.46 | ||
| Normal weight | Underweight | 1,16 (-10,71; 13,03) | 4.22 | 0.999 | |
| Overweight | -7,84 (-14,96; -0,71) | 2.54 | 0.017 | ||
| Obese grade I | -5,21 (-14,98; 4,56) | 3.48 | 0.563 | ||
| Obese grade II/III | -8,74 (-22,32; 4,84) | 4.83 | 0.369 | ||
| Overweight | Underweight | 9 (-3,17; 21,16) | 4.33 | 0.23 | |
| Normal weight | 7,84 (0,71; 14,96) | 2.54 | 0.017 | ||
| Obese grade I | 2,62 (-7,5; 12,75) | 3.6 | 0.95 | ||
| Obese grade II/III | -0,9 (-14,74; 12,94) | 4.92 | 1 | ||
| Obese grade I | Underweight | 6,38 (-7,5; 20,26) | 4.94 | 0.697 | |
| Normal weight | 5,21 (-4,56; 14,98) | 3.48 | 0.563 | ||
| Overweight | -2,62 (-12,75; 7,5) | 3.6 | 0.95 | ||
| Obese grade II/III | -3,53 (-18,89; 11,84) | 5.47 | 0.968 | ||
| Obese grade II/III | Underweight | 9,9 (-6,88; 26,68) | 5.97 | 0.46 | |
| Normal weight | 8,74 (-4,84; 22,32) | 4.83 | 0.369 | ||
| Overweight | 0,9 (-12,94; 14,74) | 4.92 | 1 | ||
| Obese grade I | 3,53 (-11,84; 18,89) | 5.47 | 0.968 | ||
| Eosinophils | Underweight | Normal weight | 42,95 (-17,15; 103,05) | 21.39 | 0.262 |
| Overweight | 35,87 (-25,72; 97,46) | 21.92 | 0.474 | ||
| Obese grade I | 54,64 (-15,63; 124,91) | 25.01 | 0.186 | ||
| Obese grade II/III | 69,19 (-15,77; 154,14) | 30.23 | 0.149 | ||
| Normal weight | Underweight | -42,95 (-103,05; 17,15) | 21.39 | 0.262 | |
| Overweight | -7,08 (-43,16; 29,01) | 12.84 | 0.982 | ||
| Obese grade I | 11,68 (-37,78; 61,15) | 17.6 | 0.964 | ||
| Obese grade II/III | 26,23 (-42,52; 94,98) | 24.47 | 0.821 | ||
| Overweight | Underweight | -35,87 (-97,46; 25,72) | 21.92 | 0.474 | |
| Normal weight | 7,08 (-29,01; 43,16) | 12.84 | 0.982 | ||
| Obese grade I | 18,76 (-32,5; 70,03) | 18.24 | 0.842 | ||
| Obese grade II/III | 33,31 (-36,75; 103,37) | 24.93 | 0.669 | ||
| Obese grade I | Underweight | -54,64 (-124,91; 15,63) | 25.01 | 0.186 | |
| Normal weight | -11,68 (-61,15; 37,78) | 17.6 | 0.964 | ||
| Overweight | -18,76 (-70,03; 32,5) | 18.24 | 0.842 | ||
| Obese grade II/III | 14,55 (-63,25; 92,35) | 27.68 | 0.985 | ||
| Obese grade II/III | Underweight | -69,19 (-154,14; 15,77) | 30.23 | 0.149 | |
| Normal weight | -26,23 (-94,98; 42,52) | 24.47 | 0.821 | ||
| Overweight | -33,31 (-103,37; 36,75) | 24.93 | 0.669 | ||
| Obese grade I | -14,55 (-92,35; 63,25) | 27.68 | 0.985 | ||
| Na | Underweight | Normal weight | 1,47 (-0,28; 3,22) | 0.62 | 0.128 |
| Overweight | 0,47 (-1,32; 2,26) | 0.64 | 0.948 | ||
| Obese grade I | 0,2 (-1,86; 2,25) | 0.73 | 0.999 | ||
| Obese grade II/III | 1,04 (-1,43; 3,51) | 0.88 | 0.761 | ||
| Normal weight | Underweight | -1,47 (-3,22; 0,28) | 0.62 | 0.128 | |
| Overweight | -1 (-2,05; 0,05) | 0.37 | 0.056 | ||
| Obese grade I | -1,27 (-2,72; 0,18) | 0.52 | 0.099 | ||
| Obese grade II/III | -0,43 (-2,42; 1,56) | 0.71 | 0.974 | ||
| Overweight | Underweight | -0,47 (-2,26; 1,32) | 0.64 | 0.948 | |
| Normal weight | 1 (-0,05; 2,05) | 0.37 | 0.056 | ||
| Obese grade I | -0,27 (-1,77; 1,23) | 0.53 | 0.987 | ||
| Obese grade II/III | 0,57 (-1,46; 2,6) | 0.72 | 0.934 | ||
| Obese grade I | Underweight | -0,2 (-2,25; 1,86) | 0.73 | 0.999 | |
| Normal weight | 1,27 (-0,18; 2,72) | 0.52 | 0.099 | ||
| Overweight | 0,27 (-1,23; 1,77) | 0.53 | 0.987 | ||
| Obese grade II/III | 0,84 (-1,42; 3,1) | 0.81 | 0.835 | ||
| Obese grade II/III | Underweight | -1,04 (-3,51; 1,43) | 0.88 | 0.761 | |
| Normal weight | 0,43 (-1,56; 2,42) | 0.71 | 0.974 | ||
| Overweight | -0,57 (-2,6; 1,46) | 0.72 | 0.934 | ||
| Obese grade I | -0,84 (-3,1; 1,42) | 0.81 | 0.835 | ||
| K | Underweight | Normal weight | 0,01 (-0,2; 0,22) | 0.08 | 1 |
| Overweight | 0,05 (-0,17; 0,27) | 0.08 | 0.966 | ||
| Obese grade I | 0,11 (-0,14; 0,36) | 0.09 | 0.707 | ||
| Obese grade II/III | -0,03 (-0,33; 0,27) | 0.11 | 0.998 | ||
| Normal weight | Underweight | -0,01 (-0,22; 0,2) | 0.08 | 1 | |
| Overweight | 0,04 (-0,08; 0,17) | 0.04 | 0.881 | ||
| Obese grade I | 0,1 (-0,07; 0,28) | 0.06 | 0.444 | ||
| Obese grade II/III | -0,04 (-0,28; 0,2) | 0.09 | 0.99 | ||
| Overweight | Underweight | -0,05 (-0,27; 0,17) | 0.08 | 0.966 | |
| Normal weight | -0,04 (-0,17; 0,08) | 0.04 | 0.881 | ||
| Obese grade I | 0,06 (-0,12; 0,24) | 0.06 | 0.869 | ||
| Obese grade II/III | -0,08 (-0,33; 0,16) | 0.09 | 0.879 | ||
| Obese grade I | Underweight | -0,11 (-0,36; 0,14) | 0.09 | 0.707 | |
| Normal weight | -0,1 (-0,28; 0,07) | 0.06 | 0.444 | ||
| Overweight | -0,06 (-0,24; 0,12) | 0.06 | 0.869 | ||
| Obese grade II/III | -0,14 (-0,42; 0,13) | 0.1 | 0.569 | ||
| Obese grade II/III | Underweight | 0,03 (-0,27; 0,33) | 0.11 | 0.998 | |
| Normal weight | 0,04 (-0,2; 0,28) | 0.09 | 0.99 | ||
| Overweight | 0,08 (-0,16; 0,33) | 0.09 | 0.879 | ||
| Obese grade I | 0,14 (-0,13; 0,42) | 0.1 | 0.569 | ||
| C Reactive Protein | Underweight | Normal weight | 5,4 (-11,94; 22,74) | 6.17 | 0.906 |
| Overweight | 17,24 (-0,54; 35,02) | 6.33 | 0.051 | ||
| Obese grade I | 24,29 (4,09; 44,49) | 7.19 | 0.007 | ||
| Obese grade II/III | 23,69 (-1,14; 48,52) | 8.84 | 0.057 | ||
| Normal weight | Underweight | -5,4 (-22,74; 11,94) | 6.17 | 0.906 | |
| Overweight | 11,84 (1,49; 22,19) | 3.68 | 0.012 | ||
| Obese grade I | 18,89 (4,79; 33) | 5.02 | 0.002 | ||
| Obese grade II/III | 18,29 (-1,9; 38,48) | 7.18 | 0.081 | ||
| Overweight | Underweight | -17,24 (-35,02; 0,54) | 6.33 | 0.051 | |
| Normal weight | -11,84 (-22,19; -1,49) | 3.68 | 0.012 | ||
| Obese grade I | 7,05 (-7,59; 21,69) | 5.21 | 0.657 | ||
| Obese grade II/III | 6,45 (-14,12; 27,01) | 7.32 | 0.904 | ||
| Obese grade I | Underweight | -24,29 (-44,49; -4,09) | 7.19 | 0.007 | |
| Normal weight | -18,89 (-33; -4,79) | 5.02 | 0.002 | ||
| Overweight | -7,05 (-21,69; 7,59) | 5.21 | 0.657 | ||
| Obese grade II/III | -0,61 (-23,29; 22,08) | 8.07 | 1 | ||
| Obese grade II/III | Underweight | -23,69 (-48,52; 1,14) | 8.84 | 0.057 | |
| Normal weight | -18,29 (-38,48; 1,9) | 7.18 | 0.081 | ||
| Overweight | -6,45 (-27,01; 14,12) | 7.32 | 0.904 | ||
| Obese grade I | 0,61 (-22,08; 23,29) | 8.07 | 1 |
Bonferroni post hoc analysis was used, after ANOVA, to compare the study variables between each BMI category. In bold are the variables with statistical significance (p < 0.05).
Table 4.
Differences in proportions between each BMI category.
| Variables | Underweight | Normal weight | Overweight | Obese grade I | Obese grade II/III | |
|---|---|---|---|---|---|---|
| Gender | Female | 98a, b (57, 31%) | 438b (47, 92%) | 356b (50, 86%) | 176a, c (64, 71%) | 90c (73, 77%) |
| Male | 73a, b (42, 69%) | 476b (52, 08%) | 344b (49, 14%) | 96a, c (35, 29%) | 32c (26, 23%) | |
| Admission Diagnosis | Cardiovascular | 25a, b (14, 62%) | 152b (16, 63%) | 160a, c (22, 86%) | 81c (29, 78%) | 34a, c (27, 87%) |
| Respiratory | 13a (7, 6%) | 55a (6, 02%) | 40a (5, 71%) | 13a (4, 78%) | 5a (4, 1%) | |
| Neurological | Neurological | 22a (12, 87%) | 171a (18, 71%) | 115a (16, 43%) | 41a (15, 07%) | 11a (9, 02%) |
| Infectious | 57a (33, 33%) | 184b (20, 13%) | 96c (13, 71%) | 30c (11, 03%) | 25a, b, c (20, 49%) | |
| Surgical | 10a (5, 85%) | 141b (15, 43%) | 143b, c (20, 43%) | 65c (23, 9%) | 21b, c (17, 21%) | |
| Other | 44a (25, 73%) | 211a (23, 09%) | 146a (20, 86%) | 42a (15, 44%) | 26a (21, 31%) | |
| Use of VAD | Yes | 21a (12, 28%) | 86a (9, 41%) | 60a (8, 57%) | 27a (9, 93%) | 7a (5, 74%) |
| No | 150a (87, 72%) | 828a (90, 59%) | 640a (91, 43%) | 245a (90, 07%) | 115a (94, 26%) | |
| Use of MV | Yes | 32a (18, 71%) | 157a (17, 18%) | 110a (15, 71%) | 38a (13, 97%) | 10a (8, 2%) |
| No | 139a (81, 29%) | 757a (82, 82%) | 590a (84, 29%) | 234a (86, 03%) | 112a (91, 8%) | |
| Congestive Heart Failure | Yes | 11a (6, 43%) | 59a (6, 46%) | 44a (6, 29%) | 13a (4, 78%) | 5a (4, 1%) |
| No | 160a (93, 57%) | 855a (93, 54%) | 656a (93, 71%) | 259a (95, 22%) | 117a (95, 9%) | |
| Chronic Renal Failure | Yes | 17a (9, 94%) | 119a (13, 02%) | 82a (11, 71%) | 26a (9, 56%) | 7a (5, 74%) |
| No | 154a (90, 06%) | 795a (86, 98%) | 618a (88, 29%) | 246a (90, 44%) | 115a (94, 26%) | |
| Cirrhosis | Yes | 1a (0, 58%) | 9a (0, 98%) | 14a (2%) | 3a (1, 1%) | 1a (0, 82%) |
| No | 170a (99, 42%) | 905a (99, 02%) | 686a (98%) | 269a (98, 9%) | 121a (99, 18%) | |
| Cancer | Yes | 29a, b (16, 96%) | 149b (16, 3%) | 90a, b (12, 86%) | 23a (8, 46%) | 11a, b (9, 02%) |
| No | 142a, b (83, 04%) | 765b (83, 7%) | 610a, b (87, 14%) | 249a (91, 54%) | 111a, b (90, 98%) | |
| Immunodeficient | Yes | 2a (1, 17%) | 17a (1, 86%) | 4a (0, 57%) | 3a (1, 1%) | 1a (0, 82%) |
| No | 169a (98, 83%) | 897a (98, 14%) | 696a (99, 43%) | 269a (98, 9%) | 121a (99, 18%) | |
| Diabetes Mellitus | Yes | 61a (35, 67%) | 315a (34, 46%) | 277a (39, 57%) | 108a (39, 71%) | 56a (45, 9%) |
| No | 110a (64, 33%) | 599a (65, 54%) | 423a (60, 43%) | 164a (60, 29%) | 66a (54, 1%) | |
| Coronary Artery Disease | Yes | 12a, b (7, 02%) | 86b (9, 41%) | 106a (15, 14%) | 23a, b (8, 46%) | 14a, b (11, 48%) |
| No | 159a, b (92, 98%) | 828b (90, 59%) | 594a (84, 86%) | 249a, b (91, 54%) | 108a, b (88, 52%) | |
| Stroke | Yes | 41a (23, 98%) | 157a, b (17, 18%) | 96b (13, 71%) | 35b (12, 87%) | 11b (9, 02%) |
| No | 130a (76, 02%) | 757a, b (82, 82%) | 604b (86, 29%) | 237b (87, 13%) | 111b (90, 98%) | |
| Dementia | Yes | 29a (16, 96%) | 60b (6, 56%) | 25b (3, 57%) | 7b (2, 57%) | 4b (3, 28%) |
| No | 142a (83, 04%) | 854b (93, 44%) | 675b (96, 43%) | 265b (97, 43%) | 118b (96, 72%) | |
| Performance status | Completely independent | 113a (66, 08%) | 778b (85, 12%) | 641c (91, 57%) | 245b, c (90, 07%) | 109b, c (89, 34%) |
| Partially independent | 18a (10, 53%) | 65a (7, 11%) | 39a (5, 57%) | 18a (6, 62%) | 8a (6, 56%) | |
| Fully dependent | 40a (23, 39%) | 71b (7, 77%) | 20c (2, 86%) | 9b, c (3, 31%) | 5b, c (4, 1%) | |
| ICU deaths | Yes | 64a (37, 43%) | 172b (18, 82%) | 76c (10, 86%) | 21c (7, 72%) | 10c (8, 2%) |
| No | 107a (62, 57%) | 742b (81, 18%) | 624c (89, 14%) | 251c (92, 28%) | 112c (91, 8%) | |
| ICU readmission | Yes | 20a, b (11, 7%) | 105b (11, 49%) | 51a (7, 29%) | 14a (5, 15%) | 10a, b (8, 2%) |
| No | 151a, b (88, 3%) | 809b (88, 51%) | 649a (92, 71%) | 258a (94, 85%) | 112a, b (91, 8%) |
Z-test with Bonferroni correction of clinical and epidemiological characteristics between BMI groups. In Bold, variables with significant difference (p < 0.05). Each subscript letter denotes a subset whose columns proportions do not differ significantly from each other.
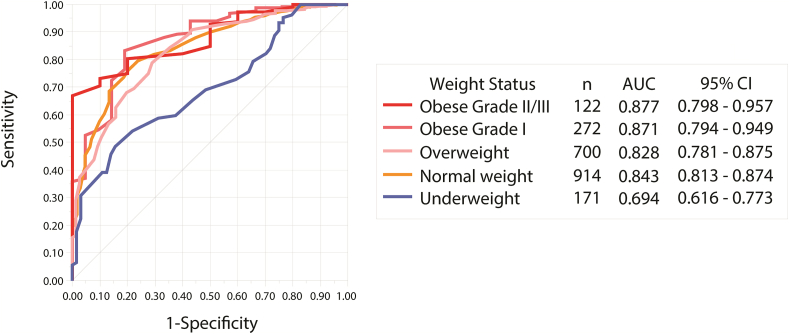
The ability of SAPS3 to predict intra-unit mortality was assessed for each BMI group. Its accuracy was excellent in all groups except in the underweight group, with an AUC of 0.69 (95% CI 0.61–0.77; p < 0.001), reflecting a significantly decreased sensitivity in its performance and Hosmer-Lemeshow goodness of fit test significance of 0.042 (Figure 2). A model including BMI and SAPS3 showed an association of the two variables with mortality, however, with poor goodness-of-fit (Hosmer-Lemeshow p-value: 0.102), suggesting incompleteness of the model (Table 5).
Figure 2.
Performance of SAPS3 Mortality Prediction According to BMI Category. The area under the receiver operating characteristics curve was calculated for each BMI stratum. SAPS3 performance was adequate in all BMI groups except for the underweight group, in which a significantly poor discriminant function was observed. P-value for all curves <0.001.
Table 5.
Binary logistic regression of BMI and SAPS3 association with mortality.
| Parameters | B | S.E. | Exp (B) | 95% C.I. for EXP(B) | P-value |
|---|---|---|---|---|---|
| Saps3Points | 0,117 | 0,007 | 1,124 | (1,109–1,14) | 0,0001 |
| BMI | -0,07 | 0,014 | 0,932 | (0,908–0,958) | 0,0001 |
| Constant | -6,036 | 0,514 | 0,002 |
Univariable analysis showed a significantly higher probability of death (OR 3.71; 95% CI 2.65–5.18), for underweight patients, in contrast to overweight, obese, and obese II/III (Figure 3). A binary regression model was performed to assess factors that could confound the assessment of mortality. The highest chance of death persisted in the underweight group, with an OR of 3.50 (95% CI 1.43–8.58, p = 0.006), while the overweight and obese groups were no longer associated with mortality. The need for mechanical ventilation or vasopressors on admission (OR 3.11 [95% CI, 4.90–8.24, p < 0.0001] and OR 2.69 [95% CI, 1.74–4 .18, p < 0.0001], respectively), were the variables that represented the highest independent risk in our model (Figure 3). Greater dependence on performing daily activities was also an independent predictor of mortality in our population (OR: 2.84 [95%CI: 1.76–4.57]). The model presented good fit with a Hosmer-Lemeshow goodness-of-fit p-value of 0.102. No difference was observed between the BMI groups for the use of these supports. Moreover, when evaluated as a continuous variable, the BMI presented statistical significance on both the univariate and multivariate analysis with a decrease of 0.04% in the odds of mortality for each additional 1 kg/m2 (Figure 4).
Figure 3.
Risk assessment model for intra-unit mortality. The white prism represents the OR in the univariate analysis, while the black prism represents the OR after adjustment in the binary logistic regression. The variables that presented statistical significance at the end of the binary logistic regression were represented. CRP (C-reactive protein); K (potassium level); MV (mechanical ventilation); VAD (vasopressor drug).
Figure 4.
Death Probability According to BMI. A modified Kaplan-Meier curve to estimate the probability of death by BMI level. For every 1 additional kg/m2, there is a 0.04% reduction in the probability of death.
4. Discussion
While SAPS3 performed well in the obese, overweight, and normal weight groups, there was a significant lack of accuracy in underweight patients. Similarly, Deliberato et al. demonstrated that the performance of others severity scores was inconsistent across BMI categories [11]. We assume that the clinical differences observed between the groups may impact the performance of the score; therefore, it should be accessed and readjusted.
We found clinically significant differences between the BMI groups in our study that may be compromising SAPS3 predictive performance in patients with low weight. These patients were older and had a higher burden of comorbidities that were independently associated with worse outcomes. Overweight and obese patients had a higher prevalence of diabetes and a lower mean SAPS3 score. The absence of significance between the creatinine values according to BMI groups may be associated with the presence of acute kidney injury at admission in underweight patients, since a lower proportion of lean mass is expected in this group [12]. In earlier studies, even after adjusting for significant comorbidities, low weight showed an association with mortality [13, 14, 15, 16]. However, in the current study, obese and overweight patients showed no protective factors, despite findings on previous research [17, 18, 19].
Studies exploring the effect of BMI on ICU outcomes have reported controversial results. Three meta-analyses have already demonstrated a J-shaped relationship between BMI and mortality, with overweight and moderate obesity being protective when compared to a normal BMI [18, 19]. This remains poorly understood, but some hypotheses are currently being discussed. Obese patients tend to be younger at the time of ICU admission, a population generally at lower risk of mortality [20]. This was evident in our findings with a lower mean age among those with higher BMI. Alternatively, medical staff, anticipating possible risks and complications, may admit obese patients earlier to the ICU in relatively stable condition to initiate aggressive interventions [4]. In support of this hypothesis, obese subjects in our study were admitted with lower SAPS3 and CCI while underweight patients presented higher mean SAPS3 and MFI scores (Table 2), albeit with poor predictive performance. Despite our study was not specifically designed for this purpose, others have suggested that obese individuals have a greater nutritional reserve, thereby offering protection against hypercatabolic states experienced during critical illness as compared to their underweight counterparts [4, 13]. Still, others hypothesize that the adipokine profile in obese patients may modulate and dampen the immunological response to severe acute illness which may be absent in the underweight population [4]. While we did not confirm obesity as a protective factor when adjusting for comorbidities, the mortality risk for underweight critically ill patients found in our study supports prior findings from the developed world [13, 14, 15, 16].
Our study has certain limitations. First, as a single-center study, there may be unmeasured local confounders that could impact the analyses performed. Also, in this study, only variables obtained at admission of patients were considered. The use of BMI as a parameter for obesity diagnosis, while useful at the population level, does not distinguish between lean mass and fat mass, thus being less precise in elderly and muscular individuals [21]. Moreover, BMI may not accurately assess visceral fat, a risk factor for disease independent of total body fat [22]. Future studies using BMI together with accurate methods of assessing body fat are suggested to address this limitation.
5. Conclusion
Overall, the SAPS3 is inaccurate for predicting mortality in critically ill underweight patients, even with this group presenting a greater chance of death. Recalibration of this tool may aid in the clinical management of these patients.
Declarations
Author contribution statement
Isabella B B Ferreira and Rodrigo C Menezes: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Kevan M Akrami: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Nivaldo Filgueiras Filho: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Bruno B Andrade: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Matheus L Otero: Performed the experiments; Wrote the paper.
Thomas A Carmo: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Gabriel A Agareno, Gabriel P Telles and Bruno V B Fahel: Performed the experiments.
María B Arriaga and Kiyoshi F Fukutani: Analyzed and interpreted the data.
Licurgo Pamplona Neto and Sydney Agareno: Contributed reagents, materials, analysis tools or data.
Funding statement
This work was supported by National Institute of Allergy and Infectious Diseases, National Institutes of Health (Intramural Research Program), USA, Universidade do Estado da Bahia (research fellowship), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (finance code 001) and Fundação de Amparo à Pesquisa do Estado da Bahia (research fellowship), Brazil. Bruno Andrade is a senior scientist from the Brazilian National Council for Scientific and Technological Development (CNPq), Brazil. The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors thank those who contributed directly or indirectly to the construction of this article, research groups GEMINI, linked to the Núcleo de Ensino e Pesquisa do Hospital da Cidade, and MONSTER, linked to the Osvaldo Cruz Foundation.
References
- 1.Haniffa R., Isaam I., De Silva A.P., Dondorp A.M., De Keizer N.F. Performance of critical care prognostic scoring systems in low and middle-income countries: a systematic review. Crit. Care. 2018 Dec 26;22(1):18. doi: 10.1186/s13054-017-1930-8. https://ccforum.biomedcentral.com/articles/10.1186/s13054-017-1930-8 [Internet]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Fact Sheets; 2018. Obesity and Overweigh.https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Internet]; Available from: [Google Scholar]
- 3.Saúde M da. G. Estatística e Informação em Saúde; 2019. Vigitel Brasil 2018: Vigilância de fatores de risco e proteção para doenças crônicas por inquerito telefônico; p. 131.http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2011_fatores_risco_doencas_cronicas.pdf [Internet]; Available from: [Google Scholar]
- 4.Marques M.B., Langouche L. Endocrine, metabolic, and morphologic alterations of adipose tissue during critical illness. Crit. Care Med. 2013 Jan;41(1):317–325. doi: 10.1097/CCM.0b013e318265f21c. http://journals.lww.com/00003246-201301000-00031 [Internet]; Available from: [DOI] [PubMed] [Google Scholar]
- 5.Popkin B.M., Corvalan C., Grummer-Strawn L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020 Jan;395(10217):65–74. doi: 10.1016/S0140-6736(19)32497-3. https://linkinghub.elsevier.com/retrieve/pii/S0140673619324973 [Internet]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wells J.C., Sawaya A.L., Wibaek R., Mwangome M., Poullas M.S., Yajnik C.S., et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88. doi: 10.1016/S0140-6736(19)32472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagai M., Kuriyama S., Kakizaki M., Ohmori-Matsuda K., Sone T., Hozawa A., et al. Impact of obesity, overweight and underweight on life expectancy and lifetime medical expenditures: the Ohsaki Cohort Study. BMJ Open. 2012 May;2(3) doi: 10.1136/bmjopen-2012-000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metnitz P.G.H., Moreno R.P., Almeida E., Jordan B., Bauer P., Campos R.A., et al. SAPS 3—from evaluation of the patient to evaluation of the intensive care unit. Part 1: objectives, methods and cohort description. Intensive Care Med. 2005 Oct 17;31(10):1336–1344. doi: 10.1007/s00134-005-2762-6. http://link.springer.com/10.1007/s00134-005-2762-6 [Internet]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farhat J.S., Velanovich V., Falvo A.J., Horst H.M., Swartz A., Patton J.H., et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J. Trauma Acute Care Surg. 2012 Jun;72(6):1526–1531. doi: 10.1097/TA.0b013e3182542fab. [DOI] [PubMed] [Google Scholar]
- 10.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chron. Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 11.Deliberato R.O., Ko S., Komorowski M., Armengol de La Hoz M.A., Frushicheva M.P., Raffa J.D., et al. Severity of illness scores may misclassify critically ill obese patients. Crit. Care Med. 2018 Mar;46(3):394–400. doi: 10.1097/CCM.0000000000002868. [DOI] [PubMed] [Google Scholar]
- 12.Baxmann A.C., Ahmed M.S., Marques N.C., Menon V.B., Pereira A.B., Kirsztajn G.M., et al. Influence of muscle mass and physical activity on serum and urinary creatinine and serum cystatin C. Clin. J. Am. Soc. Nephrol. 2008 Mar;3(2):348–354. doi: 10.2215/CJN.02870707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zampieri F.G., Colombari F. A gradient-boosted model analysis of the impact of body mass index on the short-term outcomes of critically ill medical patients. Rev Bras Ter Intensiva. 2015;27(2):141–148. doi: 10.5935/0103-507X.20150025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sakr Y., Elia C., Mascia L., Barberis B., Cardellino S., Livigni S., et al. Being overweight or obese is associated with decreased mortality in critically ill patients: a retrospective analysis of a large regional Italian multicenter cohort. J. Crit. Care. 2012;27(6):714–721. doi: 10.1016/j.jcrc.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Toft-Petersen A.P., Wulff J., Harrison D.A., Ostermann M., Margarson M., Rowan K.M., et al. Exploring the impact of using measured or estimated values for height and weight on the relationship between BMI and acute hospital mortality. J. Crit. Care. 2018;44:196–202. doi: 10.1016/j.jcrc.2017.11.021. [DOI] [PubMed] [Google Scholar]
- 16.Harris K., Zhou J., Liu X., Hassan E., Badawi O. The obesity paradox is not observed in critically ill patients on early enteral nutrition. Crit. Care Med. 2017 May;45(5):828–834. doi: 10.1097/CCM.0000000000002326. [DOI] [PubMed] [Google Scholar]
- 17.Khalooeifard R., Djafarian K., Safabakhsh M., Rahmani J., Shab-Bidar S. Dose-response meta-analysis of the impact of body mass index on mortality in the intensive care unit. Nutr. Clin. Pract. 2020 Mar doi: 10.1002/ncp.10473. ncp.10473. [DOI] [PubMed] [Google Scholar]
- 18.Akinnusi M.E., Pineda L.A., El Solh A.A. Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit. Care Med. [Internet] 2008 Jan;36(1):151–158. doi: 10.1097/01.CCM.0000297885.60037.6E. http://journals.lww.com/00003246-200801000-00020 Available from: [DOI] [PubMed] [Google Scholar]
- 19.Oliveros H., Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity. 2008 Mar 17;16(3):515–521. doi: 10.1038/oby.2007.102. [Internet] [DOI] [PubMed] [Google Scholar]
- 20.Amundson D.E., Djurkovic S., Matwiyoff G.N. The obesity paradox. Crit. Care Clin. 2010 Oct;26(4):583–596. doi: 10.1016/j.ccc.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 21.Winfield R.D. Caring for the critically ill obese patient. Nutr. Clin. Pract. 2014;29(6):747–750. doi: 10.1177/0884533614553234. [DOI] [PubMed] [Google Scholar]
- 22.Paolini J.-B.M., Mancini J., Genestal M., Gonzalez H., McKay R.E., Samii K., et al. Predictive value of abdominal obesity vs. body mass index for determining risk of intensive care unit mortality. Crit. Care Med. 2010 May;38(5):1308–1314. doi: 10.1097/CCM.0b013e3181d8cd8b. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.